Causal relationship between serum metabolites and interstitial lung disease in humans: A mendelian randomization study
Abstract
BACKGROUND:
A significant proportion of interstitial lung disease (ILD) patients experience two or more comorbidities, leading to an increasing burden of disease, frequent hospitalizations, and premature death.
OBJECTIVE:
To investigate the causal relationship between serum metabolites and ILD in humans using Mendelian randomization.
METHODS:
Genetic loci closely related to human serum metabolites were selected as instrumental variables (IVs), with the inverse-variance weighted method (IVW) as the primary method and the weighted median method (WME) and MR-Egger regression as auxiliary methods for Mendelian randomization analysis of the data. Meanwhile, the causal relationship between human serum metabolites and ILD was evaluated by OR, along with the assessment of the stability and reliability of the results via 3 methods, i.e., heterogeneity testing, gene pleiotropy testing, and sensitivity analysis.
RESULTS:
8,234 single nucleotide polymorphism (SNP) loci were included as IV, among which 23 SNP loci were selected as IV. Specifically, IVW estimated that the risk of ILD in the anti-Jo-1 antibody-positive population was 4.122 times higher than that in the negative population (95% CI: 2.311–5.954,
CONCLUSION:
A positive causal relationship may exist between anti-Jo-1 antibody positivity, anti-SSA antibody positivity, elevated ESR, elevated CRP, and ILD.
1.Introduction
Interstitial lung disease (ILD) is a group of diseases characterized by pulmonary interstitial damage, restrictive ventilatory impairment, active dyspnea, decreased quality of life, and reduced exercise capacity, including idiopathic pulmonary fibrosis, asbestosis, hypersensitivity pneumonitis, and connective tissue disease-associated ILD [1], among which idiopathic pulmonary fibrosis (IPF) is a non-neoplastic pulmonary disease characterized by the formation of scar tissue in the lungs without any known cause. As of 2017, global mortality analysis data showed that the standardized mortality rate of ILD has increased by 11.4% over the past 10 years, with a 49.8% increase in total deaths [2]. Meanwhile, the incidence and mortality of ILD are higher in men and increase with age [3]. The standardized mortality rate associated with IPF has risen by 9.85%. In addition, a significant proportion of ILD patients experience two or more comorbidities, leading to an increasing burden of disease, frequent hospitalizations, and premature death [4, 5]. The population included in this study consists of ILD and IPF patients, numbered J84 and J84.1, respectively, in the International Classification of Diseases 10th Edition (ICD-10) [6].
As a critical component of blood and an essential sample for metabolomics research, the serum contains over 1,000 endogenous small molecule metabolites, the composition of which is complex and diverse, with a wide range of polarities, including plasma proteins, growth factors, hormones, inorganic ions, amino acids, glucose, nucleosides, lipids, and steroids. Since metabolites in serum are derived from various metabolic pathways of the body, an investigation of such metabolites can provide a comprehensive understanding of the body’s metabolism, assess the physiological and pathological status of the body, and identify key disease-related metabolites as targets, which is of great significance in the clinical diagnosis of diseases [7, 8, 9].
Mendelian randomization (MR) analysis utilizes genetic variation as an instrumental variable, and the natural random allocation of genetic variation can help avoid potential confounding factors [10]. In this study, the potential causal relationship between human serum metabolites and ILD was investigated using the two-sample MR method based on pooled data, thereby providing new insights for the prevention, treatment, and prognosis assessment of ILD.
2.Material and methods
2.1Data and sources
The data on human serum metabolites and ILD were obtained from statistical data of genome-wide association studies (IEU GWAS database, https://gwas.mrcieu.ac.uk/). A total of 586,281 patients were included for serum metabolite detection, along with 384,157 ILD patients. In addition, ethical review and informed consent were obtained in the original studies. See Table 1.
2.2Instrumental variables
UK Biobank data were used as a reference in this study, with stringent thresholds adopted to exclude the impact of weak IVs. Specifically, a genetic distance (kb) of 10,000 kb, a linkage disequilibrium (LD) parameter (
2.3Research methods
2.3.1MR analysis
The genetic variables used in the analysis should be significantly associated with the exposure. In this study, after significant IVs were obtained through
The genetic variables extracted as exposure IVs should be independent of confounding factors associated with the selected exposure and outcome. In two-sample Mendelian randomization, it is difficult to validate whether this hypothesis is valid using statistical methods due to the lack of individual-level data. However, given that Mendelian randomization follows the genetic rule of “random allocation of parental alleles to offspring during gamete formation”, the effects of environmental factors and socioeconomic status on genes are relatively small.
IVs only affect the outcome through exposure instead of other biological pathways (i.e., no gene pleiotropy). At the same time, MR-PRESSO and the intercept of MR-Egger regression were applied in this study to assess whether gene pleiotropy exists between SNPs and ILD.
2.3.2Causal effect estimation
Inverse-variance weighted (IVW), MR-Egger regression, and weighted median method (wME) were utilized in this study to estimate the causal effect between depression and ILD.
2.3.3Reliability evaluation
Heterogeneity testing: Heterogeneity testing was performed in this study for IVW and MR-Egger regression, and the
Gene pleiotropy testing: The study used the intercept of MR-Egger regression and the MR-PRESSO method to test for gene pleiotropy between the included SNPs and ILD. The intercept of MR-Egger regression close to 0 indicates a minimal possibility of gene pleiotropy. Additionally, the core of the MR-PRESSO method test involves calculating the IVW results after removing each SNP, followed by calculating the residual sum of squares of the SNP’s effect and the IVW results, and finally summing the residual sum of squares for all SNPs, with a larger value indicating a more significant pleiotropy. If pleiotropy exists, abnormal SNPs are removed using MR-PRESSO to estimate the corrected results, followed by validating the differences between the pre-correction and post-correction results, thereby reducing the impact of gene pleiotropy on the results [12].
