Challenging Cases in Urothelial Cancer: Case 30: Rare Complication of BCG
A 70-year-old physician had the onset of gross hematuria in July 2018. His general health was good. He had a history of seminoma of the right testis in 1986 which was treated with an inguinal orchiectomy followed by external beam radiation. He believes the radiation field might have included part of the pelvis.
In addition to a single episode of gross hematuria he had urinary frequency. He did not have a urinary tract infection. His physical examination was normal. The prostate was small. His PSA was 0.75. He had a low testosterone and was taking topical testosterone. He never smoked cigarettes.
A renal ultrasound was normal. A flexible cystoscopy was unremarkable. Urinary cytology indicated atypical cells. An episode of gross hematuria occurred again in October 2019. Another cystoscopy was performed and was normal. The prostate was small.
In October 2020 he was evaluated for increasing urinary frequency. He had nocturia 2-3 times and daytime frequency every 2-3 hours despite not drinking a lot of fluids or caffeine products. A residual urine was 200 ml.
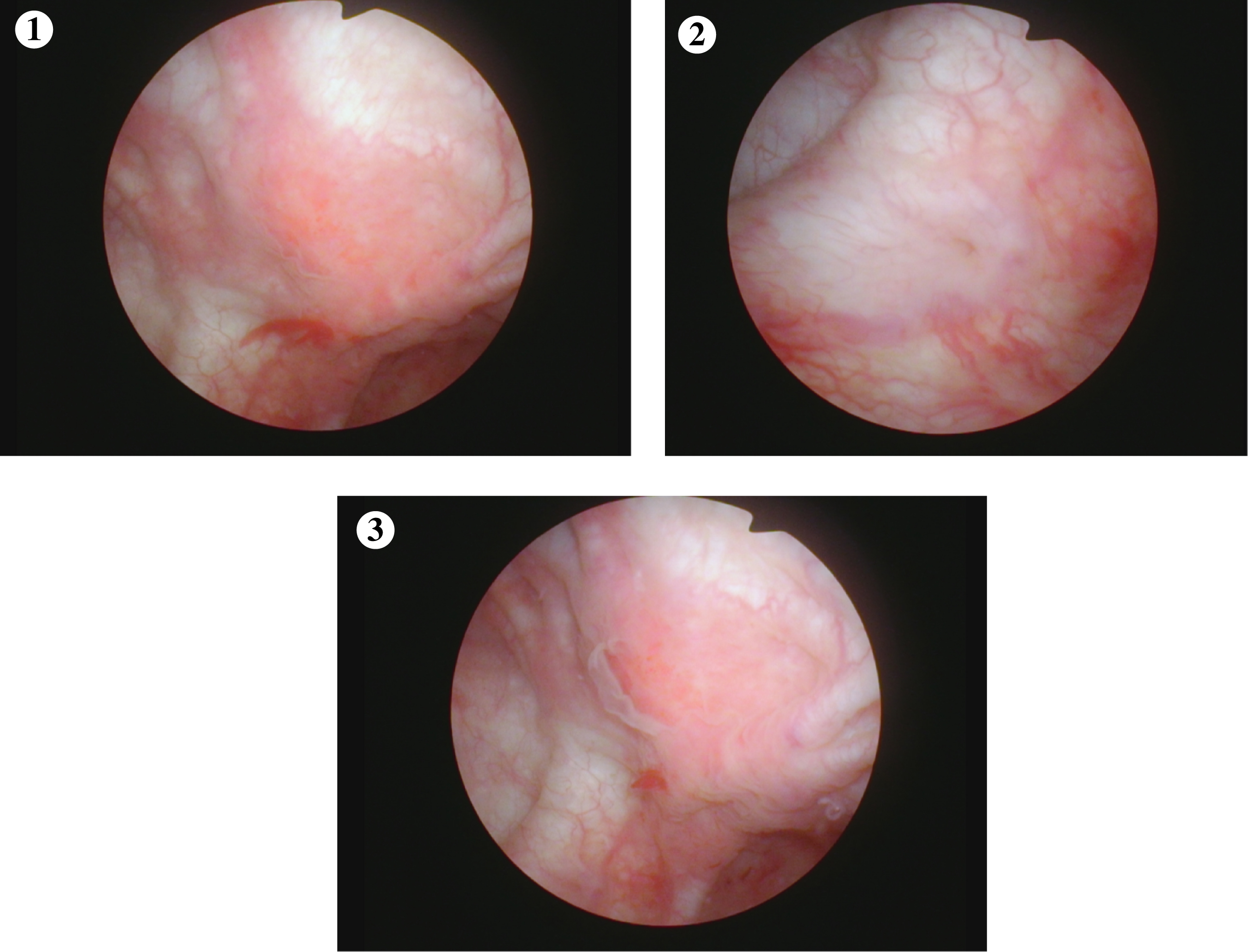
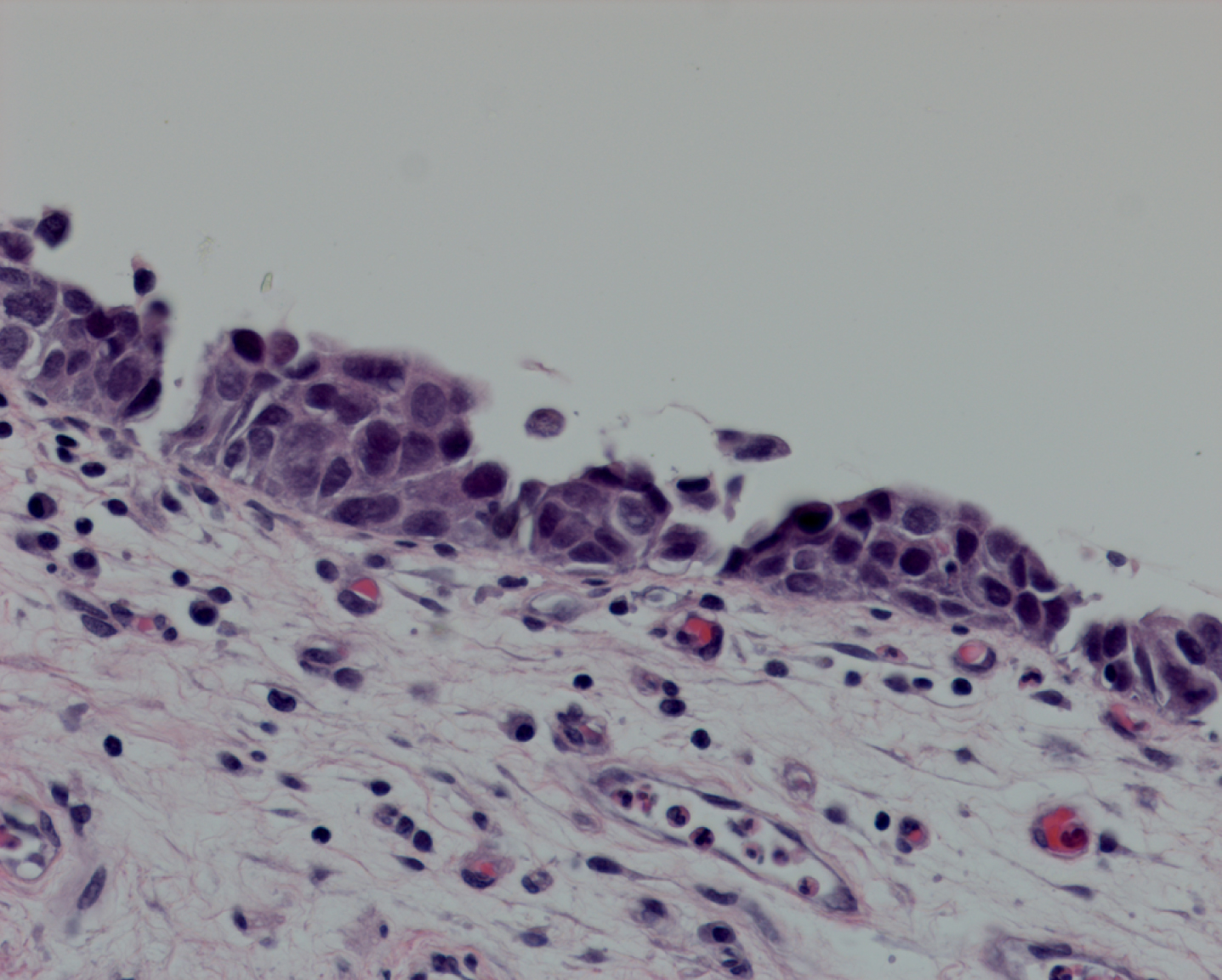
In June 2021 the frequency increased and a urine analysis showed microhematuria and a cystoscopy was performed. There was an erythematous raised area on the left wall of the bladder. (Figs. 1–3). A transurethral resection was performed. The pathology indicated a small high grade urothelial carcinoma which invaded the lamina propria, T1. One month later, August 2021, he underwent a repeat TUR BT and the diagnosis was carcinoma in situ (CIS) (Fig. 4). There was no papillary tumor and no invasion. Muscle was present and uninvolved on each of the TUR BTs.
