The prevalence and nature of communication and swallowing difficulties among adults with long-COVID
Abstract
BACKGROUND:
Long-COVID is an illness which can be experienced after contracting COVID-19, which has affected millions worldwide to date. Long-COVID is characterised by symptoms of COVID-19 which persist 12 weeks post initial onset of the virus and cannot be attributed to a pre-existing diagnosis. In the acute phase of COVID-19, swallowing and communication difficulties are common, however, to date, no studies have investigated the specific effects of Long-COVID on communication and swallowing.
OBJECTIVE:
The aim of this study was to investigate the prevalence, nature, and severity of communication and swallowing difficulties in adults with Long-COVID.
METHODS:
This online cross-sectional design survey was hosted via Qualtrics. Adults living with Long-COVID were recruited via online social media to complete a 16-item anonymous survey regarding the prevalence, nature, and severity of communication and swallowing difficulties associated with Long-COVID. The data was quantitatively analyzed using SPSS, with thematic analysis used for qualitative data.
RESULTS:
108 participants completed the survey. 79 of these individuals were eligible for inclusion in analysis, with 96.67% reporting communication difficulties, and 73.42% reporting swallowing difficulties as a result of Long-COVID. The nature of the difficulties experienced by adults with Long-COVID varied. The majority of the participants found their difficulties to be moderate in severity.
CONCLUSIONS:
There is a high prevalence of communication and swallowing difficulties among adults with Long-COVID, which vary in nature and severity. The high prevalence of communication and swallowing difficulties experienced by individuals with Long-COVID indicates the need for further research into the MDT identification and management of these difficulties, with particular involvement of SLTs in care provision and research, to promote well-being and recovery where possible.
1Introduction
Coronavirus disease (COVID-19) is an infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS- CoV-2 virus) (World Health Organisation, 2022). A systematic review found that around one third of all people infected with the COVID-19 virus are asymptomatic (Oran & Topol, 2021), however, common symptoms for those who experience them include shortness of breath, chest pain or pressure, high temperature, confusion and loss of appetite, amongst others (HSE, 2022). Although approximately 15% of those infected will become seriously ill and require medical attention, most people who are symptomatic experience mild-moderate respiratory illness and recover without requiring special treatment within several weeks (World Health Organization, 2022).
According to the National Institute for Health and Care Excellence (2022), Long- COVID is a condition in which the symptoms that develop during or after COVID-19 infection continue for longer than twelve weeks and cannot be explained by an alternative diagnosis. It typically manifests as overlapping clusters of symptoms that can fluctuate and change over time and impact any system in the body (Shah et al., 2021). Although approximately 80% of hospitalised patients with COVID-19 report symptoms persisting months after the initial onset of the infection (Carfì et al., 2020; Arnold et al., 2020), there is also evidence that shows that Long-COVID is prevalent among people who presented with mild cases of COVID-19 who did not require hospitalisation (van Kessel et al., 2021). Long- COVID is reported to impact on cardiovascular, pulmonary, gastrointestinal and neuropsychiatric systems (Mehandru and Merad, 2022), with commonly researched symptoms including persistent fatigue, anxiety/depression, tachycardia/palpitations, chest pain, insomnia/sleep disorders, cough, shortness of breath, fatigue, muscle aches and loss of smell (NHS, 2022; Banda et al., 2020; Huang at al., 2021). However, in addition to these highly researched symptoms, patients have also anecdotally reported additional Long-COVID associated symptoms which have not received research attention, despite being potentially debilitating to patient recovery, for example: Long-COVID related communication and swallowing difficulties.
Communication difficulties within the acute phases of infection have received recent attention within the literature, with reports referencing dysphonia related to respiratory illness and extubation, and confusion associated with brain fog or word finding difficulties (Archer at al., 2021; Cantarella et al., 2021; Daroische et al., 2021; Neevel et al., 2021; Regan et al., 2021; HSE, 2022; Lechien et al., 2022; Priftis, 2022). With regards to Long-COVID, few research studies have documented patient reports of dysphonia, aphonia, difficulty thinking, inability to concentrate and brain fog (Aiyegbusi et al., 2021; Verma et al., 2022). Despite few research studies being available, these issues, especially brain fog, have extensively been discussed within patient forums and in the popular media, indicating that these are patient-prioritized issues. Even though these patient reports exist, research has not yet established the prevalence, severity, or impact of these Long-COVID associated communication difficulties, resulting in a lack of management options for patients living with these challenges, and potential limitations in the individual’s ability to return to work, engage socially, or advocate for and access other treatment modalities.
Additionally, research has established swallowing difficulties as a common symptom of hospitalized patients during the acute phases of severe COVID-19 infection (Archer at al., 2021; Lima et al., 2020; Brugliera et al., 2020). This acute phase dysphagia has commonly been associated with the need for prolonged intubation and tracheostomies in the case of severe respiratory distress or the presence of pre-existing dysphagia or neurologic dysfunction (Archer at al., 2021; Lima et al., 2020; Brugliera et al., 2020; Regan et al., 2021). However, despite this research attention at the acute phase, there has been minimal investigation of dysphagia within the context of Long-COVID, and the typical symptom profile, prevalence figures, severity estimates, or impact details at the Long-COVID stage has not been established. If adults with Long-COVID are presenting with unmanaged dysphagia, this could induce other difficulties such as choking, respiratory complications such as aspiration pneumonia, or intake issues leading to weight loss and/or malnutrition. Therefore, given these potentially adverse and debilitating consequences, it is essential that further research and care developments in this field are pursued.
As is evident, there is currently limited research in relation to Long-COVID and the nature, prevalence, or severity of potentially associated communication and swallowing difficulties. As discussed, there is minimal evidence regarding Long-COVID and communication difficulties, despite patient accounts suggesting that these symptoms can develop and persist long after acute COVID-19 infections. In addition, dysphagia has also been widely discussed within acute COVID-19 literature, however, this research has not carried over into the Long-COVID research, with potential impact on patient management and outcomes. Therefore, the overall aim of this study was to survey the prevalence and nature of communication and swallowing difficulties among adults with Long-COVID, in order to establish the extent, nature, and severity of these issues with the view to aid the planning and prioritization of services and care provision in the future.
