9th UK Swallow Research Group Conference: Oral Presentations Abstracts
Swallowing outcomes in hospitalised COVID-19 patients
Dr Sally Archer1, Ms Louisa Gilpin1
1Speech and Language Therapy, Guy’s and St Thomas’ NHS Foundation Trust, London, United Kingdom
BACKGROUND: Patients with severe COVID-19 frequently require prolonged intubation and respiratory support and there are associated neurological sequelae, presenting risks for dysphagia. This study observed dysphagia outcomes from COVID-19 inpatients to inform service delivery.
METHODS: Observational study of all inpatients referred to Speech and Language Therapy (SLT) for two-months from April’20. Data on delirium, neurology, intubation and tracheostomy history were collected, with type of SLT provided. Dysphagia Therapy Outcome Measures and Functional Oral Intake Scale pre/post SLT were compared with Wilcoxon Signed Ranks test. QIP Reference10928; ethical approval not required.
RESULTS: 164 patients (104M), age 56.8±16.7y were included. Half (52.4%) had a tracheostomy:Median (IQR) time to decannulation 19 days(16-27); 78.7% had been intubated (mean 15±6.6days), 13.4% had new neurological impairment and 69.5% delirium. Individualised compensatory swallowing strategies were trialled in all and direct exercises with 11%. Dysphagia was typically severe with significant improvement at inpatient discharge (p<0.0001). Some oral intake was started at median 2 days post-initial assessment (IQR 0-8) but 29.3%(n=29) remained impaired at hospital discharge. 10 (34%) with persistent dysphagia had previous neurological diagnosis, versus 10.3% (n=7) who resolved. Patients were under inpatient SLT median(IQR) 11 days (6-20); 37.3% completed SLT while inpatients, 23.5% transferred to another hospital and 7.8% required community dysphagia follow-up.
CONCLUSIONS: Significant dysphagia was identified in a cohort of COVID-19 inpatients, where prolonged intubations and tracheostomies were frequent. Patients typically improved with individualised strategies but post-discharge follow-up was required for a minority. Inpatient services for COVID-19 should target resources for responsive tracheostomy and dysphagia management.
Are bubbles the future of dysphagia rehabilitation: A systematic review analysing evidence on the use of carbonated liquids in dysphagia rehabilitation
Dr Grace Isbister1, Dr Kathyrn Price, Dr Susannah Long, Professor David Smithard
1Lewisham and Greenwich NHS Trust, London, United Kingdom, 2UK Swallow Research Group Conference, London, United Kingdom
INTRODUCTION: Dysphagia poses a huge global health issue in our ageing population, impacting patients through risk of aspiration pneumonia, malnutrition, airway obstruction and death but also huge psychological sequalae. The use of carbonated liquids (CL) for sensory enhancement in dysphagia rehabilitation, remains an area with limited research.
This systematic review analyses the current evidence in this area, attempting to draw conclusions for potential future use in clinical practice.
METHODS: A data search of PubMed, CINAHL, EMBASE and Cochrane was undertaken by a trained professional in these databases. 5 papers were analysed and their quality was assessed using the PRISMA standards.
RESULTS: Selected publications (1992-2019) differed significantly in study design but all used videofluroscopy swallowing study (VFSS) to assess various outcome measures; these included pharyngeal transit time (PTT), pharyngeal retention (PR) and evidence of penetration/ aspiration. All studies showed encouraging results, with CL significantly reducing penetration/ aspiration and varied outcomes on PR and PTT.
CONCLUSIONS: There continues to be limited evidence to direct the use of CL in dysphagia rehabilitation. The heterogeneity of study designs specifically participants seems to be the main barrier towards this. Whilst evidence is encouraging, further prospective studies standardising patient cohorts, methodologies and quantitative outcome measures must be carried out. Longitudinal studies to examine the role of CL in rehabilitation potential and improvement of dysphagia over time is another area of interest. In conclusion CL in dysphagia rehabilitation has a potential role but without firm evidence based research, successful use in clinical practice cannot be implemented.
