The Development of a Video-based Nutrition Education Curriculum for Patients Undergoing Radical Cystectomy
Abstract
BACKGROUND:
The treatment for patients with muscle-invasive bladder cancer includes neoadjuvant chemotherapy followed by radical cystectomy. The American Urological Association guidelines stress the optimization of patient performance status in the perioperative setting. Therefore, implementation of nutrition education is critical for the multi-disciplinary care of this vulnerable patient population and wide distribution of information is critical.
OBJECTIVE:
The goal of our study was to create a nutrition-based video education series for patients undergoing chemotherapy and radical cystectomy for bladder cancer.
METHODS:
Scripts for the videos were developed through an iterative process by experts in nutrition, urology, and communication. Providers and patient advocates were recruited to perform semi-structured interviews and surveys for additional feedback. Performer facial emotion recognition (Noldus™) was used to assess displayed emotion by the presenters. Mangold VisionPlayer software was used for participant eye movement tracking of the video content. A knowledge survey was created, and Item Content Validity Index (I-CVI) was calculated with a nutrition expert advisory board. Participants were recruited for cognitive interviewing to understand the mental processes and interpretations while answering questions.
RESULTS:
The video series is available to the public on the Bladder Cancer Advocate Network (BCAN) website at the following URL: https://bcan.org/facing-bladder-cancer/nutrition-bladder-cancer/eating-healthy-bladder-cancer/. Cinematic filming methods, (smaller depth of field, lighting, and camera movement) enhanced message delivery along with music and text on screen to anchor important concepts.
CONCLUSIONS:
This study can be a framework for the development of a patient education video library accessible through electronic medical records, health care applications, and patient advocacy websites.
INTRODUCTION
In the United States, there will be an estimated 81,180 cases of bladder cancer in 2022 [1]. Treatment for muscle invasive bladder cancer often includes chemotherapy followed by radical cystectomy (RC) [2]. Malnourished patients undergoing this surgery have a 3-fold increased risk of mortality within 90 days and a 20% worse survival rate at 3 years [3, 4]. In addition, chemotherapy can lead to dysgeusia in this patient population; notably up to 73% of patients receiving cisplatin/carboplatin-based chemotherapy will have changes in taste and smell [5]. Gastrointestinal disturbances such as diarrhea and constipation are also common with both chemotherapy and surgery and can lead to inadequate nutrient intake and malabsorption [6]. Because few studies have investigated methods for meeting the nutrition needs of muscle-invasive bladder cancer patients, strategies are needed for patients and providers to minimize the detrimental impacts of cancer treatments on nutritional status.
Per the American Urological Association guidelines on the treatment of non-metastatic muscle-invasive bladder cancer to optimize patient performance status in the perioperative setting, our objective was to develop an evidence-based, nutrition focused education video series for patients undergoing RC, with or without chemotherapy. We outlined the methodology for the development of a nutrition education curriculum which through collaboration with experts in bladder cancer, oncologic nutrition, nutrition literacy, strategic communications, bladder cancer patients and caregivers.
METHODS
This non-randomized study was conducted at the Urology Clinic of the University of Kansas Health System where participants and caregivers were recruited. The study protocol was approved with expedited review by the Institutional Review Board of the University of Kansas Medical Center (IRB# 00142651). All study participants provided written informed consent. All data were collected between June 2018 to August 2021.
Video series
A nutrition education video series was created by the Nutrition Shared Resource of the University of Kansas Cancer Center. The content of the videos was designed to educate and empower patients to utilize nutrition to prepare for or recover from a radical cystectomy specifically by addressing perioperative nutritional needs and common problems reported in this patient population. The series includes a total of 14 brief videos addressing 3 topics 1) high-protein nutrition for preserving lean mass and fueling tissue repair after surgery; 2) improving diet intake with altered taste from chemotherapy; and 3) tips for managing diarrhea and constipation. For each topic, 1-2 videos explained 1 key food-based strategy and each additional video demonstrated food preparation of recipes to support key strategies.
The scripts for the videos were developed through an iterative process involving nutrition, cancer, urology, and communication experts with additional feedback from providers and patient advocates. The scripts were written in plain language as evaluated with the Center for Disease Control’s Clear Communication Index [7]. The videos were filmed using cinematic production strategies narrow depth of field (DOF), camera movement, colorizing, etc.) to increase appeal and help focus attention on the information delivery and prevent information overload.