2Methods
This mixed-methods cross-sectional anonymous survey was conducted in accordance with the CROSS guidelines (Sharma et al., 2021) and disseminated online using the Qualtrics platform. This study received ethical approval from the Research Ethics Committee of the School of Linguistic, Speech & Communication Sciences (TT55).
Individuals were eligible for participation if they were adults (aged 18 years and older) who were living with either self-reported or clinically diagnosed Long-COVID, and who had not had a diagnosis of dysphagia or communication difficulties prior to having COVID-19. Participants also had to have a sufficient command of English to adequately answer the survey questions.
Individuals living with Long-COVID were recruited for participation via single stage convenience snowball sampling between 26/09/2022 and 08/11/2022. The researcher initially approached administrators of international Facebook and Twitter support groups/pages for those living with Long-COVID via a standardized gatekeeper letter. If the administrator agreed to act as a gatekeeper, they then shared the survey link within their group/on their page and members/followers then had the option of whether they would like to participate in the study or not.
The survey was initially piloted with 3 speech and language therapists (SLTs), one of whom was living with long COVID, and a layperson. Preliminary suggestions were given around the clarity of the question phrasing and changes were made based on this feedback. The first question of the final survey related to provision of information pertaining to the study and the collection of informed consent for participation. The subsequent 16 questions were both closed- and open-ended questions which investigated participant demographics, the presence of communication and swallowing difficulties associated with Long-COVID, as documented in the available literature, and the severity of these issues (see Supplementary Material). Listed communication difficulties included: word finding difficulties; difficulty following complex conversations; taking more time than usual to follow directions; speech not as clear as it used to be; voice changes (weak, quiet, rough, hoarse, pitch changes); and “other” (for the participant to specify). Swallowing difficulties were listed as: extra effort swallowing liquids; extra effort swallowing solids; extra effort swallowing tablets; painful swallow; choking episodes when eating/drinking; dry mouth; more than 1 chest infection in the last year; regurgitation; and “other” (for the participant to specify).