Hard to swallow? A review of the quality of dysphagia care provided to patients with Parkinson’s disease admitted to hospital when acutely unwell
Mrs Heather Freeth1, Miss D’Marieanne Koomson1, Dr Alex Goodwin1,2, Dr Vivek Srivastava1,3
1NCEPOD, London, United Kingdom, 2Royal United Hospitals Bath NHS Foundation Trust, Bath, United Kingdom, 3Guy’s and St Thomas’ NHS Foundation Trust, London, United Kingdom
AIM: The aim of this study was to explore multidisciplinary care and organisational factors in the process of identifying, screening, assessing, treating and monitoring the ability to swallow in patients with Parkinson’s disease (PD) admitted to hospital.
METHODS: All UK hospitals were asked to report the details of patients with PD admitted over eight weeks. From this up to four patients per hospital were sampled for detailed review. The clinician caring for the patient at the time of admission completed a questionnaire and returned this alongside copied extracts of the case notes. These data were peer reviewed by a multidisciplinary group of clinicians to assess the quality of dysphagia care. Organisational data and the views of service users were also collected. Section 251 approval was granted to enable patient identifiable information to be collected without consent.
RESULTS: 505 clinician questionnaires and 177 organisational questionnaires were analysed; and 344 sets of anonymised case notes were peer reviewed; this included 126 patients with dysphagia. Several areas of concern were highlighted broadly in line with expectations for this group of patients, relating to issues with the documentation of swallowing status; the screening of patients for dysphagia at admission; the referral of patients to speech and language therapy; and the provision of information at discharge.
CONCLUSION: The report, which makes eleven recommendations for clinicians and management to implement in practice, highlights there is room for improvement in the quality of dysphagia care
Identifying dysphagia and demographic associations in older adults using electronic health records: A national longitudinal observational study in Wales (United Kingdom) 2008-2018
Professor David Smithard1,2, Dr Joe Hollinghurst3
1Queen Elizabeth Hospital, Stadium Road, Woolwich, United Kingdom, 2University Of Greenwich, Eltham, United Kingdom, 3University of Swansea, Swansea, United Kingdom
BACKGROUND: Dysphagia is increasingly being recognised as a geriatric giant. There is little research on the coding of dysphagia in electronic health records (EHR).
AIM: To investigate the prevalence of dysphagia recorded in EHR and associations with age, frailty, gender and deprivation.
STUDY DESIGN AND SETTING: Cross-sectional longitudinal cohort study for over 400,000 older adults (65+) in Wales (United Kingdom) per year from 2008 to 2018.
METHODS: We used the Secure Anonymised Information Linkage databank to identify dysphagia diagnoses in primary and secondary care. We used chi-squared tests and multivariate logistic regression to investigate associations between a dysphagia diagnosis and age, frailty (using the electronic Frailty Index), gender and deprivation.
RESULTS: Data indicated <1% of individuals were recorded with a dysphagia diagnosis per year. We found dysphagia to be statistically significantly (p<0.05) associated with older age, more severe frailty and more deprived areas. Multivariate analyses indicated increased Odds Ratios (OR [95% confidence intervals]) for a dysphagia diagnosis for increased age (reference 65-74: aged 75-84 OR 1.09 [1.07,1.12], 85+ OR 1.23 [1.20,1.27]), frailty (reference fit: mild frailty 2.45 [2.38,2.53], moderate frailty 4.64 [4.49,4.79] and severe frailty 7.87 [7.55,8.21]), and reduced ORs for less deprived areas (reference 1. most deprived, 2: 0.92 [0.89,0.95], 3: 0.89 [0.86,0.92], 4: 0.87 [0.84,0.90], 5. least deprived: 0.91 [0.88,0.94]).
CONCLUSIONS: The prevalence of dysphagia documented is less than that in previous studies suggesting a significant under reporting/ recording. As the older population increases, this may manifest as a major public health concern.
