Hydration health literacy in the elderly
Abstract
BACKGROUND:
Inadequate hydration in the elderly is associated with increased morbidity and mortality. However, few studies have addressed the knowledge of elderly individuals regarding hydration in health and disease. Gaps in health literacy have been identified as a critical component in health maintenance, and promoting health literacy should improve outcomes related to hydration associated illnesses in the elderly.
METHODS:
We administered an anonymous survey to community-dwelling elderly (n = 170) to gauge their hydration knowledge.
RESULTS:
About 56% of respondents reported consuming >6 glasses of fluid/day, whereas 9% reported drinking ≤3 glasses. About 60% of respondents overestimated the amount of fluid loss at which moderately severe dehydration symptoms occur, and 60% did not know fever can cause dehydration. Roughly 1/3 were not aware that fluid overload occurs in heart failure (35%) or kidney failure (32%). A majority of respondents were not aware that improper hydration or changes in hydration status can result in confusion, seizures, or death.
CONCLUSIONS:
Overall, our study demonstrated that there were significant deficiencies in hydration health literacy among elderly. Appropriate education and attention to hydration may improve quality of life, reduce hospitalizations and the economic burden related to hydration-associated morbidity and mortality.
1Introduction
A number of common hydration-related medical conditions in the geriatric population are associated with either excess total body fluid (overhydration), or reduced total body fluid (dehydration) [1–10]. Dehydration occurs when there is excess fluid loss from the body, either due to an illness, exposure to high temperatures, exertion with inadequate fluid intake or use of diuretic medications. This can result in serious imbalance of sodium ranging from hypo to hypernatremia which if not treated promptly, could result in significant morbidity and mortality [1, 4–6]. The symptoms of dehydration can range from simple dizziness and confusion to seizures and death. Some of the physical signs of dehydration that have demonstrated good specificity for detection include dry axillae, sunken eyes, and a delayed capillary refill time [2, 3].
In some individuals, the loss of as little as 2-3% of body fluid can cause physical and cognitive impairment [4]. The elderly population is at an increased risk for dehydration for a number of reasons, including a decrease in the thirst sensation, a decrease in renal perfusion, an altered sensitivity to antidiuretic hormone and neurocognitive deficits [1, 4–7] Notably, Rowat et al. identified 4 independent risk factors for dehydration upon admission to a hospital: 1) older age, 2) female gender, 3) total anterior circulation syndrome, and 4) prescribed diuretics [8].
Clinically, dehydration is a major predictor of morbidity and mortality in admitted patients [8, 9]. Rowat et al. assessed dehydration in hospitalized stroke patients and discovered that dehydrated patients were significantly more likely than hydrated patients to become dependent upon others at discharge or die during hospitalization [8]. Dehydration following a stroke also increases the risk of venous thromboembolism, and this is associated with poor health outcomes [8].
In addition to thromboembolism, there are numerous other consequences of dehydration among the elderly population, including delirium, confusion, infections, falls, and fractures [10–12]. Lastly, Hodgkinson et al. found that semi-independent patients in nursing homes who appear to be capable of obtaining their own fluids, but who cannot do so in practice, are most at risk for dehydration [13]. It is estimated that cognitively impaired residents in nursing facilities are at the highest risk of dehydration and more than one-third suffer from dehydration [14, 15]. In these cases, healthcare professionals do not present these patients with fluids because they do not perceive this group as being at risk for dehydration [15].
Dehydration also presents a tremendous economic burden some of which is potentially preventable [16]. A large retrospective study using the Healthcare Cost and Utilization Project (HCUP) project data revealed that the average age for patients admitted with the principal diagnosis of dehydration was 80.4 years. Approximately 64% of these were community dwelling white women [17]. The average length of stay (LOS) for dehydration in the HCUP data was 4.6 days and the total hospitalization charge per person was $7,442 [17].
The elderly population is also at risk for overhydration. Overhydration, or fluid overload, is caused by a number of conditions, including heart failure [18, 19], kidney failure [20, 21], and protein deficiency [22]. Iatrogenic overhydration can also occur as a result of receiving intravenous fluids [23], blood transfusions [24], and steroids [25]. The consequences of overhydration range from mild to life-threatening and include congestive heart failure and pulmonary edema, [26–28], confusion [29, 30], high blood pressure, seizure, and even death [31, 32].
The electrolyte abnormalities in elderly surgical patients and critically ill are often due to overhydration secondary to excess or inappropriate infusion of intravenous fluids [32–34]. Hence, overhydration is an independent risk factor for morbidity and mortality in elderly people with heart failure, acute or chronic renal failure or for those on dialysis [4, 5, 33, 34].
Despite numerous studies that describe why the elderly population is at an increased risk for hydration-related health issues compared to the younger population, there is little information on how much fluid elderly people consume or the health literacy of this population about proper hydration [13]. One of the few studies that investigated this, Goodman et al., concluded from the National Cancer Institute’s 2007 Food Attitudes and Behaviors Survey that a significantly greater number of individuals 55 years of age or older drink fewer than 4 cups of water per day compared to individuals between 18 and 34 years old (47% vs. 43%, p = 0.04) [35, 36]. This finding supported those of Sebastian et al. who found that while those 20–39 years of age reported drinking 4.7–5 cups of water/day, those 60+ years old reported drinking only 3.1–3.5 cups/day [37, 38]. While these data indicate that the elderly population consumes less water than the younger population, more work needs to be done to determine the specific amount of fluid that the elderly consume and to understand the elderly population’s general knowledge of hydration. In addition, there has been minimal research into how well elderly individuals understand the signs and symptoms of dehydration and overhydration.
Since the elderly are highly susceptible to problems associated with hydration, we conducted a survey to understand how much fluid elderly individuals consume on a daily basis and to determine their knowledge about optimal hydration status, the signs and symptoms of dehydration and overhydration, and some of the common associated medical conditions.
2Materials and methods
2.1Design
This was a cross-sectional study based using an anonymous survey and a convenience sample methodology. The questionnaire was designed to evaluate the health literacy of older adults in the geriatric age-group regarding the importance of hydration in health and different common disease conditions encountered in the elderly. The survey comprised of 5 demographic questions and 10 structured hydration related questions which addressed types and quantity of fluids consumed, the importance of hydration for health and the problems associated with dehydration or overhydration (Fig. 1). The study was approved by the Institutional Review Board at the University of Arkansas for Medical Sciences (UAMS) (IRB protocol #202655).
Fig.1
Hydration questionnaire utilized in the study. Demographic questions have not been included in this figure.
2.2Subjects
The survey was completed by 170 elderly, community-dwelling individuals (over the age of 60) who were patients at the Thomas and Lyon Longevity Clinic at the UAMS Reynolds Institute on Aging. A trained research technician administered the survey to participants. The participants either completed the survey themselves or the research technician read the questions and possible answers to them, and the participant indicated the answers verbally.
2.3Analysis
The survey results were analyzed with SAS software (version 9.3, SAS Institute Inc.). Categorical variables are presented as counts and percentages that were calculated with the PROC FREQ SAS procedure. Responses to questions were compared by group with either the chi-square test or Fisher’s exact test for contingency tables with cells having expected frequencies of 5 or less. The chi-square and Fisher’s exact tests were performed with the PROC FREQ SAS procedure with the options “chisq” and “fisher.” The α cut-off for significance was accepted as p < 0.05.
