Circumstances and outcomes of falls in hospital for adults with communication disability secondary to stroke: A qualitative synthesis
Abstract
BACKGROUND:
Falls are a significant patient safety concern in hospital. Adult patients with stroke, and those with communication disability, are at an increased risk of falls during their hospital admission compared to patients without stroke or communication disability.
OBJECTIVE:
The aim of this review is to determine the circumstances and outcomes of falls in hospitalised patients with communication disability following stroke.
METHOD:
A qualitative synthesis of 16 papers according to the Generic Reference Model of patient safety. This is a secondary analysis of studies in a systematic review of the association between communication disability after stroke and falls in hospitalised patients.
RESULTS:
In studies including participants with communication disability, falls commonly occurred at the patient bedside, during the day, and in transfers. However, no studies provided individual or group data specifically detailing the circumstances and outcomes of falls of the included participants with communication disability.
CONCLUSION:
Research to date provides scant evidence on the circumstances and outcomes of falls in hospital patients with communication disability after stroke. This review performs a useful function in highlighting a glaring gap in the literature and the urgent need to enrich hospital falls prevention research that includes patients with communication disability following stroke. Findings of this review are discussed in relation to providing a framework for analysis of for future research.
1Introduction
Falls are a significant patient safety concern in hospitals; impacting on the patient and the health service, and accounting for 38% of documented patient safety incidents with up to 65% of patients with stroke falling at least once during their hospital admission (Batchelor et al., 2012; Hill et al., 2007; Walsh et al., 2016). Falls potentially result in a number of adverse consequences to both the patient and health service including; serious injury, loss of functional capacity and reduced confidence and motivation to mobilise; increased length of stay; increased length of stay and can be fatal (Batchelor et al., 2012; Hill et al., 2007).
Communication disability is highly prevalent in people with stroke (O’Halloran et al., 2009), affecting an estimated 64% of this group (Mitchell et al., 2020) and including aphasia, dysarthria, apraxia of speech and cognitive communication impairments. People with communication disability have a three-fold increased risk for adverse events in hospital, including falls, compared to patients without communication disability (Bartlett et al., 2008). However, they are often excluded from falls research (Hemsley et al., 2019) and there is little information about the context of their falls or what would help prevent falls for this population. While a recent systematic review including a meta-analysis (n = 11) found no association between falls and communication disability, studies were limited by not including participants with severe communication disability, or failure to report on the severity of participants’ communication difficulties (Sullivan et al., 2020). In the only study focusing on patients with severe communication disability and their falls following stroke, these patients had twice the risk of falling while in hospital as those who could communicate basic needs (Sullivan & Harding, 2019). Further, Sze et al. (2001) suggested that patients with communication disability who have difficulties expressing their needs may engage in risk taking behaviours such as attempting to mobilise alone. In addition to difficulties communicating their needs, patients with communication disability following stroke may have difficulties understanding and following instructions, such as those required to safely transfer (e.g., sitting to standing). Indeed, Zdobysz et al. (2005) suggest a patient may fall during transferring if “the patient does not understand or remember verbal instructions” (p. 70). Further, Mion et al. (1989) and Nyberg and Gustafson (1995) reported a higher incidence of falls in patients who had difficulties following instructions. With little information available explaining the needs of this population in relation to falls in hospital, it is important to identify from prior research any contributing factors, hazards, and outcome of falls for this vulnerable and under-researched group (Hemsley et al., 2019; Sullivan et al., 2020; Sullivan & Harding, 2019).
Patient safety frameworks provide structure in collecting information about patient safety incidents and consider the interaction between contributing factors or hazards, characteristics of the patient, mitigating factors and outcomes. This can help to identify ways to prevent safety incidents and reduce their negative impacts on patients and health services. The Generic Reference Model (Runciman et al., 2006) is a patient safety framework that can be used to guide the process of collecting and classifying information about patient safety incidents. The model is underpinned by a risk management structure and outlines relationships between contributing factors, the patient safety incident and the outcomes and consequences for the patient and the organisation (see Fig. 1). As this model contains and organises the important elements of a patient safety incident to facilitate the analysis of the incident it was chosen to guide the data analysis and to provide a theoretically sound means of synthesising findings across studies (Walshe & Boaden, 2006).
Fig. 1
The Generic Reference Model (Runciman et al., 2006). Reproduced from Quality and Safety in Health Care, Runciman.W.B., Williamson, J.A.H., Deakin, A., Benveniste, K.A., Bannon, K., & Hibbert, P.D. volume 15(suppl), i82-i90, copyright 2006 with permission from BMJ Publishing Group Ltd.
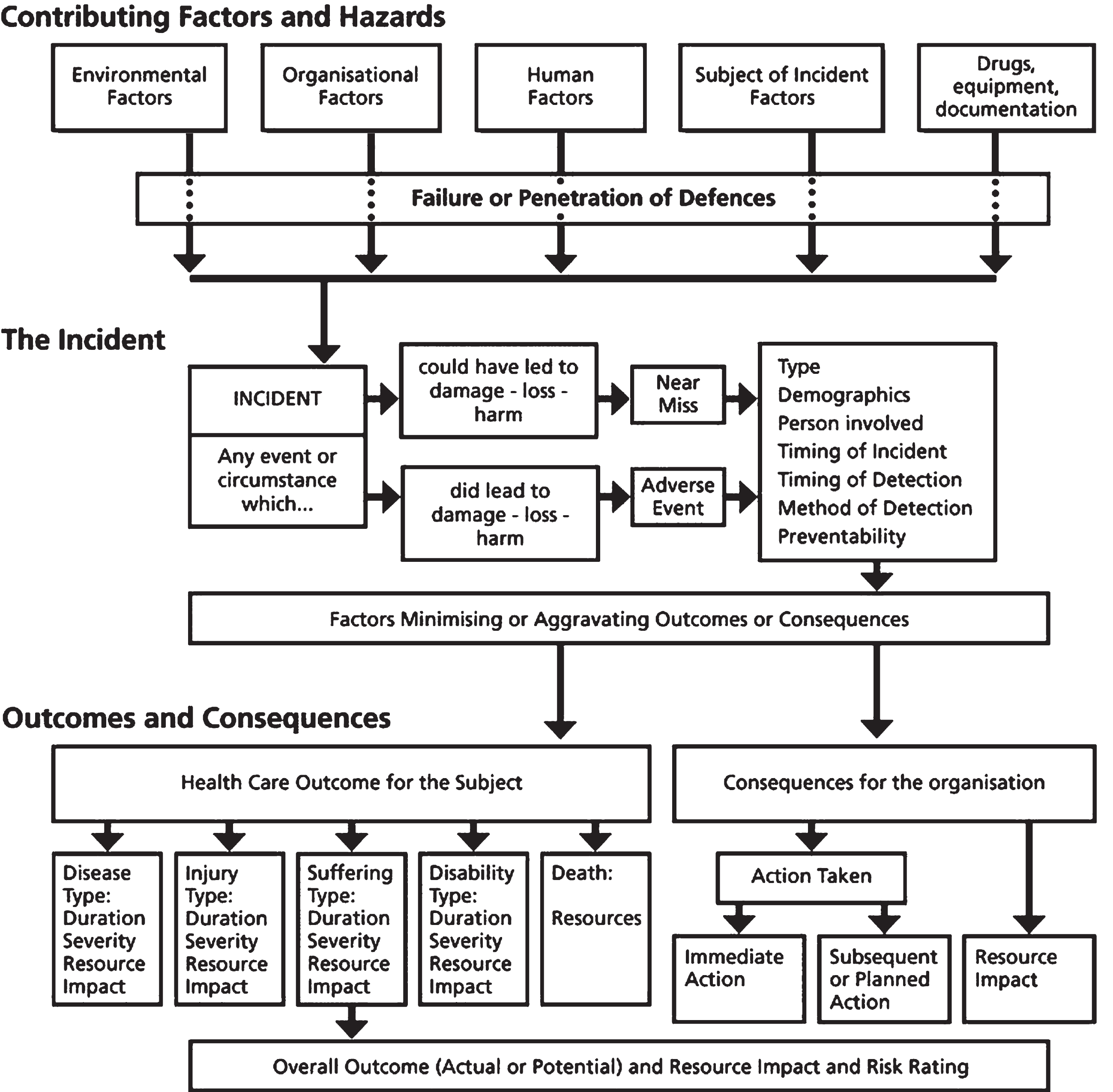
