Experiences of using an exoskeleton by care professionals in elderly care: A descriptive qualitative study
Abstract
BACKGROUND:
Work-related musculoskeletal disorders are common among care professionals in elderly care. Exoskeletons showed effectiveness in preventing and reducing low back pain in other sectors. However, the potential of using an exoskeleton in elderly care is unclear.
OBJECTIVE:
To document the experiences of care professionals using an exoskeleton in elderly care.
METHODS:
A descriptive qualitative study with individual semi-structured interviews among professionals from two elderly care institutes, facing low back pain.
RESULTS:
Twenty-two care professionals used the exoskeleton mainly at peak loads during morning and evening care. Their experiences were described in four main themes: wearing and adjusting, movement and comfort, appearance, integration into work, and perceived effects. Those who experienced (predominantly) positive effects reported having less or even no back pain, partly due to the relief of the lower back, but also to a more conscious posture and attention to ergonomically sound movement.
CONCLUSIONS:
This study led to valuable insights into experiences of using an exoskeleton in elderly care, such as the potential of mitigating and preventing low back pain, and suggestions for further development of exoskeletons to improve their usability in the context of elderly care. The latter should be followed by studies into long-term effects.
1.Introduction
Work-related musculoskeletal disorders tend to be common among healthcare professionals, especially nursing and care staff. According to Campo et al. (cited in [1]), there is a significant association between performing transfers with patients, positioning, and moving them, working in hunched or twisted positions, high workload, and an increased risk of work-related low back pain. Specific back pain, such as a herniated disc, is also clearly associated with work-related risk factors, especially lifting, and carrying, and working in hunched or twisted postures [2].
Madinei and colleagues [3] conclude, based on a review of recent literature, that passive exoskeletons supporting the lower back are a promising ergonomic intervention to reduce the risk of developing work-related low back pain. Exoskeletons have been used in the logistics sector (e.g., moving luggage at airports, moving parcels, etc.), agriculture, industry, and construction for a longer time showing high potential (e.g., [4, 5]). The development of exoskeletons and the application of prototypes and commercially available ones is therefore introduced and piloted in healthcare as well. For example, exoskeletons to support (rotation of) the trunk [6], or lifting and transfer activities of nurses in an wating room of an operation room [7], to relieve lower back strain for surgeons and surgery nurses [8], to reduce lumbar strain during patient transfers [9], pressure on joints and muscle activity in the shoulder-arm complex [10], and fatigue and pain of arm and shoulder during operations [11] are being developed or applied. To date, most (prototypes of) exoskeletons have mainly been evaluated in a laboratory setting [6, 9, 10, 11] or on a small scale for short periods in a real-life care environment [8, 11]. Kermavnar and colleagues called for more studies in real-life environments [4].
Within Sevagram and Zuyderland, two elderly care organisations in the Netherlands, care and nursing staff frequently experiences low back pain due to the physical strain of performing (care) tasks. For this reason, they wanted to systematically explore the experiences of using an exoskeleton in elderly care. They chose the Laevo exoskeleton (Laevo), a passive back-relieving exoskeleton that had been shown to reduce the strain on the lower back by 40% when bending forward [12]. Laevo is already used in various sectors such as agriculture, construction, military and automotive [13]. Both in a laboratory setting [12, 14] and in real work environments, wearing a Laevo led to objectively increased performance in static forward bending, tasks were perceived as significantly less difficult [14] and caused less back pain [14, 15]. Although Laevo was originally developed for healthcare, it has mostly been applied in other sectors. Experiences in healthcare are limited to use in an operation room [8, 16], characterised by working in a fairly structured environment for lengthy periods of time in the same posture. Application in elderly care, where activities are different, had not been previously investigated before the start of this study.
As a result, little knowledge is available on if and how an exoskeleton is deployable in elderly care, in users’ experiences that determine acceptance or perceived added value, nor in factors that influence implementation. The research objective of this study is to document the experiences of care professionals in elderly care, facing low back pain, when using an exoskeleton during their care tasks.
2.Methods
To reach this objective, a descriptive qualitative research design was applied [17].
2.1History of the project
The 16-month project was initiated by the innovation managers of Sevagram and Zuyderland, in cooperation with the company Laevo. Zuyd University of Applied Sciences was responsible for the research. Before the start of testing, application of the exoskeleton in elderly care was explored with several employees (
2.2Exoskeleton
Figure 1.
Laevo V2.57.