Five videos from the series, selected by the research team, were then evaluated for relevance and effectiveness using both qualitative and quantitative methods. Patients and caregivers participating in the pilot studies watched the videos (presented in random order), after which semi-structured interviews were conducted to get immediate feedback on content, utilization and relevance. After each video, participants were asked to complete a questionnaire assessing perceived competency of the nutritionist, technical qualities of the video (duration, pace, captions, etc.), and perceived use of the information. At the end of the study, a questionnaire collected demographic data; relevance of the information was assessed using the Personal Involvement Inventory [8]. To evaluate the production design’s impact on visual engagement and attention, eye-tracking data was collected from the participants during presentation of the videos, using an on-site portable system that consists of a Windows PC laptop computer running Mangold VisionPlayer software which displays the video while tracking eye movement through an infrared (IR) camera mounted under the monitor. Four videos were selected for this research component because of their variety and relevance to the overall content: 1) Dealing with constipation, 2) Dealing with bad taste, 3) Cooking demo –Egg muffins, and 4) Cooking demo –Chicken broth.
Knowledge questionnaire development
The research team compiled questions from previous research to assess effectiveness of the video series for changing behavioral intention and nutrition impact symptoms [8, 9]. Upon literature review, however, a tool was not found to measure knowledge obtained through nutrition education in the setting of a radical cystectomy with or without chemotherapy. Subsequently, the research team developed a questionnaire to assess knowledge of bladder cancer nutrition therapy. We drafted a series of 38 questions (6–9 questions per topic) to measure knowledge of key messages of the videos. The terminology within the videos was also utilized within the questions to foster increased understanding.
The knowledge survey was then assessed by an advisory board (n = 3) with each question analyzed for relevance to content domain, clarity, and reading difficulty [10, 11]. Experts were recruited through known contacts of the research team who are published oncology nutrition experts. An Item Content Validity Index (I-CVI) was then calculated for each question. The I-CVI was calculated with the following steps: 1) Experts ranked items on a 4-point scale ranging from 1–4 with ‘4’ being the most relevant, 2) ‘1–2’ rankings were assigned a score of ‘0’ = ’not relevant’, and ‘3–4’ rankings were assigned a score of ‘1’ = ‘relevant’. A total Scale Content Validity measure is calculated by averaging the I-CVIs for each question. Acceptable S-CVI was set at ≥0.80. Experts then provided direct comments to address clarity and reading difficulty. Questions were then adjusted accordingly to feedback provided.
To further refine the knowledge questionnaire, RC patients (pre-cystectomy or post-cystectomy) and/or caregivers were recruited to participate in cognitive interviewing. Cognitive interviewing allowed us to understand the mental processes and interpretations participants make as they answer questions [12]. This process allowed the research team to identify problems with questions such as interpretation, decision, processes, response selection, instruction, and organization.
Interviews were digitally recorded and transcribed verbatim. Transcripts were analyzed using constant comparative methods and data triangulation to ascertain recurrent themes [13]. Two researchers trained in qualitative methodology coded the transcripts separately then met to discuss item revisions arising from themes in responses.
RESULTS
Video series
The video series is available to the public on the Bladder Cancer Advocate Network (BCAN) website at the following URL: https://bcan.org/facing-bladder-cancer/nutrition-bladder-cancer/eating-healthy-bladder-cancer/.
The research team developed the scripts for the videos to address topics of interest to the target audience, both educational content about nutritional approaches to mitigating some of the treatment-relates symptomatology, and demonstration videos on the preparation of specific dishes. Members of the research team participated in the recording of the mediated content, and credentials were displayed on screen to ascertain expertise with the topics. Cinematic filming methods, which included smaller depth of field, dedicated lighting, and camera movement were used to enhance message delivery. Music was added to complement the narrative, text on screen anchored the most important concepts, and captions were provided in addition to the audio track. The videos were pretested for engagement using gaze tracking, in combination with self-reported metrics on perception of the competence of the nutritionist (four items, 5-point semantic differential scale), technical qualities of the video (seven items, 7-item Likert scale), and information presented (seven items, 7-item Likert scale). Gaze tracking (Mangold Vision™) allowed the researchers to estimate attention to the content, as well as how the different elements in the video enhance or distract from the message. Mobile eye tracking station was being set up for gaze tracking every time the recruitment of a patient was confirmed. All questionnaires were completed on paper.
