“Picture this”- Patients’ Drawings of Non-Muscle Invasive Bladder Cancer: A Novel Method to Help Understand How Patients Perceive Their Condition
Abstract
BACKGROUND:
There is a paucity of data regarding patient experiences of living with non-muscle-invasive bladder cancer (NMIBC).
OBJECTIVES:
To investigate patients’ beliefs about NMIBC utilising both a well-established verbal/linguistic method, the Brief Illness Perception Questionnaire (B-IPQ) in addition to a novel visual/perceptual method, that is, asking patients to draw their bladder as it is now and as they perceive it will be in the future.
METHODS:
Cross-sectional study of patients with NMIBC. Patients completed: (i) the B-IPQ, and (ii) 2 drawings of their bladder: as they perceived it currently and as they perceived it would look in 5 years’ time.
RESULTS:
A total of 118 patients completed the B-IPQ, of which 96 produced 2 bladder drawings. Forty-seven per cent of patients depicted no change in their bladder across time, 35% depicted improvements, while 18% drew their NMIBC as deteriorating between the two time points. Patients who drew their NMIBC worsening over time reported significantly stronger beliefs in the severity of current consequences from their NMIBC (F(2,94) = 9.07, p < 0.001, m = 5.68, 95% CI 4.38–6.88) and greater current concerns about their NMIBC (F(2,94) = 6.17, p < 0.01, m = 7.06, 95% CI 5.47–8.66). This was unrelated to cancer grade, cancer stage, treatment or demographic variables.
CONCLUSION:
This is the first study to explore beliefs about NMIBC in a sample of patients with NMIBC attending routine clinics using both a well-established and a novel method of assessing patients’ perceptions. Results highlight the usefulness of a simple non-verbal technique, in identifying patients’ concerns about the condition. Almost one fifth of patients with NMIBC may experience significant concerns about the worsening of their condition, which appear to be independent of demographic, histopathological, and treatment related variables. Further exploration of the psychological concerns of individuals with NMIBC is required in order to appropriately plan for needs led multidisciplinary approach in their care.
INTRODUCTION
There is a paucity of research related to patients’ experiences of living with a diagnosis of NMIBC. While there has been some momentum in the examination of quality of life issues within the NMIBC population [1–3] and a recognition of the importance of developing services to address the broader needs of those diagnosed with NMIBC [4], there remain significant gaps in the literature related to patients’ experiences.
One area which has received some recent attention is that of the beliefs held by patients with NMIBC about their condition [5, 6]. This move towards understanding patient perceptions of NMIBC is important as thousands of studies, over 4 decades of healthcare research, have used illness perceptions to understand patients’ responses to illness. This “common sense” model (CSM) of illness self-regulation [7] proposes that patients’ beliefs about their condition is developed from a number of factors which may include the use of information derived from healthcare sources, the persons own experience with health and illness, and lay ideas from friends, family and various media. The key issue is that this personal common sense model of a condition which develops from these diverse informational sources drives the patients cognitive, behavioural and emotional attempts to cope with a condition and consequently impacts important health outcomes including adherence to treatment [8], quality of life [9], psychological distress [10] and the use of health care resources [11]. Moreover, within cancer survivors [12] illness perceptions have been helpful in understanding fears around recurrence and patients’ engagement in health protective behaviours. Two recent studies have examined illness perceptions in NMIBC [5, 6]. While these studies did not examine illness perceptions in the context of the CSM, it is encouraging that patients with NMIBC personal model of disease has started to be considered.
Illness perceptions are complex and increasingly there is the understanding that alternative and adjunctive means of collecting data relating to patients understanding of their condition should be explored [13]. The importance of utilising both verbal (e.g. questionnaire and qualitative information) and non-verbal means of assessing individual’s illness perceptions, e.g. patient’s drawings of their condition have been proposed [13, 14], on the basis this may afford the opportunity to uncover idiosyncratic beliefs not readily accessible through more standard verbalising methods used in questionnaires or interviews. A number of studies reviewed by Broadbent and colleagues [13] have utilised patients’ drawings as a method to understand individuals experiences of their particular condition, and have highlighted the utility of this method in identifying often quite challenging concepts for patients, such as poor understanding of pathophysiology. It is noted, however, that very few studies have been carried out in populations of individuals with cancer and of these, the majority have focused on children’s experience of cancer and women with breast cancer [13]. No previous studies have examined the drawings of patients with NMIBC.
Given the paucity of data relating to the experience of living with NMIBC and the usefulness of the illness perceptions model, this exploratory study aimed to: (1) examine the illness perceptions held by patients with NMIBC routinely attending for surveillance cystoscopy or intravesical therapy treatment; (2) examine characteristics of their bladder drawings that might be associated with cancer grade and stage, treatment related variables, demographic and verbal illness perceptions; and (3) examine the utility of drawings as a method of communicating unspoken concerns for patients.
METHOD
Study design
This study utilised a cross-sectional design, and was approved through the Clinical Research Ethics Committee of the Cork Teaching Hospitals (Ref: ECM 4 (t) 12/02/19 & ECM 3 (jjj) 18/06/19). The study adhered to STROBE reporting guidelines.
Participants
Participants were eligible to participate if they had a diagnosis of NMIBC and were attending for routine surveillance cystoscopy or intravesical therapy between March 2019 and January 2020. Of 192 participants approached to take part in the study, 118 patients provided written consent and completed the B-IPQ prior to undergoing routine surveillance cystoscopy or intravesical therapy. This represents a 61.5% response rate. Of this group 96 (81%) completed the drawings. There were no associations between gender and declining to take part in the study (χ2= 0.90, df = 1, p = 0.34). There were however, significant age differences with older patients significantly less likely to take part (t = –3.65 (188), p < 0.001).
