Transition of care of patients with eosinophilic gastrointestinal diseases: Challenges and opportunities
Abstract
Eosinophilic gastrointestinal disorders (EGID) are a group of allergen-mediated conditions which are characterized by eosinophilic inflammation affecting one or more parts of the gastrointestinal tract. A disproportionately higher number of EGID patients are diagnosed in the pediatric age group. Given the chronic course of EGIDs and lack of curative therapies at this time, majority of the pediatric EGID patients may require continued care well into their adulthood. However, to date, scant data are available regarding the health care transition (HCT), the transition of care (TC), and the effectiveness of transfer of care EGID patients from pediatric-oriented to adult-oriented providers.
Herein, we review the lessons learnt from transfer of care of children with other chronic gastrointestinal and allergic conditions, analyze the current knowledge, potential barriers, the role of various stakeholders in successful transfer of care of EGID patients, propose a conceptual framework for HCT and TC of EGID patients, and identify outcome measures to ensure the quality of progression of care.
Abbreviations
COVID-19 | Corona virus disease - 2019 |
EC | Eosinophilic colitis |
EEn | Eosinophilic enteritis |
EG | Eosinophilic gastritis |
EGID | Eosinophilic gastrointestinal disease |
EoE | Eosinophilic esophagitis |
HCT | Healthcare transition |
IBD | Inflammatory bowel disease |
neEGIDs | Non-esophageal eosinophilic gastrointestinal disease |
PAGs | Patient advocacy groups |
TC | Transition of care |
1Introduction
Eosinophilic gastrointestinal diseases (EGIDs) are a heterogeneous group of chronic diseases that involve one or more parts of the gastrointestinal tract. They are characterized by eosinophilic infiltration in the absence of secondary causes of eosinophilia [1]. Even though the EGIDs are classified as rare diseases [2], they can impose a substantial healthcare burden [3]. Eosinophilic esophagitis (EoE) is the most well-studied form of EGID [4] and is estimated to affect 50 per 100,000 individuals living in the United States (US) [5]. The non-esophageal EGIDs (neEGIDs) including eosinophilic gastritis (EG), eosinophilic enteritis (EEn), and eosinophilic colitis (EC) are relatively uncommon and are estimated to affect between 2 - 8 per 100,000 individuals living in the US [6]. Nearly 40% of the EGID patients present in pediatric age group [7]. Since EGIDs can have a protracted course of illness and that we do not have a cure at this time, affected children and adolescents may continue to have ongoing symptoms and develop complications over time. As such, they may require timely evaluation and treatment which will involve transitioning their care from pediatric-oriented to adult-oriented providers as they enter adulthood.
Healthcare transition (HCT) is a dynamic process and it starts early (between 12 to 14 years of age). The goals of HCT is to provide developmentally appropriate and disease specific knowledge and tools to adolescents and young adults with chronic diseases. This allows them to take ownership of their medical condition and learn about treatment options and measured outcomes. It also fosters independence as they progress from a family-centered to a patient-centered medical care paradigm [8–10]. HCT culminates in transfer of care (TC) which can be seen as a discrete event involving official progression of management from pediatric to the adult healthcare provider as well as evolvement of care from parents to the patient.
While substantial progress has been made over the past decade in understanding the epidemiology, genetic underpinnings, diagnosis, and management of EGIDs [11], very little research has focused on the transition of care of EGID patients. To address this important yet systematically understudied area, we (a) reviewed the lessons learnt from other chronic gastrointestinal and allergic diseases, (b) summarized the current knowledge, known barriers and opportunities, and the role of various stakeholders in successful transition of care of EGID patients, (c) proposed a conceptual framework for HCT and TC of EGID patients, and (d) identified pertinent outcome measures to ensure high quality progression of care.
2Lessons from other chronic conditions
Like EGIDs, both inflammatory bowel disease (IBD) and asthma are chronic conditions and can lead to debilitating disease requiring active and maintenance therapy, and also require frequent monitoring through office-based assessments and objective testing [12, 13]. Suboptimal adherence/ compliance to medical therapy is one of the critical challenges identified during the transition of care of IBD and asthma patients. Several factors can be associated with this including the young age, disease activity status, heavy medication (or pill) burden, high cost of medications, refill inconvenience, perceived lack of benefit, feeling of being uninformed about the effect of medication, nuances of the insurance coverage, low socioeconomic status, and risk-taking behavior. It can also be associated with lack of transition readiness, higher rates of depression, anxiety, and lack of social coping skills in adolescents [14–16]. From a health systems standpoint, the need to provide adequate and appropriate transition resources and transition-related services to adolescents and young adults persist. Some of the common barriers include lack of time, system support, and/or reimbursements for services provided by the healthcare providers [17].