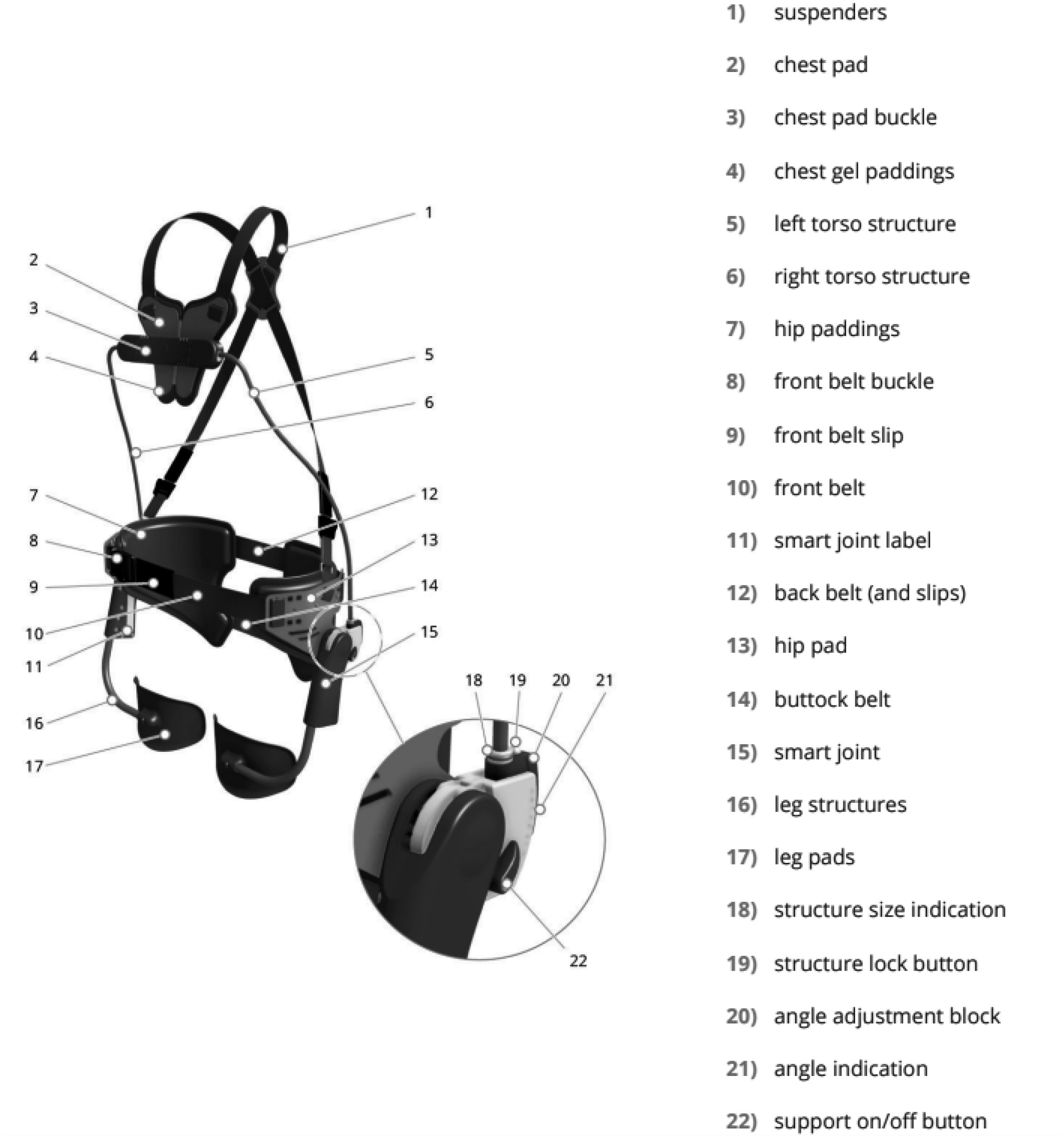
Figure 2.
Laevo FLEX.
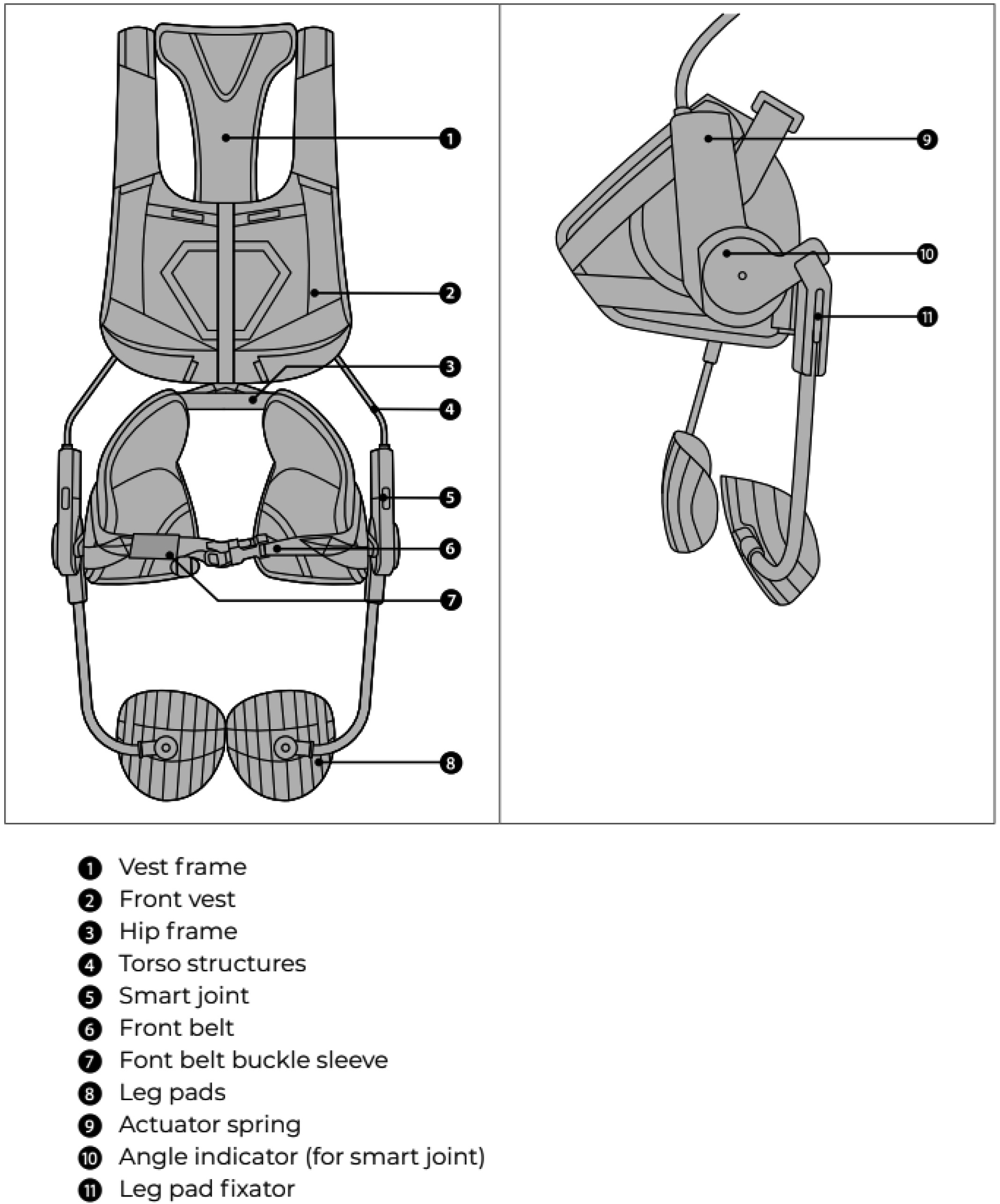
The study was started with Laevo version 2.57 (see Fig. 1). “The Laevo is a wearable device which supports bent-forward work and repetitive lifting. The Laevo decreases the forces in the lower back when bending [18].” It weighs 2.8 kg. The prototype of the next version, and the next version itself, called Laevo FLEX (see Fig. 2), were used for the following test phases. The Laevo FLEX “is a wearable device which supports the body during work in various positions, for example, when you stoop, squat, bend forward or do repetitive lifting. The FLEX decreases the strain in the lower back during these activities [19].” It weighs 4.0–4.2 kg. Main changes from version 2.57 included moving the chest structure backwards and replacing the straps for the upper body with a vest. Another difference between the FLEX and the V2.57 is the addition of the swivel between the shoulders, which reduces the pressure against the thighs when walking compared to the V2.57. The level of support is much higher. And twisted movements and bending are also possible through the swivel while maintaining comfort. Furthermore, the FLEX is dust- and waterproof. In further development, the vests of the prototype of Laevo FLEX were minimised and better adapted to the anatomy of a female body. During the test period, there were three sizes of the vests.
