Lost and misplaced items and assistive devices in nursing homes: Identifying problems and technological opportunities through participatory design research
Abstract
INTRODUCTION:
Modern healthcare, including nursing home care, goes together with the use of technologies to support treatment, the provision of care and daily activities. The challenges concerning the implementation of such technologies are numerous. One of these emerging technologies are location technologies (RTLS or Real-Time Location Systems). that can be utilized in the nursing home for monitoring the use and location of assets.
METHODOLOGY:
This paper describes a participatory design study of RTLS based on context mapping, conducted in two nursing home organizations. Rather than investigating the technological possibilities, this study investigates the needs and wishes from the perspective of the care professional.
RESULTS:
The study identified semantic themes that relate to the practicalities of lost and misplaced items in the nursing home, as well as latent themes that cover the wishes regarding technology in the nursing homes. The organizational culture and building typology may play a role in losing items.
CONCLUSION:
The participants in this study indicated that RTLS can provide a solution to some of the challenges that they encounter in the workplace. However, the implementation of new technologies should be done with care and should be integrated into existing ICT systems in order to minimize additional training and posing a burden on the workload.
1.Introduction
1.1Smart care homes and assistive technologies
Everyone has had the experience of not being able to find their keys, wallet or telephone. One forgets where he or she put the item, misplaced it, or lost it altogether. This usually goes together with feelings of frustration, unplanned search times and being delayed from continuing one’s actions. Very often, the timing of ‘losing’ an object is impeccable: right at the moment one needs to leave or really need to make that important phone call. In the domain of healthcare, it is no different. Healthcare professionals spend much time and effort retrieving lost items; time that should and could be spent on the provision of care [1]. In nursing homes, problems with losing items may be aggravated by the presence of residents with dementia, of whom is known that between MMSE scores of 19 and 9 (moderate dementia), there is a loss of optimal (independent) performance to find belongings [2, 3]. van Hoof et al. [4] identified numerous items owned by residents and informal caregivers that get lost and require staff to help look for these belongings. In the Netherlands, there is an increasing amount of pressure on care professionals working in nursing homes to improve their output and efficiency on the work floor due to budgetary constraints. In brief, as a consequence of Dutch government policies, the same amount of work has to be performed in a shorter amount of time by fewer people, and with the same or higher level of quality. This requires a well-structured division of time, without having time lost on trivial tasks such as retrieving items, which, in turn, may lead to a higher level of perceived stress. Technological solutions play an important role in improving the efficiency of care processes [4, 5, 6]. The SCHAT project (Smart Care Homes and Assistive Technologies) concerns the investigation of how location technologies can be utilized in the nursing home environment in order to address the problems of finding lost and misplaced items and monitoring the use of assistive devices.
1.2Real-time location systems
The Internet of Things (IoT) is making its appearance in the domain of healthcare, as objects as well as people can be connected to the Internet 24/7 and share data on all different sorts of variables. One of these variables is location. Information on the whereabouts of both assets and people can have many benefits for organizations [7]. Technologies that can track location indoors are commonly referred to as real-time location systems (RTLS) [8]. Healthcare is one of the major domains in which RTLS are applied. Other domains are retail, logistics and the automotive industry [8, 9]. A RTLS commonly exists of two hardware parts: tags on the one hand and location sensors on the other. Tags can be attached to the objects or people that are desired to be tracked. Location sensors are fixed beacons within a building. The transmission of information between location sensor and tag can then be translated to, for instance, a mark on a floor plan of the premises [9]. Real-time location systems are widely available from commercial providers, and within the domain of healthcare, vendors predominantly focus on solutions for hospitals [7]. Three main applications can be identified: tracking personnel, tracking patients and tracking assets [8, 10, 11].
1.3Challenges for design of technology for the nursing home
The literature on the use of RTLS in the healthcare domain points out that these systems are often inadequately integrated or poorly designed to accommodate to the specific requirements of a professional environment and the related stakeholders [11, 12]. Furthermore, these systems are often installed without careful consideration of the building’s specifications, policies and organizational cultures [11, 13]. Also accuracy and efficacy plays an important role in the acceptance of these systems [14]. These challenges, however, can also be recognized in other situations where new (information) technologies are integrated in a healthcare context [3]. Therefore, the results of the study described in this work can be expanded beyond the scope of RTLS and the realm of lost items in the nursing home, and also inform on issues and potential of technology in the nursing home in general, from the perspective of the healthcare professional. A nursing home provides an alternative place of residence where 24 hour care and assistance is offered by professional caregivers when people can no longer reside in their own home environment due to increasing need for assistance with activities of daily living, complex health care and nursing needs [15]. We define “lost items” as items of which the whereabouts are unknown, both short-term (misplaced) and long-term (missing/lost), and that require healthcare professionals to spend time looking for it. Also items that require healthcare professionals spending time finding the owner (for instance, glasses that are lying around) are included.
