The role of platelet rich plasma enriched fat graft for correction of deformities after conservative breast surgery
Abstract
BACKGROUND:
Fat transfer has been widely used after breast conservative surgery (BCS) where it aims to recover shapes as a simple, inexpensive, biocompatible method but the technique is not without complications. Platelet Rich Plasma (PRP) is a promising approach to enhance fat graft survival and subsequently improve the outcome. The aim of this study was to evaluate the effect of enriching fat graft with PRP for delayed correction of deformities after conservative surgery for breast cancer regarding esthetic outcome and incidence of complications.
METHODS:
The current study included 50 female patients who were scheduled for delayed lipofilling for correction of deformities after conservative surgery for breast cancer. The studied patients were randomly allocated into 2 groups: Group I (G I) included 25 patients scheduled for PRP enriched lipoinjection and Group II (G II) included 25 patients scheduled for lipoinjection without PRP as a control group.
RESULTS:
Number of sessions of lipoinjection was significantly less in G I in comparison to G II (P = 0.024). During the 2nd session; the amounts of fat injected and harvested were significantly less in G I in comparison to G II (P = 0.049 and 0.001 respectively). Recipient site complications were significantly more evident in G II in comparison to G I (P = 0.01). Surgeon and patient satisfactions were significantly more evident in GI in comparison to G II (P = 0.005 and 0.029 respectively).
CONCLUSION:
The addition of PRP to fat grafts is a simple, cost-effective and safe method to improve esthetic outcome and decrease complications.
1.Introduction
Good body image after surgical management of breast cancer became an integral portion of treatment [1]. Unluckily, even Conservative Breast Therapy (CBT) may result in breast contour distortion which may deteriorate after radiotherapy [2]. The destructive effect of radiotherapy on normal tissues is well documented and stands as an obstacle for any attempt of reconstruction [3,4]. Recently, fat transfer has a significant role for volume replacement even for complete breast reconstruction after mastectomy with good results [5,6]. It is an easy, simple, biocompatible and inexpensive procedure that gave results of a high level of patient satisfaction, thus improving the quality of the patient’s life with natural texture with the plus of removal of undesirable fat from other regions [7,8]. After CBT; fat transfer has been widely used to recover shape, defects, challenging irregularities and asymmetry after surgical approach which subsequently showed a decline in contralateral esthetic surgeries [8–10]. In spite of all of the previously mentioned advantages; fat transfer is not without complications either at the donor site or the recipient site. Chronic pain, edema, scarring, infection and bleeding can occur at the donor site. The recipient site complications include fat necrosis, oil cyst formation and calcifications which can occur due to injection of fat in a poorly vascularized area resulting in failure of graft fat intake [11,12]. To overcome these major drawbacks at recipient site; several studies recommended addition of autologous Platelet Rich Plasma (PRP) to the fat graft to enhance its survival as PRP- which is concentrated plasma obtained from the patient’s own blood that contains high concentrations of platelet compared to whole blood- is rich in angiogenic growth factors which have proliferation-promoting effects which are important for fat graft survival and subsequently decrease fat absorption and complications resulting in improved esthetic outcome [13–15] the aim of this study was to evaluate the effect of enriching fat graft with PRP for delayed correction of deformities after CBT regarding esthetic outcome and incidence of complications.
2.Patients and methods
2.1.Patients’ selection
Fifty female patients who were admitted to the department of Surgery, Medical Research Institute, University of Alexandria Egypt, during the period from June 2018 to May 2021 and were scheduled for delayed lipofilling for correction of defects or deformities after CBT. Lipofilling was approached at least six months after completion of radiotherapy for regeneration of unfortunate effects of radiotherapy (radiodermatitis). The studied patients were randomly allocated into two groups using closed envelope method. This study was a prospective randomized controlled study.
