Is trans-laryngeal ultrasound (TLUS) an accurate and acceptable tool in the assessment of inducible laryngeal obstruction? A protocol for the ILOTUS: A cross-sectional, two-stage feasibility study
Abstract
BACKGROUND:
Inducible laryngeal obstruction (ILO) describes an inappropriate narrowing of the larynx during breathing in. ILO can lead to several respiratory symptoms and be misidentified and treated as asthma, with associated patient morbidity and healthcare cost. ILO is also known as vocal cord dysfunction, or paradoxical vocal fold movement. The current reference assessment tool for diagnosing ILO is a video-laryngoscopy. However, timely access to specialist diagnostic laryngoscopy services may be challenging, and laryngoscopy may be poorly tolerated.
AIMS:
The aim of this cross-sectional, two-stage feasibility study is to determine whether abnormal vocal fold movements associated with ILO can be adequately visualised using trans-laryngeal ultrasound (TLUS) namely, the ILOTUS study: (ILO assessment via trans- laryngeal ultrasound). The second aim is to compare TLUS with a reference standard diagnostic tool to ascertain whether it may serve as a less invasive screening tool to assess ILO. Participants’ opinions about the acceptability of TLUS will also be gathered and compared with responses to a validated symptom score questionnaire.
METHODS:
In stage one, healthy volunteers (n = 30) will undergo TLUS to assess whether the vocal folds can be visualised,and whether narrowing of the vocal folds can be seen when they mimic ILO. Stage 2 will be conducted with a patient population(n = 30) referred to a tertiary airways service for breathlessness assessment. Participants in stage 2 will undergo the reference standard laryngoscopy as well as simultaneous TLUS. The level of agreement between TLUS and laryngoscopy will be evaluated, as well as comparison of symptom scores.
DISCUSSION:
This study will help inform future studies of the utility of TLUS in the assessment of ILO. This will be valuable for understanding whether TLUS could be offered as a non-invasive option for patients in the assessment of ILO if they are not able to tolerate or access laryngoscopy diagnostic services. It is not intended that TLUS will replace the current reference standard of video-laryngoscopy but may have potential as an early screening tool if found to be non-inferior.
1Introduction
During inhalation, healthy vocal folds open to maximise ventilation (Christensen et al., 2015 Brancatisano et al., 1983) (see Fig. 1). Inappropriate and unexpected narrowing of the vocal folds, or structures above the vocal folds (supraglottis) during inspiration can lead to associated breathlessness known as inducible laryngeal obstruction (ILO) (see Fig. 2). ILO is also known as vocal cord dysfunction and paradoxical vocal fold movement. ILO is reversible, typically triggered by an inducer (e.g exercise, or strong scents). (Christensen et al., 2015; Hull et al., 2016; Hull & Haines, n.d 2022.). For this paper ILO will be used throughout.
Fig. 1
Larynx during normal breathing.
Fig. 2
Larynx demonstrating Inducible Laryngeal Obstruction.

People with ILO often present with asthma-like symptoms, (McDonald et al., 2019), which may be treated as asthma, due to symptom similarity, leading to a high medication burden and healthcare usage, including unnecessary intubation (Balkissoon & Kenn, 2012; Forrest et al., 2012; Hull et al., 2016; Lee et al., 2020; Murphy et al., 2021). ILO can be encountered independently of asthma (i.e. as a mimic in a patient who does not have asthma), or exist as a comorbidity of asthma in a quarter to a half of asthma cases (Forrest et al., 2012; Lee et al., 2020), appearing as “difficult-to-treat” or “brittle” asthma, driving an increase in oral steroid exposure and/or hospital admissions (Balkissoon & Kenn, 2012; Leong et al., 2022). Asthma affects approximately 5.4 million people in the UK (Mukherjee et al., 2016), with annual asthma care costing at least € €1.1 billion. Some of this is spent inappropriately and needlessly on treatment of undiagnosed ILO symptoms (masquerading as asthma), as patients with asthma and ILO access healthcare services more than those with asthma alone (Mukherjee et al., 2016; Murphy et al., 2021). A prompt and accurate diagnosis of ILO has potential to reduce healthcare and patient population burden (Baxter et al., 2014; Christopher et al., 1983; Leong, Gibson, et al., 2023a; Leong, Vertigan, et al., 2023; Low et al., 2011). ILO has been identified as a national and international clinical and research priority, due to its clinical impact. (Leong, Vertigan, et al., 2023).
1.1Prevalence
Research indicates between 32–50% of patients with severe or difficult to control asthma may have inspiratory adduction of the vocal folds on inspiration. (Haines et al., 2022; Leong, Vertigan, et al., 2023; Low et al., 2011; Newman et al., 1995), with some studies estimating the prevalence of laryngeal dysfunction to be as high as 75% in individuals with asthma (Leong, Gibson, et al., 2023b;Low et al., 2011).
Assessment for ILO necessitates a thorough and systematic clinical assessment to evaluate for causes of breathlessness and is well-described in the literature. (Haines et al., 2018; Hull et al., 2016; Hull & Haines, n.d., 2022). Speech and language therapists (SLTs) are key in the multi-disciplinary assessment and treatment for ILO (Altman et al., 2000; Christopher & Morris, 2010; Murry & Sapienza, 2010; RCSLT, 2021). SLT intervention for ILO can reduce health service utilisation and asthma medication use and includes education and instruction on targeted laryngeal control techniques (Haines et al., 2022; Murphy et al., 2021). The true efficacy of SLT treatment requires further robust and prospective study. (Baxter et al., 2014; Haines et al., 2022; Mahoney et al., 2022; R. R. Patel et al., 2015).
