Cough effectiveness during airway invasion in adults with oropharyngeal dysphagia: A systematic review of literature
Abstract
BACKGROUND:
Cough and swallowing share common neuroanatomic pathways, leading to an overlap between their mechanisms. Despite the widely recognised role of cough as an airway defence mechanism, empirical evidence supporting its effectiveness for airway clearance is lacking.
OBJECTIVE:
This review summarises and appraises available evidence regarding the effectiveness of cough in response to airway penetration and/or aspiration during videofluoroscopic swallow study (VFSS) or flexible endoscopic evaluation of swallowing (FEES) in adults with oropharyngeal dysphagia (OD) of any aetiology.
METHODS:
The Preferred Reporting Items for Systematic Review and Meta-Analysis guidelines were followed. Literature search was conducted in March 2023 and updated in March 2024 across six databases without publication status, language, or date restrictions. Two independent reviewers performed screening, with disagreements resolved through consensus and majority vote. The principal investigator conducted data extraction and quality appraisal using the Downs and Black checklist.
RESULTS:
Of 6,049 studies retrieved, 25 met the eligibility criteria. Due to heterogeneous reporting, a summary of participant demographics could not be compiled. Absence of a standardised method for measuring cough effectiveness meant meta-analysis was impossible. Nonetheless, an effective cough response to penetration/aspiration was noted for some participants within 17 studies, ineffective cough responses for some within 17 studies, while one study reported a partially effective cough response for participants.
CONCLUSIONS:
Robust evidence on cough effectiveness is lacking due to study heterogeneity and inconsistent reporting. Developing a standardised tool to assess cough effectiveness would ensure consistency and comparability across studies, improving clinical reporting of VFSS and FEES outcomes.
1Introduction
Deficits of airway protection mechanisms can have a significant impact on an individual’s well-being and quality of life. This heightened vulnerability increases the risk of aspiration or ingestion of foreign material into the airway, potentially leading to aspiration pneumonia (AP) (Baijens et al., 2016).
Troche and colleagues (2014) presented a framework to enhance our understanding of airway protection mechanisms. In this framework, swallowing serves as a preventive mechanism, by stopping the entry of the foreign material into the airway, while coughing acts as a corrective mechanism, by expelling foreign material during airway invasion.
Given overlap between neural pathways and structures involved in cough and swallowing, literature reports of the co-occurrence of dystussia (cough dysfunction) and dysphagia across a wide range of patient populations is unsurprising (Hegland et al., 2014; Hutcheson et al., 2018). This evidence collectively validates the rationale for a widely incorporated use of cough into the clinical management of dysphagia. Despite this, there is lack of empirical evidence to support its role for airway clearance (Wallace et al., 2021).
1.1Research aims and questions
The aim of the present review is twofold:
1. The primary aim is to systemically identify, appraise, and synthesise the available evidence pertaining to the effectiveness of cough in response to penetration and/or aspiration for airway clearance during videofluoroscopic swallow study (VFSS) or flexible endoscopic evaluation of swallowing (FEES) in individuals with oropharyngeal dysphagia (OD) of any aetiology.
2. The secondary aim is to examine the impact of several variables on the cough responsiveness during airway invasion. These variables include cough type, timing and frequency, depth of airway invasion, objective measures of cough, and trial characteristics. This analysis considered the clinical diagnosis and severity of the disease, as well as the comparison between VFSS and FEES.
The primary research question addressed in the review is as follows:
How effective is cough in response to penetration and/or aspiration for airway clearance in adults with OD during VFSS or FEES?
It was hypothesised that effectiveness of cough for airway clearance during penetration and/or aspiration in adults with OD is multifactorial and dependent upon variables such as cough type and frequency.
2Methods
This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al., 2021). The study protocol was registered in PROSPERO, a global database designed to preclude accidental duplication of systematic reviews in the fields of health and social care (Higgins et al., 2019), registration number CRD42023408398.
2.1Eligibility criteria
The eligibility criteria were established using the PICO format (University of Canberra, 2018), defining key components of the review (Table 1). The review focused on adults due to recognised physiological and anatomical differences between adult and pediatric populations (Matsuo & Palmer, 2008). It aimed to assess the universal applicability of cough across various patient populations, considering factors like disease type and severity that could influence cough responsiveness. Pilot search phase observations indicated that restricting the search to a specific population could potentially limit the pool of relevant studies.
Table 1
Eligibility criteria
| Components | Inclusion | Exclusion |
| Participant characteristics | All clinical diagnosis of all causes of oropharyngeal dysphagia (unspecified/undifferentiated) regardless of the disease type or stage Age: ≥18 | Animal studies Only oesophageal dysphagia Age: 0–17 years |
| Intervention | Cough response (i.e., voluntary, reflexive, cough induced by tussigenic agents) | Non-cough interventions (e.g., only throat clearing, multiple swallows, etc) |
| Reference tests | Videofluoroscopic Swallowing Study, Fibreoptic Endoscopic Evaluation of Swallowing with or without any other tool | Clinical bedside swallow evaluation, other instrumental assessments (e.g., ultrasound, manometry, etc) |
| Depth of airway invasion | Airway penetration and/or aspiration, silent aspiration | Only healthy individuals (non-aspirators) |
| Study design | Primary research studies, reference lists, conference abstracts | Secondary research studies, Grey literature |
Cough was the primary intervention of interest; thus, non-cough interventions were excluded. Two types of coughs were considered for inclusion. The first type involved the presence of a reflexive cough (RC) in study participants, without a control or comparison component. RC also included the utilisation of tussigenic agents (e.g., nebulised tartaric acid). When these agents were administered to participants who did not initially demonstrate a RC response to airway penetration and/or aspiration, effectiveness was assessed by comparing the response to baseline measurements. The second type was use of voluntary cough (VC) for study participants without an automatic cough response during airway invasion. For VC responses, a comparison was made against the baseline measurements taken when the participant did not exhibit a reflexive cough response during airway penetration or aspiration (i.e., silent aspiration).
The decision not to restrict studies by participant feeding status allowed for the inclusion of individuals with various feeding methods, since different feeding regimens could affect cough responsiveness (Nakajoh et al., 2000).
Two widely-recognised instrumental assessment methods for dysphagia, VFSS and FEES, served as reference tests. These instruments offer direct visualisation of swallowing events and yield more accurate results as compared to other imaging methods for swallowing assessment (Helliwell et al., 2023).
The review considered peer-reviewed full-text articles (FTAs) and conference abstracts (CAs) as eligible publication types to ensure the inclusion of recent research (Scherer & Saldanha, 2019). However, if the full-text version of a CA was identified, the CA was excluded. Master’s theses and grey literature were excluded due to potential lack of peer review, while doctoral dissertations were included due to their adherence to rigorous peer-review process.
2.2Outcomes of interest
This review aimed to assess cough effectiveness for airway clearance, focusing on whether the cough response resulted in partial, complete, or no clearance of foreign materials from the airway. While standardised outcome measures like the Penetration-Aspiration Scale (PAS; Rosenbek et al., 1996) exist for dysphagia, there is no specific tool to evaluate cough effectiveness. As such, this review took a broad approach by including any measured attempt to expel foreign material from the airway, regardless of use of outcome measure. The secondary outcomes of interest involved analysing data in relation to factors including, but not limited to, type and frequency of cough (Table 2).
Table 2
List of outcomes of interest
| Outcomes of interest | Description |
| Airway clearance | The ability to effectively remove or clear foreign substances, secretions, or obstructions from the airway. The degree of airway clearance will be categorised as complete, partial, or no clearance, with or without the use of valid outcome measures. |
| Type of cough | The classification of cough is based on different types, including cough reflex, voluntary cough and cough induced by tussigenic agents. |
| Frequency of cough | The assessment of the number of cough episodes or occurrences in response to airway invasion. This can be described as single or sequential coughing events. |
| Timing of cough | The examination of the temporal pattern or occurrence of cough in relation to airway invasion, such as immediate coughing response or delayed coughing. |
| Depth of airway invasion | The extent of airway penetration and/or aspiration of substances into the airway. This can be assessed using validated outcome measures (e.g., PAS) or perceptually through descriptions. |
| Objective measure(s) | The quantitative assessment of cough characteristics presented in the study, such as PCF, CEV. |
| Trial characteristics | The identification of the type of bolus used during the swallowing evaluation and its correlation with the occurrence of airway invasion and subsequent cough response. |
| Reference tests | The use of instrumental assessments VFSS and/or FEES to determine the cough response during airway invasion. |
2.3Data source
A literature search was conducted across six databases: PubMed, Embase, CINAHL (Ultimate), Scopus, ProQuest Dissertations & Theses A& I, and Web of Science Core Collection. Additionally, reference lists of included studies were reviewed to identify additional sources. Contact with study authors was made to gather further information when required.
