Noninvasive Tests for Bladder Cancer Detection and Surveillance: A Systematic Review of Commercially Available Assays
Abstract
BACKGROUND:
An important reason for the high health care costs associated with bladder cancer is the need for frequent cystoscopy for detection and surveillance of this disease. Cytologic analysis of voided urine specimens can assist, but is too inaccurate to replace cystoscopy. In an effort to create reliable, objective, noninvasive mechanisms for detecting bladder cancer, a number of urine-based molecular tests have been developed with the ultimate goal of reducing the frequency of cystoscopy.
OBJECTIVE:
To summarize the performance of urine-based biomarker tests, currently commercially available in the US, as part of the initial workup for hematuria and for bladder cancer surveillance.
METHODS:
In accordance with PRISMA guidelines we performed a systematic review of the literature on the performance of NMP22, BTA, UroVysion, ImmunoCyt/uCyt, CxBladder, and Bladder EpiCheck. Median sensitivity, specificity, negative (NPV) and positive predictive values (PPV) were calculated for each test based on the included studies.
RESULTS:
Twenty-eight studies met inclusion criteria for the performance of five urine-based biomarker tests in the setting hematuria workup. Median sensitivity ranged from 65.7% –100% and specificity ranged from 62.5% –93.8%. Median NPV ranged from 94.2% –98.3% and PPV ranged from 29% –58.7%. Fourteen studies met inclusion criteria for the performance of six tests in the setting of bladder cancer surveillance. Median sensitivity ranged from 22.6% –92.0% and specificity from 20.5% –97.9%. Median NPV ranged from 52.9% –96.5% and PPV ranged from 48.1% –75.7%.
CONCLUSIONS:
Our analysis finds that while these tests may provide some clinical utility, none of the assays have thus far demonstrated objective evidence to supplant the gold diagnostic standard.
INTRODUCTION
Bladder cancer is the sixth most common malignancy in the United States (US) with approximately 83,190 new cases projected in 2024 [1]. Painless hematuria, whether gross or microscopic, is frequently the presenting symptom that prompts referral to a urologist. About 80% of patients diagnosed with bladder cancer will have non-muscle invasive (NMIBC) disease [2]. Up to 50% of these patients will experience recurrence after treatment, a fraction of whom will progress to muscle-invasive bladder cancer.
Effective bladder cancer management is dependent in large part on early detection where the disease may be at an early stage when therapy can be most effectively administered. The gold standard for detecting bladder cancer in patients undergoing workup for hematuria and those with NMIBC on surveillance is cystoscopy, however this procedure is invasive and contributes significantly to the overall cost of bladder cancer management, which is the most expensive cancer to treat per person in the US. Noninvasive tools for bladder cancer detection are also utilized. Urine cytology is a laboratory-based diagnostic test that is often obtained in combination with cystoscopy. Although noninvasive and highly specific, cytology suffers from low sensitivity for the detection of low-grade bladder tumors and results can be influenced by inter-operator variability [5]. Several factors contribute to the poor sensitivity: only a small volume of urine can be processed, and only a fraction of the sample can be used for final analysis. This reduces the likelihood of capturing tumor cells. “Background” cells including red blood cells and leukocytes also confound the analysis [6]. Furthermore, cytologic criteria that differentiate between low-grade tumors and reactive cells can be ambiguous. The low sensitivity limits the potential of urine cytology for sole use in detection protocols.
As bladder is the exclusive reservoir of urine, urine serves as a more specific medium for detection of urologic tumor markers than serum. Further, “accessing” the bladder via urine makes noninvasive detection feasible. Noninvasive urine-based tests for bladder cancer detection are currently not recommended by the American Urological Association guidelines and have yet to replace cytology [7, 8]. These tests are based on the detection of a wide variety of molecules, use an array of technology platforms, and are in different phases of development. While the ultimate goal of these biomarkers is to reduce unnecessary cystoscopies, ideal test characteristics are dependent upon the clinical scenario. In the workup of hematuria where most patients will not have malignancy, the ideal urine-based test would have a high positive predictive value (PPV) and high specificity. In patients with a history of bladder cancer on surveillance, the clinical suspicion for cancer is much higher and the ideal test would have a high negative predictive value (NPV) and high sensitivity.
In an effort to create a focused evaluation useful to the practicing clinician, we performed a systematic review of noninvasive urine-based biomarker tests commercially available in the US. We analyzed the performance of these standalone assays in the settings of hematuria workup and for bladder cancer surveillance [9, 10].
MATERIALS AND METHODS
Search strategy
This study was registered at the International Prospective Register of Systematic Reviews (PROSPERO ID: CRD42024497090) and performed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. We conducted a systematic review of all available literature meeting the search criteria for urine-based biomarker tests for the detection of bladder cancer currently available in the US. Literature search was performed on PubMed using keywords “bladder cancer” or “bladder neoplasm” or “bladder carcinoma”, and “biomarkers” or “urine biomarkers.”