Descriptive and correlational analyses were conducted using SPSS 27 (Corp, 2019) to quantitatively analyze the prevalence and severity data. Qualitative data from open-ended questions were thematically analyzed as per Braun and Clarke’s framework (2006).
3Results
Overall, 108 participants responded to the survey, with 79 individuals living with either self- or clinically-diagnosed Long-COVID ultimately being eligible for inclusion and analysis (n = 19 did not fully complete all questions; n = 10 reported having experienced communication and/or swallowing difficulties prior to having COVID-19). Locations of participants included: the United Kingdom (n = 35, 44.3%), the United States of America (n = 18, 22.78%), New Zealand (n = 8, 8.99%), Ireland (n = 6, 7.6%), Canada (n = 5, 6.32%), Switzerland (n = 3, 3.37%), Australia (n = 1, 1.27%), India (n = 1,1.27%) and Luxembourg (n = 1, 1.27%). Of the 79 respondents, 1 declined to answer (n = 1, 1.27%).
The number of months post COVID-19 for the sample ranged from four months to thirty three months, the average months post COVID-19 for the sample was 16.87 (SD 10.87) and the median number of months was 13. Only 8% (n = 6) of the participants had been hospitalised due to their experience of COVID-19.
The mean age of participants was 40 years of age (range: 18-84). The majority of participants identified as female (n = 55, 69.62), with 12 identifying as male (n = 12, 15.19%), 7 identified as non-binary/third gender (n = 7, 8.86%), 4 declining to provide an answer (n = 4, 5.06%), and 1 respondent preferring not to say (n = 1, 1.27%).
3.1Communication difficulties
Most adults with Long-COVID reported communication difficulties (n = 76, 96.2%), with distribution across the gender spectrum (female = 96.36%; male = 91.67%; non-binary/third gender = 100%). The most common presentations of communication difficulties reported by participants were word finding difficulties (n = 69, 87.34%), difficulty following complex conversations (n = 53, 67.09%), and taking more time than usual to follow directions (n = 51, 64.56%) (Figure 1).
A quarter of all participants (n = 20; 25.31%) reported experiencing Long-COVID-associated communication difficulties other than those listed in the survey (Table 1).
Fig. 1