Initially, a pilot search phase was conducted by the principal investigator (RA) to identify relevant studies and ensure that there were no existing reviews on the same topic. In collaboration with the subject librarian, adjustments in the pilot search strategy were utilised to improve its accuracy and relevance. Once the final search strategy was piloted, its quality was assessed by the second reviewer (CB) using the Peer Review of Electronic Searches Strategy (PRESS; McGowan et al., 2016), and was deemed appropriate with no revisions needed.
An electronic database search was conducted in March 2023 and updated in March 2024 using the finalised search strategy. No filters were employed, except for ProQuest database, where only doctoral dissertations were selected to ensure access to peer-reviewed data.
2.4Selection process
Two independent reviewers with expertise in dysphagia (RA, CB) performed the title and abstract screening. The data were imported into Covidence (Veritas Health Innovation) to eliminate duplicate records. Disagreements were resolved through discussion. When consensus could not be reached, the third author (CK) made the casting decision.
2.5Data collection process
A data extraction form was developed by the principal investigator (RA) to systematically collect relevant information from included studies. The form underwent several revisions to ensure its effectiveness and was pilot-tested by both reviewers, with no major modifications needed.
Handling missing or insufficient data is a common challenge during the data extraction phase (Higgins et al., 2019). Missing data were addressed by contacting study authors for access to FTAs or essential data related to the primary outcome.
Following title and abstract screening, full-text screening was performed by both reviewers. Data extraction was conducted by the principal investigator (RA). Data were inputted into an Excel spreadsheet, addressing general and specific study characteristics.
2.6Assessment of methodological quality
Methodological appraisal was conducted for FTAs only as it was not feasible to assess quality of CAs due to limited reporting within this publication type. Risk of bias was evaluated using the D&B tool (Downs & Black, 1998), which assesses methodological quality across external validity, internal validity (bias – confounding) and study power.
The certainty of evidence was evaluated using the GRADE (Grading of Recommendations Assessment, Development, and Evaluation; Meader et al., 2014) approach, which provides an overall assessment of the quality of evidence across all included studies for a specific outcome. The evidence presented in this review was assessed for quality, relevance, and overall confidence using an established rating system (Table 3).
Table 3
GRADE certainty ratings
| Certainty level | What it means |
| Very low | The true effect is probably markedly different from the estimated effect. |
| Low | The true effect might be markedly different from the estimated effect. |
| Moderate | The authors believe that the true effect is probably close to the estimated effect. |
| High | The authors have a lot of confidence that the true effect is similar to the estimated effect. |
The AMSTAR-2 (A MeaSurement Tool to Assess systematic Reviews-second edition; Shea et al., 2017) was employed to conduct quality appraisal of the review, ensuring a rigorous and transparent assessment of methodological rigor and bias in the systematic review.
3Results
The initial search took place in March 2023 and was then updated in March 2024. The final search yielded 6,049 studies, of which 3,799 studies remained following de-duplication. Two reviewers (RA & CB) independently conducted title and abstract screening for the initial search, while for the updated search, this task was carried out by (RA & CK). In cases of disagreement, decision was reached through discussion with the third author (CK), which was necessary for one study during the initial search that was ultimately excluded.
Given the lack of homogeneity amongst the studies, a meta-analysis could not be conducted, therefore, it was not feasible to present a quantitative summary of the findings. Hence, this review relied solely on a qualitative synthesis of the evidence, which cannot provide a precise estimation of the overall effect.
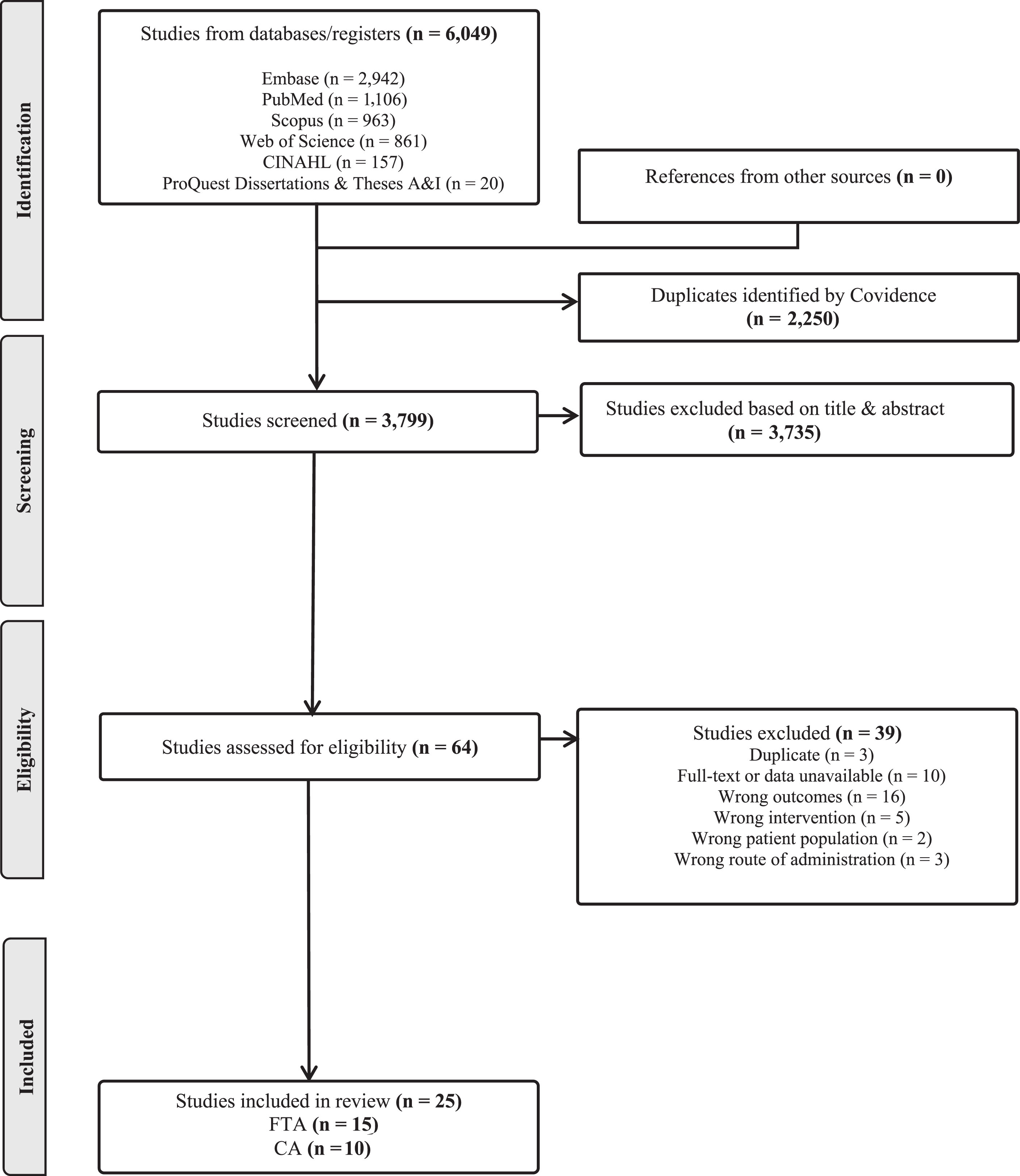
During full-text screening, 64 studies were examined, and eligibility criteria were applied. 45 contact attempts were made for 32 potentially eligible studies. This led to inclusion of one study where the author provided access to the FTA. 39 studies were excluded: 26 were ineligible, 10 had no full-text access and/or no author response, three were duplicates. Ultimately, 25 studies met the inclusion criteria, as illustrated in Fig. 1.
Fig. 1
PRISMA Flow-Chart.
Notably, four studies exhibited resemblance in terms of study objectives and methodologies, albeit with minor differences (Plowman et al., 2016; Tabor-Gray et al., 2017; Wallace et al., 2018; Wallace et al., 2021). Contact attempts were made in 2023 and 2024 to seek clarification from the authors to ensure that these were not duplicates or did not involve same participants, but no response was received. These studies were therefore included, since methodological differences indicated they were more likely to be distinct studies.
3.1Study characteristics
Analysis of the included studies was performed to determine the general characteristics of these studies (Table 4). Of the included studies, n = 15/25 (60%) were FTAs. It was not possible to obtain additional information for n = 10/25 (40%) CAs, despite correspondence with the authors. Hence, a substantial amount of data points were either missing or insufficient for further analysis.
