A Shared Decision-Making Model for Management of Small Renal Masses: Optimizing the Patient Experience
Abstract
Background:
The finding of a small renal mass (SRM) on radiological imaging and the potential of a cancer diagnosis is anxiety provoking in most patients. The decision-making process often occurs in the absence of any framework regarding the nature and treatment outcomes. This project aimed to educate patients newly diagnosed with a SRM, implement a shared decision-making (SDM) model, and assess the educational attainment and effect on a SDM intervention.
Methods:
This project assessed the educational attainment and its effect on a SDM intervention using a pre-and post- intervention survey, an educational video [Urology Care Foundation, “What is a renal mass?], and a structured provider discussion. The survey incorporated eight knowledge questions and two questions which addressed anxiety related to diagnosis and confidence in decision-making.
Results:
Fifty surveys were completed. The post intervention score showed a significant increase in patient knowledge. Wilcoxon signed rank test (P = <0.001; 2.0; CI 95% (1.54–2.46)). Thirty-nine demonstrated improvement in knowledge with a mean of 2.0, 9 were unchanged and 2 decreased. Approximately 42% of patients reported a decrease in anxiety rating by a mean of 40%. When confidence in decision-making improved, it improved by a mean of 45%.
Conclusions:
A significant improvement in understanding of SRMs was demonstrated. This model showed improved knowledge, alleviation of anxiety and improved confidence and denotes the feasibility of implementing a SDM model in newly diagnosed patients. Results should encourage providers who aspire to incorporate a SDM as a Best Practice.
INTRODUCTION
Cancer is the second leading cause of death in the U.S. with renal cell carcinoma (RCC) representing approximately 3– 4% of all adult cancers [1]. With advanced imaging, there has been a stage migration in the diagnosis towards small renal masses (SRMs) [2], which may be indolent or slow growing. The proportion of renal masses characterized as pT1, (≤7 cm) and limited to the kidney was 4% in 1989 versus 22% in 2000 [3], and is increasing. This is now over 50% [4]. This increased frequency in the detection of SRMs in the general adult population requires adjustment in oncologic management, however, the framework for the optimal approach for each patient is not immediately evident. One approach is to optimize patient choice in the adoption of shared decision-making (SDM) model which incorporates the use of an educational aid such as a video in combination with a structured provider discussion.
