The influence of the indoor environment on people displaying challenging behaviour: A scoping review
Abstract
BACKGROUND:
The care sector for persons with disabilities considers the physical environment relevant for the quality of life of people with intellectual disabilities. However, scientific evidence is limited.
OBJECTIVE:
To obtain evidence regarding comforting and encouraging environments and to develop an overview of studies addressing the effect of the physical environment on people with intellectual disabilities.
METHODS:
A scoping review, accompanied by expert panels and case findings combining scientific evidence and knowledge from practice, was performed to investigate the interaction between challenging behaviour and the physical environment. Between January and March 2020, several scientific databases were searched in the English, Dutch, and German language for relevant studies. Social media, care professionals, and experts in building physics were consulted.
RESULTS:
Studies on building-related factors as passive interventions and care- or therapy-related interventions could be distinguished. The majority of the studies report on building-related factors such as sound, acoustics, light, and colours and their influence on behaviour. Specific guidelines are lacking on how to adjust the indoor environment to an environment that is safe, comforting and encouraging for people displaying challenging behaviour. Proposed solutions are case-based.
CONCLUSION:
In future studies individual cases could be studied in a more in-depth manner, aligned and categorised to the building-related factors and to the expressions of challenging behaviour.
1.Background
For persons with intellectual disabilities the physical environment in the care sector is seen as relevant to their health, behaviour, and participation [1]. The prevalence of challenging behaviour in people with intellectual disabilities has been reported to vary between 45 to 82 percent, depending on the type of behaviour and living situation [2, 3]. The expression of challenging behaviour varies, but self-injurious as well as aggressive or destructive behaviour have been reported in people with intellectual disabilities and multiple disabilities [2]. Challenging behaviour can be triggered and enheightened when the physical environment’s facilities are not in-line with the demand for care. When long-term patterns of inappropriate behaviour occur in people with intellectual disabilities, they are referred to as persons with problem behaviour or difficult-to-understand behaviour [4]. People with difficult-to-understand behaviour express themselves differently because, for example, there may be delayed (sensory) information processing. Difficult-to-understand behaviour can manifest itself in several ways, such as poor language skills, excessive laughter, hyperactivity, a short attention span, and sleep problems [5]. Aggression and self-injury are also manifestations of difficult-to-understand behaviour in people with intellectual disabilities.
The physical environment consists of the indoor environment and the layout of a room. The indoor environment comprises the indoor climate (thermal and air quality), (day)light and colours, acoustics, and sound. The hypothesis is that if the physical environment is appropriately designed to meet the wishes and needs of people with disabilities, and fit the demand for care, challenging behaviour will decrease. Unfortunately, no scientific literature exists that gives evidence of the possible benefits of the physical environment in care facilities where people that could display challenging behaviour reside, to the demand of care of these residents. It was still possible to examine the hypothesis as literature coming from other domains shows results that the physical environment does have a positive effect on people. Evidence is given by the Healing environment concept. A Healing environment is described as an environment that positively influences both patients and staff in a hospital environment [6]. Ulrich, for example, showed that the length of stay in the hospital and the use of heavy medication could be reduced by providing a view of nature during the stay [7]. In addition, the patient’s behaviour towards staff was friendlier.
In long-term care, comparable results were found. In this context, the concept is addressed as an enriched environment supporting the health and wellbeing of residents and staff [8]. For people with intellectual disabilities in the care sector, both concepts may not apply, but elements of both concepts could be used to create a comforting and encouraging environment for those residing in a long-term care facility. However, for persons with intellectual disabilities in the care sector new practices may have evolved not yet supported by scientific evidence. Based on the expertise of care professionals, evidence from clinical practice could help identify knowledge gaps in need of further research [9]. A scoping review was executed in search of evidence regarding comforting and encouraging environments and to develop an overview of studies and clinical knowledge in which the effect of the physical environment of people with intellectual disabilities (independent of specific intellectual disabilities) is addressed. This scoping review aims to unravel current evidence and clinical knowledge on the effect of building-related factors on expressions of challenging behaviour irrespective of the type of disability.
