Understanding the why: The integration of trauma-informed care into speech and language therapy practice
Abstract
This article aims to highlight the need to integrate Trauma-Informed Care (TIC) into the practice of Speech and Language Therapy. TIC is a strength-based framework underpinned by an understanding and responsiveness to the widespread pervasiveness and impact of trauma. The literature on TIC within the field of Speech and Language Therapy is in its infancy but is progressing. In this context, there is an absence of clear guidelines for TIC in the field to support providers and administers to understand the relevance, underlying theory, and application to practice. In this paper we outline the theoretical underpinnings and application to practice. We argue that the profession requires an ongoing commitment to continuous research to corroborate communication-specific best practices of TIC to support clinicians in translating those findings into practice to best support clients.
1Introduction to trauma-informed practice
Trauma-Informed Care (TIC) is a strength-based framework underpinned by an understanding and responsiveness to the widespread pervasiveness and impact of trauma (Hopper, Bussuk & Olivet, 2010). Trauma occurs when stress overwhelms a person’s capacity to cope (Cook et al., 2003). Prolonged exposure to adversity at an early age can confer significant risk for adverse physical and mental health outcomes across the lifespan (Berliner & Kolko, 2016). As DeCandia and Guarino (2015) posit, the toll that trauma places on society, necessitates that trauma and its impact are addressed across all systems of care. The overarching aim of TIC is to facilitate opportunities that support resiliency and recovery from exposure to traumatising experiences. TIC aims to foster a sense of control and empowerment through a focus on embodied, relational, and psychological safety, for both service providers and service users (Hopper et al., 2010). TIC also considers the lived and living experiences of trauma within the person’s ecological context and thus, all systems of care have a role to play in supporting resiliency and recovery, including the field of Speech and Language Therapy.