Sensitivity analysis: The sensitivity analysis was conducted using the leave-one-out method to individually assess the impact of each SNP on the results. That is, for SNPs with a
2.4Statistical analysis
TwoSampleMR package in R 4.1.1 software was used to complete the analysis in this study. The causal relationship between serum metabolites and IDL was verified using 3 regression models: MR-Egger, IVW, and WME, in which MR-Egger regression fitted a linear function by calculating the correlation between SNPs and serum metabolites, IDL, while WME calculated the effect estimate corresponding to each SNP. Meanwhile, Cochran’s Q test was utilized to determine the heterogeneity of SNPs, with the leave-one-out method used for sensitivity analysis. The significance level was set at
3.Results
3.1Instrumental variable SNP
In the causal association analysis between serum metabolites and ILD, after removing the linkage disequilibrium parameter (
3.2MR analysis results
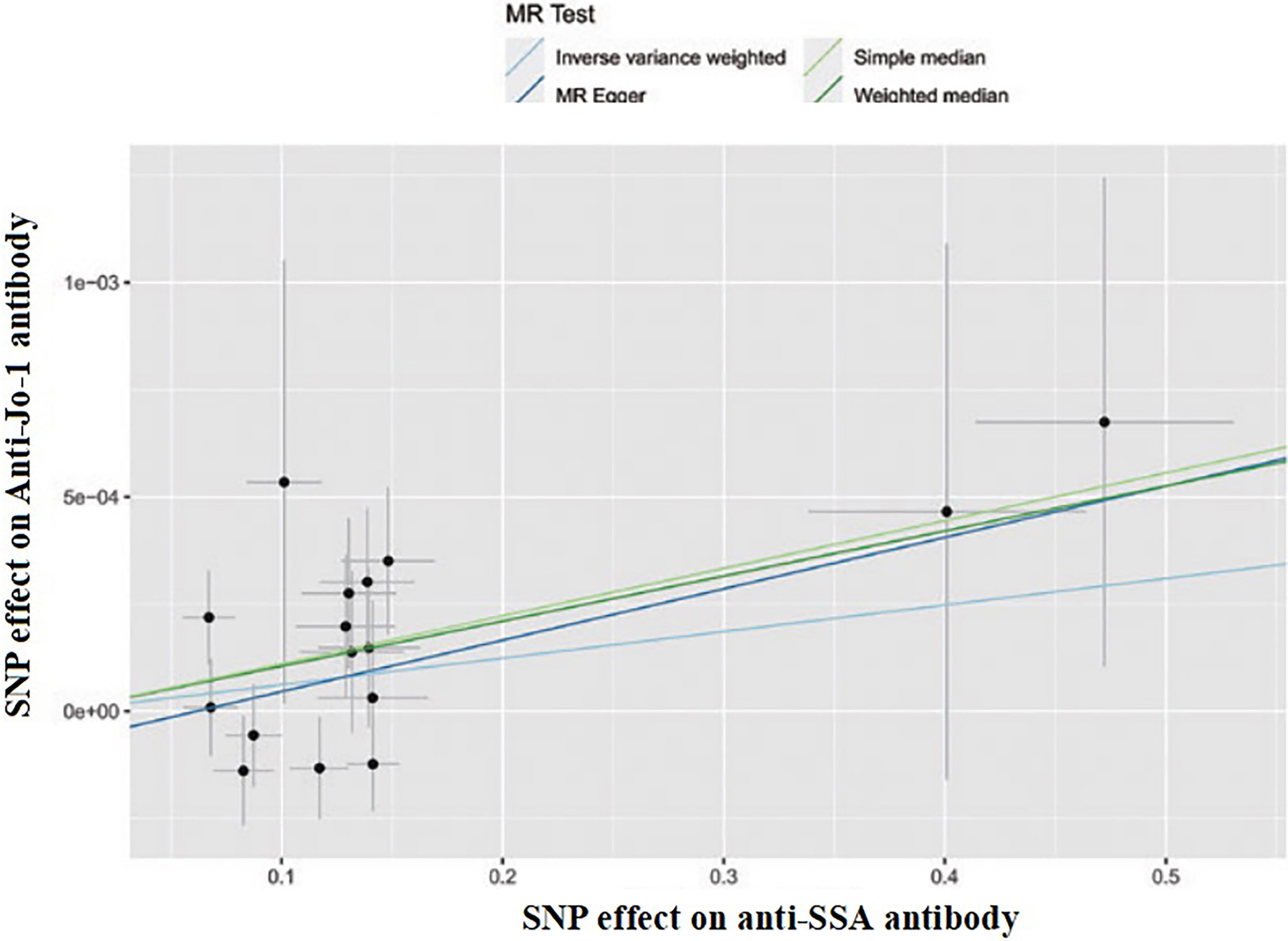
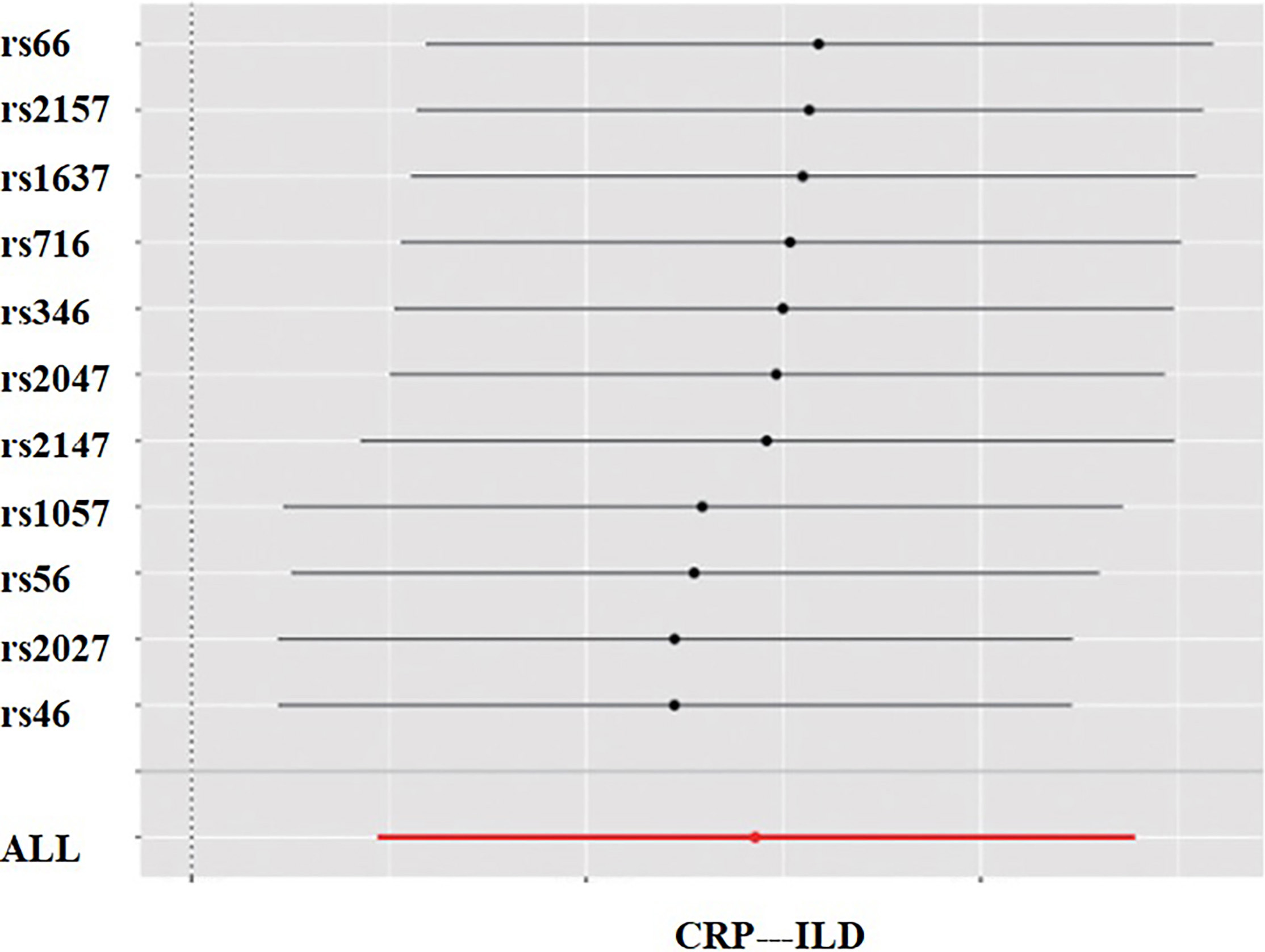
Results from IVW, WME, and MR-Egger regression indicated a positive causal relationship between serum metabolites and ILD. These products include anti-Jo-1, anti-SSA antibody, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP). IVW estimated that the risk of ILD in the anti-Jo-1 antibody-positive group was 4.122 times higher than in the negative group (95% CI: 2.311–5.954,
Table 1