The current reference standard test for diagnosis of ILO is a video-laryngoscopy whilst the patient is experiencing symptoms, which may need to be provoked, if not apparent at baseline assessment (Forrest et al., 2012). However, accessibility, particularly at short-notice to such services may be limited outside of specialist centres, thus hindering diagnosis and management. (Leong, Gibson, et al., 2023a; Leong, Vertigan, et al., 2023; Percy et al., 2022).
Laryngoscopy is an invasive procedure, and although it is associated with a low complication rate (Dziewas et al., 2019), may be an unpleasant experience for some patients. It carries a considerable financial burden and can be time-consuming. Data from our own practice points to laryngoscopy being resource- heavy due to factors such as estates, personnel and equipment required. Furthermore, post COVID-19 service disruption has led to long-term reduction in capacity for laryngoscopic-diagnosed ILO. (Haines et al., 2020; RCSLT, n.d., 2020; Sciancalepore et al., 2021; Tran et al., 2012).
Therefore, there is need for an effective, accessible, and well-tolerated screening tool for identifying ILO. Exploratory studies for assessment of ILO using TLUS in an exercise population (Giron Matute et al., 2019) and for assessing upper airway responses during mechanically assisted cough (Brekka et al., 2022) show promise as a useful method for non-invasive and accessible assessment of the upper airway, and which would provide rationale for this study for assessment of ILO in a different population thus far non-studied, that being a severe asthma. (Nasser et al., 2020).
Ultrasound assessment of laryngeal function via TLUS has been described extensively within the literature in post-thyroidectomy populations (Allen et al., 2021; Beale et al., 2020; Dedecjus et al., 2010; Fung & Lang, 2021; Gambardella et al., 2020; Knyazeva et al., 2018; Nasser et al., 2020; Noel et al., n.d.; A. Patel et al., 2021; Rybakovas et al., 2019; Su et al., 2022), and has been found to have high sensitivity as a screening tool for vocal fold palsy. It is also described as a valid and reliable real-time diagnostic tool (Allen et al., 2021; Nasser et al., 2020; A. Patel et al., 2021), which is useful for the identification of airway patency and vocal fold mobility. Further benefits include that it is cost-effective, safe, rapid, painless, non-invasive, non-irradiating, non-aerosol generating, widely available, (Beale et al., 2020), well-tolerated and does not require sedation or topical analgesia. Additionally, it may be accessed in a timely, and convenient way for patients.
The proposed two-stage pilot and feasibility study aims to determine whether TLUS can be a useful tool in the screening assessment of the abnormal vocal fold movements on inspiration seen in ILO.
2Methods: Trial design
This protocol is designed with reference to the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) guidelines (2013) (Chan et al., 2013). As a feasibility study, the protocol is also designed with reference to the CONSORT (2010) statement: extension to randomised pilot and feasibility trials (Eldridge et al., 2016).
This protocol describes a two-stage feasibility study on two populations, with stage one involving healthy volunteers, and stage two involving a convenience sample of a patient population. In each stage, the accuracy and acceptability of the TLUS procedure will be assessed.
2.1Primary aims
• To assess the sensitivity, specificity, positive and negative predictive value of the use of ultrasound in the assessment of ILO, using Laryngoscopy as reference standard in the patient population (n = 30)
• To establish technical elements that impact on success of visualisation using ultrasound (e.g depth, gain, device pre-settings, and approach used to assess vocal fold movements
• To investigate the patient and healthy volunteer perspectives on the acceptability of TLUS assessment of the vocal folds
2.2Secondary aims
• To provide recommendations to inform the development of TLUS protocols and make suggestions for further research for its use in assessment of ILO, such as impact of age, gender, BMI
• To inform the use of static and dynamic assessment techniques using TLUS
• To evaluate the symptom scores of patients in patients who have a diagnosis of ILO refuted or confirmed
2.3Participant recruitment
The study will take place at the host organisation, which is a tertiary-level severe asthma and airways service. Stage one of the study will recruit a population of healthy volunteers employed within the host organisation. Stage two will recruit a cross-sectional sample of consecutive and eligible patients referred for assessment of refractory and complex breathlessness, where laryngeal dysfunction is suspected.
2.4Stage one: Healthy volunteers
A request for expressions of interest, along with the healthy-volunteer information sheet and consent form will be sent to the host organization’s respiratory department. Inclusion criteria for volunteers are shown in Table 1.
Table 1
Inclusion and exclusion criteria
| Healthy | Patient |
| Volunteers | Population |
| Inclusion criteria | Exclusion criteria |
| •No definite signs, symptoms of, or known vocal fold paralysis | •Patients with a known vocal fold pathology |
| •Uncontrolled respiratory disease | |
| •No symptoms of voice change | |
| •No history of laryngeal or anterior neck surgeries | |
| •No history of laryngeal or neck pathology | |
| •Patient with known or suspected history of head and neck surgery | |
| •No uncontrolled respiratory disease |
2.5Stage two: Patient population
All patients who attend for an initial consultation in the Airways service who have suspected ILO and who meet the eligibility criteria (see Table 1), will be approached by the PI and be provided with a patient information sheet at least 48 hours before the planned procedure to see if they would wish to undergo TLUS concurrently with laryngoscopy (usual care). Written consent will be confirmed at the appointment for the laryngoscopy (usual care for laryngoscopy), by the PI.
2.6Equipment
2.6.1Ultrasound equipment
The device used for this study will be the Vscan Air. This consists of a dual-headed probe, which has both a curved and linear array transducers. It is used with an app that can be installed on AndroidTM or iOS® mobile devices. The Linear array transducer will be used for this study. This has a broad-bandwidth linear array: from 3 12 MHz with a centre frequency of 7.7 MHz Number of elements: 192 Footprint: 40 mm×7 mm (lens) and can achieve a depth of up to 8 cm (GE Healthcare accessed on 14.10.22).
