Contraceptive use with breast cancer incidence in Indonesia
Abstract
INTRODUCTION:
Breast cancer is the most common cancer in women worldwide and is a significant threat to public health. This study aims to conduct a systematic review of the relationship between hormonal contraceptive use and breast cancer incidence.
METHODS:
The search was conducted using Google Scholar, Proquest, Pubmed and one Indonesian database, Garuda, using English and Indonesian keywords. The inclusion criteria in this study were the publication year of the last five years, namely 2019–2023, English and Indonesian language, case-control observational research, using the Indonesian population, and full-text access.
RESULTS:
A total of 165 studies were obtained from the Google Scholar database, including 104 studies. The overall multivariate analysis revealed that there was a statistically significant association of hormonal contraception with the incidence of breast cancer with OR values in the range of 2–6.
CONCLUSIONS:
The findings of this systematic study suggest that the use of hormones can contribute to hormonal imbalances that further increase breast cell proliferation and disrupt gene expression, resulting in uncontrolled cell development/cancer. In addition, the findings recommend increasing the number of studies on this topic to obtain more adequate and possibly more diverse information.
1.Introduction
Breast cancer is the most common cancer in women worldwide and is a significant threat to public health [1,2]. It is the most commonly diagnosed cancer, with an estimated 2.26 million cases recorded in 2020 worldwide, and is the leading cause of cancer deaths among women at more than 670,000 deaths. Almost two-thirds of these deaths occur in low- and middle-income countries [3–5].
One of the risk factors that has received considerable attention from researchers is contraceptive use, apart from genetic, environmental, and lifestyle factors [6–8]. Many studies have focused on the effect of contraceptive history on breast cancer incidence with mixed results [9–12]. A number of studies have reported hormonal contraceptives to be associated with an increased risk of breast cancer especially moderate or recent use within the first 5–10 years of use [1,2,11,13–16]. However, this increased risk is relatively smaller [13–15] and may decrease with longer duration of use [1,15] and after discontinuation of use [9,16]. Nonetheless, recent studies have also reported that oral use of hormonal contraceptives for more than four years has been associated with an increased risk of breast cancer [1,11]. Meanwhile, some studies have reported no association of hormonal contraceptives with breast cancer risk [10,12] despite a family history of cancer [10].
The variation in the results of the association of hormonal contraception and breast cancer, along with a systematic review of the results of relevant studies, is important to be carried out again by including the results of studies from the Indonesian population. The incidence of cancer, including breast cancer, in Indonesia is significantly high, with predictions of an increase from year to year. In addition, there is also an increase in contraceptive use in Indonesia, especially hormonal contraceptives [17,18]. A number of studies have also evaluated the association of contraception with breast cancer incidence [17–21]. However, there has been no systematic review of these findings. Therefore, this study aims to conduct a systematic review of the relationship between contraceptive use and breast cancer incidence.
2.Methods
2.1.Search strategy and inclusion criteria
The search was conducted using databases: Google Scholar, Proquest, Pubmed, and one Indonesian database, Garuda, using English and Indonesian keywords. The search used keywords including “hormonal contraception”, “hormonal”, “contraception”, “breast cancer”, and “Indonesian” for English keywords and “hormonal contraception” and “breast cancer” for Indonesian keywords. The inclusion criteria in this study were the publication year of the last five years, namely 2019–2023, English and or Indonesian language, case-control observational research, using the Indonesian population, and full-text access.
2.2.Population
The population in this study focused on breast cancer patients in Indonesia with a history of hormonal contraceptive use.
2.3.Study design
This study only included studies with a case-control analytic observational research design.
2.4.Study selection and data extraction
The article search results using the above keywords will be deposited directly into Mendeley software. Relevant articles will then be carefully read to ensure they meet the inclusion criteria. Two independent reviewers will handle this procedure. Any disagreement will be resolved through discussion. The entire literature selection process can be seen in Fig. 1.
Data extraction includes study characteristics such as title, objective, author, year of publication, study design, sample, contraception, instrument, outcome, strengths, and weaknesses. This process was conducted independently by two authors. A third party will be involved in case of discrepancies between the two.
