Exploring the sexual experiences and challenges of individuals with cerebral palsy
Abstract
PURPOSE:
Cerebral palsy (CP) is a prevalent motor disorder affecting children, with evolving demographics indicating an increasing survival into adulthood. This shift necessitates a broader perspective on CP care, particularly in addressing the often overlooked aspect of sexuality. The purpose of this study was to investigate experiences of, challenges with, and related factors of sexuality and intimacy that people with CP are facing.
METHODS:
This was a descriptive and cross-sectional single institution survey among individuals with CP, ages 18 to 65, who had the ability to independently complete an online survey.
RESULTS:
A total of 40 respondents participated in the survey (Gross Motor Function Classification System [GMFCS] level I/II, 32.5%; III, 35%; IV, 32.5%). Of those, 45% were partnered, 60% had past sexual experience, 47.5% were currently sexually active at the time of submitting the survey, 80% had masturbation experience, and 45.8% believed it had positive effect on their self-esteem. Only 10% received sex education tailored for people with disability, whereas school (72.5%) and internet (35%) were the most common sources of sex education. Muscle spasms, positioning difficulty, and pain/discomfort were the most common physical challenges experienced during intimate activity amongst all function stratifications. Stratification analysis showed that, compared to higher functioning respondents, a smaller proportion of lower functioning respondents were partnered (GMFCS IV, 23.1%; quadriplegic, 31.6%), had past or current sexual experience (GMFCS IV, 44.4%, 36.4%; quadriplegic, 42.1%, 26.3%, respectively), and had masturbation experience (GMFCS IV, 61.5%); Also, they had worse Quality of Life Scale scores on average (GMFCS IV, 88.4; quadriplegic, 88.3) and a higher rate of reported positive effects of sexual experiences on self-esteem than negative (GMFCS IV, 38.5%; quadriplegic, 35%).
1Introduction
Cerebral palsy (CP) can be defined as a collection of permanent motor disorders that affect the development of movement and posture, leading to activity limitation [1]. Affecting 2–2.5 children per 1,000 born in the US, it is the most common childhood physical disability [2]. The current dominant clinical approach to CP is to increase functional abilities and improve motor capabilities through an assortment of interventions, including pharmacology, surgical treatments, and physical therapy. Moreover, CP is currently still seen as a pediatric condition. This perspective is gradually becoming outdated as the population of people with CP has shown a consistent improved survival rate with a growing aging population [3]. With this realization, it is important to begin thinking about life span approaches during the transition of care from pediatrics to adulthood.
An essential facet of life that the CP population may experience differently from able-bodied people is sexuality. From an early age, people with CP may receive mixed signals in regard to intimacy, physical touch, and other important aspects of sexuality. They are constantly surrounded by their guardians and caregivers, creating a lack of privacy. While many children with CP experience cuddling and affection, the majority of handling in their daily routine is functional for caregiving and health care purposes [4]. During adolescence, they may have fewer opportunities to fully experience activities that imitate gender roles [5]. In general, whether due to physical disability, stigma associated with CP, or a combination of the two, people growing up with CP may not benefit from the same experiential learning that their able-bodied counterparts receive.
With fewer opportunities to spontaneously interact with their peers, people with CP tend to experience a delay in developing skills involved in socializing. This leads to romantic relationships and sexual activities not being pursued or experienced until later ages [6]. Like their able-bodied peers, people with CP have been shown to desire intimacy and active sex lives as sexuality is an inherent trait of human beings, despite level of physical ability [7]. These desires form an important quality of life (QOL) issue for this community. In fact, a recent study assessing the QOL of 75 adults with CP found average QOL to be at the 56th percentile with the lowest ratings in “[having] a satisfactory sexual life” and “[presenting] with depression symptoms” [8]. Another survey found high rates of anorgasmia, physical limitations of CP during sex, and emotional inhibition to initiate sexual contact [9]. Many of the participants report wanting information in regard to the impact of CP on reproduction, interventions, problems with their partner, and more, but most had not been given the opportunity to ask questions or discuss sexuality with their healthcare providers.
Addressing sexuality is a critical component of life span care for adolescents and adults with CP (and can have a significant impact of their self-esteem and QOL. The purpose of this study was to bridge the gap of knowledge on sexuality in CP by learning more about the sexual and dating history of people with CP as well as how people with CP feel about sexuality and the challenges they face regarding this topic.
2Methods
2.1Participants
This descriptive, cross-sectional, non-interventional single institution survey study took place at a large medical institution with patients followed by a physical medicine and rehabilitation department and an orthopedic surgery department that follows patients with CP from childhood through adulthood. Recruitment took place between May and August 2020. Patients were eligible if they were aged 18–65 years and had a diagnosis of CP. Survey participants independently completed the survey online in a private setting outside of the clinic. Patients were excluded if they were unable to complete the survey without having to communicate through a caretaker. This exclusion criterion ensured that participants would provide honest answers to questions of a sensitive nature without any bias from their caretakers. All participants were recruited by phone call and provided verbal informed consent. The research team obtained ethical approval from institutional ethics review boards before recruiting patients. The survey itself was administered online through RedCAP, which coded and de-identified the data.
2.2Survey
This self-developed questionnaire included a range of demographic questions to determine type of CP (topographic, muscle tone), functional level, educational level, and medications. Additional survey questions covered relationship status, history of and current level of sexual activity, history of masturbation, challenges experienced related to sexual activity, and reliance on caregivers to facilitate sexual activity. Sexual activity was defined as oral, anal, and/or penetrative. Participants also had the opportunity to answer open-ended questions including strategies used to cope with challenges related to sexual experiences, concerns related to sex and sexuality, and how they would like healthcare providers to address these issues. The Quality of Life Scale (QOLS), a 15-item instrument assessing five domains of quality of life (material and physical well-being; relationships with other people; social, community and civic activities; personal development and fulfillment; and recreation) which has been validated in a study of patients with chronic illness, was also included in the survey [10].
2.3Statistical analysis
Given the descriptive and cross-sectional nature of this study, no statistical analysis was conducted. The research primarily focused on gathering and presenting descriptive data, including demographic information, sexual behavior, physical characteristics, medication usage, and participants’ self-reported experiences and concerns related to sexual health.
3Results
3.1Demographic and physical characteristics
The research team conducted a preliminary analysis of 40 respondents. All classifications and categorizations were based on survey responses that were self-reported directly by patients. The mean age of all participants was 32.3 years ([19] 20–29 years; [11] 30–39 years; [7] 40–49 years; [3] 50–59 years) with 16 male and 24 female. The sexual orientation of the participants was as follows: 32 heterosexual, one homosexual, four bisexual, and one asexual. Patient responses of functional ability were stratified according to Gross Motor Function Classification System (GMFCS) level and topographical classification. The distribution of GMFCS levels amongst participants was as follows: 13 GFMCS I/II (ambulatory without walking aid), 14 GMFCS III (ambulate with hand-held device indoors, wheeled mobility longer distances), and 13 GMFCS IV (use powered mobility, ambulate short distances with significant assistance). The distribution of topographical classification amongst participants was as follows: nine hemiplegic, 11 diplegic, 19 quadriplegic, and one other (patient unable to classify themselves). Description of overall muscle tone included 23 spastic, 13 mixed muscle tone, two dystonic, one athetoid, and one undefined. The highest reported education level of participants included 16 with graduate degrees, 15 with bachelor’s degrees, four with associate degrees, and five with high school level education.