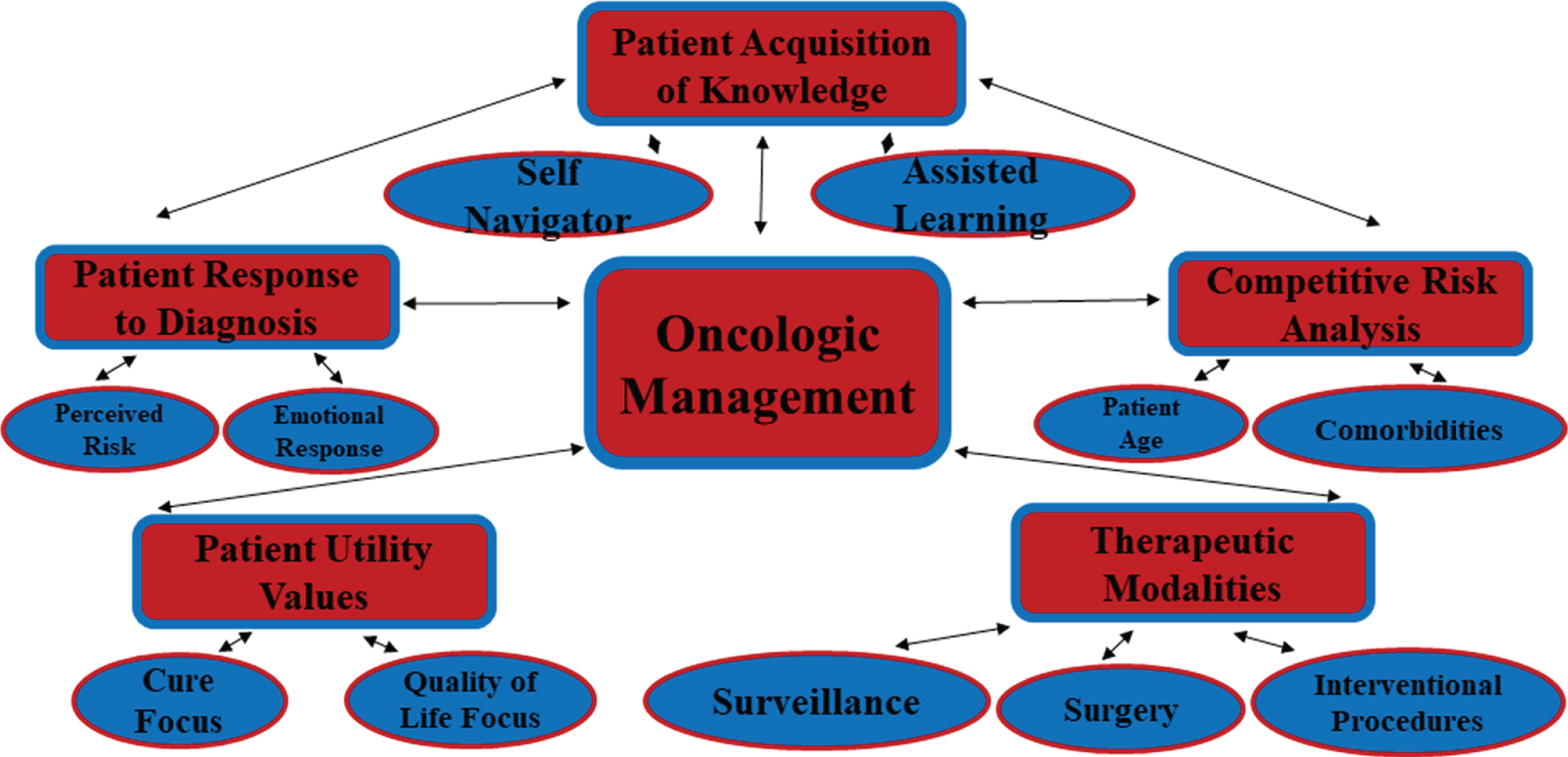
Shared decision-making “is a collaborative decision-making process between patients and their health care providers relevant to medical decisions where multiple options are considered clinically acceptable” [5]. Several issues go into treatment decision-making such as competing illness, general age, quality of life concerns, and the effectiveness of treatment [6]. We hypothesized that patients come to urology with variable degrees of knowledge and understanding (See Fig. 1). A model which is implemented seamlessly into the clinical encounter provides maximum benefit for all shareholders; patients, providers and healthcare system. A SDM pathway which clarifies the problem for the patient diagnosed with a SRM and eliminates confusion, may have significant value to the patient and provider.
Fig. 1
Oncologic Management of Smalll Renal Masses.
The aim of this project was to investigate the introduction of a SDM focused on individual patient choices and preferences, based on evidenced based management options, as to whether the SDM could improve knowledge of SRM [7].
MATERIALS AND METHODS
Adult patients diagnosed with a SRM < 4.0 cm were asked to watch the Urology Care Foundation video, “What is a renal mass?” and participate in a SDM discussion during a clinic visit with the urologist and/or NP. The objectives were:
1. Assess patient knowledge of treatment options for a SRM pre-and post- intervention.
2. Evaluate the influence of an intervention of an educational video followed by a structured discussion during a clinic visit as part of a SDM process which assesses patient knowledge, anxiety surrounding diagnosis and confidence in treatment choice.
The project setting was the urology division outpatient clinic located at the Perelman Center for Advanced Medicine, University of Pennsylvania. The participants were chosen from provider schedules of those patients referred for evaluation of a SRM. The impetus for this project was to optimize the patient experience with the potential to standardize an approach for all patients across the Genitourinary service lines.
Intervention
Project participants
The project participants were male and female patients between the ages of 18 and 80 in the urology division newly diagnosed with a SRM < 4 cm. Patients with renal masses >4 cm were excluded. Additionally, patients being treated for a secondary cancer were excluded. The patients received a written description of the purpose of the project and a letter of consent explaining that participation was completely voluntary, would not have any impact on the quality of care, and included a provision for confidentiality.
