Device-Assisted Therapy in Non-Muscle-Invasive Bladder Cancer
Abstract
Intravesical therapy is a critical component in the management of non-muscle-invasive bladder cancer (NMIBC), as it reduces rates of disease recurrence and progression. However, the presence of physiologic barriers in the urothelium reduces the penetration and distribution of intravesical chemotherapy, thereby limiting the therapeutic potential. Much progress to overcome this challenge has been made in the realm of intravesical device-assisted therapy. Novel device-assisted treatments include hyperthermia, the radiofrequency-induced thermochemotherapy effect, electromotive drug administration, and implantable drug delivery systems. Notably, chemotherapy enhanced by these device-assisted systems has shown improved oncologic efficacy relative to standard intravesical chemotherapy and comparable outcomes relative to Bacillus Calmette-Guérin (BCG) therapy in patients with intermediate- or high-risk NMIBC. Recent studies also support the utility of device-assisted therapy as a salvage treatment option in patients with BCG-unresponsive disease. Ongoing randomized controlled trials and prospective investigations will further help clarify indications and long-term safety outcomes of these treatment modalities in NMIBC. Herein, we present a comprehensive review of device-assisted therapies and discuss their clinical utilities for the management of NMIBC in the modern era.
INTRODUCTION
Bladder cancer is a commonly diagnosed cancer, with an estimated incidence of over 83,000 new cases and 16,840 cancer-related deaths in the United States in 2024 [1]. The most common subtype of bladder cancer is urothelial carcinoma, and approximately 75% of these are non-muscle-invasive bladder cancer (NMIBC) [2]. Among cases of NMIBC, approximately 10% present as CIS only, 20% as T1, and 70% as Ta [3, 4]. Transurethral resection of bladder tumor (TURBT), intravesical chemotherapy, and intravesical bacillus Calmette-Guérin (BCG) comprise the backbone of NMIBC management. For intermediate- and high-risk NMIBC, recurrence rates at five years after treatment with BCG are 14% and 28%, respectively [5]. For high-risk NMIBC, approximately 9% of cases progress after BCG treatment. Despite being an important component of the treatment of NMIBC, a global shortage, coupled with limited treatment options after BCG failure, has fueled research into new therapies and technologies for treating NMIBC.
Immune checkpoint inhibitors have shown oncologic efficacy in NMIBC, although the incidence of grade 3 or higher toxicity is approximately 13%, which is substantially higher than the rate typically seen with intravesical treatments [6]. Thus, there is a foremost need to develop efficacious therapeutic approaches with a favorable toxicity profile. An active area of investigation has been enhancing the delivery and/or efficacy of established intravesical therapies using device-assisted technology. Novel strategies include the radiofrequency-induced thermochemotherapeutic effect, hyperthermic intravesical chemotherapy, electromotive drug administration, and implantable intravesical drug delivery systems. In this review, we provide a comprehensive overview of these device-assisted therapeutic approaches, with a focus on the device mechanics, mechanisms behind cancer treatment, oncologic efficacies, safety, and tolerability.
Challenges
NMIBC represents a noteworthy disease state in the context of drug delivery, as it contains challenges due to the physiologic barriers present in the urothelium and the unique method of intravesical drug delivery. The first barrier to drug or toxin permeation into the urothelium is provided by a robust network of glycosaminoglycans (GAG) [7]. This dense extracellular matrix is comprised of a number of mucopolysaccharides, such as hyaluronic acid and chondroitin sulfate, that formulate a barrier whose integrity is essential to prevent reabsorption of urinary solutes and bacterial adherence to urothelium [8]. Various pharmaceutical agents have been employed in preclinical studies to perturb the GAG barrier function such as intravesical detergents, inhibitors of various GAG constituents, and therapeutic agents that suffuse a drug of interest within the GAG layer [9].
The subsequent barrier present for intravesical drug delivery is provided by the urothelium itself. The apical junctions of the umbrella cells regulate paracellular transport of solutes and materials even when formidable mechanical forces are present during bladder filling [10]. Tight junctions make up part of the apical junction and are crucial for regulating the transport of materials past the umbrella cells. Clinically, the effects of these barriers on drug penetration are apparent in drug diffusion studies. In one such study, intravesical Mitomycin C (MMC) diffusion was assessed by placing 20 mg MMC in 40 mg of water for a two-hour dwell time in 11 patients prior to radical cystectomy for urothelial cell carcinoma or locally invasive colon cancer [11]. Median drug concentration was highest at 5.6μg/ml in the urothelial basement membrane, 2.7μg/ml in the lamina propria, and 0.9μg/ml at the base of the muscularis. No considerable difference in drug penetration between normal tissue and tumor was noted; however, this was only assessed in a small subset of patients on study and was limited by technical difficulties. The same group conducted a similar study assessing drug penetration of 40 mg of doxorubicin diluted in 20 mg of water with a dwell time of 1–2 hours in ten patients undergoing radical cystectomy [12]. Similarly, median drug concentration was highest at 8.6μg/ml in the urothelial basement membrane, 5.3μg/ml in the lamina propria, and 1.1μg/ml at the base of the muscularis. Notable in both studies was the considerable decrease in drug concentrations at increasing tissue depths and an appreciable intersubject variability. These findings highlight the need for mechanisms of drug delivery that facilitate improved concentrations at higher depths of tissue.
METHODS
A non-systematic narrative review was performed by querying PubMed of the recent advances in device-assisted NMIBC treatment. The search was limited to articles published since 2008. Articles were then reviewed for their relevance to device-assisted management of NMIBC and were limited to human interventional studies. Devices were then subclassified based on their general mechanisms of action (Fig. 1). Articles were considered eligible if they had a retrospective or prospective design, with a priority of reporting on randomized controlled trials. Data from comprehensive prospective studies and randomized controlled trials are presented in Tables 1a–d.
Fig. 1
General mechanisms of action for devices used to administer intravesical therapies in non-muscle-invasive bladder cancer. Hyperthermia-based approaches induce regional changes at the molecular level and in the tissue microenvironment, intravesical electromotive drug administration (EMDA) devices induce electrokinetic changes that facilitate drug movement, and implantable drug delivery systems facilitate sustained drug release.
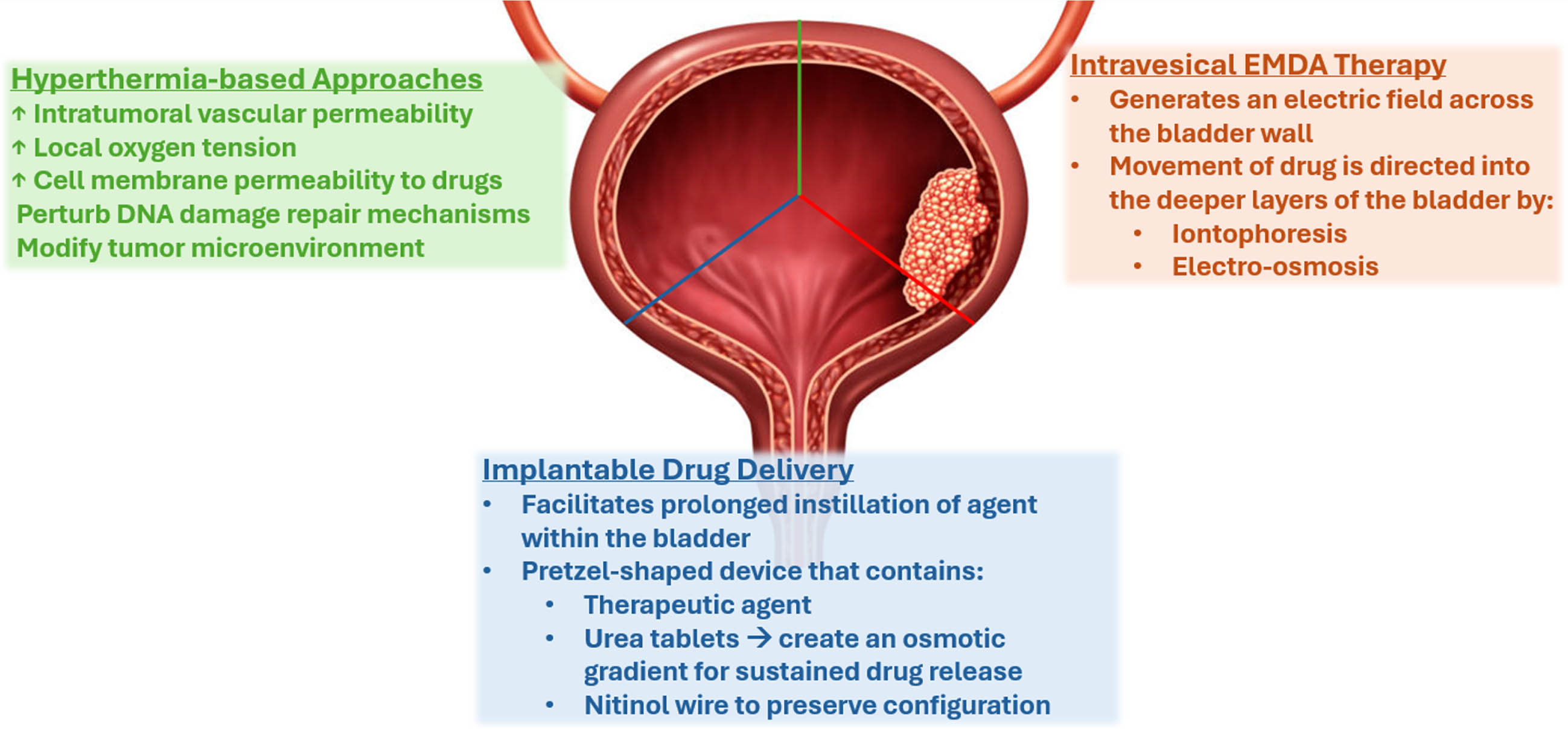
Table 1a
Studies evaluating the radiofrequency induced thermochemotherapy effect in NMIBC
| Author &Year | Setting of NMIBC Intervention | Study Design | NMIBC Features | Study Cohort | Study Outcomes |