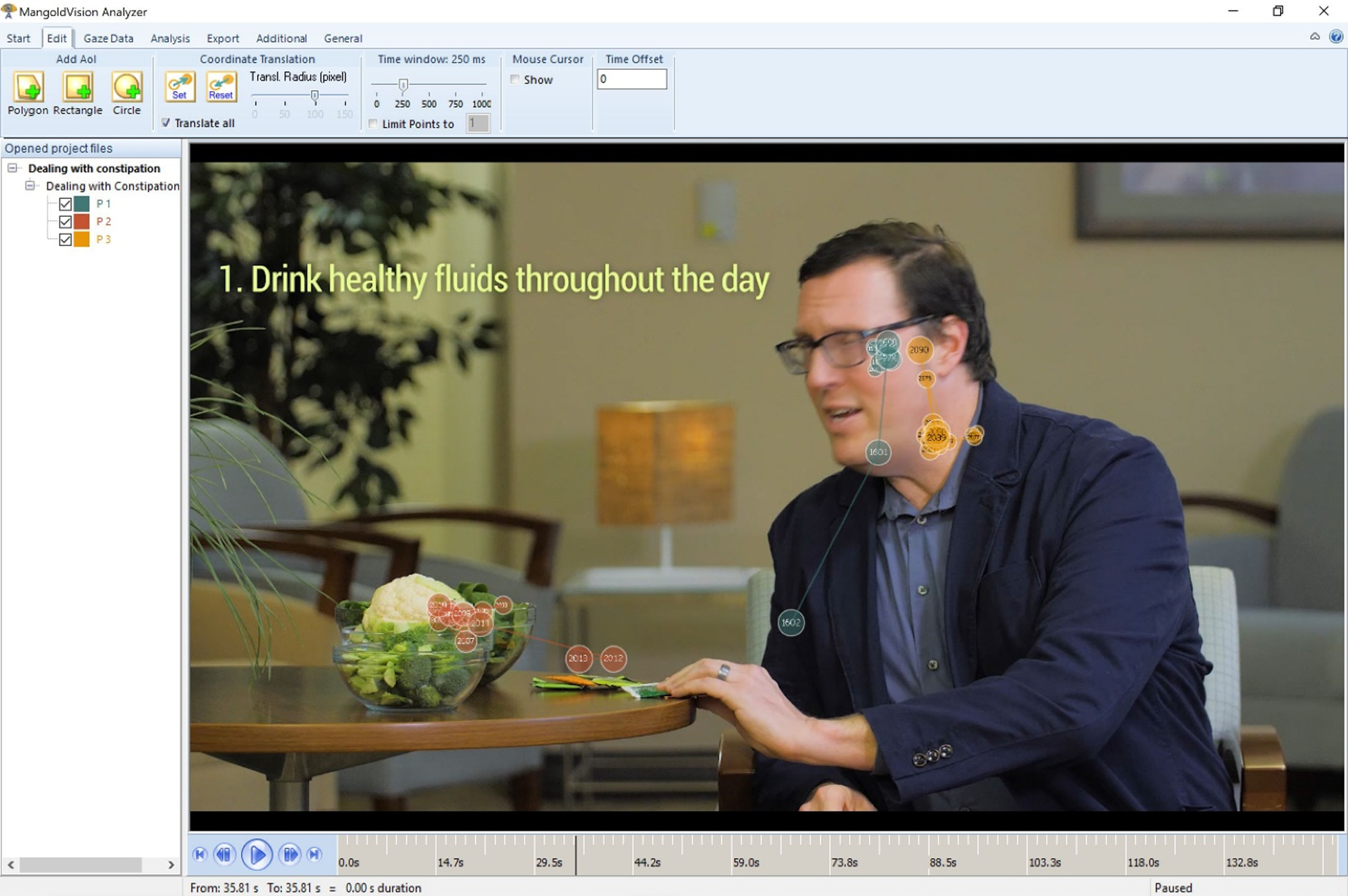
Unfortunately, recruitment was marred by significant attrition in the first two months, and then the COVID-19 pandemic put a complete stop to data collection. Anecdotal data from the two participants that completed the study shows a high level of engagement with the videos and appreciation of the content and the presenters. Gaze tracking shows that the production and editing strategies were successful in ensuring that the attention to the video content was in sync with the narrative, and that there were no distractors. An example of gaze tracking analysis is presented in Fig. 1.
Fig. 1
Gaze analysis using Mangold Vision™.