In the Generic Reference Model (Runciman et al., 2006), contributing factors and hazards for the incident are grouped into five categories: environmental factors; organisational factors; human factors; subject of incident factors; and drugs, equipment, and documentation. Table 1 provides examples of each of these factor types relating to falls in hospital. In patient safety research utilising this model, the incident is investigated in terms of the demographics of the person involved, timing of the incident, when and how the incident was detected, and preventability of the incident. Outcomes and consequences of the incident are explored for both the patient and the organisation (e.g., the hospital) in relation to the patient’s injury, suffering, and disability; and any impact on organisational resources.
Table 1
Examples of Contributing Factors and Hazards in Falls in Hospitals
| Environmental factors | Organisational Factors | Human Factors | Subject of Incident Factors | Drugs, equipment, documentation |
| Lighting; floor surface; cords/tubing; distance to bathroom; unstable furniture; position of items in reach | Staffing levels; falls prevention policy; falls prevention education | Communication breakdown; inappropriate assistance by staff/family | Intrinsic risk factors such as balance impairments, dependence for activities of daily living, neglect; footwear | Medications, equipment failure or malfunction, documentation error regarding assistance for transfers |
Factors within or intrinsic to patients with stroke (e.g., their impairments, activities or personal factors) are multifactorial and include balance impairments, increased dependence for activities of daily living tasks, and hemi-neglect (Batchelor et al., 2012; Campbell & Matthews, 2010; Walsh et al., 2016). When considering the Generic Reference Model (Runciman et al., 2006), little is known about other contributing factors for the falls of patients with communication disability after stroke including aspects of the environment and the patient’s activities on the ward. Understanding more about the circumstances and outcomes of falls in hospital patients with stroke and communication disability could provide useful information to identify appropriate prevention strategies and thus reduce the risk or incidence of falls in this vulnerable patient group.
Therefore, the aim of this review was to provide a secondary analysis of the literature located in a prior systematic review and meta-analysis, on the circumstances and outcomes of falls in hospital patients with communication disability secondary to stroke, including factors leading up to, occurring during, or following a fall. The prior systematic review (Sullivan et al., 2020) sought to identify any association between communication disability following stroke and falls and involved the same population and search terms suitable for the present review. Given the high rates of exclusion of people with communication disability in the falls literature (Hemsley et al., 2019), the studies within the prior systematic review provided an opportunity to understand more about the nature of falls in cohorts of hospital patients known to include people with communication disability following stroke. Reviewing these studies with a focus on the contextual factors surrounding falls could help to identify ways to reduce the risk of falls, and to inform the design and analytic framework of future falls risk and prevention research and patient safety programs that are inclusive of this population.
2Methods
2.1Study selection for this review
2.1.1The primary systematic review
The prior systematic review, from which the studies in this paper are drawn, was registered a priori on PROSPERO (CRD 42019137199) and followed the PRISMA guideline (Page et al., 2020). The search methods of the prior systematic review, conducted across five scientific databases in July 2019, are available from the first author and published in (Sullivan et al., 2020). In summary, the studies included in that review met the inclusion criteria of all being full papers on original research including adult participants admitted to acute or subacute hospital services following a stroke; and all including comparative falls data for people with and without communication disability (required for the meta-analysis). Studies must have included at least one participant with communication disability in the sample.
2.1.2The present review
This review expanded on the inclusion criteria of the primary review (Sullivan et al., 2020) to (a) enable the inclusion of any previously excluded studies which lacked the comparative data but met all other inclusion criteria; and (b) also require all studies to also have reported data on the circumstances or outcomes of the falls.
2.2Quality appraisal
The risk of bias of the included studies was previously assessed by two authors (Sullivan et al., 2020) using the Quality Assessment Tool for Studies with Diverse Designs (QATSDD), a 16-item tool validated and applicable to research with heterogeneous study designs (Sirriyeh et al., 2011). The QATSDD examines 14 items for quantitative and qualitative studies and 16 items for mixed methods studies; with a maximum score of 42 for quantitative and qualitative studies and 46 for mixed methods studies. Scores are converted to a percentage to allow comparison across studies. The items examine theoretical framework; research aims; setting; sample size and representativeness; data collection process and rationale; appropriateness of data analysis, reliability and validity; user involvement; and strengths and limitations. Studies are scored according to these aspects using a 4-point scale, 0 (not at all/not stated) to 3 (complete/explicitly stated) (Sirriyeh et al., 2011).
2.3Data extraction and synthesis
A data extraction table was created using Microsoft Excel to record bibliographic and methodological information, data and relevant results of each study. These data included (a) the study setting; (b) design; (c) participant demographics, including the percentage of the sample with communication disability; (d) the type and severity of communication disability and how this was assessed; (d) circumstances surrounding the fall (e.g., location of the fall, activity during the fall and time of day of the fall); and (e) outcomes from falls (e.g., injury rates).