2.6.2Laryngoscopy equipment
Laryngoscopy will be carried out using Olympus CV170 HD/NBI Imaging system with Laryngograph Endo Strobe 4K recording device and strobe stack system, (Olympus Inc, Keymed, Southend-on-Sea, UK).
2.7Procedures
For both study populations, the PI, who is trained in the TLUS procedure, will perform a TLUS scan using the Vscan Air device following a protocol designed by the PI.
2.8Stage one
The scan will be performed to identify the sonoanatomy including the thyroid cartilage and the true and false vocal folds. When the vocal folds are visualised, the healthy volunteer will be asked to breathe normally, and then vocalise (by saying “ee”) for a sustained period. They will then be asked to breath hold (valsalva manoeuvre), then take a deep breath in (3 trials). The PI will demonstrate how to mimic ILO to the volunteer. The healthy volunteer will then be asked to mimic ILO. Visualisation, or otherwise, of both true and false vocal folds (right and left), at baseline, during breathing, and when mimicking ILO will be recorded.
To review inter-rater reliability, a proportion (30%) of 10-second video recordings from the healthy volunteers will be sent to both a study collaborator (JA) and a Specialist Head & Neck Sonographer (SR) securely (using GE’s system). To de-identify the data, it will be pseudonymised.
2.9Stage Two
For the patient population, who may have either a confirmed diagnosis of asthma (co-morbid population), or have no objective evidence of, or unconfirmed asthma, and are suspected of having ILO (mimic population), the TLUS will be undertaken concurrently with provocation video-laryngoscopy (see Fig. 3), during which triggers are used to provoke typical symptoms. Each patient will complete the Newcastle Laryngeal Hypersensitivity Questionnaire, a validated symptom questionnaire (Vertigan et al., 2014). All patients will attend laryngoscopy (usual care) and will have a simultaneous TLUS performed (see image below).
Fig. 3
Simultaneous Layngoscopy and TLUS.

The PI will perform the TLUS whilst another SLT completes the laryngoscopy (usual care) and the laryngoscopy provocation protocol to induce typical symptoms (RCSLT, 2021) The PI will take a note of settings to achieve image acquisition (frequency in MHz, the pre-set setting that was used, depth and gain settings, approach (lateral or transverse), and will take note of the success of visualisation and vocal fold movements on a pseudonymised recording form. Any other factors that are deemed useful to include to help replicate findings and improve image acquisition will be recorded by the PI.
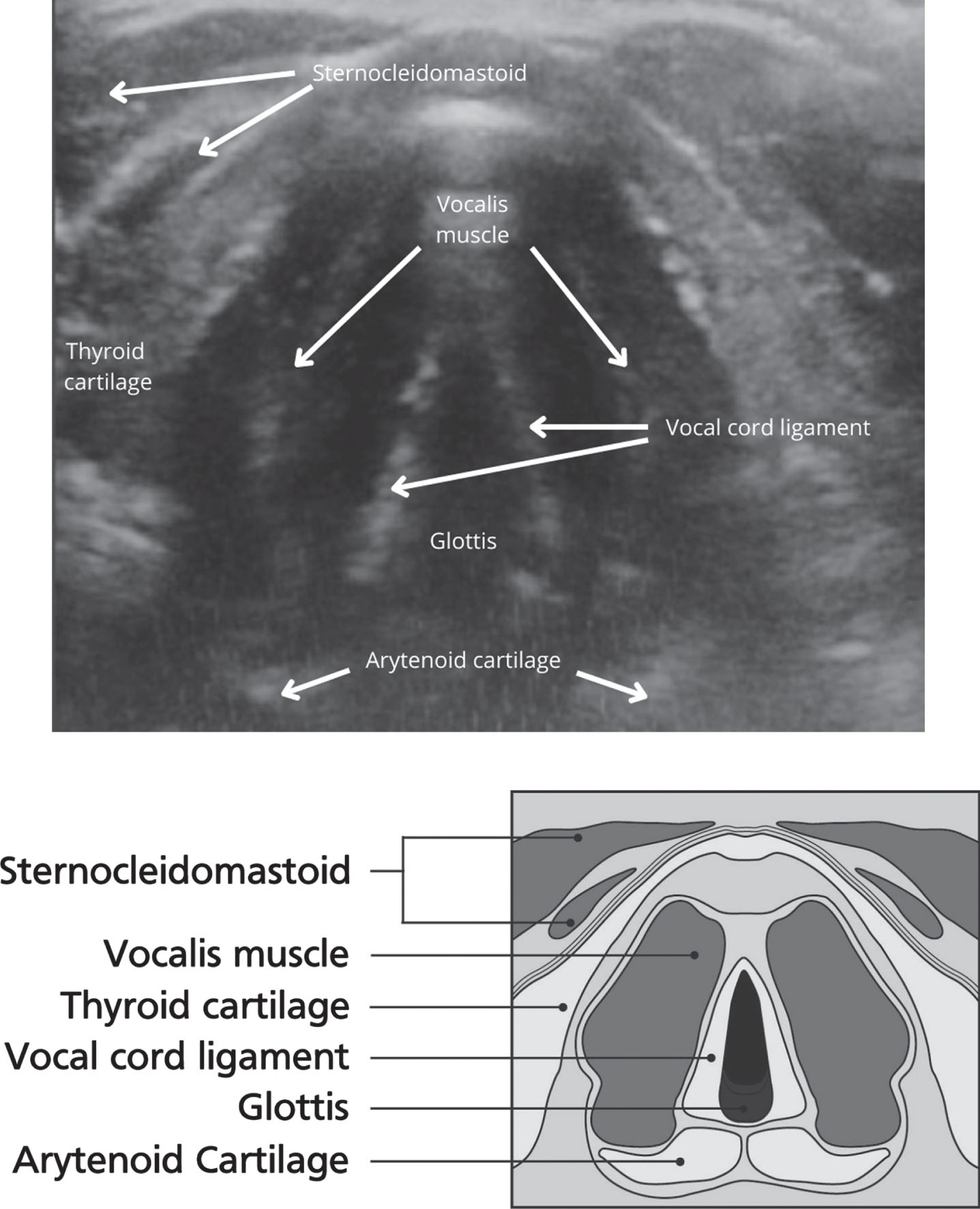
The TLUS will consist of a scan of the larynx to identify the main landmarks (hyoid bone, thyroid cartilage, arytenoid cartilages, vocal folds and false vocal folds) (see Fig. 4). The PI and SLT laryngoscopy operators will be blinded to the images and results of the other assessment (either TLUS or laryngoscopy). The screen for the laryngoscopy system will be rotated away to be unobservable by the PI to help minimise potential detection bias.
