Addressing social determinants of health through customization: Quality improvement, telemedicine, and care coordination to serve immigrant families
Abstract
PURPOSE:
The purpose of this project was to establish a pathway for electronic medical record (EMR) customization, utilizing quality improvement methodology, to both identify and address adverse social determinants of health (SDOH) among a diverse spina bifida (SB) population.
METHODS:
Starting in September 2020, the four fundamental steps were to (1) facilitate an advisory committee to safeguard the standard clinical protocols, (2) characterize barriers to implementation, (3) evaluate workflow to sustain data entry capture, and (4) manage the technology platform for seamless integration. The SB clinic was the first clinic within the enterprise to rollout the use of an adverse SDOH mitigation activity. A Spanish-speaking interpreter was scheduled for all clinics, as many families were limited in English proficiency.
RESULTS:
The customization of the EMR to support an efficient workflow to address SDOH was feasible in a large and diverse urban medical center. Of the 758 patients served in the clinic, a myelomeningocele diagnosis was present in 86% of individuals. While 52% of participants were female, ethnically 52% of individuals served were Latino. Many of these individuals disclosed being recent immigrants to the United States. Often immigration and asylum related issues were at the forefront of the SDOH issues addressed.
CONCLUSION:
Given the occurrence of adverse SDOH among individuals with SB, many of whom are new Latin-American immigrants, meaningful clinical efforts are needed to both identify and address the causes of the observed disparities. EMR customization is feasible and can identify and, through social prescriptions, address SDOH to support the provision of safe, high quality, and equitable care for vulnerable and medically complex populations at home and potentially abroad.
1Introduction
The Centers for Disease Control and Prevention (CDC) has defined social determinants of health (SDOH) as the “conditions in the environments in which people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality of life outcomes and risks” [1]. SDOH can be divided into four interrelated categories: 1) socioeconomic circumstances, 2) psychosocial factors, 3) political, economic, and cultural drivers, and 4) neighborhood environment [2, 3]. Health inequities are inextricably linked to SDOH and can persist intergenerationally, driving avoidable differences based on race, ethnicity, and socioeconomic status [4]. Although immigration itself is conceptualized as a SDOH, immigration is often a result of other antecedent SDOH. Poverty, war-associated violence, political discrimination, and work-related prospects are a few examples. In the United States (US), a substantial percentage of the pediatric population is composed of immigrant children [5], and according to the US Census Bureau, over one-quarter of children live with at least one immigrant parent [6]. Contemporaneously, in 2018, over 3.8 million people immigrated to the European Union (EU); and by 2022, 23.8 million of its residents were non-EU citizens [7]. Furthermore, across Europe, one third of refugees and migrants are children [8].
As the number of displaced populations, immigrants, and refugees is likely to continue to escalate worldwide, it is important to consider SDOH within a global health context. It is estimated that SDOH such as socioeconomics, education, housing, employment, and one’s lived environment determine 90% of health outcomes while only 10% are determined by biomedical health care [9]. Thus, SDOH are complexly concomitant with numerous chronic medical conditions, including spina bifida (SB) [10–12]. Even self-management and independence, which are essential skills when transitioning into adult-centered care, are dependent on demographics and SDOH [13]. Consequently, harmonious with a growing body of literature, these SDOH differences are documented to appear early in the lifespan and persist across the SB continuum of care, as documented through the National Spina Bifida Patient Registry (NSBPR) [14, 15].
Neural tube defects (NTDs) are characterized by aberrant closure and exposure of the embryonic neural tube, and they are one of the most common types of congenital malformations [15, 16]. The two most common types of NTDs are SB and anencephaly [17]. While it is challenging to determine the true incidence of NTDs as different measurement approaches exist [18], an estimated 300,000 babies are born with NTDs worldwide each year [19]. Global prevalence at birth is approximately 18.6 per 10,000 live births [18, 20]; whereas in the US specifically, birth prevalence of NTDs is nearly six per 10,000 live births [21]. An estimated 1,500 children are born with NTDs in the US annually [17]. Both within and outside of the US, there are wide variations in the prevalence of NTDs by race and ethnicity. For example, birth prevalence is greater among Latino people compared to White Americans, and lower among Black Americans [22]. Compared to the US, low- and middle-income countries experience higher prevalence of NTDs [23]. In some areas of Latin America, reports of birth prevalence have reached 96 cases per 10,000 live births, while in certain areas of Africa, estimates approach 75 cases per 10,000 live births [17, 24]. Even as Latino people immigrate into the US, they consistently have a higher birth prevalence ofNTDs [22].
The NSBPR – a partnership between the CDC and SB clinics throughout the US – has begun to document connections between SDOH and SB [10, 15]. An NSBPR study conducted by Schechter et al. demonstrated that wide variations in outcomes exist among people with SB related to demographic characteristics including age, gender, race/ethnicity, and health insurance status, after controlling for SB-related intrinsic characteristics [25]. Schechter et al. reported that non-Hispanic Black patients were less likely to have documented bladder/bowel continence as compared to other groups; and Latino patients were less likely than non-Hispanics. Overall, as compared to other groups, Latino and non-Hispanic Black patients and those without private insurance had poorer outcomes [25]. Another NSBPR study reinforced this evidence by demonstrating that the likelihood of having bladder continence was significantly greater among non-Hispanic White patients and those with private insurance [26]. Furthermore, an additional NSBPR publication revealed an association between non-Hispanic White race/ethnicity and private insurance and an increased likelihood of receiving surgical services to treat neurogenic bowel [19]. Chowanadisai et al., in a study not linked to the NSBPR, observed that even after controlling for socioeconomic status, satisfaction with health care was significantly lower among Latino people with SB [27].