Table 1
Interventions of building-related factors. Examples of passive non-pharmacological interventions and care- or therapy-related interventions
| Building related factors | ||
|---|---|---|
| Type of intervention | Passive non-pharmacological interventions | Care- or therapy-related interventions |
| Examples | Light grid or plan | Blue light lamps to influence sleep and wake patterns |
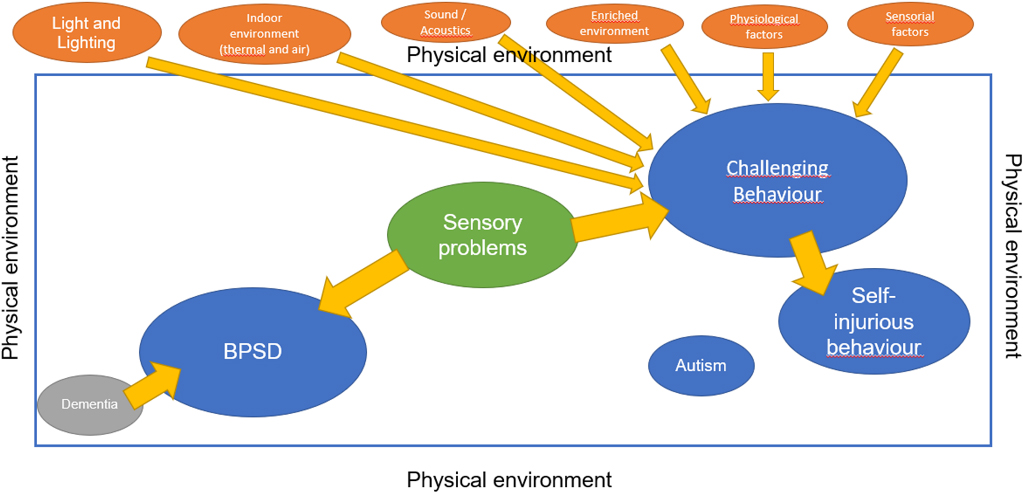
Figure 1.
Conceptualisaton of possible relations between the factors of the physical environment and challenging behaviour. Abbreviations: BPSD
2.Method
The scoping review used scientific and grey literature following the methodological framework by Arksey and O’Malley [10] and Rumrill et al. [11]. A scoping review can be used to identify knowledge parameters and gaps in literature [12]. Between January and March 2020, the databases HBO Kennisbank (a database of all publications of Dutch Universities of Applied Sciences), NARCIS, Science Direct, Scopus, Pubmed, PsycINFO, Google Scholar, Web of Science and Embase were searched to retrieve relevant studies. Table A1 in the appendix presents the keywords used in each of the databases. Keywords were categorised into three groups, Living situations, Target group and Behaviour was combined with the different keywords used per category. The final search string applied in PubMed can be found in Appendix 1. It provided guidance for all searches in the other databases. Articles published between January 2002 and March 2020 were eligible for inclusion. Studies published before 2002 were included if they provided information essential to the topic of this review not addressed in more recent studies. All levels of evidence were included and there was no restriction on the study design.
Furthermore, social media, care professionals, and experts in building physics were consulted. All search engines and digital media were searched in the English, Dutch, and German language. Case findings supplemented the theoretical approach to gain insights from experiences in daily practice on adjustments to the physical environment and its influence on behaviour. An iterative approach enabled reflection on the data collected allowing adjustments to each step of the scoping review.
Literature from other domains was also included when no results were found. The focus, however, was kept on challenging behaviour for all types and expressions of behaviour for all types of disability that cannot easily be interpreted or is considered as incomprehensible behaviour, including Behaviour of Psychosocial Symptoms of Dementia (BPSD). Based on the available evidence, the data was ‘a posteriori’ structured and conceptualised taking indoor environmental factors and their potential influence on behaviour as a starting point (Fig. 1). The results are organised from the perspective of building physics. Therefore, findings are placed in sections aligned with indoor environmental factors. Size, design and lay-out are added as a separate section.
3.Results
3.1Main findings
In general, the expert sessions with professionals and SI therapists (therapists with a focus on sensory information processing (SI)) indicate that people displaying challenging behaviour will experience negative effects of building-related factors when these do not fit the demand for care and therapy. An example is a client’s room which was refitted from a smooth shiny surface room with a metallic image causing glare to a room where natural materials were used, the walls were coloured in a soft autumn leaf-like colour and indirect light was used above the bed.