For Speech and Language Therapists (SLTs) to be trauma-informed, they must understand the potential impact and relevance of trauma to their clients. TIC aims to promote widespread trauma awareness, knowledge and practices that promote resiliency and wellbeing across a system of care (Substance Abuse and Mental Health Services Administration, 2014). This can be applied across three spheres of practice (Lotty, 2021). Firstly, trauma-specific evidence-based treatments (EBT) which require clinical training and supervision to specifically treat trauma (Mersky, Topitzes & Britz, 2019). Secondly, trauma-informed practice by non-trauma specific clinicians, and lastly, trauma-informed organisations that embed the guiding principles of TIC at an organisational level (Bloom, 2010).
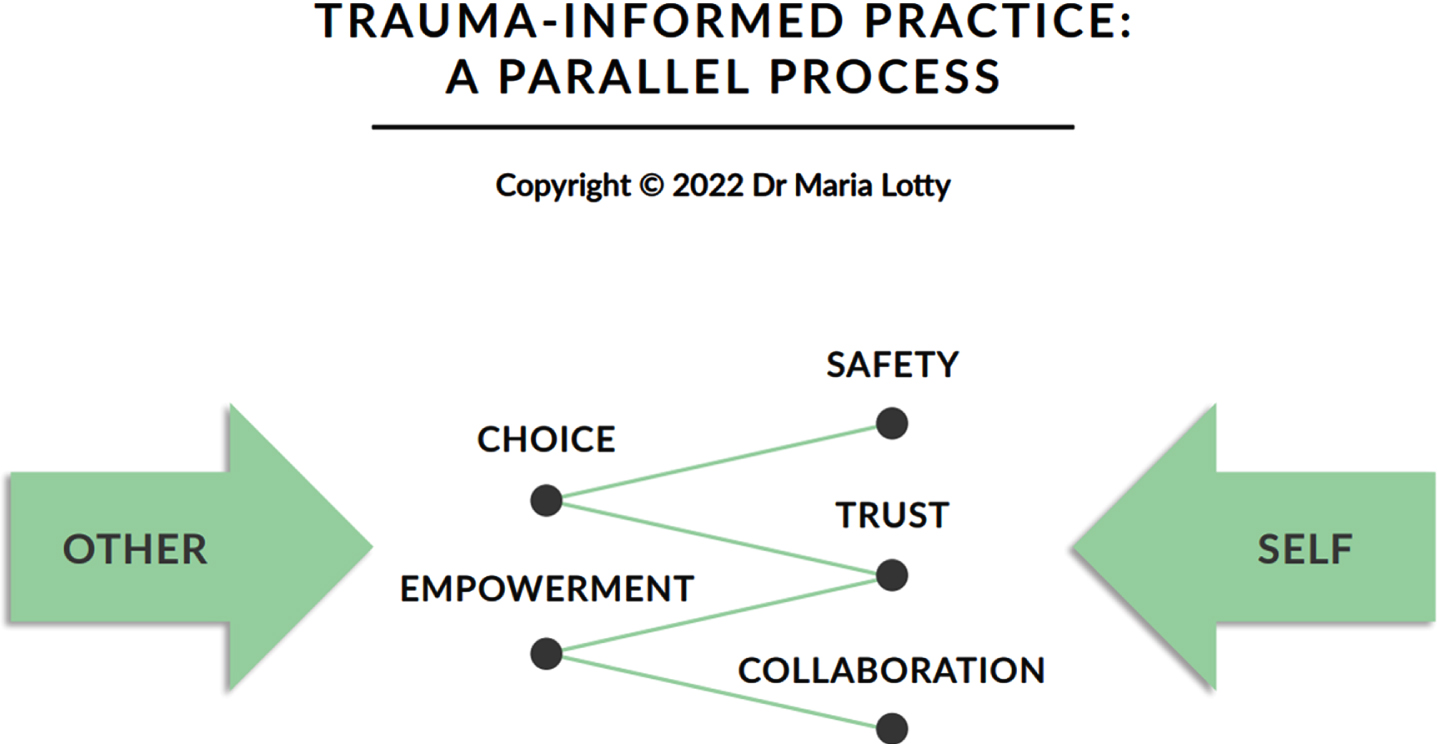
This article focuses on trauma-informed practice that can be carried out by clinicians and carers working outside formal trauma-clinical settings, including allied health professionals such as SLTs. Building on SAMHSA (2014) key principles of safety, choice, trust, collaboration and empowerment, Lotty (2021) emphasises the parallel process in TIC for the client and the clinician (see Fig. 1). This process refers to experiences that run in parallel to one another within a relationship, such as the SLT and their client, that often involve developing an understanding of the lived experience of trauma, ongoing impact, developing ways to effectively cope and minimise or avoid re-traumatisation.
Fig. 1
Trauma-informed practice: a parallel process.
Therefore, trauma-informed practice places emphasis on the centrality of safe and secure relationships as a medium for healing (Lucio & Nelson, 2016). The practice places an impetus on understanding the lived and living experience of trauma and how this drives behaviours that were developed as ways of coping (Bunting et al., 2019). While a SLT is not directly targeting healing from trauma in their clinical goals, by engaging in trauma-informed practice the therapeutic relationship between the clinician and the client allows for an additional context within which healing can occur.
The landmark Adverse Childhood Experiences (ACE) study (Felitti et al., 1998) in the United States, highlights the significant connection between childhood exposure to stress and trauma and adverse outcomes across the lifespan. The study has been replicated and results consistently highlight a significant correlation between childhood stress and trauma exposure, physical health problems, high risk behaviours, and cognitive and socioemotional difficulties (Bartlett & Steber, 2019; Bellis, Ashton, Hughes, Ford, Bishop, & Paranjothy, 2016). It is worth noting that intergenerational pathways of trauma may pose substantial risks for ACEs in the next generation, particularly in the absence of positive and protective influences on development, such as a secure child-caregiver relationship (Narayan, Lieberman & Masten, 2021).