Fig. 4
Images of Vocal folds using ultrasound and schematic diagram.
If the patient finds assessment with simultaneous laryngoscopy and TLUS too distressing, the TLUS will be stopped. Following the procedure, the PI will leave the clinical area to allow for debrief to occur between the patient and the SLT.
For each patient, the results of the TLUS and laryngoscopy will be compared for outcome, with record made of any false positive or negative results, along with the success of being able to visualise both true and false vocal folds (left and right) with TLUS. Following the procedure, the participants will be asked by the PI to complete an electronic acceptability survey designed by the PI to gain feedback on their experience.
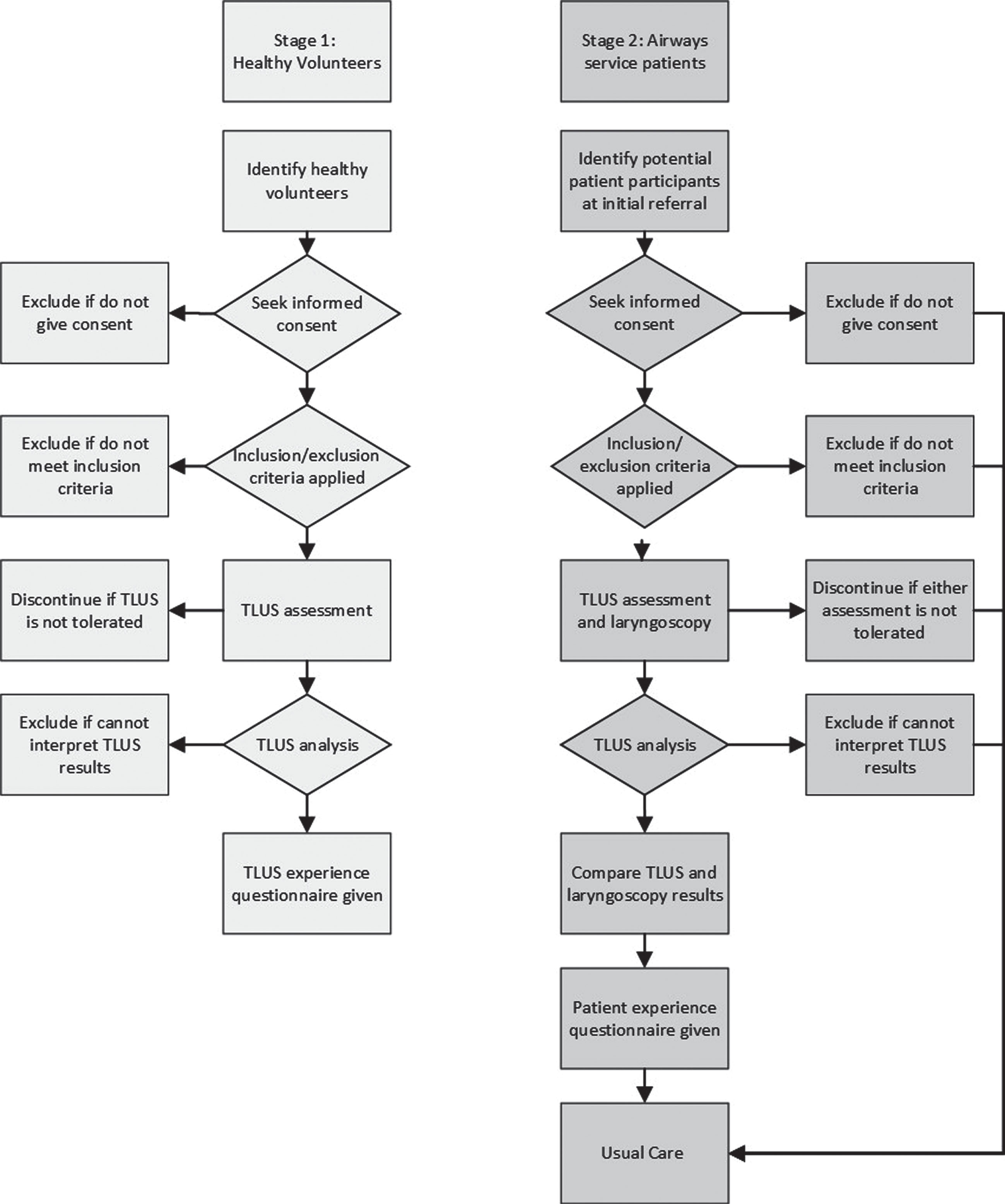
After assessment and diagnosis, patients will continue along their usual care pathway, i.e. if ILO is confirmed, they will be offered SLT intervention, and if ILO is not confirmed, the patient will continue along the medical management pathway. See Fig 5. for participant flow diagram.
Fig. 5
Participant flow diagram.