3Results
3.1Study participants
The demographic characteristics of the participants are detailed in Table 1. All of the survey respondents were community-dwelling, and most lived in the Central Arkansas area. The majority of survey respondents (57%) were between 70 and 79 years old, 80% were White, Non-Hispanic, and 20% were African Americans. There were 52% females. The majority were college graduates or greater (57%), but 35% had less than a high school education.
Table 1
Demographics (n = 170)
| Percent | |
| Age | |
| 60–69 | 20.4 |
| 70–79 | 57.4 |
| 80–89 | 20.4 |
| 90–99 | 1.9 |
| Race | |
| White, non-Hispanic | 80.0 |
| African American | 20.0 |
| Gender | |
| Female | 51.9 |
| Male | 48.1 |
| Education | |
| Less than high school | 35.0 |
| Some college | 8.4 |
| College graduate or more | 56.6 |
3.2Fluid intake
Our survey began by gauging how much and what type of fluid the participants consumed each day through recall of fluid intake on an average day. We found that the majority of respondents (56%) drank more than 6 glasses of fluid each day, with 15% drinking 9 or more glasses (Fig. 2A). Over 35% reported drinking at least 4 to 6 glasses each day, and only 9% drank 3 glasses or fewer (Fig. 2A).
Fig.2
Self-reported A) amounts and B) types of fluids the survey respondents consumed per day. Most respondents consumed 4–9 glasses of fluid per day, and the most popular drinks were water and coffee. “Other” drinks included milk, fruit and vegetable juices, and alcoholic beverages (e.g. beer or wine).
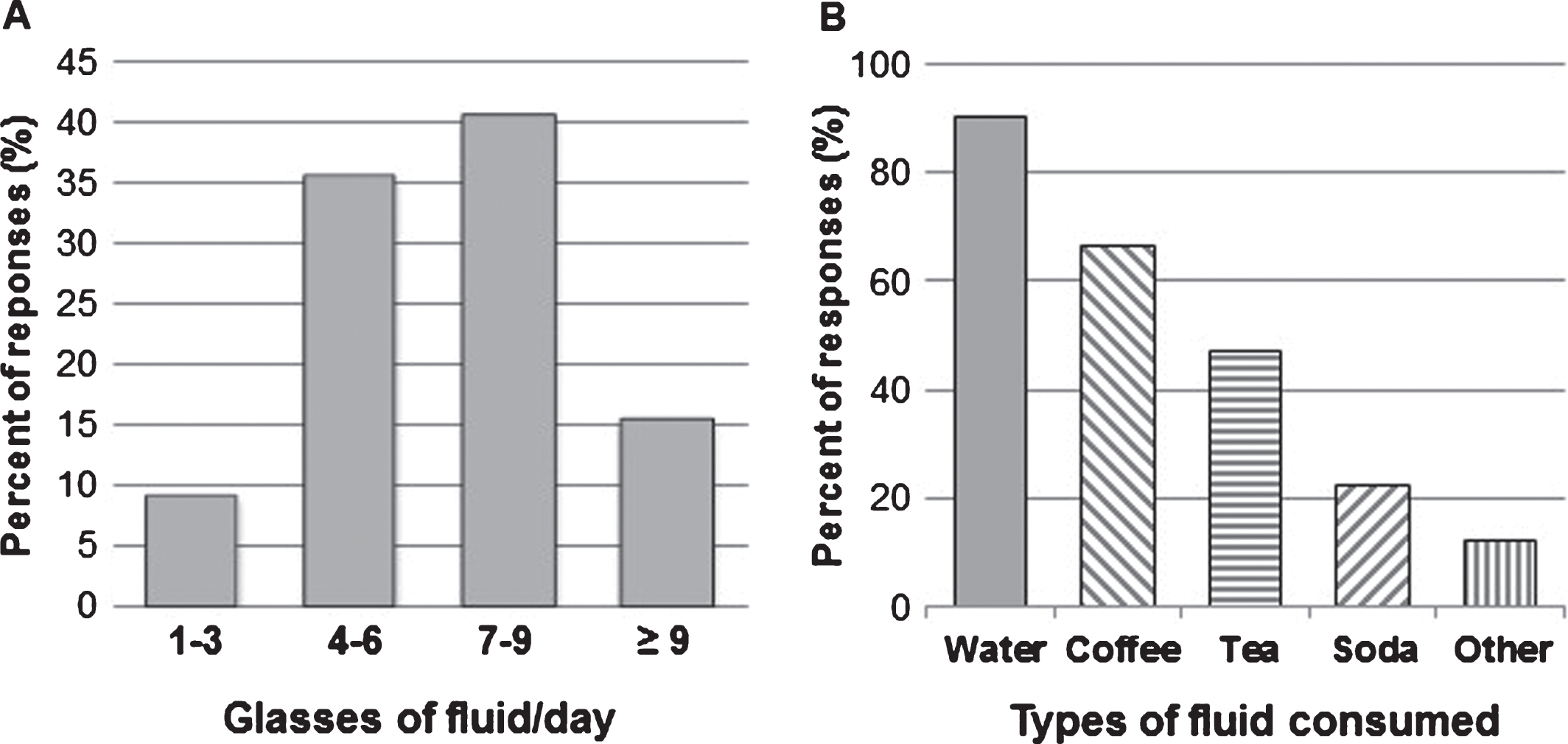
When asked about the kinds of fluids they drank, 90% reported drinking water, 66% drank coffee, and 47% drank tea (Fig. 2B). Only 22% reported drinking soda (e.g., Coke or Pepsi) (Fig. 2B). With respect to other kinds of fluids, about 12% of respondents mentioned drinking milk, fruit or vegetable juice and alcoholic beverages (e.g., beer or wine).