1.4Aim of the study
In this work we describe a study that aims to explore the context of losing items in the nursing home, as well as (latent) needs from the healthcare professional with regards to potential, technological solutions. The focus lies on the wishes and requirements from the healthcare professional, rather than the opportunities that the technology offers. This provides guidelines for the future design of technologies for the nursing home. The findings are, therefore, described in twofold: First, this study maps the causes and problems that are related to lost items in the nursing home from the perspective of healthcare professionals to answer the following: 1.) Which items tend to get lost? 2.) Whom or what causes the loss of these items? and 3.) What is the impact of losing these items? Second, the needs and wishes related to technology of the healthcare professional in the nursing home are investigated to answer the following: 4.) What are the needs of healthcare professionals with regard to technology in the nursing home? 5.) Is technology as a solution proportional to the impact of losing items? and 6.) Which additional opportunities for RTLS beyond track and trace can be identified?
2.Method
In order to be able to design solutions for the problems currently caused by losing items in nursing homes on the one hand, and taking into account the (latent) needs regarding technology use in nursing homes on the other hand, a participatory design approach [16] was applied in this study, in the form of a context mapping study.
2.1Participatory design research as a methodology
Participatory design research is a methodology that studies the tacit and latent knowledge of users [16, 17]. Participatory design methods often actively involve user in the front-end of the design process. This study was conducted in the early stages of the design process and aimed to involve the end-users as an expert and co-designer for the final design and therewith inspire and inform the research- and development team.
2.2Context mapping as a method
This study was conducted via a research method called context mapping [18, 19]. Context mapping is about documenting past experiences and create a desirable future experience from there. It makes use of generative tools that aid participants in telling their story [20]. The generative aspect of this method allows the participant to express their dreams and needs [17]. Context mapping has a very broad and explorative nature, and often explores the context beyond the research scope. This method was deliberately chosen to explore the impact of losing items, related to other problems in the nursing home and therewith identify the proportionality and additional opportunities for RTLS.
Traditionally context mapping consists of two phases for the participants: a sensitizing phase and a (group) workshop. The sensitizing phase is roughly based upon cultural probe studies [21] and mainly aims to get the participants in the right mind-set and sensitize them for the topic at hand, and hence prepare them for the second phase. This is usually done by handing out designed sensitizing packages and assignments prior to the workshop. These sensitizing exercises are usually not analyzed but merely serve to prime the participants [17].
The second phase consists of a workshop in which participants usually first get the opportunity to discuss the sensitizing phase, but second and foremost participate in one or multiple generative sessions. During these sessions the participant designs an artefact that aids and guides them in telling their stories and expressing thoughts and ideas to the other participants and researchers. It also helps them reflect on their own experiences. The researchers always prepare a toolkit prior to the start of the session in order to guide the participants in making the artefacts.
2.3Research environment and participants
A total of thirteen people took part in the study. The participants were selected to represent the broad scope of daily activities that take place in the nursing home environment. Gender was not taken into account during the selection process, due to the predominantly female workforce in Dutch nursing homes (92% of the staff members are female [22]). Informed consent was obtained from the participants by signing the given consent forms.
Table 1
Characteristics of the two participating nursing homes
| NH1 | NH2 | |
|---|---|---|
| Location | Urban, city centre | Rural, wooded area |
| Floors | 5 | 1 |
| Number of residents | About 110 | About 90 |
| Departments | Small-scale psychogeriatric ward, regular psychogeriatric ward, wards for people with physical limitations, assisted-living facility wings | Regular psychogeriatric wards, day care for people with Korsakov’s disease |
| Size of the organization | 8 out of 22 locations have nursing home capacity | 35 locations that offer nursing home care |
Figure 1.
One of the collages.
