Systematic Review of Treatment of Metastatic Non-Clear Cell Renal Cell Carcinoma
Abstract
BACKGROUND:
Metastatic and unresectable non-clear cell renal cell carcinoma comprises more than a quarter of kidney cancers but does not have standardized treatment. Non-clear renal carcinoma consists of a variety of diverse histologic subtypes, including papillary, chromophobe, collecting duct, translocation, and medullary histologies, many of which carry a poor prognosis. Many prospective clinical trials exclude these kidney cancers, and for most clinical trials of non-clear cell renal cell carcinoma, only a small number of patients are enrolled.
OBJECTIVE:
To perform a systematic review of recently published and currently enrolling prospective clinical trials for advanced non-clear cell renal cell carcinoma.
METHODS:
A systematic search of Pubmed and MEDLINE (Ovid) was conducted as per PRISMA guidelines to identify recent prospective clinical trials in non-clear cell renal cell carcinoma. To ensure a thorough search, terms not only included non-clear cell renal carcinoma but also molecular subtypes. A review of currently enrolling clinical trials was conducted on Clinicaltrials.gov and the EU Clinical Trials Register as well.
RESULTS:
A total of 33 prospective clinical trials with published results and 10 currently enrolling clinicals trials were identified. About half (48.5%) of these studies were reported in 2020 or 2021, and 36.4% were in the first-line setting. Treatments investigated in these trials included mTOR inhibitors, VEGF- and MET-targeted tyrosine kinase inhibitors, immune checkpoint inhibitors, and combinatorial strategies. Outcomes from these data revealed a wide range of response rate and progression free survival, favoring TKIs and immune checkpoint inhibitors -based combination regimens.
CONCLUSIONS:
Novel targeted therapies and immunotherapies have changed the landscape of treatment for advanced non-clear cell renal cell carcinoma. Combination regimens may provide even further clinical benefit and warrant further investigation in larger, randomized prospective clinical trials.
INTRODUCTION
Kidney cancer incidence is in the top ten among both men and women, with more than 75000 estimated cases in 2020 [1]. The most common pathology is clear cell renal cell carcinoma (ccRCC), which comprises at least 70 percent of renal cancers [2]. Many landmark trials for renal cell carcinoma (RCC) exclusively included clear cell carcinoma patients [3–5], making generalization to other types of RCC difficult.
Non-clear cell RCC (nccRCC), the remaining 25–30 percent of kidney cancers, comprises several different histologies. The World Health Organization (WHO) has classified thirteen different non-clear cell malignant renal cell histologies [2]. Of these, papillary is the most common, representing 10–15 percent of kidney cancer. Papillary RCC is further subclassified into two subtypes, type 1 and type 2, based on pathology [6]. Chromophobe RCC arises from the distal nephron and accounts for approximately 5 percent of kidney cancer and often carries a favorable prognosis [7]. Collecting duct RCCs, including medullary RCC, are rarer, comprising about 1 percent of all kidney cancers. These are aggressive tumors and carry a poor prognosis [8]. Another rare histologic variant that accounts for less than 1 percent of kidney cancer is Xp11 translocation RCC [9]. In addition to the aforementioned histologic subtypes of nccRCC, mixed histologies, such as papillary clear cell RCC (2–4 percent of kidney cancers), and unclassified RCC can be observed as well. Sarcomatoid and rhabdoid features, while not a separate histology, can be found in non-clear cell as well as clear cell histologies. Sarcomatoid features are present in 4 percent of kidney cancer but 20 percent of metastatic kidney cancer and carries a poor prognosis [10].
While many clinical trials have focused solely on the more common clear cell histology, the treatment landscape of metastatic nccRCC is rapidly evolving. Several recent published clinical trials have successfully reported treatment options for these less common kidney cancers. In this systematic review, we will discuss these recent advances as well as ongoing trials that will potentially shape the current management of advanced nccRCC.
METHODS
Search strategy
A systematic literature review was conducted in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [11]. A search was conducted on the EMBASE and MEDLINE (Ovid) databases by two co-authors (J.B. and P.B.) to identify relevant studies included through June 1, 2021. Keywords used for the searches include “Kidney Cancer” OR “Renal Cell Carcinoma” AND (“Non-clear cell” OR “Papillary” OR “Medullary” OR “Chromophobe” OR “Collecting Duct”). An additional search was conducted on the US National Library of Medicine database (clinicaltrials.gov) and European Union Clinical Trials Register (clinialtrialsregister.eu) using filters for currently enrolling phase II and phase III studies to incorporate ongoing clinical trials in advanced nccRCC.
The search was conducted by the two authors independently in three stages. In the first stage, duplicate references were removed. In the second stage, titles and abstracts from all unique references selected by the database were screened. In the final stage, a full-text reading of all remaining references was performed. A final search using Google Scholar and review of references from relevant articles was performed to ensure inclusion of all eligible studies.
Exclusion criteria
Only prospective clinical trials were considered for this review, so all abstracts, editorials, reviews, retrospective analyses, non-clinically focused studies, and non-English language articles were excluded. To narrow the scope of the review, phase I trials were excluded. Prospective trials that enrolled mostly ccRCC cases without planned nccRCC subset analyses were excluded as well. Repeated publications on the same cohort were excluded as well. To ensure only the most current data was included, the analysis was limited from January 1, 2011 to June 1, 2021.
Data extraction and synthesis
From all eligible studies with published results, the treatment intervention, number of enrolled patients, primary endpoint, objective response rate, and median progression free survival were extracted. For currently enrolling trials, the trial phase and planned treatment intervention were extracted. Outcomes between studies were compared but not combined due to heterogeneity between studies, especially regarding line of treatment and proportion between histologic subtypes included. All clinical trials were organized by category of treatment intervention, including mTOR inhibition, VEGFR-targeting tyrosine kinase inhibition, MET-targeting tyrosine kinase inhibition, immune checkpoint inhibition, and treatment combinations.
RESULTS
This systematic review yielded 13,409 records through the EMBASE and MEDLINE databases (Fig. 1). Of these, 3351 were duplicates and subsequently removed for a total of 10,058 unique sources. After sources published prior to 2011 were eliminated, 6,852 records remained. Ultimately, 33 prospective phase II and phase III clinical trials that focused on treatment of advanced nccRCC were identified, which are summarized in Tables 1–3. Out of the 33 prospective studies identified, 16 (48.5%) were reported in 2020 or 2021. Five of these clinical trials (15.2%) were randomized, whereas the remainder were single arm studies. Most trials were phase II (93.9%), with one reported phase III and one phase III/IV trial. 12 trials (36.4%) exclusively enrolled papillary RCC patients, whereas the remainder included multiple histologic subtypes. Twelve trials (36.4%) treated patients in the first-line setting, while two trials were exclusively for patients refractory to prior treatments.
Fig. 1
Inclusion and exclusion criteria for systematic review of phase II and phase III prospective clinical trials for advanced non-clear cell renal cell carcinoma.
