HPV-positive cervical squamous cell carcinoma metastasis to the breast, mimicking primary tumor
Abstract
INTRODUCTION:
Metastatic disease to the breast is a rare condition, with contralateral breast metastasis being the most common primary site.
CASE PRESENTATION:
We present the case of a patient who underwent treatment for an HPV positive squamous cell carcinoma (SCC) of the cervix who, during follow-up, complained of a nodule in her left breast. Anatomopathological results indicating squamous carcinoma, which was not able to be differentiated from breast metaplastic carcinoma. Resection of the lesion was carried out, confirming carcinoma with squamous cell differentiation with negativity for GCDFP-15, mammaglobin, p63 and SOX10, but with positivity for p16 and for high risk HPV, confirming a single metastatic lesion of cervical carcinoma.
DISCUSSION/CONCLUSION:
In the presence of SCC in the breast, the differential diagnosis may consider the presence of primary lesion, metaplastic carcinoma with squamous cell differentiation or metastatic disease. The use of markers such as p63, SOX10 and p16, may help for a definitive diagnosis.
1.Introduction
Although primary breast cancer is the most common female cancer worldwide, metastatic breast disease is a rare condition (0.5%–6.6%). It is known that lymphoma, melanoma, soft tissue sarcoma, lung cancer, gastrointestinal, genitourinary and gynecological malignancies (ovary being the main site followed by the cervix) may metastasize to the breast. However, the most common metastasis to the breast comes from the contralateral breast [1].
In the presence of the histological diagnosis of squamous carcinoma (SCC) of the breast, primary metaplastic carcinoma with squamous differentiation, primary SCC of the breast or metastatic tumor shall be considered [2–4]. In most cases, considering only the clinical presentation, it is difficult to distinguish between such conditions, whose management and prognosis are different [5].
2.Case presentation
A 40-year-old patient treated for moderately differentiated cervical SCC of a positive high-risk stage IIB Human Papillomavirus (HPV), with pelvic radiotherapy, high-dose rate - HDR and concomitant chemotherapy (CDPP), presenting complete lesion regression. One year after treatment has completed, in a follow-up consultation, patient complained of a left breast lump, present for four months, with progressive growth. Mammography showed nodulation in the upper-outer quadrant, with high density and irregularity more evident on tomosynthesis. On ultrasonography, a solid, hypoechoic and irregular nodule was observed (Fig. 1), suggesting a primary breast lesion. Systemic staging with tomography and scintigraphy did not show any other disease site.
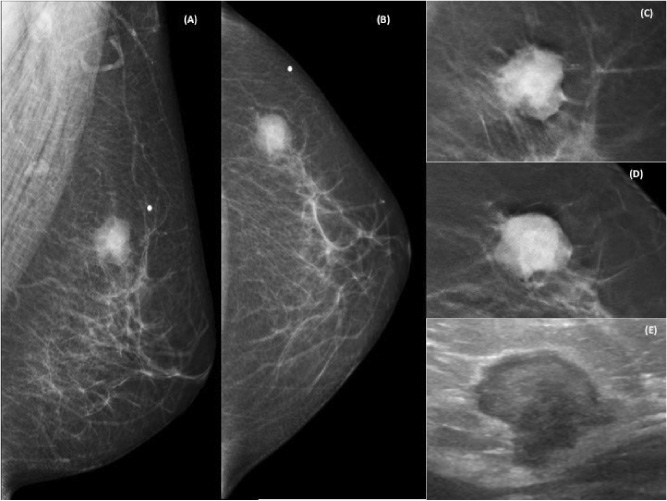
Fig. 1.
Left mammography in oblique mediolateral (a) and craniocaudal (b) views, featuring a high-density nodule, irregularly shaped and indistinct and spiculated margins, best assessed in tomosynthesis (c) and (d), located at the upper-outer quadrant, corresponding to the palpable complaint – BI-RADS® 4C. Ultrasonography (e) shows a nodule of solid, hypoechoic, irregular and angled nature.
Patient underwent core biopsy, which identified a well-differentiated keratinized SCC, Grade 1. The immunohistochemical study showed negativity for GCDFP-15 and mammaglobin, p63, SOX10, focal positivity for GATA-3 and positivity for p16 (DAB). Also estrogen and progesterone receptor and Her-2 were negative. In situ hybridization for high-risk HPV (HPV III Family 16 Probe) was inconclusive, making it impossible to rule out the likelihood of metaplastic carcinoma of the breast and requiring assessment of the entire lesion. Breast segmentectomy and sentinel lymph node biopsy were performed, the result of which was squamous differentiated carcinoma, measuring 2.7 cm, 0/2 lymph nodes. The immunohistochemical evaluation showed positivity for p16 and in situ hybridization for high-risk HPV 16 was positive (B) (Fig. 2). As immunohistochemical evaluation showed positivity for p16 and negativity for p63 and SOX10 (Table 1), it was considered the only metastasis from cervical cancer. Systemic palliative treatment with Carboplatin and Paclitaxel was carried out. At 12 months after breast surgery, the patient is alive, with no active oncological disease.
