The use of tracheostoma humidification by people with total laryngectomy in England and Wales: A cross-sectional survey
Abstract
BACKGROUND:
People with total laryngectomy (PTL) are advised to use a tracheostoma cover to protect their altered airway and optimise pulmonary health. Despite evidence for efficacy, variable adherence rates are reported.
OBJECTIVE:
To investigate the use of tracheostoma humidification by PTL in England and Wales and explore influencing factors.
METHODS:
A national multi-centre audit of PTL was completed in response to the Covid-19 pandemic over a six-month period (March to September 2020). This paper reports secondary analysis of data collected on type of humidification used by PTL. Type of humidification was dichotomised as ‘HME’ (closed-system heat moisture exchanger) or ‘non-HME’ (alternative stoma cover or no stoma cover). Univariable analysis was performed to determine the association with several potential explanatory variables including gender, age, living circumstances, distance from treatment centre, communication method and time elapsed since laryngectomy. A backwards selection procedure was used to determine the final model for multiple regression analysis.
RESULTS:
Data were obtained from 1216 PTL from 26 centres; information on type of tracheostoma humidification used was available for 1097 PTL. Most PTL (69%) used an HME. Following multiple regression analysis, time elapsed since laryngectomy (p = <0.001), living circumstances (p = 0.002) and communication method (p = <0.001) were statistically significant factors in HME use.
CONCLUSIONS:
In England and Wales most PTL use a closed-system HME, though there is marked variability across centres. HME use is influenced by time elapsed since laryngectomy, living circumstances and communication method.
1Introduction
People with total laryngectomy (PTL) have a permanent separation of the trachea and oesophagus and rely on a surgically created neck tracheostoma to breathe. Altered anatomy results in a loss of filtration and humidification capacity of the upper airways and consequent reduced respiratory resistance. The detrimental impact of this on pulmonary health is well-established, with increased bronchial secretions and reduced mucociliary clearance resulting in increased risk of chest infections, reduced respiratory capacity and negative effects on quality of life (Maurizi et al., 1986; Guye, 1887). Additionally, the permanent tracheostoma leaves PTL at risk of airway invasion by airborne particles or foreign bodies. PTL are advised to use a tracheostoma cover to protect the airway and to optimise pulmonary health.
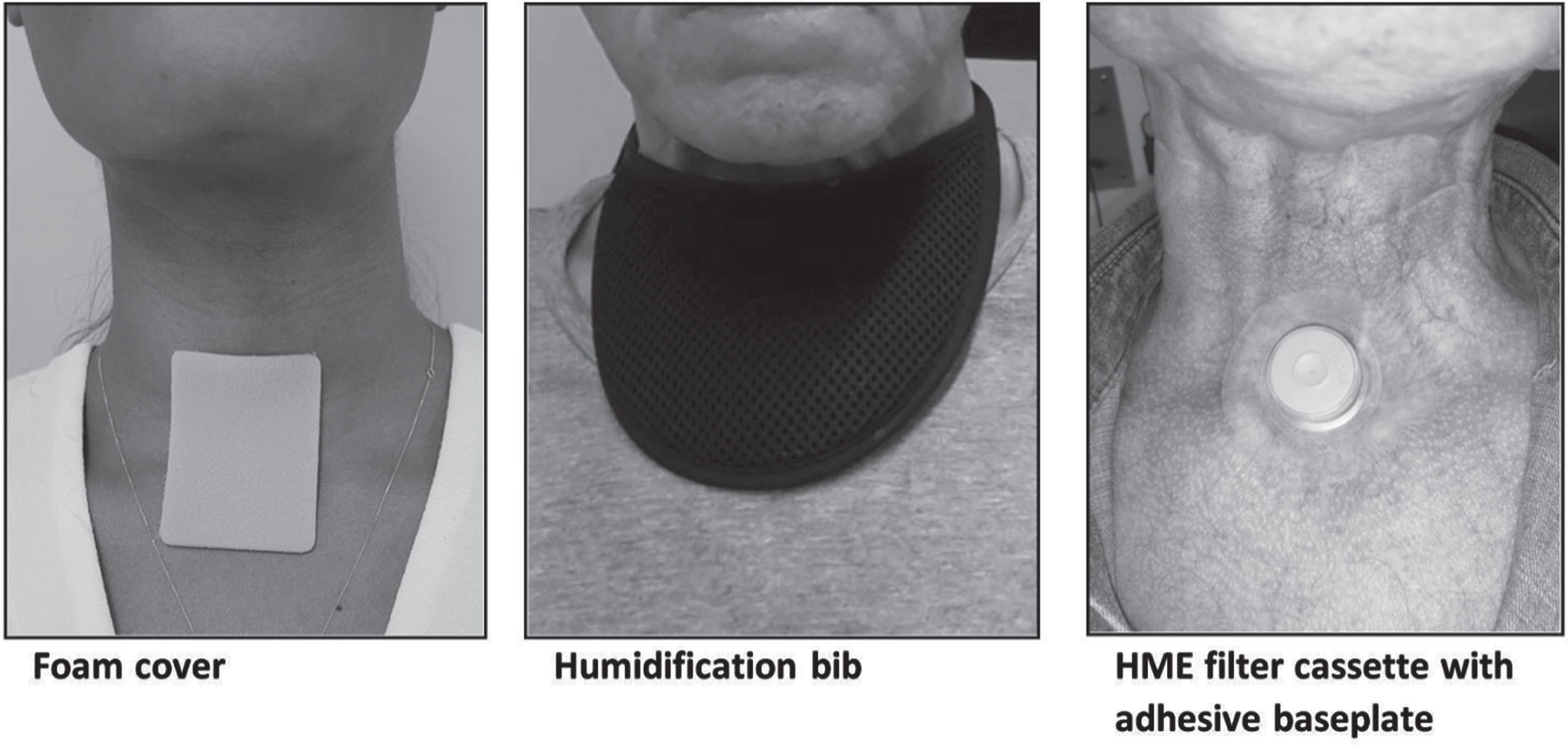