The connection between SDOH and SB implies that meaningful clinical efforts are needed to both identify the causes of the observed disparities and address them. Given the occurrence of adverse SDOH among local individuals with SB, many of whom are new Latin-American immigrants, a quality improvement-based intervention was implemented to recognize and commence to address SDOH identified in a SB clinic. The specific purpose of this stage of the project was to establish a pathway for electronic medical record (EMR) customization to both identify and begin to address SDOH among this vulnerable population.
2Methods
Utilizing quality improvement (QI) methodology, care coordination was catalyzed and NSBPR activities were supported institutionally by developing a platform for a structured data entry system (SDES) [28]. Starting in September 2020, the four fundamental steps were to (1) facilitate an advisory committee to safeguard the standard clinical protocols, (2) characterize barriers to implementation, (3) evaluate workflow to sustain data entry capture, and (4) manage the technology platform for continuous integration [29]. The advisory committee was composed of individuals with SB and family members of individuals with SB who shared their opinions and perspectives regarding the various SB clinic initiatives. This group supported the implementation of this SDOH-related project.
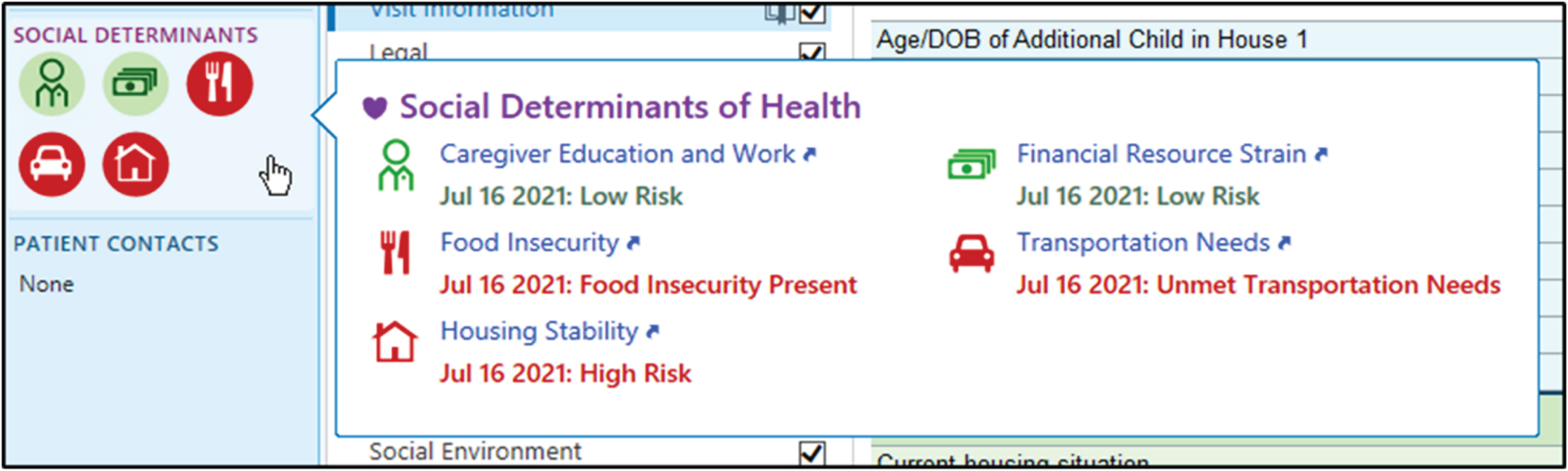
Collaboration with an EMR programmer (EPIC®) allowed for workflow customization to not only capture NSBPR variables, but also document SDOH needs into a SDOH activity (i.e., wheel) within the EMR [30]. A set number of standard SDOH specific questions were systematically included in the clinical documentation by the clinic’s licensed social worker (Fig. 1). Following this data entry step, other SDOH functionality was automatically updated in EPIC® (e.g., SDOH domain wheel, SDOH Storyboard icons, SDOH risk scores). The risk classifications were to help clinicians identify social needs, streamline localization of resources, and assist in care coordination for face-to-face or telehealth follow-up as appropriate. The SDOH that were documented during this new clinical workflow through the tool included food insecurity, transportation needs, housing stability, and financial resource strain, as well as caregiver education and work (Fig. 1). The date of assessment was recorded, and the risk classified in the following categories: low risk (green), moderate risk (yellow), and high risk (red).
Fig. 1
Social determinants of health (SDOH) specific questions are included in the social work clinical documentation. Subsequently, other SDOH activity related functionality is automatic updated in EPIC® (e.g., Storyboard icons, the SDOH domain wheel, SDOH risk scores).