Furthermore, longitudinal studies detail an enduring risk of socioemotional and behavioural problems from childhood into early adulthood for clients presenting with speech and language disorders (Whitehouse, Watt, Line & Bishop, 2009). Research reports a high prevalence of communication difficulties in those who present with psychopathology (Speech Pathology Australia, 2018), and a high likelihood of unidentified communication difficulties amongst children and adolescents with social, emotional, and behavioural problems (Hollo, Wehby & Oliver, 2014). These findings, in addition to the association between trauma and language difficulties in young children, point to a bidirectional relationship between communication and mental health difficulties (Irish Association of Speech and Language Therapists, 2021), making trauma clearly relevant to the field of Speech and Language Therapy.
2The role of child-caregiver relationships
In the face of adversity, supportive relationships can provide buffering to the impact of stress, which enables children to withstand or recover from adversity and learn important skills, thus building resilience. In fact, many sources, including Bartlett and Steber (2019) and the Center on the Developing Child at Harvard University (2022), postulate that the strongest factor linked with resilience in childhood is the consistent presence of a sensitive, nurturing, and responsive adult.
Hence, restorative child-caregiver relationships and the cultivation of social support can be considered an aim of TIC (Lotty, Dunn-Galvin & Bantry-White, 2020; McLaughlin, Colich, Rodman & Weissman, 2020). When working within early communication development, SLTs deliver intervention within the context of child-caregiver interactions. Therefore, understanding the importance these interactions and the nature of a client’s relationship, particularly when a child has faced adversity, is directly applicable to the work of a SLT (McGlinn, 2020).
Attachment processes are a fundamental part of human development, and a knowledge of attachment theory is necessary for understanding how trauma in the context of caregiving relationships can impact development (Rupert & Bartlett, 2022; Smith, William, Walsh & McCartney, 2016). An attachment relationship can be conceptualised as a deep and enduring emotional bond that connects two individuals across space and time (Ainsworth, 1973; Bowlby, 1969). Infants innately seek closeness with a primary caregiver to provide them with safety and reliable information about the world (Fonagy, Gergely & Target, 2007). Secure child-caregiver attachment is supported by the infant’s confidence in their caregivers’ consistent, reliable responses to their needs. Overtime, through reciprocal safe experiences, a trusting relationship is facilitated that greatly supports development (Ainsworth, 1973).
Insecure attachment styles develop following inconsistent or unavailable child-caregiver experiences in childhood that represent patterns of behaviour (Doolan & Byrant, 2021, Tronick, Als, Adamson, Wise & Brazelton, 1978). There are three types of insecure attachment that include avoidant, ambivalent (Ainsworth, 1973) and disorganised (Main & Soloman, 1986). Having an insecure attachment adversely impacts the child-caregiver relationship and in turn can negatively impact the developmental capacities across all areas of child development including the capacity to self-regulate, early knowledge of agency, early capabilities for receptive and expressive language and ability to deal with stress and trauma (Cook et al., 2003).
In the absence of the buffering provided by secure reliable relationships, research demonstrates the devastating, long-term impact of traumatic stress on the developing brain and body (DeCandia & Guarino, 2015; McCrory, de Brito & Viding, 2012). Prolonged, or frequent activation of the stress response, known as toxic stress, leads to a dysregulation of the neuroendocrine immune circuitry (Kuzminskaite, Vinkers, Elzinga, Wardenaar, Giltay & Penninx, 2020) and can overwhelm the neurophysiological system for coping with stress. This produces altered levels of hormones and neurotransmitters and ultimately leads to changes in brain architecture and multiple organ systems (Bucci et al., 2016).
Toxic stress also results in a heightened baseline state of physiological arousal and increased sensitivity to internal and external triggers (Center on the Developing Child at Harvard University, 2022; SAMSHA, 2014).
3The role of regulation
Neurobiological research illuminates that cognitive approaches, whether to speech and language interventions or mental health interventions are less likely to be effective when the stress arousal system is dysregulated (Raio, et al., 2013). Exposure to trauma frequently disorganises low brain areas that regulate homeostatic life support functions (Gaskill, 2019). This is manifested in the body as an embodied dysregulated experience outside of conscious awareness (Porges, 2011). Thus, it is accepted in the therapeutic community that the gold standard for trauma therapy is a phased approach, focusing on building embodied safety as a foundation (van der Kolk, 2014).