Nasogastric tube and oral care practice in acute stroke: A national survey linked to stroke registry data
Mrs Sabrina Eltringham2, Dr Ben Bray, Professor Craig Smith, Professor Sue Pownall, Professor Karen Sage
1Sheffield Teaching Hospitals Nhs Foundation Trust, Sheffield, United Kingdom, 2Manchester Metropolitan University, Manchester, United Kingdom
INTRODUCTION: Stroke-associated pneumonia (SAP) is common post stroke (Kishore et al.). A range of medical interventions and care processes are associated with risk of SAP in patients with dysphagia (Eltringham et al.). Our study purpose was to reveal variations in nasogastric tube (NGT) and oral care practices in acute stroke and explore their association with SAP.
METHODS: NHS ethical approval was obtained. Speech Therapists from 166 stroke units in England and Wales were surveyed about NGT insertion and oral care in acute stroke. Survey data were then linked to the Sentinel Stroke National Audit Programme (SSNAP). Linear regression analysis estimated the association between NGT insertion and oral care and SAP incidence.
RESULTS: Survey completion rate was 68% (N=113). Less than two thirds had a written oral protocol and approximately 90% had a written NGT protocol. There was variation in oral care and NGT processes. Multivariable analysis showed no evidence of association in incidence of SAP when teams inserted NGTs overnight compared to teams which did not (B –.505, 95% CI –2.759-1.749) and when teams had a written oral care protocol compared to those which did not (B –1.339, 95% CI –3.551 - .873).
CONCLUSIONS: There is variation in practice however our study found no evidence of an association in incidence of SAP. A larger sample at both registry and survey level might show associations which this national sample was unable to detect. Empirical studies investigating oral care interventions in stroke patients with dysphagia are needed to inform clinical guidelines.
Leaving hospital and surviving following a decision to eat and drink with acknowledged risk: Are we sustaining best practice on readmission?
Mrs Naomi Soar1, Dr Sally Archer
1Guy’s & St Thomas’ NHS Foundation Trust, London, United Kingdom
INTRODUCTION: Patients with dysphagia eating and drinking with acknowledged risk (EDAR) are supported by the FORWARD care bundle (Feeding via the Oral Route With Acknowledged Risk of Deterioration) at our Trust. Aims include reducing time nil-by-mouth (NBM) and improving discussions with patients. However the pathway following hospital discharge is not known. This study sought to identify if the bundle’s improvements are maintained on subsequent readmissions.
METHODS: Retrospective review of patients supported by FORWARD from January 2018 to December 2019. Data were collected on mortality and readmissions 6-months post-discharge, nutritional status after 24-hours of readmission and documentation of patient EDAR discussions within 7 days of readmission. Study registration is with our Trust Clinical Governance. Ethical approval was not required.
RESULTS: 316 patients were included. 63% (n=200) were discharged alive and 36% (n=114) were alive at 6-months. 37% (n=74) of live discharges were readmitted over 117 readmissions. 24-hours after readmission, 69% (n=81) were following existing diet/fluid recommendations. 14% (n=16) were NBM with artificial nutrition or awaiting swallow assessment. 9% (n=10) had new recommendations and 9% (n=10) were eating/drinking without following specific recommendations. No patients were NBM without nutrition plans. EDAR discussions occurred within 7 days in 32% (n=37) of readmissions.
CONCLUSIONS: Most patients supported by FORWARD left hospital alive. A third were alive at 6 months and readmissions were common, suggesting a need for ongoing review and support. Few were NBM on readmission and EDAR recommendations were frequently followed. Further work includes ensuring timely EDAR discussions after readmission to continue patient-centred care.
What is the baseline swallowing function of adults with laryngotracheal stenosis due to undergo reconstructive surgery?
Ms Gemma Clunie1,2, Dr Justin Roe1,2, Dr Caroline Alexander1,2, Mr Guri Sandhu1,2, Professor Alison McGregor2
1Imperial College Healthcare NHS Trust, London, United Kingdom, 2Imperial College London, London, United Kingdom
BACKGROUND AND PURPOSE: Adults diagnosed with laryngotracheal stenosis (LTS), undergo airway reconstruction surgery to improve their breathing. This surgery impacts swallowing (Haywood et al., Holman et al., 2018, Lennon et al., 2016), but most studies are retrospective and lack patient-reported outcomes. We conducted a prospective study of swallowing outcomes in adults with LTS prior to and post-reconstructive surgery to explore swallowing function in more detail.
