Metaplastic breast cancer masquerading as a recurrent haematoma: A case report
Abstract
An 85-year-old Chinese lady presented with a 5-day history of a painless left breast lump. There was no fever, nipple discharge, or history of trauma. She had a past medical history of atrial fibrillation that was managed with an oral anticoagulant.
Mammography demonstrated a dense mass in the upper outer quadrant of the left breast. Ultrasound showed an irregular, heterogeneous 4.7 cm lesion containing debris and cystic spaces with raised peripheral vascularity at the 2 o’clock position, 3 cm from nipple. No internal vascularity was detected. This was managed as a haematoma and rivaroxaban was withheld. Follow-up imaging 3-weeks later showed persistence of the lesion. Bedside needle aspiration yielded haemoserous fluid with immediate reduction in size of the lesion. However, 2 weeks after aspiration, there was recurrence of the ‘haematoma’.
Multidisciplinary review of the clinical history, examination and imaging was sought, and biopsy of the irregularly thickened areas with vascularity along the periphery of the lesion was recommended. Vacuum-assisted biopsy was performed, and histology returned as metaplastic carcinoma.
A recurring ‘haematoma’ should always prompt a search for a secondary cause, with features such as irregular thickened walls and papillary/nodular components requiring further evaluation with biopsy for histopathological correlation.
1.Introduction
Breast haematomas typically present with a history of trauma, such as seat belt injuries in road traffic accidents. Spontaneous occurrence of breast haematomas is rare, although these have been reported to occur in patients on anticoagulation [1,2]. Breast haematomas are typically managed conservatively unless large or symptomatic, for which percutaneous aspiration may be considered [3].
Historically, there have been a few case reports of breast cancers presenting as recurrent breast haematomas, specifically angio- or carcino-sarcomas [4,5]. According to Roy et al., biopsy of a haematoma should be pursued when there has been resorption of the haematoma and the residual underlying parenchyma demonstrates architectural distortion; or there is persistence of the haematoma despite treatment [1]. Other indeterminate or suspicious features which would prompt subsequent biopsy include thickening or enhancing cyst walls, mural nodularity, or an irregular cyst contour [6].
We present a case of a recurrent predominantly cystic lesion that was initially managed as a haematoma, but was subsequently found to demonstrate suspicious sonographic features that prompted a biopsy which eventually yielded histology of metaplastic breast carcinoma. This case augments our understanding of the management of persistent or recurrent ‘haematomas’ in the breast, with particular consideration for underlying malignancy.
2.Case report
An 85-year-old Chinese female presented with a 5-day history of a painless lump in her left breast. There was no fever, nipple discharge, or history of trauma to the breast. Her relevant past medical history included atrial fibrillation for which she had been long term oral anticoagulation (rivaroxaban). She had no history of breast surgery or intervention.
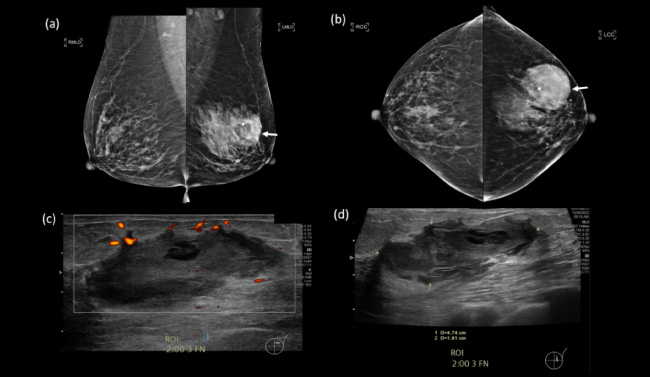
On examination, there was a sizeable palpable mass in the upper outer quadrant of the left breast (Fig. 1). Mammography revealed a high-density mass with rather well-circumscribed margins and no associated calcifications. Ultrasound showed an irregular, heterogeneous lesion with internal debris and cystic spaces at the 2 o’clock position, 3 cm from the nipple, measuring 4.7 × 4.7 × 1.8 cm. There was peripheral vascularity but no demonstrable internal vascularity. This was managed as a haematoma and the patient’s oral anticoagulation was withheld.