A number of different tracheostoma covers are available (Fig. 1). Simple stoma covers with no humidification properties (e.g. scarves) are used primarily for aesthetics and stoma protection. Foam-based covers or specially designed bibs also offer humidification properties (Quail et al., 2016). Closed-system heat moisture exchange devices (HMEs) comprising a filter cassette secured with an adhesive baseplate or laryngectomy tube offer humidification and filtration (Scheenstra et al., 2010). Closed-system HMEs have been available on prescription in the UK since the mid-1990 s and are now considered the optimum method of humidification and filtration for PTL. The use of HMEs as soon as possible post-surgery is recommended in best practice clinical guidelines (Clarke et al., 2016). Initiation of HME use at day one post-surgery has been reported (Ebersole et al., 2020).
Fig. 1
Types of tracheostoma cover.
While closed system HMEs are more expensive than alternative stoma covers (Quail et al., 2016), the benefits are well recognised including the reduction of coughing, shortness of breath, mucous production, plug formation and chest infections (Ebersole et al., 2020; Jones et al., 2003; Scheenstra et al., 2010). There is a correlation between duration of HME use and pulmonary benefit (Ackerstaff et al., 1998). HME use has been found to significantly enhance quality of life for PTL (Ackerstaff et al., 2003), and can offer PTL with surgical voice restoration (SVR) improved digital occlusion for voicing and better speech intelligibility (Ackerstaff et al., 1998, 2003).
Despite evidence of efficacy, variable compliance rates with HME use have been reported, from 35% to 83% (Lorenz & Maier, 2009; Ebersole et al., 2020). Reported reasons for resistance to HME use include excessive mucus production, blockage of the filter and poor baseplate seal (Jones et al., 2003). In some healthcare systems the financial burden of HME use may be a barrier (Quail et al., 2016). Additional factors that could influence use of HME include skin irritation from adhesives, time elapsed since surgery, neck contour, the recommendations and education provided by clinicians, and ease of accommodation to airway resistance (Ackerstaff et al, 2007; Macri et al., 2016).
With the onset of the Covid-19 pandemic in March 2020, PTL were thought to be a high-risk group for contracting and transmitting Covid-19 infection through respiratory droplet formation and aerosolisation due to their altered airways (Kligerman et al., 2020; Govender et al., 2021). This paper reports on the use of tracheostoma covers as reported by patients and/or their clinicians during an audit of PTL during the first UK national lockdown period. The audit was initiated in response to queries regarding the specific risks associated with Covid-19 for PTL. Details on the background and development of the audit and data on shielding, hospital admission and mortality have been reported previously (Govender et al., 2021). The objectives of the current paper are to report secondary analysis of data collected during the audit, focusing on the following:
• The usage of tracheostoma covers by PTL in England and Wales, specifically use of a commercially available closed-system HME (termed “HME” for this analysis) versus all alternatives (termed “non-HME” for this analysis).