This principle carries through to TIC interventions by clinicians supporting increased embodied regulation prior to proceeding to work on cognitive tasks (Lotty, Bantry-White & Dunn-Galvin, 2021). Until these regions achieve statis, the individual cannot access higher brain areas to support cognitive engagement. In this respect, SLTs need to support a client’s embodied regulation, before expecting a client to be able to work on higher level cognitive skills.
The need to support regulation applies to clients, as well as the potential need to support a child’s caregiver in the importance of co-regulation of their child.
Furthermore, trauma-informed practice requires the SLT to be attuned to their own state of regulation in sessions. The clinician is thus required to develop their own skills to promote regulation such as grounding and deep breathing. Grounding which involves noticing or slowing down breathing, tapping, or counting fingers as the breath goes in, can reduce autonomic nervous system activation (Yehuda, 2016). Deep breathing helps lower the neurological arousal that takes place during a stressful reaction. Others find prearranged hand movements (e.g., lowering palm into a gentle ‘calm down’ motion) helpful in calming them enough to listen and orientate to their surroundings (Yehuda, 2016).
The aforementioned impact of trauma and the neurobiology of stress can place children at greater risk for adverse developmental, emotional, and academic outcomes (McCrory et al., 2012). Converging evidence suggests that trauma exposure, particularly in early life, alters emotional regulatory capacities, which is the ability to modify one’s arousal and emotional state to promote adaptive behaviour (Gross & Thompson, 2007). Indeed, early life trauma exposure is a potent risk factor for neuropsychiatric disorders including anxiety, depression, and posttraumatic stress disorder, that are also hallmarked by abnormalities in the processing and regulation of emotion (Marusak, Martin, Etkin & Thomason, 2015).
Children who have experienced adversity are more vulnerable to dysregulation of affect and behaviour, distortions in attributions, interpersonal difficulties and difficulties with executive functioning (D’Andrea, Ford, Stolbach; van der Kolk, 2012).
4Trauma-informed care and communication skills intervention
There is a growing body of evidence suggesting that children who experience maltreatment have significantly poorer speech and language abilities in terms of receptive, expressive, and pragmatic language skills when compared to children who had not experienced maltreatment (Rupert & Bartlett, 2022). This is reflected in a number of meta-analyses (Byrne, 2017; Hyter, 2021; Sylvester, Bussieres & Bouchard, 2016) and Speech-Language Pathology Australia’s Clinical Guidelines to Speech Pathology in Mental Health Services, which emphasise infant and early childhood mental health and attachment as it relates to communication development (Speech Pathology Australia, 2018). Studies applying trauma-informed practice to Speech and Language Therapy are emerging (Haritopoulos, 2022), as well as those exploring SLTs attitudes and knowledge about trauma-informed practice (Roberson & Lund, 2022).
A trauma-informed SLT underpins their practice with the core TIC principles and brings a trauma-informed mind set and skillset to their practice (Lotty, 2021).
Acknowledging and understanding the underlying impact trauma history can have on a client’s communication abilities and presentation, will mean including trauma as part of a thorough case history and will alter the way the SLT addresses their client’s communication needs in intervention. The SLT, as a starting point, is concerned with supporting the client to experience a felt sense of safety in their presence and in the intervention environment. For example, by clearly explaining to clients what they can expect, by giving choices and control and by asking a child’s caregiver what might make their child feel most comfortable. The trauma-informed clinician would also know the importance of trying to understand and anticipate the client’s triggers as to avoid re-traumatization in the activities selected as part of intervention (Yehuda, 2016). For example, a child may be sensitive to touch from adults due to a history of physical abuse yet would benefit from tactile prompts for speech production and would require more support in establishing a felt sense of safety prior to tactile motor speech therapy.
The trauma informed SLT understands the importance of collaborative practice with the key players in the child’s life that all have a role in supporting the child’s resilience and recovery. These often include caregivers, teachers, early years professionals, social workers, and other mental health professionals who through collaborative practice can support the child through a consistent and coordinated approach.