Table 4
General characteristics of included studies
| Citation | Record type | Study design | Journal | Funding source(s) | Conflicts of interest |
| Wu et al., 1997 | FTA | Observational study | Laryngoscope | NR | NR |
| Lefton-Greif et al., 2000 | FTA | Cross-sectional study | The Journal of Pediatrics | NR | NR |
| Eisbruch et al., 2002 | FTA | Observational study | International Journal of Radiation Oncology Biology Physics | NR | NR |
| Wolf &Meiners, 2003 | FTA | Cross-sectional study | Spinal Cord | NR | NR |
| Nguyen et al., 2007 | FTA | Cross-sectional study | Lung | NR | NR |
| Seidl et al., 2008 | FTA | Cross-sectional study | European Archives of Oto-Rhino-Laryngology | NR | NR |
| Bekelis et al., 2010 | FTA | Case report | Dysphagia | NR | NR |
| Bianchi &Cantarella, 2011 | FTA | Case series | Dysphagia | NR | NR |
| Leder &Lerner, 2013 | FTA | Case report | QJM: monthly journal of the Association of Physician | R | NR |
| Tabor-Gray et al., 2021 | FTA | Case-control study | Dysphagia | R | R |
| Wallace et al., 2021 | FTA | Cross-sectional study | International Journal of Speech-Language Pathology | NR | R |
| Plowman et al., 2021 | FTA | Cross-sectional study | Journal of Thoracic and Cardiovascular Surgery | NR | R |
| Borders &Troche, 2022 | FTA | Cross-sectional study | Journal of Speech, Language, and Hearing Research | R | R |
| Jamróz et al., 2022 | FTA | Mixed method study | Polish Otorhinolaryngology Review | NR | R |
| Ohno et al., 2022 | FTA | Observational study | Dysphagia | R | R |
| Yu et al., 2009 | CA | Cross-sectional study | American Journal of Geriatric Psychiatry | NR | NR |
| Hunter et al., 2011 | CA | Cohort study/clinical trial | International Journal of Radiation Oncology Biology Physics | R | NR |
| Gaziano et al., 2015 | CA | Cross-sectional study | Dysphagia | R | NR |
| Plowman et al., 2016 | CA | Cross-sectional study | Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration | NR | NR |
| Ledl &Mertl-Roetzer, 2017 | CA | Observational study | Dysphagia | NR | NR |
| Tabor-Gray et al., 2017 | CA | Cross-sectional study | Dysphagia | NR | NR |
| Everton et al., 2018 | CA | Cross-sectional study | European Stroke Journal | NR | NR |
| Jaffe et al., 2018 | CA | Case series | American Journal of Respiratory and Critical Care Medicine | NR | NR |
| Wallace et al., 2018 | CA | Cross-sectional study | Dysphagia | NR | NR |
| York et al., 2022 | CA | Cross-sectional study | Dysphagia | R | NR |
R = Reported, NR = Not Reported.
3.2Participants demographics
The included studies involved 2,134 adult participants, all aged 18 or older, with dysphagia associated with various medical conditions such as neurodegenerative disease (n = 5, 20%) and head and neck cancer (n = 3, 12%). Data on participant sex was available for 1,177 (55%) participants, with 740 (63%) male and 437 (37%) female participants. Majority of the studies reported the mean age (n = 13/25; 52%), while only one study reported the median age. Demographic information of 957 participants across eight studies was not explicitly provided.
3.3Primary outcomes of interest
The included studies exhibited heterogeneity in terms of reporting of cough effectiveness (Table 5).
Table 5
Key characteristics of included studies
| Citation | No. of participants & clinical diagnosis | Sex & age (years) | Depth of airway invasion (P and/or A) | Type/Timing /Frequency of cough | Cough objective measure (s) | Outcome measure(s) | Trial characteristic (bolus type) | Cough response effectiveness (no. of participants) | ||
| Effective | Partially effective | Ineffective | ||||||||
| Wu et al., 1997 | n = 28 Dysphagia | M = 17, F = 11 Mean age = 64.7 Range = 23–82 | A &P | NR | NR | NR | Thin liquid &puree | n = 14/28 | NR | n = 25/28 |
| Lefton-Greif et al., 2000 | n = 70 Ataxia telangiectasia | M = 39, F = 31 Mean age = 10.7 Range = 1.8–30 | A | NR/delayed/NR | NR | NR | Thin liquid &puree | NR | NR | n = 1/70 |
| Eisbruch et al., 2002 | n = 26 HNC | NR | A &P | NR | NR | NR | Thin liquid, puree, soft &solid food | NR | NR | n = 0/22 (Pre-therapy n = 2/20 (Post- therapy) n = 2/13 (Late post-therapy) |
| Wolf &Meiners, 2003 | n = 51 Cervical spinal cord injury | M = 35, F = 16 Mean age = 43.4 Range = 16–89 | A | RC/NR/NR | NR | NR | Thin liquid &creamy food | n = 20/51 (Pre-therapy) n = 2/51 (Post-therapy) | n = 13/51a (Pre-therapy) n = 1/51a (Post- therapy) | |
| Nguyen et al., 2007 | n = 89 HNC | M = 89 Median = 60 Range = 34–86 | A | RC/ NR /NR | NR | NR | Thin liquid, puree, soft &solid | n = 46/89 (Pre-therapy) n = 25/30 (Post-therapy) | NR | n = 17/89 (Pre-therapy) n = 5/30 (Post-therapy) |
| Seidl et al., 2008 | n = 101 Neurological disorders | M = 63, F = 38 Mean age (SD) = 60.2±16.35 | A &P | NR | NR | PAS | Thin liquid &solid food | n = 72/101 | NR | NR |
| Bekelis et al., 2010 | n = 1 Atlantoaxial traumatic injury | M = 1 61 | A | NR/immediate &delayed/NR | NR | NR | Thin liquid, thick liquids &puree | NR | NR | n = 1/1 |
| Bianchi &Cantarell, 2011 | n = 2 Laryngectomy | M = 2 69 &79 | A | NR | PEF &CPF | NR | NR | n = 2/2 | NR | NR |
| Leder &Lerner, 2013 | n = 1 Dysphagia | M = 1 71 | A | RC/NR | NR | NR | Medication | NR | NR | n = 1/1 |
| Tabor-Gray et al., 2021 | n = 32 (ALS) n = 34 (control) Neurodegenerative disease | M = 16, F = 16 (ALS) Mean age (SD) = 62.31±10.75 Range = 36–83 M = 18, F = 16(control) Mean age (SD) = 55.53±14.9 Range = 37–86 | A &P | RC/NR/NR | CPD, PEFR, PERT &CVA | PAS | Thin liquid, thin honey, puree &solid | n = 26/32 | NR | n = 1/32 |
| Wallace et al., 2021 | n = 13 Dysphagia | M = 9, F = 4 Mean age = 7 Range = 29–95 | A &P | RC/NR/NR | Acoustic intensity | PAS | Thin liquid, thick liquid, puree, soft &solid food | 4/17c | NR | 13/17c |
| Plowman et al., 2021 | n = 182 Cardiac disease | M = 122, F = 60 Mean age (SD) = 62.3±13.3 | A &P | NR | NR | PAS &Yale residue rating scale | Gatorade, puree &solid | n = 8/53 | NR | n = 17/53 |
| Borders &Troche, 2022 | n = 33 (A, 68 trials) n = 30 (P, 55 trials) Neurodegenerative disease | M = 27, F = 6 (A cohort) Mean age (SD)= 70.10±10.21 Range=56–89 M = 26, F = 4 P cohort) Mean age (SD) = 68.96±9.08 Range=41–82 | A &P | VC/NR/single &sequential | PCF, CEV &CVA | PAS, 100-point visual analog scale | Thin liquid | A = 26% d P = 51% d | A = 60% d P = 91% d | A = 12% d |
| Jamróz et al., 2022 | n = 99 Unilateral laryngeal paralysis | M = 40, F = 59 Mean age = 50.67 Range = 18–78 | A &P | NR | NR | PAS | NR | NR | NR | n = 4/12 |
| Ohno et al., 2022 | n = 154 Dysphagia | M = 97, F = 57 Mean age (SD) = 69.2±16.8 | A &P | RC &VC/NR/NR | NR | PAS | Barium gelatine jelly &thick liquid | n = 15/87e n = 18/87e n = 30/42e | n = 8/42a,e | |
| Yu et al., 2009 | n = 49 Schizophrenia | M = 2, F = 17 Mean Age (SD)= 70.6±4.6 | A &P | NR | NR | NR | NR | NR | 10% a | |
| Hunter et al., 2011 | n = 72 HNC | NR | A | NR | NR | NR | Thin and thick liquid, puree &solid | NR | n = 10/15 | |
| Gaziano et al., 2015 | n = 62 Neurodegenerative disease | NR | A | NR | NR | PAS | Thin &paste | n = 1/20 | NR | n = 7/20 |
| Plowman et al., 2016 | n = 26 Neurodegenerative disease | NR | A | NR | NR | PAS, NRRS, PCR &LVC | NR | 65% c | NR | 1% c |
| Ledl &Mertl-Roetzer, 2017 | n = 724 Dysphagia | NR | A &P | RC/NR/NR | NR | PAS | Thin liquid, jelly &solids | 74.4% c | NR | NR |
| Tabor-Gray et al., 2017 | n = 30 Neurodegenerative disease | NR | A | NR | NR | PAS & LVC | Thin & paste | 65%c | NR | 1%c |
| Everton et al., 2018 | n = 17 Stroke survivors | Sex = NR Mean age = 74 | A & P | NR | NR | PAS | Thin fluids | NR | 5 ml = 2%a (Number of swallows) 50 ml = 0%a (Number of swallows) | |
| Jaffe et al., 2018 | n = 2 Dysphagia | Case 1 = M Case 2 = F Case 1 = 81 Case 2 = 86 | A | NR | NR | NR | NR | n = 1/2 | NR | n = 1/2 |
| Wallace et al., 2018 | NR | NR | A &P | RC &VC/NR/NR | Acoustic intensity | PAS | NR | 14/44c | NR | 30/44c |
| York et al., 2022 | n = 206 Lung Transplant | M = 105, F = 101 Mean age = 58.6 | A &P | NR | NR | PAS | NR | n = 26/82 | NR | n = 15/82 |