2.3Participants
To be eligible to participate in the study, professionals from Sevagram or Zuyderland had to meet the following inclusion criteria: 1) nurses aid, nursing assistant or nurse; 2) does morning and evening bedside care; 3) contract of at least 24 hours per week; and 4) chronic low back pain (longer than 3 months).
Exclusion criteria included: 1) red flags (identified using a screening tool based on the Royal Dutch Society for Physiotherapy’s guideline on low back pain) [20]; 2) a lumbosacral radicular syndrome (LRS) [20]; and 3) too much pressure on the chest or upper legs or other complaints at the first session with the exoskeleton despite careful fitting and adjustment. Participants were recruited through social media posts and internal communication channels and team managers. Furthermore, employees with low back problems were actively approached on site.
2.4Procedure
Potential participants were invited to an initial session; prior to this, they received a comprehensive information letter including a consent form and provided informed consent. When determining the duration of testing, it was assumed that it generally takes about four weeks to get used to wearing and using the exoskeleton. Participants were reminded that they could stop at any time in case of complaints. For the first test phase, it was envisaged that each participant would use the exoskeleton for eight weeks. With the time needed to get used to the exoskeleton in mind, follow-up measurements ideally would take place after four and eight weeks of use. As it gradually turned out that participants often stopped using the exoskeleton earlier, these times were not feasible for follow-up measurements, and times were determined individually for each participant.
During the first session, after fitting of the exoskeleton, each participant was observed by an occupational and/or physiotherapist while performing relevant activities related to stature, posture, and movement patterns; first without and then with use of the exoskeleton to observe possible differences arising from wearing the exoskeleton. Participants were also observed in the first days of use by the physiotherapists involved, so that possible complaints or problems due to (incorrect) use of the exoskeleton could be noticed in time and the settings of the exoskeleton could be adjusted. Furthermore, during the test period participants’ working activities were scheduled in a way that frequent use of the exoskeleton and variation of experiences were possible.
2.5Data collection and analysis
After fitting the exoskeleton and after a period of use, participants individually participated in a semi-structured interview. The interview guide was informed by the Dutch version of the Quebec User Evaluation of Satisfaction with assistive Technology (D-QUEST) [21] and the Theoretical Framework including the Technology Acceptance Model (TAM) as described by [22, p. 276]. It starts with questions about socio-demographic and background variables, followed by open questions on topics as factual use of the exoskeleton, experiences (perceived effect; influences from the physical and social environment, e.g. reactions from colleagues, residents and their relatives) and opinions about characteristics of the exoskeleton, future use, suggestions for improvement and implementation in the organisation. Face validity, structure and comprehensibility were considered with one occupational therapist from Zuyd University of Applied Sciences and two physiotherapists from Sevagram and Zuyderland. This interview had an estimated duration of 30 minutes and took place during working hours, at the location where the participant worked. Currently applicable measures related to COVID-19 were taken into account. If a participant preferred a telephone interview or an online consultation, this was arranged. With the consent of the participants, the interview was recorded. The audio recording was summarised in writing and then deleted. The summary was sent to the participant for review (member-check). Participants had one week to add, change, or delete information if they wished. Without a response, it was assumed that they agreed with the content of the summary, and it was used for data analysis. The interview data obtained in this way were analysed inductively using conventional content analysis [23] and the results are described by themes in the following section.