Study selection
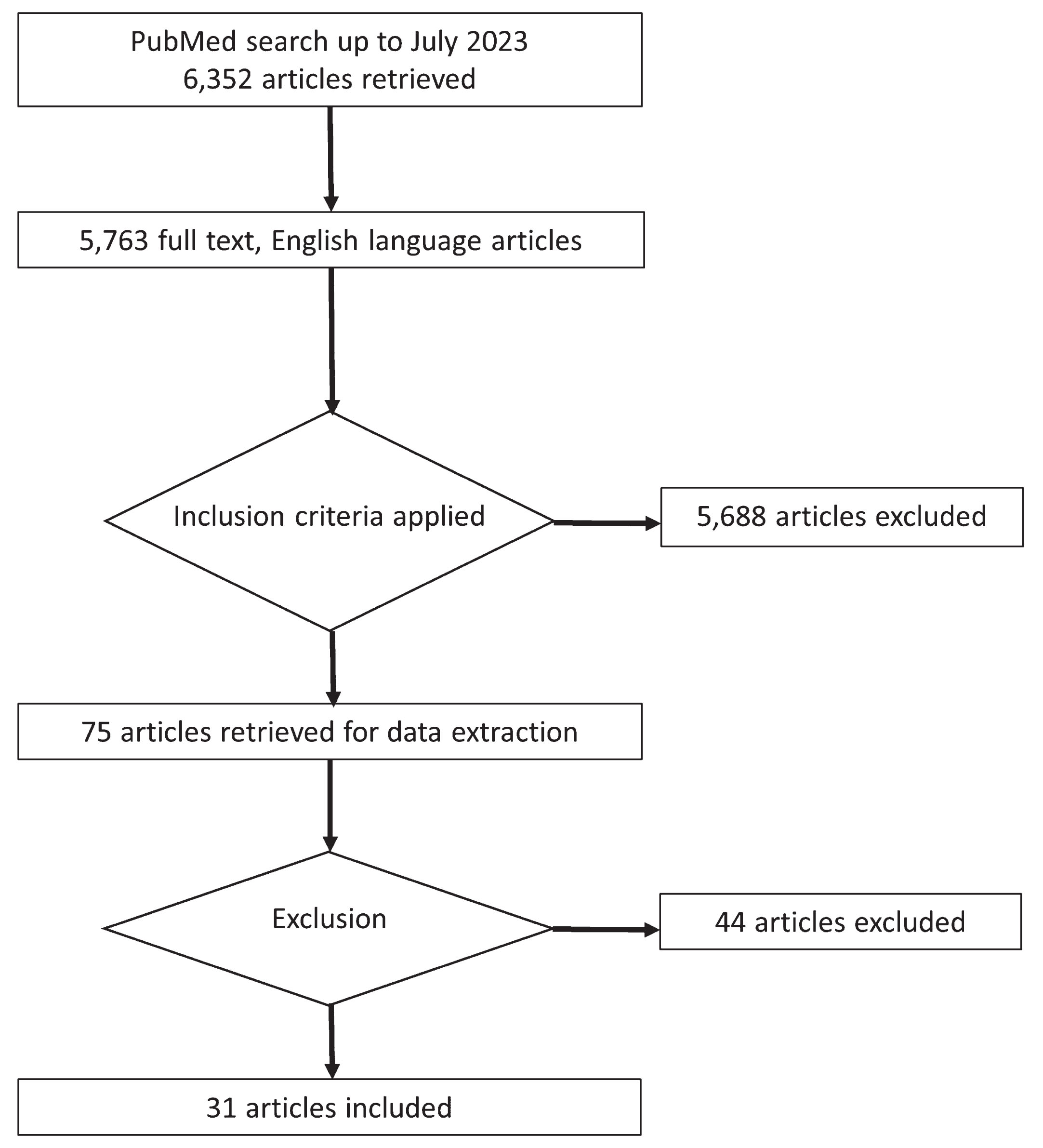
A schema of the study selection process is shown in Fig. 1. From the overall search strategy described above, only articles available with full text and in the English language were selected. Abstracts were then screened and those based on the study of biomarkers commercially available as of July 2023 were included. These included NMP22, BTA, UroVysion, ImmunoCyt/uCyt, CxBladder, and Bladder EpiCheck. Studies were then excluded if they had fewer than 15 patients, examined biomarker performance only in combination with another test, studied biomarker performance outside the setting of hematuria workup or surveillance, or the study population was limited based on patient characteristics (tumor grade, smoking status, etc.). Initial search and study selection was performed JRH, with final decisions for inclusion and exclusion made in consultation with APM. In case of initial disagreements, both coauthors again reviewed the entire study independently before reaching a consensus.
Fig. 1
Flow chart depicting the process of systematic literature selection and review in accordance with PRISMA guidelines.
Data extraction and analysis
Biomarker performance results were extracted from each selected article using a pre-defined collection form. Extracted data included publication details, number of patients overall, proportion of female patients, smoking history, number of patients in subgroups undergoing hematuria workup or NMIBC surveillance, and statistical performance of each test for the overall patient population, subgroups, and by cancer grade. Standalone biomarker test performance was determined by comparison with pathologic diagnosis on transurethral resection. Primary endpoints included test sensitivity, specificity, negative and positive predictive values in the setting of hematuria evaluation and/or bladder cancer surveillance. Test performance regarding sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV) were extracted from each study. The mean, standard deviation, median and range were then calculated for each biomarker based on the number of studies included.
RESULTS
Search results
Our initial literature search yielded 6,352 articles, of which 5,763 were in the English language and had full text available. The abstracts of these articles were screened and 75 met the inclusion criteria. The full-text articles were then evaluated; 44 studies were excluded for evaluating biomarker test performance outside the clinical scenarios of hematuria workup or bladder cancer surveillance (Fig. 1).
