Well-being and Perceptions of Supportive Resources among Caregivers of Patients with Bladder Cancer
Abstract
BACKGROUND:
The unique burden of treatment and survivorship of patients with bladder cancer can negatively impact caregiver experience and their use of supportive care resources.
OBJECTIVE:
To assess caregivers’ well-being and their perception of potential supportive resources.
METHODS:
In this cross-sectional survey, caregivers of patients with bladder cancer (N = 630) were recruited through the nationwide Bladder Cancer Advocacy Network Patient Survey Network. We used stakeholder-developed questionnaires to examine caregiver well-being (i.e., physical well-being, tiredness, fear, worry, sadness), the perceived helpfulness of potential resources (i.e., web-based and print-based information, specialized support, personal stories of other caregivers, phone-call and online chat with other caregivers), and influencing factors.
RESULTS:
Caregivers more frequently reported emotional well-being as a moderate to serious problem (67% for fear, 78% for worry, 66% for sadness) compared with physical well-being (30%) and tiredness (47%). Decreased well-being was associated with female gender of the caregiver, higher than high school education, or caring for a patient with advanced (versus non-invasive) bladder cancer. Of six potential resources, “web-based information” was perceived as “very helpful” among 79% of respondents, followed by “personal stories from other caregivers” (62%). Caregiver preferences for “web-based information” was not associated with any specific demographic or clinical factors.
CONCLUSIONS:
Caregivers reported moderate to serious problems with emotional and physical well-being. Web-based platforms were perceived as beneficial supportive resources for bladder cancer caregivers. Future intervention research should target the influencing factors identified in this study to optimize the health outcomes of caregivers and enhance the supportive care resources for improving their well-being.
INTRODUCTION
Cancer impacts not only patients with cancer but also their caregivers who may represent spouses, relatives, or friends. Caregivers play important roles in providing care and support during cancer survivorship [1]. The number of cancer survivors is estimated to increase from 16.9 million in 2019 to 22.1 million by 2030 in the United States (US) [2, 3]. Caregivers of cancer patients thus have an expanding role in improving healthcare delivery and outcomes, particularly as growing numbers of patients with cancer are discharged from the hospital earlier and survive longer as diagnostic and treatment options improve [4]. Related to their expanded role in healthcare delivery, caregivers experience physical, social, emotional, and financial burdens [5, 6]. In addition, caregivers of cancer patients experience higher levels of burden and distress than non-cancer caregivers due to the unpredictability and often life-threatening nature of cancer and its treatment [7]. The caregiving experience and burden of caring for patients with cancer can decrease caregivers’ quality of life (QOL), which in turn negatively impact the cancer patients’ health outcomes [8, 9]. Thus, caregivers of patients with cancer require support as they provide care and assistance in the management of cancer.
Patients with bladder cancer and their caregivers face a unique burden from treatment-related symptoms and stress. For this reason, the challenges they face are of particular interest. Bladder cancer is the sixth most common cancer in the US [3]. Approximately 75% of patients are diagnosed with non-muscle-invasive bladder cancer and are managed with frequent surveillance cystoscopy, transurethral resection of bladder tumors, and intravesical treatment due to the high rates of recurrence and progression [10]. The remaining 25% have muscle-invasive bladder cancer and are often treated with cystectomy and urinary diversion or combined-modality therapy with intensive surveillance [11]. These complex treatments can lead to common symptoms and treatment-related complications, such as significant lower urinary tract symptoms, frequent urinary tract infections, hematuria, and dehydration [10, 12], as well as significant psychosocial issues such as uncertainty and distress [13]. In addition, bladder cancer, with a median age of 75 years, is prevalent among the elderly population [3] who often experience physical, functional, and cognitive declines and comorbid conditions that require frequent and intense caregiving. Providing care and support for an elderly cancer population with complex treatment-related symptoms and complications, as well as comorbid conditions, can contribute to an increased caregiver burden, which warrants the need for helpful cancer-specific caregiver resources and support.
Despite the treatment complications and related psychosocial challenges and their potential impacts on bladder cancer caregivers, little is known about caregiver well-being associated with bladder cancer and caregivers’ perceptions of supportive care resources. We conducted a national survey to understand the well-being and supportive care needs of caregivers of patients with bladder cancer. The survey was conducted in partnership with the Bladder Cancer Advocacy Network (BCAN), a national organization supporting bladder cancer patients and their caregivers. Our objectives of the study were to 1) describe well-being of bladder cancer caregivers and how they perceive the helpfulness of potential resources; and 2) identify the clinical and demographic factors influencing these outcomes.
MATERIALS AND METHODS
Study design sample and procedure
A cross-sectional online survey was administered using a convenience sampling method. Self-identified caregivers of individuals with bladder cancer were recruited from the Patient Survey Network (PSN) between June 2018 and January 2019. Inclusion criteria were individuals 1) who had ever been a caregiver of patients with bladder cancer and 2) who were able to read and write in English.
Using a combination of online, print, and word-of-mouth advertisement through BCAN, bladder cancer patients and caregivers were invited to join the PSN, established to incorporate patients and caregivers in the research process and to identify patient-centered research topics for prioritization in bladder cancer [14]. For recruitment of this study, we sent an email to PSN participants asking them to complete the survey if they self-identified as a caregiver of somebody with bladder cancer at any point in time or to forward the survey to someone who could identify themselves as a bladder cancer caregiver at any point in time. We also posted the survey on support forum online sites, such as Inspire (https://www.inspire.com/groups/bladder-cancer-advocacy-network/) - the largest online sup-port forum for patients with bladder cancer and their caregivers. Participants were asked to provide online consent prior to answering questions. All data collected were de-identified, and thus, the study was exempted from the Institutional Review Board (IRB) approval.