METHODS: Following ethical approval and informed consent, we recruited patients with LTS undergoing airway reconstruction surgery at the National Airway Reconstruction Centre to an observational study. We collected patient-reported (PROMS), clinician-reported, and instrumental outcome measures pre- surgery, 2 weeks, and 4-6 months post-surgery. Descriptive statistics and non-parametric statistical tests were used to analyse data.
RESULTS: Twenty-two consecutive participants (11:11 male: female) have been recruited to date with research ongoing. Baseline assessments are as follow: Median and interquartile range (IQR) of PROMS: Dysphagia Handicap Index (DHI) 16 (0-36.50), EAT-10 2.5 (0-16); clinician reported: FOIS 7 (6-7); instrumental assessment: PAS 1 (1-3), 100 ml water swallow speed 1.01 (1-1.6).
CONCLUSIONS: We have defined the swallowing profile of adults with LTS prior to reconstructive surgery. Baseline outcomes demonstrate the multifactorial nature of swallowing function but also demonstrate that in the context of qualitative data on patient’s experiences of swallowing (Clunie et al., 2021) there is a disparity between clinician report and patient reported assessment of dysphagia. Further results from this study will lead individualised patient pathways and better information provision prior to surgery.
Expiratory muscle strength training (EMST) for dysphagia in primary and recurrent head and neck cancer (HNC): A case series
Mrs Grainne Brady1,2, Mrs Kate Ashforth1, Ms Jocelyn Brazier1, Mrs Lauren Leigh-Doyle1, Dr Justin Roe1,2,3
1The Royal Marsden NHS Foundation Trust, London, United Kingdom, 2Department of Surgery and Cancer, Imperial College London, London, United Kingdom, 3Imperial College Healthcare Trust, London, United Kingdom
BACKGROUND: EMST is a device-driven exercise therapy with an emerging evidence base for the treatment of dysphagia in HNC.
METHODS: Performance Status Scale for Head and Neck Cancer (PSS-HN), Normalcy of Diet (NOD) and Eating in Public (EIP) scores, Penetration Aspiration Scale (PAS) and Dynamic Imaging Grade for Swallowing Toxicity (DIGEST) were retrospectively reviewed in HNC patients who underwent EMST.
Project approval: Service Evaluation Committee, Royal Marsden NHS Foundation Trust (SE752).
RESULTS: EMST was completed in 17 patients (primary disease (n=8), recurrent disease n=9)). Disease sites included the oropharynx (n=12), larynx (n=1), hypopharynx (n=1), oral cavity (n=1) and unknown primary (n=1). Primary disease treatments included transoral robotic surgery (TORS) (n=1), TORS with post-operative chemoradiation (n=1), radiation (n=1) and chemoradiation (n=5). Late effects were noted in the majority of primary disease patients (n=5). All recurrent disease patients had previous radiation +/- surgery. Treatments for recurrence included open surgery (n=5), TORS (n=2), re-irradiation (n=1) and immunotherapy (n=1). Baseline mean PSS-NOD improved from 27.5 (95% CI: 18.4 to 36.9) to 37 post treatment (95% CI: 26.8 to 47.4) (n=17). PSS-EIP of 25 or below was noted 53% (n=10) at baseline which reduced to 23% (n=4) post treatment (n=17). Baseline PAS score of 8 was noted for 77% (n=10), which reduced to 47% (n=6) post treatment (n=13). Baseline DIGEST summary score of 4 was noted in 36% (n=4), this reduced to 27% (n=4) post-treatment (n=13).
CONCLUSION: EMST may have contributed towards positive functional outcomes for our small cohort of patients. Further research is required.