3.Results
3.1.Journal search
Based on the identification results from a number of databases, 104 studies were obtained from the Google Scholar database, 44 studies from the Proquest database, 11 studies from the Pubmed database, and 6 studies from the Garuda Indonesia database, with a total of 165 studies. A total of 31 studies were excluded due to duplication and other reasons. Furthermore, out of 134 studies, 113 had to be excluded, leaving 21 studies. However, 12 studies from the total were decided not to be taken, leaving 9 studies. Finally, only 5 studies were successfully included in this study.
3.2.Study inclusion characteristics
3.2.1.Study setting
The entire literature was conducted in several locations in Indonesia to investigate the risk factors of contraceptive use history on breast cancer incidence from 2019-2022 (2019: 2 studies and 2022: 3 studies).
3.2.2.Population
All cases were women diagnosed with breast cancer, with controls being women with cancers other than breast cancer [17,22,23] and women who were not currently or ever diagnosed with breast cancer [18,24] with a 1:1 sample ratio. The largest number of samples was 388 people [17], and the least was 88 people [24].
3.2.3.Variables
All studies focused on the effect of hormonal contraceptive variables, including history and duration of use, on breast cancer incidence. Only one study did not specify the type of contraception and duration of use [17]. All information about the independent variables was obtained through questionnaire instruments. The incidence of breast cancer was based on the results of diagnosis and examination.
3.2.4.Outcome
Based on the final multivariate results, all literature stated that there was a significant association of hormonal contraception with breast cancer incidence with OR values in the range of 2–6 (Table 1). A total of three studies reported that the duration of hormonal contraceptive use affected the incidence of breast cancer [18,22,23], while one study stated that there was no effect [24]. Two studies found that history and type of contraceptive use were risk factors for breast cancer incidence [17,24].
Fig. 1.
Prism diagram.
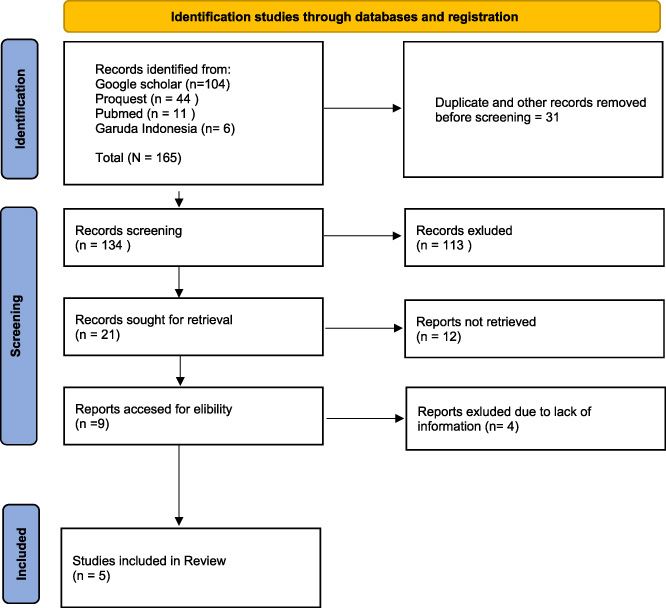
Table 1
Characteristics of inclusion studies
| No | Title | Purpose | Country/Year/Author | Study design | Sample cases and controls | Contraception | Instrument | Outcomes |
| 1 | Influence of hormonal risk factors in breast cancer patients [22] | To determine the influence of hormonal risk factors on breast cancer | Indonesia/2019/ Yenda H. et al. | Case-control | Cases: 147 women with breast cancer Controls: 147 non-breast cancer women Total: 294 people | Type: Pills Duration: ≥5 years <5 years | Questionnaire | There is a significant relationship between the length of use of contraceptive pills and breast cancer. Multivariate results showed that the effect of hormonal contraceptive pills was 3.16 times (p = 0.035). |
| 2 | Analysis of factors associated with the incidence of breast cancer [23] English title: Analysis of Risk Factors Incidence of Breast Cancer in The Foundation of Cancer Indonesia in Bandar Lampung | To find out the risk factors that greatly influence the incidence of breast cancer | Indonesia/2019/Nurhayati et al. | Case-control | Cases: 63 women with breast cancer Controls: 63 women without breast cancer Total: 126 people | Type: Pills, Injections, Implants Duration: ≥5 years <5 years | Questionnaire | There is a very significant effect of a long history of hormonal contraceptive use on the incidence of breast cancer, with an OR value of 6.041 (p = 0.001). The variable long history of contraceptive use was found to have the most significant influence on the incidence of breast cancer. |
| 3 | The relationship between the use of hormonal contraception and the incidence of breast cancer [17] | This research aims to determine the relationship between the use of hormonal contraception and the incidence of breast cancer. | Indonesia/2022/ Sari UM and Khati SA | Case-control | Cases: 194 women with breast cancer Controls: 194 non-breast cancers Total: 388 people | Type: not mentioned Duration: not mentioned | Questionnaire | After controlling for confounding variables, history of contraceptive use was the most influential risk factor for breast cancer incidence (OR=3.784, p < 0.001). |
Table 1 (Continued)
| No | Title | Purpose | Country/Year/Author | Study design | Sample cases and controls | Contraception | Instrument | Outcomes |