Measures
A group of stakeholders of BCAN research, including patient advocates, clinicians, and researchers, met monthly to discuss and make decisions about the design and implementation of the survey. The detailed information about the multistakeholder group and the survey development process can be found elsewhere [14, 15]. Based upon group discussion, the measures used in this survey were derived from existing questionnaires such as the Caregiver Burden Scale [16] and Caregiver Oncology Quality of Life [17]. Caregiver well-being (i.e., physical well-being, tiredness, fear, worry, sadness) was measured with a four-point Likert scale from ‘not a problem’ to ‘serious problem’. The potential resources for caregivers included 1) web-based information about bladder cancer and treatment options; 2) print-based information about bladder cancer and treatment options; 3) contact information for individuals that can offer one-on-one specialized support (e.g., social worker, financial counselor); 4) personal stories from other caregivers that describe how they cared for a loved one with bladder cancer; 5) phone call with another bladder cancer caregiver; and 6) real-time question and answer online chat with another bladder cancer caregiver. The perceived helpfulness of the potential resources was measured with a three-point Likert scale (not helpful, somewhat helpful, very helpful). Participants also provided demographic information regarding themselves (i.e., age, gender, race, ethnicity, education, relationship to the patient), and patient clinical characteristics (i.e., bladder cancer diagnosis, treatment, urinary tract reconstruction, time since diagnosis).
Data analysis
Descriptive statistics were computed to summarize the demographic/clinical characteristics, caregiver well-being and their perception of resources. To identify the influencing factors of caregiver well-being, we conducted logistic regression to examine the relationships between caregiver well-being and caregiver/caregiving recipient characteristics (age, gender, education, relationship to patient, bladder cancer stage, and treatment). The 4 levels of well-being were combined into 2 categories (i.e., not a problem/minor problem vs. moderate/serious problem) for logistic regression using “not a problem/minor problem” as the referent. To identify factors influencing caregiver perception of supportive care resources, we conducted Chi-squared tests and Fisher’s exact test to determine whether perceived helpfulness of the resources was related to caregiver/caregiving recipient characteristics (age, gender, education, relationship to patient, bladder cancer stage, and urinary tract reconstruction). P values < 0.05 were considered statistically significant. All statistical analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
Participant characteristics
A total of 630 participants identified themselves as caregivers of bladder cancer patients. After excluding 71 caregivers who did not answer at least one question regarding caregiver well-being and resources, 559 caregivers were included in the analysis. The majority of caregivers self-identified as a spouse or partner, female, white, non-Hispanic, and had completed at least a college education (Table 1). The age of caregivers ranged from 21 to 85 years, with a mean of 61 years. Regarding patient characteristics, 34.5% reported non-invasive bladder cancer, 38.2% invasive bladder cancer, and 27.3% metastatic bladder cancer. Caregivers reported that patients most often received bladder removal (58.8%), followed by bladder-sparing treatments (22.6%) and systemic therapy only (18.6%). Approximately 59% (n = 328) of the caregivers reported that their patients underwent cystectomy for bladder cancer treatment, including 64.8% (n = 212) who underwent ileal conduit and 33.7% (n = 110) who underwent neobladder or Indiana pouch.
Table 1
Caregiver and Caregiving Recipient Characteristics (N = 559)
| Characteristic | n | Frequency (%) |
| Caregiver’s Relationship to the Patient | 549 | |
| Spouse/Partner | 460 (83.8%) | |
| Non-Spouse/Partner | 89 (16.2%) | |
| Caregiver’s Gender | 522 | |
| Male | 85 (16.3%) | |
| Female | 437 (83.7%) | |
| Caregiver’s Race | 520 | |
| White | 493 (94.8%) | |
| Non-White | 27 (5.2%) | |
| Caregiver’s Ethnicity | 518 | |
| Hispanic, Latino/a, or Spanish origin | 16 (3.1%) | |
| Other | 502 (96.9%) | |
| Caregiver’s Age, years | 517 | |
| Mean (SD), Range | 61.4 (11.1), 21– 85 | |
| ≦ 60 | 216 (41.8%) | |
| 61– 70 | 193 (37.3%) | |
| ≧ 71 | 108 (20.9%) | |
| Caregiver’s Education | 520 | |
| High school or less | 53 (10.2%) | |
| College (some or graduate) or technical school | 324 (62.3%) | |
| Post-college graduate | 143 (27.5%) | |
| Patient’s Bladder Cancer Diagnosis | 539 | |
| Non-invasive bladder cancer (Ta, T1, CIS) | 186 (34.5%) | |
| Invasive bladder cancer (T2, T3, T4) | 206 (38.2%) | |
| Metastatic bladder cancer (spread to beyond the bladder) | 147 (27.3%) | |
| All Types of Previous Treatment | 559 | |
| TURBT | 354 (63.3%) | |
| Cystectomy | 328 (58.7%) | |
| Partial Cystectomy | 12 (2.2%) | |
| Nephrectomy | 31 (5.6%) | |
| Chemotherapy | 292 (52.2%) | |
| Radiation | 105 (18.8%) | |
| Intravesical therapy | 252 (45.1%) | |
| Immunotherapy | 112 (20.0%) | |
| Clinical Trials | 57 (10.2%) | |
| Not sure | 3 (0.5%) | |
| Treatment | 558 | |
| Bladder-sparing treatments | 126 (22.6%) | |
| Bladder removal | 328 (58.8%) | |
| Systemic therapy only | 104 (18.6%) | |
| Urinary Tract Reconstruction (among Cystectomy) | 327a | |
| Ileal Conduit | 212 (64.8%) | |
| Neobladder/Indiana Pouch | 110 (33.7%) | |
| Not sure | 5 (1.5%) | |
| Time since diagnosis | 523 | |
| 1-2 years | 90 (17.2%) | |
| 3– 5 years | 228 (43.6%) | |
| >5 years | 205 (39.2%) |
a1 respondent, who did not answer the question, was excluded.