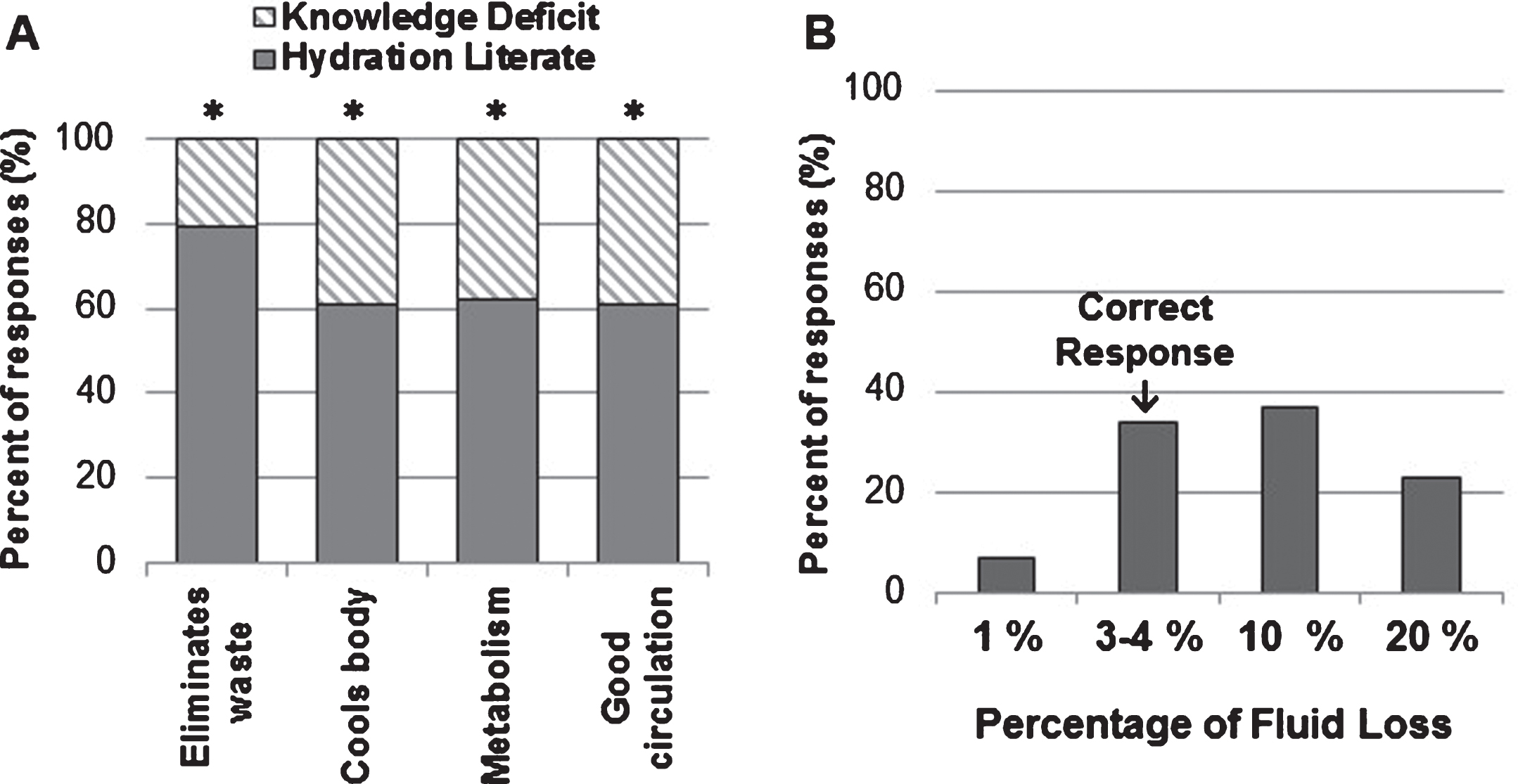
3.3Importance of hydration
We next determined how much each participant knew about the importance of fluid intake for the function of the body. The majority of respondents (79%) were aware that adequate fluid intake was important for eliminating waste from the body, and at least 60% of respondents had significant knowledge about hydration to identify that cooling of the body, metabolism, and maintaining good circulation were related to adequate fluid intake (p < 0.05, Fig. 3A).
While the majority of respondents appeared to understand the physiologic functions of fluid intake, only 34% correctly identified the amount of fluid loss (3-4% of body fluid) required for the signs and symptoms of dehydration to develop (Fig. 3B). The majority of respondents (60%) reported that the signs and symptoms of dehydration begin after the loss of 10% or higher of body fluid. This represented a significant knowledge deficit in the elderly regarding how critically important fluids are for the body (p < 0.05, Fig. 3B).
Fig.3
Survey respondents were asked about A) The importance of adequate fluid intake for bodily function. About 60–80% displayed sufficient hydration literacy regarding specific body functions requiring adequate fluid intake. B) Only 34% of respondents were able to correctly answer at what percentage of fluid loss dehydration signs and symptoms would begin to appear. *P-value <0.05.
3.4Conditions that cause dehydration or overhydration
The participants were also surveyed about their knowledge of medical conditions that can cause dehydration or overhydration. A significant percentage of respondents were aware that diarrhea (68%) orvomiting (59%) caused dehydration (p < 0.05, Fig. 4A). However, a significant gap in hydration health literacy was observed in 60% of the respondents when they failed to associate fevers or kidney failure with fluid loss (p < 0.05, Fig. 4A). Only about 55% of the respondents were aware that diuretics and excessive perspiration can cause dehydration (Fig. 4A).
Fig.4
The survey included questions asking about A) Conditions that cause excess fluid loss and B) Conditions that cause excess fluid retention. Only ∼60% percent of respondents were able to correctly identify conditions associated with excess fluid loss (diarrhea and vomiting) and excess fluid retention (heart failure and kidney failure). *P-value<0.05.
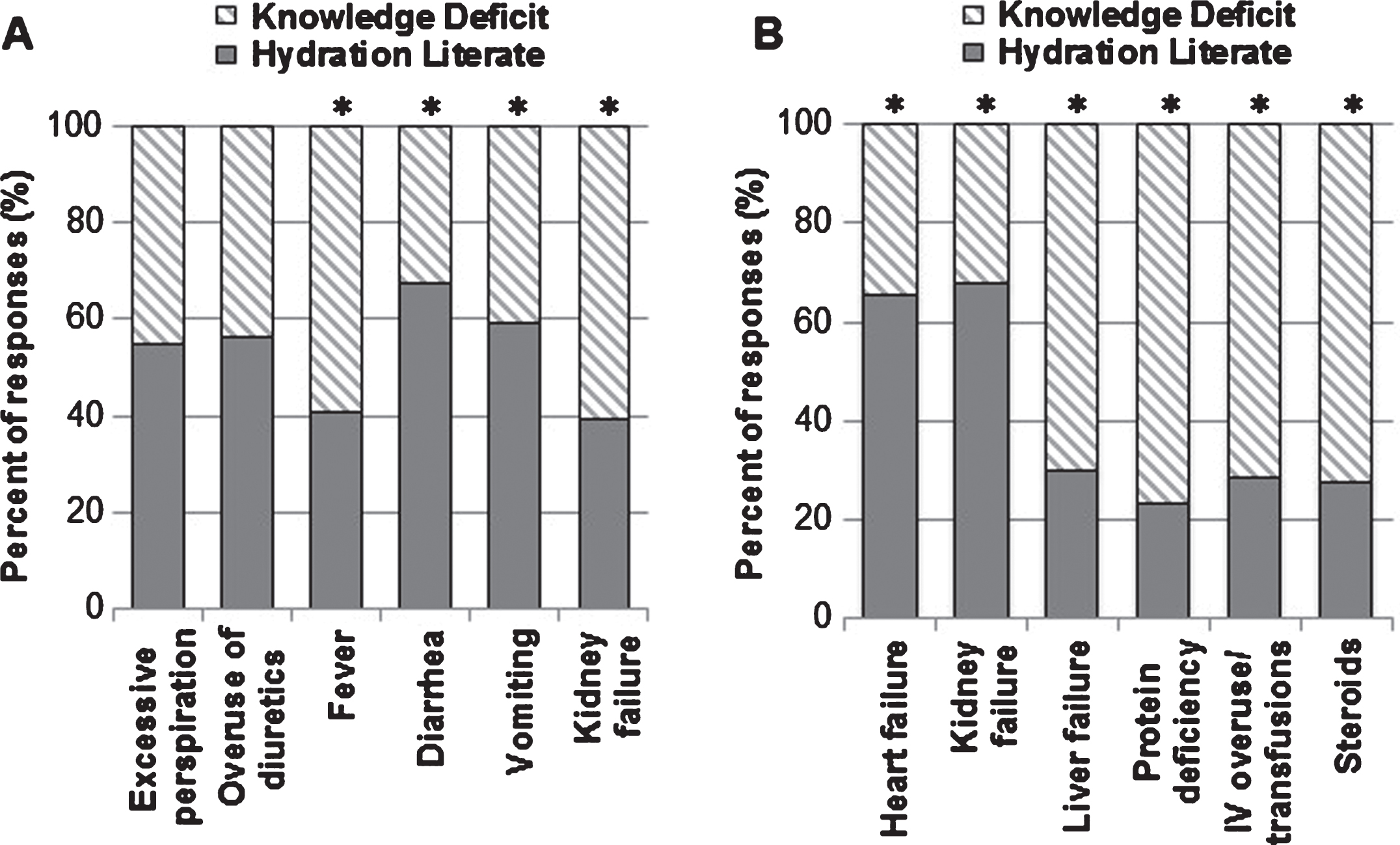
Health literacy regarding overhydration was also limited but a significant percentage of respondents seemed to be aware that heart failure (65%) and kidney failure (68%) were conditions where excess fluid accumulated in the body (p < 0.05, Fig. 4B). However, there were serious knowledge gaps regardingcertain conditions and fewer than one-third of respondents knew that liver failure (30%), receiving excess intravenous fluids or a blood transfusion (29%), receiving steroids (28%) or protein deficiency (23%), could result in problems with overhydration (p < 0.05, Fig. 4B).