| Colombo et al., 2011 [17] | Adjuvant | RCT | Intermediate- and high-risk NMIBC | 83 Total: –42 RITE –41 Intravesical chemotherapy alone | RFS at a follow-up of 10 years: –RITE: 53% – Control: 15% |
| Arends et al., 2016 [22] | Adjuvant | RCT | Intermediate- and high-risk NMIBC | 132 Total (per-protocol): – 60 RITE – 72 BCG | RFS at 24 months (per-protocol) – RITE: 81.8% – BCG: 64.8% Study closed prematurely due to slow accrual. |
| Tan et al., 2019 [23] | Adjuvant | Phase III RCT | Intermediate- and high-risk NMIBC after BCG exposure | 104 Total: – 48 RITE – 56 Institutional second-line therapy or BCG | RFS at a mFU of 36 months: HR of 1.33 (95% CI: 0.84–2.10), p = 0.23 |
Table 1b
Studies evaluating conductive hyperthermia in NMIBC
| Author &Year | Setting of NMIBC Intervention | Study Design | NMIBC Features | Study Cohort | Study Outcomes |
| Sousa et al., 2014 [33] | Ablative | Pilot/feasibility trial | Intermediate- and High-risk NMIBC | 15 Total: all receiving ablative hyperthermia followed by TURBT | CR at TURBT: 53% 3-year RFS: 85% |
| Ekin et al., 2015 [41] | Adjuvant | Prospective, non-randomized study | High-risk NMIBC | 43 Total: all receiving adjuvant chemo-hyperthermia | RFR: – 12 months: 82% – 24 months: 61% |
| Soria et al., 2016 [40] | Adjuvant | Single-arm phase I-II trial | Low-, intermediate-, and high-risk NMIBC | 34 Total: all receiving adjuvant chemohyperthermia | RFR (mFU of 41 months): 64.7% PFR (mFU of 41 months): 76.5% |
| Sousa et al., 2016 [34] | Ablative, adjuvant | Prospective, non-randomized study | Intermediate- and High-risk NMIBC | 40 Total: – 24 Ablative – 16 Adjuvant | Ablative – CR: 62.5% – 4-year RFS: 79.2% Adjuvant 2-year RFS: 87.5% |
| Guerrero-Ramos et al., 2022 [30] | Adjuvant | Phase II RCT | High-risk NMIBC | 50 Total: – 25 Intravesical BCG – 25 HIVEC with MMC | RFS at 24 months: – Intravesical BCG: 71.8% – HIVEC with MMC: 86.5% Time to recurrence: – Intravesical BCG: 16.1 months– HIVEC with MMC: 21.5 months |
| Tan et al., 2023 [32] | Adjuvant | Phase II RCT | Intermediate-risk NMIBC | 259 Total: – 131 43°C for 60 minutes – 128 Normothermia | Disease-free Survival at 24 months: –43°C for 60 minutes: 61% – Normothermia: 60% |
| Angulo et al., 2023 [31] | Adjuvant | Phase III RCT | Intermediate-risk NMIBC | 319 Total: – 106 Normothermia – 107 43°C for 30 minutes – 106 43°C for 60 minutes | RFS at 24 months: – Normothermia: 77% – 43°C for 30 minutes: 82% – 43°C for 60 minutes: 80% |
Table 1c
Studies evaluating electromotive drug administration in NMIBC
| Author &Year | Setting of NMIBC Intervention | Study Design | NMIBC Features | Study Cohort | Study Outcomes |
| Colombo et al., 2001 [62] | Ablative Treatment | Prospective, non-randomized study | Low-risk NMIBC | 80 Total: – 36 MMC – 29 RITE – 15 EMDA-MMC | CR: – MMC: 27.7% – RITE: 66% – EMDA-MMC: 40% |
| Decaestecker et al., 2018 [53] | Ablative Treatment | Prospective, non-randomized study | Single or multiple papillary NMIBC | 32 Total: all receiving a single EMDA-MMC instillation | CR: 28% – PR: 11% – SD: 61% |
| Di Stasi et al., 2011 [55] | Neoadjuvant | Phase III RCT | Low-, intermediate-, and high-risk NMIBC | 374 Total: – 124 TURBT alone – 126 Passive MMC – 124 EMDA-MMC | RFR (mFU of 86 months): – TURBT: 36% – Passive MMC: 41% – EMDA-MMC: 62% PFR (mFU of 86 months): – TURBT: 79% – Passive MMC: 81% – EMDA-MMC: 84% Median Time to Recurrence: – TURBT: 12 months – Passive MMC: 16 months – EMDA-MMC: 52 months |
| Di Stasi et al., 2003 [54] | Adjuvant | Prospective randomized study | High-risk NMIBC | 108 Total: – 36 TURBT+BCG – 36 TURBT+Passive MMC – 36 TURBT+EMDA-MMC | CR at 3 months: – TURBT+BCG: 56% – TURBT+Passive MMC: 28% – TURBT+EMDA-MMC: 53% CR at 6 months: – TURBT+BCG: 64% – TURBT+Passive MMC: 31% – TURBT+EMDA-MMC: 58% |
| Di Stasi et al., 2006 [56] | Adjuvant | Phase III RCT | High-risk NMIBC | 212 Total: – 105 TURBT+BCG – 107 TURBT+BCG+EMDA-MMC | RFR (mFU of 88 months): – TURBT+BCG: 41.9% – TURBT+BCG+EMDA-MMC: 57.9% PFR (mFU of 88 months): – TURBT+BCG: 78.1% – TURBT+BCG+EMDA-MMC: 90.7% Median Time to Recurrence: – TURBT+BCG: 21 months – TURBT+BCG+EMDA-MMC: 69 months |
| Gan et al., 2016 [57] | Adjuvant | Prospective, non-randomized study | High-risk NMIBC | 107 Total: All receiving adjuvant sequential BCG/EMDA-MMC | RFR: – At one year: 87% – At two years: 93% |
| Racioppi et al., 2018 [59] | Adjuvant | Single-center, single-arm phase II trial | BCG-unresponsive tumors | 26 Total: all receiving adjuvant EMDA-MMC | RFR at 3 years: 61.5% PFR at 3 years: 84.6% |
Table 1d
Studies evaluating implantable drug delivery systems (TAR) in NMIBC
| Author &Year | Setting of NMIBC Intervention | Study Design | NMIBC Features | Study Cohort | Study Outcomes |
| Daneshmand et al., 2023 [68] | Adjuvant | Multicenter phase IIb trial | BCG-unresponsive, high-risk NMIBC | 26 total, efficacy evaluable set: – 8 TAR-200 – 8 Cetrelimab | CR as of data cutoff (May 25, 2022): – TAR-200 : 88% – Cetrelimab: 38% |
| Vilaseca et al., 2023 [69] | Adjuvant | Multicenter phase I trial | Intermediate- or high-risk NMIBC harboring select FGFR alterations | 43 total, all receiving erdafitinib via TAR-210 – C1 : 16 with recurrent, BCG-unresponsive high-risk NMIBC – C3 : 27 with recurrent, intermediate-risk NMIBC | RFR: 82% (C1) CR: 87% (C3) |
MMC, Mitomycin C; RITE, Radiofrequency-induced thermo-chemotherapy, EMDA, Electro-Motive Drug Administration; NMIBC, Non-muscle-invasive bladder cancer; CR, Complete response; PR, Partial response; SD, stable disease; TURBT, Transurethral resection of bladder tumor; BCG, Bacillus Calmette-Guerin; RFR, Recurrence-free rate; PFR, Progression-free rate; RCT, Randomized controlled trial; RFS, Recurrence-free survival; PFS, Progression-free survival; HR, Hazard ratio; CI, Confidence interval; mFU, Median follow-up.
HYPERTHERMIA
The use hyperthermia for treating malignancies has been explored since antiquity, with documents demonstrating its use to treat tumors in ancient Egypt, India, and Greece [13]. The Greek physician Hippocrates dedicated one his well-known aphorisms on the topic which stated that “Those who cannot be cured by medicine can be cured by surgery. Those who cannot be cured by surgery can be cured by heat. Those who cannot be cured by heat are to be considered incurable.” Since its initial applications, much has been done to elucidate the anti-neoplastic mechanisms of hyperthermia. Mild hyperthermia is a strategy of heating tissue to slightly above physiologic levels, generally 40–45°C, in order to elicit biologic changes while not achieving direct thermal ablation [14]. Mild hyperthermia has demonstrated an ability to alter the tumor microenvironment by increasing intratumoral vascular permeability, raising local oxygen tension, increasing cell membrane permeability to certain drugs, perturbing DNA damage repair mechanisms, and modifying the tumor immune microenvironment through a multitude of diverse pathways [15].
Multiple systems have been utilized to incorporate mild hyperthermia in the delivery of intravesical MMC. The three most utilized methods are 1) intravesical heating of the bladder tissue mediated via radiofrequency (RF) antennae, 2) conductive heating of the bladder via externally heated chemotherapy and subsequent bladder instillation, and 3) use of an external RF generator to heat both the bladder and intravesical agent.