Caregiver well-being and perceived helpfulness of the potential resources
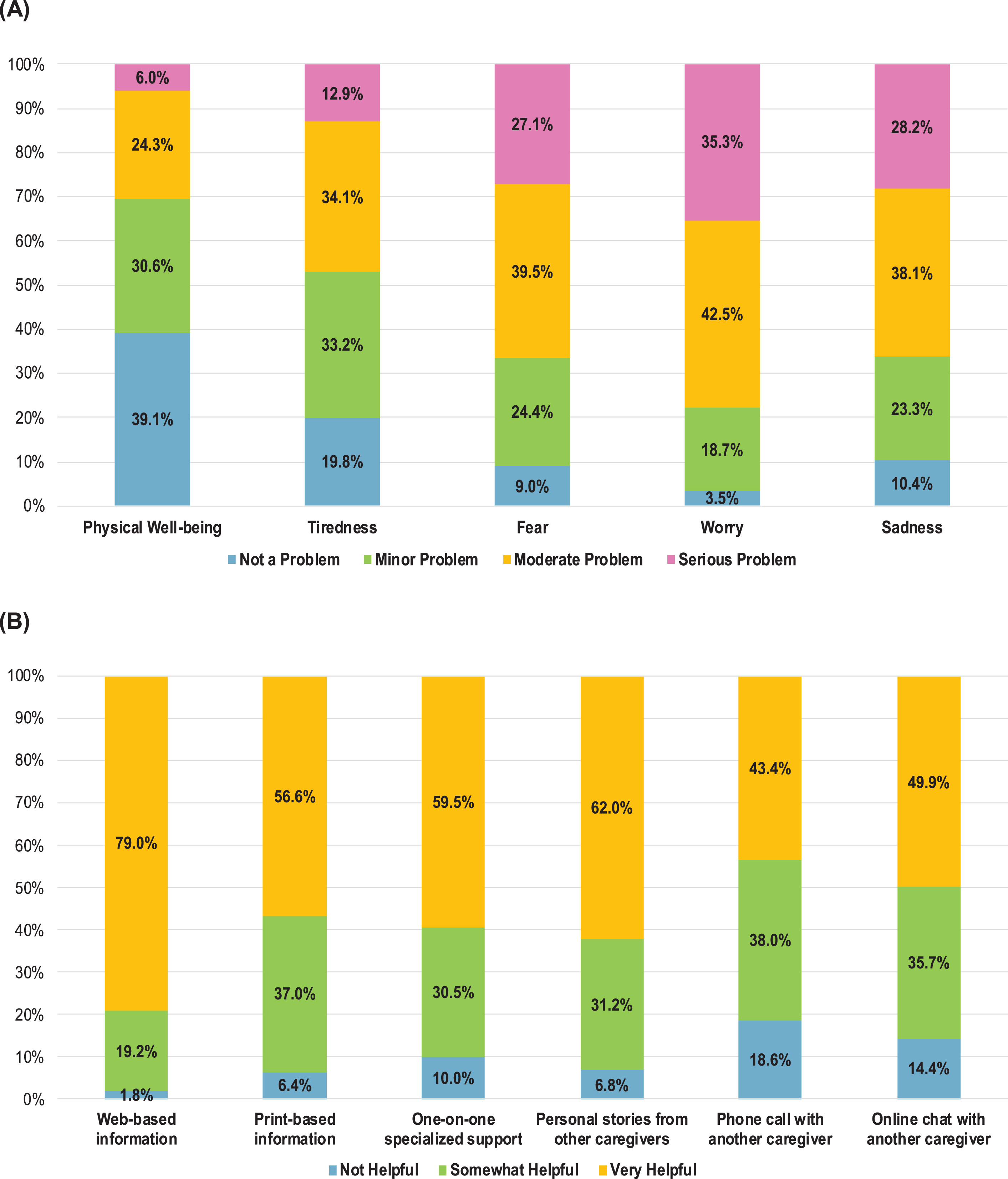
More than half of the caregivers reported that physical well-being (69.7%) and tiredness (53.0%) were “not a problem” or a “minor problem” (Fig. 1A). However, more than two-thirds of caregivers reported that fear (66.6%), worry (77.8%), and sadness (66.3%) were a “moderate” to “serious problem” for them.
The top four potentially helpful resources identified by the majority of caregivers included web-based information about bladder cancer and treatment options (79.0%), personal stories from other bladder cancer caregivers (62.0%), one-on-one specialized support (59.5%), and print-based information about bladder cancer and treatment options (56.6%) (Fig. 1B). Phone calling and online chatting with another bladder cancer caregiver were reported as ‘very helpful’ by the fewest caregivers. Nevertheless, approximately half (49.9% and 43.4%) of caregivers reported that an online chat or phone call with another bladder cancer caregiver respectively would be very helpful.
Fig. 1
(A) Caregiver well-being, (B) Perceived helpfulness of the potential resources. For both figures n = 559.
Factors influencing caregiver well-being
Caregiver age was negatively associated with the odds of their reported fear (odds ratio (OR) =0.97, 95% confidence interval (CI)=[0.94, 0.99]) after adjusting for gender, education, relationship to patient, bladder cancer stage, and treatment (Table 2). Compared with their male counterparts, being a female caregiver was associated with higher levels of tiredness (OR = 2.24, CI =), fear (OR = 2.14, CI = [1.25, 3.67]), worry (OR = 2.77, CI = [1.54, 4.99]), and sadness (OR = 1.80, CI = [1.04, 3.12]). Compared with caregivers with at most a high school education, caregivers who finished college or technical school reported significantly higher tiredness (OR = 1.99, CI = [1.02, 3.89]) and caregivers who completed post-college education reported significantly higher worry (OR = 2.34, CI = [1.04, 5.26]). Regarding cancer stage, caregivers of patients with invasive bladder cancer (T2, T3, T4) reported significantly more moderate/serious problems with physical well-being (OR = 2.08, CI = [1.16, 3.72]), tiredness (OR = 1.98, CI = [1.18, 3.32]), and fear (OR = 1.77, CI = [1.04, 3.01]) than caregivers of patients with non-invasive bladder cancer (Ta, T1, CIS). Caregivers of patients with metastatic bladder cancer also reported significantly more moderate/serious problems with all caregiver well-being outcomes than caregivers of patients with non-invasive bladder cancer. Caregiver well-being, however, did not vary significantly by patient-caregiver relationship nor by the treatment patients received.