Feasibility of integrating videofluoroscopy in multi-centre head and neck cancer trials in the United Kingdom
Professor Jo Patterson1, Ms Laura-Jayne Watson, Professor M Evans, Professor Terry Jones, Professor Cristian Simon, Dr Max Beesley, Dr Nachi Palaniappan, Professor Chris Hurt, Professor Ned Powell, Dr Max Robinson, Ms Chris Heiberg, Ms J Canham, Dr Lisette Nixon, Ms C Frayne, Hayley Timmins, C Cox, Professor Kate Hutcheson
1University Of Liverpool, Thompson Yates Building, The Quadrangle, Brownlow Hill, United Kingdom
AIM: This study evaluates the feasibility of videofluoroscopy (VF) in a large UK multi-centre study.
METHODS: PATHOS is a trial investigating de-intensification of post-surgical adjuvant treatment for HPV-positive Oropharyngeal Squamous Cell Carcinoma(OPSCC). A pre-trial feasibility questionnaire was sent to potential centres to investigate the range of VF practices. Evidence-based VF standards and an analysis plan was devised in consultation with international experts. VFs were limited to three pre- and post-treatment time points to minimise radiation exposure. Blinded central review of VFs by SLTs was planned, using three validated measures: MBS Impairment Scale(MBSImP™©); Dynamic Imaging Grade of Swallowing Toxicity(DIGEST); and Penetration-aspiration Scale(PAS). An interim analysis was conducted for quality assurance purposes on a sample of 40 VFs.
RESULTS: 28/31 recruiting centres submitted VFs. To date, 592 VFs have been submitted for central review, representing a completion rate of 51% pre-surgery, 72% pre-radiotherapy and 70% at 12 months. Reasons for non-submission were insufficient time and capacity. All VFs were evaluable on all measures. Recording quality was high, with only minor deviations to protocol. 99.5% of bolus trials were completed. 80% had functional swallows (DIGEST grade 0-1) with an excellent safety profile. Two patients had penetration, not ejected. Mean MBSImP™© scores for oral impairment were 4.9; SD 3.5; 95% CI 3.9-6.3; pharyngeal impairment 7.6; SD 2.9; 95% CI 7.4-9.4.
CONCLUSION: VF is feasible in large multi-centre UK trials. Preliminary results indicate favourable swallowing profiles for patients at 12 months following transoral surgery and adjuvant treatment for HPV-positive OPSCC
The school dinner hall environment: A qualitative observational study of five UK mainstream primary schools
Ms Sally Morgan1, Ms Sumayya Ali, Ms Charlotte Barnett, Ms Natasha Brown, Ms Paige Cooney, Ms Hannah Ford, Ms Ayala Lebrett, Ms Sophie Ogilvie, Ms Ngozi Sweeney, Professor Celia Harding
1City, University of London, Division of Language & Communication Sciences, London, United Kingdom
STUDY PURPOSE: Adapting the environment is a management option for children with dysphagia. There is little research investigating school dinner halls and limited formal guidance despite these being a space where eating, drinking and mealtime skill development could be targeted.
METHODS: This ethically approved observational study examined five UK mainstream primary school dinner halls and took place prior to the Covid19 pandemic. Eleven lunchtime observational visits were made by one researcher. The researcher recorded sound pressure levels alongside general observations of the physical and social environment, guided by some published frameworks. The observations were then analysed through both descriptive statistics and qualitative methodologies, by several research project students.
RESULTS: All schools had recorded sound levels that breached UK and/or WHO guidelines. Some positive approaches to support the acoustic environment were noted, with others identified for further improvement, for example blinds on windows, water-filled bucket for cutlery disposal. Positive and negative physical and social environmental factors were evident within and between schools; for example, use of visuals to support choice making, dining furniture configuration and sizes, time allowance, non-verbal and verbal communication from school staff, adult mealtime role models.
CONCLUSIONS: School dinner halls were not found to be environments conducive to positive to social eating, drinking and mealtime skill development. This study highlights the need for further investigation of these spaces and exploration of approaches to improve these environments for all children, including those with eating and drinking difficulties.
