Influence of variables on breast self-examination: Potential barrier or enhancement of breast cancer prevention
Abstract
INTRODUCTION:
Breast self-examination (BSE) is an important tool for early detection of breast cancer and can contribute to increased awareness and familiarity with breast tissue. This study aimed to review factors that influenced BSE in preventing breast cancer.
METHODS:
In the initial stage of searching for journal articles, 186 journals were obtained, then screening was carried out within a time span of 2019–2024 and using Indonesian and English 54 journals. Of the 12 journals reviewed, the results showed that 4 journals reviewed had conducted pre and post-BSE practices, and 8 journal reviews conducted BSE practices conducted by students and health workers.
RESULTS:
Several factors play an important role in implementing BSE, namely age, knowledge, history of exposure to information, family history, ethnicity, and attitude. Overall, the study shows that the need to create awareness and educate women, especially rural women, on the importance of BSE as a preventive measure for breast cancer is paramount.
CONCLUSIONS:
Factors influencing the implementation of BSE can be a barrier or an enhancement in breast cancer prevention.
1.Introduction
Breast cancer (BC) develops from breast cells in the inner lining of the milk ducts (ductal carcinoma) or lobules that secrete milk. It appears as a complex, irregular lump or mass in the outer upper quadrant of the breast [1]. This is the most prevalent cause of cancer mortality in women worldwide [2]. BC is economically burdened, causing public health issues [3].
According to Sergiusz et al. (2021), women have a 12% lifetime risk of breast cancer, with individual risk influenced by factors like family history, physical exercise, mutations, obesity, artificial light overexposure, consuming processed foods, breast cancer history, radiation therapy, and other medicines [4].
Timely identification of breast cancer can decrease the incidence of illness and death. Mammography, clinical breast examination (CBE), and breast self-examination (BSE) are recognized as efficient methods for early identification of breast cancer [5]. BSE is an affordable and non-intrusive screening technique for breast cancer that focuses on the patient’s needs. It improves the chances of detecting breast cancer early by recognizing any alterations or irregularities that could suggest its presence [6].
Both the American Cancer Society and the World Health Organization advise that women with an average risk of getting breast cancer should perform monthly breast self-examinations (BSE) in addition to undergoing routine mammograms. Cancer prevention is a crucial element in all cancer control strategies, as it has the potential to prevent 40% of all cancer-related deaths [7]. Although BSE is not a conclusive diagnostic method, it can assist a woman in becoming acquainted with her breast tissue and identifying any alterations that may require additional examination [8].
BSE involves manual and visual inspection. In a mirror, check for swelling, redness, dimpling, puckering, pitting, and nipple inversion. Use the middle finger pad to press each breast and underarm area circularly to provide comprehensive covering. Breast soreness is lower 3--5 days after menstruation, thus BSE should be done then [9]. BSE has been shown to detect breast cancer early. BSE can help young women become breast aware and detect breast cancer early, according to a Turkish study [10]. Another study in Iran revealed that after about 10 years of follow-up, BSE allowed women to find their cancer early [11].
BSE helps detect breast cancer early and raises awareness of breast tissue. Only two-thirds of women want to practice it once a year, and one-third want to do it monthly; nearly half were right. Insufficient BSE education among women is the cause. Its usefulness in lowering breast cancer mortality is still being studied, but it is an important part of breast cancer prevention and detection [12].
The aim of this systematic review aims to summarize Early detection of breast cancer with breast self-examination.
2.Materials and methods
2.1.Methods
Systematic review guidelines and PRISMA were followed. The first stage of the journal article search yielded 186 journals, then 54 journals were found after screening from 2019 to 2024 in Indonesian and English. The literature review subject and study objectives with variables were used to review 11 of these 30 publications.
2.2.Literature search
A thorough literature search was performed with the specified search strategy. This systematic review conducted journal searches across three databases: Google Scholar, Science Direct, and PubMed. The languages employed were English and Indonesian. The most recent search took place in March 2024. The search terms used were “early detection of breast cancer with breast self-examination”, “breast self-examination”, and “early detection”.