Measures
Brief Illness Perception Questionnaire (B-IPQ) [15]
The B-IPQ is a 9 item self-reported assessment of illness perceptions which has been used across a wide variety of medical and surgical conditions [16].
Each item of the B-IPQ assesses one dimension of cognitive illness perceptions and is scored on a VAS from 0-10. Illness perceptions assessed are: Consequences (0 = no effects at all, ranging through to 10 = severely affects my life), Timeline (0 = a very short time, ranging through to 10 = forever), Personal Control (0 = absolutely no control, ranging to 10 = extreme amount of control), Treatment control (0 = not at all, ranging through to 10 = extremely helpful), Illness Identity (0 = no symptoms at all, ranging to 10 = many severe symptoms), Concern (0 = not at all concerned, ranging through to 10 = extremely concerned), Coherence (0 = don’t understand at all, ranging through to 10 = understand very clearly 10), and Emotional response (0 = not at all affected emotionally, ranging through to 10 = extremely affected emotionally). The final item of the B-IPQ assesses cause related to the illness and asks participants to list the three most important causes of their condition. Higher scores represent a stronger belief in that illness perception. While some studies have tended to calculate total or “subscale” scores for the B-IPQ the developers [16] recommend caution in taking this approach in that it diminishes the scale to a “general level of threat” and as such, it is less helpful in clinical applications. On this basis, mean scores were calculated for each of the B-IPQ items.
Drawings
Participants were provided with two A4 pieces of paper and provided with written instructions asking them to “draw how you imagine your bladder to look right now” on the first sheet and to “draw how you imagine your bladder to look in 5 years time” on the second sheet. In line with previous studies [17–19] participants were informed that “drawing talent” was not important and that a “simple sketch” would also be fine. The drawings were completed by 81% (n = 96) of participants. All participants completed their drawings in less than 2 minutes.
Demographic and illness related data
Participants were asked to provide data related to time of diagnosis and treatment undergone in relation to NMIBC, marital status, living circumstances, employment status, mental health history, smoking status and alcohol consumption. Cancer stage and grade, intravesical treatment history and any missing data was retrieved from patient medical files.
Procedure
Participants were provided with an information sheet about the study at presentation at the clinic. After sufficient time had elapsed for them to read the information sheet (as observed by the researchers present in the clinic) they were approached by a member of the research team. On gaining signed consent participants were provided with a small booklet of demographic and psychometric questionnaires to complete which assessed a number of psychological phenomena including mood and coping strategies as part of a larger longitudinal study. This paper describes the findings related to the B-IPQ and drawings.
Analysis
Drawings were analysed using a combination of approaches by a researcher blinded to the other data of the participant. After being individually scanned into jpeg files, the National Institutes of Health Image-J software [20] was employed to trace the outline using the freehand function to allow for the irregular shapes of the bladder drawings. This permitted measurement of the total area of each bladder drawing in addition to measurement of the area of damage depicted. This procedure allowed the percentage area of the bladder damaged to be calculated [21]. Interpretation of damage was decided by 2 raters (HLR and RC) who independently classified each drawing as depicting damage or not. Agreement between the raters was high for both “current” and “5 years time/future” drawings (kappa’s 0.93 and 0.81 respectively), and any disagreements were resolved through discussion and referral to a third rater (DGF). This permitted differences in drawings to be examined between demographic and clinical factors in addition to exploring within subject changes in the drawings “currently” and in “5 years’ time”. Secondly, where participants also used emotional representations (e.g. emoji’s or free text) these were analysed using a content analytic approach. Rating of emotional depictions was also undertaken by 2 raters (HLR and RC) and disagreements resolved by referral and discussion with a third rater (DGF).
IBM’s Statistical Package for the Social Sciences (SPSS) version 25 was utilised in the statistical analyses. Interval data were analysed to examine for normality of distribution utilising examination of a combination of sources including Q-Q plots, histograms, skewness and kurtosis measurements. Levene’s test was used to examine homogeneity of variance between groups. Based on these examinations, parametric tests were utilised throughout the analyses except where specifically stated. Descriptive statistics were used to describe the characteristics of the sample (e.g. gender, age, employment status, age at diagnosis, treatment TURBT v TURBT and intravesical therapy). T-tests and one way ANOVA’s permitted examination of differences between groups (e.g., gender, treatment modality), with covariates and Bonferroni post-hoc comparisons. Chi2 or Fishers Exact test as appropriate were utilised to examine the association between categorical variables e.g. gender and depiction of damage. Pearsons correlations enabled associations between variables to be examined (e.g. age, age at onset, illness representations, area of drawings). Differences between groups (e.g. gender, treatment received) in terms of drawings were analysed using independent t-tests or Mann-Whitney U tests where the size of the two groups were not generally homogenous. Within group differences, e.g. changes in perceived bladder damage over time were calculated using paired t-tests. Given the number of tests undertaken, and to control for the possibility of type 1 error, significance levels were set at p < 0.01.
RESULTS
Participants
One hundred and eighteen participants completed the B-IPQ. Of this group 96 (81%) completed 2 drawings of how they perceived their bladder to look ‘currently’ and in ‘5 years’ time’. Reasons for non-completion of drawings included “not knowing” what their bladder looked like and not being “good” at drawing. There were no differences between the group who completed drawings versus those who did not complete the drawings in relation to age, age at onset, or duration of time since diagnosis (t(116)’s < –1.13, p’s > 0.26), or in terms of gender, treatment (TURBT v TURBT and intravesical therapy), reason for attendance (intravesical therapy v surveillance) living circumstances (alone v with family v with others) or marital status (single v married/life partner v divorced/separated v widowed) (χ2< 0.59, df’s = 1, p’s > 0.11). When examining differences between those participants who did and did not provide drawings, the only significant difference found was in relation to the individuals perception of understanding of their bladder cancer (B-IPQ coherence), with those who did not provide a drawing having a significantly poorer understanding of their NMIBC (t(114) = 2.92, p = 0.004). From this point forward the analysis is completed on n = 96 who completed both B-IPQ and bladder drawings.