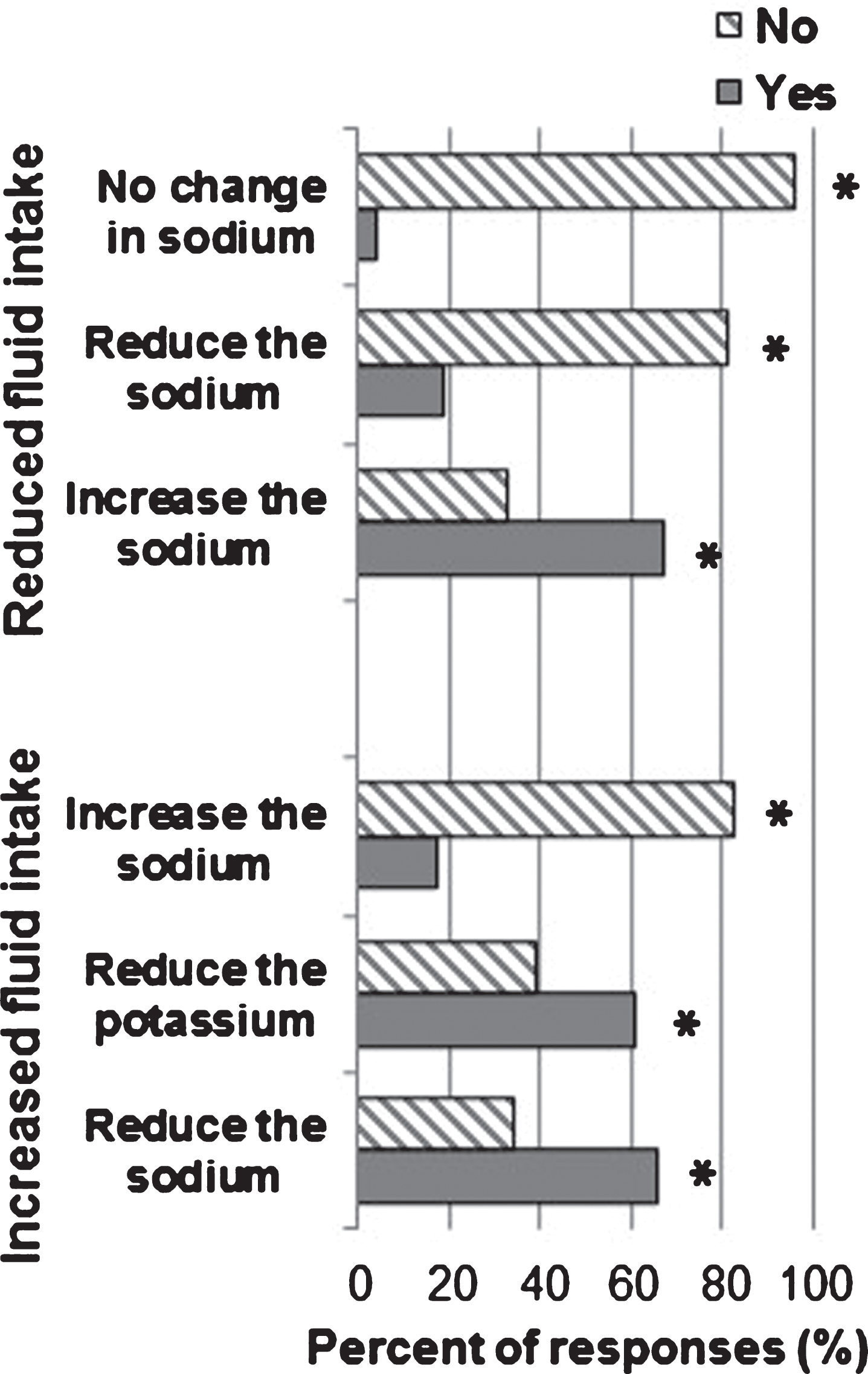
3.5Effects of dehydration and overhydration
We were also interested in learning how much the respondents knew about the effect of dehydration and overhydration on the concentration of sodium in the blood. Approximately two-thirds of respondents answered that reduced fluid intake could increase sodium and excess fluid intake could reduce sodium. However, just over 60% of the respondents believed that an increased fluid intake would reduce potassium concentrations, and nearly 20% believed that reduced fluid intake, or dehydration, would actually reduce the sodium levels in the blood (p < 0.05, Fig. 5).
Fig.5
Survey respondents were asked about how reduced or increased fluid intake would affect sodium levels in the blood. A small majority of the subjects believed that there was increase in sodium level with reduced fluid intake, while a minority of the subjects believed that sodium level increased with increased fluid intake. Yes vs No; *P-value<0.05.
3.6Symptoms of dehydration and overhydration
Lastly, there were significant deficits in the health literacy of respondents about medical complications associated with dehydration and overhydration. The most common association with that the respondents made with dehydration was the symptom of dizziness (70%, p < 0.05, Fig. 6A). However, a high percentage of respondents were not aware that low blood pressure (54%), fainting (54%), increased heart rate (58%), excessive sleepiness (70%), seizures (78%) and even death (72%) could be a consequence of dehydration (p < 0.05, Fig. 6A).
Fig.6
Signs and symptoms of A) reduced body fluid and B) excess body fluid were addressed by the survey. A significant number of respondents were hydration literate for one symptom each in regards to reduced and excess body fluid. For the other signs and symptoms, there was a knowledge deficit, for which certain symptoms was significant. *P-value<0.05.