Table 2
Logistic Regression for Caregiver Well-being
| Physical Well-being | Tiredness | Fear | Worry | Sadness | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Caregiver Age (continuous) | 1.00 (0.97, 1.02) | 0.99 (0.97, 1.01) | 0.97 (0.94, 0.99) | 0.97 (0.95, 1.00) | 0.98 (0.96, 1.01) |
| Caregiver Gender | |||||
| Male | 1 (Referent) | 1 (Referent) | 1 (Referent) | 1 (Referent) | 1 (Referent) |
| Female | 1.75 (0.94, 3.28) | 2.24 (1.26, 3.97) | 2.14 (1.25, 3.67) | 2.77 (1.54, 4.99) | 1.80 (1.04, 3.12) |
| Caregiver Education | |||||
| High school or less | 1 (Referent) | 1 (Referent) | 1 (Referent) | 1 (Referent) | 1 (Referent) |
| College or technical school | 1.37 (0.66, 2.86) | 1.99 (1.02, 3.89) | 1.20 (0.62, 2.33) | 1.63 (0.80, 3.34) | 1.20 (0.62, 2.34) |
| Post-college graduate | 2.07 (0.94, 4.55) | 2.03 (0.98, 4.20) | 1.30 (0.63, 2.67) | 2.34 (1.04, 5.26) | 1.31 (0.64, 2.70) |
| Relationship to patient | |||||
| Non-Spouse/Partner | 1 (Referent) | 1 (Referent) | 1 (Referent) | 1 (Referent) | 1 (Referent) |
| Spouse/Partner | 0.82 (0.43, 1.57) | 0.68 (0.36, 1.28) | 1.05 (0.52, 2.13) | 0.83 (0.35, 1.97) | 0.75 (0.36, 1.54) |
| Bladder Cancer stage | |||||
| Non-invasive (Ta, T1, CIS) | 1 (Referent) | 1 (Referent) | 1 (Referent) | 1 (Referent) | 1 (Referent) |
| Invasive (T2, T3, T4) | 2.08 (1.16, 3.72) | 1.98 (1.18, 3.32) | 1.77 (1.04, 3.01) | 1.40 (0.78, 2.53) | 1.31 (0.78, 2.21) |
| Metastatic (spread to beyond the bladder) | 2.66 (1.44, 4.92) | 2.26 (1.29, 3.93) | 2.59 (1.41, 4.76) | 4.22 (1.90, 9.38) | 4.44 (2.29, 8.61) |
| Treatment | |||||
| Bladder-sparing treatments | 1 (Referent) | 1 (Referent) | 1 (Referent) | 1 (Referent) | 1 (Referent) |
| Bladder removal | 1.27 (0.66, 2.44) | 1.63 (0.92, 2.90) | 0.78 (0.44, 1.41) | 0.69 (0.36, 1.34) | 1.11 (0.63, 1.96) |
| Systemic therapy only | 1.20 (0.57, 2.53) | 1.65 (0.85, 3.18) | 1.19 (0.60, 2.34) | 1.39 (0.62, 3.11) | 1.57 (0.81, 3.06) |
Abbreviations: CI, confidence interval; OR, odds ratio.
Factors influencing perceived helpfulness of the potential resources
Caregivers’ perception of greater helpfulness of the specialized support was associated with patient’s advanced cancer stage and having neobladder/Indiana pouch (vs. ileal conduit) (Table 3). Greater levels of perceived helpfulness of personal stories from other bladder cancer caregivers were associated with female gender and advanced cancer stage. Greater levels of perceived helpfulness of a phone call with another caregiver were associated with caregiver age < = 60 years, female gender, being a non-spousal caregiver, and advanced cancer stage. Greater levels of perceived helpfulness of an online chat with another caregiver were associated with caregiver age < = 60 years and being a non-spousal caregiver. However, caregivers’ perception of the potential resources was not associated with their education level.