Project design
The project design incorporated a 10 item pre- and 16 item post-intervention survey focusing on the educational attainment and assessment of a baseline understanding of SRMs and the available treatment options. The pre-intervention survey was administered as the initial step (See Table 1). Prior to the start of each clinic, the NP identified the patients who were being evaluated for a new diagnosis of a SRM. Once the patient was in a room, the NP approached the patient, gave appropriate introductions and explained the purpose of the survey. The NP informed the patient that their participation was completely voluntary, would not affect their care, and that no information will be collected in conjunction with the patient’s identity. Patients who gave verbal consent to participate were given a survey packet containing an informed consent cover letter explaining the purpose of the project, the survey, an envelope, and a writing utensil. Patients were then instructed to choose the best possible answer to each question and to write an answer where appropriate. The NP was available to answer any questions related to the survey content. Participants were instructed to place the completed survey in the envelope provided and return it to the NP. A completed and returned survey served as informed consent. After completing the pre-intervention survey, project participants watched the Urology Care Foundation’s video, “What is a renal mass?”[8]
Table 1
Preintervention Survey
| •Are small renal masses uniformly aggressive or latent? |
| •Is the removal of the kidney the best way to treat a small renal mass? |
| •Are you familiar with partial nephrectomy as an option? |
| •Are you familiar with ablative therapy? |
| •Can small renal masses be observed? |
| •Do small renal masses < 4cm regularly spread to other sites? |
| •Can focally treated small renal masses recur? |
| •Can you retreat small renal masses? |
| •How anxious are you related to your diagnosis of a SRM? (with 1 being not at all anxious and 4 being extremely anxious) |
| 1 2 3 4 |
| •How confident are you in your ability to make a decision about managing your diagnosis of a SRM? (with 1 being not at all confident and 4 being extremely confident) |
| 1 2 3 4 |
http://www.urologyhealth.org/urologic-conditions/kidney-cancer/videos. The project participants then participated in a structured SDM discussion. The SDM discussion replicated the SDM model published by Elwyn et al. 2012 [9]. The patient’s initial preference was documented followed by the choice talk, option talk and decision talk. Following the structured SDM discussion, the patient’s informed preferences were documented in the electronic medical record. The treatment options discussed with the patient included active surveillance, ablative therapy, and surgery. At the conclusion of the clinic visit, the project participants received a post- intervention survey (See Table 2). The same number was assigned to each pair of pre- and post-intervention surveys so that pre- and post- intervention results from each project participant could be matched for comparison.
Table 2
Postintervention Survey
| •Are small renal masses uniformly aggressive or latent? |
| •Is the removal of the kidney the best way to treat a small renal mass? |
| •Are you familiar with partial nephrectomy as an option? |
| •Are you familiar with ablative therapy? |
| •Can small renal masses be observed? |
| •Do small renal masses < 4cm regularly spread to other sites? |
| •Can focally treated small renal masses recur? |
| •Can you retreat small renal masses? |
| •How anxious are you related to your diagnosis of a SRM? (with 1 being not at all anxious and 4 being extremely anxious) |
| 1 2 3 4 |
| •How confident are you in your ability to make a decision about managing your diagnosis of a SRM? (with 1 being not at all confident and 4 being extremely confident) |
| 1 2 3 4 |
| •How helpful was the educational video in clarifying your treatment decision? |
| Not helpful Somewhat helpful Very helpful |
| •How helpful was the structured discussion with the provider during your clinic visit in clarifying your decision? |
| Not helpful Somewhat helpful Very helpful |
| •How helpful was the video in alleviating anxiety related to your treatment decision? (with 1 being not at all helpful and 4 being extremely helpful) |
| 1 2 3 4 |
| •How helpful was the provider clinic visit in alleviating your anxiety related to your treatment decision? (with 1 being not at all helpful and 4 being extremely helpful) |
| 1 2 3 4 |
| •How helpful was the video in improving confidence related to your treatment decision? (with 1 being not at all helpful and 4 being extremely helpful) |
| 1 2 3 4 |
| •How helpful was the provider clinic visit in improving confidence related to your treatment decision? (with 1 being not at all helpful and 4 being extremely helpful) |
| 1 2 3 4 |
Study of the intervention
The approach chosen for assessing the impact of implementing standardized patient education and the SDM model was a pre-and post- intervention survey assessing patient knowledge, anxiety surrounding diagnosis and confidence in treatment choice. The patient’s initial preference and informed preferences were also documented. The pre-and post-surveys were completed during the clinic visit.