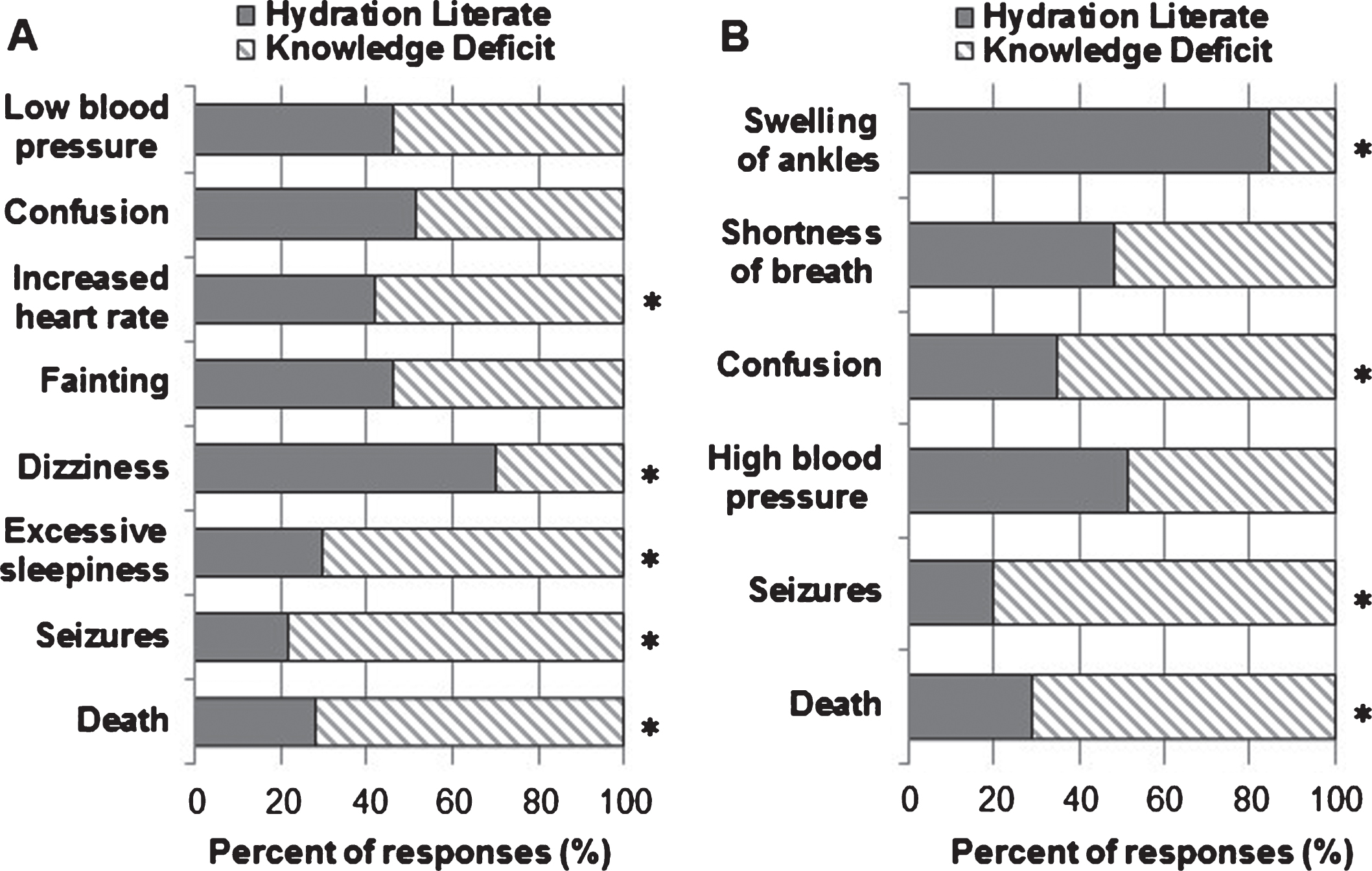
With respect to overhydration, the majority of participants knew that swelling of the ankles (84%) was a sign of overhydration (p < 0.05, Fig. 6B). However, there was a significant knowledge deficit knew regarding seizures (80%), confusion (65%), and death (71%) as complication of overhydration (p < 0.05, Fig. 6B). Common consequences of fluid overload in the elderly such as shortness of breath and high blood pressure were also only recognized by about 50% of the respondents.
4Discussion
Here, we report the results of a survey conducted to help identify health literacy needs of the elderly regarding the importance of hydration, especially with respect to various health conditions. Our results uncover significant gaps in hydration health literacy in the elderly in spite of the fact that the majority of our survey respondents reported that they consumed an adequate amount of fluid on a daily basis and acknowledged that proper hydration was important for eliminating waste. However, knowledge regarding temperature control, metabolism and circulation was less optimal and was reflected in answers to questions addressing signs and symptoms in addition to medical complications associated with inadequate hydration.
Interestingly, our findings on the amount of fluid consumed mirror the results of a study by Lindeman et al. which reported that 71% of community-dwelling elderly adults (mean age 74.1 years old) drank at least 6 glasses of water per day [39]. Other studies reported the likelihood of drinking fewer than 4 cups of water per day to be significantly higher among people over 55 years of age as opposed to young adults (47% vs. 43%, p = 0.04) [35, 36]. Specifically, the 2005-2008 NHANES study reported that adults over age 60 consumed just over 3 cups of water per day (3.1–3.5 cups/day), more than a cup less than those 20–39 years of age (4.7–5.0 cups/day) [37, 38]. However, these discrepancies could have been the result of recall bias, especially in patients with dementia, unless they or their caregivers had been instructed to document fluid intake [14].
How much fluid should elderly people actually drink each day? The standard recommendation is to drink 8 glasses of fluid per day [40], but there is some disagreement. Both Lindeman et al. and Negoianu et al. suggest that elderly people who drink 8 glasses of water per day may actually be overhydrated [39, 41]. Caution does need to be exercised in the elderly because many older people have reduced renal and/or cardiac function and a one-size-fit-all approach of 8 glasses might cause fluid-overload and exacerbate heart failure. In fact, heart failure patients are often fluid restricted to 1–1.5 liters of fluid per day in addition to being on diuretics [42, 43]. European Food and Safety Agency (EFSA) has set guidelines for adequate intake of water for healthy men and women at 2.5 L/d and 2.1 L/day respectively [44]. A recent study of total fluid intake of adults collected 7–day fluid records from adults in 13 different countries and showed wide geographical variation in the total amount of fluid consumed with only 40% of men and 60% of women complying with the EFSA guidelines [44]. This study, although large, was limited by the percentage of people in the geriatric age-group and did not have any objective measurement of hydration status.
It is important to remember that overhydration occurs not only in common conditions of heart and renal failure, it is also iatrogenic in the hospital setting and is independently associated with all cause morbidity and mortality, especially with more than 7% of positive fluid balance [45, 46]. Hence, it will be useful to have accurate and portable tools for measurement of hydration status, especially for the medically complex geriatric population with renal insufficiency and/or cardiac decompensation. A number of instruments have been developed to measure hydration status but the sensitivity and specificity of bioelectric impedance devices still requiresrefinement [47].