Sociodemographic, histopathology and treatment variables for the 96 participants are presented in Table 1. Mann-Whitney U and Chi 2 or Fishers exact test as appropriate did not show any significant differences between those attending for surveillance cystoscopy and those attending for intravesical therapy on any of the demographic (χ2 < 1.36, df’s = 1, p’s > 0.24), or illness perceptions data (p’s > 0.013).
Table 1
Sociodemographic and histopathological variables for 96 patients with NMIBC
| Variable | Value |
| Age years, mean (sd; range) | 67.81 (9.83; 39–85) |
| Gender, % male | 69 (71.9) |
| Ethnicity, n (%) | |
| White | 96 (100) |
| Marital status, n (%) | |
| Single | 16 (17.7) |
| Married /life partner | 62 (64.6) |
| Divorced/ separated | 8 (8.3) |
| Widowed | 10 (10.4) |
| Living circumstances, n (%) | |
| Alone | 21 (21.9) |
| With family | 70 (72.9) |
| With others | 5 (5.2) |
| Employment status, n (%) | |
| Employed (full time/part time/ homemaker / voluntary) | 24 (25) |
| Unemployed | 6 (6.3) |
| Retired or other (disability) | 65 (67.7) |
| Missing | 1 (1) |
| Alcohol consumption, % yes | 54 (56.3) |
| Smoking history, n (%) | |
| Non-smoker | 54 (56.3) |
| Ex-smoker | 28 (29.2) |
| Current smoker | 14 (14.6) |
| Age at diagnosis of NMIBC years, mean (sd, range) | 62.6 (10.28, 33–83) |
| Tumour grade*, n (%) | |
| Low grade | 55 (57.3) |
| High grade | 41 (42.7) |
| Tumour stage, n (%) | |
| CIS | 3 (3.1) |
| pTa | 75 (78.1) |
| pT1 | 18 (18.8) |
| Papillary with concurrent CIS, n (%) | 17 (17.7) |
| Time since diagnosis years, mean (sd, range) | 5.28 (5.17, 0–24) |
| Reason for attendance at clinic, n (%) | |
| Surveillance cystoscopy | 82 (85.4) |
| Intravesical therapy | 14 (14.6) |
| Initial treatment, n (%) | |
| TURBT | 68 (70.8) |
| TURBT plus intravesical therapy | 28 (29.2) |
| Intravesicle therapy stage, n (%) | |
| Induction1 | 14 (14.6) |
| Maintenance2 | 11 (11.5) |
| Refractory3 | 3 (3.1) |
*2016 WHO classification system; 1once weekly instillation of BCG for 6 weeks plus a further 6 week course if persistence or recurrence of tumour; 2once weekly instillation for 3 weeks every 3–6 months for 1–3 years; 3disease persistence despite a second course of BCG (second induction or induction and maintenance BCG).
Characteristics of drawings
All participants generated ‘anatomical’ drawings or depictions of their bladders. Annotations or text within the drawing was added by 21 participants (e.g. “cancer”, “bladder damage”, or “all healthy”, “smaller”, “clear”, or “OK” in the bladder). Nine participants utilised an additional emotional representation, for example an emoji.
Drawings of participants “current bladder”, in line with the simple and unstructured anatomical nature of the pictures tended to represent the bladder in a disease focused way, with or without tumour present. Drawings also demonstrated prominent emotional responses to NMIBC, both positive and negative in nature. Specific feelings of sadness, fear, happiness and hope that NMIBC would not return were expressed via either emoji’s or annotations on the drawings. Understandable concerns regarding the presence of tumours was also identified in relation to the bladder in the “current” drawings.