The feasibility of 3D food printers for people with dysphagia and their supporters: Views of key stakeholders on an immersive experience of 3D food printing
Prof Bronwyn Hemsley1,2, Prof Susan Balandin1,3, Ms Fiona Given1, Ms Courtney Reddacliff1, Dr Tuck Wah Leong1, Dr Valerie Gay1, Dr Stephen Dann4
1The University of Technology Sydney, Building 20 Broadway, Ultimo, Australia, 2The University of Newcastle, Newcastle, Australia, 3Deakin University, Melbourne, Australia, 4Australian National University, Canberra, Australia
The aim of this ethically approved inter-disciplinary research was to identify the views of key stakeholders across disciplines in dysphagia management, including an adult with dysphagia, on the use of 3D food printers by people with dysphagia and their supporters. In total, 16 participants took part in an ‘immersion’ experience in either using the 3D food printer directly (n=13), or in directing its use over Zoom online (due to COVID-19 distancing) (n=3). Following the immersion, participants took part in focus groups to discuss their experiences and potential barriers or facilitators to the use of 3D food printers in dysphagia management. Overall, users identified several design issues impacting their experiences of using the 3D food printer. Filling capsules with the pureed food was commonly seen as difficult and messy, with increased cost of time and effort in preparing food and cleaning machine parts. While reporting the experience was engaging and enjoyable, participants’ expectations were not met in terms of (a) the usability of the device and its responsiveness (e.g., in the response to the touch screen, in guiding users through steps or error responses to fix printing difficulties), and (b) the attractiveness of the foods printed. However, they saw opportunities in creating novel food shapes and increasing participation and choice for people with dysphagia. User-centred co-design of 3D food printers and the inclusion of people with dysphagia, carers, speech language therapists, and occupational therapists in engineering design teams is important. The implications of 3D food printing across the disciplines are discussed.

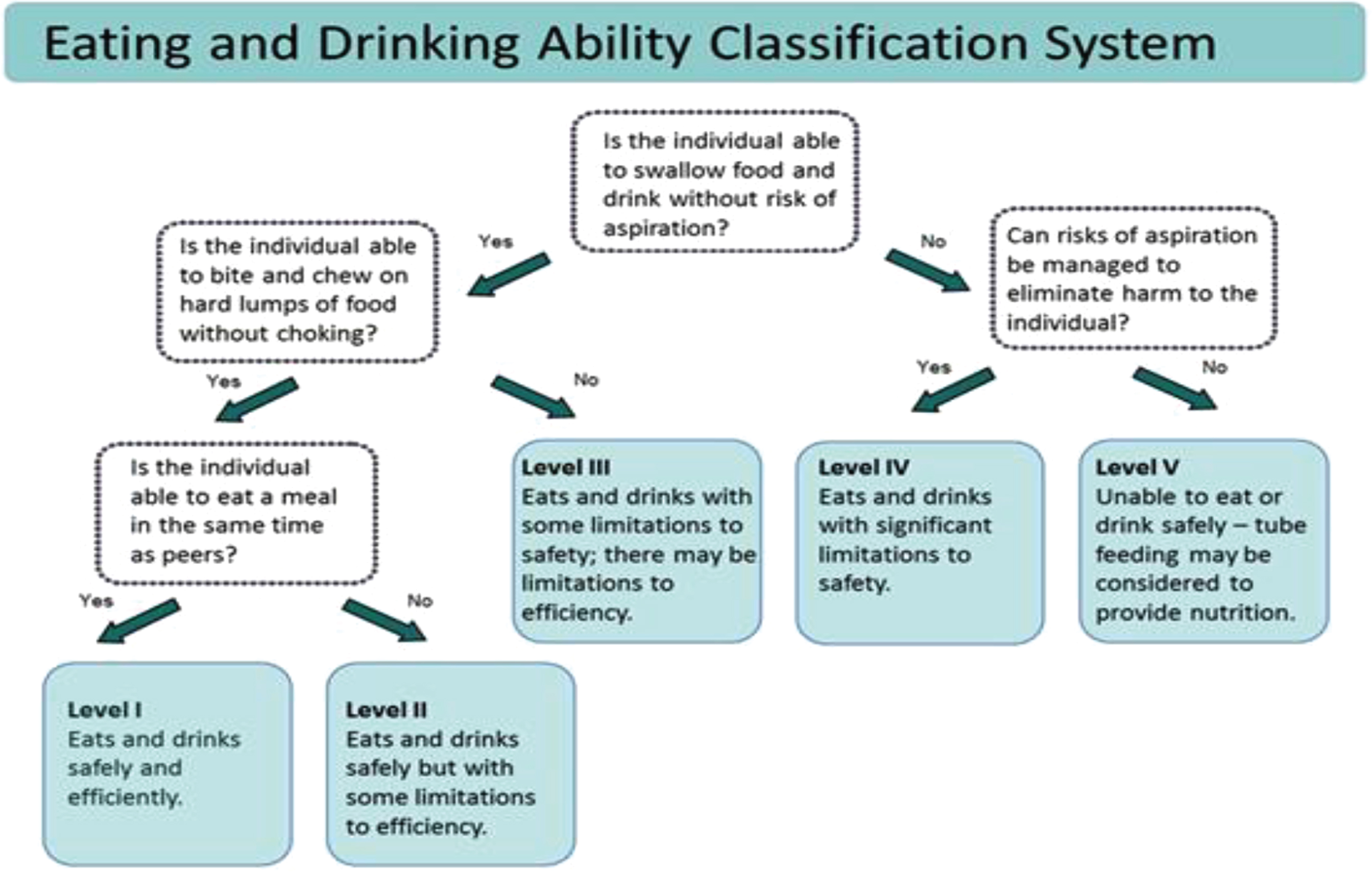
Mini-EDACS: Development of the eating and drinking ability classification system for young children with cerebral palsy