Group I (G I) included 25 patients scheduled for Platelet Rich Plasma (PRP) enriched lipoinjection and Group II (G II) included 25 patients scheduled for lipoinjection without PRP as a control group. Patients who have had inadequate donor sites, those who were on anticoagulant or antiplatelet therapy and smokers were excluded from the current study. Six patients met exclusion criteria and so the number of patients before application of exclusion criteria was 56 patients.
2.2.Ethical considerations
Institutional research Committee approved the protocol before the study started. The study was prospectively explained to patients and written informed consent was obtained before study entry.
2.3.Statistical analysis of the data
Data were fed to the computer and analyzed using IBM SPSS software package version 22.0. (Armonk, NY: IBM Corp). Qualitative data were described using number and percent. Quantitative data were described using range (minimum and maximum), mean, standard deviation and median. The Shapiro- Wilk test was used to verify the normality of distribution. Significance of the obtained results was judged at the 5% level. The mean value of age, size of the lesion, duration of operation, and the time between localization and the start of the operation were calculated and compared across both groups using independent sample T test. Length of incision, pain scores and overall cost of the localization procedure were calculated and compared across both groups using Mann--Whitney U Test. Side of the lesion, site in relation to the breast, preoperative radiological and pathological findings, frozen section and margin status were compared across both groups using chi square test and Fisher exact test.
2.4.Study protocol
All patients included in the current study were subjected to thorough history taking with stressing on previous chemotherapy and radiotherapy, full clinical examination with detailed breast examination, ultrasound and mammography of breasts, routine laboratory investigations and detailed metastatic workup. Patients were examined in the upright standing position. There were preoperative photographs taken to be compared with postoperative ones to assess esthetic outcome. Both donor and recipient sites were marked. Donor areas were the areas where fat is available to a sufficient extent: abdomen , lateral thighs and flanks. Coleman’s technique is the most frequently used technique worldwide. This technique consisted of fat harvesting, fat processing and lipoinjection [1]. Fat harvesting: local infiltration of the donor sites with Klein’s solution containing local anesthetic 10 ml lignocaine+0.25 mg adrenaline in 500 ml Ringer’s solution. Liposuction: by slight negative pressure using a blunt-tipped Coleman’s cannula (2 mm) mounted over a 50 ml Luer Lock syringe. Fat processing: the harvested fat was transferred to a 50-ml Falcon tube ready for centrifugation at 3000 rpm for 3 min the fat was separated into three layers; upper oily layer, middle purified fat and lower blood and debris. Purified fat was transferred into 3- and 1-ml Luer Lock syringes. For Group I patients; PRP preparation was under complete strict aseptic technique. An amount of blood was withdrawn from patient’s peripheral vein in a tube containing sodium citrate anticoagulant. The whole blood was centrifuged at 3000 rpm for 5 min. the supernatant part was called PRP while red blood cells were discarded at the bottom of the tube [16,17]. The PRP obtained was added to the prepared processed fat; we mixed 5 ml of PRP with 50 ml of centrifuged fat tissue (10%) and the mixture was left for 4–5 minutes after good mixing [18]. Fat injection: using a 1-mm lipoinjection needle attached to a 1-ml syringe on withdrawal in a retrograde, radial, multi- layered and multi-diectional technique at the subcutaneous layer and within the glandular defects in both groups [19]. Riggotomy technique was needed in some cases in both groups to dissect adhesions to facilitate injection and formal distribution of injected fat [20]. The skin was closed with non-absorbable simple suture material. Simple dressings and steristrips were used on the grafted area and compressive dressings at the donor site (to prevent hematoma formation). Postoperatively; early wound inspection after 48 hours was done for both donor and recipient sites for any local complications. Esthetic outcome was evaluated in both groups both subjectively and objectively at 3 and 6 months after lipofilling procedure by comparing postoperative photos with preoperative ones by a panel of two surgeons experienced in oncoplastic breast surgery (regarding shape and symmetry) and radiologically by ultrasonography/mammography at 6 months after lipofilling procedure. Patient satisfaction was assessed by Kyungpook National University Hospital (KNUH) breast reconstruction satisfaction questionnaire [15].