The findings of the scoping review could be categorised as building-related factors. Building-related factors are considered indoor environmental factors which can be added, removed, or optimised via modification of building installation elements. Distinctions can be made in passive non-pharmacological interventions and care- or therapy-related interventions (active non-pharmacological interventions). In the consensus statement of the Summit on Intellectual Disability and Dementia adjustments in the physical environment are noted as relevant non-pharmacological interventions before therapy with pharmacological intervention in the case of challenging behaviour of people with an intellectual disability or in the case of dementia BPSD [1]. A potential risk for the client must be judged appropriately, and the environment should have a calm, comforting and encouraging appearance [13]. This can be translated for the separate building-related factors in the following order.
Table 1 shows how building-related factors can be used as different interventions. Thinking ahead or making changes to the lighting plan is an example of a passive non-pharmacological intervention and the use of blue light lamps to influence sleep and wake patterns is an example of therapy-related intervention.
Table 2
Overview of the results on building-related factors as non-pharmacological interventions
| Building-related factors | Target group | |||
|---|---|---|---|---|
| Challenging behaviour | Dementia | Older people | ||
| Floor plan | Size | Behaviour, well-being and loneliness (L) | ||
| Design | Closed environment was reported as a cause of aggression (L) | |||
| Layout | The position of the kitchen is relevant due to olfactorily triggers (L) | Position of the kitchen (L) | ||
| Sound & Acoustics | Noise and an overload of sounds should be avoided (L) | React anxiously to sudden loud noises (L) | Be aware of speech intelligibility (L) | |
| Might have relaxing, comforting, and encouraging influences (L) | ||||
| (Day)light & Colours | Reduction in symptoms of sleep disturbance, BPSD, and Quality of Life (L) | |||
| The use of colours is perceived to have effects (CF) | ||||
| Indoor climate | Thermal | Prefers to be kept warm (CF), gives sense of security | Prefers to be kept warm, gives sense of security (L) | The ability to regulate body temperature, which is partly dependent on circadian rhythm, additionally decreases with age (L) |
| Temperature (L) | ||||
| Air | Odours produced by cooking activities could stimulate the appetite and the function of the saliva glands (L) | |||
Legenda: Based on Literature (L); Based on case findings (CF).
The focus in this report will be on building-related factors such as non-pharmacological intervention. Building-related factors comprise the floor plan (size, design and layout), sound and acoustics, (day)light and colours, and indoor climate (thermal and indoor air quality). Table 2 shows an overview of the results on building-related factors such as non-pharmacological interventions. In the next paragraphs the findings from three different diagnosis groups will be described in more detail.
3.2Size, design, and layout
Several studies indicate that the size of the living facility impacts the behaviour and well-being of a client. Living in a residential group with more than seven residents is associated with more loneliness while living with residents of their own choice or living with family members causes less loneliness [14, 15, 16]. Furthermore, a prevalence of self-injurious behaviour of 7–50% in larger residential centres has been reported compared to 2–5% in smaller community settings [17]. Besides the ward ambiance, a closed environment was reported as a cause for aggression [18, 19]. The latter applies to both being trapped as well as feeling trapped [20]. Regarding the layout of the floor plan no information could be found except regarding the kitchen. The position of the kitchen is relevant due to olfactorily triggers see also 3.5.
3.3Sound and acoustics
Regarding sound and acoustics, McGill showed that noise and an overload of sounds should be avoided and that clients displaying challenging behaviour should be taught how to deal with noises and sounds [21]. From research on dementia, it is known that persons with dementia can react anxiously to sudden loud noises [22]. In addition to offering coping strategies to deal with sounds and noises, it is also highly relevant to be aware of speech intelligibility. This can be disturbed in a comparable way as in older people with hearing problems. A lab study by Sato demonstrated that the speech intelligibility score, measured by speech intelligibility test with older persons (
3.4(Day)light and colours
Light has a positive effect on people. Light affects the visual and circadian system as well as mood and motivation. All three mechanisms interact with each other [25]. Unknown is what optimal light conditions are for people displaying challenging behaviour. Individual differences are expected and categorisation could also be based on the character of the challenging behaviour. For people with dementia it is known that the quality of the light conditions contributes to a reduction in symptoms such as sleep disturbance, BPSD and quality of life. With adjusted light conditions less fear, unrest, aggression, risk to falls, apathy and sleep disturbance might occur [26, 27]. No literature was found describing effects due to the use of colours. In practice, though based on the case findings, the use of colours is perceived to have effects on people with intellectual disabilities, but no scientific evidence has yet been found.