3Current state of transition of care in EGIDs
In an online survey, HCT readiness was assessed in adolescents and young adults aged 13–25 years diagnosed with EoE and eosinophilic gastroenteritis and their parents using the Self-Management and Transition to Adulthood with Rx Questionnaire - a six domain self-report tool. This study found that over 75% of patients and parents had no HCT knowledge and their HCT readiness scores were lower than that of other chronic health conditions [18]. Another online survey examined EoE patients’ perceptions on the challenges faced by them during their transition to adult healthcare and found that most respondents struggled with meal planning, food shopping, cooking/ finding foods that did not exacerbate their condition. Almost 50% of them were worried about managing their condition in the future. They also did not fully understand the nuances of their insurance coverage. [19] In another study adults with a diagnosis of EoE were found to have significantly higher life insurance premiums (by 19%) when compared to those without a diagnosis of EoE [20].
Taken together, there are very limited data on the HCT and TC process involving EoE and ne-EGIDs. Particularly, there are no reports from countries other than the US. Available data suggests that there is significant deficit in EGID-related HCT knowledge, preparation, and readiness, and there are no studies on assessing the effectiveness of transition programs in EGID populations. These observations perhaps also reflect the lack of awareness about the transition of care of EGID patients among healthcare providers which is further illustrated by the absence of mention of TC in the updated consensus recommendations for management of children and adults with EoE [21, 22].
4Developing transition of care program for EGID patients
The overarching goal of the transition of care program for EGID patients should be to implement optimal care and the continuity of that care through a shared decision-making process. At the very core, it should aim towards alleviating parents’ fears in allowing independent care management decisions by the adolescent patient, and create a comfortable and supportive environment for the young patient to transition to adult care especially in the context of psychologic and behavioral issues among adolescents with EGIDs [23–25]. Furthermore, the transition program should be a continually learning algorithmic approach that facilitates ongoing quality improvement and learning for all stakeholders (Fig. 1).
Fig. 1
Elements essential for transition of care of EGID patients.
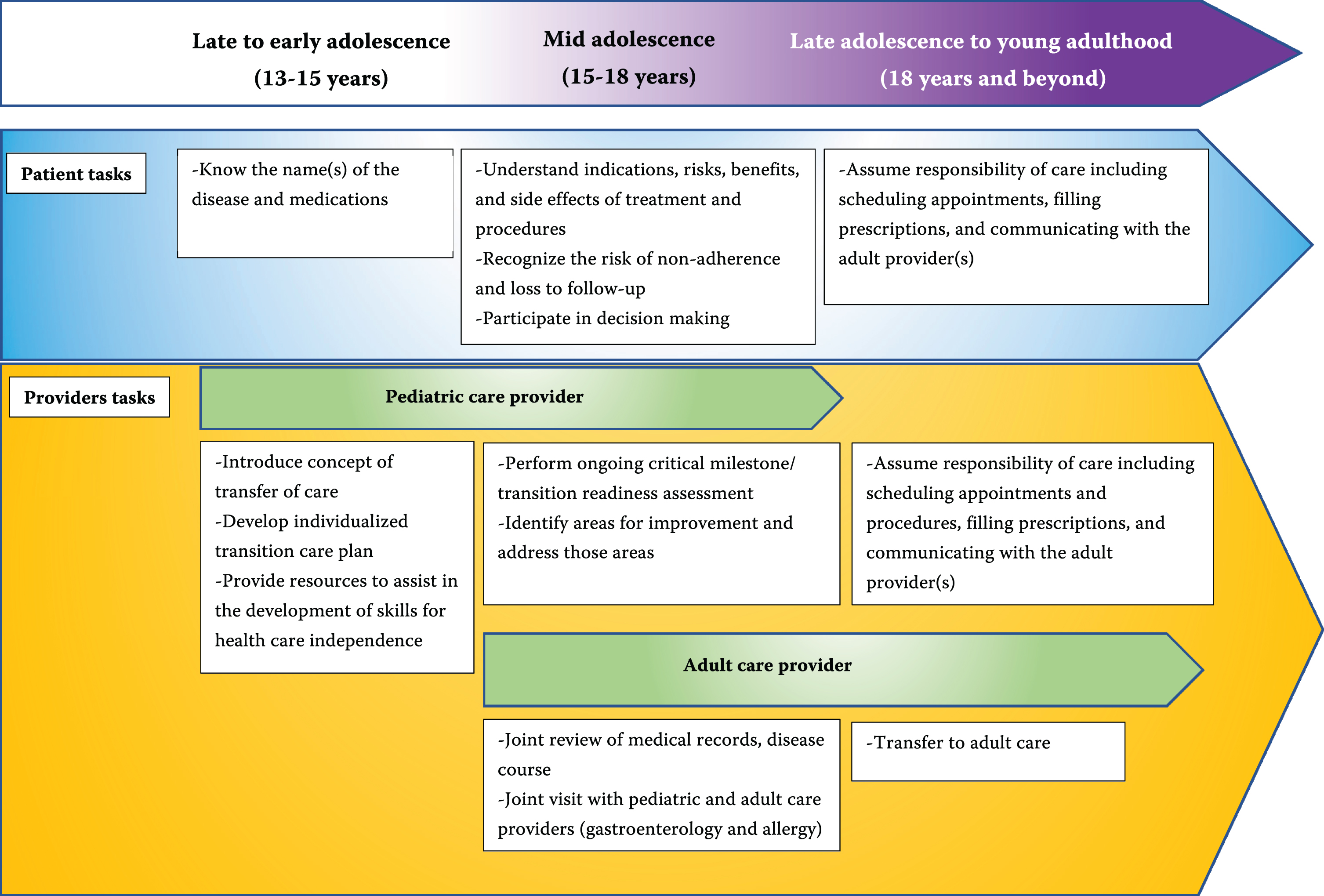
4.1Proposed transition care model
Structured transition programs have been shown to improve medical treatment plan adherence and disease control in chronic diseases [26]. For EGID patients, a diverse group of providers including a pediatric gastroenterologist, adult gastroenterologist, allergist, dietitian, social workers, and psychologists are enrolled to provide optimal care across their lifespan. As such, specialized disease-based approach focusing on engaging adolescent EGID patients, their caregivers, and the stakeholders can facilitate progression of their care. However, this approach is often personnel-heavy, tailored to the needs of a specific institution, and requires considerable resources for implementation and delivery. As such, it cannot be easily translated or transferred to another site/institution. Efforts are needed to develop an EGID transition of care pathway which can be easily adapted across the institutions and practice platforms.