3.Results
The current study included 50 female patients who were admitted to the department of Surgery, Medical Research Institute, University of Alexandria, Egypt, during the period from June 2018 to May 2021 and were scheduled for delayed lipofilling for correction of defects or deformities after conservative surgery for breast cancer. The studied patients were randomly allocated into 2 groups: Group I included 25 patients scheduled for PRP enriched lipoinjection to correct the defect or deformity at the site of previous CBS and Group II included 25 patients scheduled for lipoinjection without PRP as a control group. Regarding the distribution of the studied patients based on age and site, side, stage and pathological type of the tumor, type of primary surgical technique and timing of lipofilling after last radiotherapy setting; no significant differences were observed between the two groups as shown in Table 1. Regarding the distribution of studied patients according to lipofilling sessions; number of sessions needed were significantly less in G I in comparison to G II. Three cases only (12%) in G I needed a 2nd session while in G II; ten cases (40%) needed two sessions for correction of deformity with significant difference between the 2 groups (P = 0.024) as shown in Table 2. The amount of blood withdrawn in G1 ranged between 20–60 ml. As regard the amount of fat harvested during both sessions; no significant difference between both groups in the 1st session (P = 0.212) but in the 2nd session; it was significantly less in G I in comparison to G II (P = 0.049) as the defects were minimal in G I after the 1st session in comparison to G II as shown in Table 2. Regarding the amounts of fat needed to be injected during both sessions; no significant difference between both groups in the 1st session (P = 0.327) but in the 2nd session; the injected amounts were significantly less in G I in comparison to G II (P = 0.001) as the defects were minimal after the 1st session as shown in Table 2. According to follow up findings after lipofilling; donor site complications had no significant difference between both groups but recipient site complications were significantly more evident in G II in comparison to G I specifically calcifications, oil cyst and fat necrosis (P = 0.01); Oil cysts after 6 months were present in 4% of (PRP enhanced lipofilling) and 12% in lipofilling without PRP, fat necrosis in 8% and 24% in G I and G II respectively and calcification in 4% and 16 % in G I and G II respectively as shown in Table 3. Regarding surgeon and patient satisfaction; they were significantly more satisfied in G I in comparison to G II). Surgeon satisfaction was mainly good in G I (52%) and in G II; it was mainly fair (48%) with significant difference between the 2 groups (P = 0.005). Similar findings were observed regarding the patient satisfaction as 60% of patients in G I were satisfied while only 36% of patients in G II were satisfied with significant difference (P = 0.029).