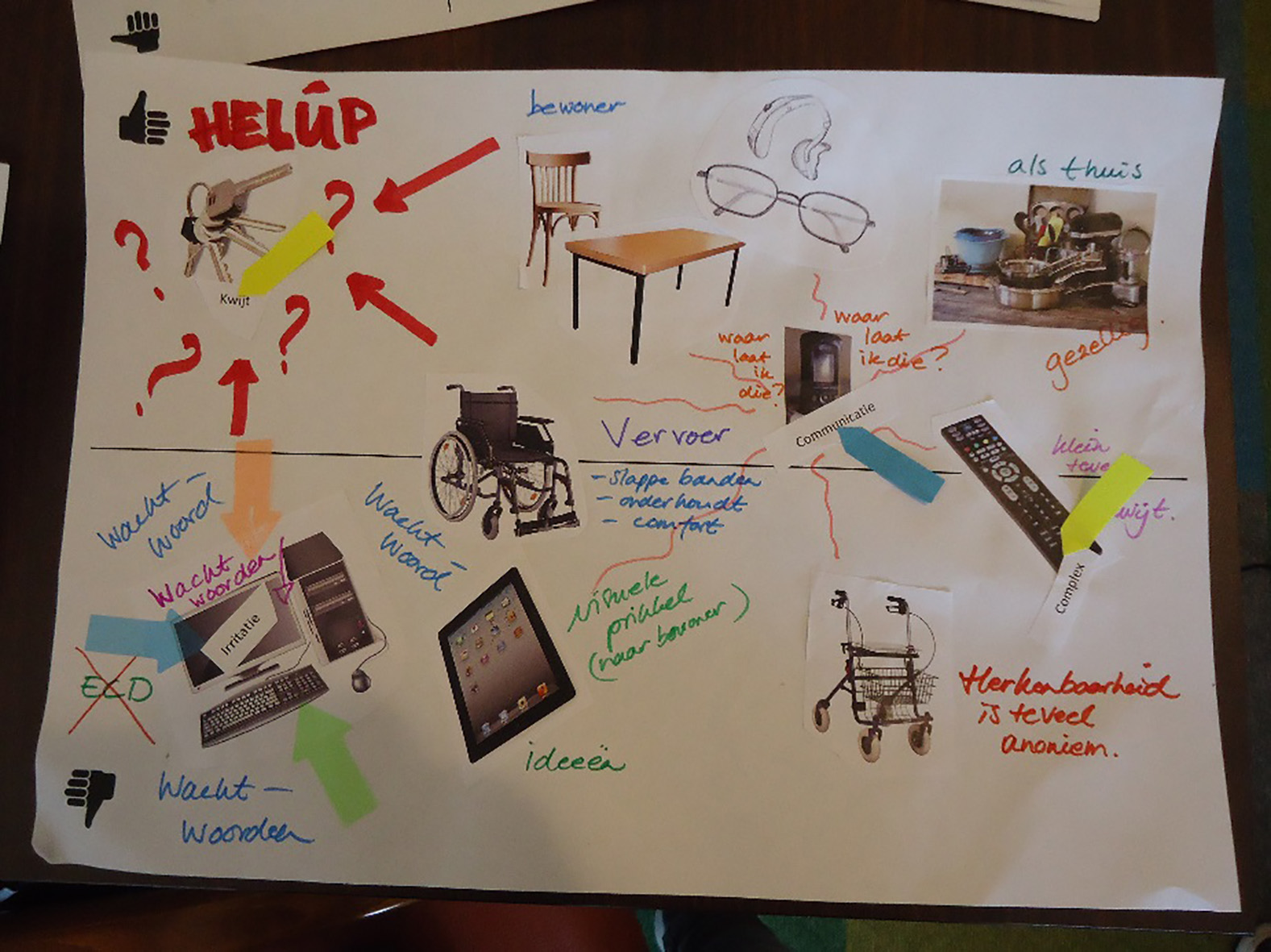
Figure 2.
First analysis of the findings on the wall.

Three workshops were conducted divided over two nursing homes. These two nursing homes will be further referred to as NH1 and NH2. The first session took place in NH 1 with a total of 4 participants. The second and third session took place in NH2 with respectively 4 and 5 participants. This adds up to a total of 13 participants (female
2.4Sensitizing phase
All participants were given sensitizing packages at least two weeks prior to the session, to be used during five shifts. The main components were a small diary, which was designed to be carried along during the shift, and a bigger workbook, which could be filled out during the reporting at the end of the day. Both booklets were similar to a journal, and were meant for documenting experiences that aimed to prime the user in the context of assets and the use of technology, but not specifically on lost items. The assignments in the workbook differed per day, one example is: “Draw the inside of a storage room in the nursing home and elaborate on what items are inside”. The smaller diary was designed to make notes of frustrations and solutions that were encountered during the day, which the users could later reflect upon. The sensitizing packages were not meant to be analyzed, but make the user aware of their context before entering the workshops.
2.5Workshops
Each of the three workshops was carried out via the same set-up and took 150 minutes. The workshops started with a general discussion of the sensitizing phase. After the discussion, the workshop was composed of two generative exercises. For both exercises a toolkit was designed by the researchers [20]. The workshops ended again with a general discussion. All the sessions were recorded on video and audio.
2.5.1Generative exercise 1: Making a collage
In this exercise the participants were asked to document their positive and negative experiences with regards to assets that can be found in the nursing home. They received a toolkit with a canvas, a set of images of assets in the nursing home, a list of words, coloured markers and indication stickers.
The assignment took twenty minutes and afterwards the participants presented their collages to each other and the researchers (examples of a collage: Fig. 1). The problems and opportunities related to the use of assets that came forward in the presentations were documented on the wall.
2.5.2Generative exercise 2: Making a mock-up
The problems and opportunities that were documented in the first exercise served as a basis for the second exercise. In this exercise the participants were asked to design a paper prototype of a piece of technology that addresses one of the problems or opportunities they encountered during the first exercise. The technology did not have to be feasible or realistic. The participants were presented with a new toolkit with, among other: blocks of wood, cardboard, paper, plastic cups, sticks, beads, buttons, drawing pins, glue, scissors and tape.
The participants designed a three-dimensional prototype to express their thoughts and make their design explicit. The exercise took thirty minutes and was followed by plenary presentations of the prototypes by the participants (Fig. 3). The participants were asked to respond upon one another. The results were discussed in the group and again documented on the wall.