Fig. 2.
Histology - (a) invasive carcinoma with squamous differentiation and keratinization in breast segmentectomy material (Histological section, hematoxylin and eosin, 100x); (b) strong and diffuse immunopositivity for the p16 marker (p16, DAKO, 200 x); (c and d) detection of signals by the in-situ hybridization technique (ISH) for high risk HPV (Ventana Infomr HPV III Family 16 probe for HPV genotypes 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58 and 66) - 200 and 400x increase, respectively.
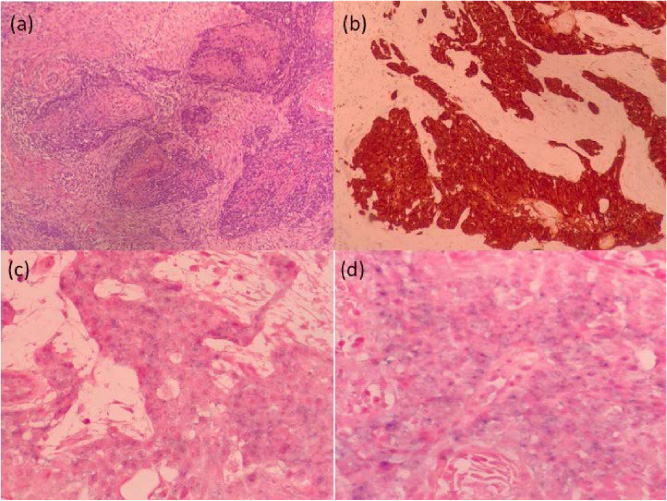
Table 1
Differential diagnosis of squamous cellular carcinoma (SCC) of the breast by immunohistochemical evaluation
| Primary SCC | Metaplastic with SCC component | IDC | Metastatic SCC | Current case | |
| p63 | 42% positive | 58% positive | - | negative | |
| 70% positive | 11% positive | ||||
| CK 5/6 | 63% positive | 62% positive | - | - | |
| 75% positive | 0% | ||||
| p16 | negative or 14% positive | negative or 14% positive | positive - high expression | positive | |
| ER/ PR/ Her2 | negative | negative | - | negative | |
| SOX10 | 78% TN | 45% all TN | negative | negative |
[i] IDC = Invasive ductal carcinoma; TN = triple negative tumor; ER = estrogen receptor; PR = progesterone receptor
3.Discussion
In a patient diagnosed with breast squamous cell carcinoma, the presence of metaplastic breast carcinoma with squamous differentiation, or a primary breast SCC, must be considered. However, in the presence of previous cervical neoplasia, a third hypothesis of metastatic cervical neoplasia may be considered.
The evaluation for the presence of HPV in the breast lesion does not make the diagnosis based on the characteristic of the lesion. In patients with breast cancer and cervical intraepithelial neoplasia [6] or invasive cervical cancer [7], HPV is present in breast lesions in up to half of the cases. In general, the presence of HPV in breast cancer ranges from 20.9% to 23% [8] and the literature discuss the possible association of HPV in breast cancer carcinogenesis [7]. Pure and metaplastic breast SCC are rare entities, and generally have a basal expression, with the expression of genomic HPV being observed in 14% of patients [9].
By immunohistochemistry, p16 expression is associated with high-grade lesions and the presence of invasive disease to the cervix, also suggesting previous HPV[10,11] infection, and p63 expression for metaplastic breast carcinoma [3]. On the other hand, high p16 expression was observed in approximately 40.1% of breast tumors [12], not being specific to the cervix. P16 and HPV are usually present in invasive lesions of the cervix, but their positivity in the breast does not exclude metastatic origin.
Negativity for mammaglobin and GCDFP-15 suggests the non-mammary origin of the tumor [13], in spite of the focal expression of GATA-3. Due to the question regarding the origin of SCC, immunohistochemistry was performed using p63, SOX10 and RE/RP/Her2 (Table 1). If it were primary of the breast, it would be triple negative, a condition associated with SCC. However, negativity for p63 suggested absence of primary breast squamous cell carcinoma or metaplastic carcinoma. Negativity for SOX10 may be present in breast cancer, but its absence also occurs in the presence of metastatic squamous cell carcinoma disease. Thus, negativity for SOX10 [14], the expression of p16 and the hybridization to HPV 16, associated with a past of cervical cancer, strengthen the hypothesis of metastatic disease of the cervix.