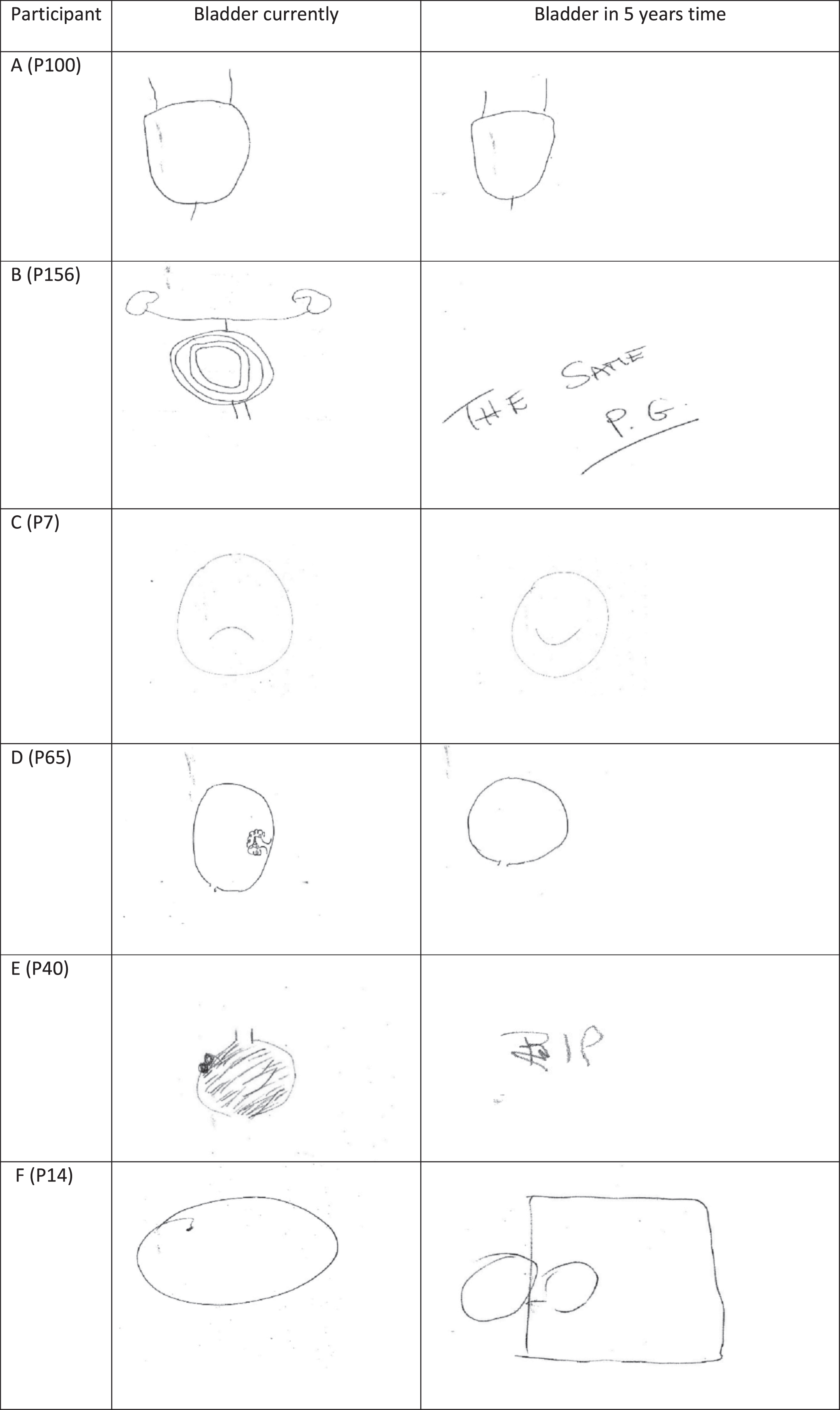
Examples of drawings provided by patients of their bladders as perceived currently and in 5 years’ time are shown in Fig. 1. Of the drawings provided, variations can be observed in terms of anatomical correctness with respect to the bladder: many of the participants depicted very simple drawings of a balloon / ball shape with no changes over time (Panel A) while others drew more detail (panel B). Some individuals used emoji depictions within their drawings (Panel C), whereas other used the drawings to depict improvements in damage caused by cancer (Panel D) or cancer recurrence (damage; Panel’s E & F).
Fig. 1
Examples of patients’ bladder drawings. P100: similar simple drawings lacking anatomical detail; P156: current drawing with more anatomical detail; P7: use of emoji depictions within the drawings; P65: drawings reflecting improvement over time; P40: drawings reflecting anticipation of recurrence and death; P14: drawings represent current clear bladder but anticipation of recurrence and urostomy (verbatim from patient in undertaking drawing).
Paired t-test indicated no statistically significant changes in patients’ drawings of the area of their bladder, between current and future perceptions (t(95) = 1.09, p = 0.28). There was a significant association between current symptom burden (illness identity) and future perceptions of damage depicted at 5 years (r = 0.27, p < 0.01). Independent t-tests indicated no statistically significant differences between grade of cancer (high/low) and area of the bladder drawing or damage depicted (t(94)’s < 2.26, p > 0.03). Kruskal-Wallis H indicated no significant differences between cancer stages and area of the bladder drawing or damage depicted (H’s < 5.49, p’s > 0.06).
Beliefs about NMIBC
Participants’ responses on the B-IPQ ranged between 0 and 10 on all items. Mann-Whitney U analysis indicated the only significant differences between the treatment groups (TURBT alone v TURBT and intravesical therapy) on the illness perception items was in relation to symptoms experienced as part of their condition. As such patients who had undergone intravesical therapy reported significantly greater symptom burden (p < 0.01). There were no significant gender differences on any of the illness perceptions (t(94)’s < –2.57, p’s > 0.01) although there was a trend towards significance in relation to emotional perceptions with women reporting a greater impact (M = 5.44) than men (M = 3.58; t(94) = –2.57, p = 0.012). Pearsons correlations indicated no significant relationships between current age or age at diagnosis and the illness perceptions variables (r’s < –0.26, p’s > 0.02). Understandably, there was a significant association between duration of living with NMIBC and stronger belief in NMIBC being more chronic or long term (r = 0.33, p < 0.01) but duration of diagnosis was not significantly associated with any other illness perception.
When asked about the top 3 reasons perceived to be the cause of their NMIBC, 24% cited smoking as the most important perceived factor for them, followed by diet (6.3%), chemicals in the environment (6.3%) and ageing (5.2%). Over one-third (35.4%) said they were unsure of any specific cause for their NMIBC. Remaining responses accounted for < 4% and ranged from ‘genetics’ to ‘bad luck’. Only 28% of participants provided a response to the second most important cause of their NMIBC; the most frequently noted reasons were stress (5%), smoking (4%) and work exposure to chemicals (4%) with uncategorisable responses accounting for the remaining 13 responses. Eleven responses were recorded for the third most important reason and the most frequently cited reason was diet (2%).
