Chronic diarrhoea in older adults and the role of dietary interventions
Abstract
Chronic diarrhoea affects up to 10% of older adults, impacts quality of life and has potential adverse medical outcomes. Dietary changes can be effective but, if not managed correctly, could negatively impact health. This review summarises the prevalence, potential causes, and complications of chronic diarrhoea in older people. The evidence for dietary treatments, and the nutritional implications, are described.
1Introduction
Chronic diarrhoea can be disabling for older people. It may impede social interactions, impact adversely on confidence yet is a health problem that is the subject of limited research. The number of adults worldwide 65 years and older is expected to double with the global proportion increasing from 9.3% in 2020 to 16% by 2050. The projected life expectancy post 65 years has increased from 17 years in 2015–2020 to 19 years by 2045–2050, especially in Central and South Easter Asian and South American countries [1]. With greater life expectancy, we also expect continuing quality of life (QOL). Unfortunately, almost all diseases impact unfavourably on quality of life, and this is especially the case for older adults experiencing chronic diarrhoea [2]. In addition to medical therapies, chronic diarrhoea may also be responsive to dietary interventions. This review outlines causes of chronic diarrhoea in older adults with a view to raising awareness of dietary interventions that might be considered.
2Defining and classifying chronic diarrhoea
The British Society of Gastroenterology (BSG) defines chronic diarrhoea based on stool consistency and frequency [3] (Table 1). Irritable bowel syndrome (IBS) and functional diarrhoea are two types of chronic diarrhoea, defined by the Rome Criteria IV (Table 1). The term functional diarrhoea is used to describe chronic diarrhoea once all other gut-related disorders, such as coeliac disease, inflammatory bowel disease, microscopic colitis, colorectal cancer or diverticulitis, have been ruled out [4].
Table 1
Criteria for chronic diarrhoea; British Society of Gastroenterology, Rome IV criteria for irritable bowel syndrome and functional diarrhoea
| BSG guidelines for the investigation of | Rome IV criteria for Irritable bowel | Rome IV criteria for functional diarrhoea |
| chronic diarrhoea in adults | syndrome –Diarrhoea and Mixed | |
| Duration of more than 4 weeks | Duration of more than three months | Duration of more than three months. |
| Increased stool frequency Stool consistency between types 5–7 on the Bristol stool chart | 1. Defecation 2. Change in stool frequency 3. Change in stool form | Loose or watery stools at least 25% of the time |
| Persistent alteration from normal stool consistency | Abdominal pain on average at least 1 day/week in the last 3 months that is associated with at least 2 of the following | Not usually associated with pain |
Although chronic diarrhoea is a risk factor for the development of faecal incontinence, the two are not synonymous. Faecal incontinence is defined by the involuntary loss of sphincteric control [5]. While chronic diarrhoea may be associated with urgency and incontinence, this is more likely due to the volume and liquid consistency of stool in the rectum rather than to the involuntary loss of sphincteric control.
3Prevalence of chronic diarrhoea in older adults
The prevalence of chronic diarrhoea is difficult to determine due to variations in its definition and diagnostic criteria, as illustrated in Table 2. Furthermore, patients have different interpretations of what diarrhoea comprises. A UK prevalence study of 596 older adults living in the community found that 10% experienced functional diarrhoea, as defined by the Rome III criteria, but only 1% considered that they had diarrhoea [6]. A recent global study conducted by the Rome Foundation surveyed over 73 000 individuals in 33 countries [7]. The pooled prevalence of functional diarrhoea and IBS in older adults (>65 years) was 4.1% and 1.7%, respectively. The prevalence of chronic diarrhoea was similar for younger age groups 4.6% (18–39 year olds) and 5.1% (40–64 year olds). However, rates of IBS were much lower in older adults compared to the younger adults.
Table 2
Prevalence of chronic diarrhoea in older adults
| Author | County | Age | Criteria | Prevalence (%) |
| Talley [90] 1992 | United States of America | 65 + n = 328 | Loose or water stools and/or stool frequency was more than three stools per day | 14.2 |
| Drossman [91] 1993 | United States of America | 45 + n = 5430 | Not specified | 1.8 |
| O’Keefe [2] 1995 | United States of America | 65 + n = 704 | 1. The passage of more than three stools a day and or2. The passage of loose or watery stools, often in the past year. | 19.2 |
| Zhao [92] 2019 | China | 60 + n = 688 | Gastrointestinal symptoms rating scale (GSRS) | 34.7 |
| Singh[28] 2018 | United States of America | 60–69 n = 712 70 + n = 676 | Bowel health questionnaire Bristol Stool Chart Type 6 or 7 plus stool frequency of > 21 bowel movements per week | 9.7 9.6 |
| Chaplin [6] 2000 | England | 65 + n = 596 | Rome II | 10 |
| Sperber [7] 2020 | Worldwide (23 countries) | 65+ n = 8843 | Rome IV | 4.1 |
In older adults there are a number of confounding factors to consider when determining the prevalence of chronic diarrhoea. The self-reported prevalence may be lower due to age related memory decline, leading to problems with recall [8]. Furthermore, older adults with chronic diarrhoea are less likely to seek medical advice for digestive symptoms unless they have alarm symptoms such as blood in the stools [9]. Finally, abdominal symptoms could be reduced in older adults due to reduced gut pain perception with age [10].
4Common causes of chronic diarrhoea in older adults
Common causes of chronic diarrhoea in older adults are shown in Table 3. Chronic diarrhoea is a symptom that requires careful assessment, particularly if occurring for the first time in older adults. Older adults are at the greatest risk of colorectal cancer, diverticular disease, radiation enteritis, ischaemic colitis and microscopic colitis [11]. Therefore, a thorough history and examination are required to determine if chronic diarrhoea is due to reversible underlying pathology. There should be a low threshold for further investigations to exclude such pathology.
Table 3
Common causes of chronic diarrhoea in older adults (11, 14)
| Organic causes |
| Colorectal cancer |
| Clostridium difficile |
| Diverticular disease |
| Inflammatory bowel diseases |
| Ischaemic colitis |
| Microscopic colitis |
| Radiation enteritis |
| Medication related |
| Magnesium |
| Laxatives |
| Non-steroidal anti-inflammatory drugs |
| Lithium |
| Polypharmacy –more than five medications |
| Diet-responsive |
| Irritable bowel syndrome |
| Coeliac disease |
| Small intestinal bacterial overgrowth |
| Bile acid diarrhoea |
| Pancreatic insufficiency |
| Sucrase-isomaltase deficiency |
| Lactose intolerance |
Many prescribed or over the counter medications can cause diarrhoea; this has been thoroughly reviewed elsewhere [12]. Many of these medications are also commonly prescribed to older adults, such as proton pump inhibitors, magnesium supplements and non-steroidal anti-inflammatory drugs. Laxatives are often prescribed to older adults, and overuse of these, or continued use without requirement, may also lead to diarrhoea. In addition to the side effects of individual medications, polypharmacy, defined as taking more than five medications, is associated with an increased prevalence of diarrhoea [13, 14] and is more common in older adults [11].