a = Study did not specify whether cough was partially effective or ineffective, so cells were merged. b = In this study, cough reflex was described as ‘’ strong” if judged to be sufficient to clear aspirated material or ‘’weak” if insufficient.CRT responses were elicited using three concentration levels (0.4, 0.6 and 0.8 mol/L). Participates were grouped based on PAS scores: PAS 1 (n = 48), PAS 2-5 (n = 45) and PAS 6-8 (n = 13). Data on weak and strong CRT responses for each concentration level were presented for each subgroup. In this table, data on the ‘’strong CRT” and ‘’Weak CRT” for both PAS 2-5 and PAS 6-8 group have been combined and presented together. c = Study provided number or percentage of in/effective coughs as a proportion of all coughs. d = Study provided number or percentage of in/effective coughs as a proportion of all penetration/aspiration events. e = Participants exhibited RC to clear residue. If ineffective, voluntary cough was trialed. If ineffective, cough was induced with tussigenic agent. Of n = 42 participants who underwent tussigenic provocation, n = 4 continued to have no cough response. P = Penetration, A = Aspiration, PAS = Penetration-Aspiration Scale, NR = Not Reported, M = Male, F = Female, HNC = Head and Neck Cancer, ALS = Amyotrophic Lateral Sclerosis, FVC = Forced Vital Capacity, PEF = Peak Expiratory Flow, FEV = Forced Expiratory volume in 1 s, CPF = Cough Peak Flow, NRRS = Normalised Residue Ratio Scale, PCR = Pharyngeal Constriction Ratio, LVC = Laryngeal Vestibule Closure Status, CPD = Compression Phase Duration (ms), PEFR = Peak Expiratory Flow Rate (L/s), PERT = Peak Expiratory Rise Time (ms), CVA = Cough Volume Acceleration (L/s/s), 1 = Mean±Standard Deviation Range (minimum–maximum), CiTA = Cough-inducing method using Tartaric Acid, CRT = Cough Reflex Testing.
3.3.1Effective cough response
Of FTAs, n = 10/15 (66%) reported the presence of an effective cough response in study participants, while the remaining n = 5/15 (33%) studies did not report presence of an effective cough response during airway penetration and/or aspiration. Of FTAs including participants with effective cough responses, n = 6/10 (60%) used validated tools, while n = 4/10 (40%) did not use any validated outcome measures and relied on descriptive terms to determine cough effectiveness. Nguyen and colleagues (2007 : 243) described the cough reflex as being ‘’graded as present and effective, ineffective, intermittently effective, or absent”. Similarly, Wolf and Meiners (2003 : 349) presented ‘’five levels of impairment of laryngeal function...represented the prevalence and severity of dysphagia. In level 3 ... the coughing reflex was readily employed to clear the trachea.” Bianchi and Cantarell (2011) and Wu and colleagues (1997) reported airway clearance following cough response in study participants, without using any specific descriptors to determine extent of cough effectiveness.
The presence of an effective cough response in study participants was reported in n = 7/10 (70%) of CAs, while n = 3/10 (30%) did not report presence of an effective cough response. Of those with an effective cough response, n = 6/7 (86%) used validated tools. In contrast, n = 1/7 (14%) did not specify use of any tool.
3.3.2Partially effective cough response
Among the FTAs, n = 1/15 (7%) reported the presence of a partially effective cough response in study participants, while n = 13/15 (87%) did not, and in n = 1/15 (7%), the reporting of cough response was unclear. Borders and Troche (2022) reported partially effective cough in participants by utilising the Penetration-Aspiration Scale (PAS; Rosenbek et al., 1996) along with a 100-point visual analogue scale (Curtis et al., 2021), to estimate the proportion of aspirate material expelled from the airway during penetration and aspiration events. On the other hand, Wolf and Meiners (2003) provided a five-point grading system that coupled swallow and cough function together, where one represented most and 5 represented least impaired. For example, at level 2, they reported ‘’Severe residue and aspiration of saliva... together with an impaired coughing reflex were present” (Wolf and Meiners, 2003 : 349). Based on the given information, it was difficult to determine if the cough was ‘’partially effective” or ‘’ineffective” for airway clearance.
Of CAs, n = 8/10 (80%) did not report the presence of a partially effective cough response in study participants, while in n = 2/10 (20%), the reporting of cough response was unclear. Everton and colleagues (2018) provided a description of airway clearance with two different volumes of thin liquids, stating that ‘’aspirated material was rarely fully cleared”. Likewise, Hunter and colleagues (2011) did not clearly distinguish participants with no response from those with inefficient response for airway clearance.
3.3.3Ineffective cough response
The presence of an ineffective cough response was reported in n = 11/15 (74%) FTAs, while n = 2/15 (13%) did not, and in n = 2/15 (13%), the reporting of cough response in study participants was unclear. In studies with insufficient details on the cough response, descriptions were used to assess cough responsiveness. For instance, Bekelis and colleagues (2010 : 156) stated, ‘’the patient coughed...but was not able to clear aspirated material completely from the airway.” Consequently, determining complete or partial effectiveness of cough based on data provided was not possible. Notably, only one study reported the presence of consistently ineffective or absent cough response, however, there was lack of clarity on number of participants with consistently ineffective cough response versus those with an absent cough response (Nguyen et al., 2007).
Of CAs, n = 6/10 (60%) reported the presence of an ineffective cough response in study participants, n = 1/10 (10%) did not, and in n = 3/10 (30%) studies, the reporting of cough response was unclear. In their abstract, Yu and colleagues (2009) provided a description of cough ineffectiveness, without explicitly indicating whether the cough was partially effective or completely ineffective.
3.4Secondary outcomes of interest
3.4.1Depth of airway invasion
In the included studies, n = 14/25 (56%) reported the occurrence of both penetration and aspiration events in participants, while n = 11/25 (44%) reported aspiration events only. Among studies examining penetration and aspiration events, n = 4/14 (28%) specifically reported presence of a cough response to both penetration and aspiration. Effective cough in response to penetration was reported in n = 4/25 (16%) studies, while n = 10/25 (40%) studies reported an effective cough in response to aspiration events. Borders and Troche (2022) also reported partially effective cough in response to both penetration and aspiration in their study.
Conversely, n = 2/25 (8%) studies reported an ineffective cough response to penetration, while n = 14/25 (56%) reported an ineffective cough in response to aspiration. In n = 7/25 (28%), it was not specified whether the cough response was in response to airway penetration or aspiration.
3.4.2Type, timing, frequency of cough response
In n = 8/25 (32%), cough type was specified, with n = 6/25 (24%) studies reporting the occurrence of RC, n = 1/25 (4%) reporting occurrence of VC and n = 2/25 (8%) reporting both RC and VC. However, n = 16/25 (64%) studies did not provide information on the type of cough assessed.
Of studies with VC or both RC and VC responses, cough instructions were presented in three studies. Although the cough instructions and frequency of the cues were not standarised, Borders and Troche (2022) provided comprehensive information regarding the instructions when airway invasion was evident. Tabor-Gray and colleagues (2021) utilised scripted instructions to prompt coughing and rate perceived airway sensation magnitude of urge to cough. However, similar to Ohno and colleagues (2022), neither study provided sufficient detail about frequency and pattern of cough instructions. Therefore, consistency in instruction delivery remained unclear in these studies.