Table 3
Factors Associated with Perceived Helpfulness of the Potential Resources to Caregiver
| Web-based information | Print-based information | Specialized support | |||||||||||||
| Variable | n | NH | SH | VH | χ2 | n | NH | SH | VH | χ2 | n | NH | SH | VH | χ2 |
| Age | |||||||||||||||
| ≦ 60 | 215 | 1.9% | 14.9% | 83.2% | 212 | 7.5% | 37.3% | 55.2% | 215 | 7.0% | 28.8% | 64.2% | |||
| 61– 70 | 192 | 1.6% | 16.1% | 82.3% | 8.66 | 187 | 3.7% | 38.0% | 58.3% | 3.96 | 190 | 11.6% | 31.0% | 57.4% | 4.24 |
| ≧ 71 | 105 | 1.0% | 27.6% | 71.4% | 106 | 8.5% | 33.0% | 58.5% | 103 | 12.6% | 29.1% | 58.3% | |||
| Gender | |||||||||||||||
| Male | 84 | 2.4% | 20.2% | 77.4% | 0.68 | 83 | 8.4% | 37.4% | 54.2% | 1.06 | 84 | 10.7% | 38.1% | 51.2% | 3.86 |
| Female | 432 | 1.6% | 17.4% | 81.0% | 426 | 5.6% | 36.6% | 57.8% | 428 | 9.3% | 28.3% | 62.4% | |||
| Education | |||||||||||||||
| ≦ High school | 53 | 1.9% | 17.0% | 81.1% | 52 | 1.9% | 26.9% | 71.2% | 51 | 7.8% | 25.5% | 66.7% | |||
| College or technical school | 318 | 1.6% | 17.0% | 81.4% | 1.56 | 316 | 5.4% | 38.6% | 56.0% | 8.05 | 319 | 8.5% | 29.8% | 61.7% | 4.67 |
| Post-college graduate | 143 | 1.4% | 21.7% | 76.9% | 140 | 9.3% | 37.9% | 52.8% | 140 | 13.6% | 32.1% | 54.3% | |||
| Relationship to patient | |||||||||||||||
| Spouse/Partner | 453 | 2.2% | 19.0% | 78.8% | 1.96 | 448 | 6.0% | 36.0% | 58.0% | 2.72 | 447 | 11.0% | 30.6% | 58.4% | 3.41 |
| Non-Spouse | 87 | 0% | 19.5% | 80.5% | 85 | 9.4% | 41.2% | 49.4% | 87 | 4.6% | 31.0% | 64.4% | |||
| Cancer stage | |||||||||||||||
| Non-invasive | 184 | 1.1% | 16.3% | 82.6% | 181 | 2.8% | 38.1% | 59.1% | 177 | 14.7% | 33.9% | 51.4% | |||
| Invasive | 198 | 3.0% | 21.2% | 75.8% | 4.03 | 197 | 7.6% | 34.0% | 58.4% | 7.94 | 200 | 7.0% | 28.0% | 65.0% | 10.35* |
| Metastatic | 147 | 1.3% | 18.4% | 80.3% | 144 | 8.3% | 41.7% | 50.0% | 146 | 8.2% | 30.1% | 61.7% | |||
| UT reconstruction | |||||||||||||||
| Ileal conduit | 206 | 1.5% | 21.8% | 76.7% | 1.99 | 204 | 8.3% | 30.9% | 60.8% | 3.64 | 207 | 9.7% | 27.0% | 63.3% | 6.94* |
| Neobladder/ Indiana pouch | 109 | 0.9% | 15.6% | 83.5% | 106 | 4.7% | 40.6% | 54.7% | 107 | 1.9% | 32.7% | 65.4% | |||
| Personal stories from other caregivers | Phone call with another caregiver | Online chat with another caregiver | |||||||||||||
| Variable | n | NH | SH | VH | χ2 | n | NH | SH | VH | χ2 | n | NH | SH | VH | χ2 |
| Age | |||||||||||||||
| ≦ 60 | 215 | 4.6% | 27.0% | 68.4% | 213 | 11.7% | 41.3% | 47.0% | 211 | 9.5% | 33.6% | 56.9% | |||
| 61– 70 | 190 | 5.8% | 35.3% | 58.9% | 8.23 | 185 | 21.6% | 38.4% | 40.0% | 11.92* | 183 | 15.9% | 36.6% | 47.5% | 10.9* |
| ≧ 71 | 104 | 10.6% | 31.7% | 57.7% | 105 | 25.7% | 32.4% | 41.9% | 102 | 20.6% | 38.2% | 41.2% | |||
| Gender | |||||||||||||||
| Male | 84 | 13.1% | 34.5% | 52.4% | 9.11* | 83 | 25.3% | 42.2% | 32.5% | 5.98* | 83 | 20.4% | 39.8% | 39.8% | 5.71 |
| Female | 429 | 5.1% | 30.1% | 64.8% | 424 | 16.7% | 37.5% | 45.8% | 417 | 12.7% | 34.8% | 52.5% | |||
| Education | |||||||||||||||
| ≦ High school | 52 | 1.9% | 32.7% | 65.4% | 50 | 14.0% | 32.0% | 54.0% | 50 | 18.0% | 30.0% | 52.0% | |||
| College or technical school | 317 | 6.3% | 29.0% | 64.7% | 4.76 | 317 | 18.0% | 38.8% | 43.2% | 2.93 | 311 | 12.5% | 36.0% | 51.5% | 2.46 |
| Post-college graduate | 142 | 7.8% | 35.9% | 56.3% | 138 | 20.3% | 39.1% | 40.6% | 137 | 16.1% | 37.2% | 46.7% | |||
| Relationship to patient | |||||||||||||||
| Spouse/Partner | 450 | 7.8% | 32.0% | 60.2% | 4.78 | 444 | 20.5% | 37.8% | 41.7% | 6.39* | 437 | 16.0% | 36.4% | 47.6% | 9.16** |
| Non-Spouse | 87 | 2.3% | 27.6% | 70.1% | 86 | 9.3% | 39.5% | 51.2% | 85 | 4.7% | 34.1% | 61.2% | |||
| Cancer stage | |||||||||||||||
| Non-invasive | 181 | 11.6% | 27.6% | 60.8% | 175 | 26.9% | 38.3% | 34.8% | 175 | 18.9% | 34.3% | 46.8% | |||
| Invasive | 199 | 5.0% | 30.2% | 64.8% | 10.76* | 200 | 16.0% | 32.5% | 51.5% | 21.55** | 192 | 12.5% | 33.3% | 54.2% | 6.80 |
| Metastatic | 146 | 4.1% | 36.3% | 59.6% | 143 | 11.2% | 46.1% | 42.7% | 144 | 10.4% | 40.3% | 49.3% | |||
| UT reconstruction | |||||||||||||||
| Ileal conduit | 207 | 4.8% | 30.0% | 65.2% | 1.10 | 203 | 15.3% | 36.4% | 48.3% | 2.23 | 199 | 15.6% | 36.7% | 47.7% | 3.28 |
| Neobladder/ Indiana pouch | 107 | 3.8% | 25.2% | 71.0% | 107 | 9.3% | 37.4% | 53.3% | 105 | 10.5% | 31.4% | 58.1% | |||
Abbreviations: NH, not helpful; SH, somewhat helpful; UT, urinary tract; VH, very helpful. * p-value < 0.05, ** p-value < 0.01 (Fisher’s exact test was used for p-value for gender, relationship to patient, and UT reconstruction variables.)