After the first author had extracted data from the included studies, the data were analysed using qualitative synthesis according to the Generic Reference Model (Runciman et al., 2006). This involved the first author coding the data according to factors within the Generic Reference Model (Runciman et al., 2006). Analysis was finalised in discussion with co-authors in order to reach consensus on the categories and themes identified within the data.
3Results
The PRISMA flow diagram, depicting the screening and selection of studies, is presented in Fig. 2.
Fig. 2
Study Selection Flowchart.
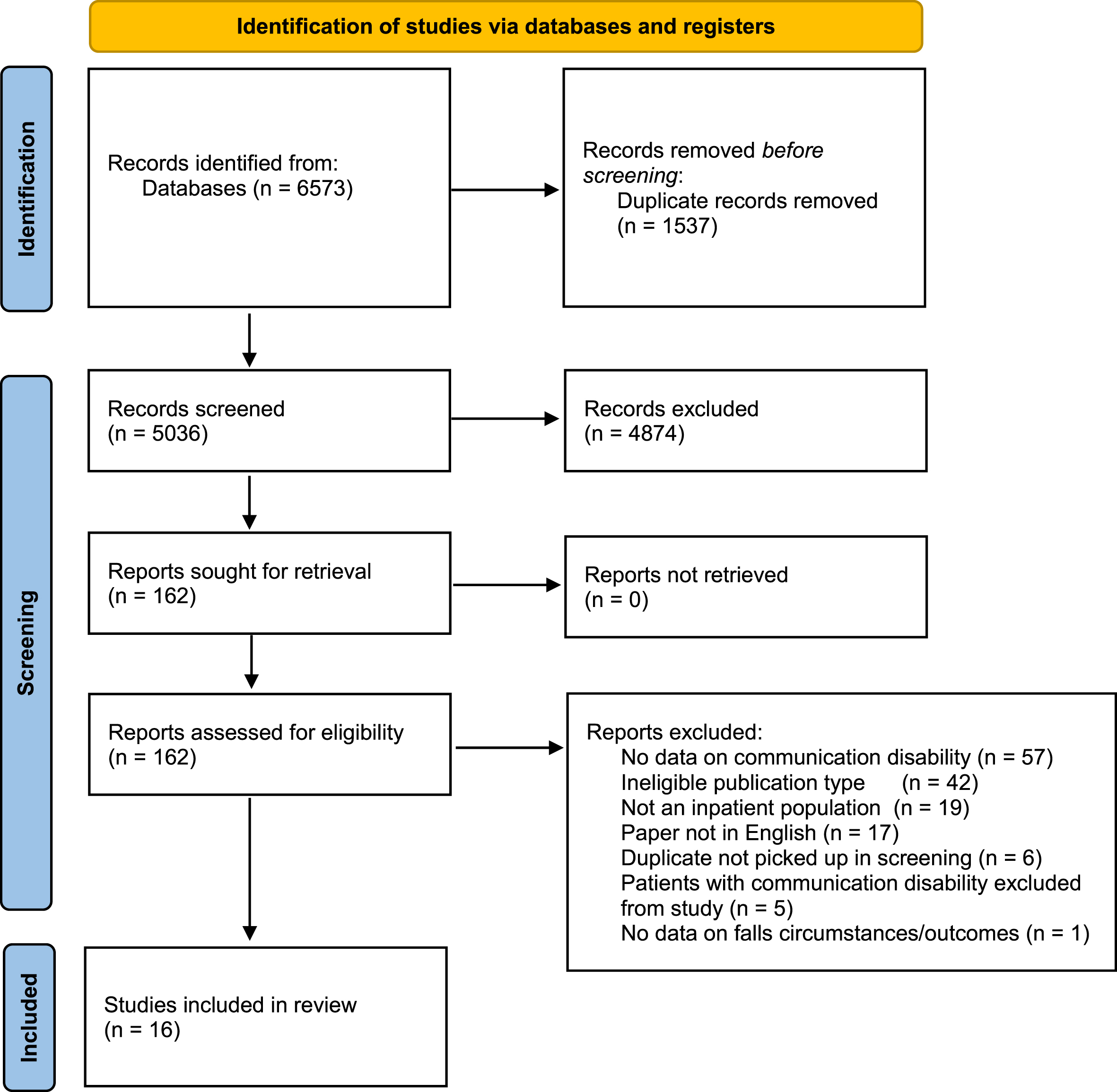
Of the 16 studies included in the prior systematic review (Sullivan et al., 2020), 15 met the expanded inclusion criteria for this review (see Table 2). Despite being selected due to known inclusion of patients with communication disability, none of the included studies specifically provided results on the circumstances and outcomes of falls for this population. The Generic Reference Model (Runciman et al., 2006) guides the reporting of the results with a focus on patient safety and the results are discussed specifically in relation to patients with stroke and communication disability.
Table 2
Matrix of results according to Generic Reference Model
| Contributing Factors and Hazards | Circumstances of falls | Outcomes and Consequences | |||||||||||||
| Study | Environmental Factors | Organisational Factors | Human Factors | Subject of incident factors | Drugs, equipment, documentation | Type | Location | Timing of Incident | Activity Occurring | Patient injury | Patient suffering | Patient disability | Patient Death | Impact on organisational resources | Action Taken |
| Baetens et al. (2011) | X | X | X | X | |||||||||||
| Bugdayci et al. (2011) | X | X | X | X | X | X | X | ||||||||
| Byers et al. (1990) | X | X | X | X | |||||||||||
| Chaiwanichsiri et al. (2006) | X | X | X | X | X | X | |||||||||
| Czernuszenko (2007) | X | X | X | X | X | X | X | ||||||||
| Czernuszenko and Czlonkowska (2009) | X | X | X | X | X | X | X | X | |||||||
| Nyberg and Gustafson (1996) | X | X | X | ||||||||||||
| Sinanovic et al. (2012) | X | X | X | ||||||||||||
| Sullivan and Harding (2019) | X | X | X | ||||||||||||
| Sze et al. (2001) | X | X | X | X | X | X | |||||||||
| Teasell et al. (2002) | X | X | |||||||||||||
| Tsur and Segal (2010) | X | X | X | X | X | X | X | ||||||||
| Ullah et al. (2019) | X | X | X | X | X | X | |||||||||
| Zdobysz et al. (2005) | X | X | X | X | |||||||||||
3.1Risk of bias
The average risk of bias score across the included studies was 48.7%; with a range from 11.9% (Sinanovic et al., 2012) to 64.3% (Sullivan & Harding, 2019). The quality ratings of included studies are further detailed in Table 3.