Radiofrequency induced thermochemotherapy effect (RITE)
The Synergo system SB-TS 101 (Medical Enterprises, Amsterdam, Netherlands) allows for concomitant hyperthermia to be applied to the bladder with intravesical instillation of either MMC or epirubicin. The system utilizes a specialized disposable 20 Fr 3-way catheter modified with an integrated miniature RF antenna and five thermocouples to assess bladder and urethral temperatures [16]. The RF generator provides 915 MHz of non-ionizing radiation directly to the bladder to raise tissue temperature to 42±2°C. Five total thermocouples monitor both the urethral and bladder temperature while cooled chemotherapy is instilled within a closed circuit for the putative benefits of urethral comfort and drug stability. The treatment is given in an outpatient setting to patients with either no or local anesthetic gel applied to the urethra. Dwell time is planned for 60 minutes and mitomycin is dosed at 20 mg in 50 mL of water and refreshed with another 20 mg MMC in 50 mL of water halfway through the treatment time [17]. Epirubicin was also administered in earlier studies, but contemporary use of the system has replaced it in favor of MMC.
Initial studies of intermediate- to high-risk NMIBC by van der Heijden et al. utilized two treatments of 20 mg MMC in 40 mL of water and demonstrated favorable outcomes [18]. In 90 patients who underwent an induction course of six to eight weekly sessions and a maintenance course of four to six monthly sessions, one- and two-year rates of recurrence were 14.3% and 24.6%, respectively. The BCG-exposed cohort of patients (n = 41) experienced recurrence rates of 23.1% and 41.2% at one and two years, respectively. Subsequently, a single-center series reported by Moskovitz et al. demonstrated similar responses in intermediate- to high-risk subjects, with 20 patients (91%) experiencing no recurrence at a median follow-up of 10 months [19]. The experience from this institution was later updated with 64 patients, 47 (73%) of whom were high-risk, undergoing adjuvant therapy in a modified protocol where the maintenance course was changed to six sessions at six-week intervals. At a median follow-up of 23 months, the two-year median recurrence-free survival (RFS) was 32.8% [20].
Columbo et al. described the results of a multicenter, randomized controlled trial comparing adjuvant RITE to normothermic MMC in treatment-agnostic NMIBC [21]. Eighty-three patients with intermediate- to high-risk papillary NMIBC with or without carcinoma in situ (CIS) were randomized to receive 20 mg MMC in 50 ml of water with replacement of the solution after 30 minutes for a total dwell time of 1 hour with or without hyperthermia. Approximately 40% of patients in both arms had received prior treatment with either BCG or chemotherapy, and the presence of grade 3 tumors was 26% in the RITE arm and 17% in the MMC arm. At a minimum follow-up of two-years, 75 patients (90%) were evaluated, and recurrence was noted in six (17%) and 23 (58%) patients in the RITE and MMC arms, respectively. The authors reported on long-term outcomes after a median follow-up of 90 months and demonstrated 5- and 10-year median RFS to be 62% and 53% in the RITE arm compared to 21% and 15% in the MMC arm [17]. These results suggest a sustained, durable, and superior response experienced by patients undergoing RITE; however, the bladder preservation rate and overall survival was similar between the two arms.
Similarly, Arends et al. reported on the results of a randomized controlled trial in which 184 patients with intermediate- or high-risk bladder cancer were randomized to RITE or BCG [22]. The majority (69%) of patients had intermediate-risk papillary-only disease. Patients were randomized to six weekly treatments and six maintenance treatments of RITE, or induction intravesical BCG with 1 year of maintenance therapy. The intention-to-treat analysis did not demonstrate a difference in terms of 24-month RFS (78.1% RITE vs. 64.8% BCG, p = 0.08), but the per-protocol analysis did demonstrate a difference in 24-month RFS (81.8% RITE vs. 64.8% BCG, p = 0.02). Unfortunately, the study closed prematurely and therefore was underpowered to assess its endpoints.
Tan et al. reported on the phase 3, multicenter HYMN trial, which randomized patients with BCG-exposed intermediate- to high-risk cancer with either RITE or a choice between a second course of BCG induction with maintenance or institutional standard of care [23]. A total of 104 patients were assessed; however, the trial was closed prematurely due to a higher than expected rate of recurrence of carcinoma in situ (CIS) noted in the RITE arm. With a median follow-up of 36 months, assessment of co-primary endpoints demonstrated no significant differences in either the disease-free survival (DFS) rate of all subjects or the 3-month complete response (CR) rate in CIS patients. Planned sub-group analysis, however, demonstrated a considerably lower DFS in subjects who harbored CIS with or without papillary disease at baseline (HR: 2.1; p = 0.01). Some important considerations in this study were that it was performed prior to the FDA and AUA definitions of BCG-refractory NMIBC, and thus included a heterogeneous group of BCG exposed patients. Therefore, a second round of BCG therapy, utilized in 59% of controls, remained a highly efficacious treatment for this patient population. Similarly, 23% of control patients were given MMC via electromotive therapy, which is a novel mechanism of drug delivery that may not represent a pragmatic standard of care treatment used throughout most institutions. Given these results, a subsequent retrospective study assessing outcomes in 299 patients with intermediate- to high-risk patients, most of whom were BCG-exposed or refractory (85% and 65%, respectively) was conducted [24]. Heterogenous dosing was utilized with 80 mg of MMC or 100 mg of epirubicin utilized in the neoadjuvant/ablative setting and 40 mg of MMC or 60 mg of epirubicin in the adjuvant setting. The 6-month CR rate for those with CIS±papillary disease (n = 128) or neoadjuvant treatment (n = 22) was 56% while 1- and 2-year RFS for all papillary patients were 79% and 60%, respectively. Patients treated with ablative dosing were noted to have improved RFS (HR 0.54) on multivariate analysis; however, it is unclear if this secondary to patient characteristics.
Study design in this space has matured over time, with a focus on specific patient populations, notably patients experiencing T1 high-grade (HG), CIS, or BCG-exposed NMIBC. Halachmi et al. assessed 56 patients with T1 HG disease, 30 (54%) of whom were treatment naïve, who received RITE [25]. At median follow-up of 18 months, 2-year and 4-year estimated RFS were 43% and 51%, respectively. However, it should be noted that five patients (9%) discontinued therapy prior to the first evaluation secondary to adverse events and were not included in the final analysis. Notably, one patient developed a grade 3 urethral stricture, and another required a cystectomy solely due to troublesome lower urinary tract symptoms. Witjes et al. reported on a retrospective dataset of patients with CIS, with or without papillary disease, who underwent RITE [26]. Fifty-one patients were assessed, 34 of whom received prior BCG with 17 deemed BCG-refractory, 15 BCG-relapsing (recurrence after 12 months) and two being BCG-intolerant. The 3-month CR rate was 92%, and after a median follow-up of 27 months, 51% of responders experienced a recurrence.
The safety profile of RITE is similar to that of other intravesical therapeutics. Lower urinary tract symptoms tend to predominate, with the most common being bladder pain and bladder spasms during treatments. Specific adverse events to note with this treatment are bladder pain and sensitivity during treatment, the relatively higher rate of urethral strictures noted in multiple studies, and the presence of posterior wall thermal reactions [19, 22]. Posterior wall thermal reactions are a unique side effect ascribed to RITE. Due to the location of the RF antennae, a small erythematous lesion can develop at the posterior bladder wall during cystoscopy [19]. Due to its appearance, it can be mistaken for CIS; however, these are benign and resolve spontaneously.
When comparing RITE or BCG for intermediate- to high-risk tumors, chemohyperthermia (CHT) resulted in considerably more bladder pain during sessions (OR: 26.3), bladder spasms (OR 15.5), posterior wall thermal reactions (OR: 5.8), and urethral strictures (OR 2.3) compared to BCG. RITE was noted to have a significantly lower rate of urinary frequency (OR: 0.6), incontinence (0.2), hematuria (0.6), and fatigue (0.2) than BCG. Serious adverse event rates were similar between both arms.
The role for RITE therapy in NMIBC is being further clarified as randomized controlled trials help clinicians gain an understanding of its benefits and pitfalls. Data from these trials suggest an improvement in RFS in patients with intermediate- to high-risk disease compared to normothermic MMC; however, benefit over BCG was only seen in the intention-to-treat analysis when compared to a predominantly intermediate-risk, treatment-naive cohort; and no benefit was noted in a BCG-exposed cohort. Future trials assessing patients with BCG-unresponsive disease will help further define the role of this treatment in the salvage setting.
COMBAT Bladder Recirculation System
The COMBAT Bladder Recirculation System (BRS, Combat Medical, Wheathampstead, UK) is a device that utilizes conductive heating via temperature exchange from externally heated chemotherapy to the bladder wall, resulting in an increase in bladder temperature. Unlike the RITE system, which achieves bladder wall hyperthermia by direct bladder wall heating, the BRS utilizes passive heat exchange from instilled agent to achieve mild hyperthermia. This system mirrors the concept seen in the more established method of hyperthermic intraperitoneal chemotherapy (HIPEC) in which chemotherapy is heated and administered intraperitoneally, allowing for conductive heating to occur in the peritoneal cavity. Given its similar mechanism of action, this type of therapy has also been labelled as hyperthermic intravesical chemotherapy (HIVEC).
The BRS system is composed of a disposable aluminum foil heat exchanger which externally heats the chemotherapeutic agent. A priming solution of approximately 50 mL is utilized, and a 16 Fr modified 3-way foley catheter with temperature and pressure sensors is used to help instill the agent. The BRS employes a relatively isobaric environment within the bladder, with safety sensors identifying elevated pressures during filling. The majority of studies are conducted with a one-hour hyperthermic instillation time of MMC and a temperature of 43±1°C, though the system does allow for some variability in these settings. General treatment schedules consist of weekly treatments for 6 weeks during the induction period, followed by once monthly treatments during the maintenance period.