Diagnosing and managing chronic diarrhoea in older adults can be more difficult due to other chronic comorbidities, the impact of polypharmacy and a possible decline in cognition. Due to the number of adverse consequences associated with chronic diarrhoea, investigations into possible causes are vital for preserving life quality and managing potential consequences.
5Consequences and complications of chronic diarrhoea in older adults
Chronic diarrhoea is associated with nutritional consequences. Suboptimal dietary intake, especially for protein, calcium and folate, has been found in older adults with chronic diarrhoea [15]. Requirements for protein, calcium, vitamin B12 and vitamin D are greater in older compared with younger adults. Avoidance of foods suspected to trigger diarrhoea can lead to macro- and micro-nutrient deficiencies and subsequently malnutrition [16] (Table 4). Malnutrition is common among older adults, with half of community older adults malnourished or at risk of malnutrition [17] and almost 50% of older adults entering residential care facilities are already malnourished [18]. Malnourished older adults are more likely to be admitted to hospital, and hospital admissions are likely to be longer than at risk or nourished older adults [17].
Table 4
Consequences that may arise from chronic diarrhoea and risk factors associated with dietary interventions
| Consequences arising from chronic diarrhoea in older adults and poorly managed dietary interventions | ||
| Risk factor | Related to | Consequence |
| Reduced oral intake | Overly restricting foods and food groups to manage symptoms | Malnutrition Risk of disordered eating patterns such as ARFID |
| Osteoporosis | Undiagnosed coeliac disease or overly restricting dairy products to manage symptoms of IBS or lactose intolerance | Increased risk of fracture or breaking of bones |
| Anaemia | Undiagnosed coeliac disease or overly restricting fruit and vegetables in the elimination phases of the low FODMAP or sucrase-isomaltase deficiency diets. | Low energy, shortness of breath, headaches |
| Increased falls risk | Increased frequency and urgency of toilet visits, especially for frail older adults | Increased risk of fracture |
| Reduced skin integrity | Skin breaking down from frequent bowel motions | Increased risk of the development of pressure areas or ulcers |
| Reduction of the gut microbiome diversity | Reductions in fibre content of the diet while following a low FODMAP or low sucrase-isomaltase diet | Changes in numbers of bacteria associated with the production of short chain fatty acids required for overall gut health and overall body health |
| Reduction in QOL | Stress and anxiety regarding increased bowel frequency, exacerbated while following restrictive elimination diets. | Limiting activities of daily living Increased risk of anxiety and depression |
Undiagnosed causes of chronic diarrhoea, such as coeliac disease, may also lead to osteoporosis and anaemia. Any of these conditions could place older adults, especially frail older adults, at increased risk of falls and subsequent risk of fractures, exacerbated if lactose or dairy products are reduced or avoided. Frail older adults are more likely to have reduced independence and experience worse health outcomes than non-frail older adults [19]. The addition of chronic diarrhoea to their frailty could, for some, be enough to tip the balance from independence to dependence. For those frail older adults who are bed bound, frequent bowel motions may reduce skin integrity increasing risk of pressure ulcer development.
The gut microbiome changes are we age [20]. Older adults are at greater risk of reduced diversity of the gut microbiome. Reduction in some microbes, such as Prevotellaceae, and an increase of other types of bacteria such as Enterobacteriaceae, have been observed in centenarians [21] and older adults with frailty [22]. Faecalibacterium prausnitzii, one of the species of butyrate producing bacteria essential in maintaining the integrity of the colon, has also been found to be reduced in frail older adults [23]. Changes in the microbiome can be associated with changes in diet. Claesson et al. found that when older adutls moved into residential care a change to a lower fibre diet occurred, and this was associated with a difference in the microbiome profiles and also increased frality compared to older adults living independently. The changes in their microbiome occurred within a year, with a reduction in short-chain fatty acids (SCFA) butyrate, acetate and propionate observed [23]. SCFAs are important for maintaining the integrity of the gastrointestinal mucosa and immune system, as well as having a role in maintaining the pH of the colon, glucose homeostasis and appetite regulation [24]. Microbial diversity and production of SCFAs increase when dietary fibre is increased, especially if those diets are also high in fruit, vegetables and legumes, such as the Mediterranean diet [25]. Changing to a Mediterranean style diet is associated with improved overall cognitive and functional outcomes in older adults [26]. Thus, changes in diet to manage chronic diarrhoea, especially if reducing dietary fibre, may exacerbate or accelerate gut microbial changes.
Quality of life for both younger and older people with chronic diarrhoea is significantly affected [2, 13]. Older adults with diarrhoea are reported to have lower social functioning and mental health scores in a medical outcomes general health survey (MOS) than older adults without any gastrointestinal concerns [2]. Proximity to a toilet and ease of access is also likely to impact social life. For older adults, this may mean that they are less likely to socialise. The relationship between the gut and mental health is well documented. Up to 75% of patients with IBS experience anxiety and depression [27], and chronic diarrhoea is commonly associated with individuals suffering from depression [27, 28]. What is unknown is if gut symptoms lead to anxiety and depression or being anxious or depressed causes gut symptoms
6Examples of dietary treatments to manage chronic diarrhoea in older adults
After appropriate investigations do not reveal an alternative cause, dietary manipulation may be warranted. The following section describes causes of chronic diarrhoea in older adults where expert dietary changes can add value to the management of these conditions.
6.1Irritable Bowel Syndrome
IBS, known as a disorder of gut-brain interaction, is characterised by abdominal pain. Diarrhoea is a symptom of some types of IBS; diarrhoea predominant (IBS–D), mixed (IBS–M), where individuals can experience both diarrhoea and constipation, unspecified (IBS-U) if the person does not meet the criteria for either constipation or diarrhoea and has periods of no symptoms and post infective IBS after exposure to gastroenteritis. IBS may result from multiple causes such as motility disturbances, visceral hypersensitivity or changes to the gut microbiome [29]. The reported prevalence of IBS in older adults varies greatly (Table 5). Studies using the Rome Criteria III and IV to diagnose IBS mostly report lower prevalence, except for a Japanese study, suggesting that geographical and cultural differences may impact IBS rates. The Rome Foundation Global study [7] found 50% lower prevalence rates when using the Rome IV criteria compared to the Rome III criteria, likely reflecting changes in criteria specificity. For example, the prevalence of IBS in a Russian study using the Rome III compared to the Rome IV criteria reduced from 16.5% to 5.9%. The evidence is conflicting as to whether the prevalence of IBS is greater [13, 28, 30] or lesser [31, 32] for older adults compared to younger adults. This is also likely due to different criteria used and geographical differences; America, Iran, Japan and China (Table 5).