2.3.Inclusion criteria
This systematic study included 15–70-year-old women of reproductive age with no cancer history. Open access full-text English and Bahasa Indonesia journals from the last 10 years. Exclusion criteria were cancer in general, cervical cancer, TB cancer, duplicate or overlapping participants, commentaries, editorials, reviews, and no full text. Abstracts were reviewed to identify relevant studies. Full texts were then evaluated for inclusion and deletion. Researchers collected and recorded authors, year of publication, country, study design, sample size, age, length of cancer sickness, therapy type, instruments, and outcomes from the mentioned publications to resolve any doubts.
2.4.Study design
Four of the 11 publications assessed conducted pre- and post-BSE procedures, and seven conducted student and health worker BSE practices. The 5 publications above utilized a prospective study cross-sectional research design, 3 used a descriptive design, and 3 used a pre-post quasi-experimental methodology. Three studies came from Turkey, while others were from Ethiopia, Ghana, Africa, Indonesia, Bangladesh, Jordan, Nepal, and Mexico.
2.5.Study selection
The first stage of the journal article search resulted in 186 journals, and 54 journals were found after screening from 2019 to 2024 in Indonesian and English. Of these, 30 articles matched the topic of the literature review, and 11 articles matched the inclusion requirements in the tabular diagram in Fig. 1, thus becoming the analysed studies.
Fig. 1.
Flow chart.
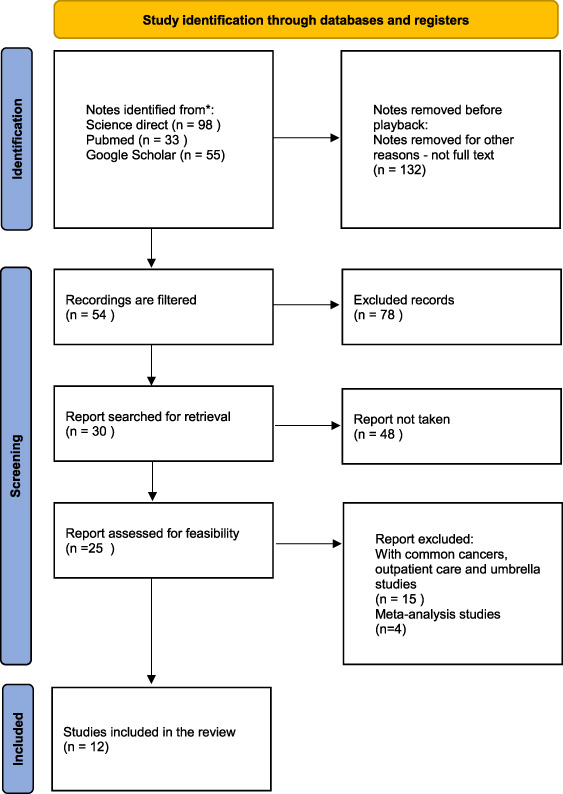
Table 1
xx.
| First Author/ year | Participant age | Participant type | Area | Sample | Result |
| Samuel Derbie Habtegiorgis et al. [13] | 12–65 year old | Health workers and students | Ethiopian | 14.908 | The pooled prevalence for health workers or students was 53% (95% CI: 41, 65), and for others 25% (19, 30). Good knowledge of breast self-examination (AOR: 3.69: 95% CI: 2.70, 5.05), positive attitude toward BCSE (AOR: 2.72: 95% CI: 1.74, 4.24), getting to know people with breast cancer (AOR: 2.77: 95% CI: 1.51, 5.09), family history, and personal history. |
| Rita Dadz et al. [14] | 15–49 years old | Health worker Family member 17 Others | Ghana | 385 | The average age of women was 24.54±7.19. Only 3.1% of women were uneducated, and 58.9% were single. Despite 88.3% awareness of breast cancer, 64.9% had adequate understanding, and only 94 (37.6%) practice BSE. Over 50% of responders could not do BSE. A substantial correlation exists between breast cancer knowledge and BSE practice ( |
| Wubareg Seifu et al. [15] | N/A | N/A | Afrika | 19.228 | In the included studies, 25 (44.64%) were from West Africa, 22 (39.29%) East Africa, 5 (8.93%) North Africa, 3 (5.36%) Central Africa, and 1 (1.79%) South Africa Africans practiced 44.0% (95% CI: 36.63, 51.50) and 17.9% (95% CI: 13.36, 22.94) breast self-examination ever and regularly. Subgroup analysis showed substantial differences between subregions, with West Africa having the most excellent practice (58.87%, 95 CI%: 48.06, 69.27) and South Africa having the lowest (5.33%, 2.73, 10.17). |
| Yohana Azhar et al. [16] | 15–50 years old | Student | Indonesia | N/A | The prevalence of BSE practice in the country was 43.14 percent (95% CI: 36.08–50.20, p < 0.00001 Java has more BSE than non-Java (44.58% versus 41.62%). University students had the most significant BSE prevalence at 49.90%. Good BSE knowledge, attitude, family history, family support, and BC information exposure were statistically linked with BSE practice. |