3.5Indoor climate (thermal and indoor air quality)
No studies were found that reported on thermal influences, their interaction with people displaying challenging behaviour and the influence on their behaviour. Also, the case findings identified with the participating care professionals showed that this has not yet been addressed. However, a case from practice mentioned that a client displaying challenging behaviour prefers to be kept warm. They then experience, as the care workers indicate, a sense of security. This phenomenon has also been reported for people with dementia.
There is a difference in how people experience the thermal environment. This is determined, for example, by gender, age, clothing, activity and culture [28, 29, 30]. The ability to regulate body temperature, which is partly dependent on circadian rhythm, additionally decreases with age.
People with dementia experience functional olfactory limitation due to biological ageing but most of all due to the pathology of dementia syndrome. This indicates that it will be highly relevant to maintain an appropriate indoor air quality [31]. The use of certain odours might have a positive influence. Odours produced by cooking activities could stimulate the appetite and the function of the saliva glands [31]. This aspect indicates the importance of the position of the kitchen in long-term care facilities.
Regarding the influence of temperature on dementia it is known that people with severe dementia have less control over thermal comfort. The mechanical mechanism of the thermostat, which has a delay in changing the temperature and feeling the desired temperature, confuses people with dementia. This could result in people with dementia taking off their clothes when the room is not immediately cool enough or trying to put more clothes on when the room is not immediately warmer. All this could evoke incomprehensible behaviour like BPSD. Therefore, thermostats should be designed differently, namely in a more comprehensible manner compensating for the limitations due to the pathology [32]. However, as previously stated, scientific evidence of thermal influences on persons with intellectual disabilities needs yet to be established.
4.Reflection on the findings
The above findings address the building-related factors as a passive non-pharmacological intervention only. The relevance of our findings is supported by the consensus statement of the Summit on Intellectual Disability and Dementia that recognised adjustments in the physical environment as relevant non-pharmacological interventions and favoured these adjustments over therapy with pharmacological intervention in the case of people with an intellectual disability that display challenging behaviour or in the case of people with dementia displaying BPSD [1]. The evidence on building-related factors and the influence on the behaviour of persons with intellectual disabilities are scarce. Several studies explored the impact of the size of the residential group and the impact on behaviour in persons with intellectual disabilities [14, 15, 16, 18, 19, 20]. The smaller the setting the more positive the reported effect on the feeling of loneliness [14, 15, 16] or the exhibition of aggressive behaviour was [19]. Regarding the impact of sound environment, few studies describe a relevant impact on the behaviour of persons with intellectual disabilities [21, 24]; the impact can be positive and cause relaxation and comforting behaviour but also negative if an overload of sounds is experienced. McGill therefore advocates providing strategies on how to deal with noises and sounds [21]. However, no specific guidelines are provided. Specific information on optimal lighting conditions and the indoor climate is missing for this specific group. Studies in persons with dementia may provide a starting point for future research.
Studies reporting on care- or therapy-related interventions were also found; these comprise for instance the well-known ‘snoezelen’ rooms [33], and a maybe less-known use of soundscaping. Soundscaping was used in the study by Van den Bosch in which five different sound sources (beach, silence, urban, forest, music) were used, aiming to create a safe and comforting environment for people displaying challenging behaviour. The silence mode increased boredom behaviour [34]. However, the efficacy of ‘snoezelen’ rooms in dementia care is limited [35], and evidence in persons with profound intellectual disabilities suggests it may only be significant in certain target behaviours [26].
The focus of this scoping review was on the building-related factors. Understanding how building-related factors may influence people displaying challenging behaviour contributes to improving spaces as passive non-pharmacological interventions both in renovated and newly built residences.
The scoping review has been executed to retrieve the scope of the question/issue raised to set directions for future research. The findings are, therefore, not generalisable to all people displaying challenging behaviour and their residence. Future research could include a systematical approach of multiple case-controlled studies in which single or combined building-related factors are adjusted in the indoor environment to the demand of care and quality of life for people displaying challenging behaviour, while taking into account ethics and privacy considerations. Furthermore, this scoping review also showed the added value of combining clinical knowledge, building physics expertise and practice-based findings. Based on this experience, a collaboration of researchers and care facilities for persons with intellectual disabilities is recommended to systematically collect data on adjustments in the indoor environment and their effect on the behaviour of individual persons. An expert group encompassing researchers, care professionals, building facility management personnel, and experts in building physics would be beneficial to gain evidence-based knowledge in real-life situations.