4.2Existing barriers and opportunities
These can be broadly categorized, albeit with overlaps, as patient and parent, healthcare providers, and the healthcare system related factors and are summarized in Table 1.
Table 1
Existing barriers for developing an effective health care transition in EGIDs
| Patient and Parent | Provider | Healthcare system |
| •Inability to recognize EGIDs as chronic disease requiring long-term management and follow-up | •Limited understanding of differences between symptoms, diagnostic testing, and available treatments in the pediatric versus adult practice | •Limited transition programs |
| •Absence of a written individualized transition care plan | ||
| •Lack of transition readiness (as measured by TRAQ) | •Incompatibility between the electronic health record platforms between different institutions | |
| •Adherence to treatment plan during adolescence and transition | •Availability of other healthcare providers (e.g., Allergists and Immunologists focused on EGIDs, dietitians who are well-versed with challenges unique to EGID patients) | Limited avenues to identify adult provider to transition care |
| •Limited program funding (infrastructure, educational materials, administrative support) | ||
| Understanding of the long-term implications of treatment (e.g., commonly used dietary elimination or medication approach) | Involvement of other sub-specialists to manage co-morbidities associated with EGIDs (e.g., involvement of Dermatology, Pulmonology, Rheumatology) | Lack of resources (e.g., funding for a transition coordinator) |
| •Reimbursement for transition services (more prolonged and more frequent clinic visits, combined adult/pediatric clinic visits) | ||
| •Acceptance to transition to an adult provider | •Lack of training in transitional care | |
| •Level of parental involvement | •Long wait-times for evaluation by sub-specialists and for endoscopic evaluations | |
| •Level of parental involvement Financial burden (insurance process related to scheduling procedures, obtaining medications, related to travel to another EGID center for care | Communication gaps between adult and pediatric providers within the same institution and/or across the institutions | In certain circumstances, the complexities related to the lack of medical records and/or disjointed health systems |
| •Adult providers’ comfort on interactions with adolescents |
One of the most important patient and parent-related factor is their inability to recognize that EGIDs are chronic diseases requiring long term management and frequent follow-ups. This can contribute towards their lack of preparedness to transition to adult oriented providers. Although not well understood at this time, it will be important to study the impact of patient demographics (race, age, ethnicity, socio-economic status, and patient education) and their cultural beliefs and attitudes, trust in the healthcare system, and perceived benefits of transfer of care to adult-oriented providers.
The factors related to healthcare providers include the extent of awareness among physicians about the differences in presentation, diagnosis, and management of EGIDs in children versus adults, continuation or establishing care with other sub-specialists who may have a key role in managing EGID related issues (such as Allergist and Immunologist, Dietician, Dermatologist, Pulmonologist, etc), and developing tools to track the outcomes as an adult EGID patient.
The healthcare system related issues include only a few specialized centers focused on EGIDs [27, 28], identifying an adult provider(s) to whom the care can be transferred, wait-time to establish care [29, 30], and the barriers associated with the lack of compatible medical record systems or with disjointed health systems wherein prior testing, results, and data are not readily available for review by the adult providers.
5Outcomes and health literacy in EGID patients
The ideal transition of care outcomes for EGID patients must be applicable in pediatric and adult settings, subject to continuous assessment over time, and be predictive of critical clinical endpoints such as resolution of eosinophilic inflammation in eosinophilic gastritis or complications such as development of esophageal stricture in EoE.
5.1Generic checklist
A generic transition checklist for EGID patients could include assessing their transition skill attainment such as carrying health insurance information, awareness of health privacy rights, ability to self-assess symptoms, independent communication with treating physician/ nurse, awareness of disability resources for disease imposed limitations can potentially address barriers found to transcend particular conditions [17].