Table 1
Patient characteristics of included studies
| Study [Reference] | n (overall) | Age (median or mean) | Female (%) | Smoker (current or former %) | Hematuria (%) | Gross hematuria (% of all hematuria) | History of UC (% yes) | History of CIS (%) | History of high grade (%) | History of stage T1 or higher (%) | Patients with cancer detected | Detected high grade (%) | Detected CIS (%) |
| NMP 22 | |||||||||||||
| Kelly [16]a | 1677 | 63 | 38 | – | 93 | 54 | 0 | – | – | – | 222 | 30 | 4 |
| Todenhofer [22]a | 808 | 67 | 20.2 | – | n/a | – | 0 | – | – | – | 115 | 22 | 21.1 |
| Ritter [20]a,b | 198 | 70 | 23.7 | 44 | 55.2 | 26 | – | – | – | 61 | 25.9 | 5 | |
| Dogan [13]a,b | 136 | 60 | 25 | – | 64 | – | 36 | – | – | – | 45 | 29 | – |
| Grossman [14]a | 1331 | 58.7 | 43 | – | 100 | – | 0 | – | – | – | 79 | 32 | 7 |
| Bangma [12]a | 385 | – | 0 | 98.5 | 100 | – | 0 | – | – | – | 5 | 0 | – |
| O’Sullivan [19]a | 485 | 64 | 31.7 | 61 | 100 | 100 | 0 | – | – | – | 66 | 29 | 3 |
| Hwang [15]a,b | 1021 | 65 | 24 | – | 41.5 | – | 58.5 | – | – | – | 125 | 40 | 0.8 |
| Zippe [23]a | 330 | 63 | 23 | – | 54.9 | 62.8 | – | – | – | – | 18 | 55.6 | 11.1 |
| Arora [11]a | 53 | 59 | 9.4 | 66 | 100 | – | – | – | – | – | 38 | 34 | – |
| Miyanga [17]a | 309 | – | 53.1 | 100 | 0 | – | – | – | – | 22 | 50 | 4.5 | |
| Moonen [18]a | 106 | 66.4 | 25.5 | – | 26 | – | – | – | 29 | 33.8 | 20.7 | ||
| Sanchez Carabayo [21]a | 112 | 65.5 | 35 | – | 100 | 0 | – | – | – | – | 43 | 39.5 | 2.3 |
| BTA | |||||||||||||
| Kirollos [24]a,b | 98 | 67 | 30.6 | – | 25 | 62.5 | 45 | – | – | – | 27 | – | – |
| UroVysion | |||||||||||||
| Schomler [28]a,b | 216 | 65.7 | 19 | – | 31.5 | – | 50 | – | – | – | 54 | – | – |
| Lotan [27]a,b | 120 | 65 | 24 | – | 30.8 | – | 58.3 | – | – | – | 33 | – | – |
| Dimashkieh [26]a,b | 957 | – | 36 | – | 43 | – | 57 | – | – | – | 299 | – | – |
| Todenhofer [22]a | 808 | 67 | 20.2 | – | n/a | – | 0 | – | – | – | 115 | 22 | 21.1 |
| ImmunoCyt | |||||||||||||
| Deininger [31]a | 444 | 67 | 15.3 | 32.2 | 100 | – | 0 | – | – | – | 68 | – | – |
| Todenhofer [22]a | 808 | 67 | 20.2 | – | n/a | – | 0 | – | – | – | 115 | 22 | 21.1 |
| Cha [30]a,b | 1182 | 65 | 22.2 | – | 100 | 22 | – | – | – | – | 245 | 41.3 | 5.3 |
| Odisho [32]a,b | 128 | 68.8 | 14.5 | – | 36 | – | 62 | – | 56 (including CIS) | 72 | – | – | |
| Schmitz–Drager [33]a | 293 | – | – | – | 100 | 22 | – | – | – | – | 27 | 55.6 | – |
| CxBladder | |||||||||||||
| O’Sullivan [19]a | 485 | 64 | 31.7 | 61 | 100 | – | 0 | – | – | – | 66 | 29 | 3 |
| Kavalieris [10]b | 1036 | – | 18.9 | – | – | – | 100 | 10.1 | 44 | 18.7 | 156 | 46 | 18.6 |
| Lotan [9]b | 1016 | – | 22.6 | – | – | – | 100 | 9.9 | 44.6 | 18 | 151 | – | – |
| Konety [38]a,b | 852 | – | – | – | 51 | – | 48.8 | – | – | – | 94 | – | – |
| Davidson [36]a | 884 | 65 | 34 | 41 | 100 | 64 | 0 | – | – | – | 51 | 49 | 5.9 |
| Davidson [35]a | 571 | – | 32 | 47 | 100 | 64.1 | 0 | – | – | – | 44 | 66 | 20.5 |
| Kavalieris [37]a | 587 | – | 19.3 | 58.1 | 100 | 100 | 0 | – | – | – | 72 | – | – |
| EpiCheck | |||||||||||||
| Witjes [42]b | 353 | 70.5 | 22.5 | 81.6 | – | – | 100 | 10.7 | 39.3 | 26.6 | 68 | 41 | 44 |
| Trenti [40]b | 243 | 74 | 18.9 | – | – | – | 100 | 20.2 | 36.6 | 11.9 | 69 | 43 | – |
| Trenti [41]b | 487 | 74 | 22.2 | – | – | – | 100 | 12.1 | 43.8 | 17.9 | 92 | 41 | – |
| D’Andrea [39]b | 357 | 70.6 | 23 | 80.7 | – | – | 100 | 10.1 | 47.6 | 27.2 | 38 | 47 | – |
aStudy evaluated test performance in workup of hematuria or initial diagnosis. bStudy evaluated test performance in non-muscle invasive bladder cancer surveillance. n/a=percentage of patients with gross hematuria not reported. UC, urothelial carcinoma; CIS, carcinoma in situ.