Figure 3.
Some of the prototypes that were designed by the participants

2.5.3Analysis of the data
The recorded audio of the sessions was transcribed, and the collages and prototypes were collected for further analyses. For both assignments, the discussions were transcribed. From the transcriptions, illustrative quotes were selected in order to reflect typical statements related to the research topic. The body of data existed of quotes, pictures of the prototypes and the collages and was analysed twice, to prevent bias from a single researcher. During the first analysis “on the wall” (Fig. 2), part of data was coded and put into themes. In a second analysis, the main researcher conducted a more thorough analysis, coding all the data. The codes were then clustered into themes. Semantic as well as latent themes have derived from the data, describing the two different research directions. The data analysis followed the structure set out by Brown and Clarke [23] for qualitative research. The data concerning losing items in the nursing home led to a set of semantic (or explicit) themes and insights. The themes and insights concerning the use of technology were mainly latent (or implicit) in character.
3.Results
The results are described in two sections. In Findings 1, the themes that specifically relate to lost items are described. In Findings 2, themes are described that relate to technology in the nursing home on a more holistic level.
3.1Findings 1: Lost items
One of the objectives of the study was to get insight in the type of assets and objects that get lost in the nursing home, whom or what causes the loss of this objects and what the impact is, as perceived by the healthcare professionals.
3.1.1Which items tend to get lost?
From the study came forward which items tend to get lost in the nursing home, as described by the participants. The items are clustered into six themes. These themes are described below.
Portable items of healthcare professionals
All of the participants mentioned they carry around one or more items during their work routines. These items are predominantly keys, (smart) phones and digital enhanced cordless telecommunications (DECT) devices. The main cause of the loss of these items is that the care professionals left the items in one place while taking care of a care recipient. Often the items were left forgotten when leaving the room on the way to the next person.
Portable/worn items of inhabitants
This theme came to the fore in both nursing homes, but even stronger in NH2. Items that are worn by the residents of the nursing home tend to get lost. Often these items are critical for conducting activities of daily living, such as glasses, hearing aids and even dentures. Items get lost, misplaced or even thrown away, and are not always found back again.
Laundry of inhabitants
An often mentioned problem that is related to losing items, and which is a cause of much frustration with the participants, is the loss of laundry of residents. In NH1 the laundry is done by a commercial party, while at NH2 the laundry is done at the facility. However, participants from both NH1 and NH2 mentioned that laundry often gets lost.
Specialized and paired items
This theme came to the fore in NH2. Often specialized items come in pairs, for example an extra wide bed that is purchased together with an extra wide toilet chair. These items are often used together, for instance, for residents with obesity. However, a problem that regularly occurs is that pairs become separated and one of the items goes missing. Another example mentioned by one of the participants is a ball blanket: the location of the cover set that was purchased with it is often unknown. The participants identified a lack of dedicated storage for paired items.
Assets for general use – owned by nursing home
This theme encompasses objects that are owned by the nursing home, but not necessarily used by the employees of the nursing home only. Assets that are mentioned include wheelchairs for general use, remote controls for televisions and kitchen supplies. These items are used by the employees, the residents and even visitors. There are, thus, three groups of stakeholders that can play a role in items getting lost.
Medical and assistive devices
Medical or assistive devices are predominantly used by the healthcare professionals in daily routines. This theme came to the fore stronger in NH1 than in NH2. Participants of NH2 mentioned only the relatively small assets, such as the thermometer and sphygmomanometer. In NH1, larger medical and assistive assets were lost as well, such as the mobile hoists, concentrators and medicine carts. Also the smaller devices were more often mentioned than by the participants of NH2. The layout of the building (single floor versus multi-floor) plays a role in the loss of oversight where these items are.
3.1.2What or who causes the loss of items?
In the section below is described whom or what causes the loss of items. Eight themes have derived from the analysis. For each theme a short description is given, and related to the type of items that are affected by the mentioned cause. Furthermore, whenever applicable, it is described in which of the two nursing homes the theme was more or even solely evident.
Not putting items on a dedicated storage place
Some items have a dedicated storage place. These items are assets that are mainly used by the healthcare professionals. The main cause of the loss of these items is the fact that these are not put back on their dedicated storage location. This is often caused by a high work pressure or by a lack of time or disregard.
Portability
A theme found in both nursing homes, which was more outspoken in NH1, are the difficulties regarding the portability of items. The items predominantly mentioned are keys and phones. These items often remain in the room of a resident after the care professional is done taking care. The problems regarding the portability of these items are partly attributed to the absence of work clothing or practical uniforms with pockets. Both nursing homes strive to maintain a homelike atmosphere and, therefore, the employees are not required to wear a vest. However, everyday clothing does not always have a sufficient amount of pockets-of sufficient size-available to carry around the items.