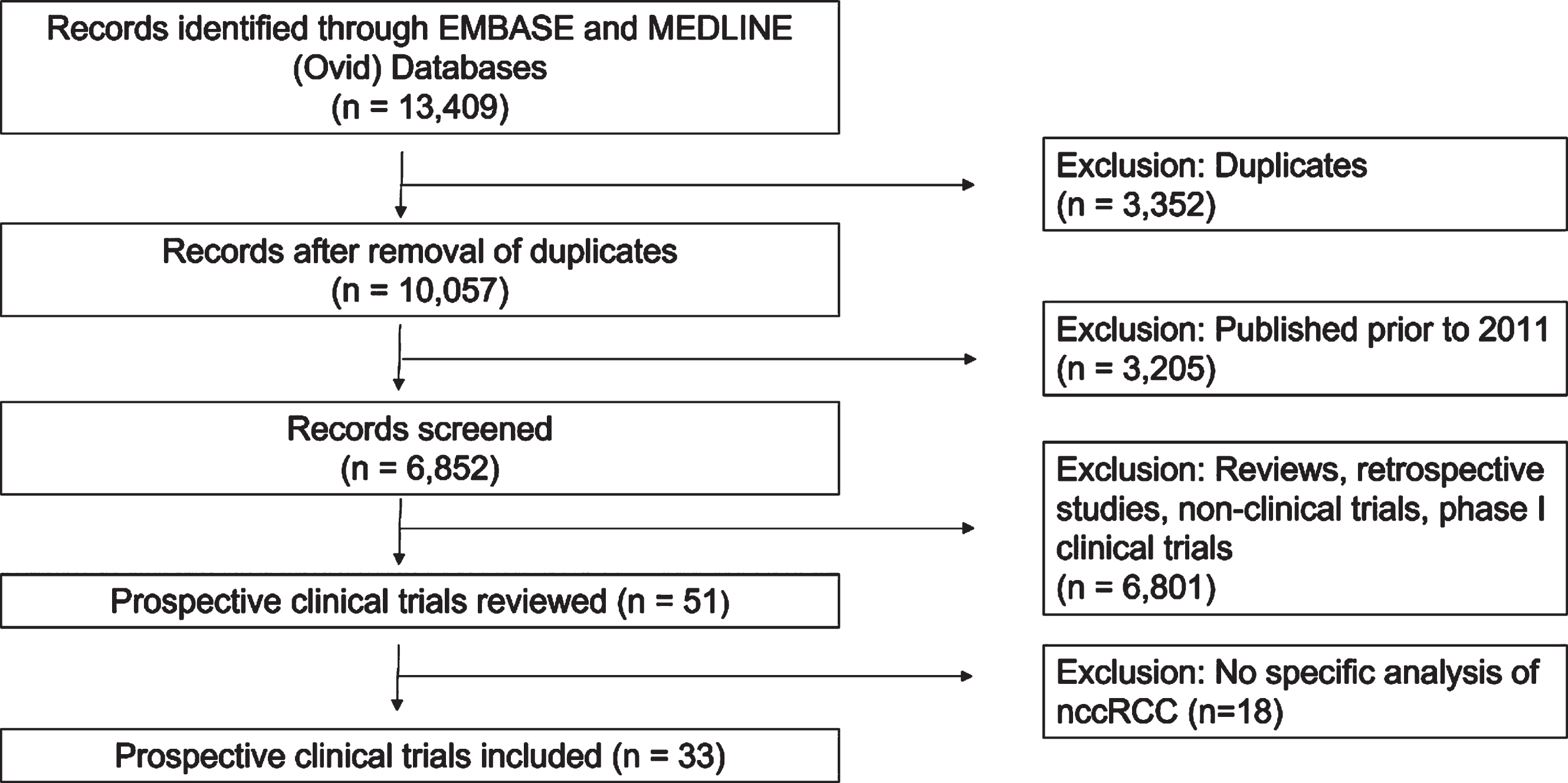
Table 1
Results of recent prospective studies of mTor inhibitors in treatment of advanced non-clear cell renal cell carcinoma
| Study/Reference | Report | Phase | Enrollment | Intervention | Disease | Histology | Primary | ORR | Median PFS |
| Date | (n) | Setting | Endpoint | (%) | (months) | ||||
| Koh et-al. [15] | 2013 | II | 49 | Everolimus | Multiple lines | Multiple subtypes | Median PFS | 10.2 | 5.2 |
| Escudier et-al. (RAPTOR) [22] | 2016 | II | 88 | Everolimus | First-line | Papillary | 6-months PFS | 1 (0–5) | 4.1 (3.6–5.5) |
| Voss et-al. [16] | 2016 | II | 35 | Everolimus+Bevacizumab | First-line | Multiple subtypes | 6-months PFS | 29 | 11.0 (3.8–19.3) |
| Feldman et-al. [17] | 2020 | II | 39 | Everolimus+Bevacizumab | First-line | Papillary variant | 6-months PFS | 35 | 13.7 (10.8–16.4) |
| Hutson et-al. [18] | 2021 | II | 31 | Everolimus+Lenvatinib | First-line | Multiple subtypes | ORR | 26 (12–45) | 9.2 (5.5-NE) |
| Mahoney et-al. [21] | 2016 | II | 13 | Temsirolimus+Bevacizumab | VEGFR-TKI refractory | Multiple subtypes | 4-months PFS | 7.7 | 5.6 (3.4–13.7) |
Table 2
Results of recent prospective studies of tyrosine kinase inhibitors advanced non-clear cell renal cell carcinoma
| Study/Reference | Report Date | Phase | Enrollment (n) | Intervention | Disease Setting | Histology | Primary Endpoint | ORR (%) | Median PFS (months) |
| Molina et-al. [29] | 2012 | II | 23 | Sunitinib | Multiple lines | Multiple subtypes | ORR | 4.5 | 5.5 (2.5–7.1) |
| Tannir et-al. [30] | 2012 | II | 55 | Sunitinib | ≤2 prior systemic therapies | Multiple subtypes | ORR and PFS | 5 | 2.7 (1.4–5.4) |
| Lee et-al. [31] | 2012 | II | 31 | Sunitinib | Any line | Multiple subtypes | ORR | 36 (19–52) | 6.4 (4.2–8.6) |
| Ravaud et-al. [52] (SUPAP) | 2015 | II | 61 | Sunitinib | First-line | Papillary | ORR | 11.7 | 6.6 (2.8–14.8) (type 1 pRCC) |
| 5.5 (3.8–7.1) (type 2 pRCC) | |||||||||
| Tannir et-al. [25] (ESPN) | 2016 | II | 68 | Sunitinib vs. Everolimus | First-line | Multiple subtypes | PFS | 9 vs. 3 | 6.1 (4.2–9.4) vs. 4.1 (2.7–10.5) |
| (not significant) | |||||||||
| Armstrong et-al. [26] (ASPEN) | 2016 | II | 109 | Sunitinib vs. Everolimus | First-line | Multiple subtypes | PFS | 18 vs. 9 | 8.3 (5.8 –11.4) vs. 5.6 (5.5–6.0) |
| (significant) | |||||||||
| Bergmann et-al. [28] | 2020 | II | 22 | Sunitinib vs. Temsirolimus | First-line | Multiple subtypes | PFS | 30 vs. 16.7 | 13.2 vs. 9.3 |
| (not significant) | |||||||||
| Jung et-al. [34] | 2018 | II | 29 | Pazopanib | Multiple lines, no prior TKI | Papillary, chromophobe, unclassified | ORR | 28 (12–44) | 16.5 (10.9–22.1) |
| Costello et-al. [35] (PINCR) | 2020 | II | 35 | Pazopanib | ≤1 prior systemic therapies | Multiple subtypes | 12-months OS | 11 | 7.5 (5.0–11.0) |
| Park et-al. [36] | 2018 | II | 40 | Axitinib | Temsirolimus-refractory | Multiple subtypes | PFS | 37.5 | 7.4 (5.2–9.5) |
| Negrier et-al. [53] (AXIPAP) | 2020 | II | 44 | Axitinib | First-line | Papillary | 24-week PFS | 28.6 (15.7–44.6) | 6.6 (5.5–9.2) |
| Choueiri et-al. [44] | 2012 | II | 74 | Foretinib | ≤1 prior systemic therapies | Papillary | ORR | 13.5 (6.7–23.5) | 9.3 (6.9–12.9) |
| Choueiri et-al. [47] | 2017 | II | 111 | Savolitinib | Multiple lines | Papillary | ORR | 7 | MET-driven: 6.2 (4.1–7.0) |
| MET-independent: | |||||||||
| 1.4 (1.4–2.7) | |||||||||
| Schoffski et-al. [48] (CREATE) | 2017 | II | 23 | Crizotinib | Multiple lines | Type 1 Papillary | ORR | 17.4 (4.9–38.8) | 5.8 (2.6–30.5) |
| Twardowski et-al. [49] | 2017 | II | 50 | Tivatinib+/- Erlotinib | ≤1 prior systemic therapies | Papillary | ORR | 0 | Single agent: 2.0 (1.8–3.0) |
| Combination: 3.9 (1.8–7.3) | |||||||||
| Srinivasan et-al. [50] | 2020 | II | 83 | Erlotinib+Bevacizumab | ≤2 prior VEGF-TKI therapies | HLRCC or sporadic papillary | ORR | 51 (40–61) | 21.1 (15.6–26.6) |
| Leger et-al. [51] | 2020 | II | 20 | Capmatinib | ≤4 prior systemic therapies | Type 1 Papillary | ORR | 15 | TBD |
| Procopio et-al. [41] (BONSAI) | 2021 | II | 25 | Cabozantinib | First-line | Collecting duct | ORR | 35 | 6 |
| Choueiri et-al. [45] (SAVIOR) | 2020 | III | 60 | Savolitinib vs. Sunitinib | Multiple lines | MET-driven Papillary | PFS | 27 (13.3–45.5) vs. 7 (0.9–24.3) | 7.0 (2.8-NE) vs. 5.6 (4.1–6.9) |
| (not significant) | |||||||||
| Pal et-al. [38] (PAPMET) | 2021 | II | 147 | Cabozantinib vs. Sunitinib (and Savolitinib, Crizotinib) | ≤1 prior systemic therapies | Papillary | Median PFS | 23 vs. 4 | 9.0 (5.6–12.4) vs. 5.6 (2.9–6.7) (significant) |
Table 3
Results of recent prospective studies of immune checkpoint inhibition in advanced non-clear cell renal cell carcinoma
| Study/Reference | Report | Phase | Enrollment | Intervention | Disease | Histology | Primary | ORR | Median |
| (months) | Date | (n) | Setting | Endpoint | (%) | PFS | |||
| Vogelzang et-al. [54] (CHECKMATE374) | 2020 | III/IV | 44 | Nivolumab | ≤3 prior systemic therapies | Multiple subtypes | High grade immune AEs | 13.6 (5.2–27.4) | 2.2 (1.8–5.4) |
| Gedye et-al. [55] (UNISON) | 2021 | II | 83 | Niviolumab | Multiple lines | Multiple subtypes | ORR | 17 | 4.0 (3.6–7.4) |
| Atkins et-al. [56] (HCRN G16-260) | 2021 | II | 35 | Nivolumab → Ipilimumab + Nivolumab | First-line | Papillary, chromophobe, unclassified | 1-year PFS | 14.3 6.3 | 4.0 (2.7–4.3) Not reported |
| Mcdermott et-al. [57] (KEYNOTE427-Cohort B) | 2021 | II | 165 | Pembrolizumab | First-line | Papillary, chromophobe, unclassified | ORR | 26.7 (20.1–34.1) | 4.2 (2.9–5.6) |
| McGregor et-al. [58] | 2019 | II | 65 | Atezolizumab + Bevacizumab | Multiple lines | Multiple subtypes | ORR | 26 | 8.3 |
| Powles et-al. [64] (CALYPSO) | 2020 | II | 42 | Savolitinib + Durvalumab | Multiple lines | Papillary | ORR | 27 | 4.9 (2.5–12.0) |
| Lee et-al. [67] (CA209-9KU) | 2021 | II | 47 | Nivolumab + Cabozantinib | ≤1 prior systemic therapies | Multiple subtypes | ORR | 48 (31.5–63.9) | 12.5 (6.3–16.4) |
An additional 121 trials were identified on clinicaltrials.gov, of which 27 were actively enrolling patients, and 10 fit the criteria of being prospective interventional studies that exclusively enrolled patients with non-clear cell renal cell carcinoma (Table 4). A similar search on the EU clinical trials registry yielded 10 results, of which 3 fit the prespecified criteria. All three trials were duplicates of currently enrolling trials identified on clinicaltrials.gov.