As for the timing of the cough response, n = 23/25 (92%) studies did not report the timing of cough initiation during airway compromise. Lefton-Greif and colleagues (2000) reported a delayed cough response, while Bekelis and colleagues (2010) reported both immediate and delayed cough responses in study participants.
None of the included studies specified frequency of cough responses during airway invasion. Wallace and colleagues (2021) mentioned that only the first expulsive manoeuvre following these events was evaluated. Likewise, Tabor-Gray and colleagues (2021) analysed of the airflow measures for the first cough response to each stimulus trial, without reporting the number of coughs produced by participants.
3.4.3Objective measures of cough
In n = 5/25 (20%) of the included studies, objective measures of cough were presented. Bianchi and Cantarell (2011) presented two case studies of patients post-partial laryngectomy, who underwent a swallowing rehabilitation program aimed at improving cough function, measured through parameters like Peak Expiratory Flow (PEF) and Cough Peak Flow (CPF). While no significant improvement in swallowing function were reported, it did result in enhanced CPF values after ten sessions. Despite the absence of respiratory issues during follow-up period, the last VFSS showed persistent tracheobronchial aspiration, which was cleared by voluntary coughing.
Borders and Troche (2022) investigated the relationship between Peak Expiratory Flow Rate (PEFR), Cough Expiratory Volume (CEV), and Cough Volume Acceleration (CVA) with airway clearance in patients with neurodegenerative disease, aiming to establish clinically meaningful cut-off values. It was revealed that higher values of PEFR and CEV were associated with a greater proportion of residue expelled from the subglottis.
Tabor-Gray and colleagues (2021) examined reflexive airway responses in Amyotrophic Lateral Sclerosis (ALS) patients compared to healthy controls, focusing on Compression Phase Duration (CPD), Peak Expiratory Rise Time (PERT), PEFR, and CVA for the first cough response. It was reported that ALS individuals demonstrated reduced PEFR, longer PERT, and lower CVA.
Wallace and colleagues (2018) evaluated cough strength using acoustic intensity measured via a lapel microphone, finding it ineffective in discriminating between effective and ineffective cough responses for airway clearance, a conclusion supported by another study by Wallace and colleagues (2021).
3.4.4VFSS versus FEES
VFSS was used to assess swallowing function in n = 16/25 (64%) studies, while n = 8/25 (32%) used FEES, and n = 1/25 (4%) presented evidence from both FEES and VFSS. Wu and colleagues (1997) conducted a controlled comparative study where individuals with chronic dysphagia underwent VFSS and FEES during a period of two weeks. In n = 11/28 (39%) of study participants, disagreements were observed in the assessment of effective cough reflex, with results suggesting that FEES exhibited greater sensitivity in detecting an effective cough reflex during airway compromise when compared to VFSS.
3.4.5Trial characteristics
In n = 17/25 (68%) studies, the type of bolus presented during the instrumental assessment was reported. Notably, liquid bolus emerged as the most commonly used bolus type as compared to others. Only one reported an incident of aspirin pill aspiration (Leder & Lerner, 2013), while in the n = 9/25 (36%) studies, the characteristics of the bolus were not provided.
In the study by Wallace and colleagues (2021), coughing events in response to airway penetration occurred with various bolus textures, reportedly with thin liquid (water), mildly thick liquid (juice), and soft diet (banana). Cough responsiveness showed inconsistencies, with two effective coughs for water and banana, and two for mildly thick juice, while three coughs were ineffective for water and one for mildly thick juice. In addition, bolus volume significantly impacted the airway invasion, as noted in studies by Everton and colleagues (2018) and Gaziano and colleagues (2015), with larger liquid volumes correlating with increased penetration and aspiration events.
3.5Assessment of methodological quality
Quality assessment of the FTAs revealed that a significant number of studies exhibited poor methodological quality (n = 13/15, 87%), while the remaining studies were deemed to have fair methodological quality (n = 2/15, 13%), as shown in Table 6.
The evidence presented in this review is determined to have a “very low” level of certainty due to factors such as the predominance of observational study designs, insufficient data, limitations in the intervention method (e.g., lack of blinding, loss of follow-up), and inconsistent data reporting.
Table 6
Risk of bias in each study
| Domain | Reporting | External validity | Internal validity-bias | Internal validity-confounding | Power | Total score |
| Citation | ||||||
| Wu et al., 1997 | 7 | 0 | 1 | 0 | 0 | 8 |
| Lefton-Greif et al., 2000 | 6 | 0 | 1 | 0 | 0 | 7 |
| Eisbruch et al., 2002 | 5 | 0 | 0 | 1 | 0 | 6 |
| Wolf &Meiners, 2003 | 9 | 0 | 0 | 2 | 0 | 11 |
| Nguyen et al., 2007 | 5 | 0 | 0 | 1 | 0 | 6 |
| Seidl et al., 2008 | 6 | 0 | 1 | 0 | 1 | 7 |
| Bekelis et al., 2010 | 3 | 0 | 0 | 0 | 0 | 3 |
| Bianchi & Cantarella, 2011 | 3 | 0 | 0 | 0 | 0 | 3 |
| Leder & Lerner, 2013 | 5 | 0 | 0 | 0 | 0 | 5 |
| Tabor-Gray et al., 2021 | 8 | 0 | 4 | 2 | 0 | 14 |
| Wallace et al., 2021 | 6 | 0 | 3 | 1 | 0 | 10 |
| Plowman et al., 2021 | 8 | 0 | 4 | 2 | 1 | 15 |
| Borders & Troche, 2022 | 11 | 0 | 4 | 1 | 0 | 16 |
| Jamróz et al., 2022 | 6 | 0 | 1 | 0 | 0 | 7 |
| Ohno et al., 2022 | 7 | 0 | 2 | 2 | 0 | 11 |
Note: The scoring ranges for the evaluation criteria are as follows: Excellent (E) = 26–28, Good (G) = 20–25, Fair (F) = 15–19, Poor (P) =≤14.
4Discussion
The primary aim of this review was to systematically identify, evaluate, and summarise the literature on the effectiveness of cough in response to penetration and/or aspiration during VFSS or FEES in individuals with OD of any aetiology. The 25 included studies exhibited variations in how effectiveness of cough response for airway clearance was reported. For example, some reported total number of in/effective cough responses, while others reported numbers of participants with in/effective cough responses. Given a lack of uniformity, meta-analysis was impossible. Moreover, it is difficult to provide conclusive evidence of cough effectiveness.
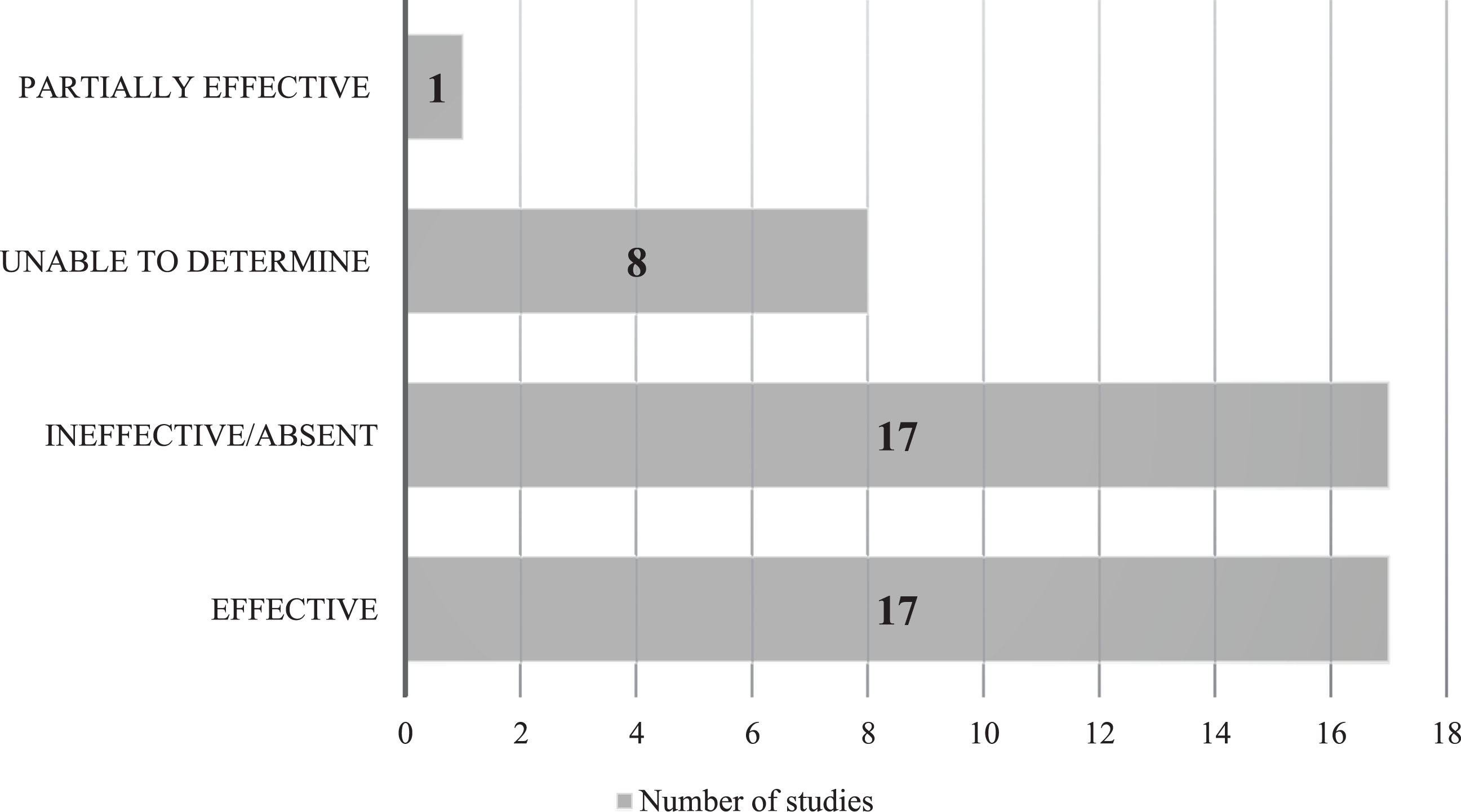
Despite these discrepancies, an effective cough response was observed in 17 studies for some participants, while 17 studies reported ineffective cough responses (Fig. 2). One study indicated a partially effective cough response for participants. The categories in the figure were not mutually exclusive, with some studies reporting all three categories of cough responses, while others reported one of two of these categories.