Relationship between anti-Jo-1 antibody positivity and ILD by regression analysis via 3 methods
| Method | b | SE | Wald |
| OR | 95% CI |
|---|---|---|---|---|---|---|
| IVW | 0.181 | 0.067 | 10.038 | 0.009 | 4.122 | 2.311 |
| WME | 0.126 | 0.061 | 7.325 | 0.017 | 1.432 | 1.311 |
| MR egger | 0.175 | 0.154 | 1.121 | 0.021 | 1.124 | 1.433 |
Table 2
Relationship between anti-SSA antibody positivity and ILD by regression analysis via 3 methods
| Method | b | SE | Wald |
| OR | 95% CI |
|---|---|---|---|---|---|---|
| IVW | 0.767 | 0.343 | 11.082 | 0.021 | 2.781 | 1.413 |
| WME | 0.224 | 0.253 | 9.423 | 0.033 | 2.643 | 1.433 |
| MR egger | 0.097 | 0.122 | 2.358 | 0.091 | 1.742 | 0.321 |
Table 3
Relationship between ESR and ILD by regression analysis via 3 methods
| Method | b | SE | Wald |
| OR | 95% CI |
|---|---|---|---|---|---|---|
| IVW | 0.281 | 0.050 | 10.032 | 0.000 | 2.781 | 1.331 |
| WME | 0.126 | 0.061 | 7.325 | 0.007 | 1.432 | 2.511 |
| MR Egger | 0.375 | 0.054 | 8.121 | 0.002 | 3.124 | 1.257 |
Table 4
Relationship between CRP and ILD by regression analysis via 3 methods
| Method | b | SE | Wald |
| OR | 95% CI |
|---|---|---|---|---|---|---|
| IVW | 0.281 | 0.250 | 5.231 | 0.000 | 1.022 | 2.311 |
| WME | 0.362 | 0.161 | 4.351 | 0.072 | 1.424 | 0.711 |
| MR egger | 0.554 | 0.154 | 7.114 | 0.001 | 2.624 | 2.433 |
Figure 1.
SNP effect on anti-Jo-1 antibody.
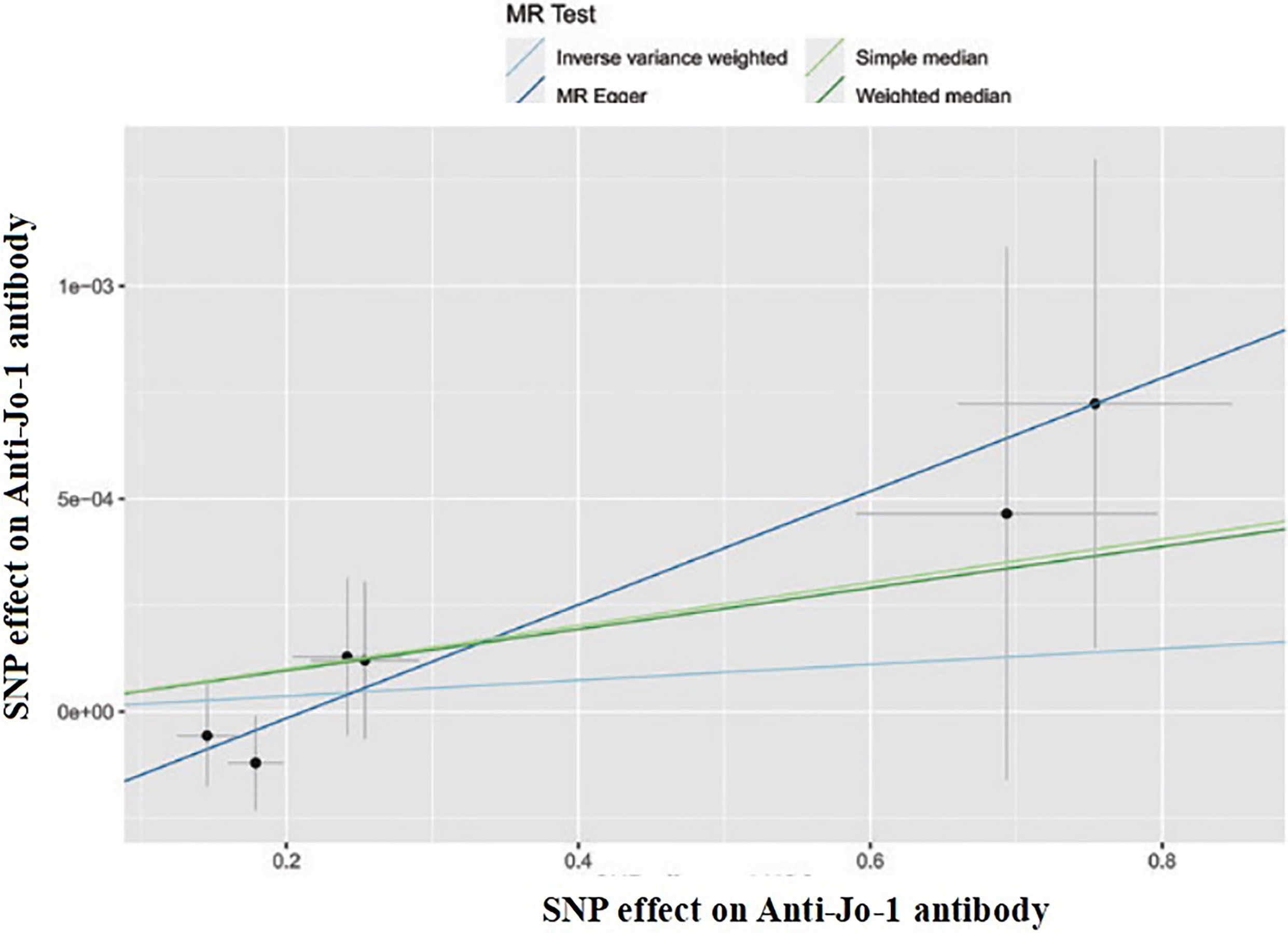
Figure 2.