Through collaborative practice, the SLT has a role to play in supporting those providing trauma-specific treatment in helping them understand the child’s communication abilities, receiving input from those who understand the details of the child’s trauma history, and in being part of a coordinated service plan for clients who have trauma history. For example, it may be clinically beneficial that the child and family access trauma-specific services before undertaking communication intervention. This may be the case in situations where there is a major rupture within the child-caregiver relationship, or where caregivers are experiencing significant mental health challenges of their own.
Trauma-informed practice also involves the risk of vicarious trauma to the SLT. Vicarious trauma is considered a profound and lasting emotional and psychological consequence of repeated indirect exposure to the traumatic experiences of others (Padmanabhanunni & Gqomfa, 2022). Incidences which increase vulnerability to vicarious trauma in the work environment include excessive workload and unclear scope of work (Ravi, Gorelick & Pal, 2021). Trauma-informed SLTs and their supervisors must therefore understand the importance of self-care to reduce the risk of the onset of vicarious trauma that may potentially lead to compassion fatigue and burnout (Rupert & Bartlett, 2022).
SLTs also require the systems they work in to acknowledge their exposure to vicarious trauma and governing bodies regarding Speech and Language Therapy need to delineate relevant scope of work and practice guidelines to support SLTs in this regard.
Finally, while the training and governance of SLTs differs globally, trauma is a global phenomenon. Understanding the neurobiology and impact of trauma allows the practitioners to apply this learning to all clients they work with regardless of where they practice. Therefore, it would be highly beneficial for TIC to be included in all SLT training core curriculum, and for governing bodies to include trauma-related practice guidelines within their scope. This of course could then be tailored to the local context but the importance of understanding the impact of trauma is universal.
5Conclusion
TIC is a relatively new framework for working with individuals who experience trauma. The evidence-base to support its effectiveness is still in the early stages of development. This is even more so the case in the application of TIC to practice within Speech and Language Therapy. Nevertheless, the relevance of TIC to work within Speech and Language Therapy beyond specialized treatment mental health settings cannot be understated.
Thus, we have highlighted some of the key foundational reasons for the relationship between trauma exposure and the field of Speech and Language Therapy, some of the key ways that elements of TIC can be implemented within Speech and Language Therapy, and hope to also shed light on the need for an ongoing commitment to continuous research to corroborate best practice of TIC specific to communication sciences. This will in turn support the further application of TIC to enhance the services provided to clients and supports provided to clinicians as well.
Acknowledgments
The authors have no acknowledgements.
Conflict of interest
The authors have no conflicts of interest to declare.
References
1 | Ainsworth, M. D. S. ((1973) ). The development of infant-mother attachment. In B. Cardwell & H. Ricciuti (Eds). Reviewof child development research (Vol.3, pp. 1–94) Chicago: University of Chicago Press. |
2 | Bartlett, J. D. , & Steber, K. (2019). How to implement Trauma-Informed Care to build resilience to child trauma. Retrieved from: How to Implement Trauma-Informed Careto Build Resilience to Childhood Trauma – Child Trends. |