| Rumpa Sarker et al. [17] | 18–26 years old | Student | Bangladesh | 400 | Significant differences were observed in pre-test versus post-test scores for breast cancer symptoms (2.99±1.05 versus 6.35±1.15; p < 0.001), risk factors (3.35±1.19 versus 7.56±1.04; p¡ 0.001), treatment (1.79±0.90 versus 4.63±0.84), prevention (3.82±1.32 versus 7.14±1.03; p < 0.001), and screening (1.82±0.55 versus 3.98±0.71; p < 0.001). A significant shift in BSE practices was observed between the pre-test and post-test (21.3% versus 33.8%; p < 0.001). |
Table 1 (Continued)
| First Author/ year | Participant age | Participant type | Area | Sample | Result |
| Suhad Ahmad et al. [18] | 20–60 years | High school Diploma Part of Bachelor Bachelor’s degree Higher education | Jordan | 126 | Most participants were married (F = 128, 64%) and averaged 36.18 years old (SD = 10.87). However, 73 people (36.5%) do not practice BSE, 53 (26.5%) aim to do so monthly. The logistic regression model revealed a substantial positive predictive value of confidence for practicing BSE in both the previous year (B = 0.141, p < .001) and this year (B = 0.130, p < .001). |
| Nagihan Küçü Akarsu et al. [19] | 20–69 years | N/A | Turkey | 119 | 81.5 percent of women rarely did BSE. After the post-test, BC, risk factor, and screening knowledge were more accurate. Turkish women showed significant gains in awareness of BC, risk factors, screening, and BSE actions following training (p < 0.001). Effect size (Cohen’s d) measured training efficiency. The training significantly impacted knowledge and ability to perform BSE scores, as Cohen’s d was 1.01, indicating a big effect size. |
| Manisha et al. [20] | 20–49 | Housewife Agriculture Service Business Daily wages/labor Others | Nepal | 262 | One-fourth (27.1%) practiced BSE, and 93.0% did so poorly. Ethnicity from Brahmin/Chhetri, use of contraceptive devices, personal history of breast lump, family history of breast cancer, and knowledge of BSE [AOR = 2.099, 95% CI (1.106–3.981)]. |
| Sahika Simsek-Cetinkaya et al. [20] | N/A | Nursing Students | Turkey | 103 | The standard patient simulation group had the highest total score for breast self-examination skills, with significant differences (p < 0.05). The artificial intelligence-assisted screen-based simulations practice group had greater student satisfaction scores than the regular patient simulation group (p < 0.05). |
| Aysel Ozdemir et al. [21] | N/A | Nursing | Turkey | 72 | Hybrid simulation-based BSE training improved students’ knowledge, application, ability, and pathological evaluation scores compared to conventional training (p < 0.05). Students who used hybrid simulation-based training showed reduced anxiety and increased excitement and motivation (p < 0.05). Students who got hybrid simulation-based training had higher education and counseling scores than those who received classical-based training (p < 0.05). |
Table 1 (Continued)
| First Author/ year | Participant age | Participant type | Area | Sample | Result |
| Dehisy Marisol Juárez-García et al. [22] | 20 years | Mexican women | Mexico | 738 | The exploratory factor analysis yielded 6 components with Cronbach’s alpha scores between 0.65 and 0.84. Age, self-efficacy, obstacles, and health motivation were linked with BSE practice (OR 1.05; CI 1.03–1.07). |