Measures
The data collection tools included a pre-and post-intervention survey with a combination of yes or no questions, and Likert questions with answer options on a 4-point Likert scale. Face validity of the survey was determined through an informal process by asking a few individuals who were representative of the patient population whether or not the questions made sense and if they were easily understood. Content validity was determined by carefully reviewing educational content, components of the SDM pathway, and survey questions with several provider colleagues. The majority of survey questions were knowledge questions based on the video content and questions pertaining to anxiety related to diagnosis and confidence in choosing a management strategy.
The post-intervention survey included additional questions designed to evaluate the intervention. The questions were written to measure the combined effect of the educational video content and the structured SDM discussion during a single clinic visit. Basic demographic questions were also included in the survey and stratified by age range 18– 34, 35– 64 and >65 years old, sex, educational status and co-morbidities.
A Flesch-Kincaid readability formula assessed the pre- and post- surveys at a fifth-grade reading level, and a compellation of test readability scores of 8 readability formulas gave a score of a fourth-grade reading level [10]. The educational video is a product of the Urology Care Foundation. The language in the video was consistent with the language used it the pre- and post-intervention surveys. The data was collected in entirety at the time of the clinic visit.
Analyses
Data was compiled and organized in Microsoft Excel. The outcome measured was the pre-and post- survey knowledge, anxiety surrounding diagnosis and confidence in management choice by the project participants regarding the treatment options for SRMs. A table was used to display the participant sample, demographic data and size of the SRM. The Wilcoxon signed rank test was used to analyze the post intervention response as measured by post intervention score improvement and a histogram was used to display this data. Descriptive statistics were used to describe the self-assessment responses pertaining to anxiety and confidence as well as the responses related to the helpfulness of the interventions and to document the change in preferences.
Ethical considerations
There were no specific ethical considerations or conflicts of interest identified in the IRB process. This project was categorized as a quality improvement process during an IRB review process to enhance the patient encounter. The project design allowed for an easy intervention and administration of the pre-and post- intervention survey, and overall, was non-disruptive in the clinical encounter.
RESULTS
Fifty surveys were completed and returned with a response rate of 100 percent. Sample demographics revealed 60% male and 40% female with 42% of participants in the 34– 65 years of age category and 54% >65 years of age. Forty percent of the participants completed high school education and 38% obtained a college degree. The principle co-morbidities were hypertension in 33%, diabetes mellitus in 23%, cancer in 18% and other in 22% respectively in participants (See Table 3). The sample size was n = 50. The median size for the SRM was 2.0×1.0 cm.