Dr Diane Sellers1, Dr Lindsay Pennington2, Dr Elizabeth Bryant3, Dr Kath Benfer4, Dr Kelly Weir5, Professor Christopher Morris6
1Chailey Clinical Services, Nr Lewes, United Kingdom, 2Institute of Health and Society, Newcastle University, Newcastle, United Kingdom, 3School of Health Sciences, University of Brighton, Brighton, United Kingdom, 4Queensland Cerebral Palsy and Rehabilitation Research Centre, Child Health Research Centre, Faculty of Medicine, University of Queensland, Brisbane, Australia, 5School of SHS - Allied Health Science, Griffith University, Southport, Australia, 6PENCRU, University of Exeter, Exeter, United Kingdom
AIM: Eating and Drinking Ability Classification System (EDACS) was developed to classify function of people with cerebral palsy (CP) in 5 levels from 3 years. This study aimed to develop and test Mini-EDACS, describing developing eating and drinking abilities of children with CP between 18-36 months.
METHODS: Mini-EDACS was developed in 3 stages: i)EDACS was applied to existing longitudinal videoed standardised feeding evaluations of children with CP aged 18-36 months (n=130) and content was modified to describe distinct levels of ability and mealtime performance for younger children with CP; ii)content was refined and validity of Mini-EDACS was established through an international Delphi survey; iii)inter-observer reliability was assessed by comparing Mini-EDACS levels assigned by expert speech and language therapists (SaLTs) from video data and parent report. Ethics approval was granted by NHS Health Research Authority, London–South East Research Ethics Committee: 17/LO/1557.
RESULTS: Mini-EDACS contains age-appropriate descriptions of eating and drinking ability for children 18-36 months with CP, including suitable drinking methods, and descriptions indicating learning of biting, chewing, swallowing, and drinking skills. 89 stakeholders including parents, health professionals, and care staff participated in the Delphi survey; agreed levels of content validity were achieved after 1 round of Delphi Survey. 13 experienced SaLTs completed paired ratings from 43 video recordings: absolute agreement was 58%; ICC: 0.78 (95% CI 0.63-0.87); Kappa: 0.43.
CONCLUSION: Mini-EDACS provides a valid classification system of eating and drinking performance of young children with CP. Reliability data suggests moderate to good agreement when rating Mini-EDACS levels from video recordings.