Table 4
Ongoing prospective clinical trials in non clear-cell renal cell carcinoma
| Study | Launch Date | Phase | Intervention | Disease Setting | Histology | Reference |
| NCT03541902 (CABOSUN Ii) | 2018 | II | Cabozantinib vs. Sunitinib | Multiple lines | Multiple subtypes | [42] |
| NCT03685448 (UNICAB) | 2019 | II | Cabozantinib | Refractory | Multiple subtypes | [43] |
| NCT03075423 (SUNIFORECAST) | 2017 | II | Ipilimumab + Nivolumab | First-line | Multiple subtypes | [62] |
| NCT03274258 | 2017 | II | Ipilimumab + Nivolumab | Multiple lines | Medullary | [63] |
| NCT05043090 (SAMETA) | 2021 | III | Savolitinib + Durvalumab vs. Sunitib vs. Durvalumab | First-line | MET-driven papillary | [66] |
| NCT04267120 (LENKYN) | 2020 | II | Pembrolizumab + Lenvatinib | First-line | Multiple subtypes | [68] |
| NCT04704219 (KEYNOTE-B61) | 2021 | II | Pembrolizumab + Lenvatinib | First-line | Multiple subtypes | [69] |
| NCT04413123 | 2020 | II | Ipilimumab + Nivolumab + Cabozantinib | Multiple lines | Multiple subtypes | [70] |
| NCT04068831 | 2019 | II | Avelumab + Talazoparib | Second-Line or later | FH- and SDH- Deficient | [71] |
| NCT04644432 | 2020 | II | Based on DNA and RNA signatures | First-Line | Multiple subtypes | [93] |
Studies will be presented according to mechanism of action of therapeutic agents, which generally fit into four categories. The first category is mTOR inhibitors that target this signaling pathway, including everolimus and temsirolimus. Four single arm clinical trials and multiple arm trials used mTOR inhibitors. A second category is tyrosine kinase inhibitors (TKI) that target molecular alterations implicated in RCC carcinogenesis, notably VEGFR, and MET. 14 completed single arm trials and 2 currently enrolling studies exclusively treated patients with TKIs. All 5 multi-arm studies compared TKIs to other TKIs or mTOR inhibitors. Another category of treatment for nccRCC is immune checkpoint inhibition, targeting the PD-1/PD-L1 axis. Seven clinical trials, including two of which are currently enrolling patients, treated patients with immune checkpoint inhibitors. The final category that is being explored is combination between immunotherapy and TKIs, which included two trials with reported results and four currently enrolling trials.
mTOR inhibitors
The PI3K/Akt/mTOR signaling pathway was one of the first targeted by direct inhibition in kidney cancer. This pathway has been found to be dysregulated in RCC, resulting in aggressive tumors and overall poor prognosis [12, 13]. Everolimus and temsirolimus were both mTOR inhibitors previously approved for RCC treatment, however early studies primarily focused on the clear cell subtype. One of these early studies was REACT, which was an expanded access trial that provided everolimus to metastatic RCC patients refractory to VEGF-targeted therapy. Although this study primarily enrolled ccRCC patients, a subgroup analysis considered 75 patients with nccRCC and demonstrated 1.3% ORR and median PFS of 12.4 weeks [14]. Later prospective trials evaluated everolimus in management of advanced nccRCC. One such multicenter phase II trial enrolled 49 patients, who were treated with everolimus. In this trial, reported median PFS, the primary endpoint, was 5.2 months, which was significantly highest in chromophobe RCC (p = 0.084). Secondary endpoints included ORR, which was 10.2%, and median OS, which was 14.0 months [15].
Everolimus has also been studied in combination with other treatments. A single-institution trial evaluated the combination of everolimus and bevacizumab for front-line treatment. 35 patients were treated, 23 of whom had unclassified RCC. The primary endpoint was PFS at 6 months, which was 53%, and this significantly associated with histology (p < 0.001). Highest PFS rate was seen in chromophobe RCC, papillary RCC, or unclassified RCC with papillary features [16]. This cohort was subsequently expanded to include a total of 39 patients with papillary features, including 20 from the original cohort. By enrolling patients with this subtype with a more favorable response, 6-month PFS, the primary endpoint improved from 53% to 78% and ORR improved slightly from 29% to 35%. Median PFS was 13.7 months (95% CI 10.8–16.4), and median OS was 33.9 months (95% CI 23.3–71.9). No significant differences were seen between papillary RCC and unclassified RCC with papillary features [17].
Another phase II trial of 31 patients investigated the combination of everolimus and lenvatinib, a multikinase inhibitor, for first-line treatment of advanced nccRCC. ORR, the primary endpoint, was reported as 26% (95% CI 12–45). ORR amongst papillary RCC was 15% (95% CI 3–38) and for chromophobe RCC was 44% (95% CI 14–79). Median PFS by investigator assessment was 9.2 months (95% CI 5.5-NE) and median OS was 15.6 months (95% CI 9.2-NE). This combination met its prespecified endpoint and demonstrated promising efficacy compared to single agent everolimus or TKIs [18].
Temsirolimus is another mTOR inhibitor that is administered intravenously. The ARCC study was a multicenter phase III trial that compared temsirolimus to interferon-alpha in advanced RCC [19]. In a subsequent exploratory analysis of 73 patients exhibiting non-clear cell histology (18% of the entire cohort), median OS with temsirolimus was 11.6 months (95% CI 8.9–14.5) compared to the interferon arm 4.3 months (95% CI 3.2–7.3). Median PFS for the termsirolimus arm was 7.0 months (95% CI 3.9–8.9) and for the interferon arm was 1.8 months (95% CI 1.6–2.1). Reported OS hazard ratio was 0.49 (95% CI 0.29–0.85) and PFS hazard ratio was 0.38 (95% CI 0.23–0.62), indicating significantly improved survival with temsirolimus in the subset of patients with nccRCC [20]. Temsirolimus was also evaluated in combination with bevacizumab in a phase II trial of patients who were refractory to VEGF-based tyrosine kinase inhibition. In the subset of 13 patients with nccRCC, ORR was 7.7% and clinical benefit rate was 76.9%. Median PFS was 5.6 months (95% CI 3.4–13.7), and median OS was 13.1 months (95% CI 5.0–24.6), neither of which were statistically different from the simultaneously treated ccRCC cohort [21].
Studies also evaluated mTOR inhibitors in specific histologic subtypes. RAPTOR, a phase II multicenter prospective trial analyzed the efficacy of everolimus in metastatic papillary RCC. Primary endpoint was 6-months PFS in the 46-patient per protocol population. This was reported as 34% (80% CI 25–45), whereas 6-month PFS in the 88-patient intent-to-treat population at final analysis was 33% (80% CI 26–40). In the intent-to-treat population, median PFS was 4.1 months (95% CI 3.6–5.5), and median OS was 21.4 months (95% CI 15.4 –28.4) [22]. For metastatic chromophobe RCC, a separate retrospective study compared treatment with mTOR inhibitors and antiangiogenic agents but found no significant differences in OS, ORR, or time to treatment failure [23].
Tyrosine kinase inhibitors
Sunitinib, a multikinase inhibitor that targets VEGFR, PDGFR, and c-kit, is active in patients with localized and metastatic RCC. This agent became one of the first TKIs to be used in nccRCC after demonstrating improved progression-free survival compared to sorafenib, another VEGFR-targeting TKI [24]. Two prospective randomized trials, ESPN and ASPEN, directly compared sunitinib to everolimus in metastatic nccRCC. In the ESPN trial, 68 patients were treated prior to planned interim analysis. This was a negative trial, as there was no significant difference between PFS amongst the two arms, as median PFS was 6.1 months (95% CI 4.2–9.4) in the sunitinib arm and 4.1 months (95% CI 2.7–10.5) in the everolimus arm (p = 0.6). At final analysis, there was no significant difference in overall survival, 16.2 months (95% CI 14.2-NA) in the sunitinib arm and 14.9 months (95% CI 8.0–23.4) in the everolimus arm (p = 0.18) [25]. The ASPEN trial enrolled 108 patients and met its prespecified level of significance for primary endpoint, PFS. Median PFS in the sunitinib arm was 8.3 months (80% CI 5.8–11.4) compared to 5.6 months (80% CI 5.8–11.4) in the everolimus arm (HR 1.41, 80% CI 1.03–1.92, p = 0.16). In subgroup analysis, PFS was improved in the sunitinb arm for papillary and unclassified RCC and improved in the everolimus arm for chromophobe RCC. There was no significant difference in median OS between sunitinib, 31.5 months (95 % CI 14.8-NR) and everolimus, 13.2 months (95% CI 9.7–37.9) with reported HR 1.12 (95% CI 0.7–2.1, p = 0.6). ORR was 18% (95% CI 7–28) in the sunitinib arm and 9% (95% CI 1–16) in the everolimus arm [26]. Further biomarker analysis from this trial evaluated twenty-three plasma-based angiokines. OPN, HGF, and VCAM-1 were found to be prognostic for worse OS, however no angiokines were found to predict comparative outcomes with sunitinib and everolimus [27].
Similarly, in the phase II study sponsored by CESAR, sunitinib was compared to temsirolimus in 22 patients with advanced RCC. This trial did not achieve its prespecified endpoint, as the difference in median PFS between sunitinib and temsirolimus, 13.2 vs 9.3 months, was not statistically significant. There was also no significant difference in median OS, 19.8 vs. 19.4 months [28].