Nature of communication difficulties reported by participants.
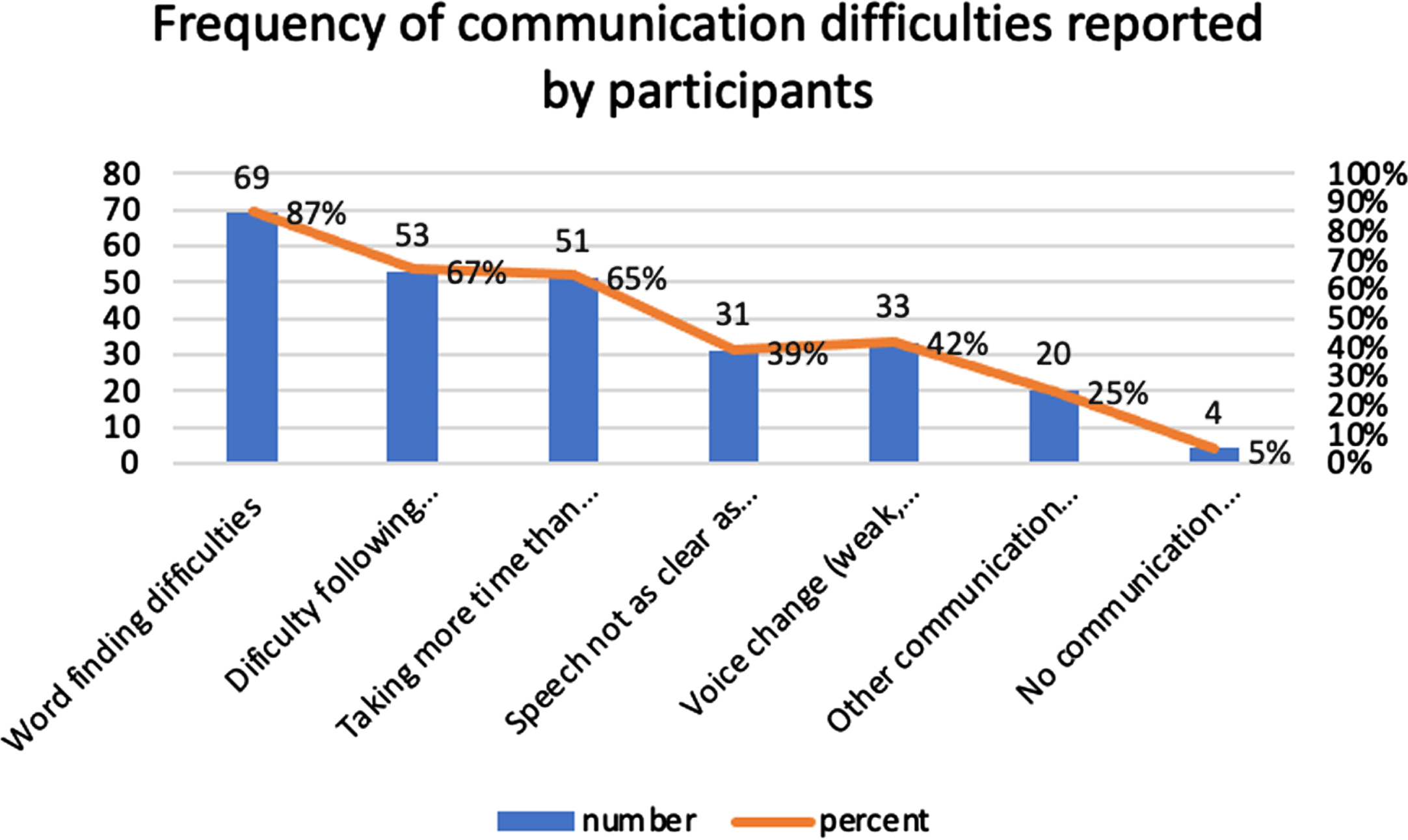
Table 1
Qualitative descriptions of participants’ communication difficulties
| Nature of difficulty | N (%) respondents who experienced the difficulty | Examples |
| Fluency difficulties | 5 (6.33%) | “stutter”, “Terrible stuttering, almost unable to speak for weeks at a time. At other times, completely unable to speak for 5-10 min”, “Stuttering, slurring, tics” |
| Word finding difficulties | 4 (5.06%) | “Muddling up words”, “words coming slowly, speaking hurts my chest”, “I get mixed up wit my words daily” |
| Reading and writing difficulties | 4 (5.06%) | “unable to read or write”, “Reading, writing, understanding audio”, “Worse dyslexia“ |
| Other difficulties | 4 (5.06%) | “hearing issues”, “My tongue feels clumsy.”, “brain fog” |
| Cognitive- communication difficulties | 3 (3.8%) | “cognitive communication difficulties”, “Lose track of what I am saying due to short term memory and processing issues” |
Respondents were asked to rate communication difficulties experienced as a result of Long- COVID on a six-point Likert scale ranging from 0 (no difficulties) to 5 (severe difficulties). Of the 79 participants, 72 responded to this question (Figure 2). The mean severity of communication difficulties was 3.81 (moderate severity).
Fig. 2
Severity of communication difficulties reported by participants.
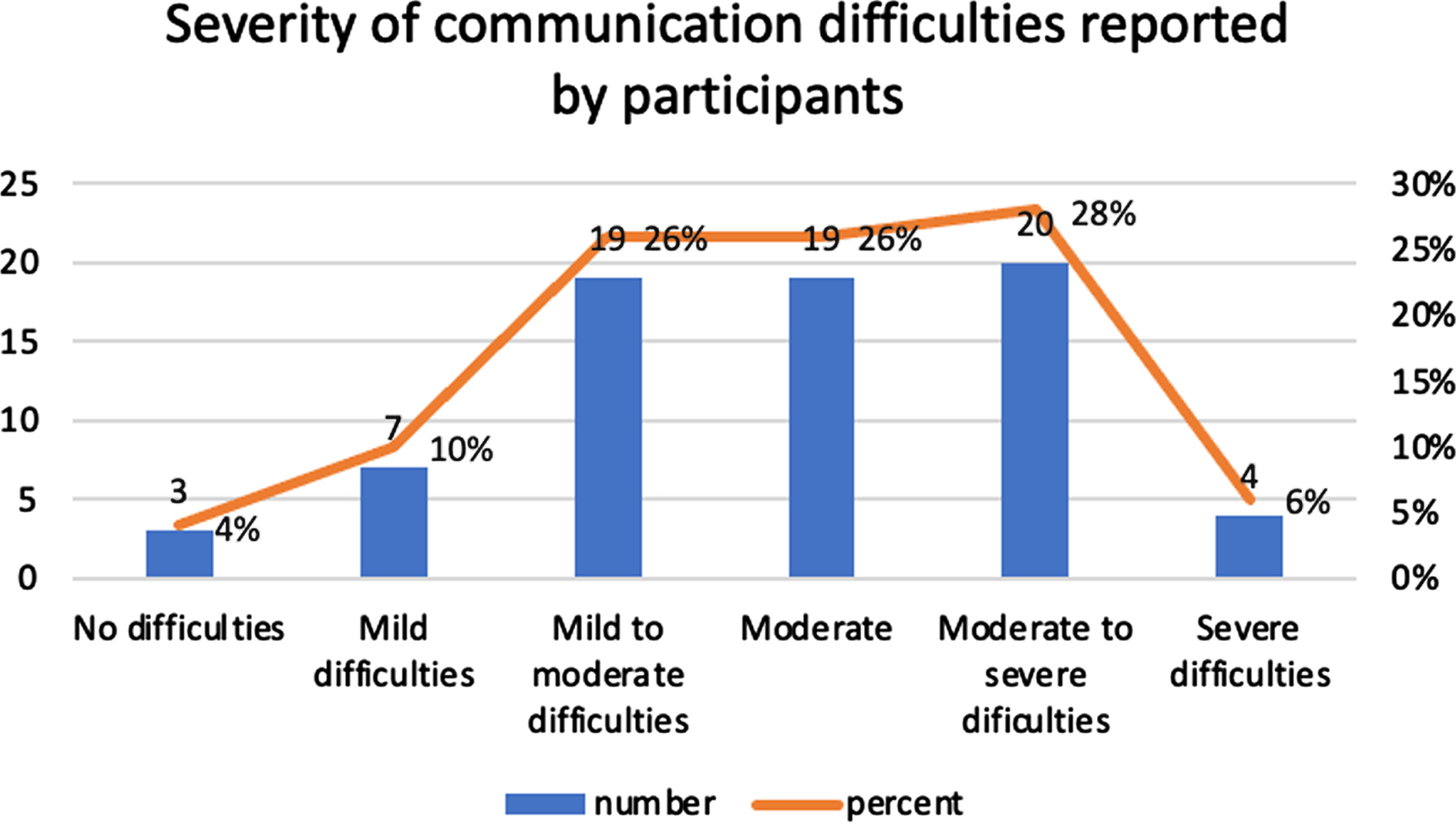
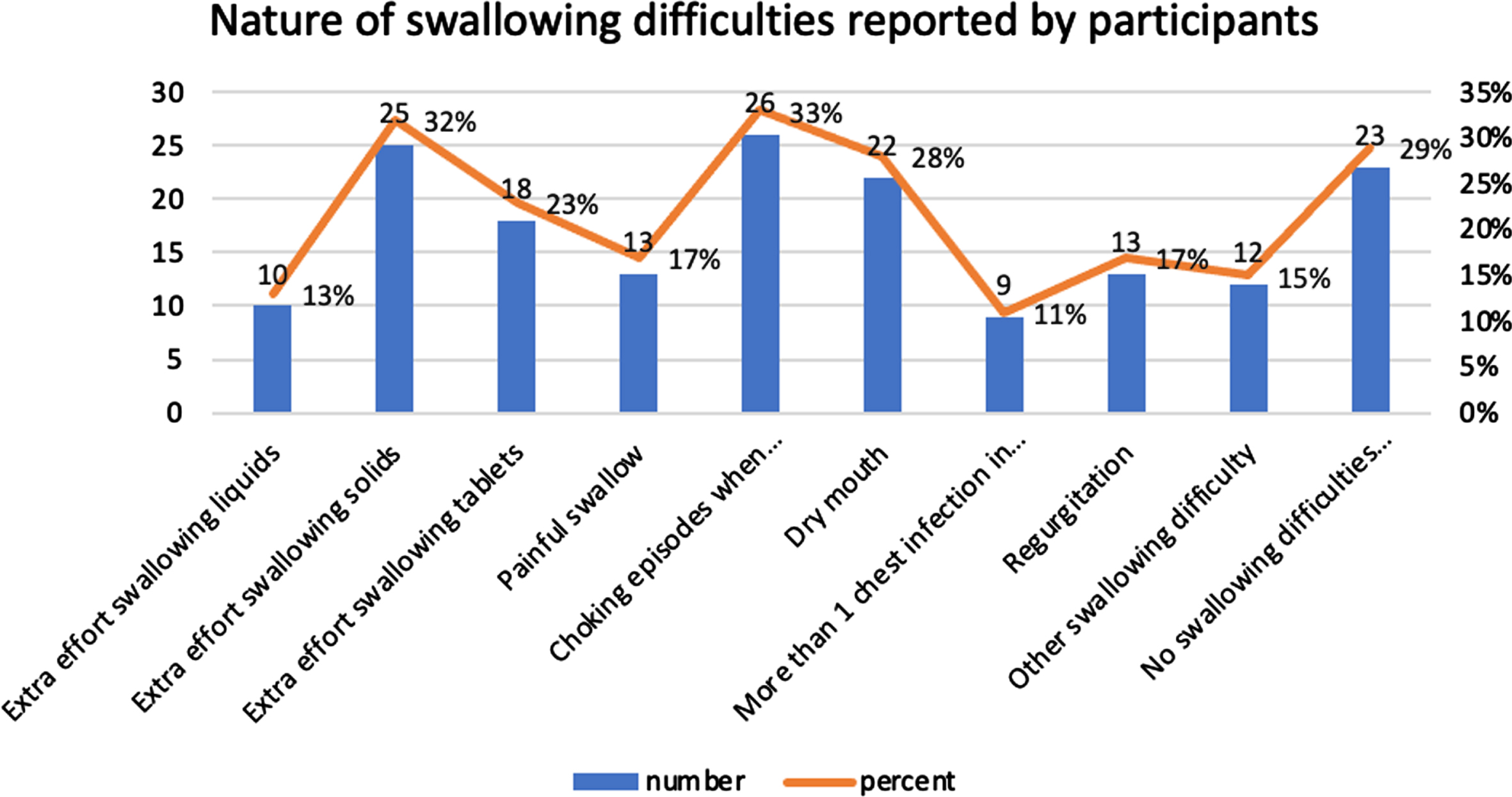
Fig. 3
Nature of swallowing difficulties reported by participants.
One-way ANOVAs were conducted, with no significant differences found between: age and severity of communication difficulties (F(6,65)=.642, p = .696); gender identity and severity (F(3,64)=1.26, p = .295); or participant location and severity (F(6,64)=1.15, p = .344).
3.2Swallowing difficulties
Most participants reported Long-COVID related swallowing difficulties (n = 58, 73.42%), with distribution across the gender spectrum (female = 72.73%; male = 75%; non-binary/third gender = 71%).
The most common Long-COVID-related swallowing difficulties reported were choking episodes when eating and drinking (n = 26, 32.91%), extra effort swallowing solids (n = 25, 31.65%) and dry mouth (n = 22, 27.85%).
A cohort of participants (n = 12, 15.18%) reported experiencing Long-COVID-associated swallowing difficulties other than those listed in the survey (Table 2).