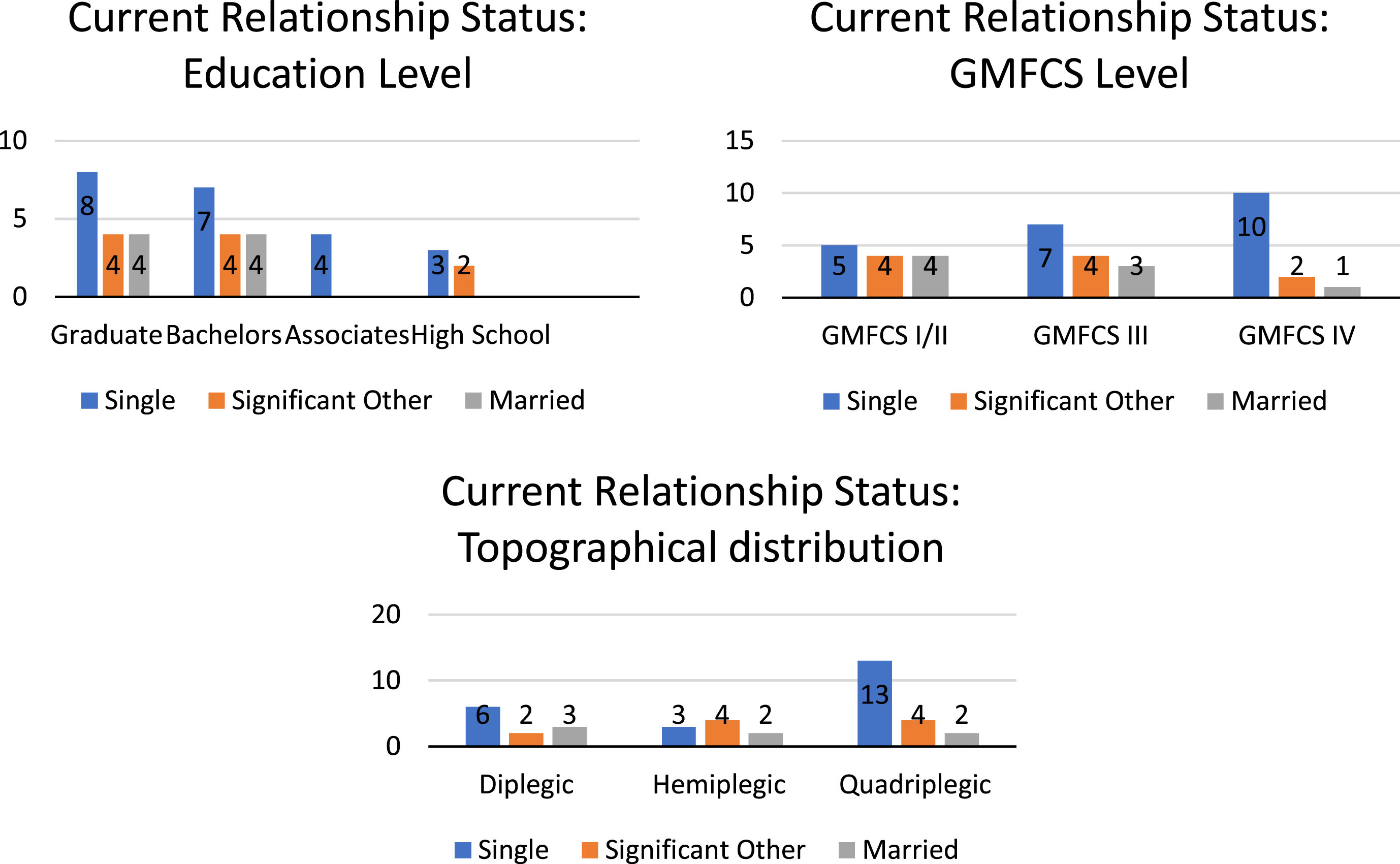
3.2Relationship status
Of respondents, 22 were single and 18 were partnered (married or with a significant other). Higher functioning respondents (GMFCS I/II) had higher rates of being partnered (61.5%) as compared to GMFCS III (50%) and GMFCS IV (23.1%) (Fig. 1). Those classified as hemiplegic had higher rates of being partnered (66.7%) versus diplegic (45.5%) and quadriplegic (31.6%). When relationship status was stratified by education level, it was found that participants with bachelor’s degrees were 53% partnered, followed by 50% with graduate degrees, 40% with high school degrees, and 0% with associate degrees.
Fig. 1
Current relationship status by (a) education level, (b) Gross Motor Function Classification System (GMFCS) level, and (c) topographical distribution.