| The Spanish version of the HBMS is competent, valid, and reliable for assessing Mexicans’ breast cancer and BSE beliefs, and it should be applicable to other Spanish-speaking persons. | |||||
| Kibret Asmare et al. [23] | 20–70 years | Wome Gondar town | Northwest Ethiopia | 571 | A 94.7% response rate was achieved, with 541 women from 571 participating in the study. Here, 56%, 46%, and 45.8% of women had acceptable knowledge, positive attitudes, and breast self-examination (BSE). Knowledge, attitudes, and practices toward breast self-examination were significantly associated with women College and above AOR: 3.8 (95% CI: 1.43–10.14), spouses College and above AOR: 3.03 (95% CI: 1.04–8.84), Women College and above AOR: 4.18 (95% CI: 1.59–10.92), history of breast cancer AOR: 6.06 (95% CI: 2.19–16.74), and knowledge level AOR: 2.67. |
3.Discussion
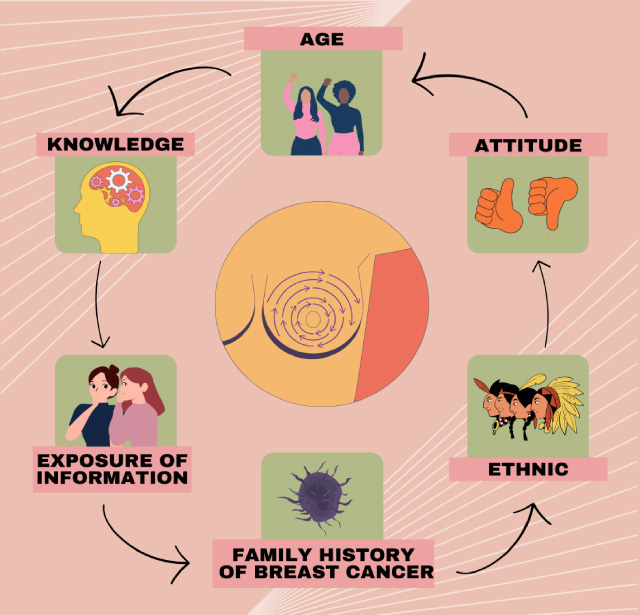
Table 1 shows that certain countries’ BSE understanding is still low. According to the journal review (Fig. 2), several factors influence BSE.
Fig. 2.
Factor influence BSE.
3.1.Age factor
Age can alter women’s knowledge, motivation, and capacity to detect breast cancer early. About 85% of breast cancer cases occur in women over 50, while 5% occur in women under 40 [24]. The majority of Jordanian women aged 20–60 knew about breast cancer and relied on social media for information. However, one-third of individuals did not, and Suhad Ahmad, 2022 claimed inadequate practice in Jordan [18].
Additionally, Manisha (2023) studied. Over half of the 262 women studied had poor health backgrounds. Most had poor breast self-examination knowledge. Low BSE awareness and practice among Nepalese women aged 20–49 were important factors. Age can impact perception and cognition [20].
As people age, they become better at understanding thinking and learning [25]. In middle age, individuals will be more active in society and social life and prepare more for successful adjustment in old age [26]. Intellectual, problem-solving, and verbal abilities are reported to have almost no decline at the age of 20–35 years [27]. Old age affects thinking patterns, but declining understanding power can affect a person’s knowledge and attitude. With good knowledge, women of childbearing age, especially those over 30, can motivate themselves and others to do BSE [28].
3.2.Knowledge
Breast cancer awareness and self-examination are essential for early detection and treatment, which can improve outcomes for women with breast cancer. Educational initiatives for breast cancer awareness in women have been found to increase BSE knowledge and practice [29].
A 2022 Rumpa Sarker research of 400 female college students aged 18–26 demonstrated significant gains in breast cancer and BSE knowledge and awareness after an educational intervention. Study participants’ knowledge of breast cancer symptoms, risk factors, therapy, prevention, screening measures, and the BSE examination process grew considerably from pre-test to post-test. BSE practice also increased pre-test scores by 21.3% and post-test scores by 33.8% [17].
In Indonesia, Yohana, 2023 found a low frequency of 43.14%. Knowledge, attitude, family history, support, and information affect BSE practices. Research reveals that adolescent girls’ BSE knowledge and attitudes are linked. Education has greatly improved BSE understanding and practice. Community-based programs are crucial for breast cancer awareness and detection [16].