Table 5
The prevalence of irritable bowel syndrome in older adults
| Prevalence of irritable bowel syndrome in older adults | ||||
| Author | County | Age | Criteria | Prevalence (%) |
| Talley et al. [90] 1992 | United States of America | 65 + | Manning | 11 |
| Drossman [91] 1993 | United States of America | 45+ | Not specified | 9.4 |
| Kay et al. [8] 1994 | Denmark | 70+ | At least two of the following: A) Abdominal pain B) Distension or borborygmi C) Altering stool consistency | Female –12.3 Male –6.1 |
| O’Keefe et al. [2] 1995 | United States of America | 65–98 | Manning | 17.1 |
| Minocha et al. [93] 2006 | United States of America | 50+ | Rome II | 7.6 |
| Matsumoto et al. [32] 2013 | Japan | 60+ | Rome III | 9.3 |
| Zhao et al. [13] 2019 | China | 60–69 | Rome II | Female –2.3 Male –2.8 |
| 70–80 | Rome II | Female –2.8 Male –2.7 | ||
| Sorouri et al. [30] 2020 | Iran | 60+ | Rome III | 1.1 |
| Sperber et al. [7] 2020 | Worldwide (23 countries) | 65+ | Rome IV | 1.7 |
Lifestyle modifications and simple dietary changes [33, 34] can improve symptoms for almost 50% of patients with IBS Pharmacological therapies recommended for IBS include low-dose tricyclic antidepressants and antispasmodics; however, these may improve some but not all symptoms [35]. Psychological therapies such as cognitive behavioural therapy[36] and gut-directed hypnotherapy [37] may also be effective for some people. First-line lifestyle approaches include managing stress, eating regularly, and limiting caffeine, alcohol, high-fat foods, and high-fibre foods. When the above strategies do not offer adequate relief, investigating potential food triggers may need to be conducted. Identifying and reducing the intake of fermentable oligo-, di-, mono-saccharides and polyols (FODMAPs) has become a leading management strategy for those with IBS that do not respond to first line general lifestyle and dietary advice [33, 34].
6.2The low FODMAP diet as treatment for IBS
Recent clinical guidelines for the United European Gastroenterology and European Society for Neurogastroenterology and Motility on functional bowel disorders with diarrhoea strongly recommend the use of the low FODMSP diet in patients with IBS-D when other measures have failed [38]. FODMAPS are poorly absorbed and become osmotically active in the small bowel. For some, increased motility occurs, leading to diarrhoea and fermentation in the large bowel, the result of which is wind, bloating and abdominal pain [39]. The low FODMAP diet has consistently been shown to effectively manage symptoms in those with IBS [40–45]. However, these intervention studies have been conducted in adults with a mean age of 50 years or younger. Recently, the effectiveness of the low FODMAP diet was studied in an older population with a mean age of 76 years [15]. Although small in number, this study provides the first evidence that the low FODMAP diet was equally effective for older adults, significantly reducing symptoms of diarrhoea and pain in those at low risk of serious underlying pathology.
The low FODMAP diet consists of three phases: elimination, reintroduction and then liberalisation or personalisation of the diet. The elimination phase of the low FODMAP diet reduces the poorly absorbed carbohydrates and the mechanism that drives symptoms. But in doing so this also reduces prebiotic fibres. Prebiotics are important substrates for the microbiota, leading to the production of short-chain fatty acids (SCFA). While following a low FODMAP diet, changes of the gut microbiome have been observed in some studies [46, 47], including one with older adults [48] but not all [49]. The second and third stages are vital to prevent unnecessary restriction of high FODMAP foods, which may impact nutritional status and gut microbiota diversity. Older adults are already at risk for malnutrition [17] and changes to gut microbiota diversity [20], especially if living in long-term residential care, [50]. Therefore, expert instruction throughout the three phases of the FODMAP diet is required. A gentle modified approach, which is now being advocated for high risk groups [51], may be the better option for some older adults as fewer foods are restricted.
6.3Coeliac disease
Following a strict gluten free diet continues to be the main treatment for managing coeliac disease. Those with coeliac disease develop an immune response to epitopes of gliadin, a major protein in gluten. This results in a lymphocytic infiltrate and the flattening of the small intestinal villi, leading to malabsorption of nutrients and corresponding GI symptoms [52]. Although there is a hereditary component, with 40% of the world’s population carrying the predisposing HL-DQ2 or HL-DQ8 gene, there is incomplete penetrance resulting in approximately 1% of most populations being affected [53].
Once thought to be a disease associated with childhood, diagnosis of coeliac disease can occur at any stage of life. In a large population-based study, the incidence was greatest for those in their thirties (92/416, 22.1%), followed by children and adolescents from 0–19 years old (84/416, 20.2%) and those in their forties (84/416, 20.2%). However, coeliac disease was also frequently diagnosed in those aged 60 years and older 51/416 (12.3%) [54]. The prevalence of coeliac disease first diagnosed after 60 years varies considerably, with rates ranging from 5% [55] to 27% [56], and is thought to be increasing [53]. Diagnosis of coeliac disease can be delayed for older people [57]. This delay in diagnosis may lead to a significantly increased risk of complications for adults over 60 years compared to those aged 18–40 years [58]. For example, anaemia is common for older adults presenting with coeliac disease, as high as 75% for women and 80% for men [57], compared to 50% for younger age groups. Osteoporosis and weight loss are also more likely to be a feature of older adults at diagnosis than for younger adults [55].
Most people with coeliac disease experience significant symptom improvements when following a strict gluten-free diet. However, for those with refractory coeliac disease, symptoms persist despite being gluten-free and immunosuppressive treatment is required [59]. The symptom profile of coeliac disease for an older adult compared to a younger adult is similar, although older adults may experience more dyspepsia and abdominal bloating [55]. Even without troubling symptoms, a gluten-free trial may increase energy and well-being, often masked when patients become used to low-grade fatigue. Older adults can manage a gluten-free diet and most achieve sustained clinical improvements [57]. Preventing delays in diagnosis and ensuring dietetic involvement is essential in the nutritional management of coeliac disease for older adults, especially if there has been unintended weight loss or malnutrition.
6.4Small intestinal bacterial overgrowth
Small intestinal bacterial overgrowth (SIBO) occurs when there is an overgrowth of the usual low number of small intestinal bacteria. SIBO may be a result of other underlying conditions, such as coeliac disease, small bowel diverticulosis or small bowel fistulas [60], or a primary condition due to factors such as altered small bowel motility [61] or resulting from a change in the pH of the small intestine allowing bacteria to colonise [62].