2.10Fidelity
In the proposed study, fidelity will be ensured via a number of methods including: appropriate training of the PI in the use of TLUS assessment equipment and the interpretation of results, use of a standardised protocol, accurate record-keeping of results using a standardised pro-forma, inter-rater reliability checks of healthy volunteer data, and use of standardised data analysis methods.
3Data analysis
The outcomes of the TLUS and laryngoscopy assessments in stage one and stage two will be analysed using SPSS. For stage one, outcomes will be whether the vocal cords can be visualised, and whether mimicked ILO can be visualised. For stage two, outcomes will be whether vocal cord movements indicative of ILO can be visualised.
Two by two tables will be generated to calculate values of sensitivity (whether a participant can be confirmed as having ILO, or mimicked ILO) and specificity (whether ILO, or mimicked ILO, can be ruled out for a participant), and confidence intervals for visualisation of the vocal folds using TLUS. ROC curves will be calculated to demonstrate the relationship between sensitivity and specificity and the potential benefit of TLUS. Percentage agreement between TLUS and laryngoscopy for confirmation or non-confirmation of ILO will also be calculated, along with positive and negative predictive values.
A true-positive finding would be the ability of TLUS to detect impaired laryngeal movements on inspiration, which concurs with abnormal movements on laryngoscopy. A false-positive finding would be the detection of abnormal movement on TLUS when normal movement is visible on laryngoscopy. A true-negative finding would be accurate detection of normal laryngeal movements by TLUS imaging, which concurs with normal movements of laryngoscopy. A false-negative finding would be the detection of normal movements on TLUS, whilst abnormal movements are visible on laryngoscopy.
Measurements of the distance between the arytenoids, if available, for healthy volunteers and patients during normal breathing, deep inspiration, and during ILO (mimic in stage one and actual in stage two), will be compared.
Numerical data from the acceptability questionnaires will be analysed using Microsoft Excel to generate mean values and ranges. Qualitative questionnaire data will be analysed using thematic analysis (Braun & Clarke, 2006), with themes generated to aid understanding of participants’ experiences of the TLUS and laryngoscopy procedures.
4Discussion
The purpose of this two-stage study is to assess whether TLUS is a useful triage screening tool in the assessment of ILO when compared to the current reference standard test of video-laryngoscopy, and to inform future studies on the diagnostic test accuracy of laryngeal ultrasound.
The study aims to investigate the feasibility of TLUS in the assessment of ILO in relation to the accuracy and acceptability of the procedure, as well as gathering data on variables which impact on the success of TLUS visualisation. It also aims to gather further patient data to inform TLUS protocols (e.g. age and BMI) and data on variation in vocal fold movements in people with and without ILO.
Diagnostic screening with TLUS may help identify patients with asthma who also have ILO (comorbid population), or patients whose symptoms of breathlessness have been misdiagnosed as having asthma (mimic population). If this can be identified, this may have the potential to help reduce healthcare utilisation, allowing health resources to be used more appropriately, and have potential significant impact on morbidity for patients and their families, with potential for significant patient benefit.
4.1Future research
This is a feasibility study to inform a larger scale investigation of the utility of TLUS in the screening of ILO in patients with suspected ILO. Feasibility will be assessed in line with a typology (Orsmond & Cohn, 2015) that looks at whether the following features are effective: recruitment and sampling, procedures, acceptability of the assessment, resources available, and evaluation of the results.
Ethical approval: The study has been approved by HRA and Health and Care Research Wales (HCRW), IRAS project ID: 298631 Protocol number: n/a REC reference: 22/NW/0209. Sponsor Lancashire Teaching Hospitals NHS Foundation. HRA and Health and Care Research Wales (HCRW) Approval granted 27.07.22. Retrospectively registered on ClinicalTrials.gov Identifier: NCT05686941.
Harms: Any adverse effects and harm will be recorded and assessed. If more than 60% of patients in Stage two cannot tolerate dual procedures with TLUS and laryngoscopy, the study will be discontinued. There are no known risks to the patient in the use of laryngeal Ultrasound. The treatment is non-invasive and does not involve radioactive substances. As the patient will be undergoing usual care, there is no risk of missing an ILO diagnosis.
4.2Roles and responsibilities
Contributors: CS, KB, LH, SR and RS were responsible for the overall development of an ethically sound protocol, involved in the conception and production of the study and the development of the initial protocol. CS drafted the manuscript. CS, RS, RG, SS and PL edited drafts of the manuscript and contributed to critical revision and final approval of manuscript.
4.3Sponsor
Lancashire Teaching Hospitals NHS Foundation Trust (LTHTR)
Name and contact information for the trial sponsor: Dr Kina Bennett, Lancashire Teaching Hospitals Trust.
Funding
This study was partially funded by a bursary from (€800) Council for Allied Health profession Research (CAHPR), bursary for time to perform ultrasound scan on 30 healthy volunteers. CAHPR will have no input into the writing of the findings; the decision to submit the report for publication. NIHR research internship-funded time was used in the writing-up of this manuscript.
Dissemination
Results will be disseminated through peer-reviewed journals, presentation of scientific abstracts at National and international conferences, and presentations in relevant conferences. There are no plans to grant public access to the full protocol, participant-level dataset, and statistical code.
Study end definition
The study will end when the last participant has been completed and data has been collected. The study will close early if it is found during Stage one that ultrasound is not useful (limited successful viewings of the vocal folds i.e under 30% of vocal folds visualised) in the assessment of vocal fold function.
The trial will be discontinued if the feedback from patients is adverse for the experience of TLUS, or in the case of any serious adverse events, such as panic reaction to undergoing TLUS. There are not anticipated to be any serious adverse effects, as the TLUS is less invasive than usual care laryngoscopy.