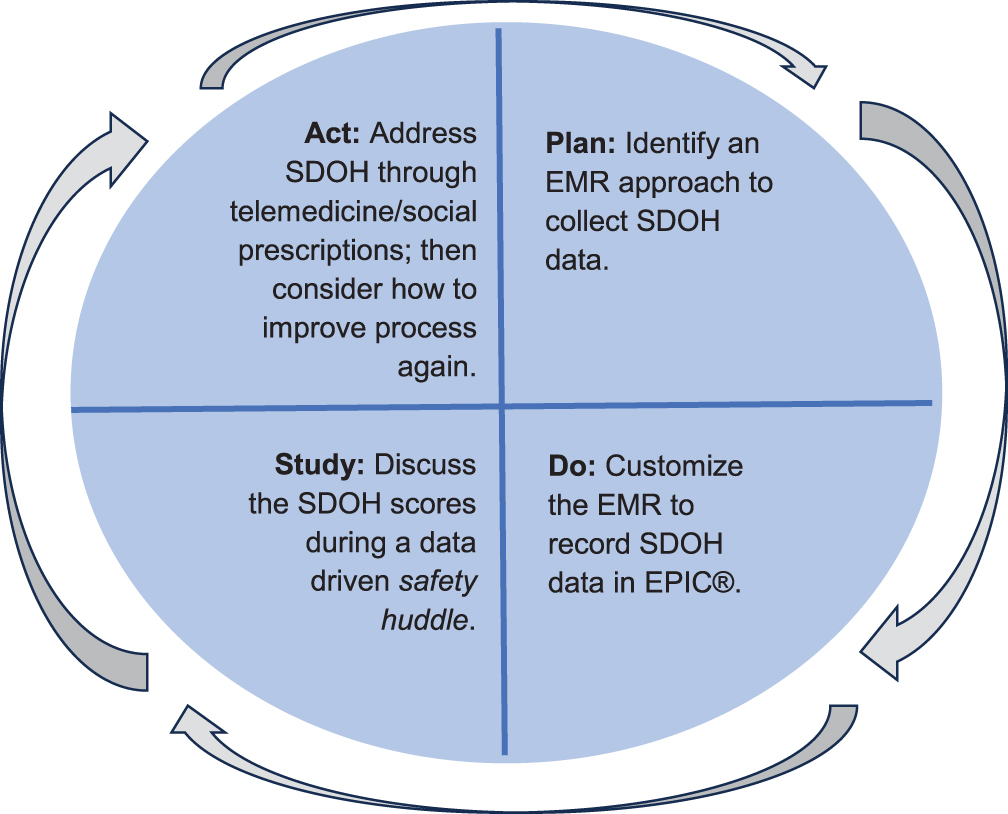
The Model for Improvement [31] was the central QI conceptual framework. “This model is based upon three fundamental questions that frame the improvement efforts: (1) What are we trying to accomplish? (2) How will we know that a change is an improvement? (3) What changes can we make that will result in improvement?” [32]. Additionally, a SDOH-minded approach to accomplishing a QI project requires that the definition of the problem to be addressed has a scope beyond the clinical setting. Therefore, the following question was asked: “What contextual factors in the life of a child or family are barriers to our quality and outcomes goals?” [33]. Hence, Plan-Do-Study-Act (PDSA) cycles were performed to drive the process of (1) identifying an EMR approach to collect SDOH data, (2) customizing the EMR to create fields for data capture and display, (3) capturing data into EPIC® by a social work colleague, (4) discussing the SDOH scores during a data driven safety huddle, and (5) addressing SDOH needs through the nursing and social work clinical staff (Fig. 2). As usage of PDSA cycles have been shown to improve the paper-based screening of SDOH, the aim was to document the feasibility of implementing a broader approach utilizing EMR customization [30, 34].
Fig. 2
Plan-Do-Study-Act for a social determinants of health (SDOH) related project. EMR: Electronic medical record.
3Results
3.1Population demographics
A myelomeningocele diagnosis was present in 86% of individuals served in the clinic (n = 758 total clinic participants). Other documented diagnoses were lipomyelomeningocele, meningocele, and fatty filum. In addition, the data demonstrated the diverse population that attends the SB clinic at Texas Children’s Hospital/Baylor College of Medicine (TCH/BCM). While 52% of participants were female, ethnically 52% of individuals served were Latino. The sample also included 9% Black, 4% multiracial, 3% Asian, and 1% of individuals who identified as “other.” Many of these individuals disclosed being recent immigrants who had resided in the US for only a couple of years or less. Therefore, to facilitate communication, a Spanish-speaking interpreter was scheduled for each clinic, as many families were limited in English proficiency.
3.2EMR customization
The SB clinic was the first clinic within the enterprise (the largest pediatric hospital system in the nation) to rollout the use of the EMR’s SDOH activity. The EMR was leveraged through the systematic use of the SDES, which allowed data entry based on predefined categories and conditions. The SDES not only permitted standardization of NSBPR registry data entry and collection, but also allowed easier reporting back of the SDOH discrete data and more efficient cross-care coordination and telemedicine appointments. The SDOH activity and wheel was implemented in the EMR on April 2, 2022, and fully operational on all individuals in the multidisciplinary SB program by April 5, 2022.