Quality and design
There was substantial variation in the reporting of patient demographics, smoking status, and bladder cancer history among the included studies (Table 1). Test performance was evaluated and analyzed separately for detection in the context of hematuria workup versus surveillance. A minority of studies reported the pathologic grade of detected bladder cancer.
NMP22
Nuclear matrix proteins (NMPs) are a family of molecules involved in nuclear structure, gene expression, and DNA replication. In noncancerous cells, NMP22 contributes to chromatin distribution during cell division. However, in urothelial carcinoma, NMP22 levels are elevated due to increased cell turnover and apoptosis. Because multiple benign urologic processes including infection, inflammation, urolithiasis and urinary tract manipulation increase surface shedding and cell turnover, false positives can be seen in these settings. There are two forms of this test that are approved for use by the US Food and Drug Administration (FDA): a qualitative point-of-care test (BladderChek) and a quantitative NMP22 enzyme-linked immunosorbent assay (ELISA), for which cutoff values have not been standardized, although 10 units/mL is often used.
Our analysis included 13 studies on the use of NMP22 for workup of hematuria or irritative voiding symptoms [11–23]. The median sensitivity and specificity were 61.2% and 85.7% respectively, with NPV and PPV of 94.1% and 29.0%, respectively (Table 2). The median sensitivity for high-grade tumors was 82.3%.
Table 2
Performance of urinary biomarkers in hematuria workup for bladder cancer
| Biomarker N of studies (n of patients) | NMP22 N = 13 (6176) | BTA N = 1 (24) | UroVysion N = 4 (1756) | ImmunoCyt/uCyt N = 5 (2756) | CxBladder N = 5 (2963) | Bladder EpiCheck N = 0 |
| Sensitivity, % | ||||||
| Mean±SD | 61.2±26.3 | – | 67.6±11.3 | 85.0±7.4 | 91.0±5.6 | – |
| Median | 69.6 | 100.0 | 65.7 | 86.8 | 93.0 | – |
| Range | 20.5–100 | – | 57.1–81.8 | 73.9–93.6 | 82.0–95.5 | – |
| HG Median | 82.3 | – | 94.4 | 91.7 | 97.0 | – |
| Specificity, % | ||||||
| Mean±SD | 86.5±7.0 | – | 93.5±5.6 | 68.9±24.8 | 61.1±21.0 | – |
| Median | 85.7 | 74.0 | 93.8 | 77.4 | 62.5 | – |
| Range | 75.0–96.6 | – | 86.3–100 | 25.0–86.6 | 34.2–85.0 | – |
| NPV, % | ||||||
| Mean±SD | 90.9±9.4 | – | 77.9±35.3 | 86.7±17.8 | 98.3±0.6 | – |
| Median | 94.1 | – | 94.2 | 94.9 | 98.3 | – |
| Range | 75.0–100 | – | 25.0–97.5 | 60.0–97.0 | 97.6–98.9 | – |
| PPV, % | ||||||
| Mean±SD | 37.3±24.2 | – | 62.9±33.1 | 50.1±14.1 | – | – |
| Median | 29.0 | – | 58.7 | 51.8 | – | – |
| Range | 7.1–76.5 | – | 34.4–100 | 34.4–62.5 | – | – |
–not reported by any articles meeting study criteria. SD, standard deviation; HG, high grade
Three studies examined NMP22 for NMIBC surveillance [13, 15, 20]. The median sensitivity and specificity in these studies were 22.6% and 97.9%, respectively (Table 3). Although only reported in one study, the sensitivity was 7.1% for low-grade (LG) tumors and 12.5% for high-grade (HG) tumors. The NPV and PPV were 68.6% and 65.5%, respectively.
Table 3
Performance of urinary biomarkers in surveillance for bladder cancer.
| Biomarker N of studies (n of patients) | NMP22 N = 3 (697) | BTA N = 1 (44) | UroVysion N = 3 (1223) | ImmunoCyt/uCyt N = 1 (99) | CxBladder N = 2 (2052) | Bladder EpiCheck N = 4 (1440) |
| Sensitivity, % | ||||||
| Mean±SD | 21.6±12.0 | – | 77.2±17.0 | – | 92.0±1.4 | 65.4±2.7 |
| Median | 22.6 | 36.0 | 73.6 | 85.5 | 92.0 | 65.6 |
| Range | 9.1–33.0 | – | 62.2–95.7 | – | 91.0–93.0 | 62.3–68.2 |
| LG Median | – | – | – | – | – | 43.1 |
| HG Median | – | – | – | – | 97.0 | 86.1 |
| Specificity, % | ||||||
| Mean±SD | 91.3±13.3 | – | 85.2±1.5 | – | – | 86.1±2.8 |
| Median | 97.9 | 79.0 | 85.2 | 20.5 | – | 87.2 |
| Range | 76.0–100 | – | 84.1–86.2 | – | – | 82.1–88.0 |
| NPV, % | ||||||
| Mean±SD | 68.6±13.3 | – | 61.3±53.7 | – | 96.5±0.7 | 90.4±5.5 |
| Median | 68.6 | – | 87.7 | 52.9 | 96.5 | 91.7 |
| Range | 59.2–78.0 | – | 0–97.4 | – | 96.0–97.0 | 82.9–95.1 |
| PPV, % | ||||||
| Mean±SD | 65.5±48.8 | – | 78.3±20.5 | – | – | 52.3±10.8 |
| Median | 65.5 | – | 75.7 | 57.3 | – | 48.1 |
| Range | 31.0–100 | – | 59.2–100.0 | – | – | 44.8–68.2 |
–not reported by any articles meeting study criteria. SD, standard deviation; LG, low grade; HG, high grade.