Table 3
Demographic Data for Oncologic Management of Small Renal Masses
| Age | Sex | Education | Co-Morbidities | Size of SRM (cm) |
| >65 | Male | College | Htn, DM, MI, CA | 3.2×2.7 |
| >65 | Male | College | Htn, CA | 1.4×1.3 |
| 35–64 | Female | High School | Neuroendocrine Tumor, CA | 1.5×1.5 |
| 35–64 | Male | High School | Htn, DM, CA | 1.0 |
| >65 | Male | High School | Htn, DM, Cerebral Amyloid Angiopathy | 1.9×1.7 |
| >65 | Male | College | Htn, CA | 2.4×2.1 |
| >65 | Male | High School | Htn, DM, MI, | 2.5×1.5×2.5, |
| 2.3×2.7×2.4 | ||||
| 35–64 | Male | High School | Htn, DM, | 3.0 |
| 35–64 | Female | College | None | 1.9×1.4×2.0 |
| 35–64 | Male | High School | Htn, Valve Replacement | 2.6×2.1×1.9 |
| 35–64 | Male | College | Htn, DM, CA, Lung Disease | 1.2, 2.4, 2.2 |
| >65 | Male | High School | Htn, DM | 3.0 |
| 35–64 | Female | High School | Htn, DM, TB | 2.0 |
| >65 | Female | High School | Htn, CA | 1.7×2.4 |
| >65 | Male | Graduate School | Htn, CVA | 2.0 |
| >65 | Female | High School | CA | 3.0×2.6×3.1 |
| >65 | Male | High School | Pacemaker, Heart Valve | 2.3×1.2×1.7 |
| >65 | Male | College | Htn, CA, Aortic Replacement | 1.1×0.8 |
| >65 | Male | College | Htn, DM, CA | 1.3×1.3 |
| >65 | Male | College | CA, Colon Cancer | 1.0 |
| >65 | Male | High School | DM, MI, CA, Valve, Pacemaker | 2.1×1.9, |
| 0.1×0.9 | ||||
| 35–64 | Male | College | None | 1.6×1.1×1.2 |
| 35–64 | Male | College | Htn | 2.6×2.7×3.4 |
| >65 | Male | College | Htn, CA, CAP, Marginal Cell Lymphoma | 1.6×1.7×1.7, |
| 0.9×0.9×0.9 | ||||
| >65 | Male | Graduate School | CA | 1.8 |
| >65 | Female | Graduate School | Htn | 1.7×1.7×1.7 |
| 35–64 | Male | College | Htn, DM | 0.9×0.9 |
| 35–64 | Male | Graduate School | Htn, DM | 1.3×1.2 |
| >65 | Male | College | Htn, DM | 1.7×1.3, 2.3×2.0 |
| >65 | Male | Graduate School | Htn, Renal Insufficiency, Hypothyroidism | 1.9 |
| >65 | Male | Graduate School | MI, Cardiac Ablation | 1.8×1.9 |
| >65 | Female | College | None | 1.9 |
| 35–64 | Male | High School | DM | 2.3×2.2×2.3 |
| 35–64 | Female | High School | Htn, DM | 3.1×2.9×2.9 |
| 35–64 | Female | College | None | 1.0×1.1 |
| 35–64 | Male | High School | Htn, DM, HIV | 1.0, 0.5 |
| 35–64 | Female | College | Htn, DM, CA, | 2.0×2.5×2.3 |
| 18–34 | Female | College | None | 2.0×1.5×0.7 |
| 35–64 | Female | High School | Htn, GERD, Sleep Apnea | 1.0×1.5×1.5 |
| 35–64 | Female | College | Htn, CA | 0.9×0.9×0.8 |
| 35–64 | Female | High School | DM | 1.4 |
| >65 | Female | High School | Ulcerative Colitis | 1.0 |
| >65 | Male | Graduate School | Aflutter/AFib | 1.4×1.2 |
| 35–64 | Male | Graduate School | Htn, DM, GERD | 1.6 |
| 18–34 | Male | College | None | 2.8 |
| >65 | Female | Graduate School | Thyroid Disease | 1.6 |
| >65 | Female | High School | Htn, DM, Lymphoma, Sleep Apnea | 0.7 |
| >65 | Female | High School | Htn, DM, Depression | 1.0 |
| >65 | Female | High School | Htn, Osteoporosis | 1.0, 1.8×1.6, |
| 1.0×0.9, 1.2×1.2, | ||||
| 0.9×0.8 | ||||
| 35–64 | Female | High School | Crohn’s Disease, ITP | 1.1 |
Note. The data demonstrate age, sex, educational level, co-morbidities’ and size of SRM.
