Challenging Cases in Urothelial Cancer
Case 12
SK is a 64 year old healthy appearing man who is a former heavy cigarette smoker who presents with gross hematuria. Five years ago he had a left nephroureterectomy for a high grade Ta urothelial cancer in the left renal pelvis. He underwent regular bladder surveillance for two years but failed to continue monitoring until the recent episode of hematuria.
His past medical history is pertinent for aortic and mitral valve cardiac surgery 10 years ago. He had a metallic valve placed. He has been taking warfarin since.
He had a non-contrast CT scan because his serum creatinene is 1.45. The imaging study identified a 4 cm mass in the posterior portion of the bladder close to the dome. The rest of the exam was normal.
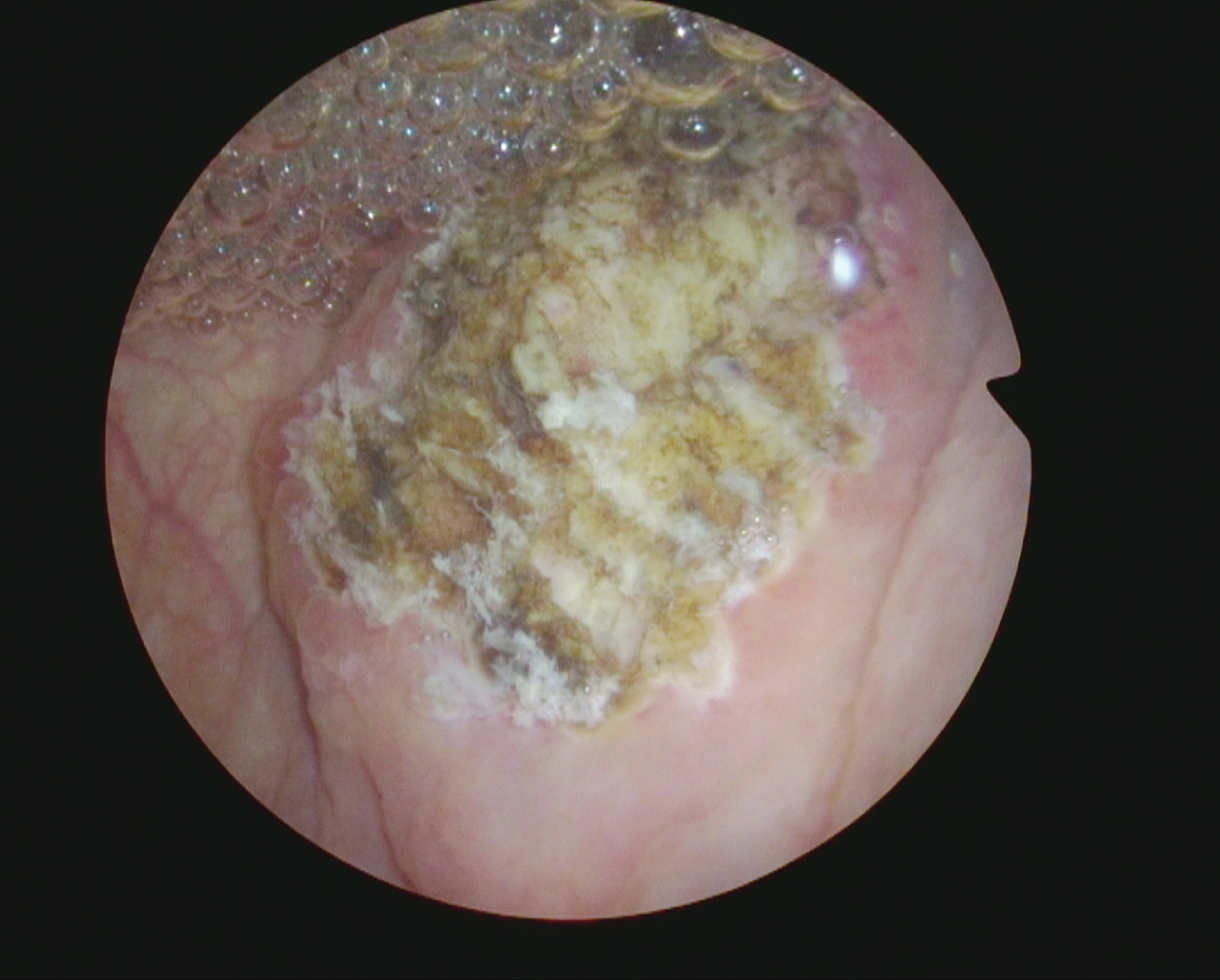
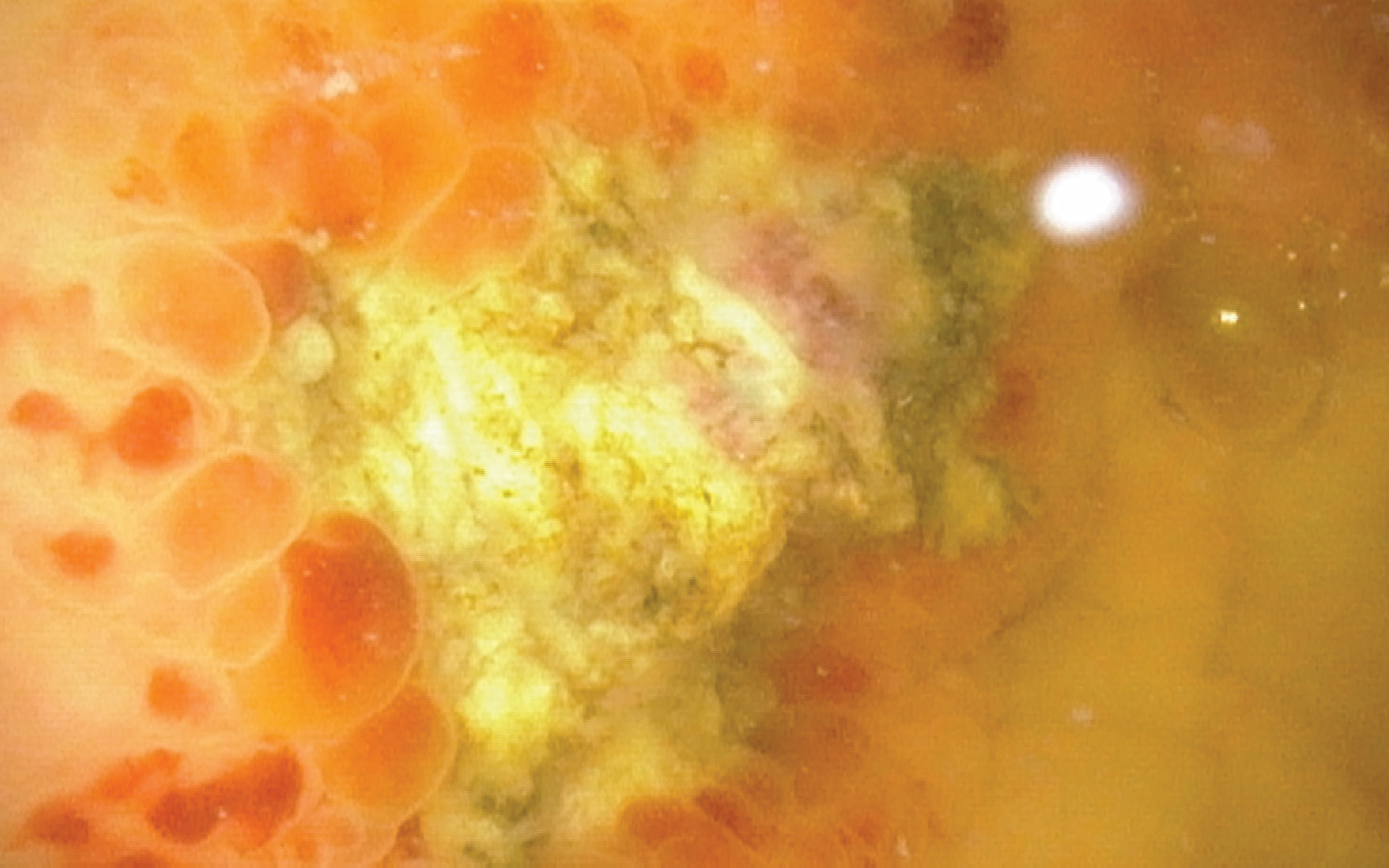
Outpatient flexible cystoscopy identified a solitary 5 cm papillary tumor located in the dome of the bladder (Fig. 1). There were no other suspicious areas in the urothelium. A transurethral resection of the tumor was performed (Figs. 2, 3). I felt that all of the tumor was resected (Fig. 4). My clinical impression was that this was a high grade Ta or T1 urothelial carcinoma. The pathology report, however, indicated that the tumor was high grade and invaded the muscularis propria, i.e. pT2.
Fig. 1
Large papillary tumor.

Fig. 2
Papillary tumor at TUR BT. Note use of angled loop for tumor posterior wall.