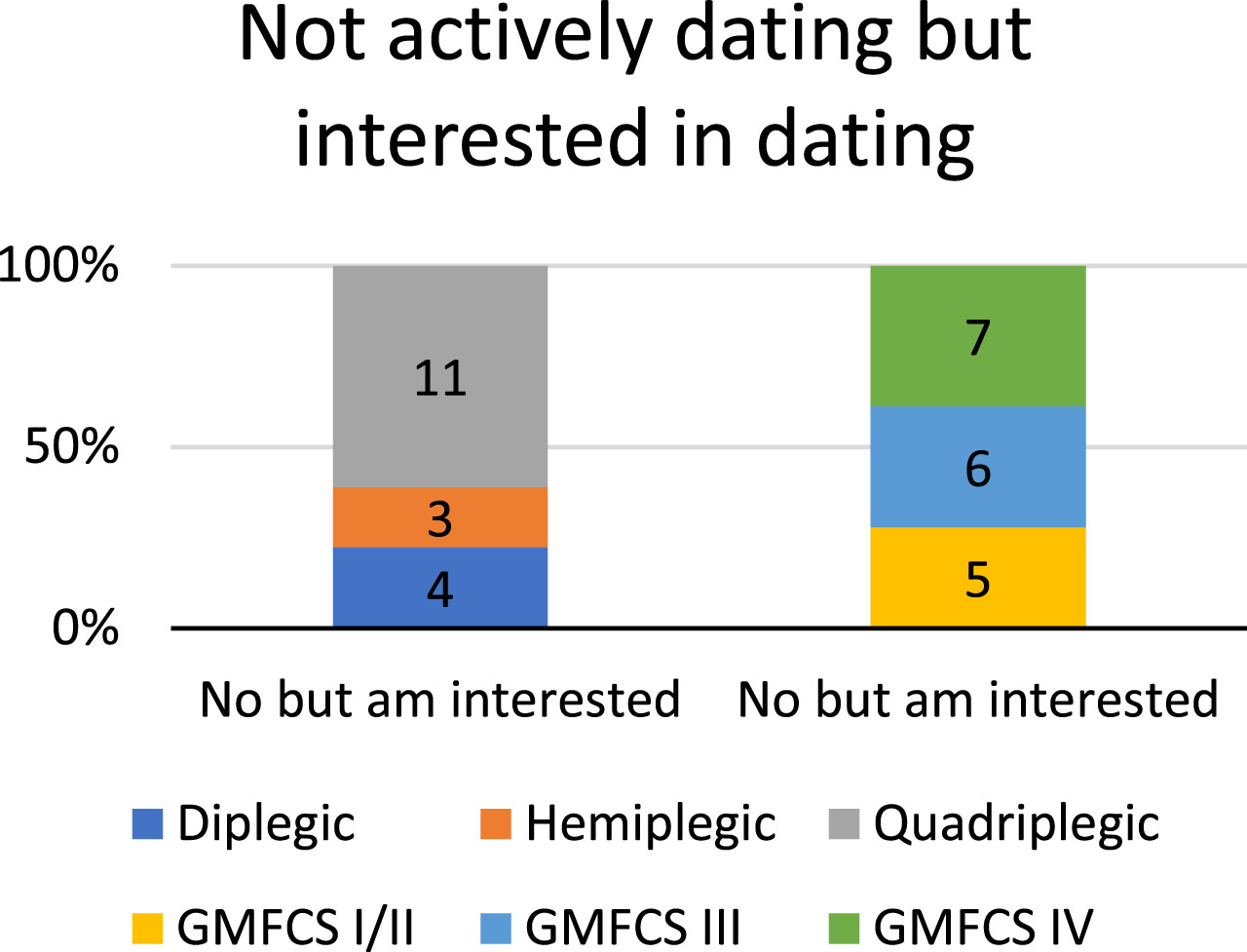
3.3Dating
Of the 22 respondents who were not in a relationship, only two (both GMFCS IV and quadriplegic) reported to be actively dating while 18 were not dating but interested in dating and two were not interested in dating (Fig. 2). The respondents with the highest rates of interest in dating were quadriplegic (61.1%) and GMFCS IV (38.9%). Conversely, those that had the lowest interest in dating were hemiplegic (16.7%) and GMFCS I/II (27.8%). The two respondents who were not interested in dating were GMFCS III (diplegic) and GMFCS IV (quadriplegic).
Fig. 2
Active dating status by Gross Motor Function Classification System (GMFCS) level and topographical distribution.
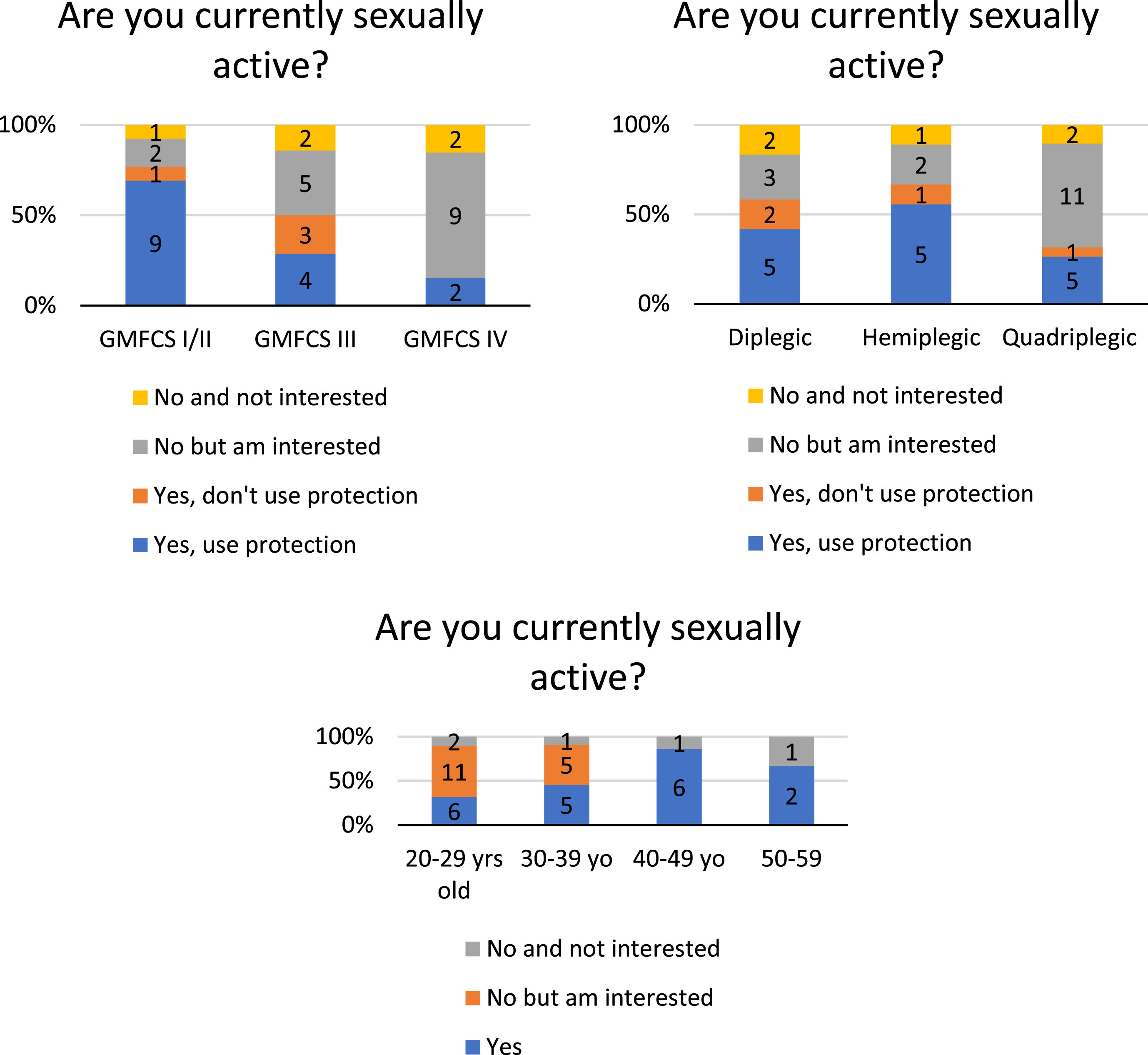
3.4Sexual activity
Of all respondents, 60% reported a history of past sexual experience; this was most commonly reported by those classified as GMFCS I/II (84.6%), hemiplegic (77.8%), aged 40–49 years (85.7%), and with a graduate degree (68.8%). Respondents with the lowest reported past sexual experience include GMFCS IV (44.4%), quadriplegic (42.1%), aged 20–29 years (31.6%), and with an associate degree (25%) (Fig. 3). These trends were also seen in the 19 respondents (47.5%) who reported being currently sexually active, with GMFCS I/II (76.9%) and hemiplegic (66.7%) most sexually active (Fig. 4). Those that were GMFCS IV and quadriplegic had the lowest rates of current sexual activity (15.4% and 31.6%, respectively). Of the 19 respondents who reported being sexually active and using protection, the following were reported as methods of protection: intrauterine device (1), condoms (9), oral contraceptive pills (1), contraceptive injection (1), female partner using a form of birth control (3).