Association between drawing characteristics and demographic, illness related and illness perception variables
Correlation coefficients were examined between area of the bladder drawings and demographic and illness related variables. There were no significant associations between bladder area drawn and patients’ age, age at diagnosis, duration of time since diagnosis, and any of the illness perception variables (r’s < –0.12, p’s > 0.24). There were no significant differences between cancer grade and illness beliefs (t(94)’s < –2.52, p > 0.02). Kruskal-Wallis H indicated no significant differences between cancer stages and illness beliefs (H’s < 3.15 (2), p’s > 0.21) or BCG treatment phase and illness beliefs (H’s < 3.95 (20), p’s > 0.14).
Participants were coded into 3 groups based on their drawings: (a) those that depicted no changes in their bladder over time (46.9%, n = 45); (b) those that depicted improvements in NMIBC (35.4%, n = 34); and (c) those depicting worsening or recurrence of NMIBC (17.7%, n = 17).
There were no associations between depictions of damage over time and treatment modality of participants (TURBT v TURBT and intravesical therapy), reason for clinic attendance (BCG v surveillance cystoscopy), cancer grade (high or low) or cancer stage (CIS, pTa, pT1) (χ2’s < 2.55, df = 2, p’s > 0.25).
To examine whether there were any differences between the 3 drawing groups and demographic variables, one way ANOVA’s were undertaken. There were no significant differences identified between the groups in relation to participants age, age at diagnosis of NMIBC or time since diagnosis of NMIBC (F(2,90)’s < 0.83, p’s > 0.44).
Differences between the 3 drawing groups and illness perceptions were also examined. Table 2 indicates mean scores for the groups. Given the association between illness identity (symptom burden), as measured by the B-IPQ and treatment modality (TURBT alone v TURBT & intravesical therapy) ANOVA was undertaken utilising a categorical covariate of treatment group. Results indicated statistically significant differences across groups on a number of variables (Table 2). For consequences on life (F(2,94) = 9.07, p < 0.01), Bonferroni post-hoc comparisons showed that patients who drew worsening of their NMIBC reported significantly greater consequences than those who depicted no change in the bladder at 5 years (p < 0.01). Similarly for concerns about NMIBC (F(2,94) = 6.17, p < 0.01), post-hoc contrasts showed those who drew worsening of their NMIBC at 5 years reported significantly greater symptom burden currently and stronger patient concerns than the no change group at the p < 0.01 significance level.
Table 2
Verbal illness perceptions (B-IPQ mean scores) held by participants who classified their drawings as depicting ‘no change’, ‘improvement’ and ‘deterioration’
| B -IPQ item$ | No change | Improvement | Deterioration | Total | F(2,93) |
| n = 45 | n = 34 | n = 17 | n = 96 | ||
| Consequences: How much does your illness affect your life? (‘10’- severely affects my life) | 2.36 | 3.71 | 5.76 | 3.44 | 9.07*** |
| Timeline: How long do you think your illness will continue? (‘10’ –forever) | 5.91 | 6.06 | 8.06 | 6.35 | 2.79 |
| Personal control: How much control do you feel you have over your illness? (‘10’-extreme amount of control) | 5.00 | 6.35 | 3.00 | 5.13 | 4.74 |
| Treatment control: How much do you think your treatment can help your illness? (‘10’- extremely helpful) | 8.82 | 8.76 | 7.76 | 8.61 | 1.45 |
| Illness identity: How much do you experience symptoms from your illness? (‘10’- many severe symptoms) | 2.25 | 2.59 | 4.65 | 2.80 | 4.23 |
| Concern: How concerned are you about your illness? (‘10’-extremely concerned) | 3.87 | 5.29 | 7.00 | 4.93 | 6.17** |
| Coherence: How well do you feel you understand your illness? (‘10’ understand very clearly) | 7.91 | 7.50 | 7.59 | 7.71 | 0.28 |
| Emotional representation: How much does your illness effect you emotionally? (e.g. does it make you feel angry, scared, upset or depressed?) (‘10’ –extremely affected emotionally) | 3.13 | 4.68 | 5.53 | 4.10 | 4.41 |
$participants were asked to respond specifically in relation to NMIBC; **p < 0.01; ***p < 0.001.
DISCUSSION
This is the first study to utilise a novel visual/ perceptual method in exploring illness perceptions in patients with NMIBC. The process of asking participants to produce a drawing of their bladder currently and how they anticipate their bladder to look in 5 years time aimed to allow participants to access less verbal linguistic representations of their condition. We further aimed to examine this alongside the more traditional verbal and linguistic models of examining illness perceptions.
The drawings completed in this study clearly portrayed some of the key illness perception dimensions. For example, illness identity and illness coherence were represented by the majority of the patients in their attempts at producing ‘anatomical’ drawings of their bladders, while emotional representations were depicted by patients use of emoji’s. Of particular interest were the depictions of damage in the drawings and the change across time as drawn by the patients. Almost 20% of the sample drew damage in their bladder in the future. Interestingly this perception of future damage at 5 years was unrelated to current demographic or clinical variables. It is suggested that the drawings of damage may represent two complementary dimensions; pathophysiology and fear of cancer recurrence (FCR). FCR is cited as one of the top 5 concerns and most frequently endorsed unmet needs for cancer patients [22]. It is reported to occur in 31–97% of cancer survivors and to be of moderate to high levels in 22–87% of survivors [22–25]. FCR has been shown to be higher in patients with NMIBC who continue to smoke after diagnosis [26]. Indeed while FCR is considered an understandable response to a cancer diagnosis it can be a chronic issue for some patients with extremely disabling impacts on psychological, quality of life and health related behaviours [22]. Patients in the current study who drew worsening disease progression had significantly stronger concerns about NMIBC and negative consequences beliefs which is commensurate with the association between FCR and its negative impact on patients. There is emerging literature in relation to brief helpful strategies for managing FCR [27] and in line with the increased recognition of the need to develop appropriate survivorship services for individuals who have received a diagnosis of NMIBC [4], and recent studies highlighting almost 50% of individuals with NMIBC would like help with managing fears associated with return of cancer [28], the observations of the current study in that almost one fifth of patients drew their condition as worsening irrespective of clinical or demographic variables suggests that FCR may be an important factor to examine further in this population.