• The factors that may influence HME use by PTL in England and Wales.
Based on literature and clinical experience, we postulate the following factors may influence HME use: age, gender, time elapsed since surgery, distance from the treating centre, employment status, living circumstances and primary communication method.
2Methods
This paper has been prepared with reference to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist for cross-sectional studies (Von Elm et al., 2007).
2.1Ethical considerations
The Health Research Authority decision tool (http://www.hra-decisiontools.org.uk/research/) identified the project as service evaluation, which was approved by the Applied Health in Cancer Governance Group at the lead NHS site. Individual sites sought local approval to share data which was originally collected under the Control of Patient Information (COPI) notice during the Covid-19 pandemic. Whilst deemed service evaluation, this work conforms with the Code of Ethics of the World Medical Association (Declaration of Helsinki).
2.2Study design and setting
A national multi-centre audit of PTL was completed in response to the Covid-19 pandemic over a six-month period (March to September 2020). The background and development of the project has been described in detail previously (Govender et al., 2021). This is a secondary analysis of data collected during the audit.
2.3Participants
All PTL under the care of participating centres were eligible for inclusion. Data were collected during the six-month period on PTL who were reviewed by Speech and Language Therapy (SLT) either in person or via telehealth during the first national lockdown.
2.4Data collection
Data were obtained via case note review and survey questions. A data capture worksheet (devised in Excel, password protected and encrypted) was used to collect data. Personal identifying information was minimised as advised by the information governance team. Verbal patient consent was obtained, whenever possible.
Data were collected on the potential explanatory variables described above. The type of tracheostoma cover used was recorded at two time points: before the onset of the Covid-19 pandemic (time point 1) and during the six-month period of data collection (time point 2). This paper reports on data collected from time point 1 to describe HME use among PTL in England and Wales before the onset of Covid-19. Data on incidence of Covid-19 infection, hospital admission and shielding advice were also collected and have been reported previously (Govender et al., 2021). Detailed analysis of factors influencing primary communication method will be reported independently of this paper.
2.5Data analysis
Analyses were carried out using SPSS for Windows. A univariable analysis was initially performed to evaluate the association between each potential explanatory variable and HME use, using Pearson’s chi-square test for categorical variables and the two-sample t-test or Mann-Whitney U test for continuous variables. Logistic regression analysis was conducted to examine the association of selected variables with HME. A backwards selection procedure was used to determine the final model (criteria for entry p < 0.05 and for removal p > 0.1). The overall fit of the model was ascertained using the Hosmer and Lemeshow goodness of fit test.
3Results
3.1Participants
Twenty-five centres from England and one centre from Wales submitted data for analysis. Data were collected on a total of 1216 PTL. Details of the participating centres and patient demographics are described in previous work (Govender et al., 2021).
3.2HME vs non-HME use
Data on type of tracheostoma cover were available for 1097 PTL. The majority (n = 835, 69%) used a closed-system HME. A range of alternative tracheostoma covers was used by 17% (n = 219). Only four percent (n = 43) were recorded as not using a tracheostoma cover (Table 1). For subsequent analysis PTL were grouped into HME users (n = 835, 69%) or non-HME users (n = 262, 21%). One hundred and nineteen (10%) PTL were excluded from further analysis due to missing data. Patient demographics are illustrated in Table 2.