DISCUSSION
We investigated the well-being of caregivers of patients with bladder cancer and their perception of the usefulness of different supportive resources. The caregiver experience was marked by decreased emotional and physical well-being. Cancer stage and caregiver characteristics such as gender, education, and age were associated with caregiver well-being. Also, web-based materials and personal stories were perceived to be very helpful by the highest number of caregivers. Although caregivers’ perceived helpfulness of personal stories was associated with gender and cancer stage, their perceived helpfulness of web-based information was not associated with any of the demographic and patient cancer-related factors we examined.
In this study, more than two-thirds of caregivers reported fear, worry, and sadness as moderate to serious problems compared with 30– 47% reporting physical well-being and tiredness. Caregivers in other malignancies such as pancreatic cancer follow a similar pattern of QOL decrease in all domains, but most pronounced for emotional/psychological QOL [18]. In addition, we found that caregivers who are of younger age, female, with an advanced degree, and caring for a patient with advanced stage of cancer were more likely to experience decreased emotional well-being. Similar to findings of prior studies among patients with various malignancies and their caregivers [19, 20], older caregivers in this study reported less fear than their younger counterparts, which may be related to decreased fear of death with increased age as demonstrated in other studies [21]. Compared with male caregivers, female caregivers reported higher levels of fear, worry, and sadness in our study, which has also been demonstrated in a prior study regarding depression in cancer caregivers [22]. In addition, patients having advanced cancer stage increased the odds of caregivers reporting more serious problems with fear, worry, and sadness in our study. Our findings are consistent with the association between caregivers’ emotional well-being and impairment of patients with advanced cancer reported in a study of 364 caregivers of breast, digestive, and lung cancer patients [23]. Interestingly, among patients with advanced cancer, the patient’s own physical and emotional health may influence the emotional well-being of their caregivers. Prior studies showed that patients’ anxiety, depression, and emotional distress, which occur frequently as cancer progresses, were likewise associated with caregivers’ anxiety, depression, and emotional distress [9, 24]. Unfortunately, given the study design, we could not assess the interplay between patient and caregiver well-being, but future research should investigate this important relationship.
Our study also identified the resources that caregivers perceived to be helpful in managing the emotional and physical burden of caregiving. According to a survey of 196 caregivers of renal cell carcinoma patients, unmet information needs are associated with elevated anxiety and depression [25]. Improving helpfulness of resources for caregivers can fulfill unmet needs and improve their well-being. We found that caregivers perceived information about bladder cancer and treatment options as well as connections to other bladder cancer caregivers as helpful resources. Given that the average age of caregivers in our study was 61 years, one might question the relationship between older age and limited use of technology [26]. However, 79% of the caregivers reported web-based information about bladder cancer and treatments as very helpful. Although this may be due to selection bias related to use of the online platform for our survey, a prior study also corroborated the utility of Internet-based resources among caregivers, demonstrating that 93% of younger cancer caregivers and 76% of caregivers over the age of 65 were willing to access Internet-based tools [27]. We found that, similar to these results, web-based information was perceived to be very helpful by the respondents of all age groups although such perception was most common among those younger than 60 years. These findings suggest that older age does not preclude the use of internet/web-based programs for supportive oncologic care.
We also found that specialized support was perceived to be more helpful for caregivers taking care of patients with advanced disease. The association between specialized support and advanced cancer was not surprising, as the complexity of treatments and care can increase for invasive or metastatic disease compared with non-invasive cancer. For example, advanced cancer patients may see a nutritionist after bowel resection for an ileal conduit or neobladder, for poor appetite during surgery recovery, or for failure to thrive due to metastatic disease. Patients with an ileal conduit also benefit from visits with ostomy nurses to manage skin and appliance issues. Caregivers of patients with a neobladder may especially be more likely to find specialized support helpful, perhaps because of the upfront need to train the neobladder (e.g., necessary maintenance using irrigation) and the education needed to perform clean intermittent catheterization. Accessing specialized support may increase caregivers’ capacity in managing cancer-related issues, and thus help reduce caregiver burden and improve caregiver well-being. Prior research has demonstrated that when caregivers receive education to increase their self-efficacy and mastery of caregiving tasks, they experience better well-being [28]. In contrast, caregivers for those with earlier stages of bladder cancer did not perceive as much benefit to specialized support services, which may be due to the lower maintenance and less specialized knowledge required to care at home for a patient undergoing treatments such as surveillance cystoscopy or maintenance BCG.
Despite being the first study to investigate caregivers’ well-being and their perception of the useful-ness of supportive resources in bladder cancer care, our study has several limitations. First, we did not use a validated instrument but rather a stakeholder-modified questionnaire with questions that were derived from existing questionnaires. Patient and caregiver advocates involved in the study design felt that existing validated questionnaires did not capture the important and relevant information about their well-being, but wished to limit the number of questions to reduce survey burden. An additional limitation of our study is its cross-sectional design, which does not capture the impact of bladder cancer and its treatment on caregiver physical and psychological health over time. For example, while 69.7% of caregivers in our study did not report significant problems in physical well-being, one longitudinal study has shown that cancer caregiving is related to objective physical impairments such as increased rates of arthritis, back pain, and heart disease [29]. Third, our cohort may not be representative of the general population of caregivers for bladder cancer patients, given the great proportion of white, female caregivers with college or higher education. However, it should be noted that the majority of bladder cancer patients are white and male [3], and thus the expected demographics for spousal caregivers would be more likely white and female. Finally, the caregiver well-being and supportive care needs assessment reported in this study may not be generalizable to those who are not familiar with the online network and/or electronic survey given the online recruitment through the BCAN PSN. Patients and their caregivers with lower socioeconomic status, lower health literacy, or predominantly non-English speaking are underrepresented in our study. However, these people might be some of the most vulnerable and isolated populations and might not be familiar with the BCAN PSN.