Fig. 1.
(a, b) Mediolateral-oblique (MLO) and cranio-caudal (CC) mammographic views of both breasts, with a dense mass in the upper outer quadrant of the left breast (arrows). (c, d) Targeted ultrasound of the left breast showed an irregular cystic lesion with internal debris at the 2 o’clock position, 3 cm from the nipple. Mild peripheral vascularity was noted.
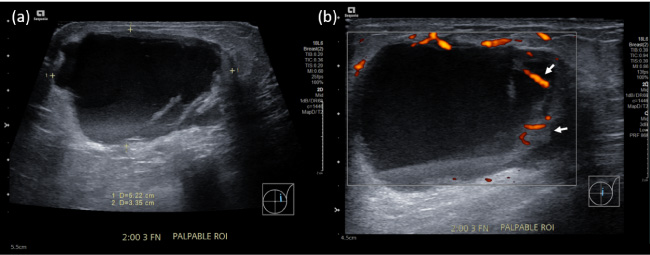
The lesion persisted at a 3-week follow-up and a bedside ultrasound-guided needle aspiration was performed, with immediate reduction in size. The fluid aspirated was purely haemorrhagic and resembled altered blood products. Two weeks after the aspiration, the lesion recurred and now measured 5.4 × 5.2 × 3.4 cm (Fig. 2). The lesion’s irregular margins with associated vascularity were again demonstrated, and new thickened septations were observed. There was also a new discrete nodular component along the periphery with prominent vascularity.
Fig. 2.
(a, b) Recurrence of the lesion two weeks after needle aspiration. Thickened septations with prominent vascularity were clearly demonstrated.
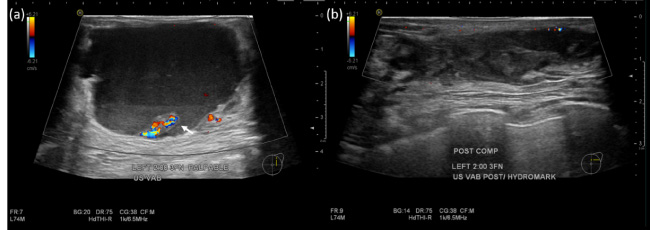
Following a repeat ultrasound-guided aspiration of the haemorrhagic components, a, vacuum-assisted biopsy with a 9-Gauge biopsy device was performed targeting the peripheral nodular component and portions of the walls that appeared more thickened and irregular (Fig. 3).
Fig. 3.
(a) Pre-biopsy ultrasound demonstrating a focal papillary component with prominent vascularity (arrow). (b) Post-biopsy ultrasound showed significant reduction in size of the lesion.
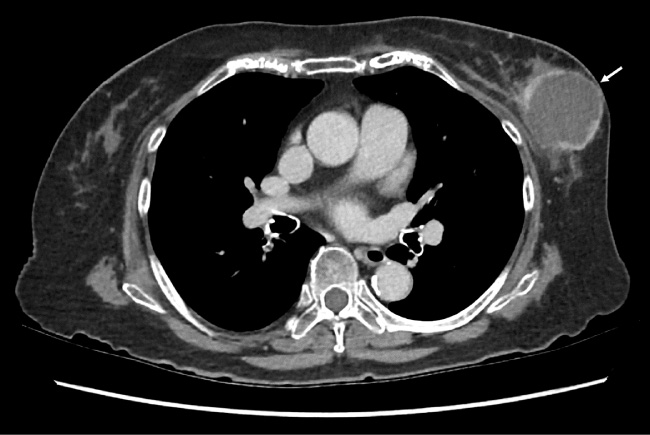
Histology showed numerous pieces of breast tissue extensively involved by tumour, composed predominantly of spindle cell carcinoma and focal squamous cell carcinoma, suggestive of metaplastic carcinoma. Staging computed tomography of the chest, abdomen and pelvis showed a complex solid-cystic lesion in the left breast with thick, nodular, enhancing walls (Fig. 4). There was no evidence of nodal or distant metastasis.