HIVEC has been utilized in both the neoadjuvant/ablative setting and in the adjuvant setting, with the majority of studies focusing on its role as a form of adjuvant therapy. Plata et al. reported on the experience of nine centers in Spain utilizing HIVEC with MMC in the adjuvant setting in 502 patients from 2012 to 2020 [27]. The patients were of European Association of Urology (EAU) intermediate- (59%) or high-risk (41%), with a majority of patients being BCG-naïve (90%). Patients were treated with adjuvant HIVEC MMC at 40 mg for 1 hour, with a majority of patients receiving both induction and maintenance treatments (n = 402, 80%), and were followed for a median of 24 months. The five-year RFS, progression free survival (PFS), and overall survival (OS) for the overall cohort were 50% (53% for intermediate-risk and 47% for high-risk), 89% (94% for intermediate-risk and 84% for high-risk), 66% (74% for intermediate-risk and 60% for high-risk), respectively.
Multiple smaller, single-institution studies have demonstrated similar therapeutic efficacy. Magalhães et al. reported on 57 patients with EAU intermediate- (IR) or high-risk (HR) disease who underwent a standard six-week induction course of 40 mg of MMC via HIVEC followed by monthly maintenance treatments for 6 months [28]. The median DFS (mDFS) for the overall cohort was 42 months, with the IR cohort experiencing an improved mDFS of 44 months and the HR cohort exhibiting a mDFS of 39 months. When controlled for recurrences during therapy, patients who were able to complete maintenance therapy had considerably improved mDFS and had a significant improvement in OS (HR: 42.8). Similarly, Conroy et al. reported on 57 high-risk NMIBC patients, half of whom had received prior BCG [29]. They detailed a 12-month RFS, PFS, and OS of 68%, 82%, and 95% for patients who were treated with a standard induction course and a maintenance course of two-cycles of three weekly instillations. However, 20% of patients progressed on study, with 7% progressing to muscle-invasive bladder cancer (MIBC).
In order to assess the comparative efficacy of other treatments to HIVEC MMC, three randomized controlled trials were performed in subjects with high-risk and intermediate-risk NMIBC. HIVEC-HR was a multicenter trial randomizing patients with EAU high-risk, papillary-only NMIBC to either BCG or HIVEC MMC [30]. The HIVEC arm was administered 40 mg of MMC distilled in 40 mL of water in a six-week induction course, with six additional weekly instillations as maintenance. A majority (90%) of subjects were treatment-naïve and only 1 patient had prior treatment with BCG. A total of 50 patients were randomized, and 48 patients received treatment. The primary outcome of 24-month RFS was 86.5% in the HIVEC arm and 71.8% in the BCG arm, demonstrating no significant difference (HR: 0.4; p = 0.2). Similarly, the 24-month PFS was 95.7% in the HIVEC arm and 71.8% in the BCG arm (HR: 0.1; p = 0.07).
The HIVEC-I was a phase 3 trial randomizing patients with intermediate-risk NMIBC in a 1 : 1:1 fashion to four weekly then three monthly instillations of 40 mg of MMC in normothermic conditions (n = 106), 43°C for 30 minutes (n = 107), or 43°C for 60 minutes (n = 106) [31]. The primary outcome of 24-month RFS was 77% for normothermia, 82% for the 30-minute HIVEC arm, and 80% for the 60-minute HIVEC arm (p = 0.6). Pooled assessment of all HIVEC-treated subjects compared to normothermic subjects also demonstrated no difference in RFS at 24 months. Health related quality of life was assessed and demonstrated no considerable difference between the three arms. One of the issues the authors noted was a lower rate of events than was expected at 24 months. A rate of approximately 30–40% was hypothesized; however, the outcomes showed only 20–25% rate of recurrence, leading to a sample size that was underpowered to detect the anticipated magnitude of change. The subsequent HIVEC-II trial randomized patients in a 1 : 1 fashion with EAU defined intermediate-risk NMIBC to induction therapy of six weekly instillations of 40 mg of MMC in either normothermia (n = 128) or 43°C for 60 minutes [32]. At a median follow-up of 24 months, the 24-month DFS was 61% in the HIVEC arm and 60% in the normothermic arm. PFS was noted to be higher in the normothermic arm (HR: 3.44, p = 0.02) in the intention to treat analysis, but was found to not be significant in the per protocol analysis (HR: 2.55; p = 0.06). Notably, patients undergoing HIVEC therapy were less likely to complete their treatment when compared to the normothermic arm (59% vs 89%, respectively). Final takeaways from the authors were that hyperthermic MMC cannot be recommended over standard normothermic MMC in intermediate-risk patients.
Multiple studies have assessed HIVEC with variations in dosing and timing. In the neoadjuvant ablative setting, doses of 80 mg were generally employed for the purposes of chemoablating tumors prior to resection. Sousa et al. described their results of a pilot study in which 15 patients with intermediate- to predominantly high-risk NMIBC were treated with 80 mg MMC in 50 mL of distilled water for six sessions prior to planned TURBT and random bladder biopsies [33]. Partial response (PR) was defined as >50% tumor reduction. The investigators reported a visual PR rate of 40%, a visual CR rate of 60%, and a pathologic CR rate of 53%. Patients who experienced a PR went on to receive normothermic monthly maintenance for 1 year. The responses of an expanded cohort of 24 total patients, 60% of whom had prior BCG exposure, was later described by the same group [34]. Visual PR was noted in 33% of subjects while a histologic CR was observed in 62.5%. The overall four-year incidence of recurrence was 21%. The increased dosage was well tolerated, with 96% of planned instillations being administered. The most common adverse events were irritative voiding (42%), bladder spasms (33%), and pain (30%), which were consistent across studies incorporating different dosages.
Higher doses have also been utilized to treat higher-risk patients, including those who are BCG-unresponsive. Grimberg et al. reported on the use of adjuvant HIVEC with 120 mg MMC diluted in 60 ml of water [35]. The analysis cohort included 14 intermediate- to predominantly high-risk patients, a majority of whom had prior BCG exposure (79%). DFS was 85% at a median follow-up of 11 months, and both recurrences were noted in patients who had discontinued therapy after two doses due to adverse events. Adverse events in this group were all grade 1 and 2, and included lower urinary tract symptoms as noted in other studies. Unique to this group was the presence of rash in four patients (29%), which was thought to be related to an MMC allergy, and a grade 2 leukopenia. Further assessment of hematologic parameters did not show concerns for myelosuppression with the 120 mg in 60 mL dose.
Promising outcomes in treating BCG-unresponsive patients with 80 mg of MMC via HIVEC have subsequently led to larger retrospective series assessing this very high-risk patient cohort. Pijpers et al. assessed 56 BCG-unresponsive patients treated at multiple centers who were planned to receive a six-week induction followed by a monthly maintenance regimen for six months [36]. CIS was present in 32 patients (57%). After a median follow-up of 32.2 months, the 1- and 2-year RFS in patients with high-grade disease were 53% and 35%, respectively. Notably, the CR for subjects with CIS was 70% at 6 months, 45% at 12 months, and 33% at 18 months. Pignot et al. also described their multicenter experience of treating 116 patients with BCG-unresponsive disease at standard dosing of 40 mg of MMC via HIVEC [37]. Thirty-six patients (31%) had CIS and 14 patients (12%) had a prior history of upper tract carcinoma. After a median follow-up of 20.6 months, the 1- and 2-year RFS were 63% and 39%, respectively.
The safety profile of HIVEC is similar to that noted in other forms of CHT. It has been tolerated well across different dosages, with the most common symptoms being the lower urinary tract symptoms of urinary tract pain, frequency, and hematuria. An adverse event of note for this therapy is a pruritic rash, thought to be attributable to a MMC allergy. This was noted from 4–29% of patients across the different dosing groups in the various prospective studies [31, 32, 35].
Regarding optimal dosing, recent porcine studies have demonstrated that the standard 40 mg MMC in a 60-minute hyperthermic dwell time show only a modest increase in median bladder wall MMC concentration when compared to the same dose and time in normothermic conditions (471 ng/mL vs 329 ng/ml; p = 0.012) [38]. However, when the doses are increased to 80 mg MMC, there is a considerable increase in bladder wall concentration in the hyperthermic group (7135 ng/mL vs 617 ng/ml; p = 0.004), and this is similarly mirrored with a 120 mg dose. Of note, these porcine studies also utilized priming solutions of 40 mg of MMC in 40 mg of saline in addition to the experimental dose, further increasing the working concentration of the reported dose.
Overall, the role of the Combat BRS HIVEC system is evolving, but a number of clinical trials and prospective studies have identified disease states in which there is potential and those in which there is likely little benefit. The HIVEC-I and II studies assessing EAU intermediate-risk NMIBC have not demonstrated any benefit in this group, even with the inclusion of maintenance therapy. The HIVEC-II study actually demonstrated a worse PFS, which was thought to be attributed in part to the inability of some patients to complete therapy. This has led the authors to conclude that there is no role for HIVEC MMC over normothermic MMC in this patient population. The HIVEC-HR trial demonstrated that 40 mg of MMC via HIVEC had comparable results to BCG in the high-risk population, and this seems to be in-line with other studies demonstrating a more encouraging efficacy in higher-risk patients. The most promising results of the BRS HIVEC system are observed in the higher dose chemoablative neoadjuvant setting and in the BCG-unresponsive setting, where higher doses of 80 mg of MMC are generally utilized. Both settings have shown promising results; however, prospective phase 2 or 3 studies in the BCG-unresponsive setting are lacking. Given the evidence from the pre-clinical porcine studies and the aforementioned clinical studies, focusing on higher-risk patients with increased dosages may play a key role in future studies.