| 4 | Breast cancer risk factors: hormonal contraception [18] English title: Risk Factors for Breast Cancer: Hormonal Contraception | To analyze breast cancer risk factors, which are associated with the duration of contraceptive use | Indonesia /2022/ Yuniastini et al. | Case-control | Cases: 150 women diagnosed with breast cancer Control: 150 women not diagnosed with breast cancer Total: 300 people | Type: Pills, injections, implants, IUD. Duration: ≥5 years <5 years | Questionnaire | The results showed that the length of use of hormonal contraceptives affects the incidence of breast cancer (p < 0.001; OR = 4.275). |
| 5 | Risk factors for the use of hormonal contraceptives on the incidence of breast cancer at Bhayangkara Hospital, Makassar [24] English title: Risk Factors for Hormonal Contraceptive Use of Breast Cancer Incidence in RS. Bhayangkara Makassar | To determine the risk factors for using hormonal contraceptives on the incidence of breast cancer | Indonesia /2022/Hatima H. et al. | Case-control | Cases: 44 women with breast cancer Controls: 44 non-breast cancer Total: 88 people | Types of contraception: Progesterone combination Duration: <2 years >2 years | Questionnaire | It was found that the use of progesterone combined with hormonal contraceptives had a 2.793 times risk of developing breast cancer compared to mothers who did not use hormonal contraceptives (p < 0.001). Duration of hormonal contraceptive use is not a significant factor in the incidence of breast cancer. |
4.Discussion
This systematic review was conducted to see the effect of hormonal contraceptive use on the incidence of breast cancer. Based on a review of five literatures [17,18,22–24], it was found that the use of hormonal contraceptives has a significant effect and is a risk factor for breast cancer incidence with a considerable risk. This finding is consistent with previous systematic reviews supported by meta-analysis [2,11,25,26].
The studies in this study defined contraceptive use as a history of ever using or using hormonal contraception, the type of contraception used, and the duration of use. Two studies reported that history of contraceptive use and type of contraceptive used were significant in breast cancer incidence [17,24], while duration of use was found to have no effect in one out of four studies [18,22–24]. It is possible that duration did not affect the reported studies due to the length of contraceptive use, which only ranged from approximately 2 years [24]. Several studies reported that breast cancer risk showed a trend towards increased significance in the duration of hormonal contraceptive use of more than four years and even the first five years or more of use [1,11,15,27,28]. This is in line with the results of studies that report contraceptive use ≥5 years has a greater odds ratio of experiencing breast cancer [18,22,23], compared to those who are only about two years or more [24].
The significant association between hormonal contraceptive use and breast cancer incidence based on history and duration of use may be due to the role of steroids, namely estrogen and progesterone. These studies emphasize that the use of hormonal contraceptives can contribute to hormonal imbalances that further increase breast cell proliferation and disrupt gene expression, resulting in uncontrolled cell development/cancer [17,18,22–24]. In a study by Hatima et al. [24], the type of progesterone combined contraceptive was found to be more risky in developing breast cancer than the duration of use. This is in line with previous studies, which found that exposure to combined hormones can increase the risk of breast cancer [29,30]. The average breast cancer patient involved in this study was in the age range of more than 30 or 50 years, whereas in two studies, it was reported that age ≥50 years was a risk factor for breast cancer in women. The increased use of combined hormonal contraceptives at this age may be associated with menopausal hormone therapy, which is likely to lead to the development of breast cancer [29]. Furthermore, the finding of hormonal contraceptives as a significant risk factor for breast cancer in the last 5 years of studies may also be related to the use of contemporary hormonal contraceptives with diverse formulations (i.e., patterns and compositions) that are currently prescribed. Thus, the potential risk is more significant than with conventional hormonal contraceptives [31].