Table 1
Clinicopathological criteria before lipoinjection in both groups
| Item | Group I (G I) (n = 25) | Group II (G II) (n = 25) | P-value |
| Age(y) | 0.466 | ||
| Range | 38–52 | 41–51 | |
| Mean ± SD | 44.68 ± 4.19 | 45.44 ± 3.029 | |
| Side | 0.564 | ||
| Right | 14(56%) | 16(64%) | |
| Left | 11(44%) | 9(36%) | |
| Site of primary tumor | 0.927 | ||
| Upper outer quadrant | 11(44%) | 13(52%) | |
| Lower outer quadrant | 3(12%) | 4(16%) | |
| Upper inner quadrant | 3(12%) | 2(8%) | |
| Lower inner quadrant | 3(12%) | 3(12%) | |
| Central | 5(20%) | 3(12%) | |
| Pathology of primary tumor | 0.480 | ||
| IDC | 21(84%) | 19(76%) | |
| ILC | 4(16%) | 6(24%) | |
| Stage | 0.529 | ||
| I | 8(32%) | 6(24%) | |
| II | 17(68%) | 19(76%) | |
| Timing after last radiotherapy setting (months) | 0.305 | ||
| Range | 6–12 | 6–11 | |
| Median | 9 | 8.5 | |
| Mean | 9.08 | 8.58 | |
| Type of primary surgical technique | 0.757 | ||
| Lateral mammoplasty | 8(32%) | 10(40%) | |
| Round block | 3(12%) | 3(12%) | |
| Medial mammoplasty | 4(16%) | 2(8%) | |
| Central quadrantectomy | 3(12%) | 1(4%) | |
| Glandular flaps | 7(28%) | 9(36%) |
Table 2
Distribution of studied patients according to lipofilling Sessions
| Item | Group I (G I) (n = 25) | Group II (G II) (n = 25) | P-value |
| Number of sessions | 0.024 | ||
| 1 | 22(88%) | 15(60%) | |
| 2 | 3(12%) | 10(40%) | |
| Amount of fat harvested per session (ml) | |||
| 1st session | 210–480 | 250–550 | 0.212 |
| Mean | 348.8 | 398.6 | |
| 2nd session | 60–100 | 110–170 | 0.049 |
| Mean | 83.3 | 142 | |
| Amount of pure fat injected per session (ml) | |||
| 1st session | 80–190 | 100–220 | 0.327 |
| Mean | 140.4 | 168.4 | |
| 2nd session | 20–50 | 60–95 | 0.001 |
| Mean | 36.66 | 73.93 |
Table 3
Distribution of studied patients according to follow up findings after lipollifing
| Item | Group I (G I) (n = 25) | Group II (GII) (n = 25) | P-value |
| Donor site complications | 0.736 | ||
| Ecchymosis | 3(12%) | 2(8%) | |
| Altered sensation | 1(4%) | 2(8%) | |
| Haematoma | 2(8%) | 2(8%) | |
| Recipient site complications | 0.01 | ||
| Seroma | 1(4%) | 1(4%) | |
| Infection | 2(8%) | 2(8%) | |
| Ecchymosis | 2(8%) | 1(4%) | |
| Calcifications | 1(4%) | 4(16%) | |
| Oil Cyst | 1(4%) | 3(12%) | |
| Fat necrosis | 2(8%) | 6(24%) | |
| Surgeon satisfaction | 0.005 | ||
| Excellent | 5(20%) | 1(4%) | |
| Good | 13(52%) | 5(20%) | |
| Fair | 6(24%) | 12(48%) | |
| Insufficient | 1(4%) | 7(28%) | |
| Patients’ satisfaction | 0.029 | ||
| Very satisfied | 6(24%) | 2(8%) | |
| Satisfied | 15(60%) | 9(36%) | |
| Unsatisfied | 3(12%) | 9(36%) | |
| Very unsatisfied | 1(4%) | 5(20%) |
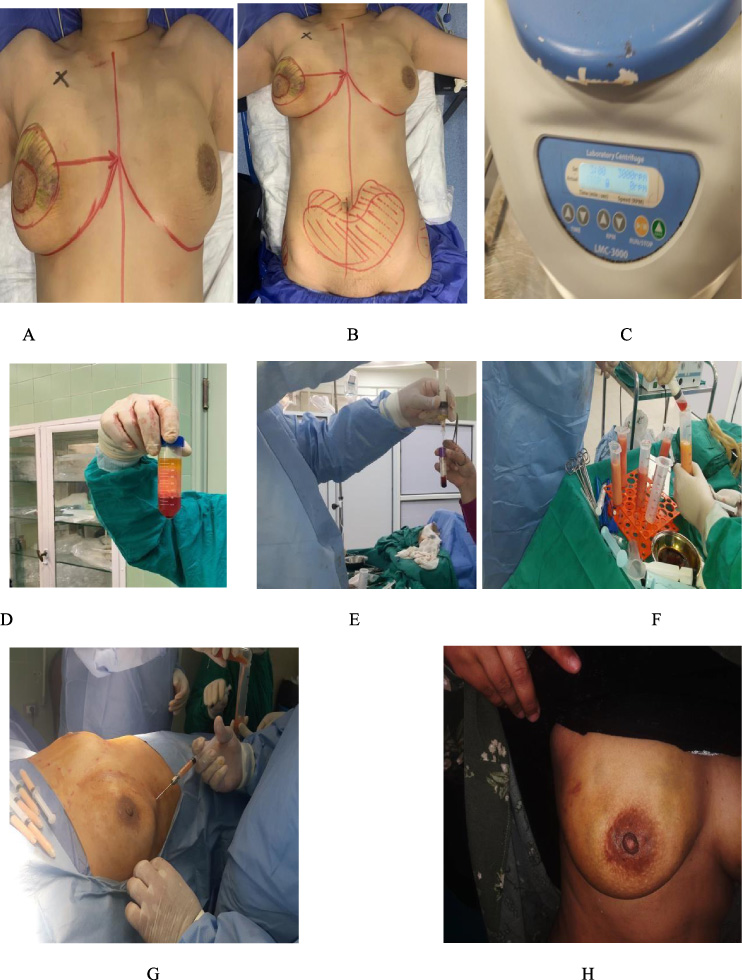
Fig. 1.