Overall, patients reported relatively low levels of perceived consequences of NMIBC on their life, few symptoms associated with their condition, strong beliefs in treatment being able to control their condition and a good understanding of NMIBC, which is generally in line with previous studies [6]. Our sample reported a reasonable level of personal control over their condition. It is well established that illness perceptions are dynamic in nature and thus can change in accordance with an individuals’ experience and the acquisition of ‘new’ information about how, for example, their condition responds to efforts to control NMIBC, such as attending for regular cystoscopy or reducing smoking behaviours. It is suggested that our cohort, with a mean time since diagnosis of 5 years, had developed a personal model of their NMIBC whereby their perceived personal control of NMIBC had been enhanced. Further work examining how enhanced perceptions of control relate to outcomes such as depression and anxiety and attendance for routine cystoscopy in the NMIBC population would be well placed in terms of taking a multifactorial approach to managing this group of patients.
Patients’ knowledge about smoking as a causal factor associated with their NMIBC was poor. Almost a quarter cited smoking as a causal factor, however our data set did not permit us to examine whether the causative factors identified by patients were indeed risk factors for our patient population (e.g. history of smoking or exposure to passive smoke). Given the previous reports of around a 50% association between smoking and bladder cancer [29], the low understanding of smoking as a causative factor in bladder cancer is concerning from a public health perspective and highlights the importance of ongoing education for both patients and the general population around this topic.
The finding that patients who had undergone intravesical therapy reported significantly greater symptom burden on the B-IPQ, but did not demonstrate significant depictions of damage over time, is commensurate with previous drawing studies [21, 30]. This reflects the biopsychosocial model of health and illness that objective severity of disease tends to be only moderately associated with the impact on a patient’s life [31]. The beliefs patients hold about their condition, which may differ from those held by treating physicians, are important in determining outcomes including adherence to treatment, psychological distress and quality of life [8–12].
Using drawings in healthcare communication is not new to medicine and physicians and surgeons have creatively used drawings to illustrate and enhance patient understanding [32–34]. A similar level of understanding can be conveyed by asking for the patient’s perspective in terms of drawings of their damaged organ or organ systems. Using the patient’s drawings as a starting point offers the potential to improve our understanding of the illness experience, inform, and personalise clinical interventions. Within both the endocrinology [30] and cardiac settings [21] drawings provided by patients have illustrated patient’s information needs. Addressing these information needs has the potential to increase patient empowerment and understanding of their condition. Indeed, within NMIBC health literacy has been shown to be related to attendance for surveillance cystoscopy [35]. Similarly, where emotions have been drawn this offers a door-way to discussing such concerns. While psycho-oncology services are increasingly available to patients with a diagnosis of cancer, studies have shown that there exists considerable unmet psychological care needs within urological cancers [36, 37]. A large number of people who could benefit do not access care [38]. Male cancer patients’ may be more reluctant to seek psychological help [39], and men living in rural areas, many of whom would be in the population served in the current study, can be challenging to engage in cancer related psycho-social services [40]. The use of drawings as part of routine care may be helpful in engaging patients in the process of considering the role of interdisciplinary treatment. Future studies might usefully evaluate patients’ perceptions of the task and likewise surgeons’ perspectives of its usefulness in clinical practice.
Limitations
In terms of limitations of the current study, the cross sectional nature of the study means that causation cannot be implied. However, it is suggested that the results may be generalizable in that the patients who took part were recruited from routine outpatient clinics and as such would be more likely to be representative of the general population of NMIBC outpatient clinic attendees. The participation rate of 61.5%, while commensurate with similar drawing studies [21, 30] might introduce some bias in relation to the findings. While we cannot exclude the possibility that the most or least distressed individuals chose to participate or provide drawings, it is of interest that individuals who did not provide drawings only differed on reporting significantly lower beliefs related to illness coherence, that is understanding of their condition. It is possible that this reflects some element of health literacy, a somewhat neglected but important area for urological practice [41, 42]. Importantly, given the scarcity of psychological data relating to this population of individuals with NMIBC and the insights provided in terms of potential concerns relating to cancer recurrence, we believe that this research is an important early step in starting to flesh out the gaps in understanding of patients experience of living with NMIBC and a more person centred management of the individual with NMIBC.
CONCLUSIONS
In the current study, asking patients to draw their bladder alongside more established quantitative measures has allowed for a more enriched understanding of patients perceptions of their condition than just using either assessment method in isolation. Drawings provided by patients, in addition to being simple, quick and cost neutral, are inclusive and provide a control for any language, literacy or verbal communication barriers. Patients representation of their condition through drawings offer the potential to address concerns, open communication channels and provide an element of understanding which may not have been captured by clinical interview, examination or verbal/linguistic psychometric measures alone. Given the life-long involvement of patients with NMIBC with the screening and surveillance process, methods that aim to additionally capture the visual perceptions of NMIBC may help engage patients and establish a helpful aid to communication of their personal model of NMIBC.