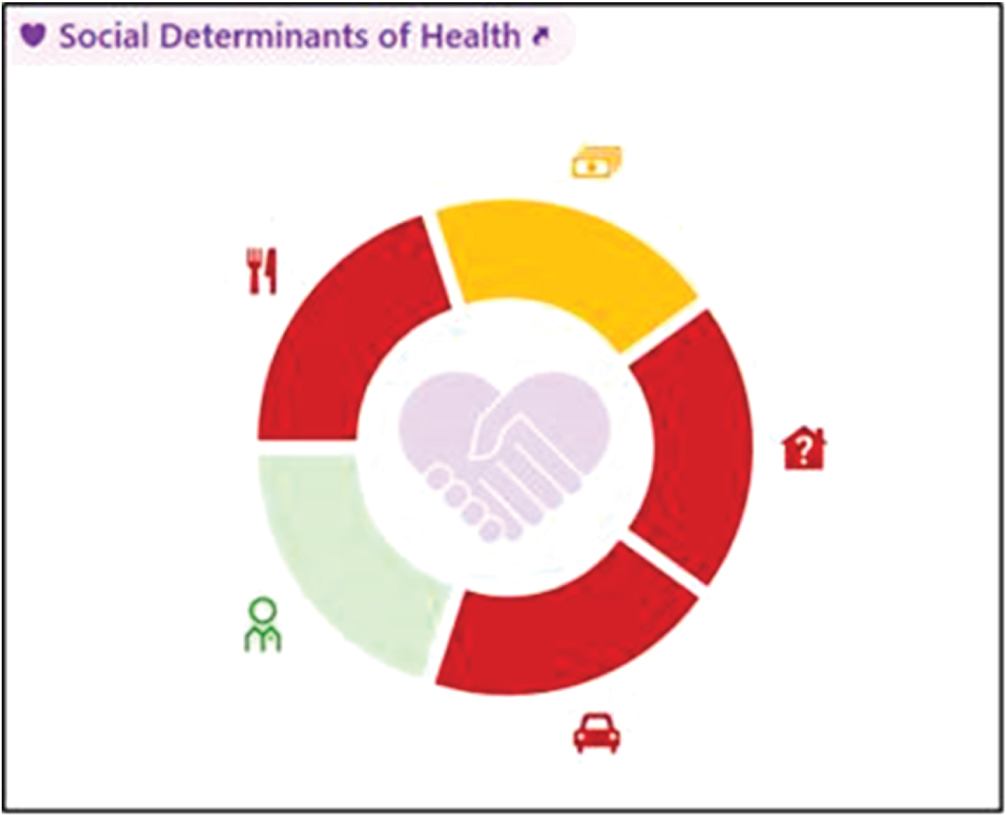
The SB multidisciplinary clinic at TCH/BCM meets weekly and members of the team, including SB physicians, nurses, care coordinators, clinic staff, and social workers, review the individuals scheduled for team clinic prior to their appointments. The SDOH wheel (Fig. 3) was prepopulated based on the social worker’s clinical documentation. The wheel for each patient was reviewed in this pre-clinic meeting with the team in order to plan to address needs where risk had been identified at the past visit and in the interim since the individual was last evaluated by the SB multidisciplinary team. During these safety huddle meetings and through care coordination efforts, an EMR visual SDOH wheel was useful in addressing adverse social determinants (e.g., food insecurity concerns, transportation needs, immigration related requirements).
Fig. 3
The Social Determinants of Health wheel is a part of the electronic medical record’s SDOH activity. The color-coded risk classifications help clinicians identify social disparities, streamline localization of resources, and assist in care coordination for face-to-face or telehealth follow-up as appropriate.
3.3Immigration and social work
The care providers paired with social work addressed the identified SDOH risks in the SB multidisciplinary clinic. Post-clinic, the social worker followed up on the documented SDOH to ensure that attempts had been made to address the needs. When food insecurity was identified as a need, the phone number for the family’s local food pantry was provided. If transportation was an identified need, a referral could be placed and education provided for medical transport through public insurance when appropriate. Often immigration and asylum related issues were at the forefront of the SDOH issues, and the clinic social worker (who had specialized knowledge in this area) was able to counsel the families in appropriate steps and directions for assistance. Frequently, this prompted physician-initiated documentation for legal purposes. In summary, the SDOH activity and wheel supplied care providers with an additional means to document, increase awareness, and most importantly, address adverse SDOH that were identified among families served.
4Discussion
In a way, all medicine is social medicine, as the late psychiatrist Leon Eisenberg noted, and the call for health care professionals to address SDOH in clinical practice is greater now than ever before. In order to improve outcomes and ameliorate inequities, it is crucial for care providers to better understand and address a family’s social circumstances [35]. Knowledge of SDOH can help connect families to essential community-based resources, facilitate care coordination services, and guide clinical decision-making [36]. On a broader scale, states may use SDOH information to inform QI and program evaluation initiatives, provide data for surveillance efforts, and help develop evidence-based public health policy [36]. As EMR utilization has globalized, this workflow and EMR customization are provided in the hopes of aiding the upscaling of this SDOH mitigation-related intervention across other SB clinics in the service of immigrant and asylum-seeking families [37]. The presented framework can assist in the care and advocacy of displaced populations both in the US and potentially abroad. An international perspective is relevant given the globalization of the use of EPIC® throughout Europe, Latin America, and other regions. For example, EPIC® is used throughout the United Kingdom, Norway, Denmark, and Finland [38, 39]. As diverse populations continue to immigrate to Europe, addressing SDOH will be crucial in improving the overall wellbeing of these vulnerable populations. SDOH include many factors such as income, education, immigration, etc., all of which are important to address in clinical medicine everywhere [40].
The US Department of Health and Human Services’ Healthy People 2020 initiative underscored the importance of addressing SDOH by advocating for the creation of “social and physical environments that promote good health for all” [21]. Under this charter, social and physical determinants include language, culture, and access to health care services and schools, as well as limited exposure to deleterious social norms, physical barriers, and hazards [41]. Therefore, there is a link between SDOH and the well-documented health disparities among minority populations [21]. The SDOH framework encompasses four categories of interrelating factors: 1) socioeconomic circumstances, 2) psychosocial factors, 3) political, economic, and cultural drivers, and 4) neighborhood environment [42, 43].