(A) 44 years old female patient who had CBT (Round block technique followed by RT), suffered a defect at the site of surgery. (B) Preoperative marking at both donor and recipient sites. (C) Centrifuge. (D) Centrifuged fat is separated into three layers: upper oily layer, middle purified fat and lower blood and debris. (E) Aspiration of upper layer (PRP). (F) Enriching the fat graft by PRP. (G) Injection of PRP enriched fat graft. (H) Six months follow up with satisfactory result after one session.
4.Discussion
The current study investigated the effect of adding PRP to the processed fat for lipofiling in patients who were submitted to CBS and suffered deformities or defects and we concluded that PRP enriched lipofilling can improve the esthetic outcome (surgeon and patient satisfaction) and can decrease local complications (calcification, oil cyst formation and fat necrosis) at the recipient site. Our results are similar to the results of several studies which concluded that PRP can stimulate endothelial cells near their application site, favoring proliferation and formation of new capillaries as PRP is rich in angiogenic growth factors, and inhibit the apoptosis of adipocytes as insufficient neovascularization was the main limitation for fat survival [14,21–23]. In our study; the mean amounts of fat harvested were 348.8 ml in G I and 398.6 ml in G II in the 1st session with no significant difference between both groups while in the 2nd session; it was significantly less (P = 0.049) in G I (83.3 ml) in comparison to G II (142 ml) (P = 0.049). Similar findings were observed regarding the amount of fat injected in both groups (140.4 ml versus 168.4 ml in the 1st session with no significant difference and 36.66 ml versus 73.93 ml in the 2nd session with significant difference between both groups; P = 0.001). Our explanation to the significant decrease in the amount of fat needed to be harvested and injected in the second session in group I was that defects in group I after the 1st session which needed to be corrected by a 2nd session were minimal in comparison to G II in whom the defects were still more manifest and needed larger amount of fat to be injected to be corrected. This was explained in the current study by the effect of PRP as its angiogenic effects decreased the absorption rate of fat and subsequently achieved the greatest benefit from the fat injected in the 1st session and this finding was supported by the fewer number of sessions in G I in comparison to G II (Three cases only (12%) in G I needed a 2nd session while in G II; ten cases (40%) needed two sessions for correction of deformity with significant difference between the 2 groups (P = 0.024). These results were similar to those concluded by many recent studies [24–26] who concluded that supplementation of autologous fat grafts with PRP improved breast soft-tissue defects, compared with centrifuged fat grafting alone. Salgarello et al., [24] treated 100 patients with breast soft tissue defects, applying fat grafting alone to 50 patients and a combination of PRP and fat grafting at a 1:2 ratio (0.5 ml PRP for each 1 ml of fat) to the other 50. After 1 year of follow-up the group treated with PRP obtained a graft maintenance of 69% compared with 39% in the control group (p = 0.0001). In the current study; after enhancement of grafted fat with PRP; the mean rate of reabsorption was significantly less in G I (PRP enhanced fat graft) in comparison to G II (lipofilling without PRP) after 3 and six months; measured subjectively, by the surgeon and patient satisfaction and after 6 months; measured radiologically by U/S mammography. The interval between the sessions was for inter- procedural healing and the maximum volume absorption to occur before subjective assessment. In 2013; Salgarello et al., [24] used ultrasound, magnetic resonance imaging (MRI), and mammography to evaluate the radiologic findings for 24 breasts subjected to lipofilling plus PRP procedures; they