Better understanding the life of the user to improve the design of orthopaedic footwear
Abstract
BACKGROUND:
A relatively high number of users is dissatisfied with their orthopaedic device. The term ‘user practice’ was introduced to emphasise the idea that users of orthopaedic devices perform activities within an environment, which are characteristic for that environment.
OBJECTIVE:
To investigate to what extend orthopaedic shoe engineers map the specific environments in which users live and the activities they perform within these environments during the first intake for custom made orthopaedic footwear.
METHODS:
Orthopaedic shoe engineers were recruited from orthopaedic service providers across The Netherlands. The intake with a new client for orthopaedic footwear was recorded and analysed using four user environments: daily life at home, transport, work, and leisure.
RESULTS:
Our study showed that orthopaedic shoe engineers cover at best less than 50% of activities within the four user environments. Consequently, there is no guarantee that the resulting design of the orthopaedic footwear fits all of the activities and environments of the users.
CONCLUSIONS:
The principles of user practices, consisting of specific environments and activities of the user, are not yet adequately used in the field of orthopaedic shoe engineering. By not using them, too little understanding of the life of the user can result in dissatisfaction and non-usage of the orthopaedic device.
1.Introduction
In the Netherlands over the past five years approximately 171.000 users of orthoses and custom made orthopaedic footwear are registered each year [1]. Of this number of users, approximately 32.600 persons received an orthosis for the lower extremity and about 95.100 persons received orthopaedic footwear. Moreover, during the last five years, the absolute number of users of the prescriptions of orthopaedic devices for the lower extremity (ankle foot orthoses (AFO’s) and orthopaedic footwear) has shown a steady increase [1]. However, these numbers do not reflect the actual usage of the prescribed orthopaedic devices. To be effective, orthopaedic devices should be used daily by those for whom they were prescribed. Previous studies show that one out of 15 AFO’s is not used at all, and 25% of the users of an AFO is dissatisfied with their device [2]. De Boer et al. [3] reported 12% non-usage of orthopaedic footwear and 8% non-usage of orthopaedic insoles in patients with rheumatoid arthritis. In a study by Van Netten et al. [4], 19% of the patients to whom orthopaedic footwear is prescribed, reports using the devices occasionally or not at all. In a study amongst diabetic patients, 58% of patients with prescribed orthopaedic footwear wore their footwear for less than 60% of daytime hours [5]. Gaining more insight into the reasons of non-use and dissatisfaction is relevant in relation to the high costs and efforts that are involved with the manufacturing of each individual orthopaedic device, and to maximize the potential of the orthopaedic device to contribute to health benefits and participation in activities in daily life.
Previous research among AFO users showed that not enough information about the user is obtained by the orthopaedic engineer11 during intake and examination, and important information and feedback from the user was not used adequately [2]. Research shows that the environment in which users perform activities with the prescribed orthopaedic device are not systematically addressed by the orthopaedic engineer [6]. In-depth questions are necessary to understand the activities of the users in different environments and to cover the whole range of needs and wishes of the user. Analysis has shown that activities of users must be understood in the specific environment in which they are performed. Findings also show that in the intake and examination phase for the design of an AFO, the orthopaedic engineer identified only 30% of important activities performed by users and discussed only 60% of the environments in which activities were performed [6]. As a result, the orthopaedic device might not be fitting in all environments and activities of the user, which leads to dissatisfaction of the users with their orthopaedic device, and results in a substantial level of non-use or sub-optimal use of the orthopaedic devices [6].
These findings might seem unexpected, as all orthopaedic engineers are familiar with the International Classification of Functioning, Disability and Health (ICF). The ICF is a classification of health and health-related domains. As the functioning and disability of an individual occurs within a specific context, the ICF also includes a list of environmental factors [7]. Use of the ICF should result in a match between the characteristics of the user and the characteristics of the product [8]. An explanation for the lack of information about the environments gained from using the ICF might be found in the general character of the ICF. It neither facilitates a systematic and detailed analysis of the activities of users, nor supports a systematic mapping of the environments in which users are living [6]. Activities should not be considered separately from the environment in which they take place. Each individual user has a particular role in every specific environment. The combination of environment and the role of the user within this environment (e.g. employee, member of a sports team) determines the activities that a user of an orthopaedic device has to do, and the accompanying movements that have to be performed [6]. The term ‘user practice’ was introduced to emphasise the idea that activities are performed within an environment and that these activities are characteristic for that environment. The concept of ‘user practices’ is derived from the so-called ‘practice approach’, which can offer a “radically new way of understanding and explaining social and organizational phenomena” [10, pp. 1–6]. This approach focuses on what people in a certain environment of practice are doing and saying. A user practice is defined as a coherent set of activities that are performed by users of medical products in a specific environment to realize the objectives of that environment [6, 9, 10].