The diagnosis of SIBO usually relies on indirect testing such as hydrogen and methane breath testing following lactulose and glucose ingestion. Such testing has led to significant variability in the rates of SIBO which have been reported, in older adults living in care and independently, to be between 14.5% [63] and 25% [64]. Lewis et al. have suggested that prevalence of SIBO potentially increases with age; however, in their study of 62 residential care residents, the diagnosis of SIBO was usually benign with no associated GI symptoms [63]. The increasing prevalence of SIBO in older adults may be due to changes in physical activity and oral food intake, the impact of chronic diseases and/or pharmaceutical treatments impacting gut transit or the gut environment [62]. A meta-analysis of 19 studies found an increased risk of SIBO for those taking proton pump inhibitors (PPI) (OR 1.71, 95% confidence interval 1.20–2.53). Proton pump inhibitors inhibit gastric acid production, which may have a cascading effect on the rest of the digestive tract, allowing for the growth of bacteria in locations where numbers should remain low. For older adults, this could be a risk factor for SIBO as PPIs are commonly prescribed in this population.
Currently, the use of antibiotics [3], in particular Rifaximin [65], is the recommended treatment for SIBO, although all studies have been conducted in younger adults. Reoccurrence of SIBO is reported to be common, with up to 43.7% of people treated with one week of antibiotic treatment experiencing GI symptoms again at nine months [66]. Dietary interventions could be considered for those not wishing to take antibiotics or if antibiotics have not been effective. Dietary restrictions, such as following the low FODMAP diet [67] or a break from solid food altogether by consuming an elemental diet for two weeks[68], may be viable options. However, more research is needed to determine efficacy.
6.5Bile acid diarrhoea
Bile acid diarrhoea (BAD), also known as bile acid malabsorption, results in increased gut motility and colonic fluid, leading to watery diarrhoea but often without bloating, pain or increased flatulence [69]. Typically 97% of bile acids are reabsorbed in the terminal ileum and return to the liver [70], but in the case of BAD, the primary or secondary bile acids are not reabsorbed and continue to the colon. Primary BAD results from an excess of bile acid production that cannot be absorbed fully in the terminal ileum. Secondary BAD results from damage to the small intestine leading to inefficient bile acid absorption and can occur following coeliac disease, Crohn’s disease, SIBO, and terminal ileal resections. In some cases, no cause can be identified and therefore classified as idiopathic bile acid diarrhoea. It has been suggested that 41% of those who present with IBS-D may actually have BAD [12] and that BAD is most likely underdiagnosed [71]. The British Society of Gastroenterology guidelines recommended considering BAD as a possible cause of chronic diarrhoea in those who do not respond to dietary and lifestyle changes [3]. Once again, diagnosis relies on indirect testing which may lack specificity and often a clinical trial of treatment is used in place of a diagnostic test.
The main treatment option for BAD is bile acid sequestrants. However, a low-fat diet has been shown to be effective in symptom reduction and may be preferred when bile acid sequestrants are not well tolerated or for those with mild and borderline BAD [72]. Long term use of bile acid sequestrants or following a low-fat diet may pose a risk of fat-soluble vitamin deficiencies (A, E, D, K) [73]. For older adults with BAD this is an important consideration, especially in those with reduced oral intake of foods rich in fat-soluble vitamins.
6.6Pancreatic exocrine insufficiency
The pancreas releases enzymes lipase, amylase as well as proenzymes to digest food. Without these enzymes, malabsorption of nutrients can occur, leading to loose bowel motions and pain [74]. The main causes of pancreatic insufficiency are chronic pancreatitis in adults and cystic fibrosis in children [74]. However, in older adults, advancing age can cause pancreatic atrophy [12] and this, in the absence of any history or evidence of pancreatic disease [75], can result in pancreatic insufficiency. Older adults may therefore be at an increased risk of pancreatic insufficiency. Duodenal aspirates from adults over 65 years [76] have been shown to have a reduced concentration of pancreatic enzymes. Diagnosis of pancreatic insufficiency can be challenging. Faecal elastase concentration is the most commonly used diagnostic test, however it is inaccurate if stools are watery and, as faecal elastase can be lower in older adults, false negatives are more likely [77]. A therapeutic trial of pancreatic enzymes along with a history of steatorrhea and weight loss can be used to diagnose pancreatic insufficiency in the absence of positive test results [77]. Pancreatic enzyme replacement therapy (PERT) is required for the ongoing management of pancreatic insufficiency. Dietary intake changes are not necessary, however, in order to titrate the dosage of PERT to minimise symptoms, dietary education on the fat content of meals and snack foods is essential.
6.7Sucrase-isomaltase deficiency
Disaccharide enzyme deficiencies are a potential cause of mild to severe diarrhoea with bloating and abdominal pain in adults [78]. Foods containing starch are broken down into monosaccharides before being absorbed into the bloodstream. While this initially starts in the mouth with salivary α-amylase and then pancreatic amylase, most hydrolysis occurs in the small intestine by the brush border enzymes sucrase-isomaltase. In the absence of these disaccharide enzymes, the short chain carbohydrates continue to the colon, drawing fluid into the bowel, resulting in diarrhoea [78]. The malabsorbed sugars are a food source for endogenous colonic bacteria, leading to excess gas production, bloating and pain.
Several authors, however, suspect that the symptoms of disaccharide enzyme deficiency are often misdiagnosed as IBS [79–81]. A case-control study of those with and without IBS found that those with IBS had a trend to be more likely to have a genetic mutation for sucrase deficiency (p = 0.074, OR = 1.84) [82]. Sucrase-isomaltase deficiency may be due to genetic polymorphisms, mostly diagnosed in childhood but possibly not identified until adulthood, with variants in the gene reducing sucrase-isomaltase enzymatic activity or damage to the duodenal villi from coeliac disease, infections or SIBO [79]. The restriction of sucrose and high starch carbohydrate foods is considered the primary dietary strategy to manage sucrase-isomaltase deficiency [83, 84]. This dietary approach is somewhat novel and the diet can be quite restrictive. There is little published information on this dietary treatment, how and if it is possible to establish individual tolerance levels for starch and sucrose containing foods and how to ensure a nutritionally balanced diet while minimising symptoms.
6.8Lactose intolerance
Lactose, another disaccharide, can result in GI symptoms when the enzyme lactase is not present. Lactase hydrolyses lactose into galactose and glucose, which are then transported across the small intestine mucosa. Insufficient lactase or damage to the brush border of the small intestine, means lactose remains intact and continues to the colon, where it is fermented by the endogenous bacteria resulting in diarrhoea, abdominal pain, bloating and excess flatulence [85]. A systematic review of 54 articles conducted in 2010 found that the prevalence of lactose intolerance may increase with age due to decline of lactase [85]. Stefano et al. measured breath hydrogen and methane production after 20 grams of lactose [86] and found that lactose malabsorption was greater in adults aged 74 years and older (28/34 [83% ]) compared to adults less than 65 years (19/33 [58% ] p < 0.02). However, actual lactose intolerance, where symptoms develop from malabsorption of lactose, was greater in the younger population, indicating that although older adults malabsorbed lactose, they may not experience symptoms to the same degree as a younger person.