Table 1
Type of tracheostoma cover used by PTL
| Tracheostoma cover | N | % |
| HME | 835 | 69% |
| Foam cover only | 50 | 4% |
| Bib only | 139 | 11% |
| Bib and foam cover | 14 | 1% |
| Other | 16 | 1% |
| None | 43 | 4% |
| Missing data | 119 | 10% |
Table 2
Patient demographics, HME vs non-HME
| Variable | HME | Non- HME | p value |
| Age* | 69.06 (9.8) | 70.8 (10.8) | 0.02 |
| Gender*** | 0.01 | ||
| Male | 694 (78%) | 200 (22%) | |
| Female | 141 (69%) | 62 (31%) | |
| Time elapsed since surgery (months)** | 59 [24–120] | 108 [49–191] | <0.0001 |
| Living circumstance*** | 0.01 | ||
| Living with someone | 558 (79%) | 151 (21%) | |
| Lives alone | 259 (74%) | 93 (26%) | |
| In care facility | 10 (42%) | 14 (58%) | |
| Other | 8 (67%) | 4 (33%) | |
| Employment*** | 0.19 | ||
| Retired | 571 (75%) | 190 (25%) | |
| Unemployed | 61 (77%) | 18 (23%) | |
| Full-time | 59 (83%) | 14 (17%) | |
| Part-time | 41 (75%) | 7 (25%) | |
| Sick leave | 15 (78%) | 5 (22%) | |
| Other | 52 (78%) | 15 (22%) | |
| Missing | 36 (73%) | 13 (27%) | |
| Distance from centre*** | 0.92 | ||
| <5miles | 211 (74%) | 75 (26%) | |
| 5–10 miles | 262 (77%) | 80 (23%) | |
| 11–20 miles | 193 (77%) | 59 (23%) | |
| >20 miles | 165 (78%) | 47 (22%) | |
| Missing | 4 (80%) | 1 (20%) | |
| Communication method*** | <0.0001 | ||
| Surgical Voice Restoration (SVR) | 633 (80%) | 154 (20%) | |
| Non-SVR | 202 (65%) | 108 (35%) |
Summary statistics are *mean(std dev), **median [IQR] or ***counts(%).
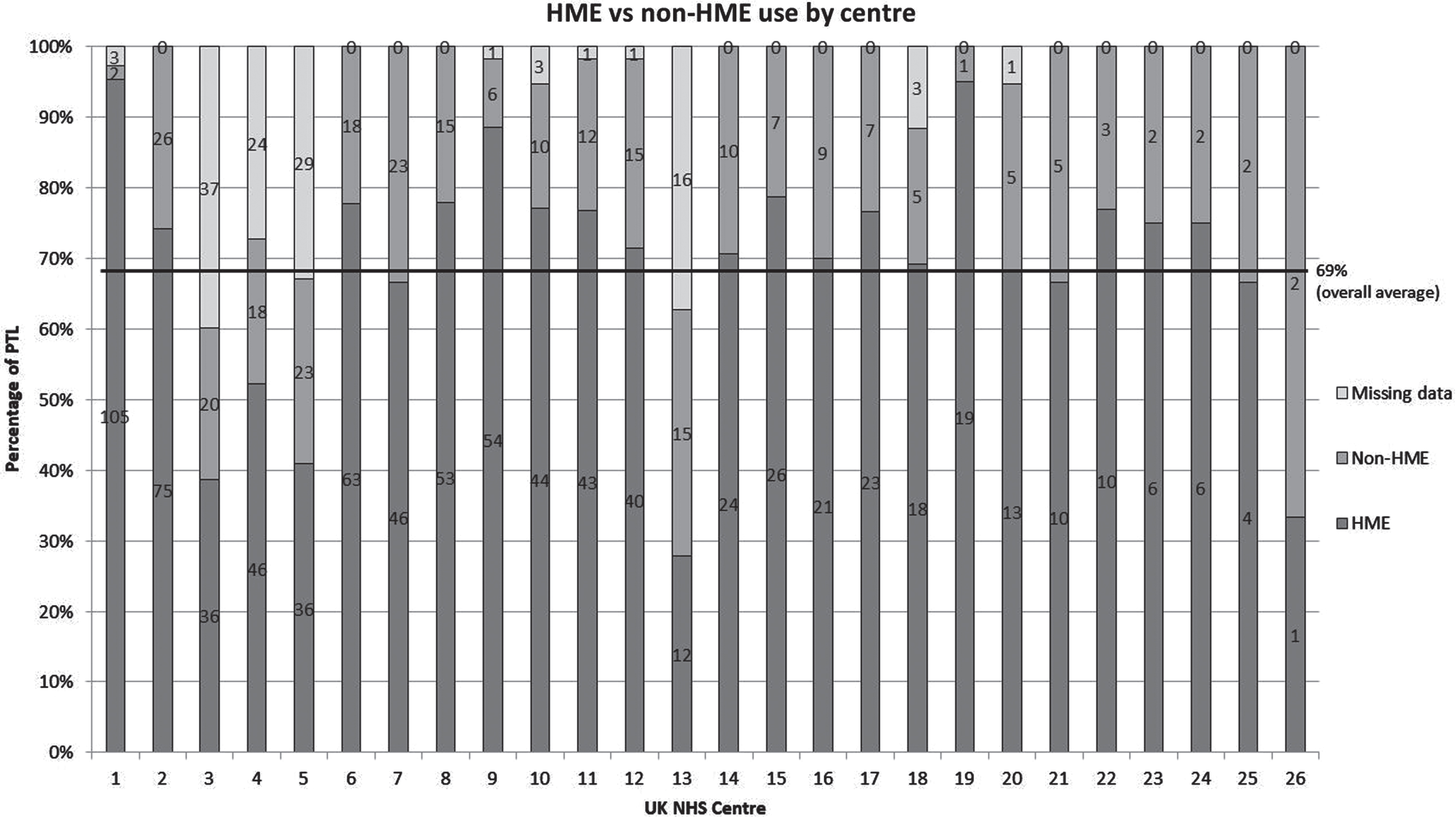
There was marked variation in the number of cases submitted for analysis and the percentage of PTL using HME across centres (Fig. 2). In two centres, (centres 1 and 19) 95% of PTL used a closed-system HME. However, in four centres (3, 5, 13 and 26) less than 50% did so. The amount of missing data also varied across centres. Centre 1 submitted the largest number of cases (n = 110) and reported the highest HME use. Centre 26 submitted only 3 cases with only 1 patient (33%) using an HME. Centre 13 had the lowest HME use at 28% (n = 12) but had a large amount of missing data (n = 16, 37%).
Fig. 2
HME vs non-HME use by centre.
3.3Factors associated with HME use
In univariable analysis, age (p = 0.02), gender (p = 0.01), time elapsed since surgery (p < 0.0001), living circumstances (p = 0.01) and communication method (p < 0.0001) demonstrated significant differences between HME users and non-HME users. Distance from the treating centre (p = 0.92) and employment status (p = 0.19) were not significant factors.