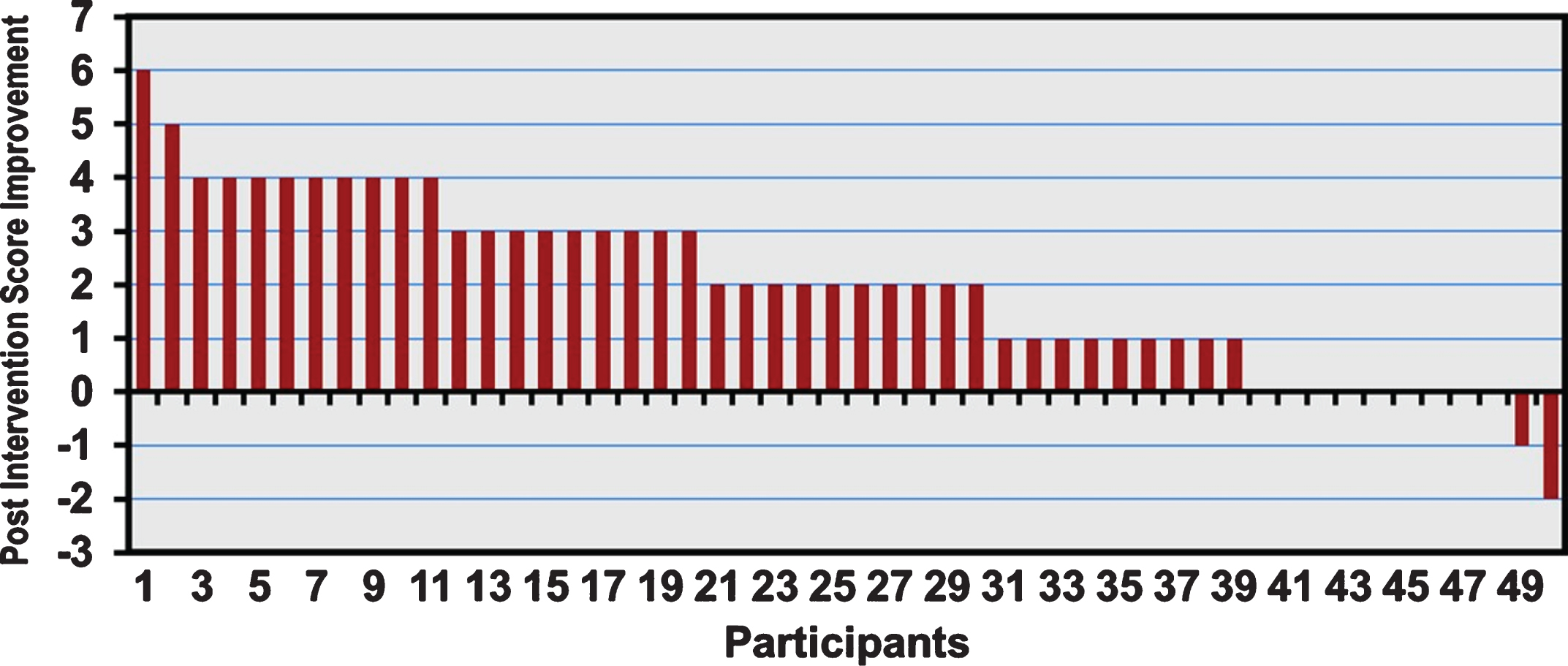
The post intervention score showed a significant increase in patient knowledge. Each participant stayed the same or demonstrated improved knowledge level with an average improvement of 2 items. Thirty-nine demonstrated improvement in knowledge with a mean of 2.0, 9 were unchanged and 2 decreased. Wilcoxon signed rank test (P = <0.001; 2.0; CI 95% (1.54– 2.46)). The raw scores were tabulated and the change or delta is displayed on the histogram (See Fig. 2). This statistical analysis demonstrated support for the intervention.
Fig. 2
Post Invention Response for Oncologic Management of Small Renal Masses.
One question pertained to the self-assessment of the patient’s anxiety related to the diagnosis and one question pertained to confidence level in decision-making. Approximately 42% of patients reported a decrease in anxiety rating by a mean of 40%. When confidence in decision-making improved, it improved by a mean of 45%.
Seventy-two percent of the participants found the educational video very helpful. Ninety-two percent participants found the structured provider discussion very helpful in clarifying their treatment decision. All participants reported that both the video and the provider discussion were helpful or very helpful in alleviating anxiety and improving confidence. The treatment preference was noted relative to the initial preference and the informed preference.
The initial treatment preferences were determined post hoc analysis. Eighteen of fifty participants expressed an initial treatment preference at the outset of their encounter, the remainder were undecided. Twenty-five of the fifty participants who were undecided, once informed, chose surveillance as a preferred treatment strategy. One participant who initially preferred surgery opted for an ablative procedure. Three of fifty participants whose initial preference was surgery, decided on more conservative management with surveillance following the SDM model encounter. Ultimately, the final decisions were as follows: surveillance 32/50; surgery 15/50 and ablative therapy 3/50.