found that the average absorption percentage of the injected volume was 15.36% at 6 months and 28.23% at 12 months after the last lipofilling session. In our study; we performed the 2nd session to those patients in whom defects needed more corrections after 6 months from the 1st session after subjective and radiological assessment. According to Salgarello et al. [24]; Oil cysts after12 months were present in 4.5% of (PRP enhanced lipofilling) and 14% in lipofilling without PRP, fat necrosis in 8.5% and 12.5% in G I and G II respectively and calcification in 16% and 20.83% in G I and G II respectively. in our study; Oil cysts after 6 months were present in 4% of (PRP enhanced lipofilling) and 12% in lipofilling without PRP, fat necrosis in 8% and 24% of G I and G II respectively and calcification in 4% and 16% of G I and G II respectively. The similarity between the two studies confirmed our findings regarding the effect of PRP in decreasing the local recipient site complications while the differences in the complication rates may arise from the difference in timing of assessment (12 versus 6 months), the sample size in both studies (50 versus 25 patients in each studied group) and PRP to processed fat ratio (1:2 versus 1:10 ratio). Regarding satisfaction; surgeon satisfaction was evaluated subjectively at 3 and 6 months after lipofilling procedure by comparing postoperative photos with preoperative ones by a panel of two surgeons experienced in oncoplastic breast surgery assessing the shape and symmetry (Excellent, Good, Fair and Insufficient) and radiologically by mammosonography at 6 months after lipo.filling procedure. Patient satisfaction was assessed by (KNUH) breast reconstruction satisfaction questionnaire [15] (Very satisfied, Satisfied, Unsatisfied, very unsatisfied). Surgeon satisfaction was mainly good in G I (52%) and in G II; it was mainly fair (48%) with significant difference between the 2 groups (P = 0.005). Similar findings were observed regarding the patient satisfaction as 60% of patients in G I were satisfied while only 36% of patients in G II were satisfied with significant difference (P = 0.029). These findings were supported by many studies (1,14,27) and were matching with the rest of our findings namely the fewer number of sessions, the lower rate of complications which subsequently reflects the benefit of enriching fat with PRP for lipofilling to correct deformities and defects after CBS. One of the main limitations in evaluating the clinical effect of PRP for enriching fat transfer is the fact that many different protocols have been used for PRP preparation giving probable variations at platelet cellular level [17,28]; needing further evaluation on the count and quality of PRP per ml. Another limitation is the low volume of cases included in the current study so we recommend further studies with larger volume of cases and longer period of follow up for more confirmation of our results and evaluation of the effect of PRP enhanced lipofilling in correcting deformities after different surgeries for breast cancer up to complete mastectomies either for immediate or delayed reconstruction. Also, we recommend the affiliation of a nutritionist to the medical panel to assess the effect of weight changes on the volume of the recipient breast and to advice patients post operatively on a diet to avoid jeopardizing their weight variations. This study was a prospective randomized controlled study which increased strength and validity of results of this research. We thought that ease and low cost of the technique of PRP enriched fat grafting would make it applicable and easily performed in most centers treating breast cancer. The use of fat graft also has the advantage of helping the patient to get ride off excess fat from undesirable sites. thus, improving the body shape and improving quality of life. Workshops, webinars and training programs should be advocated to extrapolate this study to other facilities.