Fig. 2
Reported effectiveness of participant cough responses.
The clinical diagnoses of included patients varied. Overall effective cough responses were noted by several studies in conditions like neurodegenerative disease. Although an umbrella term, this holds promise for patients with such conditions. By contrast, some conditions (e.g., unilateral laryngeal paralysis) only had one study that provided supporting evidence. Since some conditions were represented only once and since cough effectiveness may vary by pathophysiology, there is a need for confirmatory studies to support or refute existing evidence. While a few studies considered impact of secondary outcomes of interest on cough responsiveness, the presence and impact of these factors were not universally accounted for in all studies. It therefore remains unclear as to whether factors like depth of airway invasion or objectively measured cough strength have a relationship with cough effectiveness for airway protection during swallowing.
Furthermore, recognising limitations of ordinal scales like PAS (Rosenbek et al., 1996) underscores the necessity of developing a specified assessment tool for evaluating cough effectiveness. This tool should consider impact of various factors, including the type, timing, and frequency of responses, as well as the extent of clearance achieved. Implementing such a standardised tool would facilitate data pooling and enable meta-analyses, ultimately advancing our understanding of cough effectiveness. Future studies would benefit from addressing these factors to enhance generalisability of findings into clinical practice.
The methodological appraisal revealed that majority of FTAs had poor methodological quality due to inadequate reporting, poor external and internal validity of the studies and lack of information about the sample size and power of the study.
4.1Interpretation based on the literature
Numerous recent studies indicate a growing interest in cough and swallow function, primarily due to their anatomical proximity and their vital role in airway protection (Hutcheson et al., 2018). We identified some additional studies with relevant information but authors were not in a position to provide data, leading to their exclusion.
Of six studies with RC responses, two studies found that RC was ineffective in expelling aspirate material as compared to penetrate material (Tabor-Gray et al., 2021; Wallace et al., 2021). Another study found that VC was more effective in the clearance of penetrate material as compared to aspirate material (Borders & Troche, 2022). Of the two studies with the presence of both RC and VC, findings of one study suggested that VC was more effective than RC for airway clearance (Ohno et al., 2022). These findings are consistent with the previous literature suggesting that cough responses are generally more effective for material located within the airway than below the vocal folds (Han et al., 2016).
Of the included studies, five assessed objective measures of cough. Two of these studies revealed that higher PEFR values were associated with a higher proportion of residue expelled from the airway (Borders & Troche, 2022; Tabor-Gray et al., 2021). This finding is consistent with the previous literature showing that reduced PEFR values are correlated with the presence of swallowing impairments (Brandimore et al., 2014; Guillen-Sola et al., 2020; Sartor et al., 2017). In another included study, higher PCF values were associated with reduced risk of AP (Bianchi & Cantarell, 2011). These findings align with previous literature suggesting that higher PCF values are associated with reduced risk of AP (Oda et al., 2017; Kulnik et al., 2016; Sohn et al., 2018).
Regarding bolus textures, only one study specifically examined and reported cough responsiveness for different bolus textures. In line with previous findings by Miles and colleagues (2018), the cough responses exhibited inconsistencies across various bolus textures. However, in terms of bolus volume, two studies indicated that aspiration events were more likely to occur with increased volumes of liquid bolus (Everton et al., 2018; Gaziano et al., 2015). These findings contradict previous literature that reported variable cough responses across different trial volumes during aspiration events (Curtis et al., 2022; Miles et al., 2018).
The participants of included studies were a heterogenous cohort with various medical conditions. However, the majority of included studies did not specify disease severity, making it challenging to determine its impact on cough responsiveness. A recent study found no significant association between airway protective responses and disease diagnosis or duration, but the small and heterogeneous sample size prevented definitive conclusions regarding the impact of diagnosis and disease severity on cough response effectiveness (Curtis et al., 2022).
4.2Strengths and limitations
A systematic review possesses several strengths that contribute to its value as a rigorous and comprehensive search approach. To ensure the comprehensive inclusion of all necessary steps in the current review, the AMSTAR-2 tool (Shea et al., 2017) was utilised throughout the review process, emphasising the importance of meticulous and transparent methodology. While heterogeneity can pose challenges in terms of data synthesis, one of the strengths of this review was the comprehensive nature of the search process, which included studies from diverse patient populations, languages, and settings, thus contributing to a broader representation of the topic under investigation and enhancing the richness of the evidence base. The lack of language restrictions allowed for the inclusion of studies from diverse regions, providing a more comprehensive and global perspective on the research topic. Additionally, correspondence with authors served as a valuable resource in clarifying ambiguous details, resolving discrepancies, and ensuring a more comprehensive analysis of the data, thereby enhancing the comprehensiveness and accuracy of the review findings.
While the included studies in this review offer valuable insights, they exhibit several limitations. Firstly, the peer review process for CAs is less exhaustive than for FTAs, potentially introducing biases in reporting. Additionally, the absence of comprehensive lists of confounders (e.g., depth of airway invasion, medications, underlying condition) in the majority of the included studies makes them susceptible to confounding bias. Concerns about reliability arise from the use of non-validated tools and the lack of standardised protocols in cough assessment. Furthermore, the absence of control groups limits the applicability and generalisability of the findings, potentially leading to biased associations.
Limitations of the current review include substantial missing/inadequate data despite author correspondence, potential for bias due to single-person data extraction (Higgins et al., 2019), the potential presence of duplicate records with no clarification, lack of homogeneity preventing meta-analysis and reliance on a qualitative synthesis of the evidence, which is open to interpretation and may not offer a precise estimation of the overall effect. Furthermore, the D& B checklist may not comprehensively capture bias sources, potentially affecting assessment accuracy, and the lack of quality appraisal for CAs could include studies with lower methodological quality, affecting the validity and reliability of the findings.
5Conclusions
This review identified critical gaps in the literature that highlight the lack of robust evidence for cough as a strategy for airway protection. A notable limitation is the lack of protocols and guidelines for assessing cough effectiveness during airway invasion. Without these, further research into cough effectiveness will be compromised by difficulties comparing findings and synthesising evidence. We therefore recommend that such protocols and guidelines should be developed as a matter of priority. If so, robust study designs like randomised controlled trials (RCTs), particularly pragmatic RCTs, could generate essential evidence. Addressing confounding factors, recruiting larger and more representative sample sizes, and standardising outcome measures are key priorities for future research.
While evidence synthesis for cough as a strategy to enhance swallow safety is challenged by these limitations, this does not mean that it should be abandoned in clinical practice. Indeed, some studies within this review identified that cough is effective for protecting the airway, mirroring clinician experiences. In the absence of knowing which cohorts may benefit from this strategy and why, those working with dysphagia are encouraged to consider the use of cough to maximise safety and reduce potential airway obstruction or aspiration pneumonia.
Acknowledgments
The authors are grateful to Ms Éadaoin Flynn for her feedback on earlier versions of this work. We also express our gratitude to Ms Isolde Harpur, who provided her expertise as subject librarian.