In Ghana, 385 women aged 15–49 were assessed for breast self-examination awareness, knowledge, and conduct. Most cancer fatalities globally are from breast cancer, which killed 425,000 people in 2010. With older participants having poorer habits, the study found a strong association between practice and knowledge. BSE is crucial for early breast cancer detection and prevention in childbearing women, according to the study. Women should know breast awareness practices to undertake monthly self-examinations to detect abnormalities [18]. This can lower the risk of serious breast cancer, especially with regular breast awareness. Since breast cancer treatment and recovery are expensive, breast awareness can also improve economic health [14].
A study of 119 Turkish women found that 81.5% did not perform regular breast self-examination. However, correct responses to Breast Cancer, risk factors, and screening increased after training. Significant improvements were seen in post-test scores for knowledge and ability to perform BSE. The study concluded that training benefits women, but regular training is needed to update knowledge and skills, and extended follow-up is required [19].
In conclusion, educational interventions that aim to increase breast cancer awareness and promote the practice among women have been shown to be effective in increasing knowledge and awareness of breast cancer and the practice of BSE. These interventions are critical for early detection and treatment, which can significantly improve outcomes for women diagnosed with breast cancer.
3.3.Exposure of information
Knowledge of breast self-examination (BSE) helps discover breast cancer early, reducing morbidity and mortality. Although health information is more accessible, BSE practice among women is still low; thus, targeted educational interventions are needed to raise awareness and knowledge.
Nagihan Kucu found that 81.5% of women did not frequently perform it, and teaching BSE increased knowledge about breast cancer, risk factors, and screening. A significant teaching effect indicates a particularly effective impact, according to Cohen’s d analysis [19]. Teaching BSE to Turkish women shows that women know little about breast cancer, risk factors, and screening, but teaching BSE can help them learn and improve BSE.
In another Wubareg Seifu Study, Breast self-examination is advised for early breast cancer diagnosis in low-resource nations. Current African breast self-examination studies are inconsistent and unrepresentative. Systematic review and meta-analysis were used to combine research findings. The 56 meta-analyses included 19,228 persons from West, East, North, Central, and South Africa. The combined prevalence of ever and routine breast exams in Africa is 44.0% and 17.9%, respectively. This study indicated that African women rarely self-examine their breasts, necessitating behavior change and communication interventions [15].
These studies demonstrate that job experience, educational status, knowledge, and attitudes drive BSE practice, notwithstanding the need for more targeted educational interventions to raise awareness and knowledge. Health organizations and policymakers could promote BSE among women by raising awareness and considering cultural and self-care factors [30].
3.4.Family history of breast cancer
A family history of breast cancer strongly influences women’s breast self-examination (BSE). A family history of breast cancer makes women six times more likely to perform BSE. This increased practice may lead to early breast cancer diagnosis and treatment due to awareness and a desire to prevent the disease [23].
The study of 571 women indicated that 56% had enough knowledge, 46% had positive attitudes, and 45.8% did BSE. The family history of breast cancer was found to be significantly associated with BSE knowledge, attitudes, and practices, with an odds ratio (AOR) of 6.06, indicating a strong positive relationship [31].
Other studies in Jimma, Addis Ababa, and Libya indicated that women with a family history of breast cancer were more likely to do BSE. Women with a family history of breast cancer are more likely to practice BSE due to a stronger understanding of early diagnosis, a larger sense of urgency to prevent the disease, and a willingness to track the disease. Family members’ proactive health measures [23].
In conclusion, a family history of breast cancer strongly influences BSE in women. BSE is more common in women with a family history of breast cancer, which may improve breast cancer screening and outcomes. This emphasizes the need to educate women about BSE’s benefits and family history’s role in promoting it [32]. A breast cancer history can assist people in comprehending breast cancer by explaining its shapes, sizes, and colors and the elements that affect breast self-examination. A history of breast cancer can affect a person’s exposure to information, interests, attitudes, and recognition in breast self-examination [33].