Why is there so much emphasis on fluid intake? Dehydration has been identified as an independent “ambulatory care-sensitive condition” or ACSC by the Agency for Healthcare Research and Quality (AHRQ) in the United Sates [17, 48]. In a large healthcare utilization study of more than 79,000 elderly patients admitted with a principal diagnosis of dehydration, about 50% had urinary tract infections and approximately the same percentage were listed as having respiratory and/or cardiac conditions [17]. A report from 2015 concluded that $1.36 billion was spent to treat elderly patients hospitalized for dehydration [16]. Hence, one might conclude that with appropriate training and education, early recognition and management of urinary tract infections, pneumonias, and heart failure might result in substantially reduced costs for dehydration-related admissions to thehospital.
There are a number of reasons why older individuals have reduced fluid consumption. The age-associated reduction of the thirst mechanism is complex and is driven partially by changes in the hypothalamic thirst sensors as well as the peripheral baroreceptors, both of which degenerate with age to a variable extent in individuals [48–50]. Stachenfeld suggested that the mechanism for diminished thirst in the elderly was secondary to a significantly reduced ability to sense a volume deficit although their ability to respond to increased osmolality was similar to that of younger adults [50]. This hypothesis is supportive of the greater age-associated atrophy of the carotid baroreceptors, which is also a cause for orthostatic hypotension in the geriatric population, especially with dehydration [50–52]. Apart from diminished thirst, older individuals often consume less fluids because of problems associated withurinary incontinence, ambulation, manual dexterity or cognition, which predisposes them to dehydration often in poorly staffed nursing facilities [52–54].
We also explored questions related to sodium and potassium balance relative to hydration because in the out-patient setting laboratory results are discussed with the patients and/or caregivers and instructions are frequently provided regarding fluids, salt or potassium intake. Reduced water intake or free water loss is generally associated with hypernatremia, or in mild cases with normal sodium concentration [7, 43]. However, in hypovolemic dehydration due to any reason (diarrhea, vomiting, burns, diuretics), there can be significant hyponatremia [43]. Overhydration can also result in hyponatremia of varying degrees and is frequently iatrogenic in elderly hospitalized patients [7, 43]. Interestingly, the majority of our participants believed that reduced fluid intake would have no effect on sodium balance. This response was concerning because it demonstrated that the elderly participants were not aware of the effect fluid intake can have on sodium balance, and the critical importance of sodium and water regulation in health and disease.
A key pituitary hormone involved in the regulation of hydration is vasopressin or anti-diuretic hormone (ADH), which is normally released in response to dehydration to signal water conservation by the nephrons [54]. Abnormal release of vasopressin occurs in the body by malignant tumors, in response to cancer medications, opiates, pulmonary infections, brain inflammation/ischemia or for idiopathic reasons, in what is termed the syndrome of inappropriate antidiuretic hormone secretion (SIADH) [54]. Management of hyponatremia is complex and can range from simple water restriction and loop diuretics to hypertonic saline or newer drugs such as the vasopressin receptor antagonists [55]. There are a few recent studies that suggest that high levels of vasopression in the blood might be associated with insulin resistance, increased hepatic steatosis and with an increased risk for development of type 2 diabetes mellitus [56–58]. Although more conclusive evidence is required, it will certainly be a very cost effective strategy to prudently encourage water consumption in order to reduce insulin resistance. A study by Godfrey et al. recommends that caregivers take a personalized approach to hydration care, making the act of drinking fluids a pleasurable experience by increasing the aesthetic appearance of a beverage or promoting social interactions [59]. This could be a promising tactic to help older people drink more fluid, and this subject will certainly benefit from furtherstudy.
4.1Gaps in health literacy
Our data indicate that older adults are not fully aware of medical conditions that cause dehydration or overhydration. For example, only about one-third of respondents knew that the loss of 3 to 4% of body fluid can lead to dehydration, and few realized that even a simple fever in an older person could cause a serious deficit in hydration level. It appears that older adults are under the impression that they must lose a large amount of fluid to become dehydrated, and they might not recognize that their specific medical conditions or medications could place them at a much higher risk for hydration-related issues. Furthermore, few respondents were familiar with the potentially serious or life-threatening consequences of dehydration. Less than one-third knew that seizures, or even death, can occur as a result of dehydration. Thus, these individuals may not adequately increase their fluid intake to cope with conditions that cause dehydration (e.g., vomiting or fever). It is also possible that caretakers or family members lack sufficient knowledge about the importance of hydration for the elderly and they may not urge the individual to drink more fluids or seek medical attention.
With respect to overhydration, few respondents understood its significance or recognized the signs and symptoms associated with it. Less than one-third were aware of the hazards of receiving intravenous fluids, blood transfusions, or steroids at an older age. Likewise, very few of the respondents knew that seizures, confusion, and death were potential complications of overhydration. Our data indicate that we must not only augment our efforts to educate older adults and their caretakers about dehydration, but we must do the same for overhydration.
Healthcare providers also need to work towards enhancing the knowledge base and health literacy of older adults regarding the close relationship of electrolytes and water. Although we do not expect non-medical personnel to acquire expertise in this complex area, the critical role of water in regulating sodium and its effect of morbidity and mortality needs to be emphasized. This might give individuals who view water consumption as relatively unimportant a new appreciation of the power of water and hydration for health. Studies have demonstrated the positive effect of education on improving thehydration status in children but such interventions have not been tried in the elderly [60].
4.2Limitations of study
Our study participants were largely educated, white, community-dwelling residents of Central Arkansas and hence our results cannot be extrapolated to the general population with greater ethnic diversity and/or lower socio-economic and educational status. We did not evaluate the cognition of participants or record fluid intake. Another issue is that people may not fully disclose their intake of certain fluids such as alcoholic beverages, or might not consider drinks such as fruit or vegetable juices as reportable sources of fluid intake. Additionally, we did not address the controversies regarding hydration in palliative care, or hospice patients. Most studies suggest that active attempts to hydrate terminally ill patients, especially intravenously, should be avoided because such efforts are futile and might actually cause more discomfort and medical complications [14, 61]. However, this is an evolving area in medicine that requires considerable education of patients and caregivers, as well as providers [62, 63].
4.3Future directions
Dehydration and overhydration are significant health issues for the elderly population. This study provided basic information about fluid intake of elderly individuals residing in the southern part of the United States and revealed that there are significant gaps in this population’s knowledge about proper hydration. We should spearhead public awareness campaigns aimed at improving the health literacy of this vulnerable population about hydration and also advocate for the implementation of programs that educate and train healthcare workers (e.g., caretakers or nursing home personnel) on this subject. Future studies should have objective records of hydration levels and correlate these with the participants’ health, medical problems, physical performance and quality of life.
Conflicts of interest
The authors declare no conflicts of interest.
ACKNOWLEDGMENTS
This study was supported in part by the Claude D. Pepper Older American Independence Center grant, National Institute on Aging (1P30AG28718) awarded to University of Arkansas for Medical Sciences. We thank Laura Gocio for her assistance with manuscript preparation.