A short two-week elimination of lactose containing foods is sufficient to determine if lactose intolerance is present. The elimination of all dairy is not required as most people can manage small amounts of lactose [87]. Dairy products not only contain high amounts of calcium but are also a good protein source. Older adults require more protein to maintain muscle mass and calcium than any other age group [88], therefore advice regarding dietary changes needs to be done carefully to prevent unnecessary restrictions.
7Consequences and complications of dietary management for chronic diarrhoea in older adults
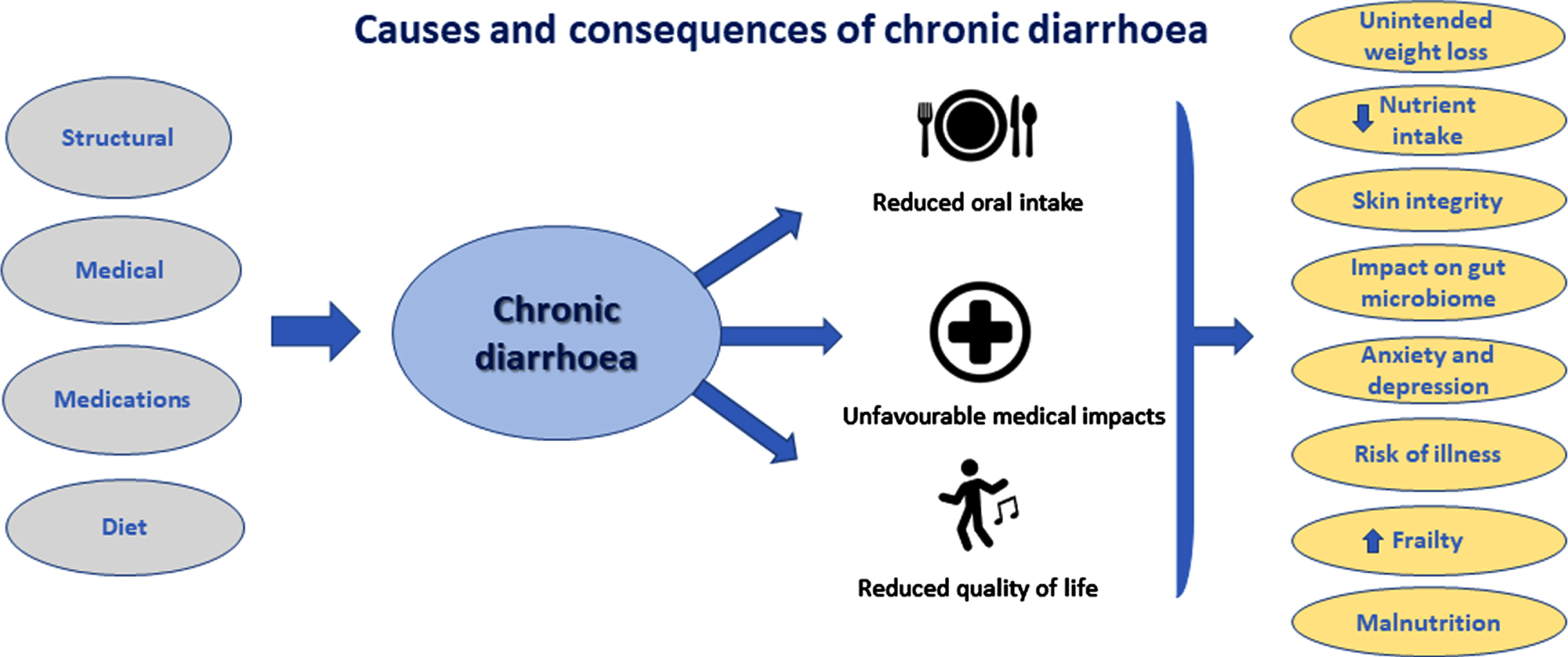
The causes and dietary management of chronic diarrhoea are varied and the consequences multifactorial (Fig. 1). Food is an integral part of life, providing adequate nutrition and opportunities for socialising and enjoyment. However, when not carefully planned, changes in diet may have unwanted consequences such as malnutrition, reduced energy levels, inadequate nutrient intake, reduction in the gut microbiome diversity, development of disordered eating patterns such as Avoidant or Restrictive Food Intake Disorder (ARFID) or negative impacts on quality of life (Table 4). For example, during the elimination phase of the low FODMAP diet changes in the microbiome has been observed [46], and nutrient deficiencies as possible due to inadequate intake of folate and vitamins when following a low wheat diet [89]. Therefore, risk factors should be considered and dietary modifications provided by those knowledgeable and experienced to prevent or minimise undesirable effects.
Fig. 1
The interplay of consequences occurring from chronic diarrhoea: dietary intake, nutritional status and other.
8Conclusion
Older adults likely present at least as frequently with chronic diarrhoea as younger adults and, therefore, common causes of chronic diarrhoea should be considered in all adults regardless of age. Many causes of chronic diarrhoea can be managed with dietary changes; however, expert guidance is needed, especially in more vulnerable populations such as older adults, so as not to cause more harm than good.