Despite low response rates in many single-arm trials, sunitinib remains a treatment option for advanced nccRCC. Three initial prospective single-arm phase II clinical trials addressed the efficacy of sunitinib in treatment of either first-line or refractory metastatic nccRCC. One single-institution trial enrolled 23 patients with metastatic nccRCC. Only one evaluable patient (4.5%) achieved partial response, however 65% of patients had a best response of stable disease. Median PFS was 5.5 months (95% CI 2.5–7.1) and was 5.6 months (95% CI 1.4–7.1) for patients with papillary histology [29]. In another trial with 55 evaluable patients, overall response rate (ORR) was 5%, however disease control rate, which included stable disease, was 58%. These rates were relatively higher with chromophobe pathology, 40% and 100%, respectively and lower with papillary pathology, 0% and 48%, respectively. Median progression-free survival (PFS) was 2.7 months (95% CI 1.4–5.4) [30]. Another phase II study enrolled 31 patients and demonstrated higher ORR at 36% with an additional 55% of patients having stable disease. Median PFS in this trial was also better at 6.4 months (95% CI 4.2–8.4) and expected median overall survival (OS) was 25.6 months [31]. Distribution of histologic subtypes was similar between the three trials, with the main difference being a higher proportion of collecting duct RCC in the trial with lowest progression free survival [30].
Real world data has mirrored findings from prospective clinical trials of sunitinib. An expanded access study of sunitinib in metastatic RCC analyzed responses in patients with nccRCC, which comprised 532 patients, or 12% of the overall study. Amongst this subset, objective response was 8%, compared with 16% in the overall cohort. Clinical benefit rate, including patients with stable disease was 51% in the non-clear cell subset, compared with 61% for all RCC patients in the study [32].
Pazopanib is another multikinase inhibitor that targets VEGFR, PDGFR, c-kit, and FGFR. First-line pazopanib for metastatic nccRCC was evaluated by the retrospective PANORAMA study. This study showed a 27% response rate and 81% disease control rate. Median PFS was 15.9 months (95% CI 5.9–25.8) and median OS was 17.3 months (95% CI 11.5–23.0) [33]. A single-arm phase II trial evaluated pazopanib for locally advanced and metastatic nccRCC. Results were similar with 28% response rate and 89% disease control rate. Median PFS was 16.5 months (95% CI 10.9–22.1), and median OS was not met at the time of publication, however 69% survival was reported within one year of follow-up [34]. Another single-arm phase II trial evaluated pazopanib in 35 patients with metastatic nccRCC. Primary endpoint was 12-months OS, reported at 65.7% (90% CI 50.5–78.9). ORR was 11% and disease control rate 71%, which was slightly lower than the other prospective pazopanib trial. Median PFS was 7.5 months (90% CI 5.0–11.0) and median OS was 18.9 months (90% CI 13.0-NE) [35].
Another multikinase inhibitor used to treat RCC is axitinib, which targets VEGFR1-3, PDGFR, and c-kit. Prospective clinical trials have evaluated its efficacy in treating non-clear cell histologies. A multi-center phase II trial that enrolled forty patients previously treated with temsirolimus demonstrated 37.5% response rate and 67.5% disease control rate. Median PFS in this study was 7.4 months (95% CI 5.2–9.5), meeting the prespecified primary endpoint, and median OS was 12.1 months (95% CI 6.4–17.7) [36].
Tyrosine kinase inhibitors in specific RCC histologies
The HGF/MET kinase signaling pathway has been implicated in tumorigenesis, metastasis, and invasiveness in renal cell carcinoma. In papillary RCC samples, MET alterations are prevalent. One study identified copy number alterations in 81% of type I papillary RCC and 46% of type II papillary RCC samples, and somatic mutations in MET were identified in 21.6% of type I papillary RCC [37]. Given the prevalence of MET alterations in RCC, this is an intriguing potential therapeutic target. Cabozantinib, a TKI that targets c-MET and VEGFR2 was compared to cabozantinib, crizotinib and savolitinib in the phase II SWOG 1500 PAPMET study. In this clinical trial, 90 patients were treated with either sunitinib or cabozantinib. Median PFS, primary endpoint of this trial, was 9.0 months (95% CI 5.6–12.4) for cabozantinib and 5.6 months (95% CI 2.9–6.7) for sunitinib, with significantly improved HR for PFS of 0.60 (95% CI 0.37–0.97; p = 0.019). ORR was also significantly higher in the cabozantinib arm (23% vs. 4%, p = 0.010), with 5% of patients demonstrating complete response. There was no significant difference in overall survival between the four treatment groups, with reported median OS of 20.0 months (95% CI 11.3-NR) in the cabozantinib arm and 16.4 months (95% CI 12.8–21.6) in the sunitinib arm [38]. In addition to comparing cabozantinib and sunitinib, the SWOG 1500 PAPMET trial enrolled an additional 57 patients to crizotinib and savolitinib arms. Both arms were closed due to hazard ratio for PFS greater than 1 at prespecified interim analysis. Retrospective studies had similarly previously reported activity of cabozantinib in nccRCC, including histologies other than papillary, with similar response rate and PFS to that found in the PAPMET trial [39, 40].
The BONSAI trial evaluated cabozantinib as first-line treatment for metastatic collecting duct RCC. 25 patients were enrolled, and reported ORR was 35%, with one patient achieving complete response. Reported median PFS was 6 months [41]. Similar to PAPMET, the ongoing phase II CABOSUN Ii trial will also compare cabozantinib to sunitinib, however this study includes all histologic subtypes of metastatic nccRCC [42]. Another currently enrolling clinical trial, UNICAB, is enrolling advanced nccRCC patients who progressed on immunotherapy. Unlike PAPMET and CABOSUN Ii, UNICAB is a single arm study [43].
Foretinib is a dual MET/VEGFR2 inhibitor. In a phase II study that enrolled 74 patients with locally advanced, bilateral multifocal, or metastatic papillary RCC, ORR, the primary endpoint, was 13.5% (95% CI 6.7–23.5). Median duration of response in this trial was 18.5 months. Reported PFS was 9.3 months (95% CI 6.9–12.9), which was slightly higher with intermittent dosing compared to continuous dosing (11.6 vs. 9.1 months). Median OS was not yet reached, but 1-year OS was 70% overall. In retrospective biomarker analysis, germline MET mutation predicted response, however somatic MET mutations, amplifications, or gain of chromosome 7 did not correlate with drug response [44].
Savolitinib is a selective MET inhibitor that was also investigated in advanced papillary RCC. This was compared to sunitinib for treatment of MET-driven unresectable, locally advanced, or metastatic papillary RCC in the SAVIOR trial. This trial was prematurely closed due to a concurrent retrospective molecular epidemiologic study that determined MET-driven status did not negatively predict outcomes for treatment with sunitinib, and therefore only 60 patients were treated rather than the planned enrollment of 180 patients [45, 46]. In terms of the primary endpoint, PFS, there was not a statistically significance between the arms (HR 0.71, 95% CI 0.4–1.4, p = 0.31). Median PFS was 7.0 months (95% CI 2.8-not calculated) in the savolitinib arm and 5.6 months (95% CI 4.1–6.9) in the sunitinib arm. There was also not a significant difference in terms of OS (HR 0.51, 95% CI 11.9-not calculated, p = 0.11) [45].
Selective MET-inhibition has also been studied in single-arm multicenter trials. One phase II trial enrolled 111 patients, 40% of whom had a MET-driven papillary RCC. The primary endpoint, ORR was 7%, although this was increased to 18% where MET alterations were present, compared to 0% for patients with MET-independent tumors (p = 0.002). Stable disease was also comparatively higher in the MET-driven papillary RCC (50% vs. 24%). Median PFS was also significantly longer in the subset of patients with MET-driven tumor, 6.2 months (95% CI 4.1–7.0) compared to 1.4 months (95% CI 1.4–2.7) in the MET-independent subset, and hazard ratio between these subsets was 0.33 (95% CI 0.20–0.52, p = 0.001) [47].
Other MET-targeting TKIs studied in advanced nccRCC include crizotinib, tivatinib, and capmatinib. The EORTC 90101 CREATE trial was a prospective phase II trial that treated 23 patients with locally advanced and metastatic type I papillary RCC, of which 4 had mutations in MET, with crizotinib. ORR, the primary endpoint, in the MET+ subset was 50% (95% CI 6.8–93.2), which was higher than 6.3% (95% CI 0.2–30.2) in the MET–subset. 1-year PFS was also higher in the MET+ patient subset at 75% (95% CI 12.8–96.1) vs. 27.3% (95% CI 8.5–50.4), and median PFS for the overall cohort was 5.8 months (95% CI 2.6–30.5). 1-year OS was similar between both subsets at 75.0% (95% CI 12.8–96.1) vs. 71.8% (95% CI 41.1–88.4), with median OS overall of 30.5 months (95% CI: 12.3-not reached) [48]. A phase II study evaluated tivatinib as a single agent and in combination with erlotinib, an EGFR-targeting TKI that has potential efficacy in FH-deficient RCC, with 25 patients enrolled on each arm. Primary endpoint was ORR, which was 0% in both arms. Median PFS was 2.0 months (95% CI 1.8–3.0) in the single-agent arm and 3.9 months (95% CI 1.8–7.3) in the combination arm. Median OS was 10.3 months (95% CI 7.3–15.7) in the former arm and 21.9 months (95% CI 6.7–21.9) in the latter arm [49]. Erlotinib as a single agent was also evaluated in combination with bevacizumab in a phase II trial that enrolled 42 patients with HLRCC and 41 patients with sporadic papillary RCC. Efficacy was much higher than in the tivatinib study, as reported primary endpoint, ORR was 51% (95% CI 40–61) overall. Median PFS was 14.2 months (95% CI 11.4–18.6). For both ORR and median PFS, better response was seen in the HLRCC subset than the sporadic papillary RCC cohort with 64% ORR (95% CI 49–77) and 21.1 months median PFS (95% CI 15.6–26.6) reported in patients with HLRCC. In the sporadic papillary RCC subset, ORR was 37% (95% CI 24–52) and median PFS was 8.7 months (95% CI 6.4–12.6) [50]. Another phase II study is evaluating capmatinib, a selective MET inhibitor in advanced papillary RCC and reported a 15% ORR with 35% of patients attaining stable disease, however survival data has not yet been reported [51].