References
[1] | Morley JE . Dehydration, hypernatremia, and hyponatremia. Clinics in Geriatric Medicine. (2015) ;31: (3):389–99. |
[2] | Shimizu M , Kinoshita K , Hattori K , Ota Y , Kanai T , Kobayashi H , Tokuda Y . Physical signs of dehydration in the elderly. Internal Medicine. (2012) ;51: (10):1207–10. |
[3] | Okuyama M , Nishida M . The physical signs of impending dehydration among elderly people in nursing homes: The association with axillary skin temperature, humidity, intraoral moisture content, and salivary components. Nihon Ronen Igakkai zasshi. Japanese Journal of Geriatrics. (2016) ;53: (4):379. |
[4] | El-Sharkawy AM , Sahota O , Maughan RJ , Lobo DN . The pathophysiology of fluid and electrolyte balance in the older adult surgical patient. Clinical Nutrition. (2014) ;33: (1):6–13. |
[5] | Schlanger LE , Bailey JL , Sands JM . Electrolytes in the aging. Advances in Chronic Kidney Disease. (2010) ;17: (4):308–19. |
[6] | Weinstein JR , Anderson S . The aging kidney: Physiological changes. Advances in Chronic Kidney Disease. (2010) ;17: (4):302–7. |
[7] | Phillips PA , Johnston CI , Gray L . Disturbed fluid and electrolyte homoeostasis following dehydration in elderly people. Age and Ageing. (1993) ;22: (suppl 1):S26–33. |
[8] | Rowat A , Graham C , Dennis M . Dehydration in hospital-admitted stroke patients. Stroke. (2012) ;43: (3):857–9. |
[9] | El-Sharkawy AM , Watson P , Neal KR , Ljungqvist O , Maughan RJ , Sahota O , Lobo DN . Hydration and outcome in older patients admitted to hospital (The HOOP prospective cohort study). Age and Ageing. (2015) ;44: (6):943–7. |
[10] | Hooper L , Bunn D , Jimoh FO , Fairweather-Tait SJ . Water-loss dehydration and aging. Mechanisms of Ageing and Development. (2014) ;136: :50–8. |
[11] | Mentes J . Oral Hydration in Older Adults: Greater awareness is needed in preventing, recognizing, and treating dehydration. AJN The American Journal of Nursing. (2006) ;106: (6):40–9. |
[12] | Schols JM , De Groot CP , Van Der Cammen TJ , Olde Rikkert MG . Preventing and treating dehydration in the elderly during periods of illness and warm weather. The Journal of Nutrition, Health & Aging. (2009) ;13: (2):150–7. |
[13] | Hodgkinson B , Evans D , Wood J . Maintaining oral hydration in older adults: A systematic review. International Journal of Nursing Practice. (2003) ;9: (3):S19–28. |
[14] | Koopmans RT , van der Sterren KJ , Van der Steen JT . The ‘natural’ endpoint of dementia: Death from cachexia or dehydration following palliative care? International Journal of Geriatric Psychiatry (2007) ;22: (4):350–5. |
[15] | Kayser-Jones J . Preventable Causes of Dehydration: Nursing home residents are especially vulnerable. AJN The American Journal of Nursing. (2006) ;106: (6):45. |
[16] | Frangeskou M , Lopez-Valcarcel B , Serra-Majem L . Dehydration in the elderly: A review focused on economic burden. The Journal of Nutrition, Health & Aging. (2015) ;19: (6):619. |
[17] | Xiao H , Barber J , Campbell ES . Economic burden of dehydration among hospitalized elderly patients. American Journal of Health System Pharmacy. (2004) ;61: (23):2534–40. |
[18] | Pellicori P , Kaur K , Clark AL . Fluid management in patients with chronic heart failure. Card Fail Rev. (2015) ;1: :90–5. |
[19] | Cotter G , Metra M , Milo-Cotter O , Dittrich HC , Gheorghiade M . Fluid overload in acute heart failure—Re-distribution and other mechanisms beyond fluid accumulation. European Journal of Heart Failure. (2008) ;10: (2):165–9. |
[20] | Khan YH , Sarriff A , Adnan AS , Khan AH , Mallhi TH . Chronic kidney disease, fluid overload and diuretics: A complicated triangle. PLoS One. (2016) ;11: (7):e0159335. |
[21] | Hung SC , Lai YS , Kuo KL , Tarng DC . Volume overload and adverse outcomes in chronic kidney disease: Clinical observational and animal studies. Journal of the American Heart Association. (2015) ;4: (5):e001918. |
[22] | Guo Q , Yi C , Li J , Wu X , Yang X , Yu X . Prevalence and risk factors of fluid overload in Southern Chinese continuous ambulatory peritoneal dialysis patients. PLoS One. (2013) ;8: (1):e53294. |
[23] | Hilton AK , Pellegrino VA , Scheinkestel CD . Avoiding common problems associated with intravenous fluid therapy. Med J Aust. (2008) ;189: (9):509–13. |
[24] | Pandey S , Vyas GN . Adverse effects of plasma transfusion. Transfusion. (2012) ;52: (s1). |
[25] | Stanbury RM , Graham EM . Systemic corticosteroid therapy—side effects and their management. British Journal of Ophthalmology. (1998) ;82: (6):704–8. |
[26] | Lobo DN . Fluid, electrolytes and nutrition: Physiological and clinical aspects. Proceedings of the Nutrition Society. (2004) ;63: (03):453–66. |
[27] | Laine GA , Allen SJ , Katz JE , Gabel JC , Drake RE . Effect of systemic venous pressure elevation on lymph flow and lung edema formation. Journal of Applied Physiology. (1986) ;61: (5):1634–8. |
[28] | Yoneda K . Anatomic pathway of fluid leakage in fluid-overload pulmonary edema in mice. The American Journal of Pathology. (1980) ;101: (1):7. |
[29] | Veiga D , Luis C , Parente D , Fernandes V , Botelho M , Santos P , Abelha F . Postoperative delirium in intensive care patients: Risk factors and outcome. Brazilian Journal of Anesthesiology. (2012) ;62: (4):469–83. |
[30] | Prowle JR , Echeverri JE , Ligabo EV , Ronco C , Bellomo R . Fluid balance and acute kidney injury. Nature Reviews Nephrology. (2010) ;6: (2):107–15. |
[31] | Malbrain ML , Marik PE , Witters I , Cordemans C , Kirkpatrick AW , Roberts DJ , Van Regenmortel N . Fluid overload, de-resuscitation, and outcomes in critically ill or injured patients: A systematic review with suggestions for clinical practice. Anaesthesiol Intensive Ther. (2014) ;46: (5):361–80. |
[32] | Boyd JH , Forbes J , Nakada TA , Walley KR , Russell JA . Fluid resuscitation in septic shock: A positive fluid balance and elevated central venous pressure are associated with increased mortality. Critical Care Medicine. (2011) ;39: (2):259–65. |
[33] | Besen BA , Gobatto AL , Melro LM , Maciel AT , Park M . Fluid and electrolyte overload in critically ill patients: An overview. World Journal of Critical Care Medicine. (2015) ;4: (2):116. |
[34] | Wizemann V , Wabel P , Chamney P , Zaluska W , Moissl U , Rode C , Malecka-Masalska T , Marcelli D . The mortality risk of overhydration in haemodialysis patients. Nephrology Dialysis Transplantation. (2009) ;24: (5):1574–9. |
[35] | Goodman AB . Behaviors and attitudes associated with low drinking water intake among US adults, Food Attitudes and Behaviors Survey, 2007. Preventing Chronic Disease. (2013) ;10. |