Recognisability
For some misplaced items in the nursing that are found by someone else than the owner or user, the problem arises that the items are not recognised, marked or labelled, in order to trace them back to their owner. These items include abandoned wheeled walkers and clothing/laundry that is returned after washing. Often, caregivers add either labels or other recognizable objects like fake flowers to these items. However, in practice this proves not to be sufficient as labels drop off, let loose, or names are not recognized.
Shared assets
Some of the more specialized items (such as extra wide beds) may be purchased by the organization and then shared between different nursing home locations of the same organization in order to cut costs. This problem was only identified among the participants of NH1. The main issue with shared assets is that the lent items are too often not properly documented, which causes confusion as to which item is in which nursing home, and whether it is in use or not. Improvements to the logistics of the nursing home is mentioned as a likely solution.
Third parties
Employees and residents are not the only people in the nursing home. Both in NH1 and NH2 volunteers, families and other visitors share the space. These third parties often are not aware of any regulation that may exist as to where to return items. One example that comes from NH2 is a number of wheelchairs that were purchased for general use, for instance, for visiting the church service on Sunday or for a walk outside. These wheelchairs are often picked up by family but not returned to the dedicated location, which gives the employees of the nursing home extra work in retrieving the lost wheelchairs.
Residents
A large part of the residents of both nursing homes have a psychogeriatric background, including dementia-associated memory loss. In addition to memory loss, symptoms as hoarding behaviour may occur among the resident population. This often results in a loss of personal items of the inhabitants. These items can be of practical use, such as glasses, hearing aids and dentures, or have an emotional value, like jewellery and picture frames. It usually a task of the health care professional to retrieve these items once lost.
Usage by multiple persons
Most of the medical and assistive assets are used by multiple groups of people, both the relatively stationary assets such as a mobile patient hoist as well as portable assets such as a shared set of keys. This leads to two problems in practice. In the case of larger items, the item may not be in its dedicated spot when it is needed by another employee. In the case of a portable item, there are two challenges. There is the challenge of finding out which person carries the item on that moment, and also where that person is. Both NH1 and NH2 use portable phones for employees to contact their colleagues in these scenarios.
No dedicated storage place
The last theme related to the availability of storage space. Some items in the nursing home do not have an dedicated storage place, but this mainly concerned specialized items that are infrequently used or items that are almost constantly in use (like a patient hoist). An example that was mentioned by one of the participants was a newly-bought pillow. One of the employees had decided that storing the pillow in the office was most logical, however, the pillow was only found back several months later.
3.1.3What is the magnitude and impact of lost items in the nursing homes?
The qualitative nature of the current study does not allow for making a precise assumption of the magnitude of lost items in the nursing home. However, from the results it became apparent that (1) in the two nursing homes the range of objects that gets lost, though they overlap in some places, are different and (2) the impact and magnitude of the problem differs per nursing home, but also per ward and per healthcare professional. The prototypes proved to be very informative on the impact lost items have on the staff in relation to other problems they experience. It appeared that, although the issue of lost items was addressed in a number of the prototypes, this was hardly the main focus. However, many of the devices designed were designed to alleviate in secondary tasks and therewith improve efficiency in non-care related processes (See: Section 3.2.1.)
Regarding the impact of lost items, first of all an important factor is that time that is spent looking for- and retrieving items is time that cannot be spent on care. The healthcare professionals in both nursing home expressed an added pressure to their already busy schedule. This can result in stress during workhours and even working overtime. Furthermore it can evoke annoyance and irritations that are sometimes involuntarily transferred to colleagues and clients. The participants expressed that having to look for items makes them feel guilty towards their clients, especially when these clients experience discomfort through the situation. Discomfort can be having to wait (for instance, waiting for a patient hoist to arrive) or not being able to communicate properly because they are without dentures, glasses or hearing aids. Some of the participants mentioned that they find it much worse when belongings of a client are lost than when practical (and therewith relatively easily replaceable) assets of the nursing home are lost. Finally, having to look for misplaced items can be privacy-infringing from the professional perspective, as often they have to search in the different rooms of the clients.
3.2Findings 2: Technology in the nursing home
In the second part of the findings, five themes related to technology in the nursing home are described. These themes mostly derived from latent knowledge of the participants, and the results of the second exercise the participants participated in. During this exercise, the participants prototyped a technology to tackle one of the challenges that derived from the first workshop.
3.2.1Efficiency in non-care related processes
From the sessions came forward that healthcare professionals see care-related tasks as their number one priority. However, in their daily array of activities also tasks that are not directly related to care – such as answering e-mails, doing laundry and filling out patient files/records – are included. Not being able to spend their time on care is frustrating for the healthcare professionals. Therefore, they prefer these tasks to be as efficient as possible.
3.2.2Information at hand
This theme is also related to efficiency, but more specific. A big point of frustration for the healthcare professionals, as came to the fore during the workshops, is needing to resort to stationary technology as the main source of information. In both NH1 and NH2 the healthcare professionals made use of desktop computers. This implies the healthcare professionals are obliged to go back to these desktop computers, whenever they require information about their clients. Moreover, both NH1 and NH2 use motion sensors around the beds of some of their clients, to be alerted whenever somebody falls out of their bed. These motion sensors often give falls alarms, and these signals come in on the DECTs. Every alarm has to be checked by the nurse, however many checks are obsolete.