In the first-line setting of treatment for advanced nccRCC, sunitinib has been studied in papillary RCC. SUPAP, a prospective stage II single-arm study, investigated sunitinib as first-line treatment for metastatic or locally advanced papillary RCC. ORR was 11.7% with an additional 58.3% achieving stable disease. Stable disease rate was higher in the patients with type 1 papillary RCC. Median progression free survival was 6.6 months (95% CI 2.8–14.8) for type 1 and 5.5 months (95% CI 3.8–7.1) for type 2. Median overall survival was 17.8 months (95% CI 5.7–26.1) for type 1 and 12.4 months (95% CI 8.2–16) for type 2 [52].
Another phase II single-arm prospective trial treated 44 patients with papillary RCC with axitinib. Primary endpoint of this study was progression free rate at 24 weeks, which was 45.2% (95% CI 32.6-+∞). ORR was 28% (95% CI 15.7–44.6), and disease control rate was 90.5%. Response rate was higher in the type 2 papillary subset (35.7%) compared to type 1 papillary RCC (7.7%). Median PFS was 6.6 months (95% CI 5.5–9.2), which was similar between type 1 and type 2. Median OS was 18.9 months (95% CI 12.8 –NR) [53].
Immunotherapy
Immune checkpoint inhibition has demonstrated promise for treatment of advanced nccRCC. Prospective trials of immune checkpoint inhibitors, including nivolumab, pembrolizumab, and atezolizumab have demonstrated efficacy in advanced nccRCC. CHECKMATE-374 was a phase III/IV trial that investigated nivolumab in refractory advanced nccRCC. This trial enrolled forty-four patients, and primary endpoint was number of high-grade immune-mediated adverse events, of which there were none. In terms of secondary efficacy endpoints, ORR was 13.6% (95% CI 5.2–27.4) with 2.3% of patients exhibiting complete response and 36.4% of patients with stable disease. Median PFS was 2.2 months (95% CI 1.8–5.4), and 14.0% (95% CI 5.4–26.5) of patients exhibited PFS after 12 months. Median OS was 16.3 months (95% CI 9.2-NE), and 52.8% (95% CI 36.2–67.0) of patients survived beyond 12 months. Median OS was higher (16.3 months vs. 11.8 months) in patients with tumor PD-L1 expression≥1% [54]. The UNISON trial (ANZUP 1602) treated 83 patients with advanced nccRCC with nivolumab. Reported ORR with nivolumab monotherapy was 17%, with 3.6% of patients achieving complete response and another 49% with stable disease. Median PFS was 4.0 months (95% CI 3.6–7.4) and PFS was 30% (95% CI 21–40%) at one year [55]. Another phase II trial of patients with advanced nccRCC, HCRN G16-260-Cohort B, treated 35 patients with nivolumab. Reported ORR was 14.3% (95% CI 4.8–30.3), and ORR was 25% for patients with PD-L1 greater than 20%. Median PFS was 4.0 months (95% CI 2.7–4.3) [56].
Pembrolizumab, another PD-1 targeting drug, was investigated for first-line management of advanced nccRCC in the phase II KEYNOTE-427 trial – cohort B. This single-arm trial enrolled 165 treatment naïve patients with different nccRCC histologies, of which the majority (72%) were papillary. ORR was 26.7% (95% CI 20.1–34.1), with 6.7% of patients achieving complete response. Median PFS was 4.2 months (95% CI 2.9–5.6), and median OS was 28.9 months (95% CI 24.3-NR). For patients with higher PD-L1 expression, measured as CPS≥1, higher ORR, median PFS, and median OS were observed. Higher ORR was observed with papillary (28.8%) and unclassified (30.8%) histology than with chromophobe histology (9.5%) [57].
A phase II study evaluated the combination of atezolizumab, an anti-PD-L1 antibody, and bevacizumab in 42 patients with metastatic nccRCC. ORR, primary endpoint of the study, was 26%. ORR was significantly higher in PD-L1 positive (67%) than in PD-L1 negative (14%) patients (p = 0.02). Median PFS, which included patients with sarcomatoid features, was 8.3 months (95% CI 5.7–10.9) [58]. These studies have demonstrated promise for immunotherapy in treatment in advanced nccRCC.
Immunotherapy has been especially promising in sarcomatoid variant RCC, which can be observed in both clear cell or nonclear cell histologies. IMMotion 151 was a phase III study that compared atezolizumab and bevacizumab to sunitinib for first-line treatment for inoperable RCC. A planned subgroup analysis examined 142 patients with sarcomatoid features, 19% of whom exhibited nonclear cell histology. Median PFS was reported at 8.3 months (95% CI 5.4–12.9) in the immunotherapy arm compared to 5.3 months (95% CI 3.3–6.7) in the sunitinib arm, and hazard ratio was 0.52 (95% CI 0.34–0.79). This effect was even more pronounced in patients with PD-L1 positive tumor, where hazard ratio for PFS was 0.45 (0.26–0.77). Median OS in the immunotherapy arm was 21.7 months (95% CI 15.3-NE) compared to 15.4 months (10.4–19.5) in the sunitinib arm, and reported hazard ratio was 0.64 (95% CI 0.41–1.01) [59]. In KEYNOTE-427, a subset of 38 patients exhibited sarcomatoid differentiation. ORR was 42.1% (95% CI 26.3–59.2), median PFS was 6.9 months (95% CI 2.8–15.4), and median OS was 25.5 months (95% CI 13.1–30.0), all of which were higher than the overall cohort [57]. A phase II trial of atezolizumab and bevacizumab included patients with sarcomatoid features, including 8 with nccRCC. ORR for these patients was 38%, which was higher than ORR for overall nonclear cell histology (26%) but lower than clear cell histology with sarcomatoid features (50%) [58]. This finding is in line with a retrospective analysis that compared patients with sarcomatoid ccRCC to nccRCC. In this analysis ORR was 14.3% (95% CI 0.4–57.9) in nccRCC compared to 35.4% (95% CI 23.4–49.6). Median PFS (HR 0.25, 95% CI 0.08–0.78, p = 0.0145) and median OS (HR 0.13, 95% CI 0.04–0.44, p = 0.0009) were both significantly improved in sarcomatoid ccRCC compared to nccRCC with sarcomatoid features [60]. Therefore, while immunotherapy has demonstrated benefit for sarcomatoid RCC, further studies are necessary to determine the utility of this treatment for nccRCC with sarcomatoid features.
Immunotherapy combinations
While single-agent immunotherapy drugs have demonstrated promise in treatment of advanced nccRCC, there may even be greater benefit in combinations with other immune checkpoint inhibitors or targeted small molecule inhibitors. A phase II study, HCRN GU-16-260-Cohort B, treated 16 patients with combination ipilimumab and nivolumab following progression prior to or stable disease at 48 weeks on single-agent nivolumab. This study found 6% ORR to the combination with PFS of 2.8 month (95% CI 2.7-NE) [56]. Similarly, the second part of the phase II UNISON trial, is currently enrolling patients with metastatic or unresectable nccRCC who progressed on single agent nivolumab for treatment with combination nivolumab and ipilimumab [55]. A retrospective study evaluated 18 patients with metastatic nccRCC treated with ipilimumab plus nivolumab. ORR was 33.3% with another 16.7% of patients with stable disease. Median progression-free survival was 7.1 months, however 61% of patients had treatment related adverse events requiring high doses of glucocorticoids [61]. A phase II clinical trial, SUNIFORECAST, will compare ipilimumab plus nivolumab to sunitinib for patients with advanced nccRCC, and is currently enrolling patients [62]. Another phase II study is currently investigating ipilimumab and nivolumab in advanced medullary RCC [63].
Combined treatment between immunotherapy and TKIs is being explored as well. The phase I/II CALYPSO trial evaluated savolitinib, a MET inhibitor, plus durvalumab, a PD-L1 inhibitor, in 41 patients with metastatic papillary RCC. ORR, the primary endpoint, was 27%. Median PFS was 4.9 months (95% CI 2.5–12), and median OS was 12.3 months (95% CI 5.8–21.3) [64, 65]. Of note, PD-L1 and MET expression were not associated with improved response or survival [65]. In the ongoing phase III SAMETA trial, the combination of savolitinib and durvalumab will be compared to both sunitinib and durvalumab monotherapy in MET-driven advanced papillary RCC [66].
CA209-9KU, a phase II trial of 47 patients treated with nivolumab plus cabozantinib in advanced nccRCC demonstrated ORR of 48% (95% CI 31.5–63.9) in patients with papillary, unclassified, or translocation-associated RCC and no responses among patients with chromophobe histology. Median PFS among the former group was 12.5 months (95% CI 29–65) and median OS was 28 months (95% CI 16.3-NE) [67]. Other clinical trials currently enrolling advanced non clear-cell RCC patients for treatment with immunotherapy/TKI combinations include LENKYN [68] and KEYNOTE-B61 [69] with pembrolizumab plus lenvatinib and a phase II study with nivolumab plus ipilimumab plus cabozantinib [70]. A planned PAPMET-2 study will also evaluate the combination of cabozantinib with immunotherapy.