Although the results of this systematic study found an effect of hormonal contraceptives on breast cancer incidence, the small number of studies included in this study certainly needs to be considered as a limitation. There are very few studies on hormonal contraception and breast cancer in Indonesia. From the Indonesian digital database, only 11 studies were found related to the search keywords, and within the last 5 years, there were only 6 studies. In addition, the significant risk values reported in these studies were due to very small sample sizes, despite multivariate level analysis compared to literature with larger samples [15,28]. In addition, the multivariate analysis model is also likely to affect the difference in risk values. Thus, the risk magnitude reported in these studies still needs further investigation with adequate samples. However, to the best of our knowledge, this study can be considered the first systematic review to focus on hormonal contraceptives and breast cancer in the Indonesian population.
5.Conclusion
The findings of this systematic study suggest a significant effect of hormonal contraceptive use on the incidence of breast cancer in the Indonesian population, especially concerning the history of use, duration, and type of contraceptive used. Duration of use was more commonly reported to be associated with breast cancer incidence. In addition, the findings recommend increasing the number of studies on this topic to obtain more adequate and possibly more diverse information.
Acknowledgements
The author would like to thank all those who have helped study and prepare this manuscript.
Funding
This article review received no external funding.
Ethics committee
Not applicable.
Conflict of interest
The authors declare that this article’s publication has no conflict of interest.
Data availability statement
The data presented in this study are available on request from the corresponding author.
Authors contribution
All authors drafted and reviewed the manuscript; S, P, ANU, MA, MAA, AAM: design of the work, data collection, and data analysis and interpretation; AAM, S., and ANU: design of the work, final approval, and supervision; ANU, MA: data collection, and data analysis and interpretation; MAA.: final approval and supervision; AAM: supervision.
References
[1] | Burchardt NA, , Eliassen AH, , Shafrir AL, , Rosner B, , Tamimi RM, , Kaaks R , Oral contraceptive use by formulation and breast cancer risk by subtype in the Nurses’ Health Study II: A prospective cohort study, Am J Obstet Gynecol [Internet], 226: (6): 821.e1–821.e26, (2022) . Available from: https:// www.ajog.org/article/S0002937821026867/fulltext. |
[2] | Barańska A, , Błaszczuk A, , Kanadys W, , Malm M, , Drop K, , Polz-Dacewicz M, Oral contraceptive use and breast cancer risk assessment: A systematic review and meta-analysis of case-control studies, 2009–2020, Cancers, 13: (22): 5654, (2021) . [Internet]. Nov 12 [cited 2024 Mar 18]. Available from: https://www.mdpi.com/2072-6694/13/22/5654/htm. |
[3] | World Health Organization. Breast cancer [Internet]. 2024 [cited 2024 Mar 18]. Available from: https://www.who.int/news-room/fact-sheets/detail/breast-cancer. |
[4] | Martei YM, , Pace LE, , Brock JE, , Shulman LN, Breast cancer in low- and middle-income countries: Why we need pathology capability to solve this challenge, Clin Lab Med [Internet], 38: (1): 161, (2018) . Mar 1 [cited 2024 Mar 18]. Available from: /pmc/articles/PMC6277976/. |
[5] | Wilkinson L, , Gathani T, Understanding breast cancer as a global health concern, Br J Radiol [Internet], 95: : 1130, (2022) . Feb 2 [cited 2024 Mar 18]. Available from: /pmc/articles/PMC8822551/. |