5.2EGID specific checklist
For EGID patients who are on dietary elimination approach, it will be important to assess their ability to read and understand nutrition labels. This will be essential for them to know which of the dietary elements they need to avoid and will help with their adherence to the specialized diet. They need to become adept at interacting with a dietitian to ensure that they are getting balanced nutrition and are minimizing their risk for nutritional deficiencies. For those who are on medications, the outcomes to track would likely include their ability to list current medications, read and understand prescription labels for appropriate dosing, adherence to the medications, refilling of medications, and identifying potential long-term consequences related to taking medications (e.g., understanding the symptoms of adrenal insufficiency in a EoE patient with adrenal dysfunction due to topical steroids).
For all EGID patients it will be important to study if they understand how to prepare for disease assessments (e.g., upper endoscopy and colonoscopy when applicable), recognize signs/symptoms of emergency situations (e.g., esophageal food impaction in EoE) irrespective of their treatment approach. An objective outcome for instance in patients with EoE could be the number patients from a particular institution or practice undergoing esophageal dilations over time.
It is conceivable that outcomes can become more well-defined to both EoE and neEGIDs in the future as we gain deeper understanding of their natural history.
6Resources needed for effective transfer of care of EGID patients
As summarized in Table 2, effective transition of care of EGID patients will require significant resources and synergy between multiple stakeholders. Ideally, it would be a multi-year process and will require buy-in from the provider, patient, caregivers/family members, and the healthcare system. Of course, there can be scenarios where there will be limited time available to orchestrate all the moving parts to ensure a smooth transition. However, in case of an established patient, for the most part, providers do have at least 2-3 years, if not more to introduce, begin, and execute transition of their care.
Table 2
Resources for transfer of care of EGID patients
| Role/ Resource | |
| Transition coordinator | •Bridge between pediatric and adult world |
| •Assess readiness and self-management skills | |
| •Improve the adherence to therapy and self-management skills | |
| Healthcare providers | •Dedicated transition clinic |
| •Longer visit (around 40 min visit) | |
| •Reminders to perform transition of care according to schedule | |
| •Pre-visit planning to review medical summary | |
| •Assistance with assessment and patient education | |
| •Foster adult-pediatric partnership | |
| Electronic health record | •Programming transition tools |
| •Design approaches to track service delivery | |
| •Monitor patient performance on desired outcomes | |
| •cross-communication between the physicians within the same institution | |
| •Networking with providers in different institutions | |
| •Standardize the transition process | |
| Telemedicine | •May substitute for an in-person visit (especially if the patient must travel long-distance to visit a specialized center) |
| •Multiple providers can engage with the patient simultaneously | |
| Patient advocacy groups (PAGs) | •Spread the importance of HCT and TC |
| •Wide reach through on-line and in-person forums | |
| •Create/ share list of providers to meet patients’ individual needs | |
| •Collaborate with researchers and healthcare providers | |