SNP effect on anti-SSA antibody.
3.3Reliability evaluation
3.3.1Heterogeneity testing
The heterogeneity testing was performed for IVW and MR-Egger regression, with
Table 5
Results of heterogeneity testing
| Method |
|
|
|---|---|---|
| IVW | 26.121 | 0.717 |
| MR egger | 27.314 | 0.921 |
Figure 3.
SNP effect on ESR.
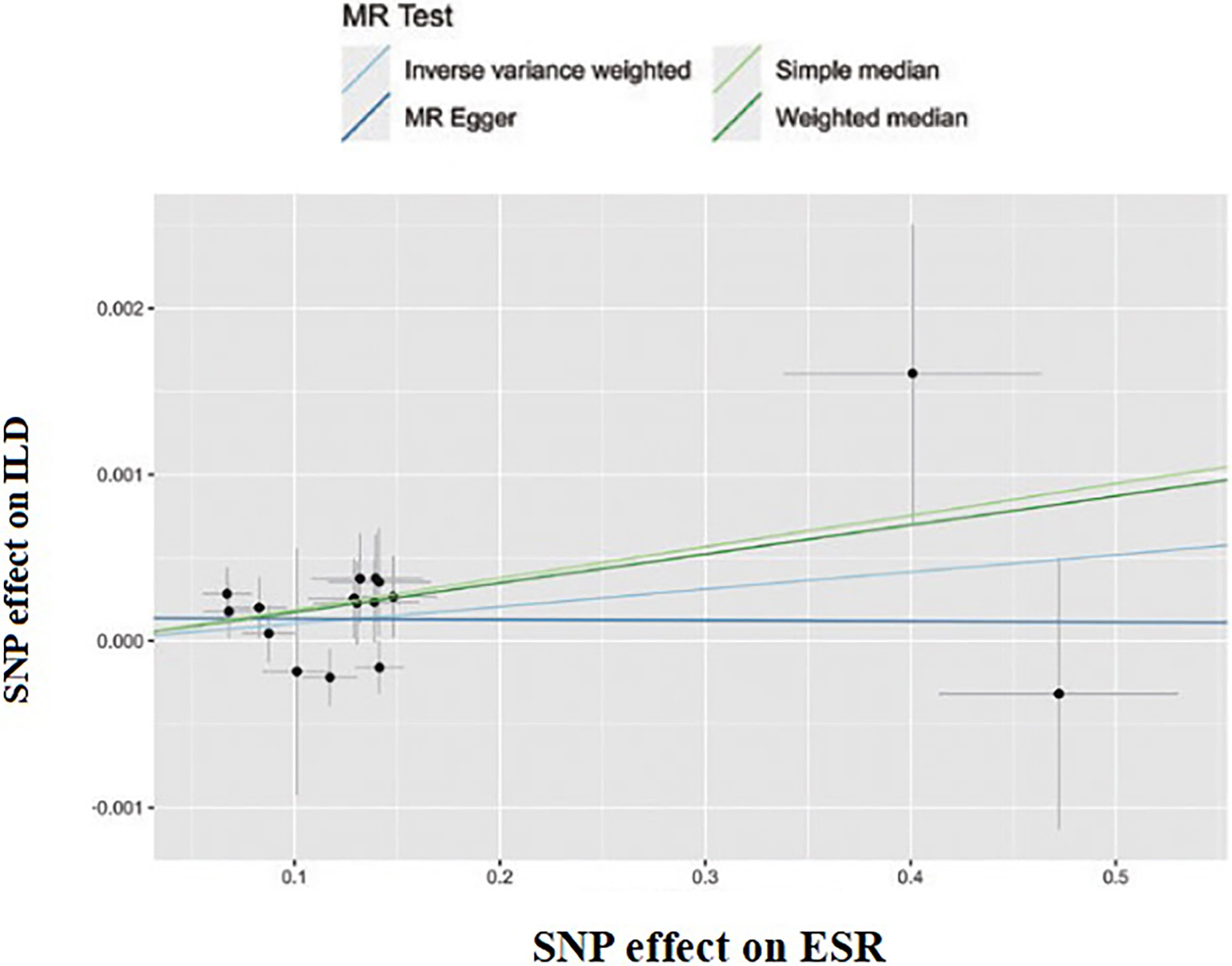
Figure 4.
SNP effect on CRP.