Acknowledgments
The authors have no acknowledgments
Funding
The authors report no funding
Conflict of interest
The authors have no conflict of interest to report
References
[1] | United Nations DoEaSA, Population division World Populations Ageing - 2019 [Available from: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Report.pdf. |
[2] | O’Keefe EA , Talley NJ , Zinsmeister AR , Jacobsen SJ , Bowel disorders impair functional status and quality of life in the elderly: a population-based study, J Gerontol A Biol Sci Med Sci.M (1995) ;50: (4):184–9. |
[3] | Arasaradnam RP , Brown S , Forbes A , Fox MR , Hungin P , Kelman L , et al., Guidelines for the investigation of chronic diarrhoea in adults: British Society of Gastroenterology, Gut (2018) ;67: (8):1380–99. |
[4] | Schmulson MJ , Drossman DA , What is new in Rome IV, J Neurogastroenterol Motil (2017) ;23: (2):151. |
[5] | Shah BJ , Chokhavatia S , Rose S , Fecal incontinence in the elderly: FAQ, Official journal of the American College of Gastroenterology| ACG (2012) ;107: (11):1635–46. |
[6] | Chaplin A , Curless R , Thomson R , Barton R . Prevalence of lowergastrointestinal symptoms and associated consultation behaviour in aBritish elderly population determined by face-to-face interview, BrJ Gen Pract (2000) ;50: (459):798–802. |
[7] | Sperber AD , Bangdiwala SI , Drossman DA , Ghoshal UC , Simren M , Tack J , et al., Worldwide Prevalence and Burden of Functional Gastrointestinal Disorders, Results of Rome Foundation Global Study. Gastroenterology. 2020. |
[8] | Kay L , Prevalence, incidence and prognosis of gastrointestinal symptoms in a random sample of an elderly population, Age Ageing (1994) ;23: (2):146–9. |
[9] | Sandler RS , Stewart WF , Liberman JN , Ricci JA , Zorich NL , Abdominal pain, bloating, and diarrheain the united states, Dig Dis Sci (2000) ;45: (6):1166–71. |
[10] | Bennett G , Talley NJ , Irritable bowel syndrome in the elderly, Best Practice & Research Clinical Gastroenterology (2002) ;16: (1):63–76. |
[11] | Schiller LR . Chronic Diarrhea Evaluation in the Elderly: IBS or Something Else? Curr Gastroenterol Rep (2019) ;21: (9):45. |
[12] | Crooks B , Limdi JK , McLaughlin J , How to manage chronic diarrhoea in the elderly? Frontline Gastroenterol (2019) ;10: (4):427–33. |
[13] | Zhao Y-F , Guo X-J , Zhang Z-S , Ma X-Q , Wang R , Yan X-Y , et al., Epidemiology of functional diarrhea and comparison with diarrhea-predominant irritable bowel syndrome: a population-based survey in China, PLoS One (2012) ;7: (8). |
[14] | Fosnes GS , Lydersen S , Farup PG , Constipation and diarrhoea-common adverse drug reactions? A cross sectional study in the general population, BMC Clin Pharmacol (2011) ;11: (1):2. |
[15] | O’Brien L , Skidmore P , Wall C , Wilkinson T , Muir J , Frampton C , et al., A Low FODMAP Diet Is Nutritionally Adequate and Therapeutically Efficacious in Community Dwelling Older Adults with Chronic Diarrhoea, Nutrients (2020) ;12: (10). |
[16] | Gorospe EC , Oxentenko AS , Nutritional consequences of chronic diarrhoea, Best Pract Res Clin Gastroenterol (2012) ;26: (5):663–75. |
[17] | Agarwal E , Ferguson M , Banks M , Bauer J , Capra S , Isenring E , Nutritional status and dietary intake of acute care patients: results from the Nutrition Care Day Survey Clin Nutr (2012) ;31: (1):41–7. |
[18] | Chatindiara I , Allen J , Hettige D , Senior S , Richter M , Kruger M , et al., High prevalence of malnutrition and frailty among older adults at admission to residential aged care, J Prim Health Care (2020) ;12: (4):305–17. |
[19] | Fhon JRS , Rodrigues RAP , Santos JLF , Diniz MA , Santos EBd , Almeida VC , et al., Factors associated with frailty in older adults: a longitudinal study. Rev Saude Publica. 2018;52. |
[20] | Kim S , Jazwinski SM , The Gut Microbiota and Healthy Aging: A Mini-Review, Gerontology (2018) ;64: (6):513–20. |
[21] | Biagi E , Nylund L , Candela M , Ostan R , Bucci L , Pini E , et al., Through ageing, and beyond: gut microbiota and inflammatory status in seniors and centenarians, PLoS One (2010) ;5: (5):e10667. |
[22] | DeJong EN , Surette MG , Bowdish DM , The gut microbiota and unhealthy aging: disentangling cause from consequence, Cell Host Microbe (2020) ;28: (2):180–9. |
[23] | Claesson MJ , Jeffery IB , Conde S , Power SE , O’connor EM , Cusack S , et al., Gut microbiota composition correlates with diet and health in the elderly, Nature (2012) ;488: (7410):178–84. |
[24] | Holscher HD , Dietary fiber and prebiotics and the gastrointestinal microbiota, Gut microbes (2017) ;8: (2):172–84. |
[25] | De Filippiss F , Pellegrini N , Vannini L , Jeffery IB , La Storia A , Laghi L , et al., High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome, Gut (2016) ;65: (11):1812–21. |
[26] | Critselis E , Panagiotakos D , Adherence to the Mediterranean diet and healthy ageing: Current evidence, biological pathways, and future directions, Crit Rev Food Sci Nutr (2020) ;60: (13):2148–57. |
[27] | Ballou S , Katon J , Singh P , Rangan V , Lee HN , McMahon C ,et al., Chronic diarrhea and constipation are more common in depressed individuals, Clin Gastroenterol Hepatol (2019) ;17: (13):2696–703. |
[28] | Singh P , Mitsuhashi S , Ballou S , Rangan V , Sommers T , Cheng V , et al., Demographic and dietary associations of chronic diarrhea in a representative sample of adults in the United States, Am J Gastroenterol (2018) ;113: (4):593–600. |
[29] | Drossman DA , Tack J , Ford AC , Szigethy E , Törnblom H , Van Oudenhove L , Neuromodulators for functional gastrointestinal disorders (disorders of Gut–Brain interaction): a Rome Foundation working team report, Gastroenterology (2021) ;154: (4):1140–71. e1. |
[30] | Sorouri M , Pourhoseingholi MA , Vahedi M , Safaee A , Moghimi-Dehkordi B , Pourhoseingholi A , et al., Functional bowel disorders in Iranian population using Rome III criteria, Saudi journal of gastroenterology: official journal of the Saudi Gastroenterology Association (2010) ;16: (3):154. |
[31] | Drossman D , Whitehead W , Camilleri M , Irritable bowel syndrome: a technical review for practice guideline development, Gastroenterology (1997) ;112: (6):2120–37. |
[32] | Matsumoto S , Hashizume K , Wada N , Hori J , Tamaki G , Kita M , et al., Relationship between overactive bladder and irritable bowel syndrome: a large-scale internet survey in J apan using the overactive bladder symptom score and Rome III criteria, BJU Int (2013) ;111: (4):647–52. |