3.2.3Automation
Technology has the potential to automate many different processes, operations and actions. One of the themes that is found around technology in the nursing home is automation. This theme covers different contexts and processes. In essence it comprises the wish to apply technology as a tool that takes away trivial labour from the healthcare professional. Examples that are mentioned are opening closets and drawers in the kitchen automatically when the professional stands close (so without the hassle of using keys) and (semi-)automatically register the inventory of the storeroom.
3.2.4Integration of technology
This theme covers both digital as tangible integration. Technological possibilities are growing, and this shows in the nursing home by the number of systems and appliances healthcare professionals work with on a daily base. Many of these systems are self-contained, which implies that with every new system that is deployed, the healthcare professionals have to learn new functions and a new interface. Furthermore, wishes were expressed to let these systems communicate more easily with one another, as often the same data has to be entered in different applications. In addition to the digital integration of systems, the participants proposed physical integration of devices. For example, having one portable appliance that contains client information, different applications and the functionality of the DECT devices, but also can replace the keys.
3.2.5Portability
Healthcare professionals often carry a number of items with them during their work, for example keys or a phone. This is one of the bigger causes for losing and spending time searching for items. Both in NH1 and NH2 the participants expressed to value a homelike environment for their residents, which implies that they try to refrain from wearing medical uniforms as much as possible. However, often their own outfits do not have pockets large enough to hold all the different items they are carrying. This results in manually carrying the items and placing them in the room of the clients when they are helping them, and forgetting to take them when they move on.
4.Discussion
In the following sections we discuss the limitations of this study, the relationship of the research outcomes to the two particular nursing homes contexts, findings of previous research and future work.
4.1Strengths and limitations of the method
Generative techniques are relatively new to the field of qualitative research in the domain of healthcare. In this study the method is especially valuable as it provides design guidelines as well as a holistic view on the context, from the perspective of healthcare professionals. The advantage of using generative techniques is that the participants can tell stories based on the visual cues of the artefacts made during the sessions, which are a direct result of their own experiences before and during the workshop and are supplemented by reflection on these experiences and discussions held with other participants. This allows the participant to contemplate their experiences and stories twice. However, it also makes for a lot of excess information, not necessarily relevant to the topic at hand.
Therefore, the results do not provide an in-depth and exhaustive overview of the problem at hand, but they provide a starting point for further research and initial design guidelines for a potential solution. The methodology itself does not require ‘creative talents’ among the participants, even though they have to create an artefact during the session. All participants were given the opportunity to shape and share their private beliefs and thoughts, before engaging into the group discussion, which is a strength of the generative approach. Furthermore, due to the qualitative nature, this study did not provide any quantifiable data regarding lost items, and it did not provide insight into the frequency of items getting lost or in how much time is spent by personnel looking for items. The chosen method suited most of the defined research questions well, but failed to describe a quantifiable impact and therewith answer the question whether RTLS technology is a solution proportional to the problem.
The sensitizing packages were designed to not take too much of the participants time, taking in regard their busy daily schedules. However, the packages were only used by a few participants, and most of these were not even completed. The researchers had overestimated the time and dedication the participants would have for this study. For future studies it would be good to do a more extensive pilot with the sensitizing packages in context, or work with a method to prime participants during the start of the workshop instead of on forehand.
4.2Relations of the findings to the nursing home organisation
Three sessions were conducted in two different nursing homes, administered by two different care organisations. The results of study showed that the type of objects that get lost and the causes objects get lost differ for the two nursing homes, and that is why there are distinct differences between the themes that come to the fore in both nursing homes. Medical and assistive assets, such as patient hoists and blood pressure meters, were discussed in more depth during the workshop in NH1 than in the workshops in NH2. The building types of NH1 and NH2 have strong differences in size and layout; NH2 is a single-floor pavilion-like building, and NH1 consists of five floors. Sometimes assets are shared between care professionals working on different floors of NH1. This suggests that the layout of a nursing home building influences the likelihood of objects getting lost. NH2 shares specialized assets including posey-beds with other nursing homes of the same organisation, which is another major cause of the more expensive items getting lost. Part of it is due to improper registration of lent out assets by the nursing home staff. This also shows that the structure and logistics of the organization have an impact on the causes of losing items. Concluding that the findings are not identical for the two participating nursing homes, each of the set of problems encountered in the two nursing homes may require a different approach to a technological solution. Therefore, the technologies cannot be fully identical. If a system is to be developed and installed in a nursing home in order to track and trace (lost) objects, the specific requirements should be evaluated individually per nursing home.