Fig. 3
Past sexual experience by (a) education level, (b) Gross Motor Function Classification System (GMFCS) level, and (c) topographical distribution.
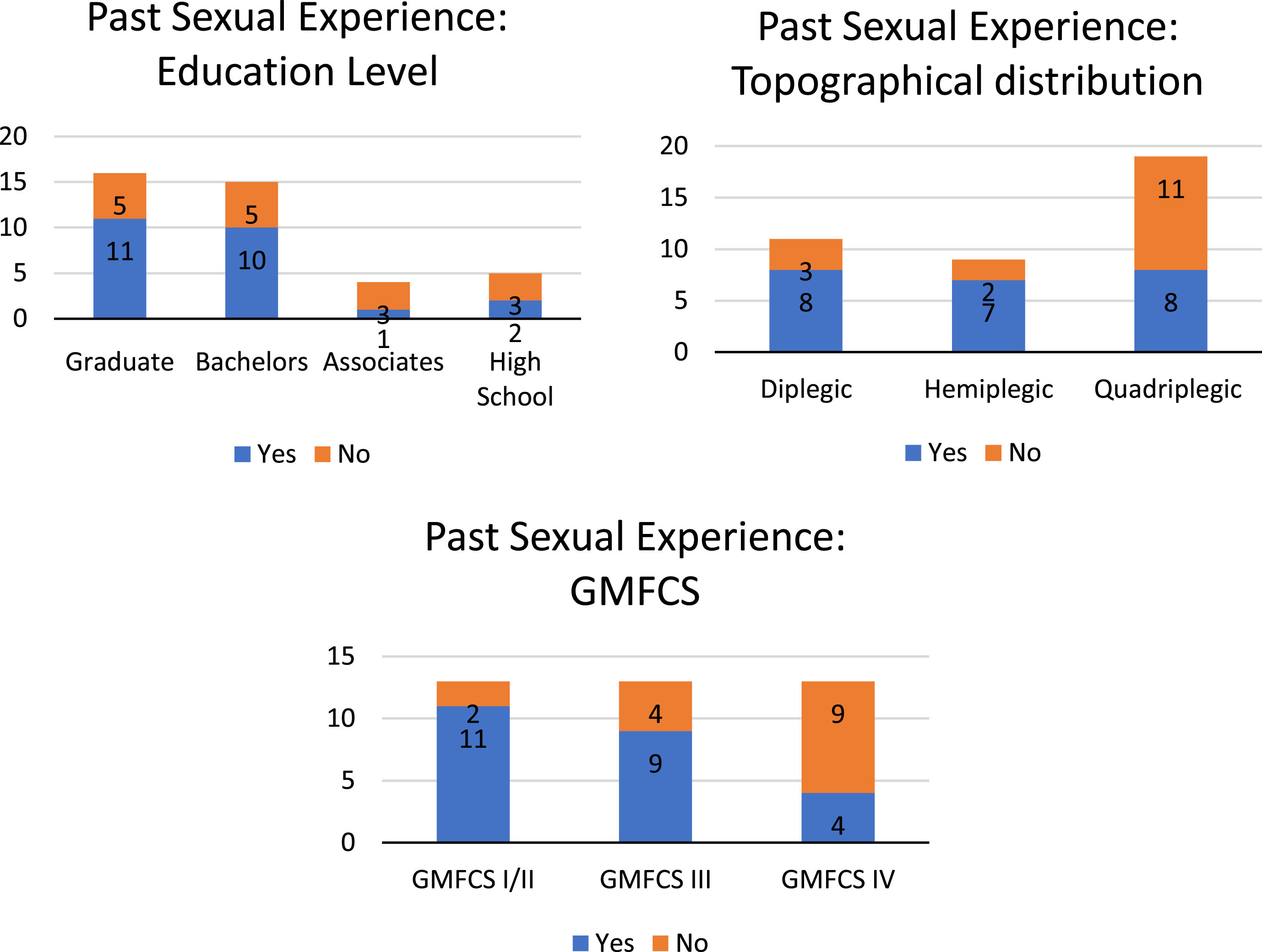
Fig. 4
Current sexual status by (a) Gross Motor Function Classification System (GMFCS) level, (b) topographical distribution, and (c) age.