Table 2
Qualitative descriptions of participants’ swallowing difficulties
| Nature of difficulty | N (%) respondents who experienced the difficulty | Examples |
| Other difficulties | 3 (3.8%) | “Laryngeal penetration due to cognitive dysphagia,” “Sore throats, recurring,” “Reflux including vomit in the mouth.” |
| Sensation of something caught in throat | 2 (2.53%) | “Frequent feeling of “something caught in throat/windpipe feeling after eating or drinking”, “Food getting stuck in my throat. I don’t always feel it straight away.” |
| Impaired swallow reflex | 2 (2.53%) | “Almost as if I forget to swallow or breathe,” “I go to swallow (just saliva) but the reflex isn’t there” |
| Breathing difficulties | 2 (2.53%) | “Almost as if I forget to swallow or breathe,” “Breathing spasms when swallowing.” |
| Difficulty swallowing saliva | n=2, 2.53% | “My cough often seemed to be me choking on saliva,” “I don’t have issues swallowing while eating. But even just swallowing saliva feels like the muscles won’t move no matter how I will them.” |
| Difficulty swallowing food | n=2, 2.53% | “General swallowing food, liquid is much easier,” “Serious choking episode while eating sift chicken. Heimlich required. Ongoing difficulty with hard and chewy food. Taking soft moist food. Difficulty chewing. Fatigue with chewing. Hard to swallow.” |
Participants also rated the severities of these swallowing difficulties. Of the 79 participants that were included in the sample, 53 responded to this question (Figure 4). The mean severity of communication difficulties was 3.81 (moderate severity).
Fig. 4
Severity of swallowing difficulties reported by participants.
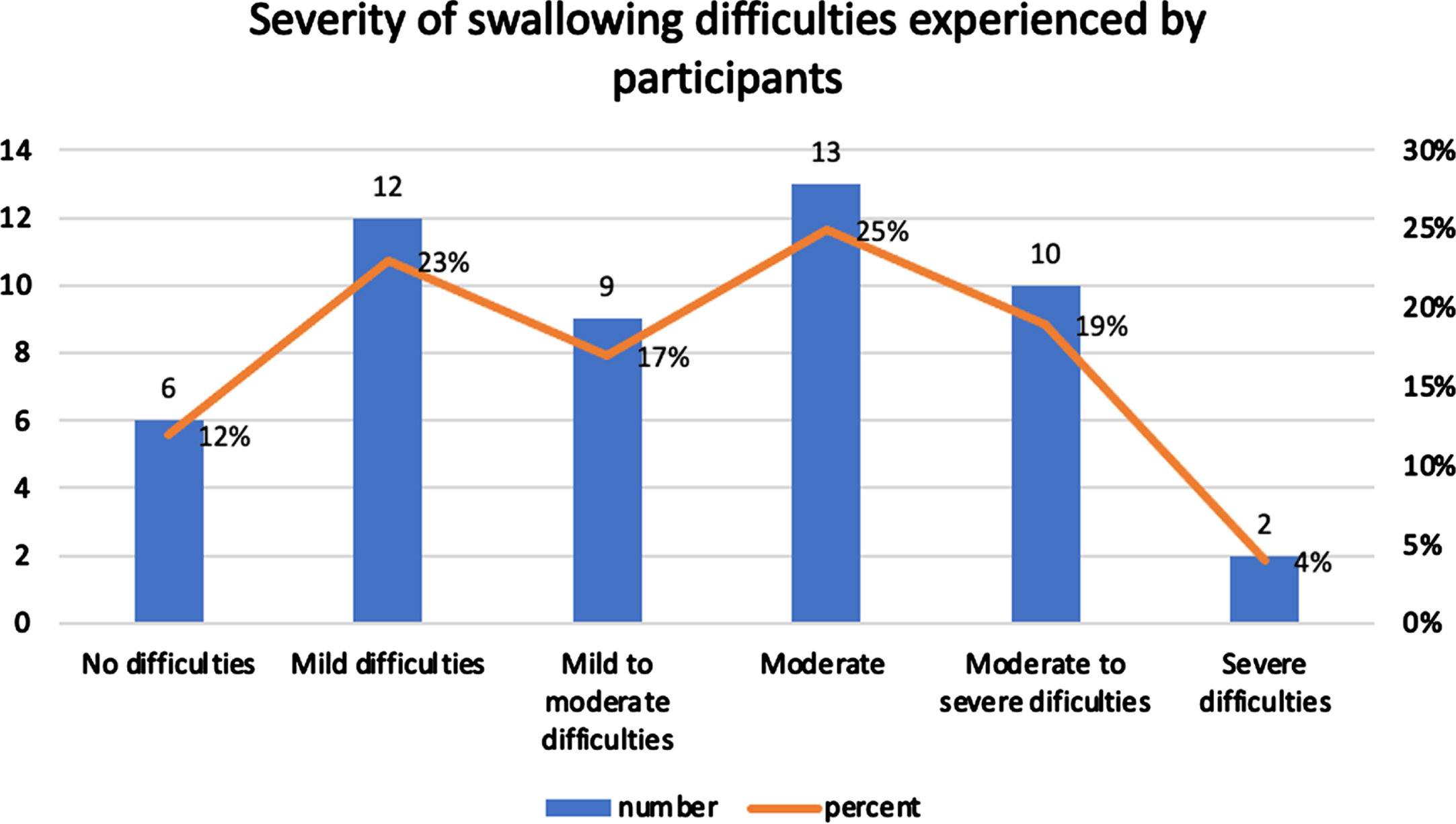
One-way ANOVAs were conducted, with no significant differences found between: age and severity of swallowing difficulties (F(6,46)=1.48, p = .205); gender identity and severity (F(6,45)=1.48, p = .205); or participant location and severity (F(3,46)=1.24, p = .629).
4Discussion
This study provided new information regarding the prevalence, nature, and severity of communication and swallowing difficulties among adults with Long-COVID.
4.1Communication difficulties
Since the beginning of the pandemic, there has been acknowledgement that communication difficulties can be experienced during the acute infectious phase of COVID-19, with symptoms often directly related to known and immediate effects of the illness (eg: dysphonia due to respiratory concerns or brain fog due to delirium) (Archer at al., 2021; Cantarella et al., 2021; Daroische et al., 2021; Neevel et al., 2021; Regan et al., 2021; HSE, 2022; Lechien et al., 2022; Priftis, 2022). These communication difficulties can reduce access to treatment, impair well-being and quality of life during the acute phases of infection, and impede or delay overall recovery. However, exploration of the resolution, persistence, or evolution of these symptoms beyond the acute infectious stage is limited, and as such, very little is known about how best to support individuals living with Long-COVID related communication difficulties within an MDT structure.