Fig. 1–3
Cystoscopic views of the bladder. Slightly raised and erythematous area on the left lateral wall.
He received 6 weeks of intravesical BCG. He tolerated it well. The cystoscopy after the BCG was negative however, the cytology was suspicious for high grade cancer. He received maintenance BCG for three weeks.
Beginning in January 2022 his lower urinary tract symptoms became much worse. He had increasing urinary frequency and eventually urgency and urge incontinence. A few months later he had nocturia hourly. Cystoscopy was performed and no cancer was identified however the bladder urothelium looked abnormal. There was a lot of inflammation. Urine cytology indicated atypical cells.
Fig. 4
Carcinoma in situ.
A variety of medications for overactive bladder were tried without improvement and a decision was made to perform a cystoprostectomy because his quality of life was dramatically altered as a result of his urinary frequency and incontinence. There was some concern that urothelial cancer might be a factor causing his symptoms. The main objective, however, was to allow him to resume a more normal life as the LUTS were such that he was home bound.
The cystoprostatectomy and ileal conduit urinary diversion was performed in October 2022. The postoperative course was complicated by a small bowel obstruction requiring lysis of adhesions on day 10. He had an intermittent fever despite negative blood cultures and a normal white blood cell count. This prompted an infectious disease consultation.
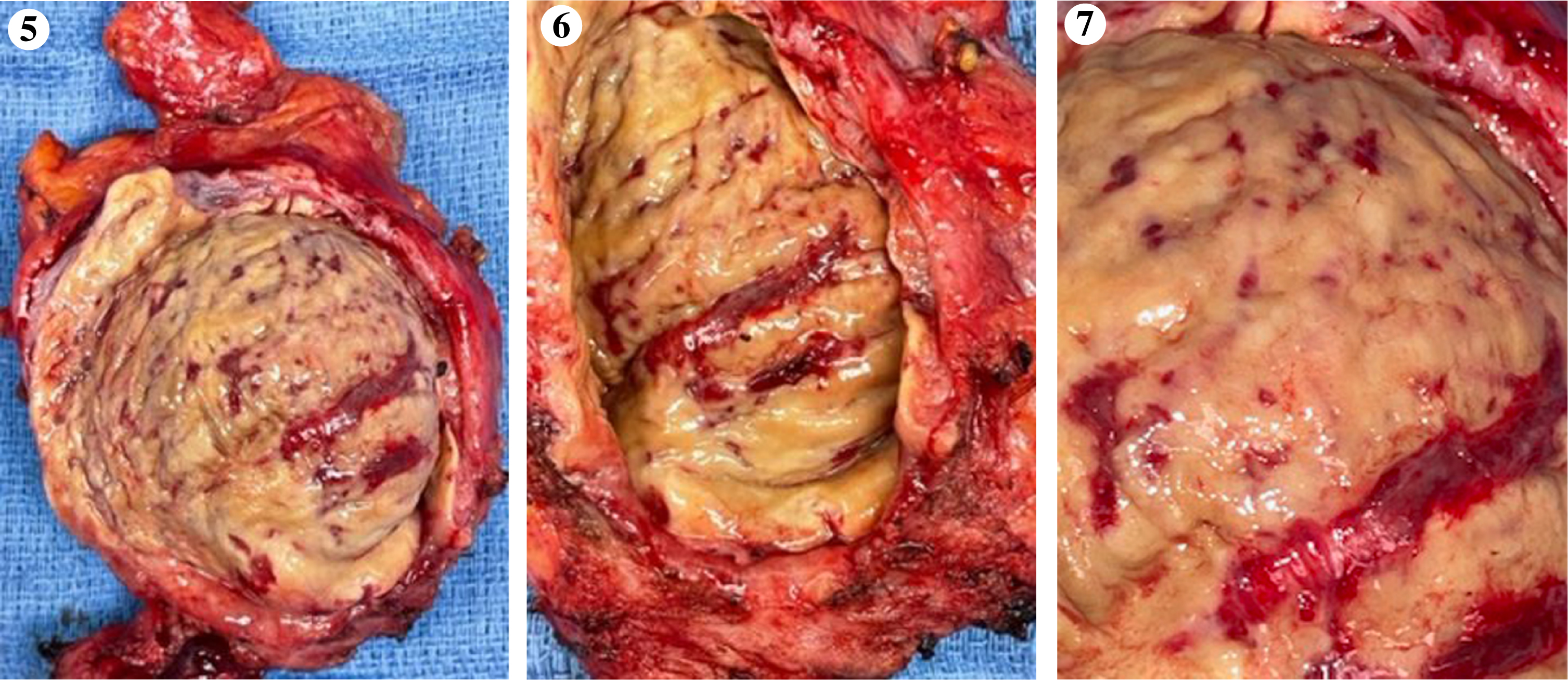
The bladder was examined after it was removed and revealed an extensive yellow fibrinous exudate covering the entire bladder (Figs. 5–7). The pathology report indicated no bladder cancer however, the histology was remarkable for diffuse mucosal necrosis encompassing the entire bladder extending into the muscularis propria and the prostatic urothelium. There were areas of granulomatous inflammation. Given the history of intravesical BCG therapy stains for acid fast bacilli were performed and were positive for mycobacterium. There were rare fungal hyphae.
Fig. 5–7
Necrotic bladder. Entire bladder has been destroyed by the intense fibranous reaction.
The patient received isoniazid and rifampin for six months.
The remainder of his recovery was uneventful with the exception of an obstructing calculous at the left ureteroileal junction which required placement of a nephroureteral stent. This was subsequently internalized with a stent exiting from the stoma and will be changed periodically. Hopefully this will be removed once ensuring there is no stenosis of the ureter at its entrance into the ileal segment.