Previous research on the principles of user practices within the context of orthopaedic engineering has revealed general environments in the field of orthopaedic devices for mobility [6]. The most important environments are: daily life at home, transport, work, and leisure. Patients live and act in the context of these different environments. The movements that are performed are characteristic for each environment. The nature and qualification of these environments co-determine the specifications for the orthopaedic device for mobility [9, 11]. The current idea is that obtaining information about the individual environments and the activities within those environments, is required to realise a better design of the orthopaedic device, in order to meet the demands of users in the different environments, and to realise a higher user satisfaction and a lower percentage of non-use. However, it is unclear to what extend orthopaedic engineers currently pay attention to these specific environments and activities in these environments during the first intake and examination with the user. Previous research suggests that orthopaedic engineers map a limited number of environments and activities [6]. However, this suggestion is based on interviews with clients after the intake, relying on their memories of the conversation.
Table 1
Description of environments and activities
| Environments and activities | Description |
|---|---|
| Daily life at home | |
| Walking indoors | Walking in a standard size house on an even floor. Small distances and low average speed |
| Manoeuvring | Moving in small indoor areas (kitchen, toilet, bathroom, etc.) |
| Walking stairs | Walking up and down inside the home using stairs |
| Housekeeping | Vacuuming, cleaning, window washing, washing clothes, etc. |
| Transport | |
| Walking outdoors | Walking outside on (partly) uneven terrain. Larger distances and higher average speed |
| Walking | Walking outside the house with low average speed, in terms of shopping etc. |
| Cycling (recreational) | Recreational |
| Cycling (non-recreational) | Commuting, getting daily groceries, etc. |
| Car | Driving by yourself |
| Bus, train, plane | Public transportation |
| Work | |
| Work professional | Office/desk work, physical work, industry, health care, etc. |
| Volunteer work | A diversity of activities like hostessing in a long-term care facility, visiting older adults, training the youth of a sports team, etc. |
| Leisure | |
| Sports | All types of sports |
| Other leisure activities | Shopping, dancing, gardening, social activities, religious activities, etc. |
| Other | |
| Other activities | Specific environment, different from previous four, relevant to the client |
The objective of the current study is to investigate to what extend orthopaedic engineers map the specific environments in which users of orthopaedic footwear live and the activities they perform within these environments during the first intake for custom made orthopaedic footwear. Since the number of users of orthopaedic footwear is higher than the number of users of orthoses for the lower extremities [1], we decided to first focus on the intake conversation of orthopaedic shoe engineers.22
2.Methods
2.1Study design
A quantitative study using observations was performed, in which the prevalence of the general environments and accompanying activities in the field of orthopaedic devices for mobility during the intake for orthopaedic footwear by orthopaedic shoe engineers was examined. Previous research on the principles of user practices within the context of orthopaedic engineering has shown four general environments in the field of orthopaedic devices for mobility: daily life at home, transport, work, and leisure [6].
2.2Participants
The participants, orthopaedic shoe engineers, were recruited from five orthopaedic shoe service providers, located across The Netherlands. Orthopaedic footwear users were approached by the participating orthopaedic shoe engineers. Adult male and female users who came in for their first pair of orthopaedic footwear were eligible for, and included in, the study.
2.3Procedure
Participating orthopaedic shoe engineers recorded the first intake with a new client either on video or audio recorder. Recordings were analysed using The Observer XT 15 [12]. The quantitative analyses were guided by the four general environments in the field of orthopaedic devices for mobility and the activities within these environments, with the option for a fifth environment specific for that individual user (Table 1). The environment ‘leisure’ was, compared to the original description of Holtkamp et al [6], divided into ‘sports’ and ‘other leisure activities’, since most sports require different demands of the orthopaedic device than for instance shopping and religious or spiritual activities.