BTA
The bladder tumor antigen (BTA) test detects the presence of human complement factor H-related protein, which protects cells from complement system activation and is found in high concentrations in the urine of patients with bladder cancer. BTA tests are reported to have a higher sensitivity than cytology, but lower specificity. Additionally, a high false-positive rate has been found in patients with hematuria and inflammatory conditions. There are two FDA-approved tests for BTA. One is a qualitative point-of-care test (BTA stat) and the other is a quantitative ELISA (BTA TRAK).
We identified one study analyzing the use of BTA in the setting of hematuria workup meeting our search criteria [24]. The sensitivity was 100% and specificity was 74%; however, the study included only 24 patients with hematuria. Other performance statistics were not reported. This study also reported on the use of BTA for NMIBC surveillance [24]. The sensitivity and specificity were 36.0% and 79.0%, respectively.
UroVysion
The UroVysion test utilizes multicolor fluorescent in situ hybridization to detect genetic changes associated with bladder cancer, specifically aneuploidy of chromosomes 3, 7, and 17 and loss of the 9p21 locus. Unlike the previously discussed tests, UroVysion results are not affected by urinary tract manipulation or inflammatory conditions, including intravesical administration of bacille Calmette-Guérin (BCG) [25]. It does, however, require trained operators to interpret the results and a relatively large number of cells for analysis.
Four studies reporting the performance of UroVysion for workup of hematuria were identified [22, 26–28]. The median sensitivity and specificity in these studies was 65.7% and 93.8%, respectively, while NPV and PPV were 94.2% and 58.7%, respectively. We identified three studies analyzing the utility of UroVysion in NMIBC surveillance [26, 27, 29]. The median sensitivity, specificity, NPV, and PPV were 73.6%, 85.2%, 87.7%, and 75.7%, respectively.
ImmunoCyt/uCyt
The uCyt test utilizes three fluorescent monoclonal antibodies to detect carcinoembryonic antigen and sulphated mucin glycoproteins that are differentially expressed on bladder cancer cells. The results of this test are not affected by urinary tract inflammation, shedding and manipulation. It also requires operator training to interpret the results, which can result in inter-operator variability. A relatively high number of cells are required for analysis.
We analyzed five studies on uCyt for hematuria workup meeting our inclusion criteria [22, 30–33]. The median sensitivity and specificity for these studies were 86.8% and 77.4%, respectively, with median NPV and PPV of 94.9% and 51.8%, respectively. The performance of uCyt specifically for NMIBC surveillance was reported in only one study [32]. The sensitivity, specificity, NPV, and PPV were 85.5%, 20.5%, 52.9%, and 57.3%, respectively.
CxBladder
A panel that utilizes quantitative reverse transcription-polymerase chain reaction (RT-PCR) to quantify mRNA expression of five genes (MDK, HOXA13, CDC2, IGFBP5, CXCR2) comprises the CxBladder test. Three forms of this test are available (Triage, Detect and Monitor) based on the clinical context. While commercially available, they are not yet approved for use by the FDA. This test has been shown to reduce the likelihood of negative cystoscopies by 39% without missing any NMIBC recurrence [34]. Additionally, performance is not affected by inflammatory conditions, including BCG therapy.
Five studies examining the use of CxBladder in the workup of hematuria were identified [19, 35–38]. The median reported sensitivity for these studies was 93.0%, with specificity and NPV of 62.5% and 98.3%, respectively. Sensitivity for HG tumors was 97%. None of the studies reported PPV. Performance of CxBladder in surveillance of NMIBC was noted in two studies, reporting mean sensitivity of 92.0% and NPV of 96.5%. Sensitivity for HG tumors in this setting was also 97%.
Bladder EpiCheck
The Bladder EpiCheck test uses RT-PCR to detect DNA methylation patterns on 15 genetic loci that are highly prevalent in bladder cancer cells. It is specifically designed for use in NMIBC surveillance. The test received FDA clearance in May 2023.
Performance in NMIBC surveillance was assessed by four studies [39–42]. Median reported sensitivity and specificity were 65.6% and 87.2%, respectively. Sensitivity for HG lesions was 86.1% and 43.1% for LG lesions. Median NPV and PPV were 91.7% and 48.1%, respectively.
Additional tests
There are three commercially available urine biomarker tests (Oncuria, UroAmp, and Bladder Care) that were excluded from analysis due to study designs that did not assess test performance in the setting of hematuria workup or surveillance. Oncuria is a multiplex immunoassay that assesses urine concentration of 10 proteins with reported sensitivity of 93% and specificity of 93% when interpreted with patient demographic data [43]. The UroAmp test combines next generation DNA sequencing and a machine learning algorithm to identify mutations in 60 genes associated with bladder cancer. The reported sensitivity is 97.4% [44]. Bladder Care is an assay that measures levels of DNA methylation on three genes with reported sensitivity of 93.5% and specificity of 92.6% [45].