| •Inform policies and interventions •Weblinks for some of the PAGs focused on EGIDs APFED (https://www.apfed.org/) CURED (http://www.curedfoundation.org/) EFC (https://www.eoscoalition.org/) EOSNETWORK (https://www.eosnetwork.org/) ausEE (https://www.ausee.org/) | |
| Professional societies and organizations | •Provide list of physicians that take care of EGID patients |
| •Publish peer-reviewed educational materials to educate stakeholders •Weblinks for some of the professional societies and organizations NASPGHAN (https://naspghan.org/) AGA (https://www.gastro.org/) ACG (https://www.gi.org/) AAAAI (https://www.aaaai.org/) ACAAI (https://acaai.org/) CEGIR (https://www1.rarediseasesnetwork.org/cms/cegir) | |
| Social media and applications | •Engaging adolescent and young adult EGID patients through social media (e.g., Instagram, Facebook, Twitter, Tik-Tok) |
| •Developing an application like the Doc4me app (http://www.doc4me-app.com) for the EGID community |
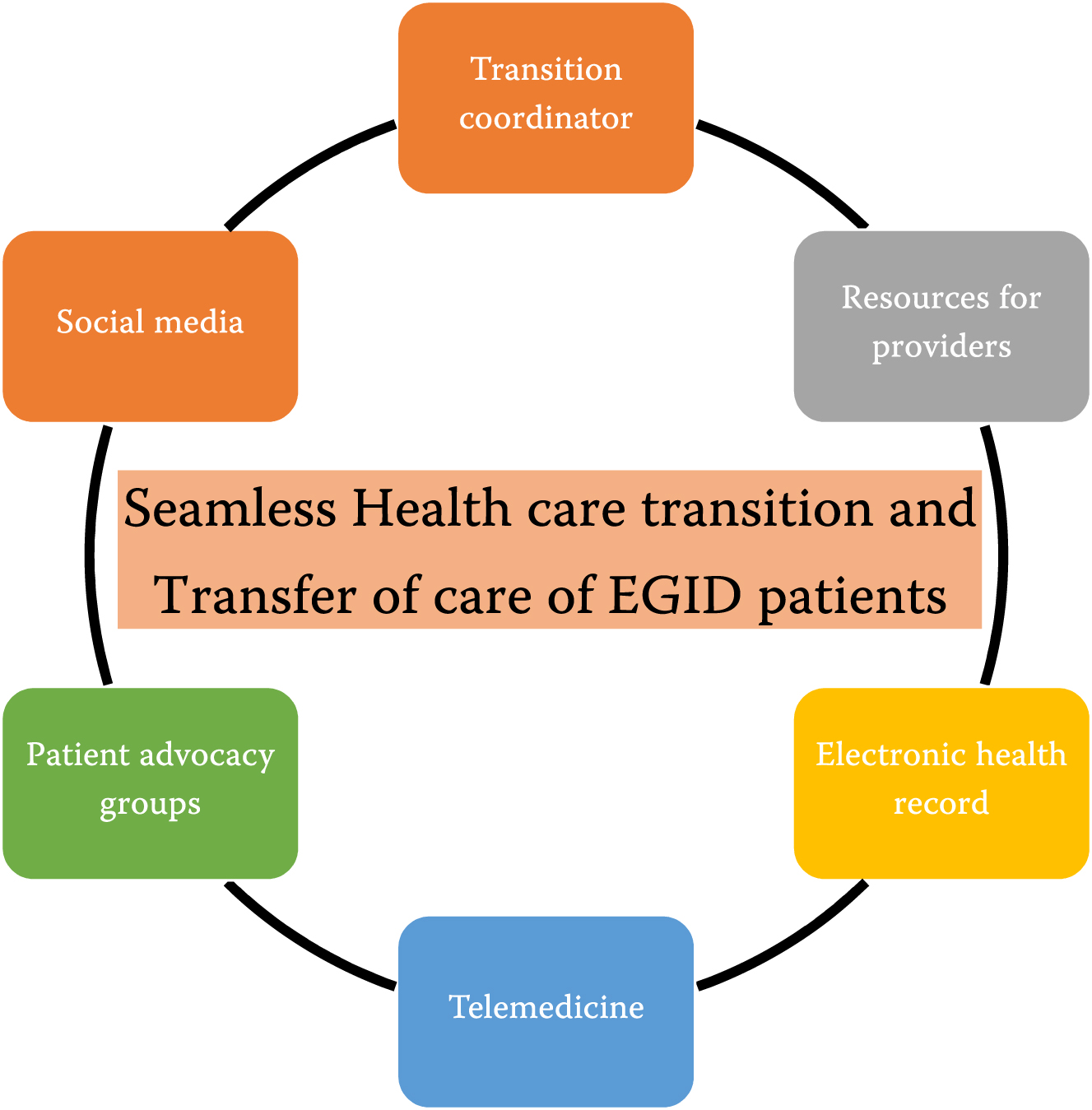
Having a transition coordinator can effectively serve as a bridge between the pediatric and adult world and assess the readiness for transition of care [31]. However, health system priorities and/or financial constraints can weigh upon the feasibility of hiring a dedicated transition coordinator for EGIDs. In these situations, as a starting point, perhaps sharing the effort of a transition coordinator for other established disorders (such as IBD or asthma) can be considered.
A dedicated EGID transition clinic visit with longer visit time for healthcare providers can support providers towards effective transition of care. Likewise, the electronic health record can be used to develop programs to ensure delivery and consistency of transition services at the right time. It can also facilitate tracking of service delivery and patients’ performance on desired program outcomes (i.e., achievement of transition skills and knowledge acquisition).
Recent circumstances due to COVID-19 pandemic have propelled telemedicine to the forefront. Since EGIDs are relatively uncommon and there are only a limited number of specialized centers capable of providing interdisciplinary care [27], using telemedicine can be quite efficient. Additionally, multiple providers can engage with the patient simultaneously obviating the need for an in-person visit [32].
Patient advocacy groups (PAGs) linked to EGIDs worldwide can play a critical role in the transition between pediatric and adult care [33]. Through their collaborations PAGs can also provide the patients perspectives to researchers and the healthcare providers to develop resources to strengthen the process of HCT and TC [34, 35]. Additionally, the professional societies can also provide general listings of physicians who take care of adult EGID patients.
Due to the generational longing to adapt social media and networking technologies, some adolescents, and young adults with EGIDs may prefer obtaining transition experiences and information from social media (e.g., Instagram, Facebook, Twitter, Tik-Tok) (63). Developing an application like the Doc4me app (http://www.doc4me-app.com) which provides resources for pediatric IBD patients, for the EGID community could be very helpful in locating adult EGID providers and increase the likelihood of a seamless transition (Fig. 2).
Fig. 2
Towards seamless transition of care of EGID patients.
7Special considerations
The timing of the TC can be impacted by the symptoms or the disease activity. For example, if a patient ready for TC is experiencing active symptoms and/or flare-up of the disease, the TC may be delayed until the symptoms resolve and/or the disease is in remission. This approach will allow smooth and stress-free progression of care and minimize burden on the accepting provider associated with managing a EGID patient who is relatively new to the practice.