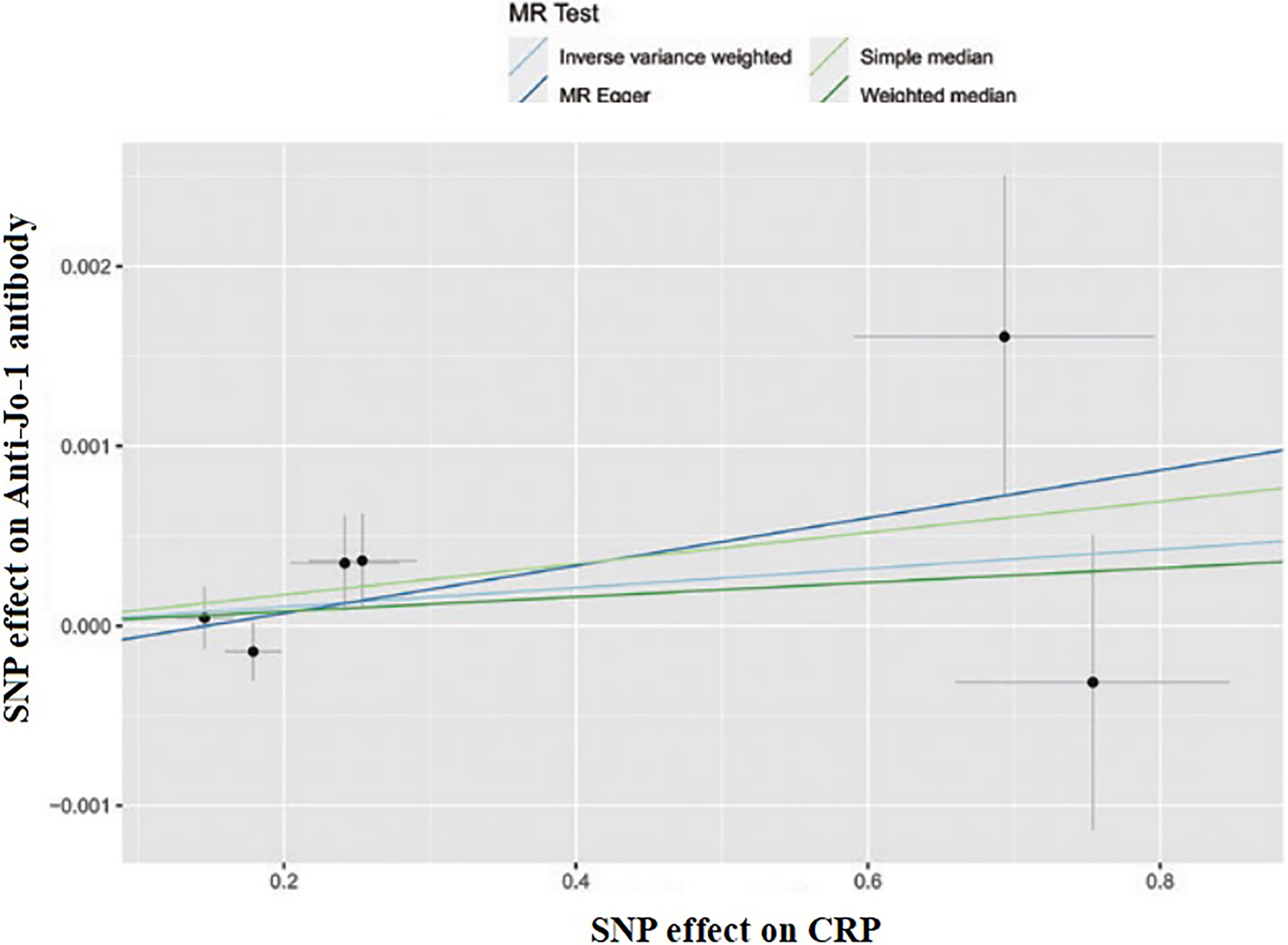
Figure 5.
Anti-Jo-1 antibody – ILD.
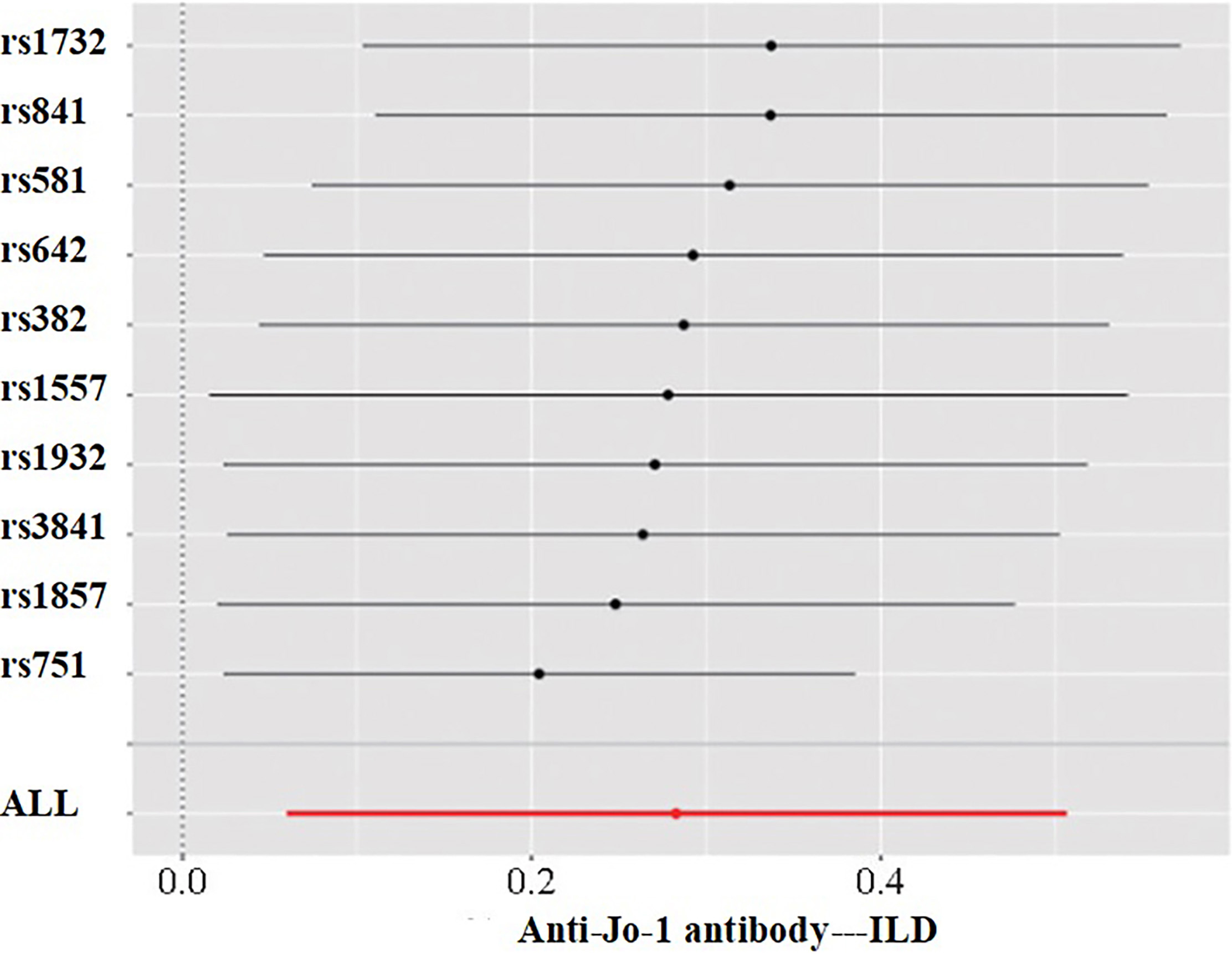
Figure 6.
Anti-SSA antibody – ILD.