In accordance with the American Academy of Pediatrics’ Policy Statement on Pediatricians and Public Health, when optimizing the health of a nation’s children, “Pediatricians and their public health colleagues are important actors in addressing the social determinants of health” and greater collaboration “ha[s] the potential to improve individual- and population-level child health outcomes” [5]. Moreover, when advocating for comprehensive change, it is helpful to consistently apply a framework that operates at the family, practice, and community levels, to effectively address SDOH in clinical practice.
4.1Family level
At the family level, care providers encounter patients facing multiple barriers, and each family’s struggles may not be obvious [44]. Systematic collection of SDOH data that includes both individual-level data reported by the family as well as community-level data regarding characteristics about the neighborhood where the family resides (e.g., geocoding) is important and is the next level of intervention for this program [45]. One future goal is to make these data more easily available to the team to help facilitate relevant screenings, resource referral, care coordination, and clinical decision making, with the goal of ultimately enhancing patient care [45]. The continued application of automated systems that use SDOH data to prompt action (e.g., clinical decision support tools, EMR pop-up reminders for services) is accelerating efforts to engage in “social prescribing” by helping providers connect families with resources within and beyond the health system (Table 1). Continual enhancement of the use of resources including community-based support groups, employment agencies, and advocacy organizations is essential. Previous studies have shown that addressing these social challenges and then further referring families to support resources builds upon individuals’ strength and resilience [44].
Table 1
Activities in support of best practice in addressing social determinants of health through social prescriptions among individuals living with spina bifida
| Activity | Resource(s) |
| Refer families to local resources by zip code. | www.findhelp.org |
| Refer families to local Family-to-Family Health Information Centers (F2Fs), federally funded centers that support families of children with complex needs. | www.familyvoices.org/lfpp/f2fs |
| Refer families to Family Voices, a national organization that provides support to families of children with medical complexity to improve health care services and policies for children. | www.familyvoices.org |
| Utilize the American Academy of Pediatrics’ Social Determinants of Health Screening Resources hub for information and tools on screening, referral, and follow-up for social determinants of health. | www.aap.org/en/patient-care/screening-technical-assistance-and-resource-center/screening-resource-library/social-determinants-of-health |
| Utilize the PRAPARE Implementation and Action Toolkit to guide implementation, data collection, and responses to social determinants of health. | www.prapare.org/prapare-toolkit |
| Connect with the Root Cause Coalition, a national network of organizations resolved to reverse and end the systemic root causes of health inequities through cross-sector partnerships. | www.rootcausecoalition.org |
| Connect with Health Leads, an innovation hub that works both locally and nationally to build partnerships with health systems, to integrate programs that connect people to essential resources such as food, heat, and housing. | www.healthleadsusa.org |
| Forge a partnership with the Catalyst Center, a national resource hub that promotes universal, continuous, and affordable coverage for all children with medical complexity. | www.ciswh.org/project/the-catalyst-center |
| Obtain quality improvement training and resources on meaningful use of electronic medical records (e.g., Institute for Healthcare Improvement). | www.ihi.org www.ama-assn.org |
| Consider health system investment in Unite Us, cross-sector collaboration software that integrates into existing workflows, screens patients for social needs, and connects patients to community resources. | www.uniteus.com |
4.2Practice level
A growing body of literature suggest that precursors to poor outcomes may be best conceptualized through a “three-hit” model for a significant segment of the SB population [15]. Whereas the first two “hits” are experienced prenatally (i.e., neural tube lesion and its environmental exposure to amniotic fluid), the third “hit” may involve combinations of additional genetic and/or nongenetic exposures, such as unfavorable SDOH. Thus, at the practice level, care providers can offer culturally sensitive care strategies. These strategies have included providing high quality interpreter services, providing families with parking and/or transportation coverage for appointments, extending clinics through telemedicine appointments, and locating primary care clinics close to where patients reside [30]. The creation of a family advisory council helped to ensure that care is accessible and responsive to the families’ needs [44, 46]. In cases of hard-to-reach families, approaches such as patient tracking and individual SB case managers have also been effective to mitigate the negative impact of the “third hit” [44].
4.3Community level
At the community level, care providers have begun to expand their activities from the clinic and work upstream by engaging in public health advocacy and policy work. Advocacy is accomplished by establishing multi-stakeholder, community-wide partnerships with local schools, non-profits, and/or faith-based organizations. Working alongside those in public health who are already engaged in SDOH work has helped to catalyze these efforts [44]. Care providers can also use SDOH data collected in the clinical setting as a starting point towards advocacy. Not only can care providers create organizations to support social causes of concern, but also the health system and family advisory councils themselves can be understood as part of the solution in their work [44, 46]. To date, community engagement has served as a tool in which care providers can bring about change and community-level shifts. It is important to track deeply rooted challenges and to use self-reflexivity about one’s own biases to increase overall health [44]. Thus far, from a unique standing in the community, awareness has been raised about the adverse impacts of SDOH on wellbeing, encouraging broader policy action in partnership with the Spina Bifida Association that strives for high quality and equitable health care nationally.
4.4Safe handoffs and social prescribing for community resources
In this practice, a preclinic safety huddle meeting is conducted as part of the quality model for continuous improvement. The safety huddle discussion centers around safe handoff practices and previously collected clinical and SDOH-screening data [47, 48]. All patients coming to clinic that day are discussed, SDOH-related needs are identified, and a care plan is implemented ahead of clinic. In this way, practical steps are taken to buttress safe handoffs across the multidisciplinary team and to address SDOH challenges.