Table 2
Frequencies of activities and environments asked for by the orthopaedic shoe engineer and mentioned by the users
| Activities asked for byorthopaedic shoe engineer | Activities spontaneously mentioned by user | |
|---|---|---|
| Daily life at home | ||
| Walking indoors | 4 | 1 |
| Manoeuvring | 0 | 0 |
| Walking stairs | 3 | 0 |
| Housekeeping | 3 | 1 |
| Transport | ||
| Walking outdoors | 6 | 2 |
| Walking | 1 | 3 |
| Cycling (recreational) | 0 | 0 |
| Cycling (non-recreational) | 2 | 1 |
| Car | 2 | 1 |
| Bus, train, plane | 0 | 0 |
| Work | ||
| Work professional | 5 | 1 |
| Volunteer work | 0 | 0 |
| Leisure | ||
| Sports | 1 | 0 |
| Other leisure activities | 5 | 0 |
| Other | ||
| Other activities | 0 | 0 |
2.4Data analysis
Activities asked for by the orthopaedic shoe engineer were marked and counted, as well as activities spontaneously mentioned by the user, to see which and how many times activities were asked about by the orthopaedic shoe engineers, as well as mentioned by the user. Also, the number of activities asked for by the orthopaedic shoe engineer, and the number of activities mentioned by the user were studied separately in order to see whether users spontaneously mention activities which are important to them, but were not addressed by the orthopaedic shoe engineer.
3.Results
A total of 2 video and 9 audio files that were recorded by five orthopaedic shoe engineers were analysed. The mean age of the participants (all male) was 37.2 years (SD
Figure 1.
Percentages of activities identified during the intake; OSE
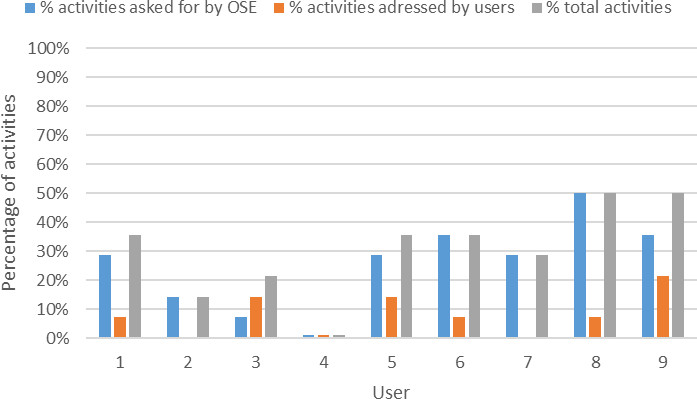
During the recordings, orthopaedic shoe engineers asked about a minimum of zero and a maximum of seven activities out of 14, with an average of four activities. Users spontaneously mentioned an average of one activity, with a minimum of zero and a maximum of three activities. The environment ‘transport’ was asked about most frequently by the orthopaedic shoe engineers, and this environment was also spontaneously mentioned most frequently by the users (Table 2). The second most often addressed environment by the orthopaedic shoe engineers as well as the users was ‘daily life at home’. The least amount of attention was paid to questions regarding activities within the environments ‘work’ and ‘leisure’. No other specific user environments were asked for. Activities that were not mentioned at all by the orthopaedic shoe engineer or the user during the intake were: manoeuvring, cycling (recreational), bus/train/plane and volunteer work.
In Fig. 1, percentages of activities asked for by the orthopaedic shoe engineers, spontaneously mentioned by the users, and the total percentage of activities talked about during the intake are shown per user. At the intake of user 4, no activities related to user environments were identified. Even in the most complete intake, only 50% of activities of the principles of user practices were covered.
4.Discussion and conclusion
The aim of this study was to investigate to what extend orthopaedic engineers map the specific environments in which users of orthopaedic footwear live and the activities they perform within these environments during the first intake for custom made orthopaedic footwear. These environments and activities have been found important within the principles of user practices to gain information from the user in order to provide orthopaedic footwear they will actually use. Results show that participants do ask about some environments and activities, but cover at best 50% of the entire range of activities and environments of the principles of user practices.
Besides activities explicitly asked about by the participants, some users also spontaneously mention activities they want to be able to perform with their orthopaedic footwear. In some cases, these activities were not previously asked about by the orthopaedic shoe engineer. But even then, no more than 50% of activities from the principles of user practices is ever covered. If a user is less assertive or talkative about his daily environments, important information about the users’ activities and environments could be entirely missed by the orthopaedic shoe engineer, resulting in an orthopaedic shoe that does not meet all or even an important part of the needs and wishes of the user [9, 11]. Some important activities, such as being able to manoeuvre within one’s house, which is a necessary part of self-management, are never asked about.