[33] | McKenzie Y , Bowyer R , Leach H , Gulia P , Horobin J , O’Sullivan N , et al., British Dietetic Association systematic review and evidence-based practice guidelines for the dietary management of irritable bowel syndrome in adults update), J Hum Nutr Diet (2016) ;29: (5):549–75. |
[34] | National Institute for Health Clinical Excellence. Irritable Bowel Syndrome in Adults: Diagnosis and Management of IBS in Primary Care: NICE; 2008 [Available from: https://www.nice.org.uk/guidance/cg61. |
[35] | Moayyedi P , Andrews CN , MacQueen G , Korownyk C , Marsiglio M , Graff L , et al., Canadian Association of Gastroenterology Clinical Practice Guideline for the Management of Irritable Bowel Syndrome (IBS), J Can Assoc Gastroenterol (2019) ;2: (1):6–29. |
[36] | Li L , Xiong L , Zhang S , Yu Q , Chen M . Cognitive–behavioral therapy for irritable bowel syndrome: A meta-analysis, J Psychosom Res (2014) ;77: (1):1–12. |
[37] | Peters S , Yao C , Philpott H , Yelland G , Muir J , Gibson P . Randomised clinical trial: the efficacy of gut-directed hypnotherapy is similar to that of the low FODMAP diet for the treatment of irritable bowel syndrome, Aliment Pharmacol Ther (2016) ;44: (5):447–59. |
[38] | Savarino E , Zingone F , Barberio B , Marasco G , Akyuz F , Akpinar H , et al. Functional bowel disorders with diarrhoea: Clinical guidelines of the United European Gastroenterology and European Society for Neurogastroenterology and Motility. United Eur Gastroent.n/a(n/a). |
[39] | Barrett JS , Gearry RB , Muir JG , Irving PM , Rose R , Rosella O , et al. Dietary poorly absorbed, short-chain carbohydrates increase delivery of water and fermentable substrates to the proximal colon, Aliment Pharmacol Ther (2010) ;31: (8):874–82. |
[40] | Eswaran SL , Chey WD , Han-Markey T , Ball S , Jackson K . A randomized controlled trial comparing the low FODMAP diet vs, modified NICE guidelines in US adults with IBS-D. Am J Gastroenterol (2016) ;111: (12):1824–32. |
[41] | De Roest R , Dobbs B , Chapman B , Batman B , O’brien L , Leeper J , et al. The low FODMAP diet improves gastrointestinal symptoms in patients with irritable bowel syndrome: a prospective study, Int J Clin Pract (2013) ;67: (9):895–903. |
[42] | Eswaran S , Chey WD , Jackson K , Pillai S , Chey SW , Han-Markey T . A diet low in fermentable oligo-, di-, and monosaccharides and polyols improves quality of life and reduces activity impairment in patients with irritable bowel syndrome and diarrhea, Clin Gastroenterol Hepatol (2017) ;15: (12):1890–9. e3. |
[43] | Böhn L , Störsrud S , Liljebo T , Collin L , Lindfors P , Törnblom H , et al. Diet low in FODMAPs reduces symptoms of irritable bowel syndrome as well as traditional dietary advice: a randomized controlled trial, Gastroenterology (2015) ;149: (6):1399–407. e2. |
[44] | Halmos EP , Power VA , Shepherd SJ , Gibson PR , Muir JG . A diet low in FODMAPs reduces symptoms of irritable bowel syndrome, Gastroenterology (2014) ;146: (1):67–75. e5. |
[45] | Staudacher HM , Whelan K , Irving PM , Lomer MC . Comparison of symptom response following advice for a diet low in fermentable carbohydrates (FODMAPs) versus standard dietary advice in patients with irritable bowel syndrome, J Hum Nutr Diet (2011) ;24: (5):487–95. |
[46] | Staudacher HM , Lomer MC , Anderson JL , Barrett JS , Muir JG , Irving PM , et al. Fermentable carbohydrate restriction reduces luminal bifidobacteria and gastrointestinal symptoms in patients with irritable bowel syndrome, The Journal of Nutrition (2012) ;142: (8):1510–8. |
[47] | Staudacher HM , Lomer MC , Farquharson FM , Louis P , Fava F , Franciosi E , et al. A diet low in FODMAPs reduces symptoms in patients with irritable bowel syndrome and a probiotic restores bifidobacterium species: a randomized controlled trial, Gastroenterology (2017) ;153: (4):936–47. |
[48] | McIntosh K , Reed DE , Schneider T , Dang F , Keshteli AH , De Palma G , et al. FODMAPs alter symptoms and the metabolome of patients with IBS: a randomised controlled trial, Gut (2017) ;66: (7):1241–51. |
[49] | Mitchell H , Porter J , Gibson PR , Barrett J , Garg M . Review article:implementation of a diet low in FODMAPs for patients with irritablebowel syndrome-directions for future research, Aliment PharmacolTher (2019) ;49: (2):124–39. |
[50] | Jeffery IB , Lynch DB , O’Toole PW . Composition and temporal stability of the gut microbiota in older persons, ISME J (2016) ;10: (1):170–82. |
[51] | Halmos EP , Gibson PR . Controversies and reality of the FODMAP diet for patients with irritable bowel syndrome, J Gastroenterol Hepatol (2019) ;34: (7):1134–42. |
[52] | Daveson AJM , Tye-Din JA , Goel G , Goldstein KE , Hand HL , Neff KM , et al. Masked bolus gluten challenge low in FODMAPs implicates nausea and vomiting as key symptoms associated with immune activation in treated coeliac disease, Aliment Pharmacol Ther (2020) ;51: (2):244–52. |
[53] | Lebwohl B , Sanders DS , Green PHR . Coeliac disease, Lancet (2018) ;391: (3915):70–81. |
[54] | Cook B , Oxner R , Chapman B , Whitehead M , Burt M . A thirty-year -study of coeliac disease in the Canterbury region of New Zealand, N Z Med J. (2004) ;117: (1189):U772. |
[55] | Casella S , Zanini B , Lanzarotto F , Villanacci V , Ricci C , Lanzini A . Celiac disease in elderly adults: clinical, serological, and histological characteristics and the effect of a gluten-free diet, J Am Geriatr Soc (2012) ;60: (6):1064–9. |
[56] | Holmes GKT , Muirhead A . Epidemiology of coeliac disease in a single centre in Southern Derbyshire 1958-2014, BMJ Open Gastroenterol (2017) ;4: (1):e000137. |
[57] | Hankey GL , Holmes GK . Coeliac disease in the elderly, Gut (1994) ;35: (1):65–7. |
[58] | Biagi F , Schiepatti A , Maiorano G , Fraternale G , Agazzi S , Zingone F , et al. Risk of complications in coeliac patients depends on age at diagnosis and type of clinical presentation, Dig Liver Dis (2018) ;50: (6):549–52. |
[59] | Hujoel IA , Murray JA . Refractory celiac disease, Curr Gastroenterol Rep (2020) ;22: (4):1–8. |
[60] | Bohm M , Siwiec RM , Wo JM . Diagnosis and management of small intestinal bacterial overgrowth, Nutr Clin Pract (2013) ;28: (3):289–99. |