Protocol amendments
Amendments to the protocol will be updated via the integrated research application system amendment tool.
Consent or assent
The PI will be responsible for collecting of consent for both the healthy volunteers and the patient participants. No biological specimens will be collected.
Declaration of interests
There are no interests to declare related to this study.
The study will be covered by the host organisations indemnity scheme.
Acknowledgments
Lisa Hayward, Blackpool Teaching Hospital, UK
Kina Bennett, Lancashire Teaching Hospital, UK
Sally Richmond: University College London, UK
Hannah Lever, Lancashire Teaching Hospital, UK
Professor Stephen Fowler, Manchester University
Monitoring, reporting and finance
The study will be conducted in accordance with approvals and advice from relevant groups e.g., Ethics and Research and Development Trust approval.
The study will be conducted in compliance with the Research Governance Framework for Health and Social Care, the Medicine for Human Use (clinical trials) Regulation 2004 and Good Clinical Practice.
No Financial agreements have been arranged.
Trial Registration: NCT05686941
Trial identifier: REC reference: 22/NW/0209
Protocol version: Date and version identifier V7. REC reference: 22/NW/0209
References
1 | Allen, J. E. , Clunie, G. M. , Slinger, C. , Haines, J. , Gaston, C. , Zaga, C. J. ,et al ((2021) ). Utility of ultrasound in the assessmentof swallowing and laryngeal function: A rapid review and criticalappraisal of the literature. International Journal of Language and Communication Disorders, 56: (1). doi: 10.1111/1460-6984.12584. |
2 | Altman, K. W. , Mirza, N. , Ruiz, C. , Sataloff, R. T. ((2000) ). Paradoxical vocal fold motion: Presentation and treatment options. Journal of Voice, 14: (1), 99–103. doi: 10.1016/S0892-1997(00)80099-5. |
3 | Balkissoon, R. , Kenn, K. ((2012) ). Asthma: Vocal Cord Dysfunction(VCD) and other Dysfunctional Breathing Disorders. Seminars in Respiratory and Critical Care Medicine, 33: (06), 595–605. doi: 10.1055/s-0032-1326959. |
4 | Baxter, M. , Uddin, N. , Raghav, S. , Leong, P. , Low, K. , Hamza, K. et al. ((2014) ). Abnormal vocal fold movement treated with botulinumtoxin in patients with asthma resistant to optimised management. Respirology, 19: (4), 531–537. doi: 10.1111/res12271. |
5 | Beale, T. , Twigg, V. M. , Horta, M. , Morley, S. ((2020) ). High-resolution laryngeal US: Imaging technique, normal anatomy, and spectrum of disease. Radiographics, 40: (3), 775–790. doi: 10.1148/rg.2020190160. |
6 | Brancatisano, T. , Collett, P. W. , Engel, L. A. ((1983) ). Respiratory movements of the vocal cords. Journal of Applied Physiology, 54: (5), 1269–1276. doi: 10.1152/jappl.1983.54.5.1269. |
7 | Braun, V. , Clarke, V. ((2006) ). Using thematic analysis inpsychology. Qualitative Research in Psychology 3: (2), 77–101. doi: 10.1191/1478088706qp063oa. |
8 | Brekka, A. K. , Vollsæter, M. , Ntoumenopoulos, G. , Clemm, H. H. , Halvorsen, T. , Røksund, O. D. , Andersen, T. M. ((2022) ). Adjustments of non-invasive ventilation and mechanically assistedcough by combining ultrasound imaging of the larynx with transnasal fibre-optic laryngoscopy: A protocol for an experimental study. BMJ Open, 12: (5). doi: 10.1136/bmjopen-2021-059234. |
9 | Chan, A.-W. , Tetzlaff, J. M. , Altman, D. G. , Laupacis, A. , Gøtzsche P.C. , Krleža-Jerić K. , et al ((2013) ). SPIRIT 2013 Statement: Defining Standard Protocol Items for Clinical Trials. Annals of Internal Medicine, 158: , 200–207. doi: 10.7326/0003-4819-158-3-201302050-00583. |
10 | Christensen, P. M. , Heimdal, J. H. , Christopher, K. L. , Bucca, C. , Cantarella, G. , Friedrich, G. ,et al ((2015) ). ERS/ELS/ACCP 2013 international consensus conference nomenclature on induciblelaryngeal obstructions. European Respiratory Society, 24: (1)445–450. doi: 10.1183/16000617.00006513. |
11 | Christopher, K. L. , Wood, R. P. , Eckert, R. C. , Blager, F. B. , Raney, R. A. , Souhrada, J. F. ((1983) ). Vocal-Cord DysfunctionPresenting as Asthma. NewEngland Journal of Medicine, 308: (26)1566–1570. doi: 10.1056/NEJM198306303082605. |
12 | Christopher, K. L. , Morris, M. J. ((2010) ). Vocal Cord Dysfunction,Paradoxic Vocal Fold Motion, or Laryngomalacia? Our UnderstandingRequires an Interdisciplinary Approach. Otolaryngol Clin North Am43: (1), 43–66. doi: 10.1016/j.otc.2009.12.002. |
13 | Dedecjus, M. , Adamczewski, Z. , Ski, J. B. , Ski, A. L. ((2010) ). Real-time, high-resolution ultrasonography of the vocal folds: Aprospective pilot study in patients before and after thyroidec-tomy. Langenbeck’s Archives of Surgery 395: (7), 859–864. doi: 10.1007/s00423-010-0694-2. |