Poly adenosine diphosphate-ribose polymerase (PARP) inhibitors are also being studied in combination with immune checkpoint inhibitors in nccRCC. One ongoing study is enrolling patients with FH- and SDH-deficient RCC to receive the combination of talazoparib, a PARP inhibitor, and avelumab, an immune checkpoint inhibitor [71].
Next generation sequencing, predictive biomarkers, and potential future therapeutic targets
Molecular analysis of nccRCC has revealed a unique characterization for these subtypes as well as potential therapeutic targets. Molecular characterization of papillary RCC has revealed MET alterations in both pathologic subtypes, though more commonly in type 1, including autosomal dominant germline mutations in hereditary papillary renal carcinoma. Other genetic alterations commonly observed in papillary RCC include TERT, CDKN2A/B, SETD2, KDM6A, SMARCB1, NF2, and FH. A molecular subtype of papillary RCC characterized by CpG island methylation demonstrated worse prognosis. This subtype also exhibited an increased Th2 immune signature, potentially despite correlating with worse survival could indicate response to immunotherapy [74]. Chromophobe histology is associated with germline FLCN and PTEN in Burt-Hogg-Dub
As immune checkpoint inhibitors that target the PD-1/PD-L1 pathway are being increasingly used in the treatment of metastatic nccRCC, expression of these potential targets has been extensively studied. In a study of 101 patients with nccRCC, immunohistochemical staining for PD-L1 demonstrated positive tumor cell membrane staining, defined by≥5% tumor cell membrane staining in 10.9% of patients. PD-L1 positive was associated with higher stage (p = 0.01) and Fuhrman grade (p = 0.03) but not with histologic subtype. Tumor infiltrating mononuclear cells demonstrated positive staining in 56.4% of patients, which was significantly associated with increased risk of death (HR 6.41, 95% CI 2.17–18.88, p < 0.001) [81]. A similar study of immunohistochemical staining for PD-1 and PD-L1 in tumor specimens from 64 patients with nccRCC found 19% of patients with PD-1 positive tumor infiltrating mononuclear cells and 46.4% of patients with intratumoral PD-L1 expression. Neither positive PD-1 expression (p = 0.88) or PD-L1 expression (p = 0.08) significantly correlated with cancer-specific survival [82]. Another study used a less stringent threshold for PD-L1 positivity, ≥1% staining by immunohistochemistry. This study analyzed tissue from 45 patients with nccRCC. In this study, 20% of tumors demonstrated PD-L1 positivity, which was associated with higher Fuhrman grade (p = 0.048) and perineural invasion (p = 0.043), but not significantly with higher stage. PD-L1 positivity was not prognostic with no significant correlation with progression-free survival (p = 0.58) or cancer-specific survival (p = 0.47) [83]. A multicenter study analyzed PD-1 and PD-L1 expression in papillary RCC specimens from 301 patients. Threshold for positivity was≥1% for PD-1 in tumor infiltrating mononuclear cells and > 5% for tumoral PD-L1. PD-1 expression was positive in 4.9% of type 1 papillary RCC and 2.4% of type 2 papillary RCC, and PD-L1 expression was positive in 7.2% of type 1 papillary RCC and 6.2% of type 2 papillary RCC. Neither PD-1 nor PD-L1 positivity was significantly associated with 5-year overall survival in either subtype of papillary RCC [84]. This was consistent with findings from prior studies that demonstrated no correlation between PD-L1 positivity and PFS or OS in papillary RCC [85, 86], although PD-L1 expression significantly correlated with worse PFS in ccRCC [85]. In another retrospective study, Xp11 translocation RCC correlated with worse response to TKIs and improved response to immune checkpoint inhibition, and they had greater density of CD8 positive infiltrating T cells. T cell immunophenotype was CD8+PD1+TIM3–LAG3+ in this population, compared to a more prevalent CD8+PD1+TIM3+LAG3– immunophenotype in ccRCC [87, 88].
A greater understanding of the molecular composition of nccRCC will lead to further therapeutic options. One case report detailed excellent response to palbociclib, a CDK4/6 inhibitor in a patient with metastatic collecting duct RCC with CDKN2A loss [89]. A pre-clinical study in renal medullary carcinoma examined the effects of SMARCB1 loss on MYC expression and replicative stress in vitro and in vivo. This study found that potential therapies that affect the DNA damage pathway, such as PARP inhibitors, including olaparib and niraparib, ATR inhibitors, and WEE1 inhibitors could all present promising therapies for this nccRCC subtype [90]. Single-cell transcriptomics has also identified potential therapeutic targets in medullary RCC, including novel targetable immune checkpoint receptors TIGIT and CD96, contrasting with low PD1 and CTLA4 expression [91]. Another study evaluated somatic and germline mutations from 116 patients with metastatic nccRCC. For somatic mutations, including ALK translocations, MET amplifications, PI3KCA mutations, and TSC1/2 mutations, 13% of patients had a potentially clinically actionable mutation. An additional 24% of patients who underwent germline testing had potentially clinically actionable mutations, most commonly in FH [92]. The INDIGO trial, which is currently enrolling patients, determines treatment based on DNA and RNA analysis for first-line treatment of advanced nccRCC. Treatment options in this clinical trial for metastatic nccRCC include targeted therapies for specific DNA mutations, sunitinib for patients who exhibit an angiogen profile, or Nivolumab patients who have an immune profile or do not qualify for other targeted treatments [93].
There are inherent limitations to this systematic review. Included studies that enrolled multiple histologic subtypes of nccRCC comprised varying proportions between these histological subtypes and therefore cannot be directly compared. Studies also had differing primary endpoints, and therefore some are not sufficiently powered for survival analysis, which is reported in this systematic review. Additionally, eighteen studies initially reviewed that did not have a nccRCC subgroup analysis were unable to be included in the final analysis.
CONCLUSIONS
Treatment of advanced nccRCC remains challenging, and response rates to most therapies remains low. Although most RCC trials focus on the more common ccRCC, trials have detailed outcomes with mTOR inhibitors, tyrosine kinase inhibitors, and immune checkpoint inhibitors. These trials are imperfect, however, with low patient accrual and heterogeneity between histologic subtypes that could limit their overall applicability. At this time, the most data supports using tyrosine kinase inhibitors, such as sunitinib, or cabozantinib in papillary RCC, especially after results of the PAPMET study. Immune checkpoint inhibition is emerging as a viable alternative and is preferred in nccRCC with sarcomatoid features. With growing data and ongoing studies involving combination strategies with immunotherapy and TKIs, this may ultimately emerge as the preferred therapy for nccRCC. Molecular characterization of advanced nccRCC will increase the arsenal of potential treatments, especially in rarer subtypes such as medullary RCC, and will hopefully improve prognosis.
ACKNOWLEDGMENTS
The authors have no acknowledgments.
FUNDING
The authors report no funding.
AUTHOR CONTRIBUTIONS
J.B. and P.B. were involved in literature review and composition of the manuscript. A.C., E.C., and J.G. helped review the manuscript and offered suggestions for improvement.
CONFLICT OF INTEREST
J.G. received institutional research funding from Astellas, Pfizer, Merck, Serono, Janssen, Genentech, and Clovis. He has also served in a consulting or CME speaking role for Bristol-Myers Squibb, Merck, Clovis, AAA, Sanofi, Bayer, Targeted Oncology, and Amgen. He is also an Oncology Drug Advisory (ODAC) committee member for the FDA.
P.B. receives institutional research funding from AstraZeneca, BlueEarth Diagnostics, Merck, and Seattle Genetics/Astellas. He also served in a consulting role for Astellas, Bayer, Bristol-Myers Squibb, Caris, Clovis, Eisai, EMD Serono, Dendreon, and Pfizer, Inc.
J.G. is an Editorial Board Member of this journal, but was not involved in the peer-review process of this paper, nor had access to any information regarding its peer-review.
J.B., A.C. and E.C. have no conflicts of interest to declare.