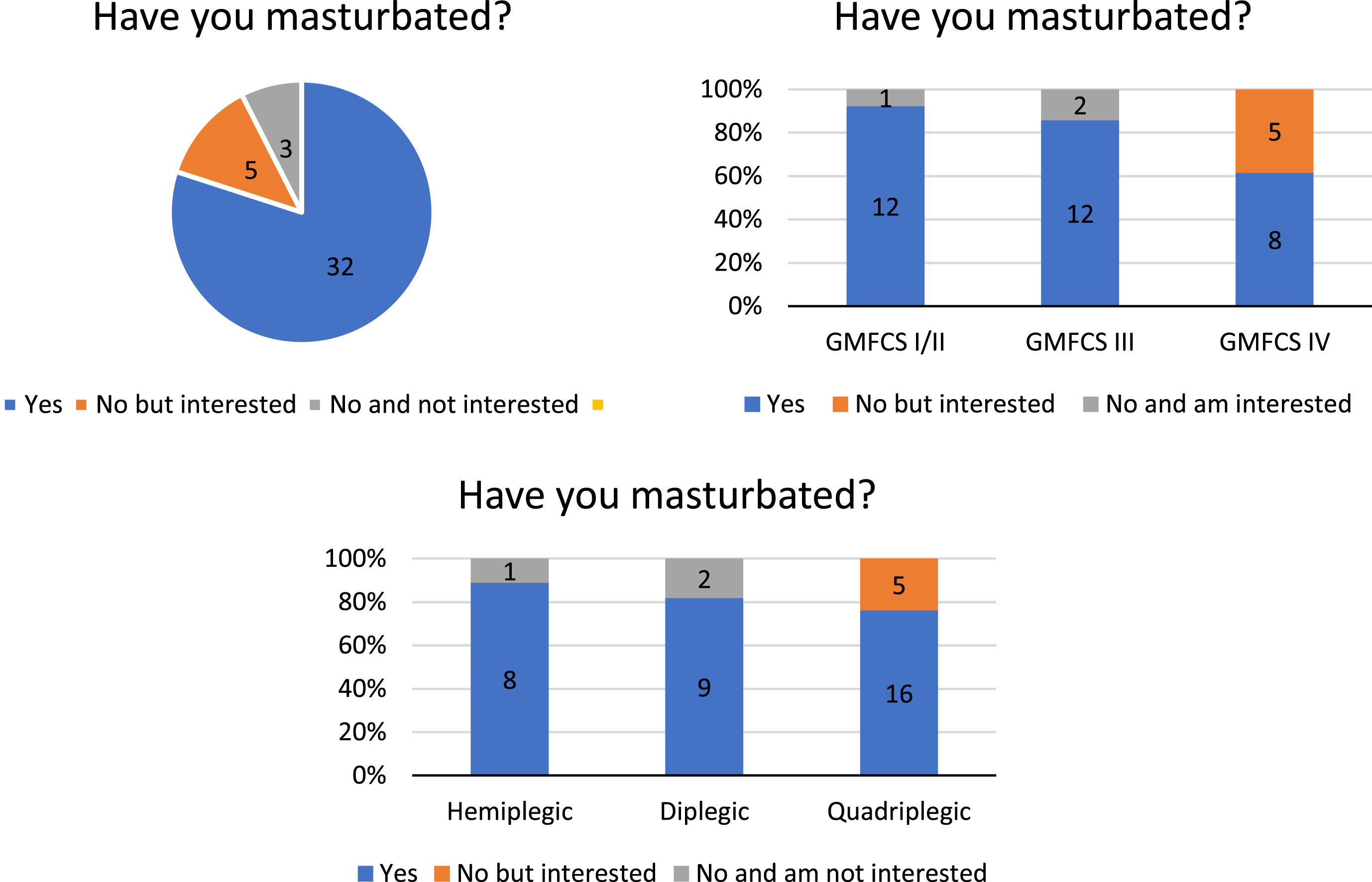
Thirty two respondents (80%) reported to have masturbated (Fig. 5). Of those, 12 were GMFCS I/II, 12 were GMFCS III, and eight were GMFCS IV; eight were hemiplegic, nine were diplegic, and 15 were quadriplegic. There were eight respondents who reported to have never masturbated, all GMFCS IV and quadriplegic, and five of them were interested in masturbation.
Fig. 5
Masturbation behavior (a) overall, (b) by Gross Motor Function Classification System (GMFCS) level, and (c) by topographical distribution.
3.5QOL
The results of the QOLS demonstrated that respondents with GMFCS IV and quadriplegia had the highest average score (88.4 and 88.3, respectively) with a range from 76–110 (higher scores indicate greater QOL). GMFCS I/II and hemiplegia were shown to have the lowest average scores (81.0 and 79.4, respectively) with a range from 54–92.
3.6Physical challenges
The most commonly reported physical challenge related to intimate activity was positioning difficulty (26 reports) followed by pain/discomfort (15), muscle spasms (14), vaginismus (9), anorgasmia (6), lack of sensation/pleasure (6), and erectile dysfunction (2). Unsurprisingly, positioning difficulty was most commonly reported by GMFCS IV (76.9%) and those with quadriplegia (78.9%). However, GMFCS I/II (61.5%) and GMFCS III (57.1%) also reported high levels of difficulty in this area (Fig. 6). There were similar rates of reported pain/discomfort and muscle spasms across all GMFCS levels; however, across topographic distribution, those with diplegia had higher reported rates when compared to hemiplegia and quadriplegia. Pain/discomfort reports ranged from 30.8% for GMFCS IV, 42.9% for GMFCS III, and 38.5% for GMFCS I/II. Muscle spasm reports ranged from 38.5% GMFCS IV, 42.9% GMFCS III, and 38.5% GMFCS I/II. Of respondents with diplegia, 63.6% reported pain/discomfort and muscle spasms versus hemiplegia (20% and 30%, respectively) and quadriplegia (31.6%). Vaginismus, while a rare complaint, was more commonly reported by GMFCS III (28.6%) and both diplegia (27.3%) and quadriplegia (26.3%). Other reported complaints included fatigue and vulvodynia. Seven respondents reported reliance on caregivers during sexual experiences, including three requiring assistance with initial positioning and one requiring assistance with transferring, undressing, and positioning.
Fig. 6
Physical challenges experienced during intimate activity by (a) Gross Motor Function Classification System (GMFCS) level and (b) topographical distribution.
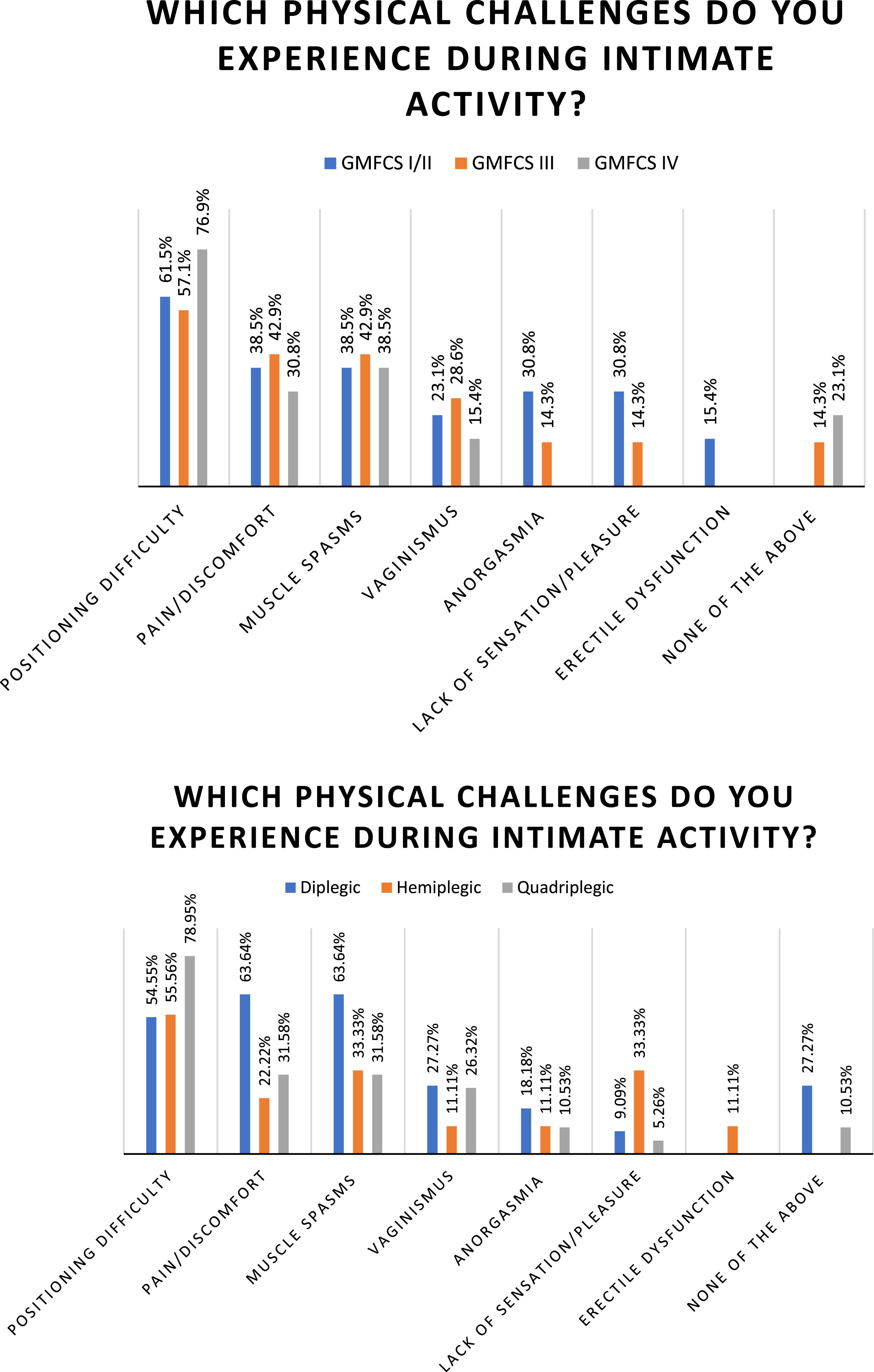