3 | Bellis, M. , Ashton, K. , Hughes, K. , Ford, K. , Bishop, J. , & Paranjothy, S. ((2016) ). Adverse childhood experiences (ACEs) in Wales and their impact on health in the adult population. European Journal of Public Health, 26: (suppl 1). Retrieved from: https://doi.org/10.1093/eurpub/ckw167.009 |
4 | Berliner, L. , & Kolko, D. J. (2016). In Hanson R. F., Lang J.(Eds.), Trauma informed care: A commentary and critique. SAGE Publications. https://doi.org/10.1177/1077559516643785. |
5 | Bloom, S. L. , & Farragherf, B. , ((2010) ). Destroying sanctuary: The crisis in human service delivery systems. Oxford University Press. |
6 | Bowlby, J. ((1969) ). Attachment and loss. Attachment, Vol 1, New York: Basic Books. |
7 | Bucci, M. , Marques, S. , Oh, Debora, S. , & Harris, N. B. ((2016) ). Toxic stress in children and adolescents. Advances in Paediatrics, 63: (1), 403–428. https://doi.org/10.1016/j.yapd.2016.04.002. |
8 | Bunting, L. , Montgomery, L. , Mooney, S. , MacDonald, M. , Coulter, S. , Hayes, D. , Davidson, G. , & Forbes, T. (2019). Developing trauma informed care in Northern Ireland: The child welfare system. Retrieved from: Developing trauma informed care in Northern Ireland: The child welfare system—Queen’s University Belfast (qub.ac.uk). |
9 | Byrne, N. ((2017) ). Systematic review of speech and language therapy outcomes for children who are in out of home care (OOHC). Speech, Language and Hearing, 20: (1), 57–61. https://doi.org/10.1080/2050571X.2016.1207399. |
10 | Center on the Developing Child at Harvard University (2022). Resilience. Retrieved from: Resilience (harvard.edu) |
11 | Cook, A. , Blaustein, M. , Spinazzola, J. , & Van der Kolk, B. (2003). Complex trauma in children and adolescents: White paper from the national child traumatic stress network complex trauma task force. Los Angeles: National Centre for Child Traumatic Stress. |
12 | D’Andrea, W. , Ford, J. , Stolbach, B. , Spinazzola, J. , & Van der Kolk, B. A. ((2012) ). Understanding interpersonal trauma in children: why we need a developmentally appropriate trauma diagnosis. American Journal of Orthopsychiatry, 82: (2), 187. https://doi.org/10.1111/j.1939-0025.2012.01154.x. |
13 | DeCandia, C. , & Guarino, K. ((2015) ). Trauma-Informed Care: An Ecological Response. Journal of Child and Youth Care Work, 25: , 7–32. https://doi.org/10.5195/jcycw.2015.69. |
14 | Doolan, E. L. , & Bryant, R. A. ((2021) ). Modifying insecure attachment style with cognitive bias modification. Journal of Behavior Therapy and Experimental Psychiatry, 73: , 101664. https://doi.org/10.1016/j.jbtep.2021.101664 |
15 | Felitti, V. J. , Anda, R. F. , Noredenberg, D. , Williamson, D. F. , Spitz, A. M. , Edwards, V. , . . . Marks, J. S. ((1998) ). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences 13 (ACE) Study. American Journal of Preventive Medicine, 14: (4), 245–258. https://doi.org/10.1016/S0749-3797(98)00017-8 |
16 | Fonagy, P. , Gergely, G. , & Target, M. ((2007) ). The parentinfant dyad and the construction of the subjective self. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 48: (3-4), 288–328. https://doi.org/10.1111/j.1469-7610.2007.01727.x. |
17 | Gaskill, R. (2019). Neuroscience Helps Play Therapists Go Low So Children Can Aim High. Retrieved from: Gaskill.pdf (ymaws.com) |
18 | Gross, J. J. , & Thompson, R. A. (2007). Emotion Regulation: Conceptual Foundations. In J. J. Gross (Ed.), Handbook of emotion regulation (pp. 3–24). The Guilford Press. |
19 | Haritopoulos, K. (2022). The Role of Speech-Language Pathologists in Trauma-Informed Practices: Feelings, Attitudes, and Reported Behaviours of Colorado School Speech-Language Pathologists. Master’s Thesis. University of Northern Colorado. |