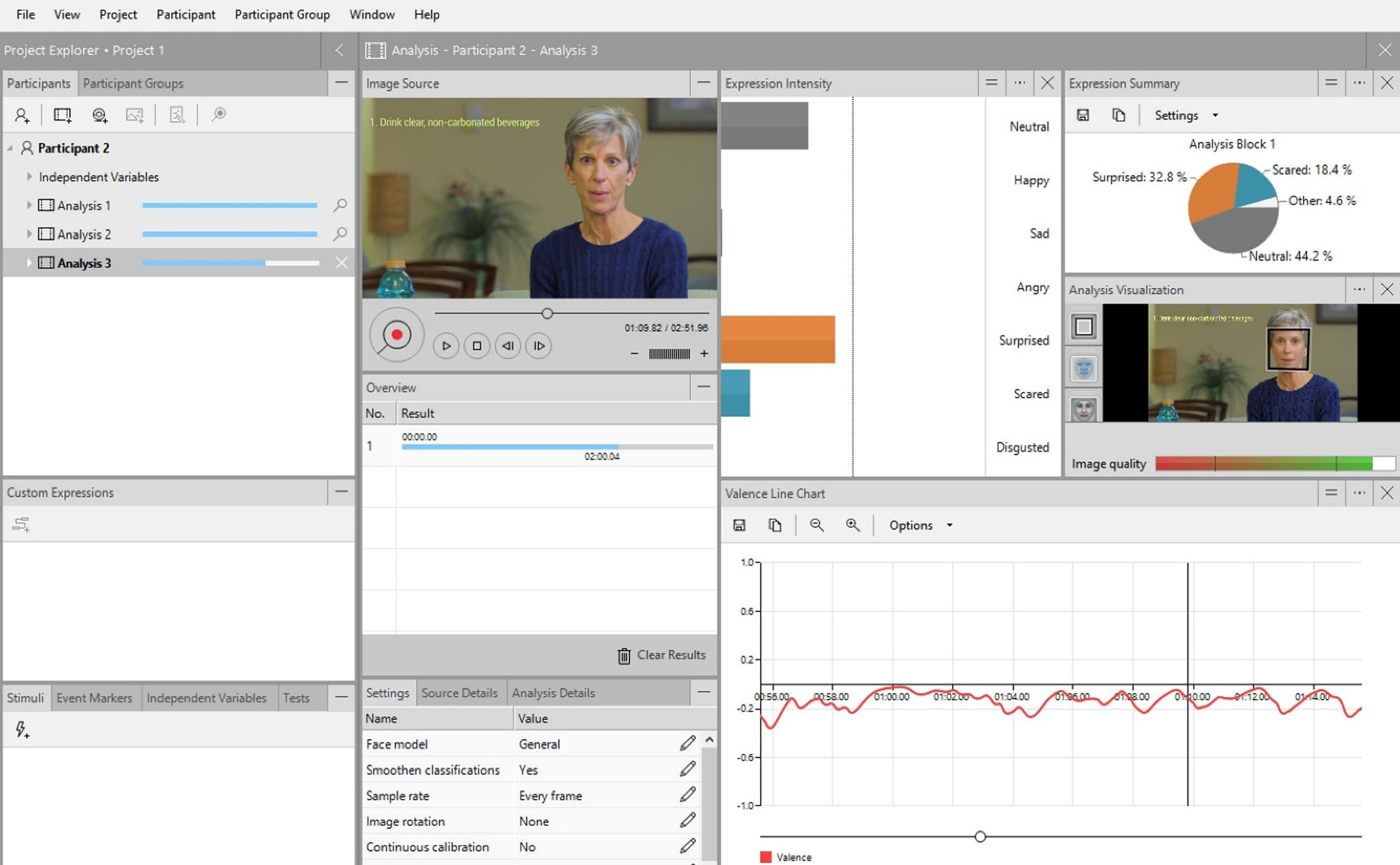
In addition to gaze tracking, facial emotion recognition (Noldus™) was used to assess displayed emotion by the presenters, to ensure that all presenters convey similar emotions. An example of facial emotion recognition analysis is presented in Fig. 2.
Fig. 2
Facial emotion analysis using Noldus™ Face Reader.
Knowledge questionnaire
The three content experts evaluated each item of the knowledge questionnaire. For all domains discussed, the, the total S-CVI was 0.98, meeting the target set a priori. Individual domain S-CVIs resulting from reviewer comments are provided in Table 1. Based upon reviewer feedback, one item was deleted, one item was added, and 8 modifications to items were made to question or answer option wording.