5.Conclusion
Most of the studies report on sound, acoustics, light, colours and the influence on behaviour. No specific guidelines are given about how to adjust the indoor environment to an environment that is safe, comforting, and encouraging for people displaying challenging behaviour. Possible solutions are case-specific. This scoping review showed that studies are needed to gain a better understanding of how building-related factors, applied as non-pharmacological interventions may influence people displaying challenging behaviour and how displaying this behavior can be prevented or lessened. In future studies these cases could be studied aligned and categorised to the building-related factors and the expressions of challenging behaviour.
Author contributions
CONCEPTION: Helianthe Kort and Emelieke Huisman.
PERFORMANCE OF WORK: Emelieke Huisman, Chantal Huisman and Sigrid Mueller-Schotte.
INTERPRETATION OR ANALYSIS OF DATA: Eme-lieke Huisman, Chantal Huisman, Sigrid Mueller-Schotte and Helianthe Kort.
PREPARATION OF THE MANUSCRIPT: Chantal Huisman, Emelieke Huisman, Sigrid Mueller-Schotte and Helianthe Kort.
REVISION FOR IMPORTANT INTELLECTUAL CONTENT: Helianthe Kort, Chantal Huisman and Sigrid Mueller-Schotte.
SUPERVISION: Helianthe Kort.
Ethical considerations
This study, as a scoping literature review, is exempt from Institutional Review Board approval.
Acknowledgments
All care professionals, experts, and Stichting ‘s Heerensloo are thanked for their valued contribution to the scoping review.
This project was co-financed by The Netherlands Organisation for Health Research and Development call Just special (Gewoon Bijzonder). (ZonMW: project number 845008503).
Conflict of interest
The authors declare no conflict of interest.
References
[1] | Dodd K, Watchman K, Janicki MP, Coppus A, Gaertner C, Fortea J, et al. Consensus statement of the international summit on intellectual disability and Dementia related to post-diagnostic support*. Aging and Mental Health. (2018) ; 22: : 1406-1415. doi: 10.1080/13607863.2017.1373065. |
[2] | Poppes P, van der Putten AJJ, Vlaskamp C. Frequency and severity of challenging behaviour in people with profound intellectual and multiple disabilities. Research in Developmental Disabilities. (2010) ; 31: : 1269-1275. doi: 10.1016/j.ridd.2010.07.017. |
[3] | Ailey SH, Friese TR, Nezu AM. Modifying a social problem-solving program with the input of individuals with intellectual disabilities and their staff. Res Nurs Health. (2012) ; 35: : 610-623. doi: 10.1002/nur.21497. |
[4] | Devine DP, Symons FJ. Biological Vulnerability and Risk for Self-Injury in Intellectual and Developmental Disabilities. In: International Review of Research in Developmental Disabilities, (2013) , pp. 37-67. doi: 10.1016/B978-0-12-401662-0.00002-6. |
[5] | Summers JA, Allison DB, Lynch PS, Sandier L. Behaviour problems in Angelman syndrome. Journal of Intellectual Disability Research. (1995) ; 39: : 97-106. doi: 10.1111/j.1365-2788.1995.tb00477.x. |
[6] | Huisman ERCM, Morales E, Hoof J, Kort HSM. Healing environment: A review of the impact of physical environmental factors on users. Building and Environment. (2012) ; 58: : 70-80. doi: 10.1016/j.buildenv.2012.06.016. |
[7] | Ulrich RS. View through a window may influence recovery from surgery. Science. (1984) ; 224: : 420-421. doi: 10.1126/science.6143402. |
[8] | Huisman ERCM, van Hout NHAM, Reinten J, Kort HSM. Steps towards an acoustical intervention in a nursing home for the benefit of residents and staff: A case study. Gerontechnology. (2018) ; 16. doi: 10.4017/gt.2017.16.4.007.00. |
[9] | Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology. (2018) ; 18. doi: 10.1186/s12874-018-0611-x. |