4.3Relations of the findings to the scope of the project
This study was conducted in the context of applying track and trace technologies in the nursing home environment in order to retrieve lost items and to monitor the use of assistive devices for maintenance purposes. The explorative nature of the method provided information beyond the scope of the project. One of the objectives of the current study was to identify future applications of this technology that could address (latent) needs coming to the fore during these workshops. A great opportunity lies in using location technology to make more processes in the nursing home more efficient, such as automatically opening (locked) doors and cabinets when a nurse is nearby. Nursing staff often carry around large sets of keys to open the doors of closed wards, medicine cabinets, and cupboards and drawers.
Efficiency on the work floor was a main theme in the results of this study. If time can be saved on retrieving lost and misplaced items, more time can be spent on the essential care processes and giving attention to the residents. This suggests that RTLS are indeed a desired, albeit latent, solution for addressing certain problems in the nursing home. However, the findings provide a set of design and implementation requirements for such systems. New RTLS need to be integrated with existing systems (rather than being an addition), both from a digital and a physical perspective. Staff do not wish to carry around more portable devices or learn to master new technologies that come on top of the existing set of assistive technologies, computer stations and DECT devices. In addition, technology needs to match with the needs and professional values of care professionals, which are mainly focussed on the quality of the provision of care and spending time with residents [5].
4.4Future research
This study provides a first insight into how sensor-based systems and information technologies like RTLS can be applied in the nursing home from perspective of end-users. It became apparent that problems related to lost items are not congruent across different nursing homes. This may suggest that individual in-depth studies need to be performed for each nursing home that wishes to implement RTLS, as the requirements also influences the choice of specific technologies. When the nursing home organization wishes to monitor the location of smaller items like dentures and keys that get lost, this requires an approach to technology produces more precise outcomes than when monitoring mainly larger items like hoists which are easier to see from a distance and do not get lost when thrown away or falling in between the cushions of a sofa. Current RTLS technologies are not small enough to provide a solution to track and trace smaller but essential items such as glasses and dentures. Furthermore, this study did not produce any quantifiable information regarding how much time is spent on retrieving lost items and the financial consequences of searching for items and replacing them. In future studies topics concerning privacy and ethics should also be addressed, as well as multi-stakeholder perspective.
5.Conclusions
Losing items in the nursing home, and not being able to (re)find these items is a real challenge in Dutch nursing homes. The scale of the problem and the types of items that get lost differ between the nursing home organizations, and even between the facilities within a particular nursing home organization. This implies that the organizational culture and building typology may play a role in losing items. The findings show that for the design of a track and trace system, no set list of items that are at risk of being lost and misplaced can be defined. A to-be-designed system should therefore be customizable per nursing home. Furthermore many different causes for losing items can be identified, of which some can be solved by establishing better organizational protocols (for example, giving items a dedicated storage place). Therefore it may also differ per nursing home whether applying complex technological systems is proportional to the encountered problems. It is clear that losing items has an impact on the healthcare professionals in their daily routines and efficiency, but at the same time it is one of many problems, challenges and trivial tasks that keep healthcare professionals from spending their time on actual care. The participants in this study have indicated that RTLS can provide a solution to some of the challenges they encounter on the work floor, but that the implementation of new technologies should be done with care and should be integrated into existing systems in order to prevent additional training and being a burden to the workload. Respecting these notions can help technology suppliers of RTLS to better fit their products to the actual needs of nursing home staff. It may also lead to the conclusion that sensor-based systems are not a panacea to all challenges encountered in the nursing home practice.
Acknowledgments
This study was funded by RAAK (Regional Atten- tion and Action for Knowledge circulation) scheme, which is managed by the Foundation Innovation Alliance (SIA – Stichting Innovatie Alliantie) (SIA project number 2015-02-24M, Project SCHAT – Smart Care Homes and Assistive Technologies). We would like to thank all participants of the sessions at the nursing home organizations for their willingness to participate and share their views.
Conflict of interest
None to report.