DISCUSSION
The finding of a SRM on radiological imaging and the potential of a cancer diagnosis is anxiety provoking in most patients [11]. Treatments may include management with surveillance, ablative therapy or surgery. One form of management may lead to overutilization of health resources while another form of management may lead to undertreatment of a life-threatening mass. The consequences of a poor understanding of treatment options may lead to increased anxiety and lack of confidence in the chosen management strategy. Patients who are well-informed about strategies for managing a diagnosis of a SRM and who participate in SDM with their provider may experience decreased anxiety and greater confidence in their treatment plan.
Implementing SDM will help patients identify treatment goals and enable them to make well-informed treatment choices without compromising oncologic outcomes. This allows for rational choices and improved confidence with their chosen management strategy. SDM is a shift away from paternalism and a movement towards a more dynamic interaction between patients and providers. Implementing a process of SDM is an effective way to provide patient-centered care and improve the quality of the patient experience [12]. While common in internal medicine, there are few studies documenting the use of SDM in the urology practice setting. SDM is associated with increased patient knowledge, a better patient experience, a greater engagement with care and possible reduction of medical costs [9, 12].
A goal of the AUA Quality Summit of 2016: Shared Decision-Making and Prostate Cancer Screening was to focus on techniques to identify and understand patient values around prostate cancer and promote incorporation of SDM into prostate cancer discussions. The Summit incorporated SDM and decision tools, and found that SDM supports collaboration between providers and patients in situations where there are multiple, preference-sensitive options [13].
Patient knowledge was improved and they were primed for active involvement in their decisions through the use of decision aids and decision coaches. One of the biggest changes in the AUA 2017 Renal Mass and Localized Renal Cancer Guidelines, was the panel’s recommendation of individualized counseling and management due to the patient, oncological and functional characteristics [14]. A decision aid specifically for small renal masses is available online [15].
Survival is high for RCC due to the natural history of these masses and the spectrum of treatment choices. Therefore, the optimal pathway for a particular individual is the focus of this project. The design concept includes in-depth education and informed decision-making. This approach may impact more appropriate choices, potentially minimize the risk of overtreatment and improve the patient experience. A busy urologist may find that this model provides a necessary educational primer prior to his provider discussion, and lead to a more focused provider- patient discussion. Advanced Practice Providers are uniquely positioned to advocate for an individualized approach by implementing the SDM model, as they can manage this emerging population of patients with SRMs and can do so with relative autonomy.
Interpretation
The focus of this project was the application of a SDM as a pathway to guide patients through this process. The clinical implication of this effort was the optimization of patient choices in the management of SRMs. This may decrease overtreatment, avoid unnecessary morbidity, and allow outcomes satisfactory to patients and health providers.
The implementation was feasible in a busy practice. An educational intervention and SDM discussion were implemented seamlessly during a clinic visit with patients newly diagnosed with a SRM. The project results demonstrated a significant improvement in patient knowledge about the nature and behavior of SRMs following an educational intervention. This change in improvement was even evident in the highly educated patients. Patients who participated in a SRM discussion report increased confidence in their management choice. Use of a SDM model in a urologic practice setting with patients diagnosed with a SRM addressed a gap not previously documented in the literature.
The AUA/Urology Care Foundation resource tool was well liked. An educational intervention paired with a SDM model was an efficient and effective way to improve patient knowledge about SRMs and provide patient-centered, evidence based care. SDM gives patients an opportunity to interact with their provider and exercise more autonomy in choosing a management strategy that best suits their individual needs.
The initial outcomes demonstrated significantly greater patient understanding of the nature and behavior of SRMs. Project participants showed improved patient knowledge, alleviation of anxiety and improved confidence in decision-making with their chosen management strategy. The more informed patient generally has a better consultative experience within the health system.
Limitations
An initial bias may exist for those willing or unwilling to participate in the project. A selection bias may exist by including only patients who seek care at an academic medical center. Additionally, the educational allotment of the project participants was higher than in the general population. In a less educated cohort, one may have seen improved results. Anxiety and confidence were measured subjectively. Future projects may benefit from additional follow up and should evaluate the influence of comorbid conditions on treatment choice.