[10] | Arksey H, Malley L. Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology: Theory and Practice. (2005) ; 8: : 19-32. doi: 10.1080/1364557032000119616. |
[11] | Rumrill PD, Fitzgerald SM, Merchant WR. Using scoping literature reviews as a means of understanding and interpreting existing literature. Work. (2010) ; 35: : 399-404. doi: 10.3233/WOR-2010-0998. |
[12] | Armstrong R, Hall BJ, Doyle J, Waters E. ‘Scoping the scope’ of a cochrane review. Journal of Public Health. (2011) ; 33: (1): 147-150. doi: 10.1093/pubmed/fdr015. |
[13] | Prasher VP, Mahmood H. Management of Dementia in Intellectual Disability. In: Seminars in the Psychiatry of Intellectual Disability. (2019) ; pp. 136-146. doi: 10.1017/9781108617444.011. |
[14] | Alexandra P, Angela H, Ali A. Loneliness in people with intellectual and developmental disorders across the lifespan: A systematic review of prevalence and interventions. Journal of Applied Research in Intellectual Disabilities. (2018) ; 31: : 643-658. doi: 10.1111/jar.12432. |
[15] | Stancliffe RJ, Lakin KC, Doljanac R, Byun SY, Taub S, Chiri G. Loneliness and living arrangements. Intellectual and Developmental Disabilities. (2007) ; 45: : 380-390. doi: 10.1352/1934-9556(2007)45[380:LALA]2.0.CO;2: . |
[16] | Stancliffe RJ, Lakin KC, Taub S, Chiri G, Byun SY. Satisfaction and sense of well being among medicaid ICF/MR and HCBS recipients in six states. Intellectual and Developmental Disabilities. (2009) ; 47: : 63-83. doi: 10.1352/1934-9556-47.2.63. |
[17] | Glaesser RS, Perkins EA. Self-injurious behavior in older adults with intellectual disabilities. Social Work (United States). (2013) ; 58: : 213-221. doi: 10.1093/sw/swt018. |
[18] | Fish R, Culshaw E. The last resort? Staff and client perspectives on physical intervention. Journal of Intellectual Disabilities. (2005) ; 9: : 93-107. doi: 10.1177/1744629505049726. |
[19] | van den Bogaard KJHM, Lugtenberg M, Nijs S, Embregts PJCM. Attributions of People with Intellectual Disabilities of Their Own or Other Clients’ Challenging Behavior: A Systematic Review of Qualitative Studies. Journal of Mental Health Research in Intellectual Disabilities. (2019) ; 12: : 126-151. doi: 10.1080/19315864.2019.1636911. |
[20] | Duperouzel H, Fish R. Hurting No-One Els’s Body but Your Own: People with Intellectual Disability Who Self Injure in a Forensic Service. Journal of Applied Research in Intellectual Disabilities. (2010) ; 23: (6): 606-615. doi: 10.1111/j.1468-3148.2010.00559.x. |
[21] | McGill P, Teer K, Rye L, Hughes D. Staff reports of setting events associated with challenging behavior. Behavior Modification. (2005) ; 29: : 599-615. doi: 10.1177/0145445503259392. |
[22] | Burton E, Torrington J. Designing environments suitable for older people. CME Journal Geriatric Medicine. (2007) ; 9: : 39-45. |
[23] | Sato H. Effect of aging of hearing on speech recognition in rooms. Gerontechnology. (2005) ; 3. doi: 10.4017/gt.2005.03.04.024.00. |
[24] | van den Bosch KA, Andringa TC, Başkent D, Vlaskamp C. The Role of Sound in Residential Facilities for People With Profound Intellectual and Multiple Disabilities. Journal of Policy and Practice in Intellectual Disabilities. (2016) ; 13: : 61-68. doi: 10.1111/jppi.12147. |
[25] | Boyce PR. Human factors in lighting, third edition. CRC Pres; (2014) . doi: 10.1201/b16707. |
[26] | Radzey G, Kreutzer B, ed., Licht und Demenz, “Infobroschüre”, Stuttgart, (2010) . https//www.demenz-support.de/Repository/dessjournal_1_2010_korr_Licht.pdf. |
[27] | Torrington JM, Tregenza PR, Noell-Waggoner LC. Lighting for people with dementia. Lighting Research and Technology. (2007) ; 39: : 81-97. doi: 10.1177/1365782806074484. |
[28] | Mishra AK, Loomans MGLC, Hensen JLM. Thermal comfort of heterogeneous and dynamic indoor condition – An overview. Building and Environment. (2016) ; 109: : 82-100. doi: 10.1016/j.buildenv.2016.09.016. |