5.Conclusions
Autologous lipoinjection offers ideal biocompatible, inexpensive, readily available and non- migratory soft tissue filler with long term results. However, even with the best technique, the survival rate is still quite variable and unpredictable. The addition of PRP to fat grafts is a simple, cost-effective and safe method to improve esthetic outcome and decrease complications and subsequently achieves both surgeon and patient satisfaction as PRP gives better fat graft survival and decreases the absorption rate. Results of this study should be extrapolated to results of other studies in a big metanalysis involving all studies addressing the use of PRP enriched fat graft for delayed correction of deformities after CBT for breast cancer within the last 10 years.
Conflict of interest
The authors declare no conflict of interest or financial ties to conclude.
References
[1] | Fontdevila J, . Lipofilling in reconstructive surgery: Indications, outcomes, and complications. Regenerative Medicine Procedures for Aesthetic Physicians, . Pinto H, , Fontdevila J (eds), (Cham), Springer; 97–108. (2019) . |
[2] | Debald M, , Pech T, , Kaiser C, , Keyver-Paik M-D, , Walgenbach-Bruenagel G, , Kalff JC , Lipofilling effects after breast cancer surgery in post-radiation patients: An analysis of results and algorithm proposal, Eur J Plast Surg, 40: (5): 447–454, (2017) . |
[3] | Stone HB, , Coleman CN, , Anscher MS , Effects of radiation on normal tissue: Consequences and mechanisms, Lancet Oncol, 4: : 529–536, (2003) . |
[4] | Nelson JA, , Disa JJ, Breast reconstruction and radiation therapy: An update, Plast Reconstr Surg, 140: : 60S–68S, (2017) . |
[5] | Fansa H, , Heitmann C, . Reconstruction using lipofilling/fat grafting. Breast Reconstruction with Autologous Tissue, . Fansa H, , Heitmann C (eds), (New York), Springer; 167–174. (2019) . |
[6] | Brondi RS, , de Oliveira VM, , Bagnoli F, , Mateus EF, , Rinaldi JF, Autologous breast reconstruction with the latissimus dorsi muscle with immediate fat grafting: Long- term results and patient satisfaction, Ann Plast Surg, 82: (2): 152–157, (2019) . |
[7] | Stivala A, , Bertrand B, , Ouar N, , Revol M, , Atlan M, , Cristofari S, Lower rates of lipofilling sessions in latissimus dorsi flap breast reconstruction with initial higher volume transfer by preservation of subfascial fat: A 3D camera-assisted volumetric case series, J Plast Reconstr Aesthet Surg, 73: (4): 681–689, (2020) . |
[8] | Biazus JV, , Stumpf CC, , Melo MP, , Zucatto AE, , Cericatto R, , Cavalheiro JA , Breast- conserving surgery with immediate autologous fat grafting reconstruction: Oncologic outcomes, Aesthetic Plast Surg, 42: (5): 1195–1201, (2018) . |
[9] | Thiessen FE, , Tjalma WA, , Tondu T, Breast reconstruction after breast conservation therapy for breast cancer, Eur J Obstet Gynecol Reprod Biol, 230: : 233–238, (2018) . |
[10] | Khan LR, , Raine CR, , Dixon JM, Immediate lipofilling in breast conserving surgery, Eur J Surg Oncol, 43: (8): 1402–1408, (2017) . |
[11] | Visscher LE, , Cheng M, , Chhaya M, , Hintz ML, , Schantz JT, , Tran P , Breast augmentation and reconstruction from a regenerative medicine point of view: State of the art and future perspectives, Tissue Eng Part B Rev, 23: (3): 281–293, (2017) . |
[12] | Liu W, , Shi K, , Zhu X, , Zhao H, , Zhang H, , Jones A , Adipose tissue-derived stem cells in plastic and reconstructive surgery: A bibliometric study, Aesthetic Plast Surg, 45: (2): 679–689, (2021) . |