References
[1] | van Hoof J., Douven B., Janssen B.M., Bosems W.P.H., Oude Weernink C.E., Vossen M.B. ((2016) ) Losing items in the psychogeriatric nursing home: the perspective of residents and their informal caregivers. Gerontology and Geriatric Medicine 2: : 1-9. doi: 10.1177/2333721416669895. |
[2] | Galasko D., Bennett D., Sano M., Ernesto C., Thomas R., Grundman M., Ferris S. ((1997) ) An inventory to assess activities of daily living for clinical trials in Alzheimer’s disease. Alzheimer Disease and Associated Disorders 11: (Supplement 2): S33-S39. |
[3] | Galasko D. ((1998) ) An integrated approach to the management of Alzheimer’s disease: Assessing cognition, function and behaviour. European Journal of Neurology 5: (Supplement 4): S9-S17. |
[4] | van Hoof J., Wetzels M.H., Dooremalen A.M.C., Wouters E.J.M., Nieboer M.E., Sponselee A.A.M., Eyck A.M.E., van Gorkom P.J.L.M., Zwerts-Verhelst E.L.M., Peek S.T.M., Vissers-Luijcks C., van der Voort C.S., Moonen M.J.G.A., van de Vrande H.A., van Dijck-Heinen C.J.M.L., Raijmakers T.E., Oude Weernink C.E., Paricharak N., Hoedemakers C.G.J.J., Woudstra J.M.M., van der Voort L., van de Werff T.C.F., van der Putten B., Overdiep R.A. ((2014) ) Technological and architectural solutions for Dutch nursing homes: results of a multidisciplinary mind mapping session with professional stakeholders. Technology in Society 36: : 1-12. http://dx.doi.org/10.1016/j.techsoc.2013.12.001. |
[5] | Nieboer M.E., van Hoof J., van Hout A.M., Aarts S., Wouters E.J.M. ((2014) ) Professional values, technology and future health care: The view of health care professionals in The Netherlands. Technology in Society 39: : 10-17. doi: 10.1016/j.techsoc.2014.05.003. |
[6] | van Dijck-Heinen C.J.M.L., Weffers H.T.G., Overdiep R.A., Aarts S., Vissers-Luijcks C., Wouters E.J.M. ((2014) ) The essential elements for a nursing home according to stakeholders from healthcare and technology. Perspectives from multiple simultaneous monodisciplinary workshops. Journal of Housing for the Elderly 28: (4): 329-356. doi: 10.1080/02763893.2014.930365. |
[7] | Krohn R. ((2008) ) The optimal RTLS solution for hospitals. Breaking through a complex environment. Journal of Healthcare Information Management 22: (4): 14-15. |
[8] | Oude Weernink C.E., van Hoof J., Felix E., Verkuijlen P.J.E.M., Dierick-van Daele A.T.M., Vossen M.B. Real-time location systems for nursing homes and nursing home care: an exploratory study of future applications. |
[9] | Malik A. ((2009) ) RTLS for Dummies. Wiley Publishing, Hoboken, NJ, USA. ISBN 978-0-470-39868-5. |
[10] | Fosso Wamba S., Anand A., Carter L. ((2013) ) A literature review of RFID-enabled healthcare applications and issues. International Journal of Information Management 33: (5): 875-891. http://doi.org/10.1016/j.ijinfomgt.2013.07.005. |
[11] | Fisher J.A., Monahan T. ((2012) ) Evaluation of real-time location systems in their hospital contexts. International Journal of Medical Informatics 81: (10): 705-712. http://doi.org/10.1016/j.ijmedinf.2012.07.001. |
[12] | Kamel Boulos M.N., Berry G. ((2012) ) Real-time locating systems (RTLS) in healthcare: a condensed primer. International Journal of Health Geographics 11: : 25. http://doi.org/10.1186/1476-072X-11-25. |
[13] | Bowen M.E., Wingrave C.A., Klanchar A., Craighead J. ((2013) ) Tracking technology: Lessons learned in two health care sites. Technology and Health Care 21: (3): 191-197. http://doi.org/10.3233/THC-130738. |
[14] | Okoniewska B., Graham A., Gavrilova M., Wah D., Gilgen J., Coke J., Ghali W.A. ((2012) ) Multidimensional evaluation of a radio frequency identification wi-fi location tracking system in an acute-care hospital setting. Journal of the American Medical Informatics Association 19: (4): 674-679. http://doi.org/10.1136/amiajnl-2011-000560. |
[15] | Sanford A.M., Orrell M., Tolson D., Abbatecola A.M., Arai H., Bauer J.M. ((2015) ) An international definition for “Nursing home”. Journal of the American Medical Directors Association 16: (3): 181-184. |
[16] | Spinuzzi C. ((2004) ) The Methodology of Participatory Design. Technical Communication 52: (2): 163-174. |
[17] | Sanders E., Stappers P., Convivial toolbox, BIS publishers. ((2012) ) Amsterdam. |
[18] | Sleeswijk Visser F., Stappers P.J., van der Lugt R., Sanders E.B.N. ((2005) ) Contextmapping: Experiences from practice. CoDesign 1: (2): 119-149. |
[19] | Elizabeth B.-N. Sanders & Pieter Jan Stappers. ((2014) ) Probes, toolkits and prototypes: three approaches to making in codesigning. CoDesign 10: (1): 5-14. |
[20] | Stappers P.J., Sanders E.B.-N. ((2003) ) Generative Tools for Contextmapping: Tuning the Tools. Third International Conference on Design & Emotion, Loughborough, Taylor & Francis. |
[21] | Gaver B., Dunne T., Pacenti E. ((2009) ) Design: Cultural probes. Interactions 6: (1): 21-29. |
[22] | Leijten R., van Gerven H., Post F. ((2015) ) Het personeel van de verpleeghuizen en verzorgingshuizen aan het woord https://www.sp.nl/sites/default/files/verpleeghuizennota2015.pdf, last retrieved March 2017 [in Dutch]. |
[23] | Braun V., Clarke V. ((2006) ) Using thematic analysis in psychology. Qualitative Research in Psychology 3: (2): 77-101. |