In the immunohistochemical evaluation of squamous cell neoplasia in the breast (Table 1), it is suggested to consider the assessment of markers p63, SOX10 and p16, a fact that, in this case, confirmed the metastatic origin of the lesion, something not previously demonstrated in the literature.
Statements
Statement of ethics
This case report was reviewed and approved by Ethics Committee of the Barretos Cancer Hospital, approval number 2290/2021.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Conflict of interest statement
The authors declare no conflicts of interest.
Data availability statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Funding sources
The authors declare that there are no Funding Sources.
Author contribution
Study concepts: de Oliveira-Junior I, Vieira RAC
Study design: de Oliveira-Junior I, Vieira RAC
Data acquisition: All authors
Data analysis and interpretation: All authors
Manuscript preparation: All authors
Manuscript editing: All authors
Manuscript review: All authors
References
[1] | Moore DH, , Wilson DK, , Hurteau JA, , Look KY, , Stehman FB, , Sutton GP, Gynecologic cancers metastatic to the breast, J Am Coll Surg, 187: : 178–181, (1998) . |
[2] | Ikenberg H, , Teufel G, , Schmitt B, , Kommoss F, , Stanimirovic B, , Pfleiderer A, Human papillomavirus DNA in distant metastases of cervical cancer, Gynecol Oncol, 48: : 56–60, (1993) . |
[3] | Koker MM, , Kleer CG, p63 expression in breast cancer: A highly sensitive and specific marker of metaplastic carcinoma, Am J Surg Pathol, 28: : 1506–1512, (2004) . |
[4] | Anne N, , Sulger E, , Pallapothu R, Primary squamous cell carcinoma of the breast: A case report and review of the literature, J Surg Case Rep, 2019: : rjz182, (2019) . |
[5] | Mangla A, , Agarwal N, , Saei Hamedani F, , Liu J, , Gupta S, , Mullane MR, Metastasis of cervical cancer to breast: A case report and review of literature, Gynecol Oncol Rep, 21: : 48–52, (2017) . |
[6] | Hennig EM, , Suo Z, , Thoresen S, , Holm R, , Kvinnsland S, , Nesland JM, Human papillomavirus 16 in breast cancer of women treated for high grade cervical intraepithelial neoplasia (CIN III), Breast Cancer Res Treat, 53: : 121–135, (1999) . |
[7] | Widschwendter A, , Brunhuber T, , Wiedemair A, , Mueller-Holzner E, , Marth C, Detection of human papillomavirus DNA in breast cancer of patients with cervical cancer history, J Clin Virol, 31: : 292–297, (2004) . |
[8] | Simoes PW, , Medeiros LR, , Simoes Pires PD, , Edelweiss MI, , Rosa DD, , Silva FR , Prevalence of human papillomavirus in breast cancer: A systematic review, Int J Gynecol Cancer, 22: : 343–347, (2012) . |
[9] | Grenier J, , Soria JC, , Mathieu MC, , Andre F, , Abdelmoula S, , Velasco V , Differential immunohistochemical and biological profile of squamous cell carcinoma of the breast, Anticancer Res, 27: : 547–555, (2007) . |
[10] | Silva DC, , Goncalves AK, , Cobucci RN, , Mendonca RC, , Lima PH, , Cavalcanti GJ, Immunohistochemical expression of p16, Ki-67 and p53 in cervical lesions - A systematic review, Pathol Res Pract, 213: : 723–729, (2017) . |
[11] | Molina MA, , Carosi Diatricch L, , Castany Quintana M, , Melchers WJ, , Andralojc KM, Cervical cancer risk profiling: Molecular biomarkers predicting the outcome of hrHPV infection, Expert Rev Mol Diagn, 20: : 1099–1120, (2020) . |
[12] | Shin E, , Jung WH, , Koo JS, Expression of p16 and pRB in invasive breast cancer, Int J Clin Exp Pathol, 8: : 8209–8217, (2015) . |
[13] | Bonacho T, , Rodrigues F, , Liberal J, Immunohistochemistry for diagnosis and prognosis of breast cancer: A review, Biotech Histochem, 95: : 71–91, (2020) . |
[14] | Qi J, , Hu Z, , Xiao H, , Liu R, , Guo W, , Yang Z , SOX10 - a novel marker for the differential diagnosis of breast metaplastic squamous cell carcinoma, Cancer Manag Res, 12: : 4039–4044, (2020) . |