3.5.Ethnic
Ethnicity can affect women’s health in many ways, so improving access to health services, promoting beneficial traditions and culture, promoting good knowledge and education, and developing community-integrated health programs are important. Due to reasons like cost, distance to health facilities, social and cultural norms, and ethnicity, women in several medium and low-income nations still struggle to access health services [34].
According to Manisha (2023), research can explain why women in Butwal Sub-Metropolitan, Rupandehi, Nepal, undertake breast self-examination (BSE). The survey found that 55.3% of the sample had insufficient BSE knowledge. Only 27.1% of the sample practiced BSE, and 93.0% had inadequate practice. Brahmin/Chhetri women were more likely to recognize and practice BSE than other ethnicities [20].
Breast cancer kills many people worldwide. Jordanian women aged 20–60 were surveyed about breast cancer knowledge and practices. Using Champion’s Health Belief Model Scale, the study found that confidence improved self-breast exams. The findings suggest eliminating cultural barriers and improving health education to promote breast self-examination [18].
These findings highlight the necessity for culturally responsive health education and awareness initiatives customized to ethnic groups’ needs and beliefs to enhance breast cancer screening rates and outcomes [35].
3.6.Attitude
Cultural views, health knowledge, and healthcare availability affect breast self-examination (BSE) attitudes across populations. The discussion about BSE guidelines and their mortality reduction has shifted attention to breast awareness and early detection methods like mammography and clinical breast examination. BSE is still a useful self-care approach, especially for low-income people who may not have access to other screening methods [34].
Self-examination for breast cancer is done by 36% of Ethiopian women and 16% regularly. This study reviewed 34 2011–2020 papers on 14,908 women. Students and health professionals made up 28.35% of participants. The study found that practice was associated with understanding breast self-examination, having a positive attitude toward it, getting to know persons with breast cancer, having a family history, and having a personal experience. Ethiopian women’s breast cancer risk can be reduced by improving awareness, the study says. Results underline the importance of breast cancer treatment and early detection [13].
Sahika Simsek (2023) examined how well undergraduate nursing students learned breast self-examination through standard patient simulation and artificial intelligence-assisted screen-based simulations. The study randomly allocated 103 nursing department students to the simulation or standard patient simulation groups. Despite higher anxiety, the frequent patient simulation group had the best breast self-examination abilities. Normal patient simulation learning taught students how to perform breast self-examinations better, but artificial intelligence-assisted simulation learning made them happier [36].
Aysel Ozdemir (2023) compares hybrid simulation-based and classical-based breast self-examination training for students’ knowledge, abilities, and pathologies. A hybrid simulation-based group was trained on a standardized patient with a wearable breast attachment, and a classical-based group was trained on a breast model, each of which included 36 students. Hybrid simulation-based training improved students’ knowledge, application steps, skills, and pathological evaluation scores. Hybrid simulation-based training reduced anxiety but boosted excitement and motivation. Hybrid simulation-based students scored higher in education and counseling than classical-based students. The study found that hybrid simulation-based training helped students accurately assess breast self-examination knowledge, abilities, and pathology [21].
Dehisy Marisol (2020) examines the psychometric features of the Spanish Health Belief Model Scale (HBMS) for breast self-examination (BSE) in Mexico. BSE practice correlates with age, self-efficacy, obstacles, and health motivation. The Spanish HBMS is valid and accurate for assessing breast cancer and BSE beliefs and should be used by Spanish speakers. Health promotion programs for Mexican women must incorporate perceived barriers, self-efficacy, and health motivation [22].
4.Conclusion
Breast self-examination is crucial for early breast cancer identification and treatment. Several studies have found low breast self-examination awareness and practice among women worldwide. Breast self-examination as a breast cancer prevention tool must be promoted to women, especially rural women.
Acknowledgements
None.
Ethics statement
Not applicable.
Conflict of interest
Each author declares that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangement, etc.) that might pose a conflict of interest in connection with the submitted article.
Data availability statement
The data presented in this study are available on request from the corresponding author.
Funding
This article received no external funding.
Authors contribution
H and ZN study design; H, ANU, and MA databases search and articles selection; All authors participate in the debate and consensus on the articles to be included. H, ANU, and YSB manuscript writing. SS, MA, ANU, and ANU proofreading of the manuscript.