Unithermia
The Unithermia Bladder Wall Thermo-chemotherapy (BWT, Elmedical Ltd, Hod-Hasharon, Israel) is another system reliant on conductive heating of the bladder via externally heated chemotherapy. The device is a compact module consisting of a peristaltic pump and an external heat exchanger to circulate temperature modulated chemotherapy within the bladder. Specialized 3-way 16 Fr Tiemmen tip and 18 Fr Nelaton tip catheters are compatible with the system, and a needle-tip temperature probe is placed within the catheter for temperature sensing. The device maintains stable hyperthermia with a goal temperature of 42.5±1°C and a maximum safety peak of 44.5°C. Instillation time varies between 45–50 minutes, and dosages vary between 40–80 mg of MMC.
Soria et al. reported on the original pharmacokinetic and clinical results in a phase 1-2 single-arm study utilizing BWT [39, 40]. A total of 34 patients who had recurrence after prior induction course of BCG were enrolled on this trial. The pharmacokinetic profile demonstrated minimal systemic absorption with BWT, and plasma levels of MMC were much lower than the reported concentration concerning for toxicity (400 ng/ml). At a median follow-up of 41 months, 44% of patients remained disease free. Median time to recurrence was 10.5 months and median time to progression was 29.5 months. The treatment was well tolerated, with four patients experiencing grade 3 adverse events consisting of bladder spasms (n = 2) and systemic cutaneous rash (n = 2). Head-to- head trials of BWT against other intravesical therapies have yet to be reported on; however, propensity matched studies have been performed to compare the efficacy of BCG-naïve NMIBC patients to either BWT or BCG [41]. The 2-year RFS was more favorable in the BCG arm (93.9% vs 76.2%, p = 0.02) with both use of BWT (HR: 5.2) and the presence of high-grade tumors (HR: 4.6) demonstrating considerably worse outcomes in univariate, but not multivariate, Cox regression analysis.
A subsequent study by Gözen et al. reported on the safety and clinical outcomes of utilizing 80 mg of MMC in a six-week induction course followed by a monthly maintenance dose for 1 year and a quarterly dose thereafter [42]. A total of 18 patients were included in the analysis with 66% of patients with T1 disease, 66% being treatment-naïve, and no patients with prior BCG treatment. At a median follow-up of approximately 15 months, 83.3% of patients did not experience a recurrence and no patients experienced disease progression. Patients tolerated the instillation well, and all adverse events experienced on study were grade 1 or 2.
BSD-2000
The BSD-2000 (BSD Medical, Salt Lake City, UT) is a deep regional hyperthermia system that utilizes an external radiofrequency delivery system, which allows for conformation of the heated zone agnostic of the targeted organ system. The setup has a patient support table, which allows for patient positioning through an external annular phased array applicator and a distilled water bolus. RF waves from 80–120 MHz are utilized to create a customizable hyperthermia plan that allows for a maximum specific absorption rate to be focused on the bladder. Inman et al. detailed the results of a pilot study assessing 15 patients with BCG-unresponsive or intolerant disease [43]. Subjects underwent an induction course of 40 mg of MMC weekly for six weeks with 60-minute dwell time followed by a 4-month maintenance course of monthly doses. The procedure was tolerated well with no subjects discontinuing therapy due to adverse events, of which none above grade 3 were noted. After a median follow-up of 3.2 years, 10 (67%) of patients experienced a recurrence and no patients progressed to muscle-invasive disease. Wen et al. detailed their retrospective single-institution results which compared a cohort of patients with intermediate- to high-risk NMIBC who were treated with normothermic MMC or hyperthermic MMC delivered via the BSD-2000 system [44]. Subjects were administered 30 mg of MMC for a six-week induction period followed by a once monthly instillation for 10 months. A total of 43 patients were assessed (25 normothermic and 18 hyperthermic). Recurrence rates were significantly lower in the hyperthermic group than the normothermic group at 12 months (11.1% vs 44%; p = 0.048) and 24 months (11.1% vs 48%; p = 0.027). The treatment was tolerated well with all patients completing both maintenance and induction courses with no adverse events above grade 3 noted. The most common adverse events in the hyperthermic arm were urinary frequency (67%), gross hematuria (11%) and suprapubic soreness (11%). The BSD-2000 is continuing to be investigated for its role in NMIBC and in organ preservation in muscle-invasive disease.
INTRAVESICAL ELECTROMOTIVE DRUG ADMINISTRATION (EMDA) THERAPY
EMDA is a strategy of utilizing a device to accelerate the delivery of chemotherapy into deep tissues of the bladder through the generation of an electric field across bladder wall [45, 46]. The movement of the intravesical ionized drug is directed from the urothelium to the deeper layers of the bladder via the electrokinetic phenomena of iontophoresis, electro-osmosis, and possibly electroporation [45]. Iontophoresis describes the phenomenon in which a current drives the movement of ions through a solution (tissue). This effectively accelerates the movement of water through tissue and promotes electro-osmosis, which is a process in which non-ionized solutions, such as MMC, are transported with water molecules across a solution or tissue [47]. The amount of drug delivered is directly proportional to the strength and duration of current applied, and inversely proportional to the ionic charge of the drug. These effects allow for better penetration of drug in shorter period of time compared to standard intravesical administration [47].
The EMDA system consists of a specialized 16 or 18 Fr triple-lumen catheter with an active electrode at the tip of a catheter specifically designed to allow for uniform distribution of current. The active electrode is connected to a current generator, and dispersive ground electrode pads are placed on the skin of the suprapubic area. Preclinical studies have shown that EMDA increases penetration and rate of transport, and reduces variability in delivery rates of MMC into the bladder tissue relative to passive diffusion [45, 46, 48, 49]. Intravesical EMDA MMC (40 mg in 100 ml of water) is typically administered with an operating current of 20 mA for a duration of 30 minutes per session, with peak concentration of MMC in the bladder achieved in 15 minutes [46].
The efficacy of intravesical MMC delivered by EMDA has been retrospectively examined in patients with intermediate- and high-risk bladder cancer. In a cohort of 65 patients who underwent complete TURBT followed by adjuvant MMC via EMDA (eight weekly sessions of induction therapy), response to treatment at six months was noted to be 83.3% and 84% for intermediate-risk NMIBC and high-risk NMIBC, respectively [50]. In a cohort of 26 patients with BCG-unresponsive NMIBC, sequential administration of adjuvant EMDA-MMC and BCG led to a PFS of 50% at two years, highlighting the potential for EMDA-MMC/BCG as a viable treatment in this challenging cohort [51]. However, an important caveat is the high risk of death from bladder cancer, which was reported to be 15% at two years. A recent retrospective study by Zazzara and colleagues further reported comparable oncological outcomes when comparing adjuvant EMDA-MMC with adjuvant intravesical BCG after TURBT in intermediate- or high-risk NMIBC, with no differences in PFS or RFS noted in matched paired analysis between patients receiving either treatment [52]. Cumulatively, these studies suggest that MMC delivered by EMDA is a valid consideration as an adjuvant treatment in appropriately selected patients with NMIBC, particularly in those who may not be candidates for BCG.
Prospectively, MMC administered by EMDA has been evaluated in several settings of NMIBC. As an ablative treatment, Decaestecker and colleagues evaluated response rates of a single dose of ablative EMDA MMC dose to avoid TURBT in patients with small (<2 cm), or single or multiple papillary NMIBC [53]. CR was experienced in 25% of subjects, and in patients with multiple tumors (n = 16), 61% of tumors remained unchanged at 2–4 weeks, indicating an insufficient ablative effect with a single dose. In the adjuvant setting, Di Stasi et al. compared EMDA-MMC with passive diffusion of MMC after TURBT in patients with high-risk NMIBC and demonstrated improved three- and six-month RFS [54]. A subsequent multi-center randomized controlled trial compared outcomes of TURBT alone, single-dose EMDA-MMC immediately post-TURBT, and single-dose EMDA-MMC immediately pre-TURBT in intermediate- and high-risk NMIBC [55]. At a median follow-up of 86 months, neoadjuvant EMDA-MMC led to a significantly improved RFS (62%) as compared to adjuvant EMDA-MMC (41%) and TURBT alone (36%). The time to recurrence was also significantly longer for neoadjuvant MMC (52 months) as compared to adjuvant MMC (16 months) and TURBT alone (12 months). Oncologic outcomes of post-TURBT EMDA-MMC compared to TURBT alone were not improved in all patients or when stratified by cancer risk.
EMDA-MMC has also been investigated as a sequential therapy with BCG in prospective studies. A randomized controlled trial comparing induction and maintenance therapy with BCG followed by EMDA-MMC (sequential arm) with BCG alone in patients with pT1 NMIBC reported a higher disease-free interval, lower RFS and PFS, and improved OS in the sequential arm [56]. Of note, the combinatorial strategy employed utilized both BCG and EMDA-MMC in the induction and maintenance schedule. Similar corroborative results were seen in a retrospective study assessing patients with high-risk NMIBC with sequential BCG and EMDA-MMC [57]. A proposed mechanism for the improved outcomes of EMDA-MMC after BCG, as compared to BCG alone, is BCG-induced inflammation that increases the permeability of the bladder mucosa, though further supportive evidence is necessary [56].