Following multiple regression analysis, time elapsed since surgery (p < 0.001), living circumstances (p = 0.003) and communication method (p < 0.001) remained statistically significant (Table 3). Time elapsed since surgery was longer for non-HME users than for HME users (median 108 months vs 59 months). Only 42% of PTL living in a care facility used an HME, compared with 77% of those living with someone or alone. SVR users were more likely to use an HME than non-SVR users (80% vs 65%).
Table 3
Variables associated with HME use from Multivariable Logistic Regression (Hosmer and Lemeshow Test >0.05)
| Variable | b | Std Error | Odds ratio | 95% CI | P value |
| Time elapsed since surgery | – 0.007 | 0.001 | 0.993 | 0.991–0.995 | <0.001 |
| Living circumstances | |||||
| Cohabiting (reference) | 0.003 | ||||
| Lives alone | – 0.263 | 0.172 | 0.768 | 0.549–1.076 | 0.125 |
| Lives in care | – 1.633 | 0.484 | 0.195 | 0.076–0.504 | <0.001 |
| Other | – 1.907 | 0.945 | 0.149 | 0.023–0.947 | 0.044 |
| Communication method | 0.851 | 0.176 | 2.34 | 1.66–3.31 | <0.001 |
4Discussion
To our knowledge, this study is the largest of current practice in the management of PTL and provides important data for benchmarking HME use. Our findings show that the majority of PTL (69%) included in the audit used a closed-system HME. While this is a lower proportion than has been quoted in previous studies (Ebersole et al., 2020), HME usage varied across centres from 28% to 95%. The centre with the largest number of cases also reported the highest HME use, while many of those centres with lower HME use also reported higher levels of missing data. This may reflect SLT capacity and resources at those centres, and such variability may indicate inequity of service across regions.
Although age was significant at univariable analysis, this was not retained following multivariable analysis indicating that older PTL are not disadvantaged in access to pulmonary rehabilitation. Similarly, although males demonstrated higher use of HME than females (78% vs 69%), this was not significant in multivariable analysis. Employment status and distance from the treating centre were not significant, suggesting that these factors do not impact on access to rehabilitation and advice or influence decision-making around humidification.
Factors found to be significantly associated with HME use in multivariable logistic regression were time elapsed since surgery, living circumstances and primary communication method.