Respondents reported a variety of techniques used to cope with physical challenges related to sexual experiences. Medications that were reported to be helpful included gabapentin for vulvodynia, muscle relaxants, nerve block injections around the clitoris, botulinum toxin injections to target spasticity, and diazepam vaginal suppositories. Clinically, there were reports of discussing challenges with a psychologist, doctor, and spouse/partner; working with a gynecologist specialized in complex pelvic pain; utilizing a vaginal dilator; and participating in pelvic floor physical therapy. Situational suggestions to utilize during sexual activity included desensitizing gel, lubricant, positioning devices (wedge pillow, sitting in chair, learning against a surface), and a glass of wine. Other alternatives included oral sex, masturbation to achieve climax, and timing sexual activity based on daily fatigue and activity levels.
3.7Medications
Many medications may impact sexuality or sexual performance. The number of respondents taking each medication that commonly have impacts on sexual performance are listed as follows: selective serotonin reuptake inhibitors (7), serotonin and norepinephrine reuptake inhibitors (6), benzodiazepines (5), dopamine-norepinephrine reuptake inhibitors (3), and second generation antipsychotics (3). Medication that may have an impact on sexual performance are listed as follows: tricyclic antidepressant (1), antimanic agent (1), central nervous system (CNS) stimulants (3), anticonvulsants (9), muscle relaxants (7) including oral baclofen (3), alpha-2 agonist (1), intrathecal baclofen pump (1), and botulinum toxin injections (2). Some of these commonly used medications, such as anticonvulsants and CNS stimulants, can increase alertness and energy, which may positively or negatively impact sexual performance depending on the individual. Muscle relaxants, such as oral baclofen, alpha-2 agonists, and botulinum toxin injections, may cause sedation or fatigue, which could then indirectly impact sexual performance.
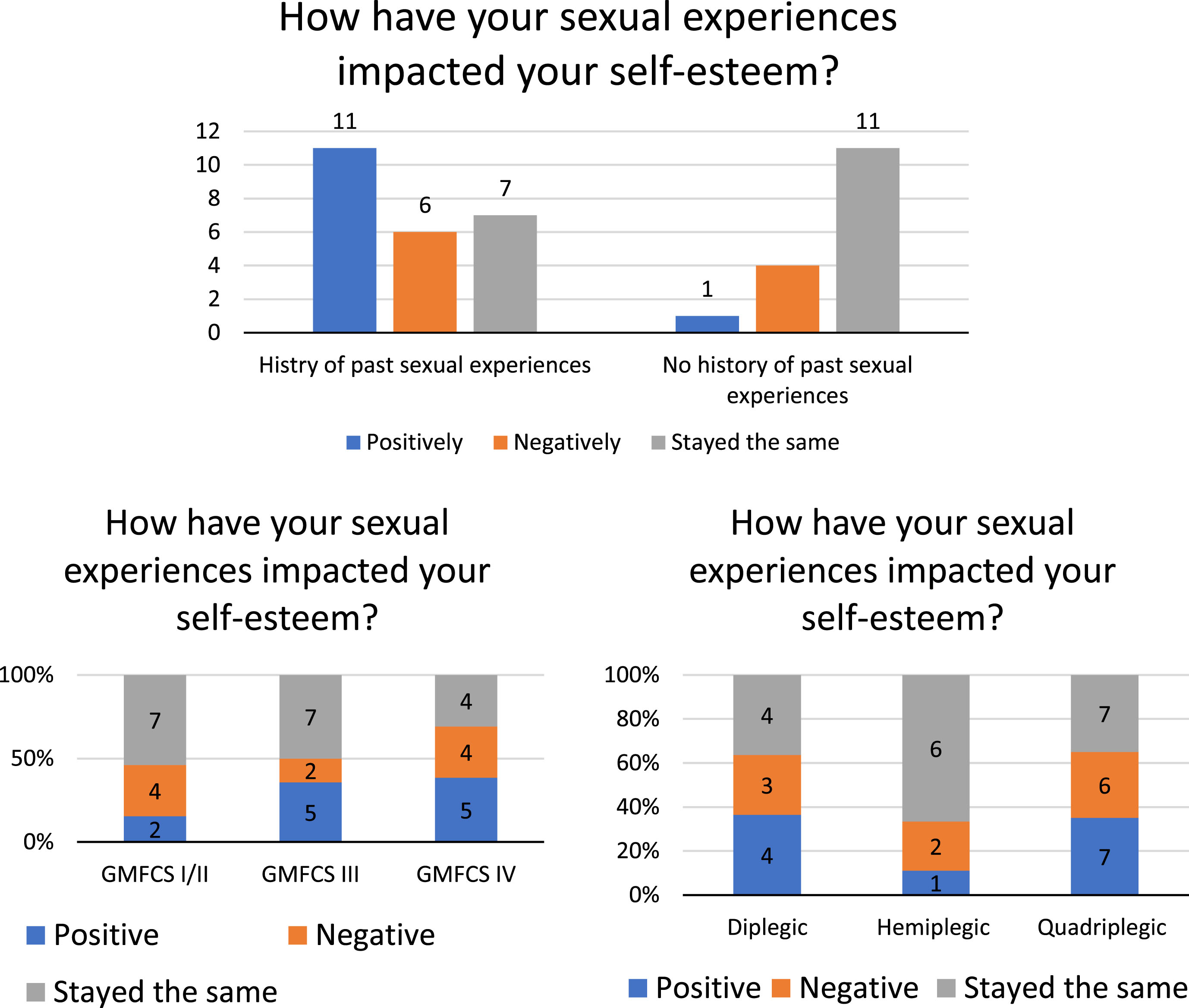
3.8Self-esteem
Respondents were asked if their sexual experiences had a positive, negative, or no impact on their self-esteem. Of the 24 respondents who reported history of sexual experience, 11 (45.8%) reported that it had a positive effect on their self-esteem while six (25%) reported a negative effect and seven (29.2%) reported no impact (Fig. 7). When stratified based on GMFCS level and topographical distribution, there were more reports of positive effects on self-esteem than negative within the following groups: GMFCS III (35.7%), GMFCS IV (38.5%), diplegic (36.4%), and quadriplegic (35%). Those groups with the highest report of negative impact on self-esteem included quadriplegic (30%), GMFCS IV (30.7%), GMFCS I/II (30.7%), and diplegic (27%). There were multiple reports of no impact on self-esteem across all GMFCS levels and topographical distribution.