Caring for individuals with dignity, respect, and an open mind can help to establish a relationship built on trust. This foundation is critical for patients to feel comfortable disclosing sensitive social challenges, with the overarching goal of finding solutions through shared decision-making [44]. Addressing SDOH in clinic with an approach that is rooted in structural humility has been key. It is important that providers are aware of the power hierarchies that exist in medicine to ensure that families feel comfortable in expressing their needs [49]. Collaborating alongside communities is foundational to social medicine [50]. Lastly, knowing about local referral assets in the community that address various SDOH, including immigration or asylum-related resources, can help immensely in supporting displaced populations. Social prescribing through QI methods has been shown to bring about much success since it involves connecting immigrant families with resources such as employment agencies and local women’s groups and resources [51, 52]. This approach extends beyond a patient’s biomedical needs, with the goal of improving their overall wellbeing and quality of life [44].
4.5Limitations
This report should be viewed within the context of the following limitations. The designed workflow leveraged significantly the social work and nurse team available to the SB program; however, institutions where social work is not a part of the multidisciplinary team may be limited in their ability to fully implement all components of the designed workflow. The project was conducted after the COVID-19 pandemic when technology had been already optimized to utilize telemedicine visits to provide follow-up. Therefore, institutions where telemedicine for care coordination or follow-up has not been initiated would have a difficult time employing this workflow completely. Another significant limitation is that no statistical analysis of related correlations is presented currently, as this brief report is meant to be a qualitative description of the QI project. Despite obtaining informal feedback during the implementation period, a formal survey from the providers was not collected. Given the above limitations, future investigational directions would include pursuing a more systematically randomized approach to assigning social work care coordination to measure the degree of improvement in care provision and the feasibility for upscaling social prescribing in other settings.
5Conclusion
A mounting body of literature suggests that precursors to poor outcomes may be best conceptualized through a “three-hit” model for a significant segment of the SB population. While these SDOH can be difficult to address in current workflow and medical documentation systems, they represent areas of medicine where improvements are impactful. Utilizing QI methodology, a pathway for EMR customization was established to identify and help address SDOH through social prescriptions among a group of diverse individuals with SB. Customizing the EMR to support an efficient workflow to address SDOH is feasible and can support the provision of quality and equitable health care for immigrant and medically complex populations at home and possibly abroad.
Acknowledgments
Funded in part by the National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention (1U01DD001265.01). The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. We are grateful to Drs. Kathryn Ostermaier and Geeta Singhal for their support of our Spina Bifida Program.
Conflict of interest
The authors have no conflicts of interest to report.
Ethical considerations
Institutional Review Board approval was sought and received for relevant portions of the quality improvement project. Informed consent was obtained for relevant portions of the project as well.
References
[1] | Social Determinants of Health. Healthy People 2030. Washington, DC: U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion; 2023 [cited 27 June 2023]. Available from: https://health.gov/healthypeople/priority-areas/social-determinants-health |
[2] | Castillo J , Ostermaier KK , Fremion E , et al. Urologic self-management through intermittent self-catheterization among individuals with spina bifida: A journey to self-efficacy and autonomy. J Pediatr Rehabil Med. (2017) ;10: (3-4):219–26. doi: 10.3233/PRM-170447 |
[3] | Routh JC , Joseph DB , Liu T , et al. Variation in surgical management of neurogenic bowel among centers participating in National Spina Bifida Patient Registry. J Pediatr Rehabil Med. (2017) ;10: (3-4):303–12. doi: 10.3233/PRM-170460 |
[4] | Advancing Health Equity: A guide to language, narrative and concepts. American Medical Association [cited 27 June 2023]. Available from: https://www.ama-assn.org/about/ama-center-health-equity/advancing-health-equity-guide-language-narrative-and-concepts-0 |
[5] | Kuo AA , Thomas PA , Chilton LA , Mascola L . Pediatricians and PublicHealth: Optimizing the Health and Well-Beingof the Nation’s Children. Pediatrics. (2018) ;141: (2):e20173848.. doi: 10.1542/peds.2017-3848 |