Although there is limited available research in this field or current acknowledgement of the potential for ongoing communication difficulties post-infection, nearly all respondents here (96.2%) reported experiencing communication difficulties which they had not experienced prior to Long-COVID, thus emphasising the high level of perceived difficulties in this sample. Elaborating on existing knowledge (Daher et al., 2020; Davis et al., 2021; Cirulli et al., 2020; Garrigues et al., 2020; Goërtz et al., 2020; Sudre et al., 2021; Halpin et al., 2021; Aiyegbusi et al., 2021), this study highlighted a broad range of communication problems that adults with Long- COVID experienced that have not previously been discussed within the literature. These symptoms persisted beyond the acute phase of infection and were self-reported on average to be moderately severe, including word finding difficulties, which 87% of participants experienced, followed by difficulty following complex conversations, taking more time than usual to follow directions and speech not being as clear as it used to be. Less common symptoms that were reported by participants included fluency difficulties, reading and writing difficulties and cognitive communication difficulties. These findings suggest that a myriad of previously under-explored receptive and expressive communication difficulties may persist among those living with Long-COVID. This is notable as the long-term impact of acute-COVID-related communication difficulties has not been fully considered as of yet. While communication difficulties may cause issues in accessing services or communicating care needs in the acute infection stage, they can have further devastating impact if they persist beyond this period, including: the ability to return to work, engage with premorbid family and social roles, and advocate for and access therapies and supports required to help them to live well with the effects of Long-COVID.
Long-COVID related MDT services remain sparse, with ongoing knowledge gaps, geographical disparities in care provision, and lack of consistent guidance from clinicians. Those living with Long-COVID in general have reported multiple barriers in accessing specialised Long-COVID care (Macpherson et al., 2022). Additionally, it is already acknowledged that those living with other communication difficulties (eg: post-stroke aphasia) can struggle to access reliable resources and effective healthcare guidance, despite efforts to make care-seeking more inclusive and supportive (Hinckley, Hasselkus & Ganzfried, 2013). Therefore, both the scarcity of available Long-COVID information or services and the self-reported communication difficulties of this group may combine to amplify inequities in care provision. As such, it is essential that a concerted, evidence-based, and multi-disciplinary approach is taken to research and service planning in the future to ensure that patient-reported issues are prioritised. It is suggested here that as the SLT is often involved in care provision during acute phases of infection (eg: in management of communication concerns such as dysphonia or delirium) (Freitas, Zica & Albuquerque, 2020), there may also be a role for them in the ongoing identification and management of these issues after the initial infection has resolved. SLTs may support individuals with Long-COVID to build on residual communication strengths, while addressing post-COVID cognitive-linguistic difficulties, thus allowing them to access other rehabilitative and supportive services (eg: physiotherapy, occupational therapy, or psychology), with the view to work as a team in facilitating real-life functioning and a return to their “typical” pre-COVID lifestyle where possible.
4.2Swallowing difficulties
This study found that 73.42% of respondents self-reported experiencing on average moderately severe swallowing difficulties which they associated with the onset of their Long-COVID. Acute-COVID-related swallowing difficulties are already acknowledged in the literature (Archer at al., 2021; Lima et al., 2020; Brugliera et al., 2020), given the interconnectedness of the respiratory, neurological, and gastro-intestional systems (Martin-Harris, 2006). Research commonly focuses on airway management and immediate safety concerns within this cohort, given their existing respiratory compromise and potential for further deconditioning. However, like the communication difficulties discussed above, specifics regarding how these issues resolve, develop, or evolve beyond the acute phase is limited. Therefore, this research here suggests for the first time the varied nature of Long-COVID-associated swallowing difficulties. Data here suggests that the most frequently experienced swallowing difficulties include choking episodes, extra effort swallowing solids, and dry mouth. These difficulties were reported in addition to extra effort swallowing tablets and liquids, pain on swallowing, having had more than one chest infection in the last year, and regurgitation. These issues elaborate on the known immediate airway concerns in the acute phase to a description of more long-term oropharyngeal and oesophageal problems which may further impair nutrition, hydration, and overall well-being and recovery. Not only would these chronic difficulties impact a person’s quality of life and ability to engage with activities of daily living, they also increase the risk of morbidity and mortality amongst adults living with Long-COVID. Although the definitive cause of these issues is currently unknown, it is hypothesised that these wide ranging difficulties could be related to lasting impact of pulmonary, digestive, or neurological damage and/or deconditioning post-infection.
As chronic dysphagia can lead to health implications including dehydration, malnutrition, aspiration pneumonia, choking, compromised general health and, in severe cases, death (American Speech-Language-Hearing Association, 2022), it is essential that future research seeks to further understand the causation, symptom profile, impact, and potential management of Long-COVID associated dysphagia in order to ensure that adequate services are available to support patients living with these concerns. Furthermore, given the SLTs knowledge and expertise in the identification and management of dysphagia, it is essential that they take an integral role in this future research and MDT management of Long-COVID-related swallowing difficulties in order to support patients and other clinicians in living well and recovering from these issues, where possible.
4.3Limitations
This self-report survey gathered subjective data only. Therefore, future investigations of the presence, nature, and severity of swallowing and communication difficulties amongst this cohort using objective/standardized tools as appropriate would be advised. Further review and refinement of questions within the survey would also be advisable, as data was not gathered as to whether respondents were living with self- or clinically-diagnosed Long-COVID. This potentially limits the reliability of findings, as there may be the potential that respondents may be experiencing illnesses other than Long-COVID. However, it was deemed appropriate to include individuals living with both self- and clinically-diagnosed Long-COVID given the paucity of specialised clinicians or diagnostic services in this field currently. In addition, the sample distribution was somewhat limited, secondary to difficulties with dissemination. The researcher encountered difficulties receiving responses from gatekeepers who were contacted via Facebook. Although 14 Long-COVID Facebook support groups were contacted, the researcher only received permission from one of the groups to post the survey link in the group, yielding a response rate of 7.14% via Facebook. This may have impacted results in that perhaps a skewed cohort responded to the survey link. In addition, although dissemination via social media was the most efficient method of sampling, given movement restrictions, this may have skewed the sample towards only socially active individuals partaking. As such, broader dissemination would be advised in future to ensure sample distribution.