ACKNOWLEDGMENTS
Thanks are extended to the staff at the Uro-oncology department, Mercy University Hospital, in particular Marion Hickey, Jane O’Brien and Kate Corcoran who helped to facilitate the recruitment process. Thank you to Elizabeth Broadbent who provided permission for the B-IPQ to be used (personal communication).
FUNDING
This research was not supported by any funding.
AUTHOR CONTRIBUTIONS
HLR and DGF conceptualised the study, undertook the statistical analysis, and wrote the manuscript; PS contributed to data analysis and critically reviewed manuscript; RC undertook data collection, contributed to data analysis critically reviewed the manuscript; CC, AR, JF & COC undertook data collection, and critically reviewed the manuscript.
CONFLICT OF INTEREST
All authors (HLR, PS, RC, CC, AR, JF, COC, DGF) have no conflicts of interest to report.
REFERENCES
[1] | Jung A , Nielsen M , Crandell J , Palmer M , Bryant A , Smith S , Mayer D . Quality of life in non-muscle invasive bladder cancer survivors: A systematic review. Cancer Nurs. (2019) ;42: :E21–E33. |
[2] | Jung A , Nielsen M , Crandell J , Palmer M , Smith S , Bryant A , Mayer D . Health-related quality of life among non-muscle-invasive bladder cancer survivors: a population-based study. BJU Int. (2020) ;125: :38–48. |
[3] | Yu E Y-W , Nekeman D , Billingham LJ , James N D , Cheng KK , Bryan RT , Wesselius A , Zeegers MP . Health-related quality of life around the time of diagnosis in patients with bladder cancer. BJU Int. (2019) ;124: :984–91. |
[4] | Mossanen M , Chang SL . Beyond bladder cancer surveillance: building a survivorship clinic (Editors Choice). BJU Int. (2020) ;125: :2–5. |
[5] | Zhang Z , Yang L , Xie D , Wang Y , Bi L , Zhang T , Wang D , Shi H , Li G , Yu Dl . Illness perceptions are a potential predictor of psychological distress in patients with non-muscle-invasive bladder cancer: a 12 month prospective, longitudinal, observational study. Psychol Health Med. (2020) ;25: :969–79. |
[6] | Tan WS , Teo CH , Chan D , Ang KM , Heinrich M , Feber A , Sarpong R , Williams N , Brew-Graves C , Ng CJ , Kelly J , DETECT II trial collaborators. Exploring patients’ experience and perception of being diagnosed with bladder cancer: a mixed methods approach. BJU Int. (2020) ;125: :669–78. |
[7] | Leventhal H , Brissette I , Leventhal EA . The common-sense model of self-regulaion of health and illness. In LD Cameron & H Leventhal (Eds). The self-regulation of health and illness behaviour (pp. 42-65) 2003, London: Routledge. |
[8] | Leventhal H , Diefenbach M , Leventhal EA . Illness cognition: Using common sense to understand treatment adherence and affect cognition interactions. Cog Ther Res. (1992) ;16: :143–63. |
[9] | Juergens MC , Seekatz B , Moosdorf , Petrie K , Rief W . Illness beliefs before cardiac surgery predict disability, quality of life and depression 3 months later. J Psychosom Res. (2010) ;68: :553–60. |
[10] | Fortune DG , Richards HL , Griffiths CEM , Main CJ . Psychological stress, distress and disability in patients with psoriasis: consensus and variation in the contribution of illness perceptions, coping and alexithymia. Br J Clin Psychol. (2002) ;41: :157–74. |
[11] | Cameron LD , Leventhal EA , Leventhal H . Symptom representations and affect as determinants of care seeking in a community-dwelling, adult sample population. Health Psychol. (1993) ;12: :171–9. |
[12] | Durazo A , Cameron LD . Representations of cancer recurrence risk, recurrence worry, and health-protective behaviours: an elaborated, systematic review. Health Psychol Rev. (2019) ;13: :447–76. |
[13] | Broadbent E , Schoones JW , Tiemensma J , Kaptein AA . A systematic review of patients’ drawing of illness: implications for research using the Common Sense Model. Health Psychol Rev. (2019) ;13: :406–26. |
[14] | Kaptein AA , Broadbent E . Illness cognitions assessment. In Ayers S, Baum A, McManus C, Newman S, Wallston K, Weinman J, West R (eds) Cambridge handbook of psychology health and medicine 2nd ed. Cambridge: Cambridge University Press. 2007:268-73. |
[15] | Broadbent E , Petrie KJ , Main J , Weinmann J . The Brief Illness Perception Questionnaire (B-IPQ). J Psychosom Res. (2006) ;60: :631–7. |
[16] | Broadbent E , Wilkes C , Koschwanez H , Weinman J , Norton S , Petrie KJ . A systematic review and meta-analysis of the Brief Illness Perception Questionnaire. Psychol Health. (2015) ;30: :1361–85. |
[17] | Reynolds L , Broadbent E , Ellis C , Gamble G , Petrie KJ . Patients’ drawings illustrate psychological and functional status in heart failure. J Psychosom Res.. (2007) ;63: :525–32. |
[18] | Scot SE , Birt L , Cavers D , Shah N , Campbell C , Walter FM . Patient drawings of their melanoma: a novel approach to understanding symptom perception and appraisal prior to health care. Psychol Health. (2015) ;30: :1035–48. |
[19] | Ramondt S , Tiemensma J , Cameron LD , Broadbent E , Kaptein AA . Drawings of blood cells reveal people’s perception of their blood disorder: a pilot study. PLoS ONE. (2016) ;11: :e0154348. |