Another important consideration would be with regards to TC of an EGID patient who is in the middle of dietary elimination therapy. In this scenario, if the patient is on a stable dietary elimination regimen, then one might consider proceeding with the TC as planned. However, if the patient is not on a stable dietary elimination therapy and/or symptomatic on the existing dietary elimination therapy then the TC may be delayed until the symptoms and/or disease activity is well controlled. However, if delaying the TC is not an option then it would be prudent to have a proper hand-off with the adult provider who will be assuming the care of the individual.
Other special considerations include the negative impact of undernutrition and vitamin and micronutrient deficiencies due to chronic eosinophilic inflammation and dietary elimination therapies in children and adolescents with EGIDs [36]. The impact of these factors are on growth are only starting to be studied in detail [37]. Furthermore, as with pediatric onset-IBD patients, all stakeholders need to be aware that the adolescents and young adults with neEGIDs can have delayed puberty or amenorrhea [38–40].
8Conclusions
With increasing prevalence of EGIDs and lack of curative therapies at this time, more and more EGID patients are expected to transition from pediatric to adult care. There is paucity of HCT and TC data to specifically inform the process of transitioning the care of an EGID patients. Developing strategies for seamless transition of EGID patients should become a priority for all stakeholders including the patients, parents, and healthcare providers.
Conflict of interest
G.H.: No potential conflicts for this project. Full disclosures as follows: Consultant: Sanofi Genzyme, Regenron, Allakos, Shire/Takeda.
A. C-R.: No potential conflicts for this project.
D.K.: Received consulting fees from Adare, Phathom, Takeda and Celgene.
J.M.S.: Received research funding from NIH, FARE, Regeneron, Sanofi, Novartis and consulting fees from Regeneron, Sanofi, Takeda, and Novartis.
B.G.: Received consulting and/or speaking fees from Johnson&Johnson, Diasorin Molecular, Nestle Nutrition, Nutricia North America, Mead Johnson Nutrition, Evolve Biosystems, Inc., and Ironwood Pharmaceuticals.
A.B.: Received research funding from Nutricia, Norgine, Thelial, SST and Bayer and received speaker and/or consulting fees from Laborie, Arena, EsoCap, Medtronic, Dr. Falk Pharma, Calypso Biotech, Alimentiv, Sanofi, Reckett Benkiser, Regeneron and AstraZeneca
E.S.D.: No potential conflicts for this project. Full disclosures as follows: Research funding: Adare/Ellodi, Allakos, AstraZeneca, GSK, Meritage, Miraca, Nutricia, Celgene/Receptos/BMS, Regeneron, Shire/Takeda; Consultant: Abbott, Adare/ Ellodi, Aimmune, Allakos, Amgen, Arena, AstraZeneca, Avir, Biorasi, Calypso, Celgene/Receptos/BMS, Celldex, Eli Lilly, EsoCap, GSK, Gossamer Bio, Landos, Morphic, Parexel/Calyx, Regeneron, Robarts/Alimentiv, Salix, Sanofi, Shire/Takeda; Educational grant: Allakos, Banner, Holoclara.
J.H.: Received research funding from Gilead, Janssen, and Abbvie.
S.K.G.: Consultant Adare, Allakos, Celgene, Gossamer Bio, QOL, UpToDate, Medscape, Viaskin. Research support from Shire and NIH U54 grant to CEGIR.
Author contributions
Study Concept and Design: G.H., A. C-R., D.K., J.M.S., A.B., E.S.D., J.H., S.K.G.
Acquisition, analysis, or interpretation of data: G.H., D.K., J.M.S., B.G., A.B., E.S.D., J.H., S.K.G.
Drafting the manuscript: G.H., A. C-R., D.K., J.M.S., B.G., A.B., E.S.D., J.H., S.K.G.
Critical Revisions of the manuscript for important intellectual content: G.H., A. C-R., D.K., J.M.S., B.G., A.B., E.S.D., J.H., S.K.G.