Conflict of interest
The authors have no conflict of interest to report. Given his role as Editorial Board member, Ciarán Kenny had no involvement with nor access to information regarding the peer review of this article.
References
[1] | Baijens, L. W. , Clavé, P. , Cras, P. , Ekberg, O. , Forster, A. , Kolb, G. F. , Leners, J. C. , Masiero, S. , Mateos-Nozal, J. , Ortega, O. , Smithard, D. G. , Speyer, R. , & Walshe, M. ((2016) ). European Society for Swallowing Disorders – European Union Geriatric Medicine Society white paper: Oropharyngeal dysphagia as a geriatric syndrome. Clinical interventions in aging, 11: , 1403–1428. https://doi.org/10.2147/CIA.S107750 |
[2] | Bekelis, K. , Gottfried, O. N. , Wolinsky, J. P. , Gokaslan, Z. L. , & Omeis, I. ((2010) ). Severe dysphagia secondary to posterior C1-C3 instrumentation in a patient with atlantoaxial traumatic injury: A case report and review of the literature. Dysphagia, 25: (2), 156–160. https://doi.org/10.1007/s00455-009-9255-7 |
[3] | Bianchi, C. , & Cantarella, G. ((2011) ). Chronic aspiration without pulmonary complications afterpartial laryngectomy: Long-term follow-up of two cases. Dysphagia, 26: (3), 332–336. https://doi.org/10.1007/s00455-010-9299-8 |
[4] | Borders, J. C. , & Troche, M. S. ((2022) ). Voluntary Cough Effectiveness and Airway Clearance in Neurodegenerative Disease. Journal of Speech, Language, and Hearing Research, 65: (2), 431–449. https://doi.org/10.1044/2021_jslhr-21-00308 |
[5] | Brandimore, A. E. , Hegland, K. , & Troche, M. S. ((2014) ). Peak expiratory flow in parkinson’s disease [Conference Abstract]. Dysphagia, 29: (6), 772–773.https://doi.org/10.1007/s00455-014-9571-4 |
[6] | Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org. |
[7] | Curtis, J. A. , Borders, J. C. , Dakin, A. E. , & Troche, M. S. ((2022) ). The Role of Aspiration Amount on Airway Protective Responses in People with Neurogenic Dysphagia. Dysphagia https://doi.org/10.1007/s00455-022-10546-x |
[8] | Downs, S. H. , & Black, N. ((1998) ). The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of epidemiology and community health, 52: (6), 377384. https://doi.org/10.1136/jech.52.6.377 |
[9] | Eisbruch, A. , Lyden, T. , Bradford, C. R. , Dawson, L. A. , Haxer, M. J. , Miller, A. E. , Teknos, T. N. , Chepeha, D. B. , Hogikyan, N. D. , Terrell, J. E. , & Wolf, G. T. ((2002) ). Objective assessment of swallowing dysfunction and aspiration after radiation concurrent with chemotherapy for head- and-neck cancer. International Journal of Radiation Oncology Biology Physics, 53: (1), 23–28. https://doi.org/10.1016/S0360-3016(02)02712-8 |
[10] | Everton, L. , Benfield, J. , Michou, E. , Hamdy, S. , & Bath, P. ((2018) ). The pattern of penetration and aspiration in acute stroke survivors [Conference Abstract]. European Stroke Journal, 3: (1), 367. https://doi.org/10.1177/2396987318770127 |
[11] | Gaziano, J. , Hendrick, A. , Tabor, L. , Richter, J. , & Plowman, E. ((2015) ). Prevalence, timing and source of aspiration in individuals with ALS [Conference Abstract]. Dysphagia, 30: (5), 627–628. https://doi.org/10.1007/s00455-015-9633-2 |
[12] | Guillen-Sola, A. , Neira, N. , Boza, R. , Marco, E. , Duarte, E. , & Messaggi-Sartor, M. ((2020) ). Evaluating usefulness of the peak expiratory cough flow as a predictor of dysphagia in subacute stroke patients [Conference Abstract]. Dysphagia, 35: (1), 150. https://doi.org/10.1007/s00455-019-10078-x |
[13] | Hegland, K. W. , Okun, M. S. , & Troche, M. S. ((2014) ). Sequential Voluntary Cough and Aspiration or Aspiration Risk in Parkinson’s Disease. Lung, 192: (4), 601–608. https://doi.org/10.1007/s00408-014-9584-7 |
[14] | Helliwell, K. , Hughes, V. J. , Bennion, C. M. , & Manning-Stanley, A. ((2023) ). The use of videofluoroscopy (VFS) and fibreoptic endoscopic evaluation of swallowing (FEES) in the investigation of oropharyngeal dysphagia in stroke patients: A narrative review. Radiography, 29: (2), 284–290. https://doi.org/10.1016/j.radi.2022.12.007 |
[15] | Higgins, J. P. T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A. (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook |
[16] | Hunter, K. U. , Lyden, T. , Haxer, M. , Feng, F. Y. , Chepeha, D. , & Eisbruch, A. ((2011) ). What is the clinical relevance of objective swallow studies in head and neck cancer (HNC) patients receiving chemoirradiation (CRT)? Analysis of aspiration in swallow studies vs. risk of aspiration pneumonia [Conference Abstract]. International Journal of Radiation Oncology Biology Physics, 81: (2), S174. |
[17] | Hutcheson, K. A. , Barrow, M. P. , Warneke, C. L. , Wang, Y. , Eapen, G. A. , Lai, S. Y. , Barringer, D. A. , Plowman, E. K. , & Lewin, J. S. ((2018) ). Cough strength and expiratory force in aspirating and nonaspirating postradiation head and neck cancer survivors. The Laryngoscope, 128: (7), 1615–1621. https://doi.org/10.1002/lary.26986 . |
[18] | Jaffe, A. , Seevaratnam, A. , & Waters, S. ((2018) ). Risk of aspiration in patients on high-flow oxygen therapy [Conference Abstract]. American Journal of Respiratory and Critical Care Medicine, (MeetingAbstracts, 197. https://www.embase.com/search/results?subaction=viewrecord&id=L622965578&from=export |
[19] | Jamróz, B. , Jamróz, J. B. J. , Chmielewska, C. J. J. , Milewska, M. M. , Osuch-Wójcikiewicz, O. W. E. , & Niemczyk, N. K. ((2018) ). Postoperative dysfagia after surgery with free flap reconstruction from formarm: Case study [Conference Abstract]. Dysphagia, 33: (4), 585–586. https://doi.org/10.1007/s00455-018-9900-0 |
[20] | Kulnik, S. T. , Birring, S. S. , Hodsoll, J. , Moxham, J. , Rafferty, G. F. , & Kalra, L. ((2016) ). Higher cough flow is associated with lower risk of pneumonia in acute stroke. Thorax, 71: (5), 474–475. https://doi.org/10.1136/thoraxjnl-2015-207810 |
[21] | Leder, S. B. , & Lerner, M. Z. ((2013) ). Nil per os except medications order in the dysphagic patient. QJM: Monthly journal of the Association of Physicians, 106: (1), 71–75.. https://doi.org/10.1093/qjmed/hcs044 |
[22] | Ledl, C. , & Mertl-Roetzer, M. ((2017) ). The effect of texture variation on penetration-aspiration in patients with neurogenic dysphagia [Conference Abstract]. Dysphagia, 32: (6), 817–818. https://doi.org/10.1007/s00455-017-9805-3 |
[23] | Lefton-Greif, M. A. , Crawford, T. O. , Winkelstein, J. A. , Loughlin, G. M. , Koerner, C. B. , Zahurak, M. , & Lederman, H. M. ((2000) ). Oropharyngeal dysphagia and aspiration in patients with ataxia-telangiectasia. The Journal of Pediatrics, 136: (2), 225–231. https://doi.org/10.1016/s0022-https://doi.org/10.1016/s0022-3476(00)70106-53476(00)70106-5 |
[24] | Matsuo, K. , & Palmer, J. B. ((2008) ). Anatomy and Physiology of Feeding and Swallowing: Normal and Abnormal. Physical Medicine and Rehabilitation Clinics of North America, 19: (4), 691–707. https://doi.org/10.1016/j.pmr.2008.06.001 |
[25] | McGowan, J. , Sampson, M. , Salzwedel, D. M. , Cogo, E. , Foerster, V. , & Lefebvre, C. ((2016) ). PRESS Peer Review of Electronic Search Strategies: Guideline Statement. Journal of Clinical Epidemiology, 75: (1), 40–46. https://doi.org/10.1016/j.jclinepi.2016.01.021 |