Table 3
Risk of Bias using QATSDD
| Study | Explicit theoretical framework | Statement of aims/objectives in main body of report | Clear description of research setting | Evidence of sample size considered in analysis | Representative sample of target group of a reasonable size | Description of procedure for data collection | Rational for choice of data collection tool | Detailed recruitment data | Statistical assessment of reliability and validity of measurement tools | Fit between stated research question and method of data collection | Fit between research question and method of analysis | Good justification for analytical methods selected | Evidence of user involvement in design | Strengths and limitations critically discussed | Total (%) |
| Baetens et al. (2011) | 3 | 3 | 2 | 0 | 2 | 3 | 1 | 2 | 0 | 3 | 3 | 1 | 0 | 3 | 26 (61.9) |
| Bugdayci et al. (2011) | 2 | 2 | 3 | 0 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 0 | 0 | 1 | 20 (47.6) |
| Byers et al. (1990) | 2 | 3 | 2 | 0 | 2 | 3 | 1 | 2 | 3 | 3 | 3 | 2 | 2 | 3 | 31 (73.8) |
| Chaiwanichsiri et al. (2006) | 1 | 2 | 2 | 0 | 2 | 2 | 0 | 2 | 0 | 2 | 1 | 0 | 0 | 0 | 14 (33.3) |
| Czernuszenko (2007) | 3 | 3 | 3 | 0 | 3 | 3 | 0 | 2 | 0 | 2 | 1 | 0 | 0 | 3 | 23 (54.8) |
| Czernuszenko and Czlonkowska (2009) | 3 | 3 | 3 | 0 | 3 | 3 | 0 | 3 | 0 | 2 | 3 | 1 | 0 | 2 | 26 (61.9) |
| Nyberg and Gustafson (1996) | 2 | 3 | 3 | 0 | 2 | 2 | 0 | 3 | 0 | 3 | 2 | 0 | 0 | 2 | 22 (52.4) |
| Schmid et al. (2010) | 2 | 3 | 2 | 0 | 1 | 2 | 2 | 1 | 0 | 2 | 2 | 0 | 0 | 3 | 20 (47.1) |
| Sinanovic et al. (2012) | 0 | 2 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5 (11.9) |
| Sullivan and Harding (2019) | 3 | 3 | 2 | 3 | 2 | 1 | 1 | 1 | 0 | 2 | 3 | 3 | 0 | 3 | 27 (64.3) |
| Sze et al. (2001) | 3 | 3 | 3 | 0 | 2 | 2 | 2 | 3 | 1 | 2 | 2 | 0 | 0 | 1 | 24 (57.1) |
| Teasell et al. (2002) | 3 | 3 | 2 | 0 | 2 | 1 | 2 | 2 | 1 | 2 | 2 | 0 | 0 | 2 | 22 (52.4) |
| Tsur and Segal (2010) | 2 | 3 | 2 | 0 | 1 | 1 | 0 | 1 | 0 | 2 | 1 | 0 | 0 | 0 | 13 (31.0) |
| Ullah et al. (2019) | 2 | 3 | 2 | 0 | 2 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 12 (28.6) |
| Zdobysz et al. (2005) | 3 | 3 | 1 | 0 | 2 | 2 | 3 | 2 | 1 | 3 | 2 | 0 | 0 | 0 | 22 (52.4) |
3.2Characteristics of participants
In total, there were 6935 participants included across the 15 studies. Twelve studies were based in a rehabilitation setting (Baetens et al., 2011; Bugdayci et al., 2011; Chaiwanichsiri et al., 2006; Czernuszenko, 2007; Czernuszenko & Czlonkowska, 2009; Nyberg & Gustafson, 1996; Sullivan & Harding, 2019; Sze et al. 2001; Teasell et al., 2002; Tsur & Segal, 2010; Ullah et al., 2019; Zdobysz et al. 2005), and the proportion of patients who fell ranged from 3.3% (Sinanovic et al., 2012) to 64.5% (Byers et al., 1990). All of the studies reviewed included at least one participant with communication disability, and the proportion of participants with communication disability ranged from 9.8 (Bugdayci et al., 2011) to 68.0% (Sullivan & Harding, 2019). Further participant characteristics are outlined in Table 4.
Table 4
Participant Characteristics
| Study &Setting | Sample size | Age Mean (SD) | Gender % male | % of participants with Communication Disability |
| Baetens et al. (2011) Rehabilitation | 73 | 64.6 (15.0) | 60 | 16.9 |
| Bugdayci et al. (2011) Rehabilitation | 99 | 61.99 (11.79) | 42.4 | 9.8 |
| Byers et al. (1990) Unspecified hospital | 313 | Fallers = 66.0 (14.8) Non fallers = 69.3 (13.8) | 56.5 | Fallers: Difficulty speaking = 18.8 Dysarthria = 11.9 Non Fallers: Difficulty speaking = 30.6 Dysarthria = 18.9 |
| Chaiwanichsiri et al. (2006) Rehabilitation | 151 | Fallers = 63.8 (10.8) Non Fallers = 62.1 (11.5) | 56.9 | Fallers: Aphasia = 20.8 Non Fallers: Aphasia = 26 |
| Czernuszenko (2007) Rehabilitation | 353 | 62 (14) | 56.4 | 38.8 |
| Czernuszenko and Czlonkowska (2009) Rehabilitation | 1155 | 61.5 (14.3) | 56.5 | 38 |
| Nyberg and Gustafson (1996) Rehabilitation | 142 | 74.8 (8.9) | 51.1 | 25.7 |
| Schmid et al. (2010) Acute | 1269 | 71.21 (13.3) | 56 | 35 |
| Sinanovic et al. (2012) Acute | 1809 | Not reported | 55.7 | Fallers: Aphasia = 77.05 |
| Sullivan and Harding (2019) Rehabilitation | 149 | 75.8 | 57 | 68 |
| Sze et al. (2001) Rehabilitation | 727 | Reported as under 65 and over 65 yrs. | 53.3 | Fallers = 32.2 Non-Fallers = 19.0 |
| Teasell et al. (2002) Rehabilitation | 238 | 72.7 (10.1) | 49.8 | Fallers = 34.5 Non-Fallers = 37.8 |
| Tsur and Segal (2010) Rehabilitation | 41 | 67 (8.9) | Not reported | Fallers = 29 |
| Ullah et al. (2019) Rehabilitation | 146 | 59.9 (13.16) | 65.8 | 55.4 |
| Zdobysz et al. (2005) Rehabilitation | 1014 | Range 20–89 | 47.5 | Not reported |
3.3Contributing factors and hazards
The contributing factors and hazards for falls were reported to varying degrees and with great diversity in the results. Although all studies reported on the person’s intrinsic risk factors for falls, there was little commonality in the factors that contribute to falls. A wide variety of medications for participants were noted in 10 of the studies (Bugdayci et al., 2011; Byers et al., 1990; Chaiwanichsiri et al., 2006; Czernuszenko, 2007; Czernuszenko & Czlonkowska, 2009; Nyberg & Gustafson, 1996; Schmid et al., 2010; Sullivan & Harding, 2019; Tsur & Segal, 2010; Ullah et al., 2019), but no evidence that this was a factor contributing to the falls in these studies. Investigation of environmental and third-party human factors beyond the patient were scant; reported in only two studies being inadequate or insufficient assistance by staff or visitors, wet flooring, and instability of a wheelchair (Czernuszenko & Czlonkowska, 2009; Tsur & Segal, 2010).