3.Results
Table 1
Participants
| Participant and test phase | Role within organisation | Age (years) | Gender | Low backpain | Tested earlier version Laevo | Duration of use | Experiences |
|---|---|---|---|---|---|---|---|
| Participant 1 Phase 1 | Nursing assistant Z | 54 | Female | Yes | Not applicable | 1 h for testing, 2 | PE: positive FU: yes |
| Phase 2 | Laevo 2.57 | 1 h LS, 3 h ES, 2 h ES | PE: positive FU: yes | ||||
| Phase 3 | Prototype FLEX | 8 | PE: new version did not fit FU: no | ||||
| Participant 2 Phase 1 | Nursing assistant S | 60 | Female | Yes | Not applicable | 1 | PE: negative FU: no |
| Participant 3 Phase 2 | Nursing assistant Z | 24 | Male | No | No | 2 h LS, 8 h LS, 4 h ES, during care ES | PE: ambivalent FU: not preventive |
| Participant 4 Phase 2 | Nursing assistant S | 58 | Female | Yes, always after ES | No | 2 | PE: positive FU: yes |
| Phase 3 | No more pain after using FLEX | Prototype FLEX | Every shift 3 h, about 6 weeks | PE: positive FU: no longer needed | |||
| Participant 5 Phase 2 | Nursing assistant S | 33 | Female | Yes | No | 2 | PE: hindering FU: longer period of testing needed |
| Participant 6 Phase 3 | Nursing assistant Z | 52 | Female | Yes | 4 | PE: negative FU: during study | |
| Participant 7 Phase 3 | Nurses aid S | 60 | Female | Yes | No | 4 | PE: negative FU: no |
| Participant 8 Phase 3 | Nursing assistant S | 62 | Female | Yes | No | 5 | PE: positive FU: yes, if less obtrusive |
| Participant 9 Phase 3 | Nurses aid S | 61 | Female | Some time ago; knee arthrosis | No | 1 | PE: positive (back), negative (knees) FU: no |
| Participant 10 Phase 4 | Nursing assistant S | 60 | Female | Yes | No | 14 | PE: positive FU: no, too obtrusive |
|
Table 1, continued | |||||||
|---|---|---|---|---|---|---|---|
| Participant and test phase | Role within organisation | Age (years) | Gender | Low backpain | Tested earlier version Laevo | Duration of use | Experiences |
| Participant 11 Phase 4 | Nursing assistant S | 33 | Female | No | No | during 2 weeks ES | PE: positive FU: other exoskeleton or improved |
| Participant 12 Phase 4 | Nurses aid S | 37 | Male | Yes | No | 2 | PE: ambivalent; need to get used to FU: perhaps in the future |
| Participant 13 Phase 4 | Nursing assistant S | 37 | Female | Yes | No | 2 h during ES for 6 weeks | PE: difficult to fit; ambivalent FU: no |
| Participant 14 Phase 4 | Nurse S | 38 | Female | Yes | No | 5–10 | PE: positive FU: yes |
| Participant 15 Phase 4 | Nurse S | 24 | Female | Yes | No | 2–3 h during care for 2 weeks | PE: positive FU: yes, if improved |
| Participant 16 Phase 4 | Nurse S | 22 | Female | Yes | No | 4 | PE: positive FU: with heavy care tasks |
| Participant 17 Phase 4 | Nursing assistant S | 58 | Female | yes, in combination with hip pain | No | 6 | PE: positive FU: yes |
| Participant 18 Phase 4 | Nursing assistant S | 22 | Female | Yes | No | 6–9 | PE: positive FU: yes, if improved |
| Participant 19 Phase 4 | Nurse S | ? | Male | Yes | No | 4 | PE: positive FU: yes |
| Participant 20 Phase 4 | Nursing assistant S | 48 | Female | yes, in combination with hip pain | No | 4–5 | PE: positive FU: yes, if needed, not preventive |
| Participant 21 Phase 4 | Nurses aid S | 31 | Female | Yes | No | 3 | PE: positive FU: yes |
| Participant 22 Phase 4 | Nursing assistant S | 37 | Female | Yes | No | during 1 week | PE: negative, increased pain FU: no |
Legend: S
During the period from October 2020 to December 2022, in total, 22 care professionals participated in the interviews about their experiences of using the Laevo exoskeleton in practice (Sevagram
3.1Wearing and adjusting
Putting on and taking off the exoskeleton independently was felt to be (reasonably) easy. Some participants still needed help the first time putting it on, but after that everyone could do it on their own. With the first version of the exoskeleton (V2.57), it was difficult to adjust and set the exoskeleton properly for the individual user. Setting up with all versions of the exoskeleton was done by an occupational or physiotherapist; this initially took about an hour for most participants, including providing instruction. In subsequent tests with (the prototype of) Laevo FLEX, most participants reported that the exoskeleton was well adjusted to them, and that it was not difficult or took a long time to find the right adjustment.
However, a few participants indicated that the right setting was not found for them, even after multiple adjustments. They said this was due to physique. For most participants, after proper adjustment (especially Laevo FLEX), the exoskeleton remained in place during all activities. For one participant, the upper part shifted while squatting; the Velcro became loose and had to be readjusted properly several times a day. The leg pads also did not stay in place properly for some participants; they slipped when walking and caused slight bruising. Sometimes Velcro was attached at the legs so that the leg pads did not keep slipping off.
3.2Movement and comfort
Participants told that wearing an exoskeleton requires adaptation of movement. The occupational and physiotherapists involved observed that using the exoskeleton changed the movement chain and that some participants tried to push through their normal movements. Bending, kneeling, squatting, and going through the knees went well for some participants; others felt hampered or felt very much that they had to do these movements in a different way than they were used to. For example, one participant had to hold onto something to get upright. The duration of getting used to it among participants varied greatly. Some got used to it quickly; for others, use had to be built up slowly because they found carrying the exoskeleton heavy.
Comfort during movement has a major influence on a positive or negative experience with the exoskeleton. Some of the participants formulated wearing an exoskeleton as not uncomfortable. Not being able to sit comfortably (with exoskeleton) in a chair anymore, for example, to write reports at the computer or help residents at the table to eat is the most frequently mentioned disadvantage. Several participants experienced the exoskeleton as warm, despite the breathable fabric with holes; the exoskeleton caused increased perspiration. Some participants described the exoskeleton as too cumbersome.