Future studies should investigate patient- and caregiver-level determinants of emotional and physical burden longitudinally by examining patient and caregiver outcomes concurrently. Also, understanding the interplay between patient-level psychologic/physical health and caregiver well-being may shed light on how to improve QOL for both patients with bladder cancer and their caregivers. Additional gaps in evidence include the need to optimize supportive care resources for caregivers of patients with cancer. A systematic review of 19 articles on psychosocial interventions for cancer caregivers reported that a lack of detailed intervention descriptions limited conclusions on how resources affect caregiver QOL [30]. Thus, a randomized trial evaluating clearly defined interventions, such as providing bladder cancer caregivers with specific web-based materials, would be an important next step toward improving their well-being. In addition, future studies should be conducted in minority and underrepresented populations, including caregivers with lower SES, lower health literacy, and non-English speaking.
CONCLUSION
We identified characteristics of caregivers who have decreased well-being, including younger age, female gender, having college or higher education, and caring for a patient with advanced cancer. We also identified the resources that caregivers perceived as helpful. In particular, web-based information about bladder cancer and treatment options can be offered to caregivers, including older adults. Caregiver networks through BCAN and other online forums are also beneficial support for caregivers of patients with bladder cancer, particularly those with advanced disease.
ACKNOWLEDGMENTS
The authors thank the research participants of the Bladder Cancer Advocacy Network (BCAN) Patient Survey Network for participating in the online survey and for their important contributions that have made the study possible. The authors also thank the research patient advocates of the BCAN Caregiver Working Group who participated in the conception and design of the BCAN caregiver survey. Ahrang Jung was supported by the National Institutes of Health (NIH) National Institute of Nursing Research (NINR) under Award Number T32NR007091 and UNC Lineberger Comprehensive Cancer Center (LCCC) Cancer Outcomes Research Program. Lixin Song was partially supported by R01NR016990 NINR (PI: Song), R21 CA212516 National Cancer Institute (NCI) (PI: Song) and University Cancer Research Fund, UNC LCCC. Angela Smith was supported by a Patient Centered Outcomes Research Institute (PCORI) Engagement Award (PI: Smith).
FUNDING
This project was supported in part by a Patient-Centered Outcomes Research Institute (PCORI) Engagement Award (PI: Smith).
AUTHOR CONTRIBUTIONS
AJ: Conception, interpretation and analysis of data, writing the article; LS: Conception, interpretation of data, writing the article; ES: Conception, interpretation of data, writing the article; RL: Conception, performance of work, writing the article; KS: Conception, performance of work, writing the article; SC: Conception, performance of work, writing the article; JG: Conception, performance of work, writing the article; AS: Conception, performance of work, interpretation of data, writing the article.
ETHICAL CONSIDERATION
The data collected were de-identified, and thus, the Institutional Review Board (IRB) at the University of North Carolina at Chapel Hill has determined that the study does not require IRB approval.
CONFLICT OF INTEREST
Dr. Smith reports grants from PCORI, during the conduct of the study; grants from PCORI, other from Merck, other from Photocure, other from Fergene, other from Urogen, grants from BCAN, outside the submitted work. Dr. Gore reports grants from FerGene, Inc., outside the submitted work. Ms. Louwers reports personal fees from BladderCancer.net, outside the submitted work. The other authors declare that they have no conflict of interest.
SUPPLEMENTARY MATERIAL
[1] The list of caregiver survey questions for this study is provided as supplementary material.
The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/BLC-200412.
REFERENCES
[1] | Kent EE , Mollica MA , Buckenmaier S , Wilder Smith A . The characteristics of informal cancer caregivers in the united states. Seminars in Oncology Nursing. (2019) ;35: (4):328–332. doi:10.1016/j.soncn.2019.06.002 |
[2] | National Cancer Institute. (n.d.). Statistics - Office of Cancer Survivorship. Retrieved October 24, 2019, from https://cancercontrol.cancer.gov/ocs/statistics/statistics.html. |
[3] | Siegel RL , Miller KD , Jemal A . Cancer statistics, 2019. CA: A Cancer Journal for Clinicians. (2019) ;69: (1):7–34. doi:10.3322/caac.21551 |
[4] | American Cancer Society (Ed.). (2019). Cancer Treatment & Survivorship Facts & Figures 2019–2021. Atlanta: American Cancer Society. Retrieved from http://www.cancer.org/research/cancer-facts-statistics.html? |
[5] | Stenberg U , Ruland CM , Miaskowski C . Review of the literature on the effects of caring for a patient with cancer. Psycho-Oncology. (2010) ;19: (10):1013–25. doi:10.1002/pon.1670 |
[6] | Romito F , Goldzweig G , Cormio C , Hagedoorn M , Andersen BL . Informal caregiving for cancer patients. Cancer. (2013) ;119: Suppl 11:2160–9. doi:10.1002/cncr.28057 |
[7] | Kim Y , Schulz R . Family caregivers’ strains: comparative analysis of cancer caregiving with dementia, diabetes, and frail elderly caregiving. Journal of Aging and Health. (2008) ;20: (5):483–503. doi:10.1177/0898264308317533 |
[8] | Ochoa CY , Buchanan Lunsford N , Lee Smith J . Impact of informal cancer caregiving across the cancer experience: A systematic literature review of quality of life. Palliative & Supportive Care. (2020) ;18: (2):220–40. doi:10.1017/S1478951519000622 |