3.4Circumstances of the incident
The circumstances of the falls in participants were reported in reference to the (a) location of the fall (Bugdayci et al., 2011; Chaiwanichsiri et al., 2006; Czernuszenko, 2007; Czernuszenko & Czlonkowska, 2009; Sze et al., 2001; Tsur & Segal, 2010; Ullah et al., 2019; Zdobysz et al., 2005), (b) time of day (Baetens et al., 2011; Bugdayci et al., 2011; Byers et al., 1990; Chaiwanichsiri et al., 2006; Czernuszenko, 2007; Czernuszenko & Czlonkowska, 2009; Sinanovic et al., 2012; Sze et al., 2001; Tsur & Segal, 2010; Ullah et al., 2019), and (c) activity being performed prior to the fall (Baetens et al., 2011; Bugdayci et al., 2011; Chaiwanichsiri et al., 2006; Czernuszenko, 2007; Czernuszenko & Czlonkowska, 2009; Sze et al., 2001). Across the studies, falls commonly occurred in the patient’s bedroom or bedside, during the day and during transfers (e.g., from bed to chair). Witnessed, unwitnessed or assisted falls were reported in only two studies (Ullah et al., 2019; Zdobysz et al., 2005), providing little detail on other factors that may contribute to these falls. Family members or visitors provided protection against falls for people with stroke in hospital population in five studies (Baetens et al., 2011; Bugdayci et al., 2011; Byers et al., 1990; Chaiwanichsiri et al., 2006; Ullah et al., 2019). However, two others reported that inappropriate assistance provided by family and visitors contributed to a fall (Czernuszenko & Czlonkowska, 2009; Tsur & Segal, 2010).
3.5Outcomes and consequences
The severity of and type of physical injury was reported in 13 studies (Baetens et al., 2011; Bugdayci et al., 2011; Byers et al., 1990; Chaiwanichsiri et al., 2006; Czernuszenko, 2007; Czernuszenko & Czlonkowska, 2009; Nyberg & Gustafson, 1996; Sinanovic et al., 2012; Sullivan & Harding, 2019; Sze et al., 2001; Teasell et al., 2002; Tsur & Segal, 2010; Ullah et al., 2019), with the majority of participants sustaining either no injury or a mild injury from falling, whereas the range of participants reporting a severe injury (such as fractures) was 0.6 (Teasell et al., 2002) to 5.6% (Baetens et al., 2011). Three studies (Czernuszenko, 2007; Czernuszenko & Czlonkowska, 2009; Ullah et al., 2019) reported a statistically significant difference in the length of stay of patients with stroke who fell in comparison to patients who did not fall. In contrast, Schmid et al. (2010) found no difference in length of stay for patients with stroke who did or did not fall.
4Discussion
This review synthesised evidence on the reported circumstances and outcomes of falls in patients with stroke in hospital, in studies where at least one participant with communication disability was included. The Generic Reference Model (Runciman et al., 2006) provided the theoretical framework for the analysis. Falls are one of the most common complications to occur after stroke (Verheyden et al., 2013) and despite the relatively low occurrence of severe injury associated with falls, the continued occurrence of falls is a persistent and challenging problem. The majority of falls in people with stroke described in studies included in this review occurred at the patient’s bedroom or bedside, and were unwitnessed, is of concern; considering that patients spend the majority of their time during hospitalisation in their bedroom and alone (West & Bernhardt, 2012). That the most common activity being performed prior to a fall was transferring (e.g., from bed to wheelchair) is also important, considering that transfers are an activity that patients often undertake on any hospital ward and are an important goal of rehabilitation (Baetens et al., 2011).
Although this body of literature was selected due to known inclusion of patients with communication disability, none reported on factors, circumstances, or outcomes of falls specifically in relation to this population. This is an unfortunate limitation in the literature that the studies included in this review did not yield further insights or help explain the increased risk of falls in patients with stroke and communication disability in hospital. In a recent systematic review of 61 studies on falls of adult hospital patients with communication disability, Hemsley et al. (2019) found that despite two thirds of the studies identifying communication disability as a contributing factor for falls, patients with communication disability were actively excluded from participation by the recruitment methods or data collection and results across all studies rarely mentioned any participants with communication disability who had been included.
The majority of studies in this review aimed to identify the intrinsic risk factors associated with falls in people with stroke, an essential element required to mitigate these patient safety incidents. Beyond this, the studies reviewed provide little insight into other factors such as environmental and organisational factors (e.g., staffing ratios) surrounding falls in patients with stroke that could inform strategies designed to reduce the risk of falls in stroke patients with communication disability. The identification of intrinsic risk factors such as balance impairments informs the development of falls prevention interventions, however, identification of these factors alone is unlikely to prevent a fall (Taylor & Hignett, 2016).
Patients with communication disability following stroke may have unique intrinsic factors that contribute to their falls due to difficulties communicating with health professionals involved in their care (Simmons-Mackie & Kagan, 2007; Sullivan et al., 2020, Sze et al. 2001). These difficulties could impact a patient’s ability to understand and follow the instructions required to transfer, use equipment and ambulate safely, resulting in a fall (Mion et al., 1989; Nyberg & Gustafson, 1995; Zdobysz et al., 2005). Thus, staff providing instruction or assisting with tasks such as transferring might need to make adaptations to their communication to meet the patient’s communication needs (e.g., for understanding information and following instructions) in order to minimise the risk of a fall.