5Conclusions
This study established that there is a high prevalence of self-reported communication and swallowing difficulties among adults living with Long-COVID, across age brackets, genders and geographical locations. The study found that although the symptoms of both communication and swallowing difficulties varied in nature and severity, most participants reported their difficulties to be moderately severe, with many respondents commenting on the impact of the difficulties on wider domains of their functioning and life. This highlights the need for greater involvement of SLTs in future MDT research into and care provision for people living with these conditions, in order to optimize available management options and the ability of patients to live well with communication and swallowing difficulties associated with Long-COVID.
Conflict of interest
Authors have no conflict of interest to declare.
References
1 | Aiyegbusi, O. L. , Hughes, S. E. , Turner, G. , Rivera, S. C. , McMullan, C. , Chandan, J. S. , Haroon, S. , Price, G. , Davies, E. H. , Nirantharakumar, K. , Sapey, E. , Calvert, M. J. TLC Study Group ((2021) ). Symptoms, complications and management of long COVID: a review. Journal of the Royal Society of Medicine, 114: (9), 428–442. https://doi.org/10.1177/01410768211032850 |
2 | Archer, S. K. , Iezzi, C. M. , Gilpin, L. ((2021) ). Swallowing and voice outcomes in patients hospitalized with COVID-19: An observational cohort study. Archives of Physical Medicine and Rehabilitation, 102: (6), 1084–1090. https://doi.org/10.1016/j.apmr.2021.01.063 |
3 | Arnold, D. T. , Hamilton, F.W. , Milne, A. , Morley, A. , Viner, J. , Attwood, M. , Noel, A. , Gunning, S. , Hatrick, J. , Hamilton, S. , Elvers, K. T. , Hyams, C. , Bibby, A. , Moran, E. , Adamali, H. , Dodd, J. , Maskell, N. A. , Barratt, S. (2020). Patient outcomes after hospitalisation with covid-19 and implications for follow-up; results from a prospective UK cohort. https://doi.org/10.1101/2020.08.12.20173526 |
4 | Banda, J. M. , Singh, G. V. , Alser, O. H. , Prieto-Alhambra, D. (2020). Long-term patient-reported symptoms of COVID-19: An analysis of social media data. https://doi.org/10.1101/2020.07.29.20164418 |
5 | Braun, V. , Clarke, V. ((2006) ). Using thematic analysis in psychology. Qual Res Psychol., 3: (2), 77–101. |
6 | Brugliera, L. , Spina, A. , Castellazzi, P. , Cimino, P. , Arcuri, P. , Negro, A. , Houdayer, E. , Alemanno, F. , Giordani, A. , Mortini, P. , Iannaccone, S. ((2020) ). Nutritional management of COVID-19 patients in a rehabilitation unit. European Journal of Clinical Nutrition, 74: (6), 860–863. https://doi.org/10.1038/s41430-020-0664-x |
7 | Cantarella, G. , Aldè, M. , Consonni, D. , Zuccotti, G. , Berardino,F. D. , Barozzi, S. , Bertoli, S. , Battezzati, A. , Zanetti, D. , Pignataro, L. ((2021) ). Prevalence of Dysphonia in Non hospitalized Patients with COVID-19 in Lombardy, the Italian Epicenter of the Pandemic. Journal of Voice : Official Journal of the Voice Foundation, S0892-1997: (21), 00108–9. Advance online publication. https://doi.org/10.1016/j.jvoice.2021.03.009. |
8 | Carfì, A. , Bernabei, R. , Landi, F. ((2020) ). Persistent symptoms in patients after acute COVID-19. JAMA, 324: (6), 603. https://doi.org/10.1001/jama.2020.12603. |
9 | Cirulli, E. T. , Schiabor Barrett, K. M. , Riffle, S. , Bolze, A. , Neveux, I. , Dabe, S. , Washington, N. L. (2020). Long-term COVID-19 symptoms in a large unselected population. medrxiv, 2020-10. |
10 | Daher, A. , Balfanz, P. , Cornelissen, C. , Müller, A. , Bergs, I. , Marx, N. , Müller, T. ((2020) ). Follow up of patients with severe coronavirus disease 2019 (COVID-19): Pulmonary and extrapulmonary disease sequelae. Respiratory Medicine, 174: , 106197. |
11 | Daroische, R. , Hemminghyth, M. S. , Eilertsen, T. H. , Breitve, M. H. , Chwiszczuk, L. J. ((2021) ). Cognitive Impairment After COVID-19-A Review on Objective Test Data. Frontiers in Neurology, 12: , 699582. https://doi.org/10.3389/fneur.2021.699582. |
12 | Davis, H. E. , Assaf, G. S. , McCorkell, L. , Wei, H. , Low, R. J. , Re’em, Y. , Akrami. , A. (2021). Characterizing longCOVID in an international cohort: 7 months of symptoms and their impact. bioRxiv. Posted April 05. |
13 | Freitas A.S. , Zica G.M. , Albuquerque C. L. D. (2020, June). Coronavirus pandemic (COVID-19): what speech therapists should know. In CoDAS (Vol. 32). Sociedade Brasileira de Fonoaudiologia. |
14 | Garrigues, E. , Janvier, P. , Kherabi, Y. , Le Bot, A. , Hamon, A. , Gouze, H. , Nguyen, Y. ((2020) ). Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. Journal of Infection, 81: (6), e4–e6. |
15 | Goërtz, Y. M. , Van Herck, M. , Delbressine, J. M. , Vaes, A. W. , Meys, R. , Machado, F. V. , Spruit, M. A. ((2020) ). Persistent symptoms 3 months after a SARS-CoV-2 infection: the post-COVID-19 syndrome?. ERJ Open Research, 6: (4). |
16 | Halpin, S. J. , McIvor, C. , Whyatt, G. , Adams, A. , Harvey, O. , McLean, L. , Sivan, M. ((2021) ). Postdischarge symptoms and rehabilitation needs in survivors ofCOVID-19 infection:A cross-sectional evaluation. Journal of Medical Virology, 93: (2), 1013–1022. |