Fig. 7
Impact of sexual experiences on self-esteem by (a) history of past sexual experience, (b) Gross Motor Function Classification System (GMFCS) level, and (c) topographical distribution.
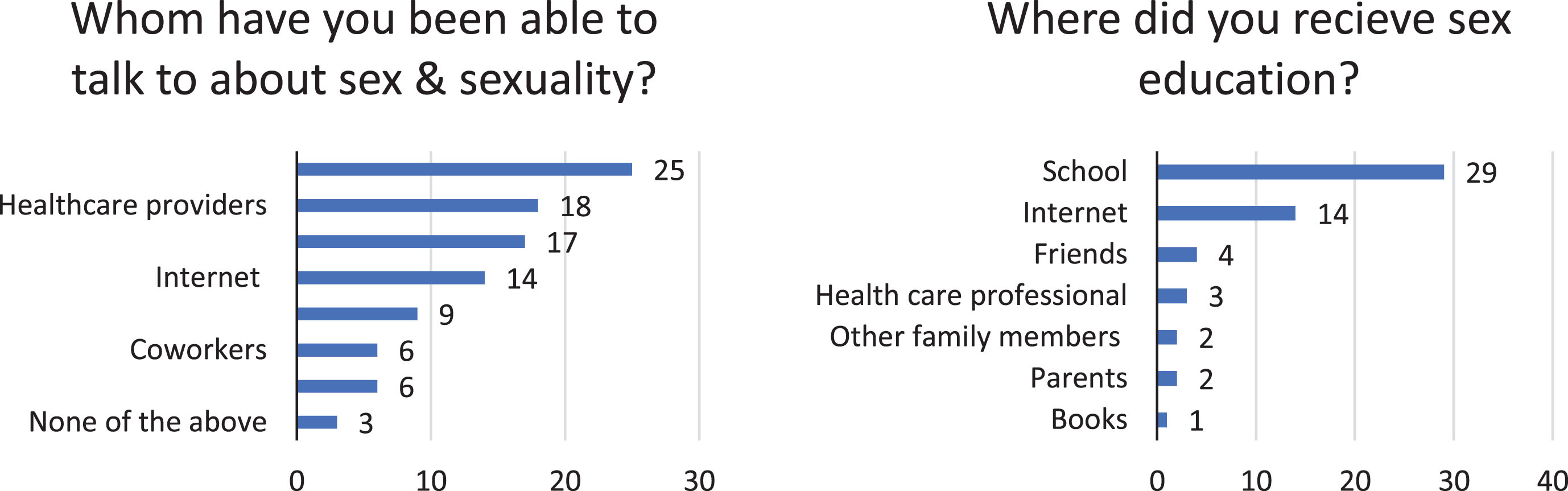
3.9Sex education
The most commonly reported source of sex education was school (29) followed by internet (14), friends (4), health care professionals (3), and family members/parents (2). Only four people reported that their sex education was specific for people with disabilities. The majority of respondents reported that they had been able to speak with friends (25), healthcare providers (18), and family (17) about sex and sexuality. Fourteen reported communicating with others through the internet, and nine were in support groups (Fig. 8).
Fig. 8
Sex education and communication by (a) people that the patients have been able to talk to about sex and sexuality and (b) resource of sex education they have received.
3.10Concerns and suggestions
An open-ended prompt in the survey asked participants to report their concerns related to sex and sexuality. Responses included difficulty and embarrassment when communicating about sexual activity, including communicating with partners about these issues. Some respondents reported self-consciousness surrounding dating and anxiety/fear of how their body will react to sex. There were also concerns raised about the logistical challenges of two people with disabilities participating in sexual activity, lack of inclusive sex toys, and challenges of utilizing various barrier methods of contraception with fine motor impairment.
Participants had multiple suggestions for ways in which healthcare providers can become more aware of these issues and help guide patients through questions and concerns. There was a common theme of wanting healthcare providers to initiate more conversations on this topic, asking patients about their successes and challenges related to sexual experiences. There was a desire for conversations to be more body and sex positive with less focus on “problems,” which can negatively impact self-esteem. Patients were looking for education and guidance as to how their CP may impact their ability to participate in sexual activity, what to anticipate for pregnancy and childbirth, how to consider birth control options, and being connected to available resources. Additionally, participants voiced a desire for more research to be conducted on aging with CP to help understand how to best manage the aging process and potential decline.
4Discussion
The findings are based on a total of 40 respondents that participated in the survey (GMFCS I/II, 32.5%; III, 35%; IV 32.5%). Overall, 45% were partnered, 60% had past sexual experience, 47.5% were sexually active, 80% had masturbated, and 45.8% believed it had positive effect on their self-esteem. Only 10% received sex education tailored for people with disability, whereas school (72.5%) and internet (35%) were the most common sources of sex education. These findings indicated a possible association between functional abilities and topographical CP classification with sexual experiences and QOL. Compared to higher functioning respondents, a smaller proportion of lower functioning participants were partnered (GMFCS IV, 23.1%; quadriplegic, 31.6%), had past or current sexual experience (GMFCS IV, 44.4%, 36.4%; quadriplegic, 42.1%, 26.3%, respectively), and had masturbation experience (GMFCS IV, 61.5%). Also, they had worse QOLS scores on average (GMFCS IV, 88.4; quadriplegic, 88.3), and higher rates of reporting positive effects of sexual experiences on self-esteem than negative (GMFCS IV, 38.5%; quadriplegic, 35%).
The primary focus of this survey was on dating, relationship status, and intimate activity. GMFCS I and II respondents had the highest percentages of people actively dating (50% and 35.7%, respectively) and the highest percentage who had engaged in intimate activities (100% and 78.6%, respectively). It is interesting to note that the GMFCS III and IV respondents had the lowest percentages of participants who were in relationships (0% and 18.2%, respectively) and had sexual experience (28.6% and 45.5%, respectively) while 25% of the GMFCS V respondents, who were in the most functionally impaired GMFCS level, were actively dating and most had experience with sex (62.5%). This indicates that GMFCS score, while a good estimate of day-to-day functioning, has little bearing on dating status and history of intimate activity.