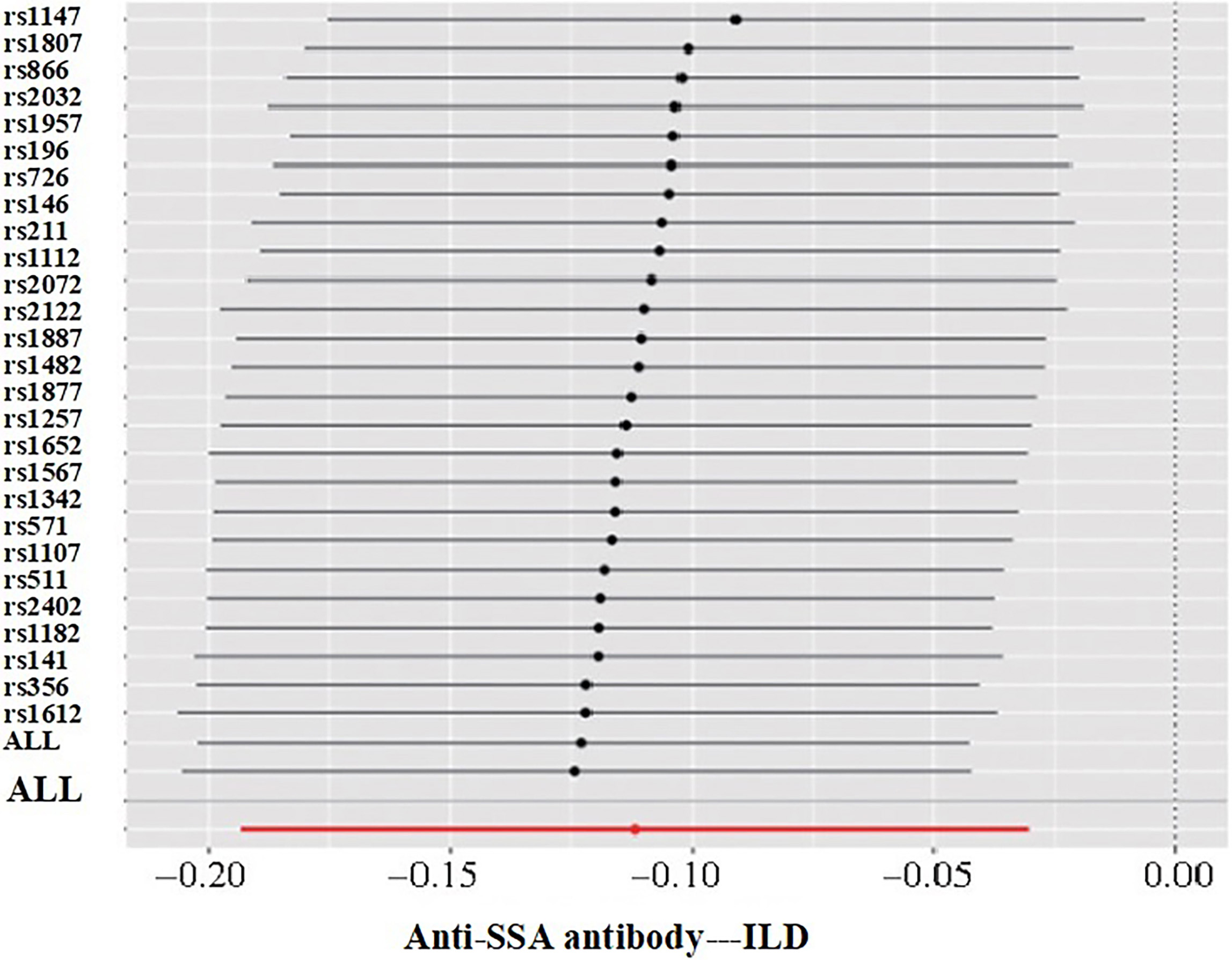
Figure 7.
ESR – ILD.
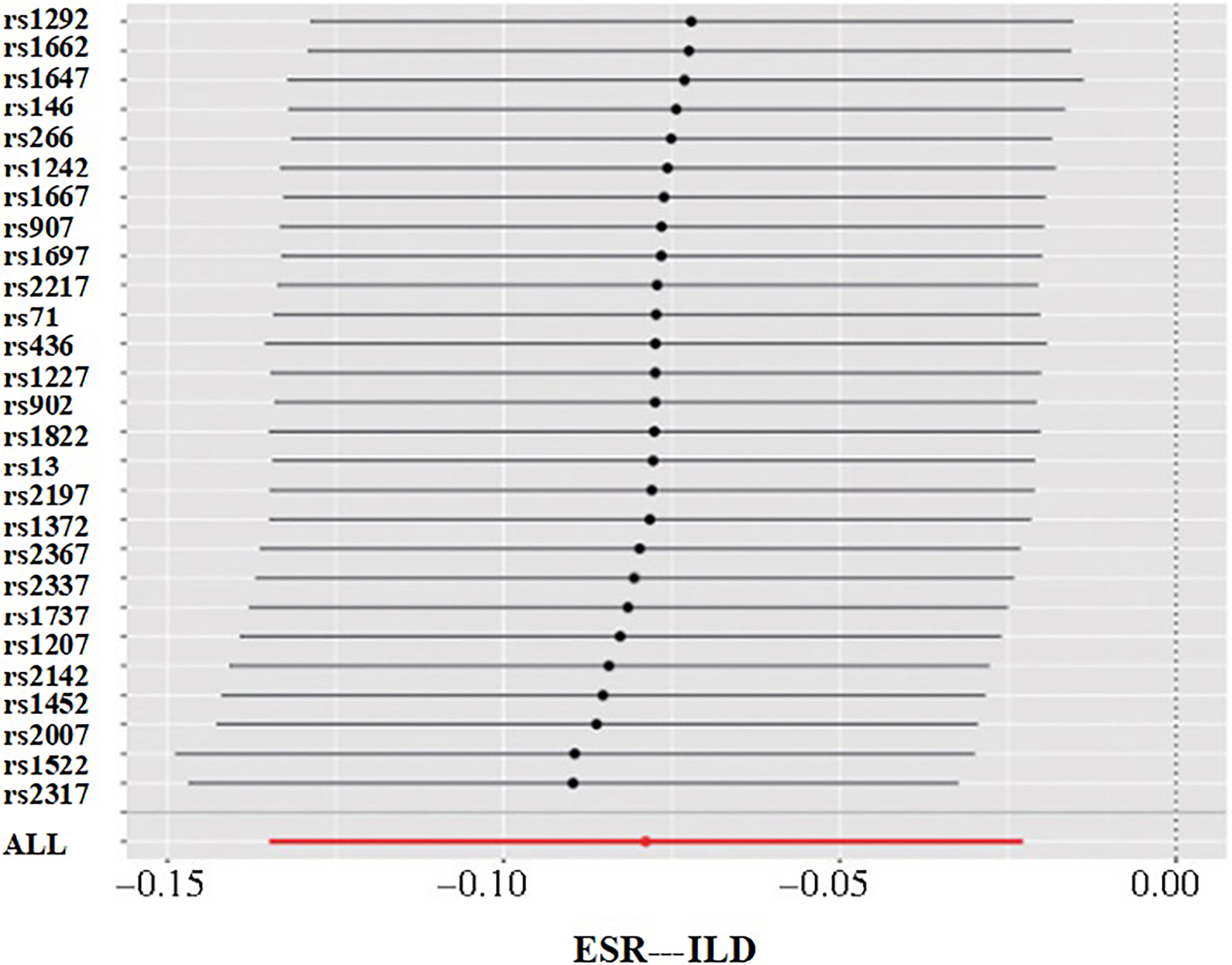
Figure 8.