[20] | Rasband W . Image J [computer software]. 1997, U. S. National Institutes of Health, Maryland, USA. Retrieved from https://imagej.nih.gov/ij/download.html |
[21] | Princip M , Koemeda M , Meister RE , Barth J , Schnyder U , Znoj H , Schmid JP , von Känel R . A picture paints a thousand words: heart drawings reflect acute distress and illness perception and predict posttraumatic stress symptoms after acute myocardial infarction. Health Psychol Open. (2015) ;2: :1–10. |
[22] | Simard S , Thewes B , Humphris G , Dixon M , Hayden C , Mireskandari S , Ozakinci G . Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Surviv. (2013) ;7: :300–22. |
[23] | Crist J , Grunfeld E . Factors reported to influence fear of recurrence in cancer patients: a systematic review. Psychooncology. (2013) ;22: :978–86. |
[24] | Koch L , Jansen L , Brenner H , Arndt V . Fear of recurrence and disease progression in long-term (≥5-years) cancer survivors—a systematic review of quantitative studies. Psychooncology. (2013) ;22: :1–11. |
[25] | Thewes B , Butow P , Zachariae R , Christensen S , Simard S , Gotay C . Fear of cancer recurrence: a systematic literature review of self-report measures. J Cancer Surviv.. (2012) ;21: :571–87. |
[26] | Kowalkowski MA , Goltz HH , Petersen NJ , Amiel GE , Lerner SP , Latini DM . Educational opportunities in bladder cancer: increasing cystoscopic adherence and the availability of smoking-cessation programs. J Cancer Educ. . (2014) ;29: :739–45. |
[27] | Tauber N , O’Toole M , Dinkel A , Galica J , Humphris G , Lebel S , Maheu C , Ozakinci G , Prins J , Sharpe L , Smith A , Thewes B , Simard S , Zachariae R . Effect of Psychological Intervention on Fear of Cancer Recurrence: A Systematic Review and Meta-Analysis. J Clin Oncol. (2019) ;37: :1–18. |
[28] | Chung J , Kulkarni GS , Morash R . Matthew A, Papadakos J, Breau RH, Guttman D, Bender J, Jones JM. Assessment of quality of life, information, and supportive care needs in patients with muscle and non-muscle invasive bladder cancer across the illness trajectory. Support Care Cancer. (2019) ;27: :3877–85. |
[29] | Freedman ND , Silverman DT , Hollenbeck AR , Schatzkin A , Abnet CC . Association Between Smoking and Risk of Bladder Cancer Among Men and Women. JAMA.. (2011) ;306: :737–45. |
[30] | Tiemensma J , Pereira AM , Romijn JA , Broadbent E , Biermasz NR , Kaptein AA . Persistent negative illness perceptions despite long-term biochemical control of acromegaly: novel application of the drawing test. Eur J Endocrinol. (2015) ;172: :583–93. |
[31] | Cook SA , Salmon P , Hayes G , Byrne A , Fisher PL . Predictors of emotional distress a year or more after diagnosis of cancer: A systematic review of the literature. Psycho-Oncol. (2018) ;27: :791–801. |
[32] | Cheung MMY , Saini B , Smith L . “It’s a powerful message’: a qualitative study of Australian healthcare professionals’ perceptions of asthma through the medium of drawings. BMJ Open. (2019) ;9: :e027699. doi: 10.1136/bmjopen-2018-027699 |
[33] | Kearns C . Is drawing a valuable skill in surgical practice? 100 surgeons weigh in. J Vis Commun Med. (2019) ;42: :4–14. |
[34] | Kearns C , Kearns N & Paisley AM . The art of consent: visual materials help adult patients make informed choices about surgical care. J Vis Commun Med. (2020) ;43: :76–83. |
[35] | Turkoglu AR , Demirci H , Coban S , Guzelsoy M , Toprak E , Aydos MM , Ture DA , Ustundag Y . Evaluation of the relationship between compliance with the follow-up and treatment protocol and health literacy in bladder tumor patients. Aging Male. (2019) ;22: :266–71. |
[36] | Paterson C , Jensen BT , Jensen JB , Nabi G . Unmet informational and supportive care needs of patients with muscle invasive bladder cancer: A systematic review of the evidence. Eur J Oncol Nurs. (2018) ;35: :92–101. |
[37] | McIntosh M , Opozda MJ , Evans H , Finlay A , Galvao DA , Chambers SK , Short CE . A systematic review of the unmet supportive care needs of men on active surveillance for prostate cancer. Psycho-Oncol. (2019) ;28: :2307–22. |
[38] | Steginga SK , Campbell A , Ferguson M , Beeden A , Walls M , Cairns W , Dunn J . Socio-demographic, psychosocial and attitudinal predictors of help seeking after cancer diagnosis. Psycho-Oncol. (2008) ;17: :997–1005. |
[39] | Faller H , Weis J , Koch U , Brahler E , Harter M , Keller M , et al. Utilization of professional psychological care in a large German sample of cancer patients. Psycho-Oncol. (2017) ;26: :537–43. |
[40] | Harrison NJ , Gunn KM , Wilson CJ . Can targeting information on cancer-related psychosocial services by male gender and rurality improve attitude to service use in this difficult-to-engage population? Psycho-Oncol. (2020) ;29: :2075–83. |
[41] | Luckenbaugh AN , Moses KA . The impact of health literacy on urologic oncology care. Urol Oncol. 2019; doi:10.1016/j.urolonc.2019.06.016 |
[42] | Scarpato KR , Kappa SF , Goggins KM , Chang SS , Smith JR. JA , Clark PE et al. The Impact of Health Literacy on Surgical Outcomes Following Radical Cystectomy. J. Health Commun. (2016) ;21: :99–104. DOI: 10.1080/10810730.2016.1193916 |