In terms of dating, hemiplegic respondents had a higher percentage of participants who were actively dating (40%) than their diplegic and quadriplegic counterparts (16.7% and 20%, respectively). Hemiplegic respondents also had a higher percentage of participants who had engaged in intimate activities than other respondents (80%). More than half of the diplegic respondents had engaged in intimate activities (66.7%) while quadriplegic respondents, with their more extensive involvement of CP, had the lowest percentage of sexual experience (45%). This may indicate a negative correlation between the extent of the body affected by CP and history of sexual experience. As a whole, topographical classification seemed to be more consistent in predicting dating status and past sexual experience than GMFCS levels.
Similar to dating and intimate activity, no correlation seemed to exist between prevalence of physical challenges and GMFCS level. Positioning difficulty, muscle spasms, and pain/discomfort were the most common physical challenges (reported by 27, 17, and 15 respondents, respectively) experienced during intimate activity amongst all stratifications of GMFCS and topographical classifications. The survey also asked how respondents cope with these physical challenges, which yielded a variety of responses from best positions, best times of day, physical therapy exercises and stretches, and useful pharmacologic agents.
To sum up, topographical classification seemed to be more strongly correlated with dating status and past sexual experience than GMFCS levels; however, neither classification system seems to be an adequate predictor for the physical challenges experienced during intimate activity. Aside from the predictive power of these CP classification systems, it is important to report that a large percentage of survey respondents were actively dating (45.2%) and a majority (59.5%) had past sexual experiences. All these results confirm that sexuality and intimacy are important QOL considerations. Members of the medical community need to dispel the misconception that people with physical disabilities cannot have sex and work to help facilitate more and better sex for people with CP.
This study faced several limitations that merit consideration. First, the exploration of sexual activity focused exclusively on penetrative forms (oral and anal), omitting non-penetrative forms such as hugging, touching a partner’s genitals or breasts, and being touched. While this may limit the comprehensiveness of understanding sexual activity among individuals with CP, valuable insights are nonetheless provided about a subset of sexual behaviors that are less frequently discussed within this population. Additionally, the sample population exhibited a higher degree of college education compared to the general CP population, potentially limiting the representativeness of the findings. Also, the survey did not specify a timeframe for defining ‘currently sexually active,’ which could lead to variability in respondent interpretation. Yet, this flexibility allowed for a broad inclusion of experiences reflective of individuals’ current lives. The absence of questions regarding the desire for tailored sex education and the lack of racial/ethnic data collection to understand the diversity of respondents represent further limitations.
Moreover, a substantial number of GMFCS I patients declined participation, possibly due to a perception of their condition as having a minimal impact on their daily lives, coupled with an absence of responses from individuals with monoplegia. This under-representation of less functionally impaired individuals with CP suggests a skewed perspective towards those with more severe conditions. Another limitation was the size and geographical scope of the survey. There were only 40 respondents, all of whom received care within the last few years in New York City. Despite these limitations, the research provides an essential glimpse into a relatively unexplored area of CP research. It underscores the diversity of sexual experiences and educational needs among individuals with CP, paving the way for more extensive, inclusive future studies that can address these identified gaps.
Moving forward, the research team plans to broaden the scope of this survey, reaching out to more patients from a wider geographical range to improve the reliability and validity of results. Additionally, the data collected can be used to provide a foundation for further studies as well as discussion topics for focus groups between patients and healthcare providers. They can also help inform the care that healthcare workers provide for their patients. For instance, use of botulinum toxin and muscle relaxants such as suppository diazepam in the pelvic areas facilitates better sex by reducing muscle spasticity.
5Conclusion
Sexual behavior is prevalent among adults with CP, highlighting the significance of addressing sexual health as an integral aspect of comprehensive CP care that can significantly influence QOL and self-esteem. Tailored sex education is an urgent necessity, underscoring the importance of healthcare providers initiating discussions about sexual health, assisting patients in navigating their concerns, and providing relevant resources. This descriptive study will be used to create a stepping stone for future research and for the improvement of the comprehensive care of people with CP.
Acknowledgments
This works is sponsored Columbia University NIH T35 Summer Research Program.
Conflict of interest disclosure
Heakyung Kim declares the following potential conflicts of interest related to this work: consultancy and advisory board member of Ipsen Pharmaceuticals; consultant for Allergan and Merz; advisory member for pediatric spasticity for Allergan; advisory board member for Pacira Biosciences.
References
[1] | Rosenbaum P , Paneth N , Leviton A , et al. A report: the definition and classification of cerebral palsy. Dev Med Child Neurol. (2007) ;49: (6):480. |
[2] | Krigger KW . Cerebral palsy: an overview. Am Fam Physician. (2006) ;73: (1):91–100. |
[3] | Brooks JC , Strauss DJ , Shavelle RM , Tran LM , Rosenbloom L , Wu YW . Recent trends in cerebral palsy survival. Part I: period and cohort effects. Dev Med Child Neurol. (2014) ;56: (11):1059–64. |
[4] | Cole SS , Cole TM . Sexuality, Disability, and reproductive issues through the lifespan. Sex Disabil. (1993) ;11: , 189–205. |
[5] | Gordon S . Living fully: A guide for young people with a handicap, their parents, their teachers, and professionals. New York: John Day; 1975. |
[6] | Wiegierink D , Roebroeck M , Donkevoort M , Cohen-Kettenis PT , Stam H . Social, intimate and sexual relationships of adolescents with cerebral palsy compared with able-bodied age-mates. J Rehabil Med. (2008) ;40: , 112–8. |
[7] | Czapla K , Otrebski W . Differences in sexual behavior of teenagers and young adults with cerebral palsy: The role of sexual needs and sexual esteem. Sex Disabil. (2018) ;36: (1):33–46. |
[8] | Maestro-Gonzalez A , Cruz Bilbao-Leon M , Zuazua-Rico D , Fernandez-Carreria JM , Baldonedo-Cernuda RF , Mosteiro-Diaz MP . Quality of life as assessed by adults with cerebral palsy. PLoS One. (2018) ;13: (2):e0191960. doi: 10.1371/journal.pone.0191960 |
[9] | Wiegerink D , Roebroeck M , Bender J , Stam H , Cohen-Kettenis P . Sexuality of young adults with cerebral palsy: Experienced limitations and needs. Sex Disabil. (2011) ;29: :119–28. doi: 10.1007/s11195-010-9180-6 |
[10] | Burckhard C , Anderson K . The Quality of Life Scale (QOLS): Reliability, validity, and utilization. Health Qual Life Outcomes. (2003) ;1: :60. doi: 10.1186/1477-7525-1-60 |