[9] | Tan JY , Molassiotis A , Lloyd-Williams M , Yorke J . Burden, emotional distress and quality of life among informal caregivers of lung cancer patients: An exploratory study. European Journal of Cancer Care. (2018) ;27: (1):doi: 10.1111/ecc.12691 |
[10] | Babjuk M , Oosterlinck W , Sylvester R , Kaasinen E , Böhle A , Palou-Redorta J . European Association of Urology (EAU). EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder. European Urology. . (2008) ;54: (2):303–14. doi:10.1016/j.eururo.2008.04.051 |
[11] | Chang SS , Bochner BH , Chou R , Dreicer R , Kamat AM , Lerner SP , ... Holzbeierlein JM . Treatment of Nonmetastatic Muscle-Invasive Bladder Cancer: American Urological Association/American Society of Clinical Oncology/American Society for Radiation Oncology/Society of Urologic Oncology Clinical Practice Guideline Summary. Journal of oncology practice / American Society of Clinical Oncology. (2017) ;13: (9):621–5. doi:10.1200/JOP.2017.024919 |
[12] | Alfred Witjes J , Lebret T , Compérat EM , Cowan NC , De Santis M , Bruins HM , ... Ribal MJ . Updated EAU Guidelines on Muscle-invasive and Metastatic Bladder Cancer. European Urology. (2017) ;71: (3):462–75. doi:10.1016/j.eururo.2016.06.020 |
[13] | Jung A , Nielsen ME , Crandell JL , Palmer MH , Bryant AL , Smith SK , Mayer DK . Quality of Life in Non-Muscle-Invasive Bladder Cancer Survivors: A Systematic Review. Cancer Nursing. (2019) ;42: (3):E21–E33. doi:10.1097/NCC.0000000000000606 |
[14] | Smith AB , Chisolm S , Deal A , Spangler A , Quale DZ , Bangs R , ... Gore JL . Patient-centered prioritization of bladder cancer research. Cancer. (2018) ;124: (15):3136–44. doi:10.1002/cncr.31530 |
[15] | Hamad J , Gore J , Chisolm S , Powell M , Lavallee DC , Lipman R , ... Smith A . Patient empowerment through engagement in bladder cancer research. Urologic Oncology. (2020). doi:10.1016/j.urolonc.2020.07.015 |
[16] | Macera CA , Eaker ED , Jannarone RJ , Davis DR , Stoskopf CH . A measure of perceived burden among caregivers. Evaluation & the Health Professions. (1993) ;16: (2):205–11. doi:10.1177/016327879301600205 |
[17] | Kaveney SC , Baumstarck K , Minaya-Flores P , Shannon T , Symes P , Loundou A , Auquier P . Validation of the American version of the CareGiver Oncology Quality of Life (CarGOQoL) questionnaire. Health and Quality of Life Outcomes. (2016) ;14: :82. doi:10.1186/s12955-016-0487-6 |
[18] | Bauer MR , Bright EE , MacDonald JJ , Cleary EH , Hines OJ , Stanton AL . Quality of life in patients with pancreatic cancer and their caregivers: A systematic review. Pancreas. (2018) ;47: (4):368–75. doi:10.1097/MPA.0000000000001025 |
[19] | Mellon S , Kershaw TS , Northouse LL , Freeman-Gibb L . A family-based model to predict fear of recurrence for cancer survivors and their caregivers. Psycho-Oncology. (2007) ;16: (3):214–23. doi:10.1002/pon.1074 |
[20] | Price MA , Butow PN , Costa DS , King MT , Aldridge LJ , Fardell JE , ... Australian Ovarian Cancer Study Group Quality of Life Study Investigators. Prevalence and predictors of anxiety and depression in women with invasive ovarian cancer and their caregivers. The Medical Journal of Australia. (2010) ;193: (S5):S52–57. doi:10.5694/j.1326-5377.2010.tb03929.x |
[21] | Sinoff G . Thanatophobia (death anxiety) in the elderly: the problem of the child’s inability to assess their own parent’s death anxiety state. Frontiers in Medicine. (2017) ;4: :11. doi:10.3389/fmed.2017.00011 |
[22] | Geng H-M , Chuang D-M , Yang F , Yang Y , Liu W-M , Liu L-H , Tian H-M . Prevalence and determinants of depression in caregivers of cancer patients: A systematic review and meta-analysis. Medicine. (2018) ;97: (39):e11863. doi:10.1097/MD.0000000000011863 |
[23] | Kehoe LA , Xu H , Duberstein P , Loh KP , Culakova E , Canin B , ... Mohile SG . Quality of Life of Caregivers of Older Patients with Advanced Cancer. Journal of the American Geriatrics Society. (2019) ;67: (5):969–77. doi:10.1111/jgs.15862 |
[24] | Segrin C , Badger T , Dorros SM , Meek P , Lopez AM . Interdependent anxiety and psychological distress in women with breast cancer and their partners. Psycho-Oncology. (2007) ;16: (7):634–43. doi:10.1002/pon.1111 |
[25] | Oberoi DV , White V , Jefford M , Giles GG , Bolton D , Davis I , ... Hill D . Caregivers’ information needs and their “experiences of care” during treatment are associated with elevated anxiety and depression: a cross-sectional study of the caregivers of renal cancer survivors. Supportive Care in Cancer. (2016) ;24: (10):4177–86. doi:10.1007/s00520-016-3245-8 |
[26] | Pew Research Center. (2014, April). Older Adults and Technology Use. Retrieved February 13, 2020, from https://www.pewresearch.org/internet/2014/04/03/older-adults-and-technology-use/. |
[27] | Lapid MI , Atherton PJ , Clark MM , Kung S , Sloan JA , Rummans TA . Cancer caregiver: perceived benefits of technology. Telemedicine Journal and E-Health.. (2015) ;21: (11):893–902. doi:10.1089/tmj.2014.0117 |
[28] | Litzelman K , Tesauro G , Ferrer R . Internal resources among informal caregivers: trajectories and associations with well-being. Quality of Life Research. (2017) ;26: (12):3239–50. doi:10.1007/s11136-017-1647-9 |
[29] | Kim Y , Carver CS , Shaffer KM , Gansler T , Cannady RS . Cancer caregiving predicts physical impairments: roles of earlier caregiving stress and being a spousal caregiver. Cancer. (2015) ;121: (2):302–10. doi:10.1002/cncr.29040 |
[30] | Treanor CJ , Santin O , Prue G , Coleman H , Cardwell CR , O’Halloran P , Donnelly M . Psychosocial interventions for informal caregivers of people living with cancer. Cochrane Database of Systematic Reviews. (2019) ;6: :CD009912. doi: 10.1002/14651858.CD009912.pub2 |