Participants reported having to be careful not to get stuck or bump into anything; they experienced difficulty manoeuvring in small spaces such as the wet room. Others found the exoskeleton uncomfortable due to straps that were too stiff or unpleasant pressure from Velcro on the hips or forearms rubbing against “screws” (the smart joint) on the sides. The upper section (from (prototype) Laevo FLEX) was perceived as too tight by some participants. Adjustments to the exoskeleton to improve wearing comfort sometimes caused other challenges. Moving the chest structures backwards from (the prototype of) Laevo FLEX improved wearing comfort but did not allow participants to wear a nursing jacket over it, so they missed the functionality of the pouches (storing duty phone, gloves, bandage scissors, pen, or keys).
3.3Appearance
Most participants were satisfied with the appearance of the exoskeleton or thought the appearance was secondary to the result:
• “I really have to admit it looks crazy. It’s not pretty or anything. A penicillin drink is not nice either but that helps too.” (P4 phase 3)
• “Yes, that’s a thing. It’s not pretty, of course, but that doesn’t count for much for me.” (P4 phase 3)
For others, appearance was the main reason to stop using it. “I became dead unhappy with this.” (P7)
Residents often initially expressed funny or surprised reactions to wearing the exoskeleton. It often opened the conversation. Common statements included:
• “What are you wearing now?” (P1 phase 1 & 2; P2; P7; P16; P18; P21)
• “What is this, what do you have to do with it and why?” (P13)
• “Are you going to space, you look like a robot?” (P10)
• “Nurse, are you going to abseil (P17)/parachute jump (P8)?”
The type of response was mainly related to the target group one works with. In people with severe dementia, the reaction often kept recurring repeatedly and explanations were felt of little use. Two residents accidentally grabbed the exoskeleton. Once because the resident thought she was grasping the bar of the passive hoist. This did not lead to dangerous situations but is an area of concern. Comments from colleagues were mostly interested questions. However, some participants experienced sceptical reactions from colleagues and found them so annoying that they wore the exoskeleton less often or even stopped wearing it.
3.4Integration into work
Participants used the exoskeleton mainly during morning and evening shifts, especially when caring for (bedridden) clients on the bed, dressing and undressing (especially compression stockings), washing, showering, and lifting clients out of bed, making transfers, assisting with toileting, and pushing the medicine trolley. In contrast, night shifts are based on calls from residents who need help, this is often occasional care. Interviewees indicated that wearing the exoskeleton is not convenient then, because they cannot walk (well) or sit down in between with the exoskeleton on (e.g., when doing administrative work such as reporting the computer). It takes too much time and effort to put it on and off all the time. Using the exoskeleton for emergencies in other departments is not an option, as you cannot run with it.
For participants who experienced a positive impact, the exoskeleton fitted well into normal working practices, regular tasks, and activities. Some found the exoskeleton more suitable for morning rather than evening care, as they must walk more in the evening. Incidentally, participants who evaluated the latest version of the exoskeleton were less bothered when wearing it. All participants are convinced that the exoskeleton is especially useful when doing rounds. This involves caring for residents for several hours in succession where heavy, physical tasks are performed continuously. Participants who did not experience a positive effect also found the exoskeleton difficult to fit into these activities. Part of fitting into work is whether to share an exoskeleton with colleagues. Sharing was not considered desirable by many participants, as the settings would have to be readjusted each time.
3.5Perceived effect of the exoskeleton
Those participants, who experienced a clear positive effect, expressed this for example by saying:
• “…a fantastic thing!” (P4 phase 2 & 3); “I’m glad I did this!” (P4 phase 3).
For others, the effect was ambivalent or negative, with some wanting to continue using it and others not. The main positive effects indicated were that it corrects posture and, above all, creates awareness of body posture while performing care tasks.
• “It signalled, not this posture, a bit straighter.” (P1 phase 1).
One participant explained that the spring of the exoskeleton straightens the back in a way and forces it into the correct posture. Several participants indicated that after a while they actually adopted that straight posture without the exoskeleton too. People know it is important, but it often slips through due to a developed routine or due to the speed of task performance.
Participants reported experiencing less back fatigue. They could bend better and found it less tiring to work in a stooped position. Some had no more back pain at all:
• “Oh, wonderful yes, no more complaints at all…” (P10).
• “I miss it when I don’t have it on. Even though it’s heavy to lift when putting it on. Now that I no longer have it, I have back problems again.” (P14).
Tasks were performed differently by wearing the exoskeleton, which was perceived as positive. For some participants, this led to adjustments in their actions and the use of proper lifting techniques, e.g., putting a bed at the right height or standing straight in front of something so that there was less twisted bending or stooping. Participants indicated that they were adopting a better posture by, for example, lowering their knees more and turning more purposefully. Several participants experienced the use of the exoskeleton as pleasant. Especially when working with bending, stretching, pushing, making transfers, and putting people on the bed, the exoskeleton provided relief. “The support the skeleton gives you, specifically that you keep a straight back, is super nice.” (P15).
Besides the positive effects, several participants reported experiencing no or negative effects of the exoskeleton (on back pain). For example, some participants felt no support. Certain movements were more difficult for them, for example, bending forward, going through the knees, standing at the bedside (because participants could then not put their upper legs against the bed) or taking a step to the side: “…then you feel it, that you have something stuck to you, then you get a bit off balance.” (P5).
According to these participants, the exoskeleton inhibits movements and wearing the exoskeleton forced them into an upright posture that their bodies were not used to. The different posture puts more strain on other muscles than usual, causing upper back complaints and making participants feel the wearing as tiring.