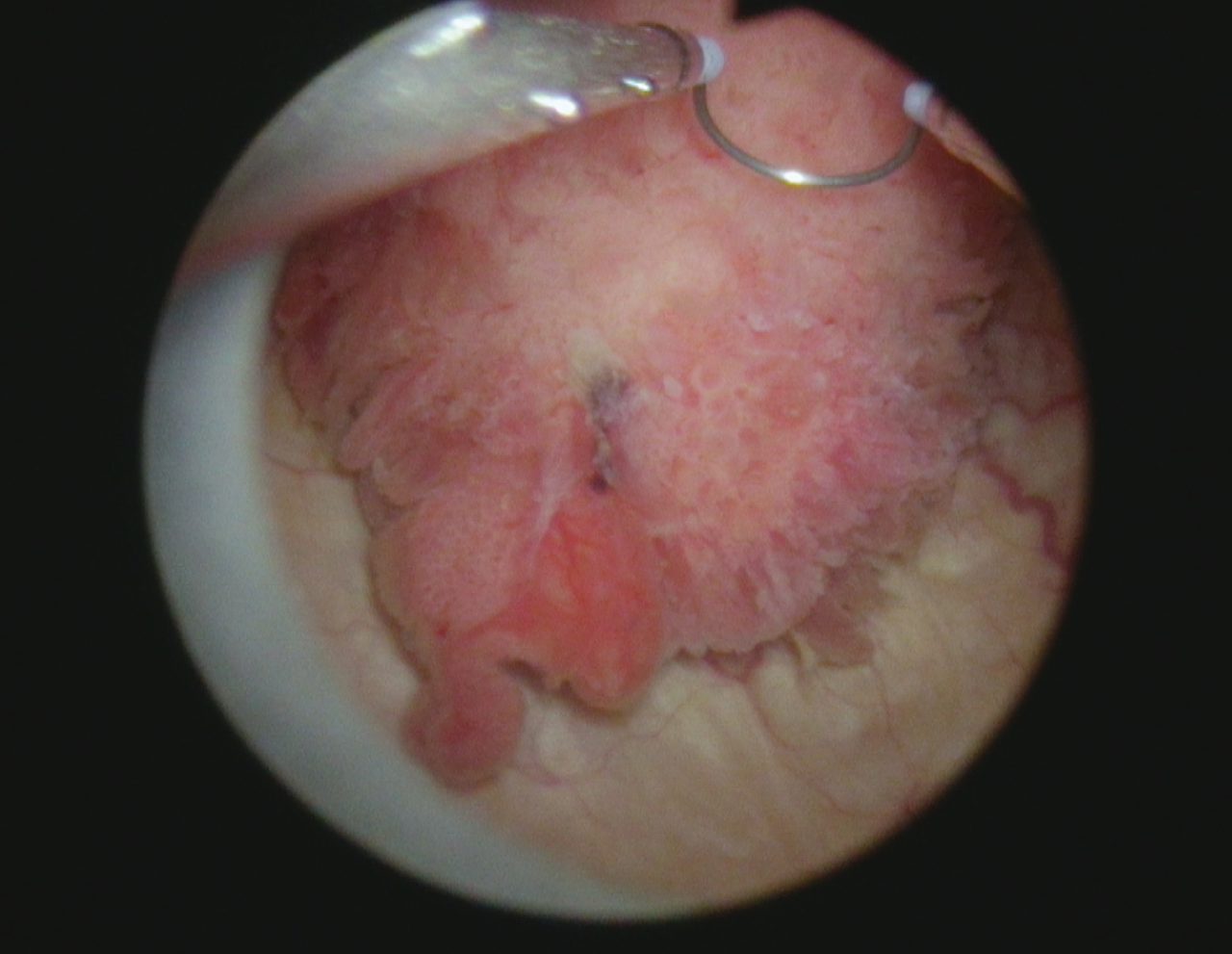
Fig. 3
Resection of tumor base.