A large number of users of orthopaedic devices is a senior citizen, especially among women [1]. Social participation, such as volunteer work and leisure activities, benefits mental health and decreases the risk for depressive symptoms in older adults [13, 14]. In addition, social participation has a significant positive impact on general cognitive status in older persons [15]. This contributes to a better quality of life. With their professional career over, more time can be spent on volunteer work and leisure activities. Previous studies have shown an increase in physical activities during retirement [16, 17]. Research has shown that participation in sports activities decreases feelings of loneliness and social isolation in seniors [18]. The orthopaedic device should therefore not hinder sports and other physical activities. However, not any question about volunteer work was asked by the participants, and leisure activities were only asked about in some cases. Almost no questions were asked about sports activities, and being able to cycle, which is a primary form of transport in The Netherlands.
A complete overall picture about all relevant activities and environments of an individual user was never reached. It is also unclear how the information that was obtained is subsequently used in the design of the orthopaedic footwear. Further research is needed to develop a tool, which will help orthopaedic shoe engineers and users to efficiently collect information about all relevant activities and environments. Additional research should focus on the effect of the usage of this tool on usage of and satisfaction with the orthopaedic device.
After identifying the different user practices of the user, an analysis for every user practice must be performed to determine accompanying intrinsic values and relevant stakeholders [9, 11]. This should then be followed by an activities-movement analysis for every user practice, and subsequent mapping of the specific conditions for every user practice. Finally, a specification for the orthopaedic device can be drawn up, where as much of the needs and wishes of the user as possible are met [11]. Over time, this process should increase the usage and satisfaction of orthopaedic devices.
After obtaining all the information about the individual’s user practices, the information must be processed in order to design and manufacture an orthopaedic device that will meet all of, or as much as possible, the needs and wishes of the user in the different user practices. When not all needs and wishes can be met within the orthopaedic device, this should be discussed explicitly between orthopaedic shoe engineer and the user in order to manage expectations. It is especially important to make a shared decision about the design of the orthopaedic device, when not all activities can be incorporated in the design because of conflicting demands on the device.
This study has some limitations. Research focussed only on orthopaedic shoe engineers and the intake with users of custom made or bespoke orthopaedic footwear. The spectrum of orthopaedic devices for mobility is much broader, and therefore future research should not only include other types of orthopaedic footwear, but also orthotics of the lower extremity. Secondly, the study population was limited to five orthopaedic shoe service providers. However, participating service providers were located across the country, and recently graduated shoe engineers, as well as experienced shoe engineers participated in this study. Finally, although the data showed users mentioning some activities spontaneously, no check was performed by the researchers with the user to confirm if all environments and activities were discussed.
In conclusion, the principles of user practices, where questions are being asked about the specific environments in which users of orthopaedic footwear live and the activities they perform within these environments, are not yet adequately used in the field of orthopaedic shoe engineering. This leads to the possibility of orthopaedic devices not meeting the needs and wishes of the user in every user practice, resulting in non-usage of and dissatisfaction with the orthopaedic device. In order to improve the process of obtaining information during the intake with the orthopaedic shoe engineer, a tool must be developed with which the required information can be gathered efficiently. The next step would be to incorporate the principles of user practices in that new tool, to adequately analyse the obtained information in order to be able to design an orthopaedic device which can be used in each of the, or most of the, activities and environments of the individual user.
Author contributions
CONCEPTION: Lianne S. van Dijk, Fred C. Holtkamp and Maarten Verkerk.
PERFORMANCE OF WORK: Lianne S. van Dijk.
INTERPRETATION OR ANALYSIS OF DATA: Lianne S. van Dijk.
PREPARATION OF THE MANUSCRIPT: Lianne S. van Dijk.
REVISION FOR IMPORTANT INTELLECTUAL CONTENT: Lianne S. van Dijk, Fred C. Holtkamp, Maarten Verkerk and Eveline J.M. Wouters.
SUPERVISION: Eveline J.M. Wouters.
Ethical considerations
All participating orthopaedic shoe engineers and users received written information about the purpose of the study prior to the recordings and gave informed consent. This study was not subjected to the Medical Research Involving Human Subjects Acts (WMO), because it only involved an observation of usual care.
Notes
1 We are aware that the naming of the profession in health care is not universal. We focus on professions at the vocational and bachelor levels.