3.6Recommendations for improvement of the exoskeleton
Participants mentioned nine suggestions for improvement: 1) Lighter, finer, smaller, more flexible, more comfortable and of elastic material, more compact and inconspicuous (P1 phase 1 & 2; P2; P4 phase 2; P6; P8; P10; P11; P12; P18; P19; P22); 2) Possibility to wear under clothes (P4 phase 2 & 3; P8; P9); 3) Longer top piece so it can be closed more easily (P5); 4) Different material (in summer) (P1 phase 2; P3; P4 phase 2; P6; P13; P22); 5) Own top piece for each user (for hygiene reasons) that is easy to clean (P1 phase 2; P4 phase 2); 6) A larger pocket or more pockets to store necessary items (P3; P4 phase 2; P5; P15–22); 7) Possibility to hang up the exoskeleton (P1 phase 2); 8) No leg pads or pads of different size, or different material (P1 phase 3; P2; P4 phase 2 & 3; P12; P18; P21; P22); and 9) Protection over the “screws” (smart joint) on the side (P5).
3.7Recommendations for implementation of an exoskeleton in elderly care
Participants and involved occupational and physiotherapists provided six suggestions for implementation: 1) Give more attention to the use of an exoskeleton through location-based promotion or a personal approach; 2) Link with occupational health and safety services and include the exoskeleton as a potentially interesting and possibly effective addition to the existing range of aids for preventing and reducing (back) pain, such as lifts and transfer boards; 3) Understanding the factors that determine whether the exoskeleton is or is not suitable for the individual user (to be able to make a good match); these could include: a) the nature of the experienced back pain (e.g. wearing the exoskeleton was experienced very differently by a participant with scoliosis than by a participant with osteoarthritis); b) determining the appropriate wearing time; c) possible other complaints (e.g., knee problems) and side effects (such as on abdominal muscles) that need to be monitored; d) factors in the social and physical environment (e.g., views and expressions of colleagues and residents, possibilities for safe storage of the exoskeleton or sufficient space so that wearing the exoskeleton is not perceived as an obstacle); 4) Importance of careful fitting, explanation, instruction, training, and proper guidance; having a person available and approachable to whom users can turn in case of questions or problems; 5) Integration of use in training and education on ergonomic behaviour; and 6) Support of managers and care coordinators in implementation.
4.Discussion
The objective of the study was fully achieved. Thirteen participants were (very) enthusiastic, four ambivalent and five participants were (very) negative about wearing the exoskeleton. Appearance, comfort, influence on movement, fitting in with regular activities and perceived effect were key to the acceptance and perceived usefulness of an exoskeleton in elderly care.
Those who were (very) enthusiastic perceived the purposeful use of the Laevo FLEX during peak workloads during morning and evening care and caring for clients (at bedside) as positive. They said to have fewer back problems as a result of using the exoskeleton, with some even indicating that their complaints have disappeared altogether. According to them, this was partly due to the relief of the lower back that the exoskeleton provided during stooped postures and activities such as lifting, carrying, and moving, but also as a result of more conscious posture and paying attention to ergonomically sound movement. Occupational and physiotherapists’ observations showed that several care professionals did not move ergonomically according to lifting and transfer protocols and tried to continue this even when wearing the exoskeleton. On the contrary, other participants indicated that, by wearing the exoskeleton, they had become much more aware of an ergonomically responsible posture and now apply it much more consistently. In their view, this was also the reason they experienced less or even no back pain because of exoskeleton use. Those who were very enthusiastic wore the exoskeleton for a longer period and would also recommend it to colleagues (with low back pain). Others stopped using it after a few shifts, because the exoskeleton did not fit well, could not be adjusted, or did not fit well with their regular work. Overall, the findings of this study indicate that the implementation of an exoskeleton can be promising for care professionals in elderly care to mitigate and prevent low back pain. The results from the first project phases have contributed to the further development of Laevo version 2.57 into Laevo FLEX to make it more suitable for use in healthcare settings.
4.1What this study adds to the literature about the use of an exoskeleton in elderly care
This research is the most comprehensive study on the deployment of a commercially available exoskeleton to support the lower back in a real-life care context to date. The findings from this study are consistent with the results of the only other study conducted in a similar real-life setting: a Finnish study concerning the deployment of Laevo in a nursing home [24]. Sixteen nursing students first evaluated the exoskeleton in an experimental set-up while performing a transfer. Half of these students intended to continue using the exoskeleton for this task. Subsequently, seven nurses used the exoskeleton briefly in elderly care. Main findings of this study comprise that the residents’ reactions ranged from rather negative about the appearance to “compassion toward the nurses who ‘had to’ use” it [24]. Also, colleagues’ opinions about the exoskeleton were diverse, but participants stressed that its positive effects motivated them to wear it [24]. Compared to this study, the current study provides even more insight into specific use cases, their experiences, and perceived effects of using the exoskeleton for healthcare workers with chronic low back pain, its use over a longer period, and factors determining the acceptance and added value of using an exoskeleton in elderly care. Settembre and colleagues assessed the Laevo exoskeleton in an intensive care unit (ICU) of a university hospital in France during the COVID-19 pandemic [25]. Perceived fatigue at the end of the shift was reduced and both participants would use Laevo again without hesitation. They found Laevo comfortable except while walking and did not feel restricted in usual gestures and activities in the ICU. As in the present study, it was found that a positive attitude of colleagues is fundamental for the acceptance of such innovative technology at work [25].
For the further implementation of the exoskeleton within elderly care, new insights from Elprama and colleagues [26] could be incorporated. It seems useful to embed the deployment in the institution’s occupational health and safety policy and to further develop the process for advising an exoskeleton for the individual worker. The importance of conveying more knowledge about the potential benefits of wearing an exoskeleton during certain tasks and activities and a more proactive safety policy was also highlighted, which is less evident in the healthcare sector where workers often work solo in a resident’s home, than, for example, in construction or logistics. According to one of the involved physiotherapists the awareness of “we either work safely or we don’t work at all” and the use of personal protection is still much less present in the care sector than in other sectors, which might render the preventive use of an exoskeleton difficult.