[6] | Sun YS, , Zhao Z, , Yang ZN, , Xu F, , Lu HJ, , Zhu ZY , Risk factors and preventions of breast cancer, Int J Biol Sci [Internet], 13: (11): 1387, (2017) . [cited 2024 Mar 18].Available from: /pmc/articles/PMC5715522/. |
[7] | Łukasiewicz S, , Czeczelewski M, , Forma A, , Baj J, , Sitarz R, , Stanisławek A, Breast cancer—epidemiology, risk factors, classification, prognostic markers, and current treatment strategies—an updated review, Cancers (Basel) [Internet], 13: (17)(2021) . Sep 1 [cited 2024 Mar 18]. Available from: /pmc/articles/PMC8428369/. |
[8] | Momenimovahed Z, , Salehiniya H, Epidemiological characteristics of and risk factors for breast cancer in the world, Breast Cancer Targets Ther [Internet], 11: : 151–64, (2019) . Apr 10 [cited 2024 Mar 18]. Available from: https://www.dovepress.com/epidemiological-characteristics-of-and-risk-factors-for-breast-cancer-peer-reviewed-fulltext-article-BCTT. |
[9] | Calle EE, , Heath CW, , Miracle-McMahill HL, , Coates RJ, , Liff JM, , Franceschi S , Breast cancer and hormonal contraceptives: Collaborative reanalysis of individual data on 53 297 women with breast cancer and 100 239 women without breast cancer from 54 epidemiological studies, Lancet (London, England) [Internet], 347: (9017): 1713–1727, (1996) . Jun 22 [cited 2024 Mar 18]. Available from: https://pubmed.ncbi.nlm.nih.gov/8656904/. |
[10] | Gaffield ME, , Culwell KR, , Ravi A, Oral contraceptives and family history of breast cancer, Contraception [Internet], 80: (4): 372–380, (2009) . |
[11] | van Weers S, , Hrzic R, , Elands R, Oral contraceptive use and breast cancer risk according to molecular subtypes status: A meta-analysis, Eur J Public Health [Internet], 32: (Supplement 3)(2022) . Oct 21 [cited 2024 Mar 18]. Available from: 10.1093/eurpub/ckac131.208. |
[12] | Samson M, , Porter N, , Orekoya O, , Hebert JR, , Adams SA, , Bennett CL , Progestin and breast cancer risk: A systematic review, Breast Cancer Res Treat [Internet], 155: (1): 3, (2016) . Jan 1 [cited 2024 Mar 18]. Available from: /pmc/articles/PMC4706804/. |
[13] | Fitzpatrick D, , Pirie K, , Reeves G, , Green J, , Beral V, Combined and progestagen-only hormonal contraceptives and breast cancer risk: A UK nested case–control study and meta-analysis, PLOS Med [Internet], 20: (3): e1004188, (2023) . Mar 1 [cited 2024 Mar 18]. Available from: https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1004188. |
[14] | Satish S, , Moore JF, , Littlefield JM, , Bishop IJ, , Rojas KE, Re-evaluating the association between hormonal contraception and breast cancer risk, Breast Cancer (London) [Internet], 15: : 227, (2023) . [cited 2024 Mar 18]. Available from: /pmc/articles/PMC10040158/. |
[15] | Niemeyer Hultstrand J, , Gemzell-Danielsson K, , Kallner HK, , Lindman H, , Wikman P, , Sundström-Poromaa I, Hormonal contraception and risk of breast cancer and breast cancer in situ among Swedish women 15–34 years of age: A nationwide register-based study, Lancet Reg Heal - Eur [Internet], 21: : 100470, (2022) . Oct 1 [cited 2024 Mar 18]. Available from: http://www.thelancet.com/article/S2666776222001661/fulltext. |
[16] | White ND, Hormonal contraception and breast cancer risk, Am J Lifestyle Med [Internet], 12: (3): 224, (2018) . May 1 [cited 2024 Mar 18]. Available from: /pmc/articles/PMC6124967/. |
[17] | Mustika Sari U, , Astuti Khati S, Hubungan Pemakaian Kontrasepsi Hormonal Dengan Kejadian Kanker Payudara, J Kesehat Tambusai [Internet], 3: (2): 145–152, (2022) . Jun 3 [cited 2024 Mar 19]. Available from: http://journal.universitaspahlawan.ac.id/index.php/jkt/article/view/4424. |
[18] | Yuniastini Y, , Murhan A, , Purwati P, , Pratiwi M, Risk factors for breast cancer: hormonal contraception, J Aisyah J Ilmu Kesehat, 7: (S1): 349–354, (2022) . |