A special cohort in which EMDA-MMC has been investigated is patients with BCG-unresponsive NMIBC. A separate retrospective study compared outcomes in patients with recurrent BCG-unresponsive high-risk NMIBC who received EMDA or CHT with those who underwent radical cystectomy [58]. Overall survival, cancer-specific survival, and complication rates were comparable between both groups; although radical cystectomy led to significantly greater high-grade disease-free survival and progression-free survival, which can be expected when comparing organ-sparing therapy to radical therapy. Of note, multifocal disease, disease recurrence, and progression risk group were associated with EMDA and CHT treatment failure. Another prospective phase II study of 26 patients with BCG-refractory high-risk NMIBC found that a majority of patients (61.5%) avoided radical cystectomy at three years of follow-up, with 15% of patients progressing to muscle-invasive disease [59]. Twelve-month DFS ranged from 25% for Ta/T1G3 + carcinoma in situ disease to 75% for TaG3 disease. These data support the utility of EMDA-MMC as a bladder-sparing therapeutic option in patients with high-grade, BCG-refractory NMIBC.
Overall, MMC delivered by EMDA has a generally safe adverse event profile. Common adverse events include drug-related cystitis, lower urinary tract symptoms, bladder spasm, and hematuria; although these have been reported at lower rates than in patients receiving BCG [54, 56, 60, 61]. EMDA-MMC has also been shown to have increased rates of suprapubic pain, dysuria, and urinary frequency compared to patients receiving MMC through RITE [62]. Reports of subcutaneous burns at the site of suprapubic electrode placement have also been reported anecdotally [63]. Sequential EMDA-MMC following BCG has not been shown to increase incidence of BCG-related adverse events compared to BCG alone, although modification of treatment regimen and/or early termination have been reported in 3–28% of patients receiving sequential treatment due to lower urinary tract symptoms, hematuria, and an inability to tolerate the catheter [56, 57].
IMPLANTABLE DRUG DELIVERY SYSTEM: TAR-200
The TAR-200 GemRIS device developed by Taris biomedical and Janssen Pharmaceutical Companies is an implantable drug delivery system designed to facilitate prolonged instillation of gemcitabine within the bladder. The pretzel-shaped device serves as an osmotic pump comprised of a 5 cm semipermeable tube containing three elements: gemcitabine tablets, an osmotic urea mini-tablet, and a nitinol wire [64, 65]. The urea and gemcitabine tablets work in concert to allow for sustained release of the drug via an osmotic gradient, while the nitinol wire preserves the configuration of the device. It is implanted using a specialized 18 Fr coudé tip catheter with a stylet to allow for the deployment of the device within the bladder lumen. It can be removed with a standard flexible or rigid cystoscope and a grasper. This pump has also been utilized for the delivery of intravesical lidocaine and initial release kinetics demonstrated that 60–70% of the drug was released over a two-week period as opposed to a standard dwell time of 1–2 hours [66].
The initial pilot study assessing TAR-200 utilized 225 mg of gemcitabine in patients with intermediate-risk NMIBC in the neoadjuvant setting to assess for safety and chemoablative efficacy. Patients were dosed with two 1-week TAR-200 cycles over a period of 4–6 weeks. Overall, 12 patients received treatment and all adverse events were grade ≤2 and predominantly lower urinary tract in nature. Five (42%) subjects experienced a CR [67]. The TAR-200 device is currently being assessed in a multitude of settings including in neoadjuvant muscle-invasive cancer, bladder sparing therapy, and in the BCG-unresponsive NMIBC space. SunRISe-1 (NCT04640623) is an ongoing multicenter three-arm phase 2b designed to assess the agents TAR-200 and cetrelimab, an anti-programmed death-1 antibody, individually and in combination. Recently, the preliminary results of the monotherapy arms were presented after a median follow-up of 11 months [68]. The TAR-200 arm demonstrated a CR of 73% while the cetrelimab arm had a CR of 36%. Results from this analysis have led to an FDA breakthrough designation of TAR-200 for BCG-unresponsive, high-risk NMIBC in patients unfit or refusing radical therapy. Further studies in this space are ongoing with SunRISe-3 assessing cetrelimab or TAR-200 alone vs. intravesical BCG in the BCG-naïve space (NCT05714202).
TAR-210, a novel osmotic pump in which gemcitabine tablets have been exchanged for erdafitinib tablets, is also being investigated in patients with NMIBC and select fibroblast growth factor receptor alterations (NCT05316155). The early interim results of patients in cohort 1, a BCG-unresponsive population, and cohort 3, an intermediate-risk NMIBC population, were also recently reported [69]. Of the 16 patients who have had their first evaluation in cohort 1, the CR rate was reported to be 82%. Cohort 3 was assessed in the neoadjuvant chemoablative setting and demonstrated 87% CR rate at time of follow-up cystoscopy.
CONCLUSION
Much progress has been made in device-assisted therapy in NMIBC. These technologies improve the delivery and enhance the efficacy of intravesical agents, leading to more sustained and targeted therapeutic action. Prospective studies have shown improved oncologic outcomes in intravesical chemotherapy enhanced by device-assisted systems in patients with intermediate- and high-risk NMIBC when compared to standard chemotherapy. When compared to therapy with BCG, mixed results are noted across intermediate- and high-risk disease states, with some studies showing similar activity and some demonstrating inferior outcomes. However, there is promising activity noted in salvage therapy for patients with BCG-unresponsive disease. Use of device-assisted neoadjuvant therapy also has shown an encouraging ability to chemoablate tumors and decrease the rate of recurrence in intermediate- to high-risk disease. Importantly, these devices are generally safe and tolerable, but these modalities have yet to be widely adopted. Ongoing clinical trials and prospective studies will further help define the role and precise indications for these treatment modalities in the management ofNMIBC.
ACKNOWLEDGMENTS
Research support was provided by the NIH Medical Research Scholars Program, a public-private partnership supported jointly by the NIH and contributions to the Foundation for the NIH from the American Association for Dental Research and the Colgate-Palmolive Company.
FUNDING
This research was supported by the Intramural Research Program of the National Cancer Institute, NIH and the NIH Medical Research Scholars Program.
AUTHOR CONTRIBUTIONS
All authors were involved with the performance and interpretation of data and all authors had access to data. S.G. was involved with conception of manuscript.
CONFLICTS OF INTEREST
S.G. and N.R. have no conflicts of interest to report.
REFERENCES
[1] | Siegel RL , Giaquinto AN , Jemal A . Cancer statistics, 2024. CA Cancer J Clin. (2024) ;74: (1):12–49. doi: 10.3322/caac.21820. |
[2] | Jubber I , Ong S , Bukavina L , et al. Epidemiology of Bladder Cancer in 2023: A Systematic Review of Risk Factors. Eur Urol. (2023) ;84: (2):176–90. doi: 10.1016/j.eururo.2023.03.029. |
[3] | Sylvester RJ , van der Meijden AP , Oosterlinck W , et al. Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur Urol. (2006) ;49: (3):466–5; discussion 475-7. doi: 10.1016/j.eururo.2005.12.031. |
[4] | Fernandez-Gomez J , Madero R , Solsona E , et al. Predicting nonmuscle invasive bladder cancer recurrence and progression in patients treated with bacillus Calmette-Guerin: the CUETO scoring model. J Urol.. (2009) ;182: (5):2195–203. doi: 10.1016/j.juro.2009.07.016. |
[5] | Matulay JT , Li R , Hensley PJ , et al. Contemporary Outcomes of Patients with Nonmuscle-Invasive Bladder Cancer Treated with bacillus Calmette-Guerin: Implications for Clinical Trial Design. J Urol. (2021) ;205: (6):1612–21. doi: 10.1097/JU.0000000000001633. |
[6] | Balar AV , Kamat AM , Kulkarni GS , et al. Pembrolizumab monotherapy for the treatment of high-risk non-muscle-invasive bladder cancer unresponsive to BCG (KEYNOTE-057): an open-label, single-arm, multicentre, phase 2 study. Lancet Oncol (2021) ;22: (7):919–30. doi: 10.1016/S1470-2045(21)00147-9. |
[7] | Cervigni M . Interstitial cystitis/bladder pain syndrome and glycosaminoglycans replacement therapy. Transl Androl Urol. (2015) ;4: (6):638–42. doi: 10.3978/j.issn.2223-4683.2015.11.04. |