CRP – ILD.
3.3.2Gene pleiotropy testing
MR-Egger regression analysis indicated an intercept of 0.011 (
3.3.3Sensitivity analysis
The sensitivity analysis of causal effects was performed using the leave-one-out method, with
4.Discussion
In this study, the causal relationship between serum metabolites and ILD was explored through Mendelian randomization analysis using pooled data from large-scale GWAS, with IVW as the main method and WME and MR-Egger regression as auxiliary methods. The findings indicated a correlation between serum metabolites and ILD. The study revealed a positive correlation between anti-Jo-1 antibody positivity, anti-SSA antibody positivity, elevated ESR, elevated CRP, and ILD. Meanwhile, the causal relationship between the serum metabolites and ILD was also investigated from a genetic perspective, suggesting that these serum metabolites may be risk factors for ILD.
Anti-SSA antibodies, previously neglected, have been shown in previous studies to be involved in transcriptional regulation, which exhibit pathogenicity without specificity and can be found in many connective tissue diseases [6]. Previous studies have suggested that immune complexes can induce endogenous interferon in patients with anti-SSA antibody-positive ILD [7, 8], activate macrophage activity, release the related chemokine CXCL10, and recruit inflammatory factors, leading to lung injury and causing pulmonary interstitial lesions [9, 10]. However, this is not supported by clinical research. A study in Norway indicated that anti-SSA antibodies could serve as a predictor of ILD [11], while another study showed that anti-SSA antibodies are associated with dermatomyositis-associated pulmonary fibrosis and disease severity [12]. The findings of this study indicated an elevated risk of ILD in patients with positive anti-SSA antibodies, with statistically significant differences, suggesting that anti-SSA antibody positivity was a risk factor for IIM-ILD.
The anti-Jo-1 antibody is an anti-aminoacyl-tRNA synthetase antibody, often associated with the occurrence of ILD, and studies have indicated an incidence of up to 73% for ILD in patients with anti-Jo-1 antibody-positive idiopathic inflammatory myopathy (IIM) [13]. Specifically, anti-Jo-1 antibody positivity can lead to ILD in IIM patients, possibly due to the formation of immune complexes with lung tissue by this antibody, which can stimulate the activity of pulmonary macrophages, resulting in the release of chemokines CXCL9 and CXCL10, followed by the recruitment to other inflammatory components under the action of these chemokines, ultimately leading to lung injury. At the same time, fibroblasts are also activated, leading to diffuse pulmonary fibrosis [10, 14]. Moreover, another study concluded that since the titer of anti-Jo-1 antibodies is closely associated with the occurrence of ILD and the severity of the disease, the dynamic observation of the titer of anti-Jo-1 antibodies in serum is beneficial for predicting changes in the severity of ILD [15]. The findings of this study indicated that anti-Jo-1 antibody positivity is a risk factor for ILD.
As a commonly used laboratory indicator reflecting the degree of systemic inflammation, the diagnostic value of erythrocyte sedimentation rate (ESR) for ILD has not been fully identified due to being influenced by various factors such as age, anemia, chronic kidney disease, etc. However, it has been found that an elevated ESR is associated with lung injury rather than muscle inflammation [16, 17], possibly due to the fact that cytokine production in the ILD environment is more likely to cause an acute-phase response compared to muscle tissue. During ILD-related inflammation, monocytes and macrophages produce inflammatory cytokines, such as interleukin-1/6, interferon-gamma, and tumor necrosis factor-alpha, which in turn induce the liver to produce acute-phase proteins [18]. Meanwhile, changes in plasma protein composition increase erythrocyte aggregation, accelerating the sedimentation rates [19, 20]. Therefore, measurement of baseline ESR and its changes over time may be a cost-effective marker for reflecting disease activity and prognosis in ILD patients.
CRP (C-reactive protein) is an acute-phase reactant protein synthesized by liver cells, and Richards et al. [14] reported that in patients with IIM combined with ILD, serum CRP and interferon-gamma-induced chemokines CXCL9 and CXCL10 appear to be associated with the expression of anti-Jo-1 antibodies, which are related to IIM-ILD. Therefore, CRP is somewhat associated with IIM-ILD but lacks high specificity due to the impact of various factors. The findings of this study are statistically significant, indicating that ESR and CRP are risk factors for ILD.
This study boasts the following advantages. 1. Unlike traditional epidemiological survey research, Mendelian randomization utilizes germline genetic variation as an exposure IV to investigate the causal relationship between exposure phenotypes and outcome phenotypes, thus avoiding the interference of confounding factors such as social environment and lifestyle and achieving true random allocation without violating ethical principles; 2. public pooled data from GWAS were used to save time and research costs, which consist of individuals of European ancestry, reducing potential bias; 3. Compared to a single SNP, 23 SNPs were used as IVs in this study, increasing the proportion of interpretation for genetic variation.
However, the study also comes with some limitations. 1. The exposure and outcome studies applied in the MR analysis should not involve overlapping participants. Since it’s impossible to estimate the degree of overlap in this study, tools (e.g., F-statistics
5.Conclusion
In conclusion, Mendelian randomization was used in the study to infer the causal relationship between serum metabolites and ILD, and the findings indicated a causal relationship between the two, with anti-Jo-1 antibody positivity, anti-SSA antibody positivity, elevated ESR, and elevated CRP being the possible risk factors for ILD. Therefore, monitoring and intervention measures for these indicators shall be incorporated into strategies for the prevention, treatment, and prognosis assessment of ILD.
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of Zhuji Hospital not directly affiliated to Wenzhou Medical University. Written informed consent was obtained from all participants.
Data availability
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Funding
This study did not receive funding in any form.
Author contributions
Zhao TT and Lv T conceived the study. Zhao TT and Lv T participated in the study design, data analysis and statistics. Zhao TT and Lv T helped draft the manuscript. All authors read and approved the final manuscript.
Acknowledgments
None to report.
Conflict of interest
None of the authors has any personal, financial, commercial, or academic conflicts of interest to report.