4.2Strengths and limitations of the study
The following aspects can be mentioned as strengths of this study. The iterative phases of our project allowed initial suggestions for improvement to be included in the further development of the exoskeleton; several participants had the opportunity to evaluate different versions of Laevo for direct comparison. In doing so, the study contributes to O’Connor’s claim to involve caregivers and nurses more in the development of exoskeletons to ease increasingly demanding care tasks [27]. Different forms of triangulation were applied: data triangulation, as the research data were collected at several points in time and in different locations of two different health care organisations, and researcher triangulation, as the data were collected and analysed by three researchers. This and the collection of data over a longer period (‘prolonged engagement’) and asking for feedback from the participants in a member check increased the credibility of the research findings [28]. The fact that the results are in line with the results of previous research with Laevo conducted in similar settings [24, 25], combined with the detailed description of the context (‘thick description’), increases the likelihood that the results of this study are also applicable to other care organisations (‘transferability’) [28]. The study proceeded in several phases and data were collected and analysed iteratively. Eventually, saturation was achieved for the qualitative data collected using interviews, which increased the robustness (‘dependability’) of the study [28]. The progress of the project and results were regularly fed back and discussed with the highly engaged members of the project team in which the various stakeholders were represented (‘peer debriefing’), which benefited the ‘confirmability’ of the study [28].
Our study had some limitations. For instance, it was difficult to recruit enough participants within both healthcare organisations, which ultimately led to a slightly smaller number of participants than originally conceived. Moreover, the way participants were recruited might have led to selection bias, as healthcare professionals were initially included with an interest in innovative technology and participation in research. This could perhaps have been avoided by running the inclusion through the Occupational Health and Safety Service and in this way approaching everyone who might be eligible to use the exoskeleton due to chronic low back pain for participation. Furthermore, the fact that the study took partly place during the COVID-19 pandemic affected the conduct and quality of the study. Caregivers and nurses were extremely heavily burdened during this period, which generally left little room to engage in innovations. Moreover, participating in a study (even though it could be done during working hours) was perceived as an extra burden. For some participants, the high workload resulted in little time for the interviews, which sometimes had to take place by telephone due to the COVID-19 measures in force.
5.Conclusion
Overall, this study led to valuable insights into experiences of 22 care professionals, such as the potential of mitigating and preventing low back pain, and suggestions for further development of exoskeletons to improve their usability in the context of elderly care. The latter should be followed by studies into long-term effects. In a follow-up project, it would be interesting to find out the effectiveness of the Laevo FLEX exoskeleton in relation to productivity, sustainable employability, absenteeism, and reintegration, and to explore the use of sensors to measure its effects.
The project was financially supported by a KIEM 2020 grant from the Taskforce for Applied Research SIA, grant number KIEM.K20.01.028 (project phase 1 and 2) and by a specific funding from the Dutch Ministry of Health, Welfare and Sport (project phase 3).
Author contributions
CONCEPTION: UR, ML, RD.
PERFORMANCE OF WORK: UR, ML, RD.
INTERPRETATION OR ANALYSIS OF DATA: UR, ML.
PREPARATION OF THE MANUSCRIPT: UR, ML, RD.
REVISION FOR IMPORTANT INTELLECTUAL CONTENT: FR, RD.
SUPERVISION: RD.
Ethical considerations
The research protocol was approved by an accredited Medical Research Ethics Committee (Medisch Ethische Toetsingscommissie Zuyderland - Zuyd, METC Z; number METCZ20200037).
Acknowledgments
The authors would like to thank all participating care professionals at Sevagram and Zuyderland as well as Charlotte Gijzen, Lisanne Dierx, Melissa Botana Gronek, Dewi Korff, Patrick Zaat, Elko Windmeijer, and Nadine Spierts for their valuable contribution.
Conflict of interest
The different versions of the Laevo exoskeleton used in this study were provided by Laevo. The authors have no conflicts of interest to report.
References
[1] | Harwood KJ, Darragh AR, Campo M, Rockefeller K, Scalzitti DA. A systematic review of safe patient handling and mobility programs to prevent musculoskeletal injuries in occupational and physical therapists and assistants. Int J Safe Patient Handl Mob. (2018) ; 8: (1): 46. |
[2] | Kuijer PPFM, Verbeek JH, Seidler A, Ellegast R, Hulshof CTJ, Frings-Dresen MHW, Van der Molen HF. Work-relatedness of lumbosacral radiculopathy syndrome. Review and dose-response meta-analysis. Neurology. (2018) ; 91: : 558. doi: 10.1212/01.wnl.0000544322.26939.09. |
[3] | Madinei S, Kim S, Srinivasan D, Nussbaum MA. Effects of back-support exoskeleton use on trunk neuromuscular control during repetitive lifting: A dynamical systems analysis. J Biomech. (2021) ; 123. doi: 10.1016/j.jbiomech.2021.110501. |