CONCLUSIONS
There was a statistically significant greater understanding of SRMs. A SDM model which incorporated an educational video and structured provider discussion showed improved patient knowledge, alleviation of anxiety surrounding the diagnosis and improved confidence with their chosen treatment plan. This initiative demonstrated the feasibility of implementing a SDM model. Results should encourage providers who aspire to incorporate a SDM as a Best Practice. Future phases include expanding the SDM to a wide variety of providers.
ACKNOWLEDGMENTS
I would like to acknowledge S. Bruce Malkowicz MD, my mentor and good friend, who inspires me each day in my professional pursuits, most notably in the field of urology. I would like to acknowledge the Nicolo Family Research Fund.
FUNDING
The authors report no funding.
AUTHOR CONTRIBUTIONS
Adele Marie Caruso, DNP, CRNP, FAANP Conception, Performance and Interpretation of Data, Initial & Final Drafts, Editing; K. Michelle Ardisson, DNP, ACNP-BC Editing; Roshan Ravishankar, BS, BA Interpretation of data; S. Bruce Malkowicz, MD Conception, Performance and Interpretation of Data, Editing.
CONFLICT OF INTERESTS
The authors have no conflicts of interest to report.
REFERENCES
[1] | Seigel RL , Miller KD , Jemal A . Cancer statistics, 2020. CA Cancer J Clin. (2020) ;70: (1):7. |
[2] | Hoch LM , Lynch J , Balaji KC . Increasing incidence of all stages of kidney cancer in the last 2 decades in the United States: An analysis of surveillance, epidemiology, and end results program data, J Urol. (2002) ;167: (1):57. |
[3] | Lee CT , Katz J , Shi W , et al. Surgical management of renal tumors 4cm or less in the contemporary cohort, J Urol. (2000) ;163: (3):730. |
[4] | Johnson DC , Vukina J , Smith AB , et al. Preoperatively misclassified, surgically removed benign renal masses: a systematic review of surgical series and United States population level burden estimate, J Urol. (2015) ;193: (30). |
[5] | Makarov DV , Fagerlin A , Chrouser K , et al. AUA White paper on implementation of shared decision making into urological practice. American Urological Association Education & Research, Inc. 2015. |
[6] | Kutilkov A , Egleston BL , Wong Y , et al. Evaluating overall survival and competing risks of death in patients with localized renal cell carcinoma using a comprehensive nomogram, J Clin Oncol. (2010) ;28: (2):311. |
[7] | Institute of Medicine: Crossing the quality chiasm: A new health system for the 21st century. Washington D.C., National Academies Press. (2001) . |
[8] | Urology Care Foundation. (2016, October 16). What is a renal mass? [Video File]. Retrieved from URL on July 7, 2019 http://www.urologyhealth.org/urologic-conditions/kidney-cancer/videos |
[9] | Elywn G , Frosch D , Thompson R , et al. Shared decision making: A model for clinical practice. JGIM. 2012;1361. |
[10] | Readability Formulas Retrieved on February 26, 2017 http://www.readabilityformulas.com/freetests/six-readability-formulas.php |
[11] | Patel HD , Riffon MF , Joice GA , et al. A prospective, comparative study of quality of life among patients with small renal masses choosing active surveillance and primary intervention, J Urol. (2016) ;196: (5):1356. |
[12] | Makarov DV , Fagerlin A , Chrouser K , et al. AUA White paper on implementation of shared decision making into urological practice, Urology Practice. (2016) ;3: (5):355. |
[13] | Makarov DV , Holmes-Rovner M , Rovner DR , et al. Quality Improvement Summit 2016: Shared Decision Making and Prostate Cancer Screening. American Urological Association Education and Research, 2017. |
[14] | Campbell SC , Uzzo RG , Allaf ME , et al. Renal mass and localized renal cancer: AUA Guideline. American Urological Association Education and Research, 2017. |
[15] | McAlpine K , Breau RH , Stacey D , et al. What is the best treatment for my small kidney tumour? A decision aide to discuss treatment options with your doctor. Kidney Cancer Canada, International Kidney Cancer Coalition, 2019. |