2 We are aware that the naming of the profession in health care is not universal. Other terms used for orthopaedic shoe engineering include orthopaedic shoe technology and pedorthics.
Acknowledgments
All participants and users are thanked for their willingness to participate in this study.
Conflict of interest
The authors have no conflict of interest to report.
References
[1] | GIPdatabank.nl. (2021) ; Available from: https://www.gipdatabank.nl. |
[2] | Holtkamp FC, Wouters EJM, van H, van Z, Verkerk M. Use of and satisfaction with ankle foot orthoses. Clinical research on foot & ankle. (2015) ; 3: : 167. doi: 10.4172/2329-910X.1000167. |
[3] | de Boer IG, Peeters AJ, Ronday HK, Mertens BJA, Huizinga TWJ, Vliet V. Assistive devices: usage in patients with rheumatoid arthritis. Clin Rheumatol. (2009) Feb; 28: (2): 119–28. |
[4] | van Netten JJ, Jannink MJA, Hijmans JM, Geertzen JHB, Postema K. Patients’ expectations and actual use of custom-made orthopaedic shoes. Clin Rehabil. (2010) Oct; 24: (10): 919–27. |
[5] | Arts MLJ, de Haart M, Bus SA, Bakker JPJ, Hacking HGA, Nollet F. Perceived usability and use of custom-made footwear in diabetic patients at high risk for foot ulceration. J Rehabil Med. (2014) Apr; 46: (4): 357–62. |
[6] | Holtkamp FC, Verkerk MJ, Hoof Joost V, Wouters E. Mapping user activities and user environments during the client intake and examination phase: an exploratory study from the perspective of ankle foot orthosis users. Technology and disability. (2016) ; 28: (4): 148–57. doi: 10.3233/TAD-160452. |
[7] | Nederlands WHO-FIC Collaborating Centre. Nederlandse vertaling van de ‘International Classification of Functioning, Disability and Health’. Houten: Bohn Stafleu Van Loghum; (2002) . |
[8] | Heerkens Y, Bougie T, Claus E. The use of the ICF in the process of supplying assistive products: discussion paper based on the experience using a general Dutch prescription guideline. Prosthet Orthot Int. (2011) Sep; 35: (3): 310–7. |
[9] | Verkerk MJ, Holtkamp FC, Wouters EJM, van Hoof J. Professional Practices and User Practices: An Explorative Study in Health Care. Philosophia reformata. (2017) ; 82: (2): 167–91. doi: 10.1163/23528230-08202001. |
[10] | Nicolini D. Practice Theory, Work, & Organization: An Introduction. Oxford, UK: Oxford University Press; (2013) . |
[11] | Holtkamp FC, Wouters EJM, Verkerk MJ. Understanding User Practices When Drawing up Requirements-The Case of Designing Assistive Devices for Mobility. Int J Environ Res Public Health. (2019) Jan; 16: (3). |
[12] | Noldus. The Observer XT 15. Wageningen: Noldus Information Technology bv; (2019) . |
[13] | Chiao C, Weng L-J, Botticello AL. Social participation reduces depressive symptoms among older adults: an 18-year longitudinal analysis in Taiwan. BMC Public Health. (2011) May; 11: : 292. |
[14] | Choi E, Han K-M, Chang J, Lee YJ, Choi KW, Han C, et al. Social participation and depressive symptoms in community-dwelling older adults: Emotional social support as a mediator. J Psychiatr Res. (2021) May; 137: : 589–96. |
[15] | Chiao C. Beyond health care: Volunteer work, social participation, and late-life general cognitive status in Taiwan. Soc Sci Med. (2019) May; 229: : 154–60. |
[16] | Stenholm S, Pulakka A, Kawachi I, Oksanen T, Halonen JI, Aalto V, et al. Changes in physical activity during transition to retirement: a cohort study. Int J Behav Nutr Phys Act. (2016) Apr; 13: : 51. |
[17] | Godfrey A, Lord S, Galna B, Mathers JC, Burn DJ, Rochester L. The association between retirement and age on physical activity in older adults. Age Ageing. (2014) May; 43: (3): 386–93. |
[18] | Hwang J, Wang L, Siever J, Medico T Del, Jones CA. Loneliness and social isolation among older adults in a community exercise program: a qualitative study. Aging Ment Health. (2019) Jun; 23: (6): 736–42. |