Table 1
Summary of results of content expert review (n = 3)
| Questionnaire Domain | S-CVI | S-CVI (after deletion of items) | Resulting Changes |
| High Protein Nutrition | 1.0 | 1.0 | 1 question deleted, 1 question added, 3 questions modified |
| GI Distress | 0.97 | 0.97 | 3 questions modified, 1 answer modified |
| Dysgeusia | 1.0 | 1.0 | 1 question modified |
Twelve participants in cognitive interviews were 68.5±9.38 years old, Caucasian (10/12), completed at least some college (11/12), and half were male (6/12). More participants (5/12) reported annual household income ≥$75,000 than other income categories, and no participants reported utilizing public assistance food programs. Participant status was self-reported and included: 1) caregiver, n = 2; 2) patient post-cystectomy, n = 3; 3) patient pre-cystectomy, n = 4; and 4) patient post-chemotherapy and cystectomy, n = 3.
Cognitive interviewing revealed several themes with respect to terminology, nutrition content, and familiarity of food items resulting in changes to 6 questions and 8 answer options. Individual comments from participants are provided in Supplementary Table.
DISCUSSION
In this study, we engaged bladder cancer nutrition experts, patients, and caregivers to develop a bladder cancer-focused nutrition education video series and corresponding knowledge assessment. The need for nutrition education among bladder cancer patients has been well-established. A series of short in length educational videos has previously proven effective as a means to positively impact dietary behaviors [14]. Our study further outlines an iterative process for the development of patient-center materials and improvement of educational tools promoting increased audience engagement and understanding. Others have used similar strategies to develop patient-centered materials with benefits to cancer patient care [15–18].
While the efficacy of patient-centered materials have been heavily examined, assessment of understanding of educational content is often overlooked. Prior research has utilized both expert review and cognitive interviews to assess content validity and reliability of questionnaires [19–22]. To our knowledge, no studies have utilized this method to design a questionnaire to directly assess the effectiveness of a nutrition education curriculum for cancer patients. We have created a valid and reliable assessment of which results of the questionnaire will be evaluated in future studies. Our study provides the framework to discern knowledge gained from educational materials. The ability to assess knowledge gained can guide nutrition professionals to tailor their educational message toward improved dietary behaviors [23].
Limitations
A major limitation of this study is the small sample size largely due to challenges resulting from COVID-19. In addition, the knowledge questionnaire has yet to be integrated on the BCAN website preventing efficacy testing.
Practice implications
The further implication of this methodology is the development of an extensive library of patient education videos accessible through electronic medical records, health care applications, and patient advocacy websites with corresponding tools to assess knowledge gain and allow for continual improvement. However, further research is warranted to determine if the video series improves knowledge of nutrition therapy for impact symptoms, enactment of recommended behavioral strategies, and management of impact symptoms in bladder cancer patients.
ACKNOWLEDGMENTS
Carrie Michael, Cheri Van Patten and Carolyn Lammersfeld for nutritional expertise.
Elizabeth Wulff-Burchfield and Nick Marchello for their acting performance.
Katie Glavin and Alexandra Dahlgren for research participant recruitment and logistics.
FUNDING
2018 Patient-Centered Clinical Research Young Investigator Award through the Bladder Cancer Advocacy Network (BCAN).
AUTHOR CONTRIBUTIONS
Conception of study: HG, MR, JHR, MG, EKL.
Data acquisition: JR, HR, MR, HG, JHR, MG, EKL.
Video recording, patient interviews: JR, MR, HG, HR, JHR, MG, EKL.
Writing and editing: JR, HG, MR, HR, JHR, MG, EKL.
CONFLICTS OF INTEREST
JR, HG, HR, MR, JHR, MG and EKL declare no relevant conflicts of interest.
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/BLC-230021.