[6] | Anderson L , Hemez P . Over a Quarter of Children Lived With At Least One Foreign-Born Parent. United States Census Bureau; 2022 [updated 13 April 2022; cited 1 November 2023]. Available from: https://www.census.gov/library/stories/2022/02/over-quarter-of-children-lived-with-at-least-one-foreign-born-parent.html#::text=While%20the%20majority%20of%20children,new%20U.S.%20Census%20Bureau%20report |
[7] | Migration and migrant population statistics. Eurostat; 2023 [updated 7 August 2023; cited 1 November 2023]. Available from: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Migration_and_migrant_popula-vtion_statistics |
[8] | Refugee and migrant children in Europe. UNICEF [cited 1 November 2023]. Available from: https://www.unicef.org/eca/emergencies/refugee-and-migrant-children-europe |
[9] | Taylor KW , Athens JK , Booske BC , O’Connor CE , Jones NR , Remington PL . Wisconsin County Health Rankings. Madison, WI: University of Wisconsin School of Medicine and Public Health; 2008. |
[10] | Braveman PA , Cubbin C , Egerter S , et al. Socioeconomic status in health research: One size does not fit all. JAMA. (2005) ;294: (22):2879–88. doi: 10.1001/jama.294.22.2879 |
[11] | LaVeist TA . Disentangling race and socioeconomic status: A key to understanding health inequalities. J Urban Health. (2005) ;82: (2 Suppl 3):iii26–iii34. doi: 10.1093/jurban/jti061 |
[12] | Adler NE , Stewart J . Health disparities across the lifespan: Meaning, methods, and mechanisms. Ann NY Acad Sci. (2010) ;1186: :5–23. doi: 10.1111/j.1749-6632.2009.05337.x |
[13] | Ridosh MM , Adams W , Magaña F , Sawin KJ , Holmbeck GN . Trajectories of self-management and independence in youth with spinabifida: Demographic predictors of growth. Child Care Health Dev. (2023) ;49: (3):508–17. doi: 10.1111/cch.13065 |
[14] | Foy AB , Sawin KJ , Derflinger T , et al. Sociodemographic disparities in fetal surgery for myelomeningocele: a single-center retrospective review. J Neurosurg Pediatr. (2021) ;1–5. doi: 10.3171/2021.7.PEDS20836 |
[15] | Castillo J , Lupo PJ , Tu DD , Agopian AJ , Castillo H . The National Spina Bifida Patient Registry: A decade’s journey. Birth Defects Res. (2019) ;111: (14):947–57. doi: 10.1002/bdr2.1407 |
[16] | Botto LD , Moore CA , Khoury MJ , Erickson JD . Neural-tube defects. N Engl J Med. (1999) ;341: (20):1509–19. doi: 10.1056/NEJM199911113412006 |
[17] | Zaganjor I , Sekkarie A , Tsang BL , et al. Describing the prevalence of neural tube defects worldwide: A systematic literature review. PLoS ONE. (2016) ;11: (4):e0151586. doi: 10.1371/journal.pone.0151586 |
[18] | Blencowe H , Kancherla V , Moorthie S , Darlison MW , Modell B . Estimates of global and regional prevalence of neural tube defects for A systematic analysis. Ann NY Acad Sci. (2018) ;1414: (1):31–46. doi: 10.1111/nyas.13548 |
[19] | Murray CJL , Lopez AD . The global burden of disease: A comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Geneva (Switzerland): World Health Organization, World Bank & Harvard School of Public Health; 1996. |
[20] | Mitchell LE . Epidemiology of neural tube defects. Am J Med Genet C Semin Med Genet. (2005) ;135C: (1):88–94. doi: 10.1002/ajmg.c.30057 |
[21] | Castillo J , Gandy K , Bradko V , Castillo H . Language and Latino immigrants living with spina bifida: Social determinants of health – the missing dimension in quality of life research. J Pediatr Rehabil Med. (2019) ;12: (4):345–59. doi: 10.3233/PRM-180586 |
[22] | Williams J , Mai CT , Mulinare J , et al. Updated estimates of neural tube defects prevented by mandatory folic acid fortification – United States, 1995–2011. MMWR Morb Mortal Wkly Rep. (2015) ;64: (1):1–5. |
[23] | Castillo J , Castillo H . Global health and chronic non-communicable conditions: Spina bifida care across a worldwide community. J Pediatr Rehabil Med. (2017) ;10: (3-4):167–8. doi: 10.3233/PRM-170471 |
[24] | Rosenthal J , Casas J , Taren D , Alverson CJ , Flores A , Frias J . Neural tube defects in Latin America and the impact of fortification: A literature review. Public Health Nutr. (2014) ;17: (3):537–50. doi: 10.1017/S1368980013000256 |
[25] | Schechter MS , Liu T , Soe M , Swanson M , Ward E , Thibadeau J . Sociodemographic attributes and spina bifida outcomes. Pediatrics. (2015) ;135: (4):e957–64. doi: 10.1542/peds.2014-2576 |
[26] | Liu T , Ouyang L , Thibadeau J , et al. Longitudinal study of bladder continence in patients with spina bifida in the National Spina Bifida Patient Registry. J Urol. (2018) ;199: (3):837–43. doi: 10.1016/j.juro.2017.11.048 |
[27] | Chowanadisai M , de la Rosa Perez DL , Weitzenkamp DA , Wilcox DT , Clayton GH , Wilson PE . The role of ethnicity and culture on functional status in children with spina bifida. J Pediatr Rehabil Med. (2013) ;6: (4):205–13. doi: 10.3233/PRM-140259 |
[28] | Bush RA , Kuelbs C , Ryu J , Jiang W , Chiang G . Structured data entry in the electronic medical record: Perspectives of pediatric specialty physicians and surgeons. J Med Syst. (2017) ;41: (5):75. doi: 10.1007/s10916-017-0716-5 |
[29] | Gold R , Cottrell E , Bunce A , Middendorf M , et al. Developing electronic health record (EHR) strategies related to health center patients’ social determinants of health. J Am Board Fam Med. (2017) ;30: (4):428–47. doi: 10.3122/jabfm.2017.04.170046 |
[30] | Castillo J , Fremion E , Morrison-Jacobus M , et al. Think globally, act locally: Quality improvement as a catalyst for COVID-19 related care during the transitional years. J Pediatr Rehabil Med. (2021) ;14: (4):691–7. doi: 10.3233/PRM-210119 |