[61] | Pimentel M , Soffer EE , Chow EJ , Kong Y , Lin HC . Lower frequency of MMC is found in IBS subjects with abnormal lactulose breath test, suggesting bacterial overgrowth, Dig Dis Sci (2002) ;47: (12):2639–43. |
[62] | Dukowicz AC , Lacy BE , Levine GM . Small intestinal bacterial overgrowth: a comprehensive review, Gastroenterol Hepatol (N Y) (2007) ;3: (2):112. |
[63] | Lewis SJ , Potts LF , Malhotra R , Mountford R . Small bowel bacterial overgrowth in subjects living in residential care homes, Age Ageing (1999) ;28: (2):181–5. |
[64] | Mitsui T , Shimaoka K , Goto Y , Kagami H , Kinomoto H , Ito A , et al. Small bowel bacterial overgrowth is not seen in healthy adults but is in disabled older adults, Hepatogastroenterology (2006) ;53: (67):82–5. |
[65] | Gatta L , Scarpignato C . Systematic review with meta-analysis: rifaximin is effective and safe for the treatment of small intestine bacterial overgrowth, Aliment Pharmacol Ther (2017) ;45: (5):604–16. |
[66] | Lauritano EC , Gabrielli M , Scarpellini E , Lupascu A , Novi M , Sottili S , et al. Small intestinal bacterial overgrowth recurrence after antibiotic therapy, Am J Gastroenterol (2008) ;103: (8):2031–5. |
[67] | Rezaie A , Pimentel M , Rao SS . How to test and treat small intestinal bacterial overgrowth: an evidence-based approach, Curr Gastroenterol Rep (2016) ;18: (2):8. |
[68] | Pimentel M , Constantino T , Kong Y , Bajwa M , Rezaei A , Park S . A14-day elemental diet is highly effective in normalizing thelactulose breath test, Dig Dis Sci (2004) ;49: (1):73–7. |
[69] | Bajor A , Tornblom H , Rudling M , Ung KA , Simren M . Increased colonic bile acid exposure: a relevant factor for symptoms and treatment in IBS, Gut (2015) ;64: (1):84–92. |
[70] | Hofmann AF . Chronic diarrhea caused by idiopathic bile acid malabsorption: an explanation at last, Expert Rev Gastroenterol Hepatol (2009) ;3: (5):461–4. |
[71] | Fernández-Bañares F , Esteve M , Salas A , Forné M , Espinós JC , Martín-Comín J , et al. Bile acidmalabsorption in microscopic colitis and in previously unexplainedfunctional chronic diarrhea, Dig Dis Sci (2001) ;46: (10):2231–8. |
[72] | Walters JR , Pattni SS . Managing bile acid diarrhoea, Therap Adv Gastroenterol (2010) ;3: (6):349–57. |
[73] | Sadowski DC , Camilleri M , Chey WD , Leontiadis GI , Marshall JK , Shaffer EA , et al. Canadian Association of Gastroenterology clinical practice guideline on the management of bile acid diarrhea, Clin Gastroenterol Hepatol (2020) ;18: (1):24–41. e1. |
[74] | Fieker A , Philpott J , Armand M . Enzyme replacement therapy for pancreatic insufficiency: present and future, Clin Exp Gastroenterol (2011) ;4: :55–73. |
[75] | Holt PR . Intestinal malabsorption in the elderly, Dig Dis (2007) ;25: (2):144–50. |
[76] | Löhr JM , Panic N , Vujasinovic M , Verbeke C . The ageing pancreas: a systematic review of the evidence and analysis of the consequences, J Intern Med (2018) ;283: (5):446–60. |
[77] | Forsmark CE . Diagnosis and Management of Exocrine Pancreatic Insufficiency, Curr Treat Options Gastroenterol (2018) ;16: (3):306–15. |
[78] | Viswanathan L , Rao SSC , Kennedy K , Sharma A , Yan Y , Jimenez E . Prevalence of Disaccharidase Deficiency in AdultsWith Unexplained Gastrointestinal Symptoms. J Neurogastroenterol Motil. 2020. |
[79] | Kim SB , Calmet FH , Garrido J , Garcia-Buitrago MT , Moshiree B . Sucrase-Isomaltase Deficiency as a Potential Masquerader in Irritable Bowel Syndrome, Dig Dis Sci (2020) ;65: (2):534–40. |
[80] | Zheng T , Eswaran S , Photenhauer AL , Merchant JL , Chey WD , D’Amato M . Reduced efficacy of low FODMAPs diet in patients with IBS-D carrying sucrase-isomaltase (SI) hypomorphic variants, Gut (2020) ;69: (2):397–8. |
[81] | Garcia-Etxebarria K , Zheng T , Bonfiglio F , Bujanda L , Dlugosz A , Lindberg G , et al. Increased Prevalence of Rare Sucrase-isomaltase Pathogenic Variants in Irritable Bowel Syndrome Patients, Clin Gastroenterol Hepatol (2018) ;16: (10):1673–6. |
[82] | Henstrom M , Diekmann L , Bonfiglio F , Hadizadeh F , Kuech EM , von Kockritz-Blickwede M , et al. Functional variants in the sucrase-isomaltase gene associate with increased risk of irritable bowel syndrome, Gut (2018) ;67: (2):263–70. |
[83] | Nilholm C , Larsson E , Roth B , Gustafsson R , Ohlsson B . Irregular Dietary Habits with a High Intake of Cereals and Sweets Are Associated with More Severe Gastrointestinal Symptoms in IBS Patients, Nutrients (2019) ;11: (6). |
[84] | Nilholm C , Roth B , Ohlsson B . A Dietary Intervention with Reduction of Starch and Sucrose Leads to Reduced Gastrointestinal and Extra-Intestinal Symptoms in IBS Patients, Nutrients (2019) ;11: (7). |
[85] | Wilt TJ , Shaukat A , Shamliyan T , Taylor BC , MacDonald R , Tacklind J , et al. Lactose intolerance and health, Evid Rep Technol Assess (Full Rep) (2010) (192):1–410. |
[86] | Di Stefano M , Veneto G , Malservisi S , Strocchi A , Corazza GR . Lactose malabsorption and intolerance in the elderly, Scand J Gastroenterol (2001) ;36: (12):1274–8. |
[87] | Misselwitz B , Butter M , Verbeke K , Fox MR . Update on lactose malabsorption and intolerance: pathogenesis, diagnosis and clinical management, Gut (2019) ;68: (11):2080–91. |
[88] | Barkoukis H . Nutrition recommendations in elderly and aging, Medical Clinics (2016) ;100: (6):1237–50. |
[89] | Kreutz JM , Adriaanse MPM , van der Ploeg EMC , Vreugdenhil ACE . Narrative Review: Nutrient Deficiencies in Adults and Children with Treated and Untreated Celiac Disease, Nutrients (2020) ;12: (2). |
[90] | Talley NJ , O’Keefe EA , Zinsmeister AR , Melton III LJ . Prevalence of gastrointestinal symptoms in the elderly: a population-based study, Gastroenterology (1992) ;102: (3):895–901. |
[91] | Drossman DA , Li Z , Andruzzi E , Temple RD , Talley NJ , Thompson WG , et al. US householder survey of functional gastrointestinal disorders, Dig Dis Sci (1993) ;38: (9):1569–80. |
[92] | Zhao A , Wang M-C , Szeto IM-Y , Meng L-P , Wang Y , Li T , et al. Gastrointestinal discomforts and dietary intake in Chinese urban elders: A cross-sectional study in eight cities of China, World J Gastroenterol (2019) ;25: (45):6681. |
[93] | Minocha A , Johnson WD , Abell TL , Wigington WC . Prevalence, Sociodemography, and QualitLife of Older Versus Younger Patients with Irritable Bowel Syndrome: A Population-Based Study, Dig Dis Sci (2006) ;51: (3):446–53. |