14 | Dziewas, R. , Brinke, M. D. , Birkmann, U. , Bräuer, G. , Busch, K. , Cerra, F. ,et al ((2019) ). Safety and clinical impact of FEES -results of the FEES registry. Neurological Research and Practice, 1: (1), 16–16. doi: 10.1186/s42466-019-0021-5. |
15 | Eldridge, S. M. , Chan, C. L. , Campbell, M. J. , Bond, C. M. , Hopewell, S. , Thabane, L. , et al ((2015) ). The distinctive featuresof a feasibility study: Objectives and guiding questions, 35: (3), 169–177. |
16 | Forrest, L. A. , Husein, T. , Husein, O. ((2012) ). Paradoxical vocalfold motion: Classification and treatment. Laryngoscope, 122: (4)844–853. doi: 10.1002/lary.23176. |
17 | Fung, M. M. H. , Lang, B. H. H. ((2021) ). A prospective studyevaluating the feasibility and accuracy of very early postoperativetrans laryngeal ultrasonography in the assessment of vocal foldfunction after neck surgery. Surgery (United States)169: (1), 191–196. doi: 10.1016/j.surg.2020.03.025. |
18 | Gambardella, C. , Offi, C. , Romano, R. M. , Palma, M. , Ruggiero, R. , Candela, G. ,et al ((2020) ). Transcutaneous laryngealultrasonography: A reliable, non-invasive and inexpensivepreoperative method in the evaluation of vocal foldmotility— a prospective multicentric analysis on a largeseries and a literature review. Updates in Surgery, 73: (3)885–892. doi: 10.1007/s13304-020-00728-3. |
19 | Haines, J. , Esposito, K. , Slinger, C. , Pargeter, N. , Murphy, J. , Selby, J. ,et al ((2020) ). UK consensus statement on the diagnosis ofinducible laryngeal obstruction in light of the COVID-19 pandemic. Clinical and Experimental Allergy 50: (12). doi: 10.1111/cea.13745. |
20 | Haines, J. , Smith, J.A. , Wingfield-Digby, J. , King, J. , Yorke, J. , Fowler, S. J. ((2022) ). Systematic review of the effectiveness ofnon-pharmacological interventions used to treat adults withinducible laryngeal obstruction. BMJ Open Respiratory Research, 9: (1). doi: 10.1136/bmjresp-2022-001199. |
21 | Hull, J. H. , Backer, V. , Gibson, P. G. , Fowler, S. J. ((2016) ). Laryngeal dysfunction: Assessment and management for the clinician. American Thoracic Society, 194: 1062–1072. doi: 10.1164/rccm.201606-1249CI. |
22 | Hull, J. H. , Haines, J. ((2018) ). Complex breathlessness, 26: 174–179. ERS publications. DOI: 10.1183/2312508X.erm9722. |
23 | Hull, J. H. , Haines, J. , Fowler, S. J. ((2018) ). Clinicalpresentation, assessment, and management of inducible laryngealobstruction. Lippincott Williams and Wilkins, 26: 174–179. doi: 10.1097/MOO.0000000000000452 |
24 | Knyazeva, P. , Makarin, V. , Seeliger, B. , Chernikov, R. , Sleptsov I. , Semenov, A. ,et al ((2018) ). Transcutaneous laryngealultrasonography (TLUS) as an alternative to direct flexiblelaryngoscopy (DFL) in the perioperative evaluation of the vocal foldmobility in thyroid surgery. Langenbeck’s Archives of Surgery, 403: (8). doi: 10.1007/s00423-018-1734-6. |
25 | Lee, J. H. , An, J. , Won, H. K. , Kang, Y. , Kwon, H. S. , Kim, T. B. ,et al ((2020) ). Prevalence and impact of comorbid laryngealdysfunction in asthma: A systematic review and meta-analysis. Journal of Allergy and Clinical Immunology, 145: (4). doi: 10.1016/j.jaci.2019.12.906. |
26 | Leong, P. , Vertigan, A. E. , Hew, M. , Baxter, M. , Phyland, D. , Hull,J. H. ,et al ((2022) ). Diagnosis of vocal cord dysfunction/induciblelaryngeal obstruction—A Delphi study protocol. PloS One17: (12). doi: 10.1371/journal.pone.0279338. |
27 | Leong, P. , Vertigan, A. E. , Hew, M. , Baxter, M. , Phyland, D. , Hull, J.H. ,et al ((2023) ) Diagnosis of Vocal Cord Dysfunction/Inducible Laryngeal Obstruction: An International Delphi Consensus Study. Journal of Allergy and Clinical Immunology. doi: 10.1016/j.jaci.2023.06.007. |
28 | Leong, P. , Gibson, P. G. , Vertigan, A. E. , Hew, M. , McDonald, V. M. , Bardin, P. G. ((2023) ). Vocal cord dysfunction/inducible laryngealobstruction—2022 Melbourne Roundtable Report. Respirology, 28: (7), 615–626. doi: 10.1111/res14518. |
29 | Low, K. , Lau, K. K. , Holmes, P. W. , Crossett, M. , Vallance, N. , Phyland, D. ,et al ((2011) ). Abnormal Vocal Cord Function inDifficult-to-Treat Asthma. American Journal of Respiratory and Critical Care Medicine, 184: (1), 50–56. doi: 10.1164/rccm.201010-1604OC. |
30 | Mahoney, J. , Hew, M. , Vertigan, A. , Oates, J.. ((2022) ). Treatmenteffectiveness for Vocal Cord Dysfunction in adults and adolescents:A systematic review. Clin Exp Allergy, 52: (3), 387–404. doi: 10.1111/cea.14036. |
31 | Matute, W. I. G. , Pedro, J. G. D. , Benedetti, P. A. , Diez, J. D. M. , Puente-Maestu, L. (2019). Exercise Induced Laryngeal Obstruction Measured by Vocal Cord Ultrasonography During Maximal Effort in Cardiopulmonary Exercise Testing. ATS Conference Abstracts A6904. doi: doi.org/10.1164/ajrccmconference.2019.199.1meetingabstracts.a6904. |