DISCUSSION
We sought to summarize current evidence on the performance of urine-based biomarker tests commercially available in the US in the setting of hematuria workup and bladder cancer surveillance. Among the five tests analyzed for initial bladder cancer detection, overall performance varied greatly, with median sensitivity ranging from 65.7% to 100%, and specificity ranging from 62.5% to 93.8%. CxBladder had the greatest reported sensitivity and NPV, while UroVysion had the highest specificity. For surveillance, sensitivity ranged from 27.8% to 92%, and specificity from 49.8% to 91.5%. CxBladder again had the highest sensitivity and NPV, but NMP22 had the highest specificity.
The high degree of variability seen in the selected studies is likely due to multiple factors. The first is study design. Within each clinical setting the study populations varied in terms of location, age, smoking history, and the proportion of patients with hematuria (versus other indications for cystoscopy). While degree of hematuria was often included, an overall assessment of patient risk, such as using American Urological Association microhematuria risk stratification, was not reported by any of the included studies, but could have improved comparisons between studies and biomarkers. Relevant clinical information regarding bladder cancer history was likely another source of variation, however this was not available for most studies. Test specific factors such as ELISA cutoff values and use of point-of-care versus lab-based tests likely also contributed. The large degree of variation in populations and study design in the available literature limits the conclusions that can be drawn.
NMP22, BTA, and UroVysion have been commercially available for over a decade and have been studied in head-to-head comparisons. More recently developed tests such as CxBladder and Bladder EpiCheck have not yet been studied to the same extent. This next generation of tests are based on newer technology and assay multiple biomarkers in order to achieve improved performance, however as of yet, no test has achieved results comparable to cystoscopy.
Apart from detection performance, there are other important differences between these tests to consider. NMP22 and BTA are available as point-of-care tests, and the rapid turn-around time may influence a clinician’s test choice given the clinical scenario. Another consideration is the financial burden of a test, which may or may not be reimbursable by insurance despite being FDA-approved. Both of these concerns may interact with patient-related factors in the ultimate decision on which test to employ.
It is important to note that there are many other urine-based tests for bladder cancer detection that are currently under development, though not yet commercially available, and so are not discussed here (XPERT BC Monitor and FGFR3 + TERT, among others). Similarly, we did not review tests that are approved and available for use in Europe, but not in the US (UriFind and ADXBLADDER).
The ideal urinary biomarker for employment in clinical practice will depend on the clinical setting (high specificity and PPV for initial diagnosis; high sensitivity and NPV for surveillance). The test should offer a high cost-benefit ratio, result quickly, be simple to interpret, and provide good reproducibility and accuracy. As the number of available urine-based biomarker tests continues to increase, we must temper our excitement with conclusive evidence based on rigorous studies. These should evaluate urine biomarkers in a prospective manner, compare performance to cytology and cystoscopy, assess impact on quality of life, and measure cost effectiveness. Additionally, future studies may include standardized risk assessments of the study population to assist in interpretation and cross-study comparisons.
The currently available urine-based tests discussed here do not yet match the diagnostic performance of cystoscopy and will continue to play an adjunctive role, mainly in the setting of equivocal cytology. As new technologies emerge and our understanding of bladder cancer progresses, we remain optimistic that urine-based tests can ultimately rival the performance of cystoscopy and reduce the costs of care for patients with bladder cancer.
ACKNOWLEDGMENTS
The authors have no acknowledgments.
FUNDING
The authors report no funding.
AUTHOR CONTRIBUTIONS
JRH: performance of work, interpretation of data, and writing the article.
APM: conception, performance of work, interpretation of data, and writing the article.
All authors had access to the data and approved the final manuscript.
ETHICAL CONSIDERATIONS
As a review of the literature, and as no animal or human research was involved, this study is exempt from any requirement for Institutional Review Board approval.
CONFLICTS OF INTEREST
APM is an Editorial Board Member of this journal, but was not involved in the peer-review process nor had access to any information regarding its peer-review. JRH reports no relevant conflicts of interest.
DATA AVAILABILITY STATEMENT
The data supporting the findings of this study are available within the article and may also be obtained on request from the corresponding author.
REFERENCES