[8] | Wyndaele JJJ , Riedl C , Taneja R , Lovasz S , Ueda T , Cervigni M . GAG replenishment therapy for bladder pain syndrome/interstitial cystitis. Neurourol Urodyn. (2019) ;38: (2):535–44. doi: 10.1002/nau.23900. |
[9] | van der Heijden AG , Dewhirst MW . Effects of hyperthermia in neutralising mechanisms of drug resistance in non-muscle-invasive bladder cancer. Int J Hyperthermia. (2016) ;32: (4):434–45. doi: 10.3109/02656736.2016.1155761. |
[10] | Jafari NV , Rohn JL . The urothelium: a multi-faceted barrier against a harsh environment. Mucosal Immunol. (2022) ;15: (6):1127–42. doi: 10.1038/s41385-022-00565-0. |
[11] | Wientjes MG , Badalament RA , Wang RC , Hassan F , Au JL . Penetration of mitomycin C in human bladder. Cancer Res. (1993) ;53: (14):3314–20. (https://www.ncbi.nlm.nih.gov/pubmed/8324743). |
[12] | Wientjes MG , Badalament RA , Au JL . Penetration of intravesical doxorubicin in human bladders. Cancer Chemother Pharmacol. (1996) ;37: (6):539–46. doi: 10.1007/s002800050426. |
[13] | Seegenschmiedt MH , Vernon CC . A Historical Perspective on Hyperthermia in Oncology. In: Seegenschmiedt MH, Fessenden P, Vernon CC, eds. Thermoradiotherapy and Thermochemotherapy: Biology, Physiology, Physics. Berlin, Heidelberg: Springer Berlin Heidelberg; (1995) ;3–44. |
[14] | Partanen A , Yarmolenko PS , Viitala A , et al. Mild hyperthermia with magnetic resonance-guided high-intensity focused ultrasound for applications in drug delivery. Int J Hyperthermia. (2012) ;28: (4):320–36. doi: 10.3109/02656736.2012.680173. |
[15] | Tydings C , Sharma KV , Kim A , Yarmolenko PS . Emerging hyperthermia applications for pediatric oncology. Adv Drug Deliv Rev. (2020) ;163-164: :157–67. doi: 10.1016/j.addr.2020.10.016. |
[16] | Colombo R , Lev A , Pozzo LFD , Freschi M , Gallus G , Rigatti P . Original Articles: Bladder Cancer: A New Approach Using Local Combined Microwave Hyperthermia and Chemotherapy in Superficial Transitional Bladder Carcinoma Treatment. Journal of Urology. (1995) ;153: (3S):959–63. doi: 10.1016/S0022-5347(01)67613-4. |
[17] | Colombo R , Salonia A , Leib Z , Pavone-Macaluso M , Engelstein D . Long-term outcomes of a randomized controlled trial comparing thermochemotherapy with mitomycin-C alone as adjuvant treatment for non-muscle-invasive bladder cancer (NMIBC). BJU Int. (2011) ;107: (6):912–8. doi: 10.1111/j.1464-410X.2010.09654.x. |
[18] | van der Heijden AG , Kiemeney LA , Gofrit ON , et al. Preliminary European results of local microwave hyperthermia and chemotherapy treatment in intermediate or high risk superficial transitional cell carcinoma of the bladder. Eur Urol. (2004) ;46: (1):65–71; discussion 71-2. doi: 10.1016/j.eururo.2004.01.019. |
[19] | Moskovitz B , Meyer G , Kravtzov A , Gross M , Kastin A , Biton K , Nativ O . Thermo-chemotherapy for intermediate or high-risk recurrent superficial bladder cancer patients. Ann Oncol. (2005) ;16: (4):585–9. doi: 10.1093/annonc/mdi124. |
[20] | Moskovitz B , Halachmi S , Moskovitz M , Nativ O , Nativ O . 10-year single-center experience of combined intravesical chemohyperthermia for nonmuscle invasive bladder cancer. Future Oncol. (2012) ;8: (8):1041–9. doi: 10.2217/fon.12.90. |
[21] | Colombo R , Da Pozzo LF , Salonia A , et al. Multicentric study comparing intravesical chemotherapy alone and with local microwave hyperthermia for prophylaxis of recurrence of superficialtransitional cell carcinoma. J Clin Oncol. (2003) ;21: (23):4270–6. doi: 10.1200/JCO.2003.01.089. |
[22] | Arends TJ , Nativ O , Maffezzini M , et al. Results of a Randomised Controlled Trial Comparing Intravesical Chemohyperthermia with Mitomycin C Versus Bacillus Calmette-Guerin for Adjuvant Treatment of Patients with Intermediate- and High-risk Non-Muscle-invasiveBladder Cancer. Eur Urol. (2016) ;69: (6):1046–52. doi: 10.1016/j.eururo.2016.01.006. |
[23] | Tan WS , Panchal A , Buckley L , et al. Radiofrequency-induced Thermo-chemotherapy Effect Versus a Second Course of Bacillus Calmette-Guerin or Institutional Standard in Patients with Recurrence of Non-muscle-invasive Bladder Cancer Following Induction or Maintenance Bacillus Calmette-Guerin Therapy (HYMN): A Phase III, Open-label, Randomised Controlled Trial. Eur Urol. (2019) ;75: (1):63–71. doi: 10.1016/j.eururo.2018.09.005. |
[24] | Brummelhuis ISG , Wimper Y , Witjes-van Os H , Arends TJH , van der Heijden AG , Witjes JA . Long-Term Experience with Radiofrequency-Induced Hyperthermia Combined with Intravesical Chemotherapy for Non-Muscle Invasive Bladder Cancer. Cancers (Basel). (2021) ;13: (3). doi: 10.3390/cancers13030377. |
[25] | Halachmi S , Moskovitz B , Maffezzini M , et al. Intravesical mitomycin C combined with hyperthermia for patients with T1G3 transitional cell carcinoma of the bladder. Urol Oncol. (2011) ;29: (3):259–64. doi: 10.1016/j.urolonc.2009.02.012. |
[26] | Alfred Witjes J , Hendricksen K , Gofrit O , Risi O , Nativ O . Intravesical hyperthermia and mitomycin-C for carcinoma in situ of the urinary bladder: experience of the European Synergo working party. World J Urol. (2009) ;27: (3):319–24. doi: 10.1007/s00345-009-0384-2. |
[27] | Plata A , Guerrero-Ramos F , Garcia C , et al. Long-Term Experience with Hyperthermic Chemotherapy (HIVEC) Using Mitomycin-C in Patients with Non-Muscle Invasive Bladder Cancer in Spain. J Clin Med. (2021) ;10: (21). doi: 10.3390/jcm10215105. |
[28] | Magalhaes JC , Sousa M , Basto R , et al. Adjuvant Hyperthermic Intravesical Chemotherapy in Intermediate- and High-Risk Non-muscle Invasive Bladder Cancer. Cureus. (2023) ;15: (9):e45672. doi: 10.7759/cureus.45672. |
[29] | Conroy S , Pang K , Jubber I , et al. Hyperthermic intravesical chemotherapy with mitomycin-C for the treatment of high-risk non-muscle-invasive bladder cancer patients. BJUI Compass. (2023) ;4: (3):314–21. doi: 10.1002/bco2.203. |
[30] | Guerrero-Ramos F , Gonzalez-Padilla DA , Gonzalez-Diaz A , de la Rosa-Kehrmann F , Rodriguez-Antolin A , Inman BA , Villacampa-Auba F . Recirculating hyperthermic intravesical chemotherapy with mitomycin C (HIVEC) versus BCG in high-risk non-muscle-invasive bladder cancer: results of the HIVEC-HR randomized clinical trial. World J Urol. (2022) ;40: (4):999–1004. doi: 10.1007/s00345-022-03928-1. |
[31] | Angulo JC , Alvarez-Ossorio JL , Dominguez-Escrig JL , et al. Hyperthermic Mitomycin C in Intermediate-risk Non-muscle-invasive Bladder Cancer: Results of the HIVEC-1 Trial. Eur Urol Oncol. (2023) ;6: (1):58–66. doi: 10.1016/j.euo.2022.10.008. |
[32] | Tan WS , Prendergast A , Ackerman C , et al. Adjuvant Intravesical Chemohyperthermia Versus Passive Chemotherapy in Patients with Intermediate-risk Non-muscle-invasive Bladder Cancer (HIVEC-II): A Phase 2, Open-label, Randomised Controlled Trial. Eur Urol. (2023) ;83: (6):497–504. doi: 10.1016/j.eururo.2022.08.003. |
[33] | Sousa A , Inman BA , Pineiro I , et al. A clinical trial of neoadjuvant hyperthermic intravesical chemotherapy (HIVEC) for treating intermediate and high-risk non-muscle invasive bladder cancer. Int J Hyperthermia. (2014) ;30: (3):166–70. doi: 10.3109/02656736.2014.900194. |
[34] | Sousa A , Pineiro I , Rodriguez S , et al. Recirculant hyperthermic IntraVEsical chemotherapy (HIVEC) in intermediate-high-risk non-muscle-invasive bladder cancer. Int J Hyperthermia. (2016) ;32: (4):374–80. doi: 10.3109/02656736.2016.1142618. |
[35] | Grimberg DC , Dudinec J , Shah A , Inman BA . Clinical trial of high dose hyperthermic intravesical mitomycin C for intermediate and high-risk non-muscle invasive bladder cancer during BCG shortage. Urol Oncol. (2021) ;39: (8):498e13-e20. doi: 10.1016/j.urolonc.2020.12.025. |
[36] | Pijpers OM , Hendricksen K , Mostafid H , et al. Long-term efficacy of hyperthermic intravesical chemotherapy for BCG-unresponsive non-muscle invasive bladder cancer. Urol Oncol. (2022) ;40: (2):62 e13-e20. doi: 10.1016/j.urolonc.2021.07.019. |
[37] | Pignot G , Baboudjian M , Lebacle C , et al. Efficacy of hyperthermic intravesical chemotherapy (HIVEC) in patients with non-muscle invasive bladder cancer after BCG failure. World J Urol. (2023) ;41: (11):3195–203. doi: 10.1007/s00345-023-04332-z. |
[38] | Tan WP , Chang A , Brousell SC , et al. Safety and efficacy of intravesical chemotherapy and hyperthermia in the bladder: results of a porcine study. Int J Hyperthermia. (2020) ;37: (1):854–60. doi: 10.1080/02656736.2020.1780328. |