[26] | Meader, N. , King, K. , Llewellyn, A. , Norman, G. , Brown, J. , Rodgers, M. , Moe-Byrne, T. , Higgins, J. P. , Sowden, A. , & Stewart, G. ((2014) ). A checklist designed to aid consistency and reproducibility of GRADE assessments: Development and pilot validation. Systematic Reviews, 3: (1), 82. https://doi.org/10.1186/2046-4053-3-82 |
[27] | Miles, A. , McFarlane, M. , Scott, S. , & Hunting, A. ((2018) ). Cough response to aspiration in thin and thick fluids during FEES in hospitalized inpatients.. International Journal of Language & Communication Disorders, 53: (5), 909–918. https://doi.org/10.1111/1460-6984.12401 |
[28] | Nakajoh, K. , Nakagawa, T. , Sekizawa, K. , Matsui, T. , Arai, H. , & Sasaki, H. ((2000) ). Relation between incidence of pneumonia and protective reflexes in post-stroke patients with oral or tube feeding. Journal of Internal Medicine, 247: (1), 39–42. https://doi.org/10.1046/j.1365-2796.2000.00565.x |
[29] | Nguyen, N. P. , Moltz, C. C. , Frank, C. , Millar, C. , Smith, H. J. , Dutta, S. , Nguyen, P. D. , Nguyen, L. M. , Lemanski, C. , Ludin, A. , Jo, B. H. , & Sallah, S. ((2007) ). Effectiveness of the cough reflex in patients with aspiration following radiation for head and neck cancer. Lung, 185: (5), 243–248. https://doi.org/10.1007/s00408-007-9016-z |
[30] | Oda, A. L. , Braga, T. E. R. , Salvioni, C. C. S. , Alves, P. C. L. , Borges, R. M. , Sierra, H. N. M. , Neves, J. W. C. , Frabasile, L. , Chieia, M. A. T. , & Oliveira, A. S. B. ((2017) ). Relationship between effectiveness of cough peak flow and maximum phonation time in patients with motor neuron disease [Conference Abstract]. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration, 18: , 291. https://doi.org/10.1080/21678421.2017.1374620/005 |
[31] | Ohno, T. , Tanaka, N. , Fujimori, M. , Okamoto, K. , Hagiwara, S. , Hojo, K. , Shigematsu, T. , Sugi, T. , Kanazawa, H. , Kunieda, K. , & Fujishima, I. ((2022) ). Cough-Inducing Method Using a Tartaric Acid Nebulizer for Patients with Silent Aspiration. Dysphagia, 37: (3), 629–635. https://doi.org/10.1007/s00455-021-10313-4 . |
[32] | Page, M. J. , McKenzie, J. E. , Bossuyt, P. M. , Boutron, I. , Hoffmann, T. C. , Mulrow, C. D. , Shamseer, L. , Tetzlaff, J. M. , Akl, E. A. , Brennan, S. E. , Chou, R. , Glanville, J. , Grimshaw, J. M. , Hróbjartsson, A. , Lalu, M. M. , Li, T. , Loder, E. W. , Mayo-Wilson, E. , McDonald, S. , & McGuinness, L. A. ((2021) ). The PRISMA statement: An updated guideline for reporting systematic reviews. British Medical Journal, 372: (71), 2020. https://doi.org/10.1136/bmj.n71 . |
[33] | Plowman, E. , Tabor, L. , Robison, R. , & Wymer, J. ((2016) ). Delineating mechanisms of dysphagia in ALS [Conference Abstract]. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration, 17: , 33. https://doi.org/10.1080/21678421.2016.1231971/0046 . |
[34] | Rosenbek, J. C. , Robbins, J. A. , Roecker, E. B. , Coyle, J. L. , & Wood, J. L. ((1996) ). A penetration- aspiration scale. Dysphagia, 11: (2), 93–98. https://doi.org/10.1007/BF00417897 |
[35] | Sartor, M. M. , Guillen-Solà, A. , Ramirez-Fuentes, C. , Duarte, E. , & Marco, E. ((2017) ). Peak expiratory cough flow and respiratory muscle function in acute stroke patients. European Respiratory Journal, 50: (suppl 61), PA3696. https://doi.org/10.1183/1393003.congress-2017.PA3696 |
[36] | Scherer, R. W. , & Saldanha, I. J. ((2019) ). How should systematic reviewers handle conference abstracts? A view from the trenches. Systematic Reviews, 8: (1), 264. https://doi.org/10.1186/s13643-019-1188-0 |
[37] | Seidl, R. O. , Nusser-Müller-Busch, R. , Westhofen, M. , & Ernst, A. ((2008) ). Oropharyngeal findings of endoscopic examination in swallowing disorders of neurological origin. European Archives of Oto-Rhino-Laryngology, 265: (8), 963–970. https://doi.org/10.1007/s00405-007-0559-7 |
[38] | Shea, B. J. , Reeves, B. C. , Wells, G. , Thuku, M. , Hamel, C. , Moran, J. , Moher, D. , Tugwell, P. , Welch, V. , Kristjansson, E. , & Henry, D. A. ((2017) ). AMSTAR: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. British Medical Journal, 358: (8122), j4008. https://doi.org/10.1136/bmj.j4008 |
[39] | Sohn, D. , Park, G. Y. , Koo, H. , Jang, Y. , Han, Y. , & Im, S. ((2018) ). Determining Peak Cough Flow Cutoff Values to Predict Aspiration Pneumonia Among Patients With Dysphagia Using the Citric Acid Reflexive Cough Test. Archives of physical medicine and rehabilitation, 99: (12), e1. https://doi.org/10.1016/j.apmr.2018.06.015 |
[40] | Tabor-Gray, L. C. , Plowman, E. K. , & Robison, R. ((2017) ). Swallowing impairment profiles in amyotrophic lateral sclerosis [Conference Abstract]. Dysphagia, 32: (1), 160. https://doi.org/10.1007/s00455-016-9766-y |
[41] | Tabor-Gray, L. , Vasilopoulos, T. , Wheeler-Hegland, K. , Wymer, J. , & Plowman, E. K. ((2021) ). Reflexive Airway Sensorimotor Responses in Individuals with Amyotrophic Lateral Sclerosis. Dysphagia, 36: (4), 574–582. https://doi.org/10.1007/s00455-020-10171-6 |
[42] | Troche, M. S. , Brandimore, A. E. , Godoy, J. , & Hegland, K. W. ((2014) ). A framework for understanding shared substrates of airway protection. Journal of Applied Oral Science, 22: (4), 251–260. https://doi.org/10.1590/1678-775720140132 |
[43] | University of Canberra. ((2018) ). UC Library Guides: Evidence-Based Practice in Health: PICO Framework and the Question Statement. Libguides.com. https://canberra.libguides.com/c.php?g=599346&p=4149722 |
[44] | Wallace, E. , Macrae, P. , & Huckabee, M. L. ((2018) ). How strong is strong enough to clear aspiration? [Conference Abstract]. Dysphagia, 33: (4), 563–564. https://doi.org/10.1007/s00455-018-9900-0 |
[45] | Wallace, E. , Macrae, P. , & Huckabee, M.-L. ((2021) ). Objective measurement of acoustic intensity of coughing for clearance of penetration and aspiration on video-fluoroscopy. International Journal of Speech-language Pathology, 23: (3), 313–320. https://doi.org/10.1080/17549507.2020.1784280 |
[46] | Wolf, C. , & Meiners, T. H. ((2003) ). Dysphagia in patients with acute cervical spinal cord injury. Spinal Cord, 41: (6), 347–353. https://doi.org/10.1038/sj.sc.3101440 |
[47] | Wu, C. H. , Hsiao, T. Y. , Chen, J. C. , Chang, Y. C. , & Lee, S. Y. ((1997) ). Evaluation of swallowing safety with fiberoptic endoscope: Comparison with videofluoroscopic technique. The Laryngoscope, 396–401. https://doi.org/10.1097/00005537-199703000-00023 |
[48] | York, J. D. , Colsky, J. , Croft, K. , Segalewitz, T. , Machuca, T. , DiBiase, L. , Anderson, A. , & Plowman, E. K. ((2022) ). Dysphagia in Lung Transplant Recipients: Prevalence, Risk Factors, and Health-Related Outcomes [Conference Abstract]. Dysphagia, 37: (4), 1080. https://doi.org/10.1007/s00455-021-10366-5 |
[49] | Yu, S. C. , Liu, C. Y. , Yu, D. K. , Wu, B. J. , & Chang, T. J. ((2009) ). Dysphagia in geriatric schizophrenic patients – A fiberoptic endoscopic examination of swallowing survey [Conference Abstract]. American Journal of Geriatric Psychiatry, 17: , A91. https://doi.org/10.1097/01.JGP.0000346964.46544.ec . |