20 | Hollo, A. , Wehby, J. H. , & Oliver, R. M. ((2014) ). Unidentified Language Deficits in Children with Emotional and Behavioral Disorders: A Meta-Analysis. Exceptional Children, 80: (2), 169–186. DOI: 10.1177/001440291408000203. |
21 | Hopper, E. K. , Bassuk, E. L. , & Oliver, J. ((2010) ). Shelter from the storm: Trauma-Informed Care in homelessness service settings. The Open Health Services and Policy Journal, 3: (2), 80–100. https://doi.org/10.2174/1874924001003020080 |
22 | Hyter, Y. D. ((2021) ). Childhood maltreatment consequences on social pragmatic communication: A systematic review of the literature. Perspectives of the ASHA Special Interest Groups, 6: , 262–287. https://doi.org/10.1044/2021_PERSP-20-00222 |
23 | Irish Association of Speech and Language Therapists (2021). IASLT response to: Appraisal of evidence for the effectiveness of Talking Therapies: Position Paper on Collaborative Layered Care Delivery Model for Talking Therapies. Retrieved from: response-to-interim-reports-on-the-moc-for-adults-accessingtalking-therapies-july2020-final.pdf (iaSpeech and Language Therapy.ie) |
24 | Kuzminskaite, E. , Vinkers, C. H. , Elzinga, B. M. , Wardenaar, K. J. , Giltay, E. J. , & Penninx, B. ((2020) ). Childhood trauma and dysregulation of multiple biological stress systems in adulthood: Results from the Netherlands Study of Depression and Anxiety (NESDA). Psychoneuroendocrinology 121: , 104835. https://doi.org/10.1016/j.psyneuen.2020.104835 |
25 | Lotty, M. ((2021) ). “Exploring Trauma-informed Foster Care as a Framework to Support Collaborative Social Worker - Foster Carer Relationships,” Irish Journal of Applied Social Studies, 21: (1), 34–50. Available at: https://arrow.tudublin.ie/ijass/vol21/iss1/4 |
26 | Lotty, M. , Dunn-Galvin, A. , & Bantry-White, E. ((2020) ). Effectiveness of a trauma-informed care psychoeducational program for foster carers–Evaluation of the Fostering Connections Program. Child Abuse & Neglect 102: , 104390. DOI: 10.1016/j.chiabu.2020.104390 |
27 | Lotty, M. , Bantry-White, E. , & Dunn-Galvin, A. ((2021) ). Trauma-informed care psychoeducational group-based interventions for foster carers and adoptive parents: A narrative review. Adoption & Fostering, 191–214. https://doi.org/10.1177/03085759211012492 |
28 | Lucio, R. , & Nelson, T. L. ((2016) ). Effective practices in the treatment of trauma in children and adolescents: From guidelines to organizational practices. Journal of Evidence-Informed Social Work, 13: (5), 469–478. https://doi.org/10.1080/23761407.2016.1166839 |
29 | Main, M. , & Solomon, J. (1986). Discovery of an insecure-disorganized/disoriented attachment pattern. In T. B. Brazelton & M.W. Yogman (Eds.), Affective development in infancy (pp. 506 95–124). Ablex Publishing. |
30 | Marusak, H. A. , Martin, K. R. , Etkin, A. , & Thomason, M. E. ((2015) ; 2014). Childhood trauma exposure disrupts the automatic regulation of emotional processing. Neuropsychopharmacology (New York, N.Y.), 40: (5), 1250–1258. https://doi.org/10.1038/npp.2014.311 |
31 | McCrory, E. , De Brito, S. A. , & Viding, E. The link between child abuse and psychopathology: A review of neurobiological and genetic research. Journal of the Royal Society of Medicine, ((2012) ) 105: (4), 151–156. https://doi.org/10.1258/jrsm.2011.110222 |
32 | McGlinn, S. ((2020) ). Communication and infant mental health. In C. Jagoe & I.Walsh (Eds.), Communication and Mental Health Disorders: Developing Theory, Growing Practice. J & R Press. |
33 | McLaughlin, K. A. , Colich, N. L. , Rodman, A. M. , & Weissman, D. G. ((2020) ). Mechanisms linking childhood trauma exposure and psychopathology: A transdiagnostic model of risk and resilience. BMC Medicine, 18: (1), 96–96. https://doi.org/10.1186/s12916-020-01561-6 |