References
[1] | Gonsalves N. , Eosinophilic Gastrointestinal Disorders,, Clinical Reviews in Allergy and Immunology 57: ((2019) ), pp. 272–285. |
[2] | Cheng K. , Gupta S.K. , Kantor S. , Kuhl J.T. , Aceves S.S. , et al., Creating a multi-center rare disease consortium –the Consortium of Eosinophilic Gastrointestinal Disease Researchers (CEGIR), Transl Sci Rare Dis 2: (3–4) ((2017) ), 141–155. |
[3] | Jensen E.T. , Kappelman M.D. , Martin C.F. and Dellon E.S. , Health-care utilization, costs, and the burden of disease related to eosinophilic esophagitis in the United States, Am J Gastroenterol 110: (5) ((2015) ), 626–632. |
[4] | Dellon E.S. and Hirano I. , Epidemiology and Natural History of Eosinophilic Esophagitis, Gastroenterology 154: (2) ((2018) ), 319–332.e3. |
[5] | Katzka D.A. , Eosinophilic esophagitis,ITC, Ann Intern Med 172: (9) ((2020) ), 66–80. |
[6] | Pesek R.D. , Reed C.C. , Muir A.B. , Fulkerson P.C. , Menard-Katcher C. , Falk G.W. , et al.. Increasing Rates of Diagnosis, Substantial Co-Occurrence, and Variable Treatment Patterns of Eosinophilic Gastritis, Gastroenteritis, and Colitis Based on 10-Year Data Across a Multicenter Consortium, Am J Gastroenterol 114: (6) ((2019) ), 984–994. |
[7] | Dellon E.S. , Jensen E.T. , Martin C.F. , Shaheen N.J. and Kappelman M.D. , Prevalence of Eosinophilic Esophagitis in the United States, Clin Gastroenterol Hepatol 12: (4) 2014. |
[8] | Crowley R. , Wolfe I. , Lock K. and McKee M. , Improving the transition between paediatric and adult healthcare: A systematic review, Arch Dis Child 96: (6) ((2011) ), 548–553. |
[9] | Blum R.W. , Garell D. , Hodgman C.H. , Jorissen T.W. , Okinow N.A. , Orr D.P. , et al., Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine, J Adolesc Heal 14: (7) ((1993) ), 570–576. |
[10] | Cooley W.C. , Sagerman P.J. , Barr M.S. , Ciccarelli M. , Hergenroeder A.C. , Klitzner T.S. , et al., Clinical report - Supporting the health care transition from adolescence to adulthood in the medical home, Pediatrics 128: (1) ((2011) ), 182–200. |
[11] | Pesek R.D. and Rothenberg M.E. , Eosinophilic gastrointestinal disease below the belt, Journal of Allergy and Clinical Immunology 145: ((2020) ), pp. 87–89.e1. |
[12] | Ng S.C. , Shi H.Y. , Hamidi N. , Underwood F.E. , Tang W. , Benchimol E.I. , et al., Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies, Lancet 390: (10114) ((2017) ), 2769–2778. |
[13] | Serebrisky D. and Wiznia A. , Pediatric asthma: A global epidemic, Annals of Global Health 85: 2019. |
[14] | Kaplan A. and Price D. , Treatment adherence in adolescents with asthma, Journal of Asthma and Allergy 13: ((2020) ), pp. 39–49. |
[15] | Bardach N.S. , Neel C. , Kleinman L.C. , McCulloch C.E. , Thombley R. , Zima B.T. , et al., Depression, anxiety, and emergency department use for asthma, Pediatrics, 144: (4) 2019. |
[16] | MacKner L.M. , Greenley R.N. , Szigethy E. , Herzer M. , Deer K. and Hommel K.A. , Psychosocial issues in pediatric inflammatory bowel disease: Report of the north american society for pediatric gastroenterology, hepatology, and nutrition, Journal of Pediatric Gastroenterology and Nutrition 56: ((2013) ), pp. 449–458. |
[17] | Gray W.N. , Schaefer M.R. , Resmini-Rawlinson A. and Wagoner S.T. , Barriers to transition from pediatric to adult care: A systematic review, J Pediatr Psychol 43: (5) ((2018) ), 488–502. |
[18] | Eluri S. , Book W.M. , Kodroff E. , Strobel M.J. , Gebhart J.H. , Jones P.D. , et al., Lack of Knowledge and Low Readiness for Health Care Transition in Eosinophilic Esophagitis and Eosinophilic Gastroenteritis, J Pediatr Gastroenterol Nutr 65: (1) ((2017) ), 53–57. |
[19] | J. R, G. F, E. M, N. H, I. K, J. W, et al., The impact of the transition from pediatric to adult care on patients with eosinophilic esophagitis: Insights from a patient perspectives survey, J Pediatr Gastroenterol Nutr [Internet]. 2019;69(Supplement 2). Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emexa&NEWS=N&AN=630751635 |
[20] | Leiman D.A. , Kochar B. , Posner S. , Fan C. , Patel A. , Shaheen O. , et al., A diagnosis of eosinophilic esophagitis is associated with increased life insurance premiums, Dis Esophagus 31: (8) 2018. |
[21] | Lucendo A.J. , Molina-Infante J. , Arias Á. , von Arnim U. , Broord A.J. , Bussmann C. , et al., Guidelines on eosinophilic esophagitis: evidence-based statements and recommendations for diagnosis and management in children and adults, United European Gastroenterology Journal 5: ((2017) ), pp. 335–358. |