[29] | Ottenheijm L, Loomans M, Kort H, Trip A. Thermal comfort assessment in a Dutch hospital setting – Model applicability. Research Tue Nl. (2005) ; 2-3. [Accessed March 29, 2022]. Available from: https//research.tue.nl/en/publications/thermal-comfort-assessment-in-a-dutch-hospital-setting-model-appl. |
[30] | van Hoof J, Kort HSM, Hensen JLM, Duijnstee MSH, Rutten PGS. Thermal comfort and HVAC design for people with dementia. In: 9th International Conference and Exhibition – Healthy Buildings 2009, HB 2009; (2009) , pp. 1-17. [Accessed March 29, 2022]. Available from: https//pure.tue. nl/ws/files/94530535/708086454159365.pdf: . |
[31] | van Hoof J, Kort HSM, Duijnstee MSH, Rutten PGS, Hensen JLM. The indoor environment and the integrated design of homes for older people with dementia. Building and Environment. (2010) ; 45: : 1244-1261. doi: 10.1016/j.buildenv.2009.11.008. |
[32] | Fernie G, Femnie B. Technological innovations for individuals with Alzheimer’s disease. American Journal of Alzheimer’s Disease and Other Dementias. (1990) ; 5: : 9-14. doi: 10.1177/153331759000500304. |
[33] | Fava L, Strauss K. Multi-sensory rooms: Comparing effects of the Snoezelen and the Stimulus Preference environment on the behavior of adults with profound mental retardation. Research in Developmental Disabilities. (2010) ; 31: : 160-171. doi: 10.1016/j.ridd.2009.08.006. |
[34] | van den Bosch KA, Andringa TC, Peterson W, Ruijssenaars WAJJM, Vlaskamp C. A comparison of natural and non-natural soundscapes on people with severe or profound inte-llectual and multiple disabilities. Journal of Intellectual and Developmental Disability. (2017) ; 42: : 301-307. doi: 10.3109/13668250.2016.1250251. |
[35] | Chung JC, Lai CK. Snoezelen for dementia. Cochrane Database of Systematic Reviews. (2002) . doi: 10.1002/14651858.cd003152. |
Appendices
Appendix
Table A1
Key words in English language used for literature search
| Living situation | Target group | Behaviour |
|---|---|---|
| Residential facilities | Mentally disabled persons | Problem behaviour |
| Longterm care | Mentally challenged | Challenging behaviour |
| Group homes | Mentally retard | Disruptive behaviour |
| Assisted living | Low intelligence | Uninhibited behaviour |
| Institutionalized | Mentally handicaped | Misunderstood behaviour |
| Small scale care | Intellectual disabilities | |
| Intramural | ||
| Environment | ||
| Building | ||
| Surrounding | ||
| Setting |
Appendix 2
Search string PubMed
(((((((((((((((((("Residential Facilities"[Mesh]) OR longterm care[Title/Abstract]) OR long-term care[Title/Abstract]) OR residential facilit*[Title/Abstract]) OR group home*[Title/Abstract]) OR assisted living[Title/Abstract]) OR institutionalized[Title/Abstract]) OR institutionalised[Title/Abstract]) OR small scale care[Title/Abstract]) OR intramural care[Title/Abstract])) OR environment*[Title/Abstract]) OR building*[Title/Abstract])) OR (surrounding*[Title/Abstract] OR setting*[Title/Abstract]))) OR "Environment"[Mesh])) AND ((((((((("Mentally Disabled Persons"[Mesh]) OR mentally disabled[Title/Abstract]) OR mentally challenged[Title/Abstract]) OR mentally retard*[Title/Abstract]) OR low intelligence[Title/Abstract]) OR mentally handicapped[Title/Abstract]) OR intellectual disabilit*[Title/Abstract])) AND ((((((((((("Problem Behaviour"[Mesh]) OR problem behaviour*[Title/Abstract]) OR problem behaviour*[Title/Abstract]) OR challenging behaviour*[Title/Abstract]) OR challenging behaviour*[Title/Abstract]) OR disruptive behaviour*[Title/Abstract]) OR disruptive behaviour*[Title/Abstract]) OR uninhibited behaviour*[Title/Abstract]) OR uninhibited behaviour*[Title/Abstract]) OR misunderstood behaviour*[Title/Abstract]) OR misunderstood behaviour*[Title/Abstract]))