34 | Mersky, J. P. , Topitzes, J. , & Britz, L. ((2019) ). Promoting evidence-based, trauma-informed social work practice. Journal of Social Work Education, 55: (4), 645–657. https://doi.org/10.1080/10437797.2019.1627261 |
35 | Narayan, A. J. , Lieberman, A. F. , & Masten, A. S. ((2021) ). Intergenerational transmission and prevention of adverse childhood experiences (ACEs). Clinical Psychology Review 85: , 101997. https://doi.org/10.1016/j.cpr.2021.101997 |
36 | Padmanabhanunni, A. , & Gqomfa, N. ((2022) ). “The Ugliness of It Seeps into Me”: Experiences of Vicarious Trauma among Female Psychologists Treating Survivors of Sexual Assault. International Journal of Environmental Research and Public Health, 19: (7), 3925. https://doi.org/10.3390/ijerph19073925 |
37 | Porges, S. W. (2011). The polyvagal theory: Neurophysiological foundations of emotions, attachment, communication, and self-regulation (Norton Series on Interpersonal Neurobiology). WW Norton & Company. |
38 | Raio, C. M. , Orederu, T. A. , Palazzolo, L. , Shurick, A. A. , & Phelps, E. A. ((2013) ). Cognitive emotion regulation fails the stress test. Proceedings of the National Academy of Sciences 110: (37), 15139–15144. https://doi.org/10.1073/pnas.1305706110 |
39 | Ravi, A. , Gorelick, J. , & Pal, H. ((2021) ). Identifying and addressing vicarious trauma. American Family Physician, 103: (9), 570–572. |
40 | Roberson, M. M. , & Lund, E. ((2022) ). School-Based Speech-Language Pathologists’ Attitudes and Knowledge about Trauma-Informed Care. Language, Speech, and Hearing Services in Schools, 53: (4), 1117–1128. https://doi.org/10.1044/2022_LSHSS-21-00172 |
41 | Rupert, A. C. , & Bartlett, D. E. ((2022) ) The childhood trauma and attachment gap in speech-language pathology: Practitioner& knowledge, practice, and needs. American Journal of Speech-Language Pathology, 31: (1), 287–302. https://doi.org/10.1044/2021_AJSLP-21-00110 |
42 | Sylvestre, A. , Bussières, È. L. , & Bouchard, C. ((2016) ). Language Problems among Abused and Neglected Children: A Meta-Analytic Review. Child Maltreatment 21: (1), 47–58. https://doi.org/10.1177/1077559515616703 |
43 | Smith, M. , Williamson, A. E. , Walsh, D. , & McCartney, G. ((2016) ). Is there a link between childhood adversity, attachment style and Scotland’s excess mortality? Evidence, challenges and potential research. BMC Public Health 16: (1), 655. https://doi.org/10.1186/s12889-016-3201-z |
44 | Speech Pathology Australia (2018). Speech Pathology in Mental Health Services. Retrieved from: Position Statements (speechpathologyaustralia.org.au) |
45 | Substance Abuse and Mental Health Services Administration (SAMHSA) (2014). SAMHSA’s concept of trauma and guidance for trauma-informed approach. HHS Publication No. (SMA) 14-4884. Rockville, MD. Substance Abuse and Mental Health Services Administration. |
46 | Tronick, E. , Als, H. , Adamson, L. , Wise, S. , & Brazelton, T. B. ((1978) ). The infant’s response to entrapment between contradictory messages in face-to-face interaction. Journal of the American Academy of Child Psychiatry 17: (1), 1–13. https://doi.org/10.1016/s0002-7138(09)62273-1 |
47 | Van der Kolk, B. A. ((2014) ). The body keeps the score: Brain, mind, and body in the healing of trauma. New York, NY: Penguin. |
48 | Whitehouse, A. J. O. , Watt, H. J. , Line, E. A. , & Bishop, D. V. M. ((2009) ). Adult psychosocial outcomes of children with specific language impairment, pragmatic language impairment and autism. International Journal of Language & Communication Disorders, 44: (4), 511–528. https://doi.org/10.1080/13682820802708098 |
49 | Yehuda, N. , ((2016) ). Communicating Trauma: Clinical Presentations and Interventions with Traumatized Children. New York: Routledge Press |