4.1Time elapsed since surgery
Average time post-surgery was 96 months (range 0–578 months). PTL who were longer post-surgery were less likely to use an HME. Adherence to HME use is improved with early introduction (Pedemonte-Sarrias et al., 2013). Therefore, PTL who had surgery since closed-system HMEs have been widely available on prescription are perhaps more likely to have commenced early use and be ongoing HME users than those who had surgery before this time. Average time elapsed since surgery for PTL with non-HME was nine years in this study. Considering HMEs have been available on prescription since the mid-1990 s, clearly other factors are involved.
4.2Living circumstances
Although previous studies have analysed factors that might predict discharge destination following laryngectomy (Panwar et al., 2018), impact of living circumstances on HME use has not been explored, as far as we are aware. We found that PTL living in a care facility were significantly less likely to use an HME. This may relate to wider issues around the complexity of adherence to healthcare recommendations in care facilities (Hughes, 2008) and has important implications for the pulmonary health of this vulnerable group. Given HME use involves specialist intervention and ongoing use of specialist consumables, it may be that lower usage in care facilities indicates a need for training and therapeutic input in this setting. Further investigation is warranted.
4.3Communication method
It is recognised that a closed-system HME improves digital occlusion for voicing and better speech intelligibility for SVR users (Ackerstaff et al., 1998, 2003). Therefore, it may be expected that PTL with SVR are more likely to use an HME. Our findings are consistent with these studies. This highlights the importance of pulmonary rehabilitation for non-SVR users, who may receive less direct SLT intervention over time than those PTL receiving regular input for voice prosthesis management.
4.4Limitations of the study
This study reports on a range of factors that may influence HME use. However, there are additional factors that may account for the variability. To optimise participation in the audit, a limited data set was selected, inevitably leading to a series of unknowns. For example, data on duration of HME use was not collected. Full adherence is considered to be ≥20 hours per day (Brook et al., 2013) and various factors could influence this. We did not collect data on the following: barriers to HME use, HME suitability for PTL or which MDT member takes responsibility for pulmonary rehabilitation at each centre. The experience level of clinicians and specific requirements around training and recommendations for HMEs could be explored in future work. We also recognise that there may be some inherent bias because centres who chose to participate in the national audit may generally be better resourced and consequently invest greater efforts in promoting HME use. There was also variation in numbers of participating centres across regions. Notwithstanding, we hope that the large numbers of individual patient data go some way toward mitigating this possible bias.
There was an amount of missing data in this study. It is not known whether this was due to service pressures, reduced contact with PTL due to the Covid-19 pandemic or other factors.
4.5Future directions
Several professional organisations produced guidelines during the Covid-19 pandemic that may have influenced advice given to patients regarding humidification, including advice regarding the use of specialist viral filter HMEs (Kligerman et al., 2020; Varghese et al., 2021; Parrinello et al., 2020). A survey of PTL in the USA (Searl et al., 2021) found that more patients reported self-initiated changes to their HME use due to the pandemic than their clinicians had advised. We note however, that the ability of closed-system HMEs to protect users against SARS-CoV-2 has not been demonstrated. The current study presents data on use in England and Wales pre-Covid-19 (time point 1). Future work could investigate behaviour change as a result of the pandemic. The impact of social factors that may outweigh clinician advice, such as the impact of marketing, social media and peer influence (Searl et al., 2021), could also be explored.
For the purpose of current analysis, PTL were divided into those using a commercially available closed-system (“HME”) and all others (“non-HME”). However, some researchers have found bibs to be superior to closed-system HMEs in terms of humidity and temperature (Quail et al., 2016). Future work could explore factors associated with the use of non-HMEs.
This study identified marked variability in HME use, with some centres reporting much higher HME use than others. The underlying reasons for variation in practice could be examined and training needs identified to support equity of access to pulmonary rehabilitation across centres.
Current findings suggest there may be education and training needs around pulmonary rehabilitation for PTL who are less likely to use an HME, such as those who are longer post-surgery, those living in care facilities, and non-SVR users. This paper supports the need to target education and training to ensure equity of access to pulmonary rehabilitation for all PTL.
5Conclusions
In England and Wales most PTL use a closed-system HME to maximise pulmonary health after surgical alteration to their upper airway. Use of HMEs varies across participating treatment centres but was found to be primarily impacted by certain factors: time elapsed since surgery (PTL with a shorter time since surgery were more likely to use an HME), living circumstances (PTL living in a care facility were less likely to use an HME than those living alone or with someone) and primary communication method (SVR users were more likely to use an HME than PTL without SVR). The average of 69% of PTL using an HME serves as a benchmark for services in England and Wales. Education and training should be targeted to ensure equity of access to pulmonary rehabilitation for all PTL.