[19] | Sulaeman R, , Irwansyah I, , Sukmawati S, , Masadah M, Riwayat penggunaan kontrasepsi hormonal pada penderita kanker payudara, J Keperawatan Terpadu (Integrated Nurs Journal), 3: (1): 10, (2021) . |
[20] | Yunus EM, , Permatasari N, , Yanti ES, Pengaruh penggunaan alat kontrasepsi hormonal terhadap kejadian kanker payudara di fasillitas pelayanan kesehatan, J Kesehat Poltekkes Pangkal Pinang, 9: (2): 143–150, (2021) . |
[21] | Jariah N, , Kurniasari L, Hubungan antara status pernikahan dan penggunaan kontrasepsi hormonal dengan kejadian kanker payudara, Borneo Student Res, 2: (2): 1131–1138, (2021) . |
[22] | Hasnita Y, , Harahap WA, , Defrin D, Pengaruh faktor risiko hormonal pada pasien kanker payudara di RSUP. Dr. M. Djamil Padang, J Kesehat Andalas [Internet], 8: (3): 522–528, (2019) . Available from: http://jurnal.fk.unand.ac.id/index.php/jka/article/view/1037. |
[23] | Nurhayati N, , Arifin Z, , Hardono H, Analisis faktor-faktor yang berhubungan dengan kejadian kanker payudara, Holistik J Kesehat, 13: (2): 175–185, (2019) . |
[24] | Hatima H, , Fitrahminarsih N, Kebidanan Akademi Kebidanan Minasa Upa Makassar J. FAKTOR RISIKO PENGGUNAAN KONTRASEPSI HORMONAL TERHADAP KEJADIANKANKER PAYUDARA DI RS BHAYANGKARA MAKASSAR, J Ris RUMPUN ILMU Kedokt [Internet], 1: (2): 77–93, (2022) . Oct 29 [cited 2024 Mar 21]. Available from: https://prin.or.id/index.php/JURRIKE/article/view/589. |
[25] | Gierisch JM, , Coeytaux RR, , Urrutia RP, , Havrilesky LJ, , Moorman PG, , Lowery WJ , Oral contraceptive use and risk of breast, cervical, colorectal, and endometrial cancers: A systematic review, Cancer Epidemiol Biomarkers Prev [Internet], 22: (11): 1931–1943, (2013) . Nov 1 [cited 2024 Mar 21]. Available from: /cebp/article/22/11/1931/69568/Oral-Contraceptive-Use-and-Risk-of-Breast-Cervical. |
[26] | Torres-de la Roche LA, , Acevedo-Mesa A, , Lizarazo IL, , Devassy R, , Becker S, , Krentel H , Hormonal Contraception and the Risk of Breast Cancer in Women of Reproductive Age: A Meta-Analysis, Cancers (Basel) [Internet], 15: (23)(2023) . Dec 1 [cited 2024 Mar 21]. Available from: /pmc/articles/PMC10705112/. |
[27] | Nur U, , El Reda D, , Hashim D, , Weiderpass E, A prospective investigation of oral contraceptive use and breast cancer mortality: Findings from the Swedish women’s lifestyle and health cohort , BMC Cancer [Internet], 19: (1): 1–9, (2019) . Aug 14 [cited 2024 Mar 21]. Available from: https://bmccancer. biomedcentral.com/articles/10.1186/s12885-019-5985-6. |
[28] | Kanadys W, , Barańska A, , Malm M, , Błaszczuk A, , Polz-Dacewicz M, , Janiszewska M , Use of oral contraceptives as a potential risk factor for breast cancer: A systematic review and meta-analysis of case-control studies up to 2010, Int J Environ Res Public Health [Internet], 18: (9)(2021) . May 1 [cited 2024 Mar 21]. Available from: /pmc/articles/PMC8123798/. |
[29] | Jones ME, , Schoemaker MJ, , Wright L, , Mcfadden E, , Griffin J, , Thomas D , Menopausal hormone therapy and breast cancer: What is the true size of the increased risk? Br J Cancer, 115: (5): 607–615, (2016) . Jul 28 [cited 2024 Mar 22]. Available from: https://www.nature.com/articles/bjc2016231. |
[30] | Beral V, , Reeves G, , Bull D, , Green J, Breast cancer risk in relation to the interval between menopause and starting hormone therapy, JNCI J Natl Cancer Inst [Internet], 103: (4): 296, (2011) . Feb 2 [cited 2024 Mar 22]. Available from: pmc/articles/PMC3039726/. |
[31] | Beaber EF, , Buist DSM, , Barlow WE, , Malone KE, , Reed SD, , Li CI, Recent oral contraceptive use by formulation and breast cancer risk among women 20 to 49 years of age, Cancer Res [Internet], 74: (15): 4078–4089, (2014) . Aug 1 [cited 2024 Mar 22]. Available from: cancerres/article/74/15/4078/592640/Recent-Oral-Contraceptive-Use-by-Formulation-and. |