References
[1] | Hanson VF, , El-Kader RGA, , Ilesanmi RE, Practice and barriers of breast self-examination among women in a rural community in South Western, Nigeria, Int J Stud Nurs, 4: (3): 46, (2019) . |
[2] | Oducado RM, New normal in nursing education: Sophomore students’ expectations of and readiness for online learning in the era of COVID-19 pandemic, SSRN Electr J, (2021) . doi:10.2139/ssrn.3765841. |
[3] | Mariotto AB, , Enewold L, , Zhao J, , Zeruto CA, , Robin Yabroff K, Medical care costs associated with cancer survivorship in the United States, Cancer Epidemiol Biomarkers Prev, 29: (7): 1304–1312, (2020) . |
[4] | Stanisławek A, Breast cancer–epidemiology, risk factors, classification, prognostic markers, and current treatment strategies — an updated review, 1–30, 2021. |
[5] | Akhtari-Zavare M, , Juni MH, , Ismail IZ, , Said SM, , Latiff LA, Barriers to breast self examination practice among Malaysian female students: A cross sectional study, Springerplus, 4: (1): 1–6, (2015) . |
[6] | Baloushah S, , Salisu WJ, , Elsous A, , Muhammad Ibrahim M, , Jouda F, , Elmodallal H , Practice and barriers toward breast self-examination among Palestinian women in Gaza City, Palestine, Sci World J, 2020: : 1–7, (2020) . doi:10.1155/2020/7484631. |
[7] | Khatib O. Guidelines for the Early Detection and Screening of Breast Cancer. EMRO Technical Publications Series, 30. . WHO World Health Organization; 1–57. (2006) . |
[8] | American Cancer Society. Breast Cancer Early Detection and Diagnosis American Cancer Society, Am Cancer Soc, 1–55, 2022. |
[9] | Reddy SB, , Acharya JP, Cross-Sectional study on knowledge about breast cancer and breast self examination among female undergraduate students in Telangana, India, J Med Res, 6: (6): 291–294, (2020) . |
[10] | Abou H, , Azayiem Bayumi E, Breast self-examination (BSE): Knowledge and practice among female faculty of physical education in Assuit, South Egypt, An Int Peer-reviewed J, 25: (2011): 1–8, (2016) . |
[11] | Mehiret G, , Molla A, , Tesfaw A, Knowledge on risk factors and practice of early detection methods of breast cancer among graduating students of Debre Tabor University, Northcentral Ethiopia, BMC Womens Health, 22: (1): 1–9, (2022) . |
[12] | Windayanti H, , Adimayanti E, , Siyamti D, Pengetahuan remaja putri tentang pemeriksaan payudara, J Midwifery, 6: (1): 1–7, (2023) . |
[13] | Habtegiorgis SD, , Getahun DS, , Telayneh AT, , Birhanu MY, , Feleke TM, , Mingude AB , Ethiopian women’s breast cancer self-examination practices and associated factors. A systematic review and meta-analysis, Cancer Epidemiol, 78: : 102128, (2022) . |
[14] | Dadzi R, , Adam A, Assessment of knowledge and practice of breast self-examination among reproductive age women in Akatsi South district of Volta region of Ghana, PLoS One, 14: (12): 1–12, (2019) . |
[15] | Seifu W, , Mekonen L, Breast self-examination practice among women in Africa: A systematic review and Meta-analysis, Arch Public Heal, 79: (1): 1–17, (2021) . |
[16] | Azhar Y, , Hanafi RV, , Lestari BW, , Halim FS, Breast self-examination practice and its determinants among women in Indonesia: A systematic review, meta-analysis, and meta-regression, Diagnostics, 13: (15): 2577, (2023) . doi:10.3390/diagnostics13152577. |
[17] | Sarker R, , Islam MS, , Moonajilin MS, , Rahman M, , Gesesew HA, , Ward PR, Effectiveness of educational intervention on breast cancer knowledge and breast self-examination among female university students in Bangladesh: A pre-post quasi-experimental study, BMC Cancer, 22: (1): 1–7, (2022) . |
[18] | Ahmad S, , Alloubani A, , Abu-Sa’da R, , Qutaiba Y, Breast self-examination: Knowledge, practice, and beliefs among females in Jordan, SAGE Open Nurs, 8: : 237796082211245, (2022) . doi:10.1177/23779608221124517. |