[39] | Milla P , Fiorito C , Soria F , Arpicco S , Cattel L , Gontero P . Intravesical thermo-chemotherapy based on conductive heat: a first pharmacokinetic study with mitomycin C in superficial transitional cell carcinoma patients. Cancer Chemother Pharmacol. (2014) ;73: (3):503–9. doi: 10.1007/s00280-014-2381-4. |
[40] | Soria F , Milla P , Fiorito C , et al. Efficacy and safety of a new device for intravesical thermochemotherapy in non-grade 3 BCG recurrent NMIBC: a phase I-II study. World J Urol. (2016) ;34: (2):189–95. doi: 10.1007/s00345-015-1595-3. |
[41] | Ekin RG , Akarken I , Zorlu F , Tarhan H , Kucuk U , Yildirim Z , Divrik RT . Intravesical bacillus Calmette-Guerin versus chemohyperthermia for high-risk non-muscle-invasive bladder cancer. Can Urol Assoc J. (2015) ;9: (5-6):E278–83. doi: 10.5489/cuaj.2708. |
[42] | Gozen AS , Umari P , Scheitlin W , Su FE , Akin Y , Rassweiler J . Effectivity of intravescical thermo-chemotherapy prophylaxis for patients with high recurrence and progression risk for non-muscle invasive bladder cancer. Arch Ital Urol Androl. (2017) ;89: (2):102–5. doi: 10.4081/aiua.2017.2.102. |
[43] | Inman BA , Stauffer PR , Craciunescu OA , Maccarini PF , Dewhirst MW , Vujaskovic Z . A pilot clinical trial of intravesical mitomycin-C and external deep pelvic hyperthermia for non-muscle-invasive bladder cancer. Int J Hyperthermia. (2014) ;30: (3):171–5. doi: 10.3109/02656736.2014.882021. |
[44] | Wen YC , Lee LM , Lin YW , et al. Loco-regional deep hyperthermia combined with intravesical Mitomycin instillation reduces the recurrence of non-muscle invasive papillary bladder cancer. Int J Hyperthermia. (2021) ;38: (1):1627–32. doi: 10.1080/02656736.2021.2001582. |
[45] | Di Stasi SM , Vespasiani G , Giannantoni A , Massoud R , Dolci S , Micali F . Electromotive delivery of mitomycin C into human bladder wall. Cancer Res. (1997) ;57: (5):875–80. (https://www.ncbi.nlm.nih.gov/pubmed/9041189). |
[46] | Di Stasi SM , Giannantoni A , Massoud R , Dolci S , Navarra P , Vespasiani G , Stephen RL . Electromotive versus passive diffusion of mitomycin C into human bladder wall: concentration-depth profiles studies. Cancer Res. (1999) ;59: (19):4912–8. (https://www.ncbi.nlm.nih.gov/pubmed/10519404) |
[47] | Kalsi J , Harland SJ , Feneley MR . Electromotive drug administration with mitomycin C for intravesical treatment of non-muscle invasive transitional cell carcinoma. Expert Opin Drug Deliv. (2008) ;5: (1):137–45. doi: 10.1517/17425247.5.1.137. |
[48] | Gurpinar T , Truong LD , Wong HY , Griffith DP . Electromotive drug administration to the urinary bladder: an animal model and preliminary results. J Urol. (1996) ;156: (4):1496–501. (https://www.ncbi.nlm.nih.gov/pubmed/8808916). |
[49] | Lugnani F , Mazza G , Cerulli N , Rossi C , Stephen R . Iontophoresis of drugs in the bladder wall: equipment and preliminary studies. Artif Organs. (1993) ;17: (1):8–17. doi: 10.1111/j.1525-1594.1993.tb00378.x. |
[50] | Carando R , Zazzara M , Cotrufo S , Ludovico GM . Intravesical Treatment with Electro-Mediated Administration of Mytomicin C as Prophylaxis for Intermediate and High-Risk Nonmuscle-Invasive Bladder Cancer: A Retrospective Multicenter Study. Urol Int. (2019) ;103: (3):285–90. doi: 10.1159/000502663. |
[51] | Juvet T , Mari A , Lajkosz K , et al. Sequential administration of Bacillus Calmette-Guerin (BCG) and Electromotive Drug Administration (EMDA) of mitomycin C (MMC) for the treatment of high-grade nonmuscle invasive bladder cancer after BCG failure. Urol Oncol. (2020) ;38: (11):850e9-e15. doi: 10.1016/j.urolonc.2020.06.031. |
[52] | Zazzara M , Nazaraj A , Scarcia M , Cardo G , Carando R , Ludovico GM . Electromotive Drug Administration of Mitomycin C (EMDA/MMC) versus Intravesical Immunotherapy with Bacillus Calmette-Guerin (BCG) in Intermediate and High Risk Non Muscle Invasive Bladder Cancer. Urol Int. (2023) ;107: (1):64–71. doi: 10.1159/000520630. |
[53] | Decaestecker K , Lumen N , Van Camp C , Oosterlinck W . Single ablative intravesical electromotive mitomycin C administration for small non-muscle-invasive bladder cancer: a prospective study. Acta Clin Belg. (2018) ;73: (5):324–7. doi: 10.1080/17843286.2018.1440706. |
[54] | Di Stasi SM , Giannantoni A , Stephen RL , Capelli G , Navarra P , Massoud R , Vespasiani G . Intravesical electromotive mitomycin C versus passive transport mitomycin C for high risk superficial bladder cancer: a prospective randomized study. J Urol. (2003) ;170: (3):777–82. doi: 10.1097/01.ju.0000080568.91703.18. |
[55] | Di Stasi SM , Valenti M , Verri C , et al. Electromotive instillation of mitomycin immediately before transurethral resection for patients with primary urothelial non-muscle invasive bladder cancer: a randomised controlled trial. Lancet Oncol. (2011) ;12: (9):871–9. doi: 10.1016/S1470-2045(11)70190-5. |
[56] | Di Stasi SM , Giannantoni A , Giurioli A , et al. Sequential BCG and electromotive mitomycin versus BCG alone for high-risk superficial bladder cancer: a randomised controlled trial. Lancet Oncol. (2006) ;7: (1):43–51. doi: 10.1016/S1470-2045(05)70472-1. |
[57] | Gan C , Amery S , Chatterton K , Khan MS , Thomas K , O’Brien T . Sequential bacillus Calmette-Guerin/Electromotive Drug Administration of Mitomycin C as the Standard Intravesical Regimen in High Risk Nonmuscle Invasive Bladder Cancer: 2-Year Outcomes. J Urol. (2016) ;195: (6):1697–703. doi: 10.1016/j.juro.2016.01.103. |
[58] | Di Gianfrancesco L , Ragonese M , Palermo G , Sacco E , Bassi P , Racioppi M . Second-Line Conservative Device-Assisted Intravesical Treatment in Selected Patients With Recurrent High-Risk Non-Muscle-Invasive Bladder Cancer. Clin Genitourin Cancer. (2021) ;19: (2):e100–19. doi: 10.1016/j.clgc.2020.11.002. |
[59] | Racioppi M , Di Gianfrancesco L , Ragonese M , Palermo G , Sacco E , Bassi PF . ElectroMotive drug administration (EMDA) of Mitomycin C as first-line salvage therapy in high risk “BCG failure” non muscle invasive bladder cancer: 3 years follow-up outcomes. BMC Cancer. (2018) ;18: (1):1224. doi: 10.1186/s12885-018-5134-7. |
[60] | Brausi M , Campo B , Pizzocaro G , et al. Intravesical electromotive administration of drugs for treatment of superficial bladder cancer: a comparative Phase II study. Urology. (1998) ;51: (3):506–9. doi: 10.1016/s0090-4295(97)00625-0. |
[61] | Riedl CR , Knoll M , Plas E , Pfluger H . Intravesical electromotive drug administration technique: preliminary results and side effects. J Urol. (1998) ;159: (6):1851–6. doi: 10.1016/S0022-5347(01)63174-4. |
[62] | Colombo R , Brausi M , Da Pozzo L , et al. Thermo-chemotherapy and electromotive drug administration of mitomycin C in superficial bladder cancer eradication. a pilot study on marker lesion. Eur Urol. (2001) ;39: (1):95–100. doi: 10.1159/000052419. |
[63] | Tan WS , Kelly JD . Intravesical device-assisted therapies for non-muscle-invasive bladder cancer. Nat Rev Urol. (2018) ;15: (11):667–85. doi: 10.1038/s41585-018-0092-z. |
[64] | Daneshmand S , Brummelhuis ISG , Pohar KS , et al. The safety, tolerability, and efficacy of a neoadjuvant gemcitabine intravesical drug delivery system (TAR-200) in muscle-invasive bladder cancerpatients: a phase I trial. Urol Oncol. (2022) ;40: (7):344e1-e9. doi: 10.1016/j.urolonc.2022.02.009. |
[65] | Grimberg DC , Shah A , Inman BA . Overview of Taris GemRIS, a Novel Drug Delivery System for Bladder Cancer. Eur Urol Focus. (2020) ;6: (4):620–2. doi: 10.1016/j.euf.2019.09.006. |
[66] | Nickel JC , Jain P , Shore N , et al. Continuous intravesical lidocaine treatment for interstitial cystitis/bladder pain syndrome: safety and efficacy of a new drug delivery device. Sci Transl Med. (2012) ;4: (143):143ra100. doi: 10.1126/scitranslmed.3003804. |
[67] | Valenberg FJPv , Heijden Tvd , Cutie C , et al. Safety, tolerability, and preliminary efficacy of TAR-200 in patients with intermediate risk non– muscle-invasive bladder cancer: A phase 1 study. Journal of Clinical Oncology. (2023) ;41: (6_suppl):505–505. doi: 10.1200/JCO.2023.41.6_suppl.505. |
[68] | Daneshmand S , Heijden MSvd , Jacob JM , et al. LBA02-03 First Results From SunRISE-1 In Patients With BCG Unresponsive High-Risk Non–Muscle-Invasive Bladder Cancer Receiving TAR-200 In Combination With Cetrelimab, TAR-200, or cetrelimab alone. Journal of Urology. (2023) ;209: (Supplement 4):e1187. doi: 10.1097/JU.0000000000003361.03. |
[69] | Vilaseca A , Jayram G , Raventos C , et al. LBA104 First safety and efficacy results of the TAR-210 erdafitinib (erda) intravesical delivery system in patients (pts) with non-muscle-invasive bladder cancer (NMIBC) with select FGFR alterations (alt). Annals of Oncology. (2023) ;34: :S1343. doi: 10.1016/j.annonc.2023.10.110. |