Further, environmental factors (e.g., floor surface, and placing items such as the call bell in reach of the patient) are modifiable and may have a significant impact on the safety of patients during their hospitalisation (Taylor & Hignett, 2016). Problems for people with communication disability gaining attention in hospital (Balandin et al., 2001; Hemsley et al., 2013) may lead patients to have difficulty in alerting staff to their basic needs and potentially increase patient risk taking behaviour to access food, toileting, and personal care (Sullivan & Harding, 2019, Sze et al. 2001). None of the studies reviewed provided a comprehensive evaluation of all these factors in the circumstances leading up falls, in prioritising attention to the intrinsic factors.
The finding that the presence of family members or visitors may be a protective factor for falls in this population (Baetens et al., 2011; Bugdayci et al., 2011; Byers et al., 1990; Chaiwanichsiri et al., 2006; Ullah et al., 2019) might help to explain the finding that falls occur while patients are alone as it is possible that family members and visitors are acting to prevent falls (e.g., by providing assistance to reach items or instructing to wait for nursing assistance or use the call bell) (Hemsley et al., 2013). However, two studies also suggested that family members and visitors may provide inappropriate assistance or supervision and contribute to a fall (Czernuszenko & Czlonkowska, 2009; Tsur & Segal, 2010), suggesting that family members and visitors should receive instruction regarding appropriate assistance and supervision needed for patients with stroke, including specific communication strategies to support patients with communication disability in hospital; and that family members and visitors should be included in falls risk policies in hospitals so that their role in preventing falls is made clear. Although studies did not specify recommendations relating to patients with communication disability, it is likely that the involvement of family and visitors in hospital could be supportive of their interactions with hospital staff (Hemsley et al., 2013).
Communication between patients and healthcare providers is essential to the provision of good healthcare (Sherman et al., 2009) and poor communication with patients with communication disability is associated with increased rates of adverse events, including falls (Bartlett et al., 2008; Hemsley et al., 2013; Hemsley & Balandin, 2014). Whilst augmentative and alternative communication, such as the use of picture boards, may help patients with communication disability communicate more effectively in hospital, these strategies are not universally applicable to every patient with communication disability (Lasker & Garrett, 2008). Communication partners such as nurses and allied health professionals, continue to play an essential role in supporting effective communication for patients with communication disability in hospital. Adapting communication to use short sentences, single step instructions, and specific language (e.g., using words such as ‘put your foot next to mine’ rather than ‘put it here’) could help to support comprehension of the safety requirements of the task, and eliminate the risk of other human factors in a fall as described in Czernuszenko & Czlonkowska, (2009) and Tsur & Segal (2010). Additionally, given the large proportion of people with stroke who have difficulties with language (O’Halloran et al., 2009) or cognitive function (Renjen et al., 2015) any preventative strategies undertaken should take into consideration the special requirements of this population.
4.1Limitations and directions for future research
This review is a secondary analysis of studies included in recent systematic review and meta-analysis investigating the association between communication disability following stroke and falls in hospital (Sullivan et al., 2020). While there is potential that some relevant studies may have been missed due to this method, the risk of this is low considering the extent of the initial search and the close similarities of that search to the aims of this review. Although the original review focussed on papers reporting quantitative data, this criterion was applied following the search, thus reapplying the criteria for this review to papers excluded due to a lack of comparative data protects against the possibility of papers using a qualitative method being excluded.
A significant limitation of the literature is the lack of specific detail regarding the circumstances and outcomes for falls in patients with stroke and communication disability. The studies included in this review offered relevant but inconsistent forms of data reporting of the circumstances and outcomes of falls in people with stroke, as shown by the use of the Generic Reference Model as an analysis tool (Runciman et al., 2006). With limited information regarding causes for falls and rates of witnessed or unwitnessed falls, a more detailed investigation of the patient experience of falls may provide further insights into how the patient themselves might learn or implement protective and preventative strategies (Wei et al., 2019). Should this be combined with more detailed information on extrinsic factors, as well as the already recognised intrinsic factors, a greater understanding of the safety framework for falls in patients with stroke could inform new protocols for keeping patients with stroke and communication disability safe in hospital.
Further research is required to understand (a) the interaction of the patient’s intrinsic factors with the other contributing factors (e.g., environmental factors) in the circumstances surrounding falls, and (b) the role of extrinsic risk factors and ways that any environmental factors may be modified, particularly for patients with communication disability. Looking beyond intrinsic factors to the communication skills of staff in relation to falls prevention, would also be important, as effective communication between healthcare providers and patients is an essential component of patient safety and increases the likelihood that patients will understand and follow recommendations (Blackstone et al., 2011).
Future research should move beyond quantification and statistical analysis of risk factors to engage more thoroughly with the complexity of the hospital environment. The reliance on quantitative methodologies for falls research potentially oversimplifies the sophisticated interactions involved in a complex and dynamic hospital environment with factors related to communication disability (Hoff & Sutcliffe, 2006); bypassing several contributing factors and hazards and outcomes that this environment might bring to falls. The present review will be used to inform the analytic framework for mixed methods research which captures the insights and understandings from people who experience a fall and those surrounding them.
5Conclusion
This synthesis review of 15 studies, located and selected using systematic search procedures, provides scant insights on the hospital falls of adults with communication disability following stroke, highlighting a glaring gap in the falls prevention literature. The findings suggest that falls commonly occur in the patient’s bedroom or bedside, during transfers, during the day, and when the patient is alone. Although severe injury is uncommon, one outcome of these falls is a significantly increased length of stay in hospital. However, limitations in the reporting of the incident characteristics or the circumstances of the fall, other contributing factors in the environment, and lack of specific data relating to patients with communications disabilities after stroke indicates a need for further research on the falls in this population. Such research should not only increase focus on the patient’s communication skills and impairments, but also take more than the patient’s intrinsic factors into account to include examination of environmental factors and outcomes to falls for this vulnerable patient group.
Acknowledgments
The authors would like to thank and acknowledge the work of Dr Joanne Steel who was engaged as a research assistant in the study.
This research has been funded by an Australian Government Research Training Program Scholarship and a Jumbunna Postgraduate Research Scholarship.
Conflict of interest
The authors have no conflict of interest to report.