[36] | Kant AK , Graubard BI , Atchison EA . Intakes of plain water, moisture in foods and beverages, and total water in the adult US population—nutritional, meal pattern, and body weight correlates: National Health and Nutrition Examination Surveys 1999–2006. The American Journal of Clinical Nutrition. (2009) :ajcn-27749. |
[37] | Sebastian RS , Wilkinson C , Goldman JD . Drinking water intake in the US: What We Eat In America, NHANES 2005-2008. United States Department of Agriculture, Agricultural Research Service, (2011) . |
[38] | Yang M , Chun OK . Consumptions of plain water, moisture in foods and beverages, and total water in relation to dietary micronutrient intakes and serum nutrient profiles among US adults. Public Health Nutrition. (2015) ;18: (07):1180–6. |
[39] | Lindeman RD , Romero LJ , Liang HC , Baumgartner RN , Koehler KM , Garry PJ . Do elderly persons need to be encouraged to drink more fluids? The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. (2000) ;55: (7):M361–5. |
[40] | Lichtenstein AH , Rasmussen H , Winifred WY , Epstein SR , Russell RM . Modified MyPyramid for older adults. The Journal of Nutrition. (2008) ;138: (1):5–11. |
[41] | Negoianu D , Goldfarb S . Just add water. Journal of the American Society of Nephrology. (2008) ;19: (6):1041–3. |
[42] | Houston BA , Kalathiya RJ , Kim DA , Zakaria S . Volume overload in heart failure: An evidence-based review of strategies for treatment and prevention. In Mayo Clinic Proceedings. (2015) ;90: (9):1247–1261. Elsevier. |
[43] | Braun MM , Barstow CH , Pyzocha NJ . Diagnosis and management of sodium disorders: Hyponatremia and hypernatremia. Am Fam Physician. (2015) ;91: :299–307. |
[44] | Ferreira-Pêgo C , Guelinckx I , Moreno LA , Kavouras SA , Gandy J , Martinez H , Bardosono S , Abdollahi M , Nasseri E , Jarosz A , Babio N . Total fluid intake and its determinants: Cross-sectional surveys among adults in 13 countries worldwide. European Journal of Nutrition. (2015) ;54: (2):35–43. |
[45] | Tsai YC , Chiu YW , Tsai JC , Kuo HT , Hung CC , Hwang SJ , Chen TH , Kuo MC , Chen HC . Association of fluid overload with cardiovascular morbidity and all-cause mortality in stages 4 and 5 CKD. Clinical Journal of the American Society of Nephrology. (2015) ;10: (1):39–46. |
[46] | Malbrain ML , Marik PE , Witters I , Cordemans C , Kirkpatrick AW , Roberts DJ , Van Regenmortel N . Fluid overload, de-resuscitation, and outcomes in critically ill or injured patients: A systematic review with suggestions for clinical practice. Anaesthesiol Intensive Ther. (2014) ;46: (5):361–80. |
[47] | Sakaguchi T , Yasumura K , Nishida H , Inoue H , Furukawa T , Shinouchi K , Miura H , Miyazaki K , Hamano G , Koide M , Abe H . Quantitative assessment of fluid accumulation using bioelectrical impedance analysis in patients with acute decompensated heart failure. Circulation Journal. (2015) ;79: (12):2616–22. |
[48] | Chen LW , Zhang W , Sun J , Mueller KJ . The magnitude, variation, and determinants of rural hospital resource utilization associated with hospitalizations due to ambulatory caresensitive conditions. Journal of Public Health Management and Practice. (2009) ;15: (3):216–22. |
[49] | Kenney WL , Chiu P . Influence of age on thirst and fluid intake. Medicine and Science in Sports and Exercise. (2001) ;33: (9):1524–32. |
[50] | Stachenfeld NS , DiPietro LO , Nadel ER , Mack GW . Mechanism of attenuated thirst in aging: Role of central volume receptors. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology. (1997) ;272: (1):R148–57. |
[51] | Shibao C , Grijalva CG , Raj SR , Biaggioni I , Griffin MR . Orthostatic hypotension-related hospitalizations in the United States. The American Journal of Medicine. (2007) ;120: (11):975–80. |
[52] | Briasoulis A , Silver A , Yano Y , Bakris GL . Orthostatic hypotension associated with baroreceptor dysfunction: Treatment approaches. The Journal of Clinical Hypertension. (2014) ;16: (2):141–8. |
[53] | Marshall KA , Burson R , Gall K , Saunders MM . Hospital admissions for malnutrition and dehydration in patients with dementia. Home Healthcare Now. (2016) ;34: (1):32–7. |
[54] | Koch CA , Fulop T . Clinical aspects of changes in water and sodium homeostasis in the elderly. Reviews in Endocrine and Metabolic Disorders. (2017) ;18: (1):49–66. |
[55] | Zhang X , Zhao M , Du W , Zu D , Sun Y , Xiang R , Yang J . Efficacy and safety of vasopressin receptor antagonists for euvolemic or hypervolemic hyponatremia: A meta-analysis. Medicine. (2016) ;95: (15). |
[56] | Taveau C , Chollet C , Waeckel L , Desposito D , Bichet DG , Arthus MF , Magnan C , Philippe E , Paradis V , Foufelle F , Hainault I . Vasopressin and hydration play a major role in the development of glucose intolerance and hepatic steatosis in obese rats. Diabetologia. (2015) ;58: (5):1081–90. |
[57] | Roussel R , El Boustany R , Bouby N , Potier L , Fumeron F , Mohammedi K , Balkau B , Tichet J , Bankir L , Marre M , Velho G . Plasma copeptin, AVP gene variants, and incidence of type 2 diabetes in a cohort from the community. The Journal of Clinical Endocrinology & Metabolism. (2016) ;101: (6):2432–9. |
[58] | Carroll HA , Davis MG , Papadaki A . Higher plain water intake is associated with lower type 2 diabetes risk: A cross-sectional study in humans. Nutrition Research. (2015) ;35: (10):865–72. |
[59] | Godfrey H , Cloete J , Dymond E , Long A . An exploration of the hydration care of older people: A qualitative study. International Journal of Nursing Studies. (2012) ;49: (10):1200–11. |
[60] | Kavouras SA , Arnaoutis G , Makrillos M , Garagouni C , Nikolaou E , Chira O , Ellinikaki E , Sidossis LS . Educational intervention on water intake improves hydration status and enhances exercise performance in athletic youth. Scandinavian Journal of Medicine & Science in Sports. (2012) ;22: (5):684–9. |
[61] | Cohen MZ , Torres-Vigil I , Burbach BE , De La Rosa A , Bruera E . The meaning of parenteral hydration to family caregivers and patients with advanced cancer receiving hospice care. Journal of Pain and Symptom Management. (2012) ;43: (5):855–65. |
[62] | Dalal S , Del Fabbro E , Bruera E . Is there a role for hydration at the end of life? Curr Opin Palliat Care. (2009) ;3: (1):72–8. |
[63] | Mercadante S , Ferrera P , Girelli D , Casuccio A . Patients’ and relatives’ perceptions about intravenous and subcutaneous hydration. J Pain Symptom Manage. (2005) ;30: (4):354–8. |