[4] | Kermavnar T, de Vries AW, de Looze MP, O’Sullivan LW. Effects of industrial back-support exoskeletons on body loading and user experience: an updated systematic review. Ergonomics. (2021) ; 64: (6): 685. doi: 10.1080/00140139.2020.1870162. |
[5] | Ten Katen L, Lindeman F, Feddema A. Praktijkervaring met exoskeletten. [Practical experiences with exoskeletons]. Tijdschrift voor Human Factors. (2019) ; 44: (1): 24. |
[6] | Kuber PM, Rashedi E. Towards Reducing Risk of Injury in Nursing: Design and Analysis of a New Passive Exoskeleton for Torso Twist Assist. Proceedings of the 2021 International Symposium on Human Factors and Ergonomics in Health Care. doi: 10.1177/2327857921101141. |
[7] | Cha JS, Monfared S, Stefanidis D, Nussbaum MA, Yu D. Supporting surgical teams: Identifying needs and barriers for exoskeleton implementation in the operating room. Hum Factors. (2020) ; 62: (3): 377. doi: 10.1177/0018720819879271. |
[8] | Hartgers R. Met een exoskelet aan je werk doen. [Getting to work with an exoskeleton.] Skipr. (2018) ; 11: : 34. doi: 10.1007/s12654-018-0193-6. |
[9] | Miura K, Kadone H, Abe T, Koda M, Funayama T, Noguchi H, Kumagai H, Nagashima K, Mataki K, Shibao Y, Sato K, Kawamoto H, Sankai Y, Yamazaki M. Successful use of the hybrid assistive limb for care support to reduce lumbar load in a simulated patient transfer. Asian Spine J. (2021) ; 15: (1): 40. doi: 10.31616/asj.2019.0111. |
[10] | Tröster M, Wagner D, Müller-Graf F, Maufroy C, Schneider U, Bauernhansl T. Biomechanical model-based development of an active occupational upper-limb exoskeleton to support healthcare workers in the surgery waiting room. Int J Environ Res Public Health. (2020) ; 17: : 5140. |
[11] | Liu S, Hemming D, Luo RB, Reynolds J, Delong JC, Sandler BJ, Jacobsen GR, Horgan S. Solving the surgeon ergonomic crisis with surgical exosuit. Surg Endosc. (2018) ; 32236: . |
[12] | Knitel K, van Eck J, Bosch T, de Looze M. Innovatieve rugondersteuning. De effecten van een passief exoskelet op spieractiviteit en volhoudtijd. [Innovative back support. The effects of a passive exoskeleton on muscle activity and perseverance.] Tijdschrift voor Human Factors. (2015) ; 40: (1): 4. |
[13] | Laevo [homepage on the Internet]. Laevo V2. Rijswijk: Laevo; [cited 27 Apr 20]. Available from: https://laevo-exoskeletons.com/home. |
[14] | Baltrusch SJ, van Dieën JH, van Bennekom CAM, Houdijk H. The effect of a passive trunk exoskeleton on functional performance in healthy individuals. Appl Ergon. (2018) ; 72: : 94. doi: 10.1016/j.apergo.2018.04.007. |
[15] | Hensel R, Keil M. Subjective evaluation of a passive industrial exoskeleton for lower-back support: A field study in the automotive sector, IISE transactions on occupational ergonomics and human factors. (2019) ; 7: (3): 213-221. doi: 10.1080/24725838.2019.1573770. |
[16] | Kolfschoten JJ. We’ve got your back. De functionele toepasbaarheid van de Laevo V2.5 voor Chirurgen en OK-assistenten. [We’ve got your back. the functional applicability of Laevo V2.5 for surgeons and OR-assistants.] Bachelor scriptie Bewegingstechnologie [Bachelor thesis Movement Technology]. Den Haag: De Haagse Hogeschool, University of Applied Sciences. 2018. |
[17] | Polit DF, Beck CT. Nursing Research: Generating and Assessing Evidence for Nursing Practice 11th ed. Philadelphia: Wolters Kluwer; (2021) . |
[18] | Laevo [homepage on the Internet]. User manual Laevo 257. Rijswijk: Laevo; [cited 28 June 24]. Available from: https://static1.squarespace.com/static/5f7d9bb22f1bc82b03f6f1b0/t/5f995ebd9b16be70ef97bb49/1603886792050/V2.57+User+manual.pdf. |
[19] | Laevo [homepage on the Internet]. User manual Laevo FLEX. Rijswijk: Laevo; [cited 28 June 24]. Available from: https://static1.squarespace.com/static/5f7d9bb22f1bc82b03f6f1b0/t/62d529f36b7eb93cfe01cdd9/1658137085643/Laevo+Flex+V3.0+-+User+Manual_v00_08_EN.pdf. |
[20] | KGNF [homepage on the Internet]. Richtlijn lage rugpijn en LRS 2021. [Royal Dutch Society of Physiotherapy. Guideline low back pain and lumbosacral radicular syndrome.] Amersfoort: KNGF; [cited 20 Nov 23]. Available from: https://www.kngf.nl/binaries/content/assets/kennisplatform/onbeveiligd/richtlijnen/lage-rugpijn-en-lrs-2021/kngf_richtlijn_lage_rugpijn_en_lrs_2021_samenvatting.pdf. |
[21] | Wessels RD, de Witte LP. Reliability and validity of the Dutch version of QUEST 2.0 with users of various types of assistive devices. Disabil Rehabil. (2003) ; 25: (6): 267-272. |
[22] | Venkatesh V, Bala H. Technology acceptance model 3 and a research agenda on interventions. Decisc Sci. (2008) ; 39: (2): 273-315. |
[23] | Hsieh H, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. (2005) ; 15: (9): 1277. |
[24] | Turja T, Saurio R, Katila J, Hennala L, Pekkarinen S, Melkas H. 2020. Intention to use exoskeletons in geriatric care work: Need for ergonomic and social design. Ergon Des. (2022) ; 30: (2): 13. doi: 10.1177/1064804620961577. |
[25] | Settembre N, Maurice P, Paysant J, Theurel J, Claudon L, Kimmoun A, Levy B, Hani H, Chenuel B, Ivaldi S. The use of exoskeletons to help with prone positioning in the intensive care unit during COVID-19. Ann Phys Rehabil Med. (2020) ; 63: : 379. |
[26] | Elprama SA, Vanderborght B, Jacobs A. An industrial exoskeleton user acceptance framework based on a literature review of empirical studies. Appl Ergon. (2022) ; 100. doi: 10.1016/j.apergo.2021.103615. |
[27] | O’Connor S. Exoskeletons in nursing and healthcare: A bionic future. Clin Nurs Res. (2021) ; 30: (8): 1123. |
[28] | Frambach JM, van der Vleuten CPM, Durning SJ. Quality criteria in qualitative and quantitative research. Acad Med. (2013) ; 88: (4): 552. |