References
1 | Baetens, T. , de Kegel, A. , Calders, P. , Vanderstraeten, G. , & Cambier, D. ((2011) ) Prediction of falling among stroke patients inrehabilitation. Journal of Rehabilitation Medicine, 43: (10), 876–883. https://doi.org/10.2340/16501977-0873 |
2 | Balandin, S. , Hemsley, B. , Sigafoos, J. , Green, V. , Forbes, R. , Taylor, C. , & Parmenter, T. ((2001) ) Communicating with Nurses: The Experiences of 10 Individuals with an Acquired Severe Communication Impairment. Brain Impairment, 2: (2), 109–118. |
3 | Bartlett, G. , Blais, R. , Tamblyn, R. , Clermont, R. J. , & MacGibbon, B. ((2008) ) Impact of patient communication problems on the risk ofpreventable adverse events in acute care settings. CMAJ, 178: (12), 1555–1562. https://doi.org/10.1503/cmaj.070690 |
4 | Batchelor, F. A. , Mackintosh, S. F. , Said, C. M. , & Hill, K. D. ((2012) ). Falls after stroke. In International Journal of Stroke (Vol. 7: , Issue 6, pp. 482–490). https://doi.org/10.1111/j.1747-4949.2012.00796.x |
5 | Blackstone, S. W. , Ruschke, K. , Wilson-Stronks, A. , & Lee, C. ((2011) ) Converging Communication Vulnerabilities in Health Care: AnEmerging Role for Speech-Language Pathologists and Audiologists. Perspectives on Communication Disorders and Sciences inCulturally and Linguistically Diverse (CLD) Populations, 18: (1), 3–11. https://pubs.asha.org/doi/full/10.1044/cds18.1.3 |
6 | Bugdayci, D. , Paker, N. , Dere, D. , Ozdemir, E. , & Ince, N. ((2011) ) Frequency, features, and factors for falls in a group of subacutestroke patients hospitalized for rehabilitation in Istanbul. Archives of Gerontology and Geriatrics, 52: (3), e215–e219. http://dx.doi.org/10.1016/j.archger.2010.11.014 |
7 | Byers, V. , Arrington, M. E. , & Finstuen, K. ((1990) ) Predictive risk factors associated with stroke patient falls in acute care settings. Journal of Neuroscience Nursing, 22: (3), 147–154. |
8 | Campbell, G. B. , & Matthews, J. T. ((2010) ) An integrative review offactors associated with falls during post-stroke rehabilitation. Journal of Nursing Scholarship, 42: (4), 395–404. https://doi.org/10.1111/j.1547-5069.2010.01369.x |
9 | Chaiwanichsiri, D. , Jiamworakul, A. , & Kitisomprayoonkul, W. ((2006) ) Falls among stroke patients in Thai Red Cross rehabilitation Centre. Journal of the Medical Association of Thailand, 89: , S47–52. |
10 | Czernuszenko, A. ((2007) ) Risk factors for falls in post-stroke patients treated in a neurorehabilitation ward. Neurologia i Neurochirurgia Polska, 41: (1), 28–35. |
11 | Czernuszenko, A. , & Czlonkowska, A. ((2009) ) Risk factors for fallsin stroke patients during inpatient rehabilitation. Clinical Rehabilitation, 23: (2), 176–188. https://doi.org/10.1177/0269215508098894 |
12 | Hemsley, B, , Steel, J. , Worrall, L. , Hill, S. , Bryant, L. , Johnston, L. , Georgiou, A. , & Balandin, S. ((2019) ) A systematic review offalls in hospital for patients with communication disability:Highlighting an invisible population. Journal of Safety Research, 68: , 89–105. https://doi.org/10.1016/j.jsr.2018.11.004 |
13 | Hemsley, , Bronwyn, , & Balandin, S. ((2014) ) A metasynthesis ofpatient-provider communication in hospital for patients with severecommunication disabilities: Informing new translational research. AAC: Augmentative and Alternative Communication, 30: (4), 329–343. https://doi.org/10.3109/07434618.2014.955614 |
14 | Hemsley, , Bronwyn, , Werninck, M. , & Worrall, L. ((2013) ) That reallyshouldn’t have happened”: People with aphasia and their spousesnarrate adverse events in hospital. Aphasiology, 27: (6), 706–722. https://doi.org/10.1080/02687038.2012.748181 |
15 | Hill, K. D. , Vu, M. , & Walsh, W. ((2007) ) Falls in the acute hospital setting - impact on resource utilisation. Australian Health Review, 31: (3). |
16 | Hoff, T. J. , & Sutcliffe, K. M. ((2006) ) Studying patient safety in health care organisations. Journal on Quality and Patient Safety, 32: (1), 5–15. |
17 | Lasker, J. P. , & Garrett, K. L. ((2008) ) Aphasia and AAC: EnhancingCommunication Across Health Care Settings. The ASHA Leader, 13: (8), 10–13. https://doi.org/10.1044/leader.FTR1.13082008.10 |
18 | Mitchell, C. , Gittins, M. , Tyson, S. , Vail, A. , Conroy, P. , Paley, L. , & Bowen, A. (2020). Prevalence of aphasia and dysarthria among inpatient stroke survivors: describing the population, therapy provision and outcomes on discharge. Aphasiology. https://doi.org/10.1080/02687038.2020.1759772 |
19 | Mion, L. , Gregor, S. , Buettner, M. , Chwirchak, D. , Lee, O. , & Paras, W. ((1989) ) Falls in the Rehabilitation Setting: Incidence andCharacteristics. Rehabilitation Nursing, 14: (1), 17–22. https://doi.org/10.1002/j.2048-7940.1989.tb00667.x |
20 | Nyberg, L. , & Gustafson, Y. ((1995) ) Patient Falls in StrokeRehabilitation - a Challenge to Rehabilitation Strategies. Stroke, 26: (5), 838–842. https://doi.org/10.1161/01.STR.26.5.838 |
21 | Nyberg, L. , & Gustafson, Y. ((1996) ) Using the Downton index topredict those prone to falls in stroke rehabilitation. Stroke, 27: (10), 1821–1824. https://doi.org/10.1161/01.STR.27.10.1821 |
22 | O’Halloran, R. , Worrall, L. E. , & Hickson, L. ((2009) ) The number ofpatients with communication related impairments in acute hospitalstroke units. International Journal of Speech- Language Pathology, 11: (6), 438–449. https://doi.org/10.3109/17549500902741363 |