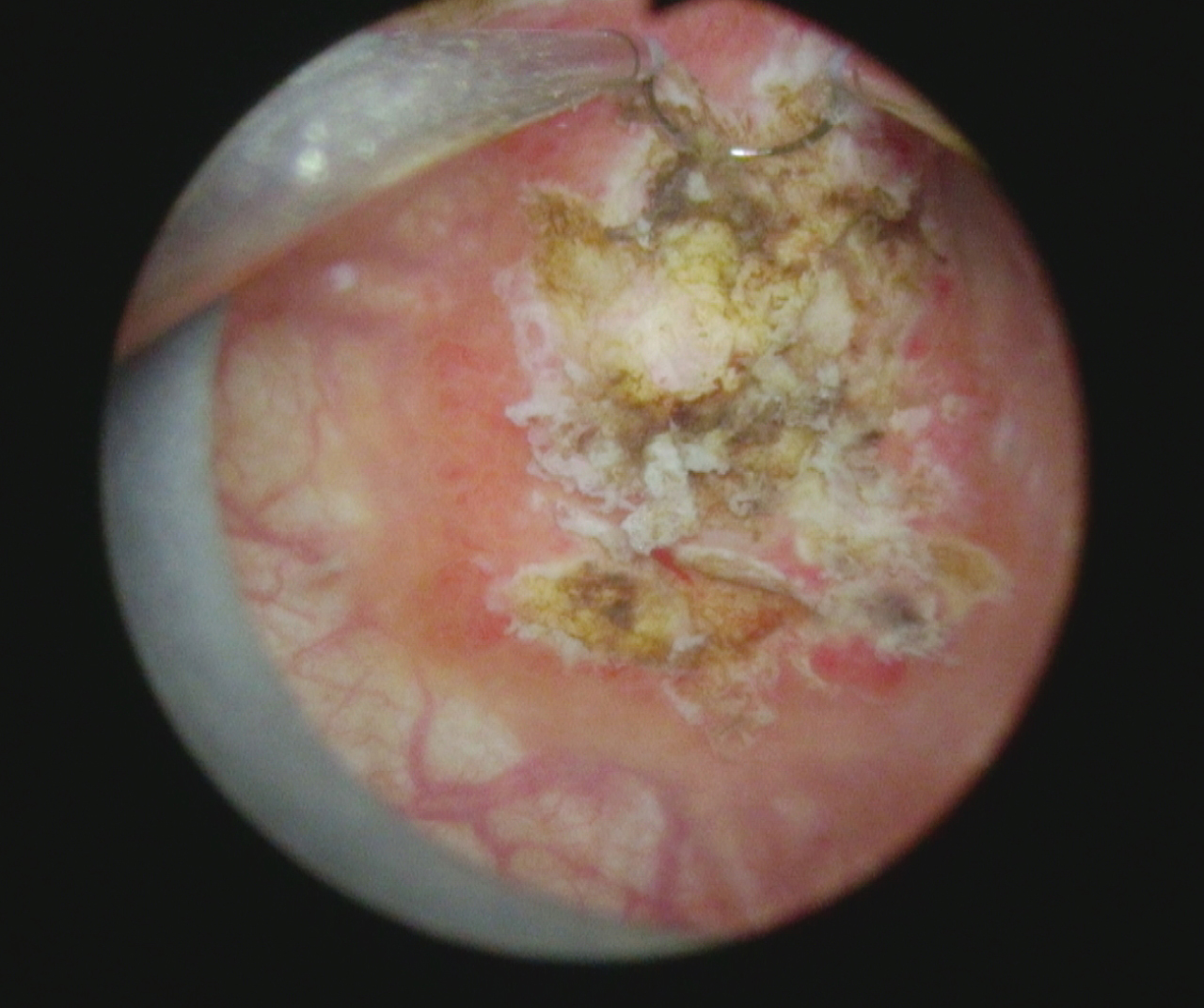
Fig. 4
Post TUR BT. Thought to be a “complete” resection.
There are several alternatives. One might consider a repeat TUR BT to determine whether there was indeed any remaining cancer. If this was negative one might give intravesical BCG or observe the patient but there would be some doubt as to the accuracy of ensuring there was no cancer remaining. A cystoprostatectomy with or without systemic chemotherapy is another option. His reduced renal function might limit the choices of chemotherapy. The patient meets the criteria for a partial cystectomy since this is his first bladder cancer, the tumor is limited to a region of the bladder, which would allow a wide margin, and the stage is cT2. There is also no carcinoma in situ.
I performed a flexible cystoscopy in the office two weeks after the TUR BT (Fig. 5) to ensure the location was indeed amenable to a partial cystectomy and to have a thorough discussion with the patient so he would understand that he is at risk of a new tumor in the bladder and eventually there was a possibility he eventually might need to have his bladder removed and thus have a urinary diversion.
Fig. 5
Cystoscopy 2 weeks post TUR BT. No obvious tumor. Location posterior bladder wall toward dome.
I performed a partial cystectomy. There was no cancer in the resected bladder tissue. The pelvic lymph node dissection not surprisingly was negative as well.
Because of the metallic valve the patient required a heparin drip postoperatively. On the second postop day his lower abdomen was noted to be markedly distended and the indwelling catheter had minimal urine output. His hemoglobin had declined although his blood pressure was stable. I elected to take the patient to the operating room and performed a cystoscopy under anesthesia as my concern was that he had clot retention. There was no blood in the bladder and the suture line was intact. One of the trauma surgeons was available at 5 am when this was taking place and we explored the pelvis and evacuated a large fresh hematoma. No active bleeding site was found. Hemostatic sealant was used and drains were placed. He recovered uneventfully. His is voiding normally.
Any comments on his management would be appreciated.
We invite our readers to review and comment on the case and management by using the online comment section below the case: https://www.bladdercancerjournal.com/challenging-cases
FUNDING
The authors report no funding.
CONFLICTS OF INTEREST
Nothing to disclose.
ACKNOWLEDGMENTS
The authors have no acknowledgments.