REFERENCES
[1] | Siegel RL , Miller KD , Fuchs HE , Jemal A . Cancer statistics, 2022. CA: A Cancer Journal for Clinicians. (2022) ;72: (1):7–33. |
[2] | Grossman HB , Natale RB , Tangen CM , Speights VO , Vogelzang NJ , Trump DL , et al. Neoadjuvant chemotherapy plus cystectomy compared with cystectomy alone for locally advanced bladder cancer. New England Journal of Medicine. (2003) ;349: (9):859–66. |
[3] | Gregg JR , Cookson MS , Phillips S , Salem S , Chang SS , Clark PE , et al. Effect of preoperative nutritional deficiency on mortality after radical cystectomy for bladder cancer. Journal of Urology. (2011) ;185: (1):90–6. |
[4] | Shabsigh A , Korets R , Vora KC , Brooks CM , Cronin AM , Savage C , et al. Defining early morbidity of radical cystectomy for patients with bladder cancer using a standardized reporting methodology. European Urology. (2009) ;55: (1):164–76. |
[5] | Bernhardson B-M , Tishelman C , Rutqvist LE . Self-reported taste and smell changes during cancer chemotherapy. Supportive Care in Cancer. (2008) ;16: (3):275–83. |
[6] | Caffo O , Fellin G , Graffer U , Luciani L . Assessment of quality of life after cystectomy or conservative therapy for patients with infiltrating bladder carcinoma: A survey by a self-administered questionnaire. Cancer: Interdisciplinary International Journal of the American Cancer Society. (1996) ;78: (5):1089–97. |
[7] | Baur C , Prue C . The CDC clear communication index is a new evidence-based tool to prepare and review health information. Health Promotion Practice. (2014) ;15: (5):629–37. |
[8] | Ajzen I . Residual effects of past on later behavior: Habituation and reasoned action perspectives. Personality and Social Psychology Review. (2002) ;6: (2):107–22. |
[9] | Argilés JM , Muscaritoli M . Unifying diagnostic criteria forcachexia: An urgent need. Clinical Nutrition. (2017) ;36: (3):910–1. |
[10] | Polit DF , Beck CT . The content validity index: Are you sure you know what’s being reported? critique and recommendations. Research in Nursing & Health. (2006) ;29: (5):489–97. |
[11] | Rubio DM , Berg-Weger M , Tebb SS , Lee ES , Rauch S . Objectifying content validity: Conducting a content validity study in social work research. Social Work Research. (2003) ;27: (2):94–104. |
[12] | Willis GB . Cognitive interviewing and questionnaire design: A training manual: US Department of Health and Human Services, Centers for Disease Control and . . . ; 1994. |
[13] | Creswell JW , Creswell JD . Research design: Qualitative, quantitative, and mixed methods approaches: Sage publications; 2017. |
[14] | Li X , Huang Y , Yin R , Pan C , Cai Y , Wang Z . Visualized nutrition education and dietary behavioral change: A systematic review and meta-analysis. Crit Rev Food Sci Nutr. (2019) ;59: (12):1976–85. |
[15] | Bigelow EO , Windon MJ , Fakhry C , Kiess AP , Seiwert T , D’Souza G . Development of a web-based, patient-centered decision aid for oropharyngeal cancer treatment. Oral Oncol. (2021) ;123: , 105618. |
[16] | O’Malley DM , Davis SN , Devine KA , Sullivan B , Bator A , Clemow L , et al. Development and usability testing of the tool to guide cancer survivorship follow-up care. Psycho-Oncology. (2020) ;29: (1):123–31. |
[17] | Naik AD , Horstman MJ , Li LT , Paasche-Orlow MK , Campbell B , Mills WL , et al. User-centered design of discharge warnings tool for colorectal surgery patients. Journal of the American Medical Informatics Association. (2017) ;24: (5):975–80. |
[18] | Mossanen M , Macleod LC , Chu A , Wright JL , Dalkin B , Lin DW , et al. Comparative effectiveness of a patient centered pathology report for bladder cancer care. J Urol. (2016) ;196: (5):1383–9. |
[19] | Gibbs HD , Ellerbeck EF , Befort C , Gajewski B , Kennett AR , Yu Q , et al. Measuring nutrition literacy in breast cancer patients: Development of a novel instrument. Journal of Cancer Education. (2016) ;31: (3):493–9. |
[20] | Lund L , Ross L , Groenvold M . The initial development of the ‘Cancer Caregiving Tasks, Consequences and Needs Questionnaire’ (CaTCoN). Acta Oncologica. (2012) ;51: (8):1009–19. |
[21] | Grarup KR , Devoogdt N , Strand LI . The Danish version of Lymphoedema Functioning, Disability and Health Questionnaire (Lymph-ICF) for breast cancer survivors: Translation and cultural adaptation followed by validity and reliability testing. Physiother Theory Pract. (2019) ;35: (4):327–40. |
[22] | Eskildsen NB , Ross L , Bulsara C , Dietz SM , Thomsen TG , Groenvold M , et al. Development and content validation of a questionnaire measuring patient empowerment in cancer follow-up. Qual Life Res. (2020) ;29: (8):2253–74. |
[23] | Marchello NJ , Daley CM , Sullivan DK , Nelson-Brantley HV , Hu J , Gibbs HD . Nutrition literacy tailored interventions may improve diet behaviors in outpatient nutrition clinics. J Nutr Educ Behav. (2021) ;53: (12):1048–54. |