23 | Page, MJ. , McKenzie, JE. , Bossuyt, PM. , Boutron, I. , Hoffmann, T.C. , Mulrow, C.D. , Shamseer, L. , Tetzlaff, J.M. , Akl, E.A. , Brennan, S.E. , Chou, R. , Glanville, J. , Grimshaw, J. , Hróbjartsson, A. , Lalu, M.M. , Li, T. , Loder, E.W. , Mayo-Wilson, E. , McDonald, S. , McGuinness, L.A. , Stewart, L.A. , Thomas, J. , Tricco, A.C. , Welch, V.A. , Whiting, P. , & Moher, D. ((2021) ) The PRISMA statement: anupdated guideline for reporting systematic reviews. BMJ, 372: (71). https://doi.org/10.1136/bmj.n71 |
24 | Renjen, P. N. , Gauba, C. , & Chaudhari, D. ((2015) ) CognitiveImpairment After Stroke. Cureus, 7: (9), e335. https://doi.org/10.7759/cureus.335 |
25 | Runciman, W. B. , Williamson, J. A. H. , Deakin, A. , Benveniste, K.A. , Bannon, K. , & Hibbert, P. D. ((2006) ) An integrated frameworkfor safety, quality and risk management: An information and incidentmanagement system based on a universal patient safetyclassification. In Quality and Safety in Health Care, (Vol. 15: , Issue (SUPPL. 1). https://doi.org/10.1136/qshc.2005.017467 |
26 | Schmid, A. A. , Wells, C. K. , Concato, J. , Dallas, M. I. , Lo, A. C. , Nadeau, S. E. , Williams, L. S. , Peixoto, A. J. , Gor-man, M. , Boice, J.L. , Struve, F. , McClain, V. , & Bravata, D. M. ((2010) ) Prevalence, predictors, and outcomes of poststroke falls in acutehospital setting. Journal of Rehabilitation Research and Development, 47: (6), 553–562. https://doi.org/10.1682/jrrd.2009.08.0133 |
27 | Sherman, H. , Castro, G. , Fletcher, M. , Hatlie, M. , Hibbert, P. , Jakob, R. , Koss, R. , Lewalle, P. , Loeb, J. , Perneger, T. , Runciman, W. , Thomson, R. , van der Schaaf, T. , & Virtanen, M. ((2009) ) Towardsan International Classification for Patient Safety: The conceptualframework. International Journal for Quality in Health Care, 21: (1), 2–8. https://doi.org/10.1093/intqhc/mzn054 |
28 | Simmons-Mackie, N. , & Kagan, A. ((2007) ) Application of the ICF inAphasia. Seminars in Speech and Language, 28: (4), 244–253. https://doi.org/10.1055/s-2007-986521 |
29 | Sinanovic, O. , Raicevic, B. , Brkic, M. , Hajdarbegovic, E. , Zukic, S. , Kojic, B. , & Imamovic, K. ((2012) ) Falls in hospitalized acute stroke patients. Medicinski Arhiv, 66: (1), 33–34. |
30 | Sirriyeh, R. , Lawton, R. , Gardener, P. , & Armitage, G. (2011). Reviewing studies with diverse designs: the development and evaluation of a new tool. Journal of Evaluation in Clinical Practice, 1-7. https://doi.org/doi:10.1111/j.1365-2753.2011.01662.x |
31 | Stroke Foundation. (2018). National Stroke Audit Rehabilitation Services Report. https://informme.org.au/stroke-data/Rehabilitation-audits |
32 | Sullivan, R. , & Harding, K. ((2019) ) Do patients with severepoststroke communication difficulties have a higher incidence offalls during inpatient rehabilitation? A retrospective cohort study. Topics in Stroke Rehabilitation, 26: (4), 4. https://doi.org/10.1080/10749357.2019.1591689 |
33 | Sullivan, R. , Harding, K. , Skinner, I. , & Hemsley, B. (2020). Falls in hospital patients with acquired communication disability secondary to stroke: A systematic review and meta-analysis. International Journal of Language & Communication Disorders, 0-15. |
34 | Sze, K. H. , Wong, E. , Leung, H. Y. , & Woo, J. ((2001) ) Falls among Chinese stroke patients during rehabilitation. Archives of Physical Medicine & Rehabilitation, 82: (9), 1219–1225. |
35 | Taylor, E. , & Hignett, S. ((2016) ) The SCOPE of Hospital Falls: ASystematic Mixed Studies Review. Health Environments Research and Design Journal, 9: (4), 86–109. https://doi.org/10.1177/1937586716645918 |
36 | Teasell, R. , McRae, M. , Foley, N. , & Bhardwaj, A. ((2002) ) The incidence and consequences of falls in stroke patients during inpatient rehabilitation: factors associated with high risk. Archives of Physical Medicine & Rehabilitation, 83: (3), 329–333. |
37 | Tsur, A. , & Segal, Z. ((2010) ) Falls in stroke patients: risk factors and risk management. Israel Medical Association Journal: Imaj, 12: (4), 216–219. |
38 | Ullah, S. , Al-Atwi, M. K. , Qureshi, A. Z. , Tantawy, S. S. , Ilyas, A. , & Wunderlich, C. A. ((2019) ) Falls in individuals with strokeduring inpatient rehabilitation at a tertiary care hospital in Saudi Arabia. Neurosciences, 24: (2), 130–136. https://doi.org/10.17712/nsj.2019.2.20180032 |
39 | Verheyden, G. , Weerdesteyn, V. , Pickering, R. M. , Kunkel, D. , Lennon, S. , Geurts, A. C. H. , & Ashburn, A. ((2013) ) Interventions for preventing falls in people after stroke. Cochrane Database of Systematic Reviews, 5: . https://doi.org/10.1002/14651858.CD008728.pub2 |
40 | Walsh, M. E. , Horgan, N. F. , Walsh, C. D. , & Galvin, R. ((2016) ) Systematic review of risk prediction models for falls after stroke. Journal of Epidemiology & Community Health, 70: (5), 513–519. https://dx.doi.org/10.1136/jech-2015-206475 |
41 | Walshe, K. , & Boaden, R. ((2006) ). Patient Safety Research into Practice. Open University Press. |
42 | Wei, W. E. , de Silva, D. A. , Chang, H. M. , Yao, J. , Matchar, D. B. , Young, S. H. Y. , See, S. J. , Lim, G. H. , Wong, T. H. , & Venketasubramanian, N. ((2019) ) Post-stroke patients with moderatefunction have the greatest risk of falls: A National Cohort Study. BMC Geriatrics, 19: (1). https://doi.org/10.1186/s12877-019-1377-7 |
43 | West, T. , & Bernhardt, J. (2012). Physical activity in hospitalised stroke patients. In Stroke Research and Treatment. https://doi.org/10.1155/2012/813765 |
44 | Zdobysz, J. A. , Boradia, P. , Ennis, J. , & Miller, J. ((2005) ) The relationship between functional independence scores on admission and patient falls after stroke. Top Stroke Rehabil, 12: (2), 65–71. |