17 | Health Service Executive. (2022). Symptoms of COVID-19. https://www2.hse.ie/conditions/covid19/symptoms/overview/ |
18 | Hinckley, J. J. , Hasselkus, A. , Ganzfried, E. (2013). What people living with aphasia think about the availability of aphasia resources. https://doi.org/10.1044/1058-0360(2013/12-0090) |
19 | Huang, C. , Huang, L. , Wang, Y. , Li, X. , Ren, L. , Gu, X. , Kang, L. , Guo, L. , Liu, M. , Zhou, X. , Luo, J. , Huang, Z. , Tu, S. , Zhao, Y. , Chen, L. , Xu, D. , Li, Y. , Li, C. , Peng, L. , Cao, B. ((2021) ). 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. The Lancet, 397: (10270), 220–232. https://doi.org/10.1016/s0140-6736(20)32656-8 |
20 | Lechien, J. R. , Chiesa-Estomba, C. M. , Cabaraux, P. , Mat, Q. , Huet, K. , Harmegnies, B. , Horoi, M. , Le Bon S. D. , Rodriguez, A. , Dequanter, D. , Hans, S. , Crevier-Buchman, L. , Hochet, B. , Distinguin, L. , Chekkoury-Idrissi, Y. , Circiu, M. , El Afia F. , Barillari, M. R. , Cammaroto, G. , Fakhry, N. , Saussez, S. ((2022) ). Features of Mild-to-Moderate COVID-19 Patients With Dysphonia. Journal of Voice : Official Journal of the Voice Foundation, 36: (2), 249–255. https://doi.org/10.1016/j.jvoice.2020.05.012 |
21 | Lima, M. S. , Sassi, F. C. , Medeiros, G. C. , Ritto, A. P. , Andrade, C. R. (2020). Preliminary results of a clinical study to evaluate the performance and safety of swallowing in critical patients with covid-19. Clinics, 75. https://doi.org/10.6061/clinics/2020/e2021 |
22 | Macpherson, K. , Cooper, K. , Harbour, J. , Mahal, D. , Miller, C. , Nairn, M. ((2022) ). Experiences of living with long COVID and of accessing healthcare services: a qualitative systematic review. BMJ Open, 12: (1), e050979. |
23 | Martin-Harris, B. (2006). Coordination of respiration and swallowing. GI Motility online. |
24 | Mehandru, S. , Merad, M. ((2022) ). Pathological sequelae of long-haul covid. Nature Immunology, 23: (2), 194–202. https://doi.org/10.1038/s41590-021-01104-y |
25 | National Institute for Health and Care Excellence (2020). COVID-19 rapid guideline: managing the long-term effects of COVID-19 | Guidance https://www.nice.org.uk/guidance/ng188 |
26 | National Health Service. (2022). Long-term effects of coronavirus (long COVID). https://www.nhs.uk/conditions/coronavirus-covid-19/long-term-effects-of-coronavirus-long-covid/ |
27 | Neevel, A. J. , Smith, J. D. , Morrison, R. J. , Hogikyan, N. D. , Kupfer, R. A. , Stein, A. P. ((2021) ). Postacute COVID-19 Laryngeal Injury and Dysfunction. OTO Open, 5: (3), 2473974X211041040. https://doi.org/10.1177/2473974X211041040. |
28 | Oran, D. P. , Topol, E. J. ((2021) ). The Proportion of SARS-CoV-2 Infections That Are Asymptomatic : A Systematic Review. Annals of Internal Medicine, 174: (5), 655–662. https://doi.org/10.7326/M20-6976 |
29 | Priftis, K. (2022). Neurolinguistic Deficits and Other Cognitive Disorders in Adults with Severe COVID-19 Infection. In Covid-19 and Speech-Language Pathology (pp. 53-71). Routledge. |
30 | Regan, J. , Walshe, M. , Lavan, S. , Horan, E. , Gillivan Murphy, P. , Healy, A. , Langan, C. , Malherbe, K. , Flynn Murphy, B. , Cremin, M. , Hilton, D. , Cavaliere, J. , Whyte, A. ((2021) ). Post-extubation dysphagia and dysphonia amongst adults with COVID-19 in the Republic of Ireland: A prospective multi-site observational cohort study. Clinical Otolaryngology : Official Journal of ENT-UK; Official Journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery, 46: (6), 1290–1299. https://doi.org/10.1111/coa.13832 |
31 | Shah, W. , Hillman, T. , Playford, E. D. , Hishmeh, L. (2021). Managing the long term effects of covid-19: Summary of nice, sign, and RCGP Rapid Guideline. BMJ. doi:10.1136/bmj.n136 |
32 | Sharma A. , Minh Duc NT. , Luu Lam Thang T. , Nam NH. , Ng SJ. , Abbas KS. , Huy NT. , Marušić A. , Paul CL. , Kwok J. , Karbwang J. , de Waure C. , Drummond FJ. , Kizawa Y. , Taal E. , Vermeulen J. , Lee Dysphagia (Springer) 67 GHM, Gyedu A. , To KG. , Verra ML. , Jacqz-Aigrain EM. , Leclercq WKG. , Salminen ST. , Sherbourne CD. , Mintzes B. , Lozano S. , Tran US. , Matsui M. , Karamouzian M. ((2021) ). A Consensus Based Checklist for Reporting of Survey Studies (CROSS). Journal of General Internal Medicine, 36: , 3179–3187. https://doi.org/10.1007/s11606-021-06737-1. |
33 | Sudre, C. H. , Murray, B. , Varsavsky, T. , Graham, M. S. , Penfold, R. S. , Bowyer, R. C. , Steves, C. J. ((2021) ). Attributes and predictors of long COVID. Nature Medicine, 27: (4), 626–631. |
34 | van Kessel S. A. , Olde Hartman T. C. , Lucassen, P. L. , vanJaarsveld, C. H. ((2021) ). Post-acute and long COVID-19 symptoms in patients with mild diseases: A systematic review. Family Practice, 39: (1), 159–167. https://doi.org/10.1093/fampra/cmab076 |
35 | Verma, H. , Shah, J. , Akhilesh, K. et al. (2022). Patients’ perspective about speech, swallowing and hearing status post-SARS-CoV-2 (COVID-19) recovery: E-survey. Eur Arch Otorhinolaryngol https://doi.org/10.1007/s00405-021-07217-2 |
36 | World Health Organization. (2022). Coronavirus disease (COVID-19). https://www.who.int/health-topics/coronavirus#tab=tab1. |