[1] | Siegel RL , Giaquinto AN , Jemal A . Cancer statistics, 2024. CA Cancer J Clin. (2024) ;74: (1):12–49. |
[2] | Cambier S , Sylvester RJ , Collette L , Gontero P , Brausi MA , van Andel G , et al EORTC Nomograms and Risk Groups for Predicting Recurrence, Progression, and Disease-specific and Overall Survival in Non-Muscle-invasive Stage Ta-T1 Urothelial Bladder Cancer Patients Treated with 1-3 Years of Maintenance Bacillus Calmette-Guerin, Eur Urol. (2016) ;69: (1):60–9. |
[3] | Botteman MF , Pashos CL , Redaelli A , Laskin B , Hauser R . The health economics of bladder cancer: A comprehensive review of the published literature, Pharmacoeconomics. (2003) ;21: (18):1315–30. |
[4] | Svatek RS , Hollenbeck BK , Holmang S , Lee R , Kim SP , Stenzl A , et al The economics of bladder cancer: Costs and considerations of caring for this disease, Eur Urol. (2014) ;66: (2):253–62. |
[5] | Reid MD , Osunkoya AO , Siddiqui MT , Looney SW . Accuracy of grading of urothelial carcinoma on urine cytology: An analysis of interobserver and intraobserver agreement, Int J Clin Exp Pathol. (2012) ;5: (9):882–91. |
[6] | Wiener HG , Vooijs GP , van’t Hof-Grootenboer B . Accuracy of urinary cytology in the diagnosis of primary and recurrent bladder cancer, Acta Cytol. (1993) ;37: (2):163–9. |
[7] | Barocas DA , Boorjian SA , Alvarez RD , Downs TM , Gross CP , Hamilton BD , et al Microhematuria: AUA/SUFU Guideline, J Urol. (2020) ;204: (4):778–86. |
[8] | Chang SS , Boorjian SA , Chou R , Clark PE , Daneshmand S , Konety BR , et al Diagnosis and Treatment of Non-Muscle Invasive Bladder Cancer: AUA/SUO Guideline, J Urol. (2016) ;196: (4):1021–9. |
[9] | Lotan Y , O’Sullivan P , Raman JD , Shariat SF , Kavalieris L , Frampton C , et al Clinical comparison of noninvasive urine tests for ruling out recurrent urothelial carcinoma, Urol Oncol. (2017) ;35: (8):531e15-22. |
[10] | Kavalieris L , O’Sullivan P , Frampton C , Guilford P , Darling D , Jacobson E , et al Performance Characteristics of a Multigene Urine Biomarker Test for Monitoring for Recurrent Urothelial Carcinoma in a Multicenter Study, J Urol. (2017) ;197: (6):1419–26. |
[11] | Arora VK , Sarungbam J , Bhatia A , Singh N , Agrawal V , Aggarwal S . Usefulness of NMP22 as an adjunct to a typical urine cytology and low-grade urothelial carcinoma, Diagn Cytopathol. (2010) ;38: (11):788–90. |
[12] | Bangma CH , Loeb S , Busstra M , Zhu X , El Bouazzaoui S , Refos J , et al Outcomes of a bladder cancer screening program using home hematuria testing and molecular markers, Eur Urol. (2013) ;64: (1):41–7. |
[13] | Dogan C , Pelit ES , Yildirim A , Zemheri IE , Canakci C , Basok EK , et al The value of the NMP22 test for superficial bladder cancer diagnosis and follow-up. Turk J Urol. (2013) ;39: (3):137–42. |
[14] | Grossman HB , Messing E , Soloway M , Tomera K , Katz G , Berger Y , et al Detection of bladder cancer using a point-of-care proteomic assay, JAMA. (2005) ;293: (7):810–6. |
[15] | Hwang EC , Choi HS , Jung SI , Kwon DD , Park K , Ryu SB . Use of the NMP22 BladderChek test in the diagnosis and follow-up of urothelial cancer: A cross-sectional study, Urology. (2011) ;77: (1):154–9. |
[16] | Kelly JD , Dudderidge TJ , Wollenschlaeger A , Okoturo O , Burling K , Tulloch F , et al Bladder cancer diagnosis and identification of clinically significant disease by combined urinary detection of Mcm5 and nuclear matrix protein 22, PLoS One. (2012) ;7: (7):e40305. |
[17] | Miyanaga N , Akaza H , Tsukamoto T , Ishikawa S , Noguchi R , Ohtani M , et al Urinary nuclear matrix protein 22 as a new marker for the screening of urothelial cancer in patients with microscopic hematuria, Int J Urol. (1999) ;6: (4):173–7. |
[18] | Moonen PM , Kiemeney LA , Witjes JA . Urinary NMP22 BladderChek test in the diagnosis of superficial bladder cancer, Eur Urol. (2005) ;48: (6):951–6; discussion 6 |
[19] | O’Sullivan P , Sharples K , Dalphin M , Davidson P , Gilling P , Cambridge L , et al A multigene urine test for the detection and stratification of bladder cancer in patients presenting with hematuria, J Urol. (2012) ;188: (3):741–7. |
[20] | Ritter R , Hennenlotter J , Kuhs U , Hofmann U , Aufderklamm S , Blutbacher P , et al Evaluation of a new quantitative point-of-care test platform for urine-based detection of bladder cancer, Urol Oncol. (2014) ;32: (3):337–44. |
[21] | Sanchez-Carbayo M , Urrutia M , Silva JM , Romani R , De Buitrago JM , Navajo JA . Comparative predictive values of urinary cytology, urinary bladder cancer antigen, CYFRA 21-1 and NMP22 for evaluating symptomatic patients at risk for bladder cancer, J Urol. (2001) ;165: (5):1462–7. |
[22] | Todenhofer T , Hennenlotter J , Esser M , Mohrhardt S , Tews V , Aufderklamm S , et al Combined application of cytology and molecular urine markers to improve the detection of urothelial carcinoma, Cancer Cytopathol. (2013) ;121: (5):252–60. |
[23] | Zippe C , Pandrangi L , Agarwal A . NMP22 is a sensitive, cost-effective test in patients at risk for bladder cancer, J Urol. (1999) ;161: (1):62–5. |
[24] | Kirollos MM , McDermott S , Bradbrook RA . The performance characteristics of the bladder tumour antigen test, Br J Urol. (1997) ;80: (1):30–4. |