Acknowledgments
The authors would like to thank all the speech and language therapists who assisted with data collection, the patients who participated in the audit, and Malcolm Babb and the National Association of Laryngectomy Clubs for valuable feedback.
No specific funding was obtained for this project.
Author contributions
RG and JP designed the work; RG, JP, JD, KF, SW, CG and ER acquired and analysed data; JD, KF, SW, CG, ER, RG and JP drafted, revised and approved the manuscript. All authors agree to be accountable for all aspects of the work.
Conflict of interest
The authors have no conflict of interest to report. Roganie Govender is on the editorial board of Advances in Communication and Swallowing. She had no involvement in the peer review process of this paper.
References
1 | Ackerstaff, A. H. , Hilgers, F. J. M. , Balm, A. J. M. & Bin Tan, I. ((1998) ). Long-term compliance of laryngectomzed patients with a specialized pulmonary rehabilitation device: Provox Stomafilter. The Laryngoscope, 108: (2):257–260. https://doi.org/10.1097/00005537-199802000-00018 |
2 | Ackerstaff, A. H. , Fuller, D. , Irvin, M. , Maccracken, E. , Gaziano, J. & Stachowiak L. ((2003) ). Multicenter study assessing effects of heat and moisture exchanger use on respiratory symptoms and voice quality in laryngectomized individuals. Otolaryngol Head Neck Surg, 129: (6):705–712. https://doi.org/10.1016/S0194-59980301595-X |
3 | Ackerstaff, A. H. , Zuur, J. K. & Hilgers, F. J. M. ((2007) ). Pulmonary Function and Rehabilitation. In Ward, E. C. & van As-Brooks, C. J., (Eds.), Head and Neck Cancer: Treatment, Rehabilitation and Outcomes, Plural Publishing, 313–324. |
4 | Brook, I. , Bogaardt, H. & van As-Brooks, C. J. ((2013) ). Long-term use of heat and moisture exchangers among laryngectomees: Medical, social, and psychological patterns. Ann Otol Rhinol Laryngol, 122: (6):358–363. https://doi.org/10.1177/000348941312200602 |
5 | Clarke, P. , Radford, K. , Coffey, M. & Stewart, M. ((2016) ). Speech and swallow rehabilitation in head and neck cancer: United Kingdom National Multidisciplinary Guidelines.&. Otology, 130: , 176–180 https://doi.org/10.1017/S0022215116000608 |
6 | Ebersole, B. , Moran, K. , Gou, J. , Ridge, J. , Schiech, L. , Liu, J. C. & Lango, M. ((2020) ). Heat and moisture exchanger cassettes: Results of a quality/safety initiative to reduce postoperative mucus plugging after total laryngectomy. Head Neck, 42: (9):2453–2459. https://doi.org/10.1002/hed.26267 |
7 | Govender, R. , Behenna, K. , Brady, G. , Coffey, M. , Babb, M. & Patterson, J. M. ((2021) ). Shielding, hospital admission and mortality among 1216 people with total laryngectomy in the UK during the COVID-19 pandemic: A cross-sectional survey from the first national lockdown. Int J Lang Commun Disord, 56: (5):1064–1073. https://doi.org/10.1111/1460-6984.12656 |
8 | Guye, C. ((1887) ). On the function of the nose in respiration. The Journal of Laryngology and Rhinology, 1: (1):41–43. https://doi.org/10.1017/S1755145500158956 |
9 | Hughes, C. ((2008) ). Compliance with medication in nursing homes for older people: Resident Enforcement or Residential Empowerment? Drugs and Aging, 25: (6)). https://doi.org/10.2165/00002512-200825060-00001 |
10 | Jones, A. S. , Young, P. E. , Hanafi, Z. B. , Makura, Z. G. G. & Fenton, J. E. Hughes, J. P. ((2003) ). A study of the effect of a resistive heat moisture exchanger (Trachi-naze) on pulmonary function and blood gas tensions in patients who have undergone a laryngectomy: A randomized control trial of 50 patients studied over a 6-month period. Head & Neck, 25: (5):361367. https://doi.org/10.1002/hed.10264 |