[19] | Akarsu NK, , Andsoy II, Evaluation of breast self-examination training in Turkish women living in Northwestern Turkey, J Prev Med Hyg, 63: (1): E76–E82, (2022) . |
[20] | Manisha BK, , Kaphle HP, Breast self-examination: Knowledge, practice and associated factors among 20 to 49 years aged women in Butwal sub-metropolitan, Rupandehi, Nepal, PLoS One, 18: : 1–18, (2023) . |
[21] | Özdemir A, , Ünal E, The effect of breast self-examination training on nursing students by using hybrid-based simulation on knowledge, skills, and ability to correctly evaluate pathological findings: Randomized controlled study, Nurse Educ Pract, 66: : 103530, (2023) . doi:10.1016/j.nepr.2022.103530. |
[22] | Juárez-García DM, , de Jesús García-Solís M, , Téllez A, Adaptation and validation of the health belief model scale for breast self-examination in Mexican women, Value Heal Reg Issues, 23: : 30–36, (2020) . |
[23] | Asmare K, , Birhanu Y, , Wako Z, Knowledge, attitude, practice towards breast self-examination and associated factors among women in Gondar town, Northwest Ethiopia, 2021: A community-based study, BMC Womens Health, 22: (1): 1–14, (2022) . |
[24] | McGuire A, , Brown JAL, , Malone C, , Mclaughlin R, , Kerin MJ, Effects of age on the detection and management of breast cancer, Cancers (Basel), 7: (2): 908–929, (2015) . |
[25] | Hu R, The age factor in second language learning, Theory Pract Lang Stud, 6: (11): 2164, (2016) . |
[26] | Solhi M, , Pirouzeh R, , Zanjari N, Middle-aged preparation for healthy aging: A qualitative study, BMC Public Health, 22: (1): 1–8, (2022) . |
[27] | Murman DL, The impact of age on cognition, Semin Hear, 36: (3): 111–121, (2015) . |
[28] | Delbaere I, , Verbiest S, , Tydén T, Knowledge about the impact of age on fertility: A brief review, Ups J Med Sci, 125: (2): 167–174, (2020) . |
[29] | Khiyali Z, , Aliyan F, , Kashfi SH, , Mansourian M, , Jeihooni AK, Educational intervention on breast self-examination behavior in women referred to health centers: Application of health belief model, Asian Pacific J Cancer Prev, 18: (10): 2833–2838, (2017) . |
[30] | Jadhav BN, , Abdul Azeez EP, , Mathew M, , Senthil Kumar AP, , Snegha MR, , Yuvashree G , Knowledge, attitude, and practice of breast self-examination is associated with general self-care and cultural factors: A study from Tamil Nadu, India, BMC Womens Health, 24: (1): 1–8, (2024) . |
[31] | Mekonnen BD, Breast self-examination practice and associated factors among female healthcare workers in Ethiopia: A systematic review and meta-analysis, PLoS One, 15: : 1–18, (2020) . |
[32] | Kayan S, , Cinar IO, An examination of variables associated with breast cancer early detection behaviors of women, Afr Health Sci, 22: (3): 133–144, (2022) . |
[33] | Karayurt Ö, , Özmen D, , Çetinkaya AÇ, Awareness of breast cancer risk factors and practice of breast self examination among high school students in Turkey, BMC Public Health, 8: : 1–8, (2008) . |
[34] | Armin J, , Torres CH, , Vivian J, , Vergara C, , Shaw SJ, Breast self-examination beliefs and practices, ethnicity, and health literacy: Implications for health education to reduce disparities, Health Educ J, 73: (3): 274–284, (2014) . |
[35] | Nayyar S, , Chakole S, , Taksande AB, , Prasad R, , Munjewar Pratiksha K, , Wanjari MB, From awareness to action: A review of efforts to reduce disparities in breast cancer screening, Cureus(2023) . doi:10.7759/cureus.40674. |
[36] | Simsek-Cetinkaya S, , Cakir SK, Evaluation of the effectiveness of artificial intelligence assisted interactive screen-based simulation in breast self-examination: An innovative approach in nursing students, Nurse Educ Today, 127: : 105857, (2023) . |