References
[1] | Lederer DJ, Martinez FJ. Idiopathic pulmonary fibrosis. N Engl J Med. (2018) May 10; 378: (19): 1811-1823. doi: 10.1056/NEJMra1705751. PMID: 29742380. |
[2] | Yao KC, Zhang GL, Liu WJ, et al. Progress in pulmonary rehabilitation nursing for patients with interstitial lung disease. Nursing and Rehabilitation Journal. (2023) ; 22: (2): 92-95. doi: 10.3969/j.issn.1671-9875.2023.02.023. |
[3] | Podolanczuk AJ, Wong AW, Saito S, et al. Update in interstitial lung disease 2020. Am J Respir Crit Care Med. (2021) Jun 1; 203: (11): 1343-1352. doi: 10.1164/rccm.202103-0559UP. PMID: 33835899; PMCID: PMC8759209. |
[4] | Hutchinson J, Fogarty A, Hubbard R, et al. Global incidence and mortality of idiopathic pulmonary fibrosis: A systematic review. Eur Respir J. (2015) Sep; 46: (3): 795-806. doi: 10.1183/09031936.00185114. Epub 2015 May 14. PMID: 25976683. |
[5] | Holland AE, Hill CJ, Glaspole I, et al. Predictors of benefit following pulmonary rehabilitation for interstitial lung disease. Respir Med. (2012) Mar; 106: (3): 429-35. doi: 10.1016/j.rmed.2011.11.014. Epub 2011 Dec 17. PMID: 22182340. |
[6] | Robbins A, Hentzien M, Toquet S, et al. Diagnostic Utility of Separate Anti-Ro60 and Anti-Ro52/TRIM21 Antibody Detection in Autoimmune Diseases. Front Immunol. (2019) Mar 12; 10: : 444. doi: 10.3389/fimmu.2019.00444. PMID: 30915082; PMCID: PMC6423153. |
[7] | Eloranta ML, Barbasso Helmers S, Ulfgren AK, et al. A possible mechanism for endogenous activation of the type I interferon system in myositis patients with anti-Jo-1 or anti-Ro 52/anti-Ro 60 autoantibodies. Arthritis Rheum. (2007) Sep; 56: (9): 3112-24. doi: 10.1002/art.22860. PMID: 17763410. |
[8] | Ai MX, Huan WY, ZN, et al. Analysis of the characteristics of pulmonary lesions in polymyositis/dermatomyositis. Journal of China-Japan Friendship Hospital. (2008) ; 22: (1): 17-19, 27. doi: 10.3969/j.issn.1001-0025.2008.01.004. |
[9] | Long K, Danoff SK. Interstitial lung disease in polymyositis and dermatomyositis. Clin Chest Med. (2019) Sep; 40: (3): 561-572. doi: 10.1016/j.ccm.2019.05.004. PMID: 31376891. |
[10] | Ma Q, Wu Q, Zhang LM, et al. Analysis of 85 cases of dermatomyositis with pulmonary interstitial lesions. Chinese Journal of Dermatology. (2014) ; 47: (2): 131-133. doi: 10.3760/cma.j.issn.0412-4030.2014.02.016. |
[11] | Gunnarsson R, El-Hage F, Aaløkken TM, et al. Norwegian MCTD study group; Molberg Ø. Associations between anti-Ro52 antibodies and lung fibrosis in mixed connective tissue disease. Rheumatology (Oxford). (2016) Jan; 55: (1): 103-8. doi: 10.1093/rheumatology/kev300. Epub 2015 Aug 28. PMID: 26320136. |
[12] | Sabbagh S, Pinal-Fernandez I, Kishi T, et al. Childhood Myositis Heterogeneity Collaborative Study Group. Anti-Ro52 autoantibodies are associated with interstitial lung disease and more severe disease in patients with juvenile myositis. Ann Rheum Dis. (2019) Jul; 78: (7): 988-995. doi: 10.1136/annrheumdis-2018-215004. Epub 2019 Apr 24. PMID: 31018961; PMCID: PMC7570952. |
[13] | Long K, Danoff SK. Interstitial lung disease in polymyositis and dermatomyositis. Clin Chest Med. (2019) Sep; 40: (3): 561-572. doi: 10.1016/j.ccm.2019.05.004. PMID: 31376891. |
[14] | Richards TJ, Eggebeen A, Gibson K, et al. Characterization and peripheral blood biomarker assessment of anti-Jo-1 antibody-positive interstitial lung disease. Arthritis Rheum. (2009) Jul; 60: (7): 2183-92. doi: 10.1002/art.24631. PMID: 19565490; PMCID: PMC2710404. |
[15] | Nakashima R, Hosono Y, Mimori T. Clinical significance and new detection system of autoantibodies in myositis with interstitial lung disease. Lupus. (2016) Jul; 25: (8): 925-33. doi: 10.1177/0961203316651748. PMID: 27252271. |
[16] | Park JK, Gelber AC, George M, et al. Pulmonary impairment, not muscle injury, is associated with elevated ESR in the idiopathic inflammatory myopathies. Rheumatology (Oxford). (2013) Jul; 52: (7): 1336-8. doi: 10.1093/rheumatology/ket162. Epub 2013 Apr 24. PMID: 23620561; PMCID: PMC3685332. |
[17] | Sun Y, Liu Y, Yan B, et al. Interstitial lung disease in clinically amyopathic dermatomyositis (CADM) patients: A retrospective study of 41 Chinese Han patients. Rheumatol Int. (2013) May; 33: (5): 1295-302. doi: 10.1007/s00296-012-2545-7. Epub 2012 Nov 10. PMID: 23143553. |
[18] | Moshage H. Cytokines and the hepatic acute phase response. J Pathol. (1997) Mar; 181: (3): 257-66. doi: 10.1002/(SICI)1096-9896(199703)181:3<257::AID-PATH756>3.0.CO;2-U. PMID: 9155709. |
[19] | Go DJ, Lee EY, Lee EB, et al. Elevated erythrocyte sedimentation rate is predictive of interstitial lung disease and mortality in dermatomyositis: A korean retrospective cohort study. J Korean Med Sci. (2016) Mar; 31: (3): 389-96. doi: 10.3346/jkms.2016.31.3.389. Epub 2016 Feb 4. PMID: 26955239; PMCID: PMC4779863. |
[20] | Gono T, Kaneko H, Kawaguchi Y, et al. Cytokine profiles in polymyositis and dermatomyositis complicated by rapidly progressive or chronic interstitial lung disease. Rheumatology (Oxford). (2014) Dec; 53: (12): 2196-203. doi: 10.1093/rheumatology/keu258. Epub 2014 Jun 26. PMID: 24970922. |