11 | Kligerman, M. P. , Vukkadala, N. , Tsang, R. K. Y. , Sunwoo, J. B. , Holsinger, F. C. , Chan, J. Y. K. , Damrose, E. J. & Kearney, A. Starmer, H. M. ((2020) ). Managing head and neck cancer patients with tracheostomy or laryngectomy during the COVID-19 pandemic.&. Neck, 42: (6):1209–1213. https://doi.org/10.1002/hed.26171 |
12 | Lorenz, K. J. & Maier, H. ((2009) ). Pulmonale Rehabilitation nach totaler Laryngektomie durch die Verwendung von HME (Heat Moisture Exchanger) [Pulmonary rehabilitation after total laryngectomy using a heat and moisture exchanger (HME)]. Laryngo -Rhino-Otologie, 88: (8):513–522. German https://doi.org/10.1055/s-0029-1225619 |
13 | Macri, G. F. , Bogaardt, H. , Parrilla, C. , Minni, A. , D’Alatri, L. , de Vincentiis, M. , Greco, A. & Paludetti, G. ((2016) ). Patients’ experiences with HMEs and attachments after total laryngectomy. Clinical Otolaryngology, 41: (6):652–659. https://doi.org/10.1111/coa.12578 |
14 | Maurizi, M. , Paludetti, G. , Almadori, G. , Ottaviani, F. & Todisco T. ((1986) ). Mucociliary clearance and mucosal surface characteristics before and after total laryngectomy. Acta Oto-Laryngologica, 102: (1-2):136–145. https://doi.org/10.3109/00016488609108658 |
15 | Panwar, A. , Wang, F. , Lindau, R. , Militsakh, O. , Coughlin, A. , Smith, R. , Sayles, H. , Lydiatt, D. & Lydiatt, W. ((2018) ). Prediction of discharge destination following laryngectomy. Otolaryngol Head Neck Surg, 159: (6):1006–1011. https://doi.org/10.1177/0194599818792211 |
16 | Parrinello, G. , Missale, F. , Sampieri, C. , Carobbio, A. L. C. & Peretti, G. ((2020) ). Safe management of laryngectomized patients during the COVID-19 pandemic. Oral Oncology, 107: , 104742. https://doi.org/10.1016/j.oraloncology.2020.104742 |
17 | Pedemonte-Sarrias, G. , Villatoro-Sologaistoa, J. C. , Ale-Inostroza, P. , Lopez-Vilas, M. , Leon-Vintro, X. & Qer-Agusti, M. ((2013) ). M. Chronic adherence to heat and moisture exchanger use in laryngectomized patients. Acta Otorrinolaringol Esp, 64: (4):247–252. https://doi.org/10.1016/j.otorri.2012.07.005. |
18 | Quail, G. , Fagan, J. J. , Raynham, O. , Krynauw, H. , John, L. R. & Carrara, H. ((2016) ). Effect of cloth stoma covers on tracheal climate of laryngectomy patients. Head & Neck. Apr;38 Suppl: 1: E480–7 https://doi.org/10.1002/hed.24022 |
19 | Scheenstra, R. J. , Muller, S. H. , Vincent, A. , Ackerstaff, A. H. , Jacobi, I. & Hilgers F. J. ((2010) ). Short-term endotracheal climate changes and clinical effects of a heat and moisture exchanger with an integrated electrostatic virus and bacterial filter developed for laryngectomized individuals. Acta Otolaryngol, 130: (6):739–746. https://doi.org/10.3109/00016480903382790 |
20 | Searl, J. , Kearney, A. , Genoa, K. & Doyle, P.C. ((2021) ). Clinical Experiences of People with a Laryngectomy During the SARS COVID-19 Pandemic. Am J Speech Lang Pathol, 30: (6):2430–2445. https://doi.org/10.1044/2021_AJSLP-21-00117 |
21 | Varghese, J. J. , Aithal, V. U. & Rajashekhar, B. ((2021) ). Self-care and clinical management of persons with laryngectomy during COVID-19 pandemic: A narrative review. Support Care Cancer, 29: (12):7183–7194. https://doi.org/10.1007/s00520-021-06333-3 |
22 | Von Elm, E. , Altman, D. G. , Egger, M. , Pocock, S. J. , Gøtzsche, P. C. & Vandenbroucke, J. P. ((2007) ). The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. The Lancet, 370: (9596):1453–1457. https://doi.org/10.1016/S0140-6736(07)61602-X |