Fig. 4.
Staging CT performed 2 weeks after the biopsy demonstrating recurrence of the lesion in the left breast, with thickened, irregular and enhancing walls (arrow).
The patient subsequently underwent left mastectomy with axillary clearance. Histopathological analysis of the surgical specimen confirmed metaplastic carcinoma with low-to-intermediate grade ductal carcinoma in situ.
3.Discussion
Breast cancer is the most commonly diagnosed cancer in women worldwide, and remains the leading cause of cancer death in women [7], with approximately 2.3 million cases and 685000 deaths in 2020 [8]. The rare subtype of metaplastic breast cancer (MBC), accounts for less than 1% of all breast cancer diagnoses [9], and is a diagnostic challenge due to its variable clinical presentation and low incidence. MBC has been described on mammography to be a high-density mass with variable margins, that is usually round, oval or lobular in shape [10,11]. On ultrasound, it is typically a heterogeneous or hypoechoic solid mass, or a mixed cystic-solid mass [11]. The complex sonographic appearance is usually related to the haemorrhagic or cystic degeneration found on histopathology [12]. This presentation of MBC as a recurrent haemorrhagic lesion is unusual, and to our knowledge has not been documented in the literature.
A review of literature showed that there are higher rates of both local and distant recurrence [10], as well as oestrogen (ER), progesterone (PR) and HER-2 receptor negativity, and tend to have a worse prognosis compared to other triple negative breast cancers. Additionally, there is suggestion that systemic treatment strategies (for example, adjuvant chemotherapy used for adenocarcinoma) may be relatively ineffective for MBC [10,13]. The tempo of metastatic MBC appears to be rapid, with Rayson et al. reporting a median survival of 8 months from the detection of metastatic disease [13], which highlights the need for early detection in this histological subgroup.
While spontaneous breast haematomas may be related to the use of anticoagulants or underlying bleeding diathesis, there is a small proportion of lesions that may be harbouring an occult malignancy. Interval follow-up imaging and clinical review is therefore vital to ensure complete clinical and radiological resolution of the suspected haematoma. A recurring or non-resolving breast ‘haematoma’ should always prompt a search for a secondary cause, with features such as irregular thickened walls and papillary/nodular component (especially if these demonstrate increased vascularity) requiring further evaluation with biopsy for histopathological correlation. In our centre, suspected breast haematomas are evaluated on a case-by-case basis, with the occasional need for a multi-disciplinary team discussion to discuss further management.
Morozova et al also highlights the importance of clear and bidirectional communication between the radiologist and sonographer in the imaging of emergent breast complaints, including that of a haematoma [14]. The importance of real-time scanning must be emphasized as it allows the radiologist to evaluate subtle findings that may not be readily appreciable on static images, such as the differentiation between tiny solid mural nodules and mobile internal debris. Radiologists in our centre routinely have face-to-face discussions with the performing sonographer which provides timely feedback and translates to better patient care.
This case report adds to our knowledge of the different presentations of MBC, as well as the growing evidence that recurrent breast haematomas should be managed with a high index of suspicion, including thorough work up with imaging and histopathological correlation when suspicious imaging features are identified.
Conflict of interest
The authors declares that they have no conflict of interest.
Author contributions
Dr Nicholas Chen Yi Png: Interpretation of data and preparation of the manuscript.
Dr Winfred Xi Tai Goh: Preparation of the manuscript and revision for important intellectual content.
Dr Clement Wenhao Chan: Conception, Supervision and Revision for important intellectual content.