[31] | Crowl A , Sharma A , Sorge L , Sorensen T . Accelerating quality improvement within your organization: Applying the Model for Improvement. J Am Pharm Assoc (2003). (2015) ;55: (4):e364–74; quiz e375-6. doi: 10.1331/JAPhA.2015.15533 |
[32] | Adams D . Quality improvement; part introduction and overview. BJA Educ. (2018) ;18: (3):89–94. doi: 10.1016/j.bjae.2017.12.002 |
[33] | Chisolm DJ . Quality in Context: The Role of Social Determinants of Health in Pediatric Quality Improvement. Pediatr Qual Saf. (2017) ;2: (5):e036. doi: 10.1097/pq9.0000000000000036 |
[34] | Friedman S , Caddle S , Motelow JE , Meyer D , Lane M . Improving Screening for Social Determinants of Health in a Pediatric Resident Clinic: A Quality Improvement Initiative. Pediatr Qual Saf. (2021) ;6: (4):e419. doi: 10.1097/pq9.0000000000000419 |
[35] | Garg A , Homer CJ , Dworkin PH . Addressing social determinants of health: Challenges and opportunities in a value-based model. Pediatrics. (2019) ;143: (4):e20182355. doi: 10.1542/peds.2018-2355 |
[36] | Honsberger K , Tanga AM , Eichner H . Identification and screening of social determinants of health among children with special health care needs in Medicaid. National Academy for State Health Policy; 2020. Available from: https://downloads.aap.org/MedHome/pdf/SHD%20Fact%20Sheet%20FINAL.pdf |
[37] | Ghosheh GO , Thwaites CL , Zhu T . Synthesizing electronic health records for predictive models in low-middle-income countries (LMICs). Biomedicines. (2023) ;11: (6):1749. doi: 10.3390/biomedicines11061749 |
[38] | Hertzum M , Ellingsen G . The implementation of an electronic health record: Comparing preparations for Epic in Norway with experiences from the UK and Denmark. Int J Med Inform. (2019) ;129: :312–7. doi: 10.1016/j.ijmedinf.2019.06.026 |
[39] | Hertzum M , Ellingsen G , Cajander Å . Implementing Large-ScaleElectronic Health Records: Experiences from implementations of Epicin Denmark and Finland. Int J Med Inform. (2022) ;167: :104868. doi:10.1016/j.ijmedinf.2022.104868 |
[40] | Social determinants of health in rural communities toolkit. Rural Health Information Hub; 2020 [cited 27 June 2023]. Available from: https://www.ruralhealthinfo.org/toolkits/sdoh |
[41] | Healthy People 2020: An Opportunity to Address the Societal Determinants of Health in the United States. Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020; 2010. Available from: https://health.gov/sites/default/files/2021-11/Committee%27s%20Report%20on%20Healthy%20People%202020-%20An%20Opportunity%20to%20Address%20Societal%20Determinants%20of%20Health.pdf |
[42] | Marmot M , Allen J , Goldblatt P , Boyce T , McNeish D , Grady M . Fair society, healthy lives. The Marmot Review; 2010. Available from: https://www.instituteofhealthequity.org/resources-reports/fair-society-healthy-lives-the-marmot-review |
[43] | Walker RJ , Williams JS , Egede LE . Influence of race, ethnicity and social determinants of health on diabetes outcomes. Am J Med Sci. (2016) ;351: (4):366–73. doi: 10.1016/j.amjms.2016.01.008 |
[44] | Andermann A . Taking action on the social determinants of health in clinical practice: A framework for health professionals. CMAJ. (2016) ;188: (17-18):E474–83. doi: 10.1503/cmaj.160177 |
[45] | DeVoe JE , Bazemore AW , Cottrell EK , et al. Perspectives in primary care: A conceptual framework and path for integrating social determinants of health into primary care practice. Ann Fam Med. (2016) ;14: (2):104–8. doi: 10.1370/afm.1903 |
[46] | Struwe S , Thibadeau J , Kelly MS , Widener-Burrows D . Establishing the first community-centered Spina Bifida research agenda. J Pediatr Urol. (2022) ;18: (6):800.e1–800.e7. doi: 10.1016/j.jpurol.2022.06.014 |
[47] | Patton LJ , Tidwell JD , Falder-Saeed KL , Young VB , Lewis BD , Binder JF . Ensuring Safe Transfer of Pediatric Patients: A Quality Improvement Project to Standardize Handoff Communication. J Pediatr Nurs. (2017) ;34: :44–52. doi: 10.1016/j.pedn.2017.01.004 |
[48] | Siefferman JW , Lin E , Fine JS . Patient safety at handoff in rehabilitation medicine. Phys Med Rehabil Clin N Am. (2012) ;23: (2):241–57. doi: 10.1016/j.pmr.2012.02.003 |
[49] | Structural competency handouts. Berkeley Rad Med Critical Social Medicine Collective Structural Competency Working Group; 2016 [cited 27 June 2023]. Available from: https://www.feinberg.northwestern.edu/sites/cpci/docs/Structural-Competency-Handouts-Berkeley-Rad-Med-Critical-Social-Medicine..pdf |
[50] | Stonington SD , Holmes SM , Hansen H , et al. Case studies in social medicine - attending to structural forces in clinical practice. N Engl J Med. (2018) ;379: (20):1958–61. doi: 10.1056/NEJMms1814262 |
[51] | Ebrahimoghli R , Pezeshki MZ , Farajzadeh P , Arab-Zozani M , Mehrtak M , Alizadeh M . Factors influencing social prescribing initiatives: a systematic review of qualitative evidence. Perspect Public Health. (2023) : 17579139231184809. doi: 10.1177/17579139231184809 |
[52] | Robidoux H , Williams A , Cormack C , Johnson E . Maternal Postpartum Depression Screening and Referral in a Latinx Immigrant Population: A Quality Improvement Study. J Immigr Minor Health. (2023) ;25: (5):1050–8. doi: 10.1007/s10903-023-01503-3 |