REFERENCES
[1] | Cancer Statistics, in Surveillance Epidemiology and End Results Program. (2020) . |
[2] | Moch H , et-al. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs-Part A: Renal, Penile, and Testicular Tumours. Eur Urol. (2016) ;70: (1):93–105. |
[3] | Motzer RJ , et-al. Nivolumab plus Ipilimumab versus Sunitinib in Advanced Renal-Cell Carcinoma. N Engl J Med. (2018) ;378: (14):1277–1290. |
[4] | Rini BI , et-al. Pembrolizumab plus Axitinib versus Sunitinib for Advanced Renal-Cell Carcinoma. N Engl J Med. (2019) ;380: (12):1116–1127. |
[5] | Choueiri TK , et-al. Nivolumab plus Cabozantinib versus Sunitinib for Advanced Renal-Cell Carcinoma. N Engl J Med. (2021) ;384: (9):829–841. |
[6] | Delahunt B , Eble JN . Papillary renal cell carcinoma: a clinicopathologic and immunohistochemical study of 105 tumors. Mod Pathol. (1997) ;10: (6):537–44. |
[7] | Amin MB , et-al. Prognostic impact of histologic subtyping of adult renal epithelial neoplasms: an experience of 405 cases. Am J Surg Pathol. (2002) ;26: (3):281–91. |
[8] | Wright JL , et-al. Effect of collecting duct histology on renal cell cancer outcome. J Urol. (2009) ;182: (6):2595–9. |
[9] | Argani P , et-al. TFE3-Fusion Variant Analysis Defines Specific Clinicopathologic Associations Among Xp11 Translocation Cancers. Am J Surg Pathol. (2016) ;40: (6):723–37. |
[10] | Blum KA , et-al. Sarcomatoid renal cell carcinoma: biology, natural history and management. Nat Rev Urol. (2020) ;17: (12):659–678. |
[11] | Page MJ , et-al. The PRISMA statement: an updated guideline for reporting systematic reviews. BMJ. (2021) ;372: :71. |
[12] | Pantuck AJ , et-al. Prognostic relevance of the mTOR pathway in renal cell carcinoma: implications for molecular patient selection for targeted therapy. Cancer. (2007) ;109: (11):2257–67. |
[13] | Husseinzadeh HD , Garcia JA . Therapeutic rationale for mTOR inhibition in advanced renal cell carcinoma. Curr Clin Pharmacol. (2011) ;6: (3):214–21. |
[14] | Blank CU , et-al. Safety and efficacy of everolimus in patients with non-clear cell renal cell carcinoma refractory to VEGF-targeted therapy: Subgroup analysis of REACT. Journal of Clinical Oncology. (2012) ;30: (5_suppl):402–402. |
[15] | Koh Y , et-al. Phase II trial of everolimus for the treatment of nonclear-cell renal cell carcinoma. Ann Oncol. (2013) ;24: (4):1026–31. |
[16] | Voss MH , et-al. Phase II Trial and Correlative Genomic Analysis of Everolimus Plus Bevacizumab in Advanced Non-Clear Cell Renal Cell Carcinoma. J Clin Oncol. (2016) ;34: (32):3846–3853. |
[17] | Feldman DR , et-al. Everolimus plus bevacizumab is an effective first-line treatment for patients with advanced papillary variant renal cell carcinoma: Final results from a phase II trial. Cancer. (2020) ;126: (24):5247–5255. |
[18] | Hutson TE , et-al. A Single-arm, Multicenter, Phase 2 Study of Lenvatinib Plus Everolimus in Patients with Advanced Non-Clear Cell Renal Cell Carcinoma. Eur Urol. (2021) . |
[19] | Hudes G , et-al. Temsirolimus, interferon alfa, or both for advanced renal-cell carcinoma. N Engl J Med. (2007) ;356: (22):2271–81. |
[20] | Dutcher JP , et-al. Effect of temsirolimus versus interferon-alpha on outcome of patients with advanced renal cell carcinoma of different tumor histologies. Med Oncol. (2009) ;26: (2):202–9. |
[21] | Mahoney KM , et-al. Phase 2 Study of Bevacizumab and Temsirolimus After VEGFR TKI in Metastatic Renal Cell Carcinoma. Clin Genitourin Cancer. (2016) ;14: (4):304–313e6. |
[22] | Escudier B , et-al. Open-label phase 2 trial of first-line everolimus monotherapy in patients with papillary metastatic renal cell carcinoma: RAPTOR final analysis. Eur J Cancer. (2016) ;69: :226–235. |
[23] | Colomba E , et-al. Metastatic chromophobe renal cell carcinoma treated with targeted therapies: A Renal Cross Channel Group study. Eur J Cancer. (2017) ;80: :55–62. |
[24] | Choueiri TK , et-al. Efficacy of sunitinib and sorafenib in metastatic papillary and chromophobe renal cell carcinoma. J Clin Oncol. (2008) ;26: (1):127–31. |
[25] | Tannir NM , et-al. Everolimus Versus Sunitinib Prospective Evaluation in Metastatic Non-Clear Cell Renal Cell Carcinoma (ESPN): A Randomized Multicenter Phase 2 Trial. Eur Urol. (2016) ;69: (5):866–74. |
[26] | Armstrong AJ , et-al. Everolimus versus sunitinib for patients with metastatic non-clear cell renal cell carcinoma (ASPEN): a multicentre, open-label, randomised phase 2 trial. Lancet Oncol. (2016) ;17: (3):378–388. |
[27] | Armstrong AJ , et-al. Angiokines Associated with Targeted Therapy Outcomes in Patients with Non-Clear Cell Renal Cell Carcinoma. Clin Cancer Res. (2021) . |
[28] | Bergmann L , et-al. A Randomized Phase IIa Trial with Temsirolimus versus Sunitinib in Advanced Non-Clear Cell Renal Cell Carcinoma: An Intergroup Study of the CESAR Central European Society for Anticancer Drug Research-EWIV and the Interdisciplinary Working Group on Renal Cell Cancer (IAGN) of the German Cancer Society. Oncol Res Treat. (2020) ;43: (7-8):333–339. |
[29] | Molina AM , et-al. Phase II trial of sunitinib in patients with metastatic non-clear cell renal cell carcinoma. Invest New Drugs. (2012) ;30: (1):335–40. |
[30] | Tannir NM , et-al. A phase 2 trial of sunitinib in patients with advanced non-clear cell renal cell carcinoma. Eur Urol. (2012) ;62: (6):1013–9. |
[31] | Lee JL , et-al. Multicenter phase II study of sunitinib in patients with non-clear cell renal cell carcinoma. Ann Oncol. (2012) ;23: (8):2108–2114. |
[32] | Gore ME , et-al. Final results from the large sunitinib global expanded-access trial in metastatic renal cell carcinoma. Br J Cancer. (2015) ;113: (1):12–9. |
[33] | Buti S , et-al. First-Line PAzopanib in NOn-clear-cell Renal cArcinoMA: The Italian Retrospective Multicenter PANORAMA Study. Clin Genitourin Cancer. (2017) ;15: (4):e609–e614. |
[34] | Jung KS , et-al. Pazopanib for the Treatment of Non-clear Cell Renal Cell Carcinoma: A Single-Arm, Open-Label, Multicenter, Phase II Study. Cancer Res Treat. (2018) ;50: (2):488–494. |
[35] | Costello BA , et-al. Phase II efficacy trial of pazopanib in nonclear cell metastatic renal cell cancer (mRCC): PINCR. Journal of Clinical Oncology. (2020) ;38: (6_suppl):696–696. |
[36] | Park I , Lee SH , Lee JL . A Multicenter Phase II Trial of Axitinib in Patients With Recurrent or Metastatic Non-clear-cell Renal Cell Carcinoma Who Had Failed Prior Treatment With Temsirolimus. Clin Genitourin Cancer. (2018) ;16: (5):e997–e1002. |
[37] | Albiges L , et-al. MET is a potential target across all papillary renal cell carcinomas: result from a large molecular study of pRCC with CGH array and matching gene expression array. Clin Cancer Res. (2014) ;20: (13):3411–21. |
[38] | Pal SK , et-al. A comparison of sunitinib with cabozantinib, crizotinib, and savolitinib for treatment of advanced papillary renal cell carcinoma: a randomised, open-label, phase 2 trial. Lancet. (2021) ;397: (10275):695–703. |
[39] | Campbell MT , et-al. Cabozantinib for the treatment of patients with metastatic non-clear cell renal cell carcinoma: A retrospective analysis. Eur J Cancer. (2018) ;104: :188–194. |
[40] | Martinez Chanza N , et-al. Cabozantinib in advanced non-clear-cell renal cell carcinoma: a multicentre, retrospective, cohort study. Lancet Oncol. (2019) ;20: (4):581–590. |
[41] | Procopio G , et-al. A phase 2 prospective trial of cabozantinib as first-line treatment for metastatic collecting ducts renal cell carcinoma: The BONSAI trial (Meeturo 2) clinical trial information—NCT03354884. Journal of Clinical Oncology. (2021) ;39: (15_suppl):4571–4571. |
[42] | Cabozantinib or Sunitinib Malate in Treating Participants With Metastatic Variant Histology Renal Cell Carcinoma. ClinicalTrials.gov. |
[43] | ANZUP - Non-clear Cell Post Immunotherapy CABozantinib (UNICAB) (UNICAB). ClinicalTrials.cov. |
[44] | Choueiri TK , et-al. Phase II and biomarker study of the dual MET/VEGFR2 inhibitor foretinib in patients with papillary renal cell carcinoma. J Clin Oncol. (2013) ;31: (2):181–6. |
[45] | Choueiri TK , et-al. Efficacy of Savolitinib vs Sunitinib in Patients With MET-Driven Papillary Renal Cell Carcinoma: The SAVOIR Phase 3 Randomized Clinical Trial. JAMA Oncol. (2020) ;6: (8):1247–1255. |
[46] | Albiges L , et-al. MET status and treatment outcomes in papillary renal cell carcinoma (PRCC): Pooled analysis of historical data. Journal of Clinical Oncology. (2020) ;38: (15_suppl):e19321–e19321. |
[47] | Choueiri TK , et-al. Biomarker-Based Phase II Trial of Savolitinib in Patients With Advanced Papillary Renal Cell Cancer. J Clin Oncol. (2017) ;35: (26):2993–3001. |