[13] | Goddard NV, , Waterhouse N, Regenerative medicine, stem cell therapies, and platelet-rich plasma: where is the evidence? Aesthet Surg J, 40: (4): 460–465, (2020) . |
[14] | Modarressi A, Platlet rich plasma (PRP) improves fat grafting outcomes, World J Plast Surg, 2: (1): 6–13, (2013) . |
[15] | Xiong BJ, , Tan QW, , Chen YJ, , Zhang Y, , Zhang D, , Tang SL , The effects of platelet- rich plasma and adipose-derived stem cells on neovascularization and fat graft survival, Aesthetic Plast Surg, 42: (1): 1–8, (2018) . |
[16] | Croisé B, , Paré A, , Joly A, , Louisy A, , Laure B, , Goga D, Optimized centrifugation preparation of the platelet rich plasma: Literature review, J Stomatol Oral Maxillofac Surg, 121: (2): 150–154, (2020) . |
[17] | Yin W, , Xu H, , Sheng J, , Zhu Z, , Jin D, , Hsu P , Optimization of pure platelet-rich plasma preparation: A comparative study of pure platelet-rich plasma obtained using different centrifugal conditions in a single-donor model, Exp Ther Med, 14: (3): 2060–2070, (2017) . |
[18] | Serra-Mestre JM, , Serra-Renom JM, , Martinez L, , Almadori A, , D’Andrea F, Platelet-rich plasma mixed-fat grafting: A reasonable prosurvival strategy for fat grafts? Aesthetic Plast Surg, 38: (5): 1041–1049, (2014) . |
[19] | Gentile P, , De Angelis B, , Di Pietro V, , Amorosi V, , Scioli MG, , Orlandi A , Gentle is better: The original gentle technique for fat placement in breast lipofilling, J Cutan Aesthet Surg, 11: (3): 120–126, (2018) . |
[20] | Simonacci F, , Bertozzi N, , Grieco MP, , Grignaffini E, , Raposio E, Procedure, applications, and outcomes of autologous fat grafting, Ann Med Surg (Lond), 20: : 49–60, (2017) . |
[21] | Eppley BL, , Pietrzak WS, , Blanton M, Platelet-rich plasma: A review of biology and applications in plastic surgery. Plast Reconstr Surg, 118: (6): 147–159, (2006) . |
[22] | Cervelli V, , Gentile P, , Scioli MG, , Grimaldi M, , Casciani CU, , Spagnoli LG , Application of platelet-rich plasma in plastic surgery: Clinical and in vitro evaluation, Tissue Eng Part C Methods, 15: (4): 625–634, (2009) . |
[23] | Samadi P, , Sheykhhasan M, , Khoshinani HM, The use of platelet-rich plasma in aesthetic and regenerative medicine: A comprehensive review, Aesthetic Plast Surg, 43: (3): 803–814, (2019) . |
[24] | Salgarello M, , Visconti G, , Rusciani A, Breast fat grafting with platelet-rich plasma: A comparative clinical study and current state of the art, Plast Reconstr Surg, 127: (6): 2176–2185, (2011) . |
[25] | Gentile P, , Di Pasquali C, , Bocchini I, , Floris M, , Eleonora T, , Fiaschetti V , Breast reconstruction with autologous fat graft mixed with platelet-rich plasma, Surg Innov, 20: (4): 370–376, (2013) . |
[26] | Cervelli V, , Bocchini I, , Di Pasquali C, , De Angelis B, , Cervelli G, , Curcio CB , P.R.L. platelet rich lipotransfert: Our experience and current state of art in the combined use of fat and PRP, Biomed Res Int, 2013: : 434191, (2013) . |
[27] | Cogliandro A, , Barone M, , Tenna S, , Morelli Coppola M, , Persichetti P, The role of lipofilling after breast reconstruction: Evaluation of outcomes and patient satisfaction with BREAST-Q, Aesthetic Plast Surg, 41: (6): 1325–1331, (2017) . |
[28] | Mazzocca AD, , Mccarthy MB, , Chowaniec DM, , Cote MP, , Romeo AA, , Bradley JP , Platelet-rich plasma differs according to preparation method and human variability, J Bone Joint Surg Am, 94: (4): 308–316, (2012) . |