References
[1] | Roy SD, , Scally J, , Troop A, , Selvachandran S, Isolated spontaneous breast haemorrhage in a patient on anticoagulation therapy: Breast biopsy or not? Surg Pract, 9: : 156–158, (2005) . doi:10.1111/j.1744-1633.2005.00273.x. |
[2] | Gani I, , Kapoor R, , Saeed M, Spontaneous breast haematoma after heparin anticoagulation, Eur J Case 7ep Intern Med, 7: (9): 001735, (2020) . doi:10.12890/2020_001735 . PMID: 32908833; PMCID: PMC7473684. |
[3] | Guzmán-Aroca F, , Berná-Serna JD, , García-Ortega AA, , Hernández-Gómez D, , Berná-Mestre JD, A new management technique for symptomatic haematomas following therapeutic vacuum-assisted biopsy, J Clin Med, 8: (9): 1493, (2019) . doi:10.3390/jcm8091493 . PMID: 31546843; PMCID: PMC6780148. |
[4] | Nathan BN, , Sellars NA, , Ebbs SR, Breast haematoma: A rare presentation of breast cancer, The Breast, 1: (3): 135, (1992) . ISSN 0960-9776. doi:10.1016/0960-9776(92)90160-4. |
[5] | Bernathova M, , Jaschke W, , Pechlahner C, , Zelger B, , Bodner G, Primary angiosarcoma of the breast associated Kasabach–Merritt syndrome during pregnancy, Breast, 15: (2): 255–258, (2006) . doi:10.1016/j.breast.2005.04.015 . Epub 2005 Jul 5. PMID: 16000250. |
[6] | Hines N, , Slanetz PJ, , Eisenberg RL, Cystic masses of the breast, AJR Am J Roentgenol, 194: (2): W122–W133, (2010) . doi:10.2214/AJR.09.3688 . PMID: 20093563. |
[7] | Lei S, , Zheng R, , Zhang S, , Wang S, , Chen R, , Sun K , Global patterns of breast cancer incidence and mortality: A population-based cancer registry data analysis from 2000 to 2020, Cancer Commun (Lond), 41: (11): 1183–1194, (2021) . doi:10.1002/cac2.12207 . Epub 2021 Aug 16. PMID: 34399040; PMCID: PMC8626596. |
[8] | Sung H, , Ferlay J, , Siegel RL, , Laversanne M, , Soerjomataram I, , Jemal A , Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries, CA Cancer J Clin, 71: (3): 209–249, (2021) . doi:10.3322/caac.21660 . Epub 2021 Feb 4. PMID: 33538338. |
[9] | Thapa B, , Arobelidze S, , Clark BA, , Xuefei J, , Daw H, , Cheng YC , Metaplastic breast cancer: Characteristics and survival outcomes, Cureus, 14: (8): e28551, (2022) . doi:10.7759/cureus.28551 . PMID: 36185859; PMCID: PMC9517584. |
[10] | Schwartz TL, , Mogal H, , Papageorgiou C, , Veerapong J, , Hsueh EC, Metaplastic breast cancer: Histologic characteristics, prognostic factors and systemic treatment strategies, Exp Hematol Oncol, 2: (1): 31, (2013) . doi:10.1186/2162-3619-2-31 . PMID: 24499560; PMCID: PMC3832232. |
[11] | Yang WT, , Hennessy B, , Broglio K, , Mills C, , Sneige N, , Davis WG , Imaging differences in metaplastic and invasive ductal carcinomas of the breast, AJR Am J Roentgenol, 189: (6): 1288–1293, (2007) . doi:10.2214/AJR.07.2056 . PMID: 18029860. |
[12] | Günhan-Bilgen I, , Memiş A, , Ustün EE, , Zekioglu O, , Ozdemir N, Metaplastic carcinoma of the breast: Clinical, mammographic, and sonographic findings with histopathologic correlation, AJR Am J Roentgenol, 178: (6): 1421–1425, (2002) . doi:10.2214/ajr.178.6.1781421 . PMID: 12034610. |
[13] | Rayson D, , Adjei AA, , Suman VJ, , Wold LE, , Ingle JN, Metaplastic breast cancer: Prognosis and response to systemic therapy, Annals of Oncology, 10: (4): 413–419, (1999) . doi:10.1023/A:1008329910362. |
[14] | Morozova A, , Cotes C, , Aran S, , Singh H, Challenges in interpretation of US breast findings in the emergency setting, Radiographics, 43: (10): e230020, (2023) . doi:10.1148/rg.230020. |