[25] | Pesch B , Nasterlack M , Eberle F , Bonberg N , Taeger D , Leng G , et al The role of haematuria in bladder cancer screening among men with former occupational exposure to aromatic amines, BJU Int. (2011) ;108: (4):546–52. |
[26] | Dimashkieh H , Wolff DJ , Smith TM , Houser PM , Nietert PJ , Yang J . Evaluation of urovysion and cytology for bladder cancer detection: A study of 1835 paired urine samples with clinical and histologic correlation, Cancer Cytopathol. (2013) ;121: (10):591–7. |
[27] | Lotan Y , Bensalah K , Ruddell T , Shariat SF , Sagalowsky AI , Ashfaq R . Prospective evaluation of the clinical usefulness of reflex fluorescence in situ hybridization assay in patients with atypical cytology for the detection of urothelial carcinoma of the bladder, J Urol. (2008) ;179: (6):2164–9. |
[28] | Schlomer BJ , Ho R , Sagalowsky A , Ashfaq R , Lotan Y . Prospective validation of the clinical usefulness of reflex fluorescence in situ hybridization assay in patients with atypical cytology for the detection of urothelial carcinoma of the bladder, J Urol. (2010) ;183: (1):62–7. |
[29] | Kehinde EO , Al-Mulla F , Kapila K , Anim JT . Comparison of the sensitivity and specificity of urine cytology, urinary nuclear matrix protein-22 and multitarget fluorescence in situ hybridization assay in the detection of bladder cancer, Scand J Urol Nephrol. (2011) ;45: (2):113–21. |
[30] | Cha EK , Tirsar LA , Schwentner C , Christos PJ , Mian C , Hennenlotter J , et al Immunocytology is a strong predictor of bladder cancer presence in patients with painless hematuria: A multicentre study, Eur Urol. (2012) ;61: (1):185–92. |
[31] | Deininger S , Todenhofer T , Hennenlotter J , Gerber V , Schwarz J , Bedke J , et al Impact of variant microscopic interpretation of the uCyt+immunocytological urine test for the detection of bladder cancer, Diagn Cytopathol. (2018) ;46: (2):111–6. |
[32] | Odisho AY , Berry AB , Ahmad AE , Cooperberg MR , Carroll PR , Konety BR . Reflex ImmunoCyt testing for the diagnosis of bladder cancer in patients with atypical urine cytology, Eur Urol. (2013) ;63: (5):936–40. |
[33] | Schmitz-Drager BJ , Tirsar LA , Schmitz-Drager C , Dorsam J , Mellan Z , Bismarck E , et al Immunocytology in the assessment of patients with asymptomatic hematuria, World J Urol. (2008) ;26: (1):31–7. |
[34] | Koya M , Osborne S , Chemasle C , Porten S , Schuckman A , Kennedy-Smith A . An evaluation of the real world use and clinical utility of the Cxbladder Monitor assay in the follow-up of patients previously treated for bladder cancer, BMC Urol. (2020) ;20: (1):12. |
[35] | Davidson PJ , McGeoch G , Shand B . Inclusion of a molecular marker of bladder cancer in a clinical pathway for investigation of haematuria may reduce the need for cystoscopy, N Z Med J. (2019) ;132: (1497):55–64. |
[36] | Davidson PJ , McGeoch G , Shand B . Assessment of a clinical pathway for investigation of haematuria that reduces the need for cystoscopy, N Z Med J. (2020) ;133: 71–82. |
[37] | Kavalieris L , O’Sullivan PJ , Suttie JM , Pownall BK , Gilling PJ , Chemasle C , et al A segregation index combining phenotypic (clinical characteristics) and genotypic (gene expression) biomarkers from a urine sample to triage out patients presenting with hematuria who have a low probability of urothelial carcinoma, BMC Urol. (2015) ;15: , 23. |
[38] | Konety B , Shore N , Kader AK , Porten S , Daneshmand S , Lough T , et al Evaluation of Cxbladder and Adjudication of Atypical Cytology and Equivocal Cystoscopy, Eur Urol. (2019) ;76: (2):238–43. |
[39] | D’Andrea D , Soria F , Zehetmayer S , Gust KM , Korn S , Witjes JA , et al Diagnostic accuracy, clinical utility and influence on decision-making of a methylation urine biomarker test in the surveillance of non-muscle-invasive bladder cancer, BJU Int. (2019) ;123: (6):959–67. |
[40] | Trenti E , D’Elia C , Mian C , Schwienbacher C , Hanspeter E , Pycha A , et al Diagnostic predictive value of the Bladder EpiCheck test in the follow-up of patients with non-muscle-invasive bladder cancer, Cancer Cytopathol. (2019) ;127: (7):465–9. |
[41] | Trenti E , Pycha S , Mian C , Schwienbacher C , Hanspeter E , Kafka M , et al Comparison of 2 new real-time polymerase chain reaction-based urinary markers in the follow-up of patients with non-muscle-invasive bladder cancer, Cancer Cytopathol. (2020) ;128: (5):341–7. |
[42] | Witjes JA , Morote J , Cornel EB , Gakis G , van Valenberg FJP , Lozano F , et al Performance of the Bladder EpiCheck Methylation Test for Patients Under Surveillance for Non-muscle-invasive Bladder Cancer: Results of a Multicenter, Prospective, Blinded Clinical Trial, Eur Urol Oncol. (2018) ;1: (4):307–13. |
[43] | Hirasawa Y , Pagano I , Chen R , Sun Y , Dai Y , Gupta A , et al Diagnostic performance of Oncuria, a urinalysis test for bladder cancer, J Transl Med. (2021) ;19: (1):141. |
[44] | Bicocca VT , Phillips KG , Fischer DS , Caruso VM , Goudarzi M , Garcia-Ransom M , et al Urinary Comprehensive Genomic Profiling Correlates Urothelial Carcinoma Mutations with Clinical Risk and Efficacy of Intervention, J Clin Med. (2022) ;11: (19):5827. |
[45] | Piatti P , Chew YC , Suwoto M , Yamada T , Jara B , Jia XY , et al Clinical evaluation of Bladder CARE, a new epigenetic test for bladder cancer detection in urine samples, Clin Epigenetics. (2021) ;13: (1):84. |