[22] | Dellon E.S. , Liacouras C.A. , Molina-Infante J. , Furuta G.T. , Spergel J.M. and Zevit N. . Updated International Consensus Diagnostic Criteria for Eosinophilic Esophagitis: Proceedings of the AGREE Conference. In: Gastroenterology. (2018), pp. 1022–1033.e10. |
[23] | Wang R. , Hirano I. , Doerfler B. , Zalewski A. , Gonsalves N. and Taft T. , Assessing Adherence and Barriers to Long-Term Elimination Diet Therapy in Adults with Eosinophilic Esophagitis, Dig Dis Sci 63: (7) ((2018) ), 1756–1762. |
[24] | Reed C.C. , Corder S.R. , Kim E. , Sanders E. , Tappata M. , Eluri S. , et al., Psychiatric Comorbidities and Psychiatric Medication Use Are Highly Prevalent in Patients with Eosinophilic Esophagitis and Associate with Clinical Presentation, Am J Gastroenterol 115: (6) ((2020) ), 853–858. |
[25] | Harris R.F. , Menard-Katcher C. , Atkins D. , Furuta G.T. and Klinnert M.D. , Psychosocial dysfunction in children and adolescents with eosinophilic esophagitis, J Pediatr Gastroenterol Nutr 57: (4) ((2013) ), 500–505. |
[26] | Goralski J.L. , Nasr S.Z. and Uluer A. , Overcoming barriers to a successful transition from pediatric to adult care, Pediatric Pulmonology 52: ((2017) ), pp. S52–60. |
[27] | Rukasin C.R.F. , Hemler J.A. , Dellon E.S. , Curry-Johnson S. and Hiremath G. , Geospatial distribution and characteristics of eosinophilic gastrointestinal disorder clinics in the United States, Ann Allergy, Asthma Immunol 123: (6) ((2019) ), 613–615. |
[28] | Hiremath G.S. , Kodroff E. , Strobel M.J. , Scott M. , Book W. , Reidy C. , et al., Analysis of Unmet Needs of Individuals Affected by Eosinophilic Gastrointestinal Disorders: Towards Health Promotion and Effective Care, Gastroenterology 152: (5) ((2017) ), S851–2. |
[29] | Liddy C. , Liddy C. , Moroz I. , Affleck E. , Boulay E. , Cook S. , et al., How long are canadians waiting to access specialty care? Retrospective study from a primary care perspective, Canadian Family Physician 66: ((2020) ), pp. 434–444. |
[30] | Leddin D. , Armstrong D. , Borgaonkar M. , Bridges R.J. , Fallone C.A. , Telford J.J. , et al., The SAGE wait times program: Survey of Access to GastroEnterology in Canada,pp, Canadian Journal of Gastroenterology 27: ((2013) ), 83–89. |
[31] | Campagna B.R. , Weatherley K. , Shemesh E. and Annunziato R.A. , Adherence to Medication During Transition to Adult Services, Pediatric Drugs 22: ((2020) ), 501–509. |
[32] | Cross R.K. , Jambaulikar G. , Langenberg P. , Tracy J.K. , Collins J.F. , Katz J. , et al., TELEmedicine for Patients with Inflammatory Bowel Disease (TELE-IBD): Design and implementation of randomized clinical trial, Contemp Clin Trials 42: ((2015) ), 132–144. |
[33] | Lara A.A. and Salberg L. , Patient advocacy: What is its role?, PACE - Pacing Clin Electrophysiol 32: (SUPPL. 2), 2009. |
[34] | Chaudhry N.A. , Pham A. , Flint A. , Molina I. , Zaidi Z. , Zimmermann E.M. , et al., College students with inflammatory bowel disease: A qualitative study of challenges associated with college transition and self-care, Heal Equity 2020. |
[35] | Kennedy S.T. and Maddux M.H. , Patient-clinician collaboration in the development of an IBD transfer toolkit, Pediatrics 2019. |
[36] | Licari A. , Votto M. , Scudeller L. , De Silvestri A. , Rebuffi C. , Cianferoni A. , et al., Epidemiology of Nonesophageal Eosinophilic Gastrointestinal Diseases in Symptomatic Patients: A Systematic Review and Meta-Analysis, J Allergy Clin Immunol Pract 2020. |
[37] | Votto M. , De Filippo M. , Olivero F. , Raffaele A. , Cereda E. and De Amici M. , Malnutrition in eosinophilic gastrointestinal disorders, Nutrients 13: ((2021) ), pp. 1–12. |
[38] | Ballinger A.B. , Savage M.O. and Sanderson I.R. , Delayed puberty associated with inflammatory bowel disease, Pediatric Research 53: ((2003) ), pp. 205–210. |
[39] | Perminow G. , Brackmann S. , Lyckander L.G. , Franke A. , Borthne A. , Rydning A. , et al., A characterization in childhood inflammatory bowel disease, a new population-based inception cohort from south-eastern Norway, -07, showing increased incidence in crohn’s disease, Scand J Gastroenterol 44: (4) ((2009) ), 446–456. |
[40] | Licari A. , Votto M. , D’Auria E. , Castagnoli R. , Caimmi S.M.E. and Marseglia G.L. , Eosinophilic Gastrointestinal Diseases in Children: A Practical Review, Curr Pediatr Rev 16: (2) ((2019) ), 106–114. |