His quality of life is back to normal and he is cancer free.
Extensive necrosis of the bladder following intravesical BCG is rare [1–4]. Although this man had radiation delivered 25 years earlier it is unlikely this played a part in this process. The radiation was for testis tumor and the patient had minimal voiding complaints prior to the diagnosis of bladder cancer and its treatment.
BCG has been extensively used for the treatment of urothelial carcinoma in situ and for prophylaxis following transurethral resection of high grade Ta or T1 urothelial cancer of the bladder. Although the vast majority of patients receive BCG with few side effects and the majority of those that occur are limited to transient dysuria or urinary frequency, there is a risk of serious systemic and local toxicity. This is why BCG is not indicated for the treatment or prophylaxis for low grade urothelial cancer of the bladder. In such cases when intravesical therapy is indicated intravesical chemotherapy is preferable.
Bladder ulceration and bladder contracture have been reported following intravesical BCG. These are rare events however side effects may not be reported so the incidence is difficult to determine. The extensive necrosis identified in this patient and the finding of mycobacterium in the tissue months after BCG instillation leave little doubt as to the cause of the tissue destruction in this case.
INFORMED CONSENT
Written informed consent for publication was obtained from the patient.
ETHICAL CONSIDERATIONS
The author has institutional review board approval for reviewing bladder cancer cases for outcome (MHS.2020.026).
CONFLICT OF INTEREST
Nothing to disclose.
REFERENCES
[1] | Asin MA , Fernandez-Ruiz M , Lopez-Medrano F , et al. Bacillus Calmette –Guerin (BCG) infection following intravesical administration as adjunctive therapy for bladder cancer. Medicine ((2014) );93: , 236–54. |
[2] | Strock V , Dotevail L , Sandberg T ,et al. Late bacillus Calmette-Guerin infection with a large focal urinary bladder ulceration as a complication of bladder cancer treatment. BJUI Int.-7. ((2011) );107: :1592–7. |
[3] | Hameed A , Sezian N , Thwain A . Bladder contracture: A review for intravesical bacillus Calmette-Guerin complication. Can J Urol. ((2007) );14: :3745–9. |
[4] | Nieder A , Sved P , Stein JP , et al. Cystoprostatectomy and orthotopic ileal neobladder reconstruction for management of bacillus Calmette-Guerin- induced bladder contracture. Urology. ((2005) );65: :909–12. |