[48] | Schoffski P , et-al. Crizotinib achieves long-lasting disease control in advanced papillary renal-cell carcinoma type 1 patients with MET mutations or amplification. EORTC 1 CREATE trial. Eur J Cancer. (2017) ;87: :147–163. |
[49] | Twardowski PW , et-al. Parallel (Randomized) Phase II Evaluation of Tivantinib (ARQ197) and Tivantinib in Combination with Erlotinib in Papillary Renal Cell Carcinoma: SWOG S1107. Kidney Cancer. (2017) ;1: (2):123–132. |
[50] | Srinivasan R , et-al. Results from a phase II study of bevacizumab and erlotinib in subjects with advanced hereditary leiomyomatosis and renal cell cancer (HLRCC) or sporadic papillary renal cell cancer. Journal of Clinical Oncology. (2020) ;38: (15_suppl):5004–5004. |
[51] | Leger PD , et-al. A phase II study of the selective MET kinase inhibitor INC280 in advanced papillary renal cell cancer. Journal of Clinical Oncology. (2020) ;38: (15_suppl):5075–5075. |
[52] | Ravaud A , et-al. First-line treatment with sunitinib for type 1 and type 2 locally advanced or metastatic papillary renal cell carcinoma: a phase II study (SUPAP) by the French Genitourinary Group (GETUG)dagger. Ann Oncol. (2015) ;26: (6):1123–1128. |
[53] | Negrier S , et-al. Axitinib in first-line for patients with metastatic papillary renal cell carcinoma: Results of the multicentre, open-label, single-arm, phase II AXIPAP trial. Eur J Cancer. (2020) ;129: :107–116. |
[54] | Vogelzang NJ , et-al. Safety and Efficacy of Nivolumab in Patients With Advanced Non-Clear Cell Renal Cell Carcinoma: Results From the Phase IIIb/IV CheckMate 374 Study. Clin Genitourin Cancer. (2020) ;18: (6):461–468e3. |
[55] | Gedye C , et-al. UNISON - nivolumab then ipilimumab+nivolumab in advanced non-clear cell renal cell carcinoma (ANZUP Part 1— Nivolumab monotherapy. Journal of Clinical Oncology. (2021) ;39: (6_suppl):325–325. |
[56] | Atkins MB , et-al. Phase II study of nivolumab and salvage nivolumab+ipilimumab in treatment-naïve patients (pts) with advanced non-clear cell renal cell carcinoma (nccRCC) (HCRN GU16-260-Cohort B). Journal of Clinical Oncology. (2021) ;39: (15_suppl):4510–4510. |
[57] | McDermott DF , et-al. Open-Label, Single-Arm, Phase II Study of Pembrolizumab Monotherapy as First-Line Therapy in Patients With Advanced Non-Clear Cell Renal Cell Carcinoma. J Clin Oncol. (2021) ;39: (9):1029–1039. |
[58] | McGregor BA , et-al. Results of a Multicenter Phase II Study of Atezolizumab and Bevacizumab for Patients With Metastatic Renal Cell Carcinoma With Variant Histology and/or Sarcomatoid Features. J Clin Oncol. (2020) ;38: (1):63–70. |
[59] | Rini BI , et-al. Atezolizumab plus Bevacizumab Versus Sunitinib for Patients with Untreated Metastatic Renal Cell Carcinoma and Sarcomatoid Features: A Prespecified Subgroup Analysis of the IMmotion151 Clinical Trial. Eur Urol. (2021) ;79: (5):659–662. |
[60] | Chahoud J , et-al. Outcomes of patients with metastatic renal cell carcinoma with sarcomatoid dedifferentiation to immune checkpoint inhibitors. Urol Oncol. (2021) ;39: (2):134e9–134e16. |
[61] | Gupta R , et-al. Clinical Activity of Ipilimumab Plus Nivolumab in Patients With Metastatic Non-Clear Cell Renal Cell Carcinoma. Clin Genitourin Cancer. (2020) ;18: (6):429–435. |
[62] | Ahrens M , et-al. A randomized phase II study of nivolumab plus ipilimumab versus standard of care in previously untreated and advanced non-clear cell renal cell carcinoma (SUNIFORECAST). Journal of Clinical Oncology. (2020) ;38: (15_suppl):TPS5103–TPS5103. |
[63] | Msaouel P , Slack-Tidwell R , Tannir NM . Phase II trial of nivolumab (nivo) plus ipilimumab (ipi) in patients with SMARCB1-deficient kidney malignancies. Journal of Clinical Oncology. (2019) ;37: (7_suppl):TPS677–TPS677. |
[64] | Powles T , et-al. A phase II study investigating the safety and efficacy of savolitinib and durvalumab in metastatic papillary renal cancer (CALYPSO). Journal of Clinical Oncology. (2019) ;37: (7_suppl):545–545. |
[65] | Rodriguez CS , et-al. Overall survival results for durvalumab and savolitinib in metastatic papillary renal cancer. Journal of Clinical Oncology. (2020) ;38: (6_suppl):619–619. |
[66] | Savolitinib Plus Durvalumab Versus Sunitinib and Durvalumab Monotherapy in MET-Driven, Unresectable and Locally Advanced or Metastatic PRCC (SAMETA). ClinicalTrials.gov. |
[67] | Lee C-H , et-al. Nivolumab plus cabozantinib in patients with non-clear cell renal cell carcinoma: Results of a phase 2 trial. Journal of Clinical Oncology. (2021) ;39: (15_suppl):4509–4509. |
[68] | Lenvatinib (LEN) in Combination With Pembrolizumab (KEYtruda) in Subjects With Locally Advanced or Metastatic Non-clear Cell Renal Cell Carcinoma (The LENKYN Trial). ClinicalTrials.gov. |
[69] | Pembrolizumab Plus Lenvatinib for First-line Advanced/Metastatic Non-clear Cell Renal Cell Carcinoma (1L nccRCC) (MK-3475-B61) (KEYNOTE-B61). ClinicalTrials.gov. |
[70] | Cabozantinib In Combo With NIVO+IPI In Advanced NCCRCC. ClinicalTrials.gov. |
[71] | Talazoparib and Avelumab in Participants with Metastatic Renal Cell Carcinoma. ClinicalTrials.gov. |
[72] | Cancer Genome Atlas Research N , et-al. Comprehensive Molecular Characterization of Papillary Renal-Cell Carcinoma. N Engl J Med. (2016) ;374: (2):135–45. |
[73] | Pal SK , et-al. Characterization of Clinical Cases of Advanced Papillary Renal Cell Carcinoma via Comprehensive Genomic Profiling. Eur Urol. (2018) ;73: (1):71–78. |
[74] | Galsky MD , et-al. Randomized Double-Blind Phase II Study of Maintenance Pembrolizumab Versus Placebo After First-Line Chemotherapy in Patients With Metastatic Urothelial Cancer. J Clin Oncol. (2020) ;38: (16):1797–1806. |
[75] | Davis CF , et-al. The somatic genomic landscape of chromophobe renal cell carcinoma. Cancer Cell. (2014) ;26: (3):319–330. |
[76] | Ricketts CJ , et-al. The Cancer Genome Atlas Comprehensive Molecular Characterization of Renal Cell Carcinoma. Cell Rep. (2018) ;23: (12):3698. |
[77] | Pal SK , et-al. Characterization of Clinical Cases of Collecting Duct Carcinoma of the Kidney Assessed by Comprehensive Genomic Profiling. Eur Urol. (2016) ;70: (3):516–21. |
[78] | Calderaro J , et-al. SMARCB1/INI1 inactivation in renal medullary carcinoma. Histopathology. (2012) ;61: (3):428–35. |
[79] | Calderaro J , et-al. Balanced Translocations Disrupting SMARCB1 Are Hallmark Recurrent Genetic Alterations in Renal Medullary Carcinomas. Eur Urol. (2016) ;69: (6):1055–61. |
[80] | Rao Q , et-al. Frequent co-inactivation of the SWI/SNF subunits SMARCB1, SMARCA2 and PBRM1 in malignant rhabdoid tumours. Histopathology. (2015) ;67: (1):121–9. |
[81] | Choueiri TK , et-al. PD-L1 expression in nonclear-cell renal cell carcinoma. Ann Oncol. (2014) ;25: (11):2178–2184. |
[82] | Abbas M , et-al. Do programmed death 1 (PD-1) and its ligand (PD-L1) play a role in patients with non-clear cell renal cell carcinoma? Med Oncol. (2016) ;33: (6):59. |
[83] | Chipollini J , et-al. Implications of Programmed Death Ligand-1 Positivity in Non-Clear Cell Renal Cell Carcinoma. J Kidney Cancer VHL. (2018) ;5: (4):6–13. |
[84] | Erlmeier F , et-al. Characterization of PD-1 and PD-L1 Expression in Papillary Renal Cell Carcinoma: Results of a Large Multicenter Study. Clin Genitourin Cancer. (2021) ;19: (1):53–59e1. |
[85] | Shin SJ , et-al. Clinicopathologic Analysis of PD-L1 and PD-L2 Expression in Renal Cell Carcinoma: Association with Oncogenic Proteins Status. Ann Surg Oncol. (2016) ;23: (2):694–702. |
[86] | Motoshima T , et-al. PD-L1 expression in papillary renal cell carcinoma. BMC Urol. (2017) ;17: (1):8. |
[87] | Bakouny Z , et-al. Integrative Clinical and Molecular Characterization of Translocation Renal Cell Carcinoma. bioRxiv. (2021) :2021.04.14.439908. |
[88] | Bakouny Z , et-al. Integrative Clinical and Molecular Characterization of Translocation Renal Cell Carcinoma. Cell Rep. (2022) ;38: (1). |
[89] | Pal SK , et-al. Exceptional Response to Palbociclib in Metastatic Collecting Duct Carcinoma Bearing a CDKN2A Homozygous Deletion. JCO Precision Oncology. (2017) (1):1–5. |
[90] | Msaouel P , et-al. Comprehensive Molecular Characterization Identifies Distinct Genomic and Immune Hallmarks of Renal Medullary Carcinoma. Cancer Cell. (2020) ;37: (5):720–734e13. |
[91] | Vokshi BH , et-al. Integrative genomics uncover mechanisms of renal medullary carcinoma transformation, microenvironment landscape and therapeutic vulnerabilities. bioRxiv. (2021) :2021.09.29.462391. |
[92] | Carlo MI , et-al. Comprehensive Genomic Analysis of Metastatic Non-Clear-Cell Renal Cell Carcinoma to Identify Therapeutic Targets. JCO Precis Oncol. (2019) ;3. |
[93] | Individualized Treatment Strategy for Patients With Metastatic Non-clear Cell Renal Cell Carcinoma (INDIGO). ClinicalTrials.gov. |