32 | McDonald, V. M. , Fingleton, J. , Agusti, A. , Hiles, S. A. , Clark, V. L. , Holland, A. E. ,et al ((2019) ). Treatable traits: A new paradigm for st century management of chronic airway diseases: Treatable Traits down under International Workshop report. European Respiratory Society, 53: . doi: 10.1183/13993003.02058-2018. |
33 | Mukherjee, M. , Stoddart, A. , Gupta, R. P. , Nwaru, B. I. , Farr, A. , Heaven, M. ,et al ((2016) ). The epidemiology, healthcare and societalburden and costs of asthma in the UK and its member nations:Analyses of standalone and linked national databases. BMC Medicine, 14: (1). doi: 10.1186/s12916-016-0657-8. |
34 | Murry, T. , Sapienza, C. ((2010) ). The Role of Voice Therapy in theManagement of Paradoxical Vocal Fold Motion, Chronic Cough, andLaryngospasm. Otolaryngologic Clinics of North America, 43: (1), 73–83. doi: 10.1016/j.otc.2009.11.004. |
35 | Murphy, J. M. , Stephen, S. , Pearson, F. , Desoyza, A. ((2021) ). P108 A systematic review to explore the relationship between inducible laryngeal obstruction and healthcare utilisation in adults with Asthma. Thorax. 76: ,A148. doi: 10.1136/thorax-2020btsabstracts.253. |
36 | Nasser, H. M. , Askoura, A. , Hussein, A. (2020). Ultrasonography diagnostic validity in structural and functional laryngeal disorders. Egyptian Journal of Radiology and Nuclear Medicine, 51-51. |
37 | Newman, K. B. , Mason, U. G. , Schmaling, K. B. ((1995) ). Clinical features of vocal cord dysfunction. American Journal of Respiratory and Critical Care Medicine, 152: (4), 1382–1386. doi: 10.1164/ajrccm.152.4.7551399. |
38 | Noel, J. E. , Orloff, L. A. , Sung, K. ((2020) ). Laryngeal Evaluation during the COVID-19 Pandemic: Transcervical Laryngeal Ultrasonography. Otolaryngol Head Neck Surg, 163: (1), 51–53. doi: 10.1177/0194599820922984. |
39 | Orsmond, G. I. , Cohn, E. S. ((2015) ). The distinctive features of afeasibility study: Objectives and guiding questions, OTJR:Occupation. Participation and Health, 35: (3), 169–177. |
40 | Patel, A. , Spychalski, P. , Aszkiełowicz, A. , Mikaszewski, B. , Kobiela, J. ((2021) ). Transcutaneous laryngeal ultrasound for vocalfold paralysis assessment in patients undergoing thyroid and parathyroid surgery-a systematic review and meta-analysis. In Journal of Clinical Medicine, 10: 22–22. |
41 | Patel, R. R. , Venediktov, R. , Schooling, T. , Wang, B. ((2015) ). Evidence-Based Systematic Review: Effects of Speech Language Pathology Treatment for Individuals With Paradoxical Vocal Fold Motion. American Journal of Speech-Language Pathology,, 24: (3), 566–584. doi: 10.1044/2015AJSLP-14-0120. |
42 | Percy, S. , Ludlow, S. F. , Tidmarsh, B. , Fowler, S. J. ((2022) ). P107 UK speech and language therapy (SLT) diagnostic and therapy services for inducible laryngeal obstruction. Thorax,77: (Suppl 1), 138. doi: 10.1136/thorax-2022-BTSabstracts.243. |
43 | RCSLT Guidance: Speech and language therapist-led endoscopic procedures: considerations for all patients during the COVID-19 pandemic. RCSLT (April, 2021). |
44 | RCSLT Guidance. Speech and language therapist-led endoscopic procedures in the COVID-19 pandemic RCSLT, 2020. |
45 | RCSLT Guidance: Guidance on voice and upper airway disorders in thecontext of COVID-19 in adult and paediatric services. RCSLT August, 2020. |
46 | Rybakovas, A. , Bausys, A. , Matulevicius, A. , Zaldokas, G. , Kvietkauskas, M. , Tamulevicius, G. ,et al ((2019) ). Recurrent laryngeal nerve injury assessment by intraoperative laryngeal ultrasonography: A prospective diagnostic test accuracy study. Wideochir Inne Tech Maloin wazyjne, 14: (1), 38–45. doi: 10.5114/wiitm.2018.80066. |
47 | Sciancalepore, P. I. , Anzivino, R. , Petrone, P. , Petrone, D. , Quaranta, N. ((2021) ). Transcutaneous laryngeal ultrasonography: Apromising tool for otolaryngologists during COVID-19. American Journal of Otolaryngology, 42: (81), 102772–102772. doi: 10.1016/j.amjoto.2020.102772. |
48 | Su, E. , Hamilton, C. , Tawfik, D. S. , Mariano, K. , Ginsburg, S. , Hopewell, S. ,et al ((2022) ). Laryngeal Ultrasound Detects Vocal FoldImmobility in Adults: A Systematic Review. Journal of Ultrasound in Medicine, 41: (8), 1873–1888. doi: 10.1002/jum.15884. |
49 | Tran, K. , Cimon, K. , Severn, M. , Pessoa-Silva, C. L. , Conly, J. ((2012) ). Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PloS One, 7: (4), 35797–35797. doi: 10.1371/journal.pone.0035797. |
50 | Vertigan, A. E. , Bone, S. L. , Gibson, P. G. ((2014) ). Development and validation of the Newcastle laryngeal hypersensitivity questionnaire. Cough, 10: (1). doi: 10.1186/1745-9974-10-1. |



