Outcomes following intensive day rehabilitation for young people in Western Australia
Abstract
OBJECTIVE:
Intensive rehabilitation aims to improve and maintain functioning in young people who experience disability due to illness or injury. Day rehabilitation may have advantages for families and healthcare systems over inpatient models of rehabilitation.
METHODS:
This study evaluated the goals and outcomes of a cohort of young people in Western Australia who attended a specialist intensive day rehabilitation programme (“iRehab”) at Perth Children’s Hospital. Analysis of the iRehab service database was performed. Rehabilitation goals and outcomes were recorded as per the Canadian Occupational Performance Measure (COPM), Children’s Functional Independence Measure (WeeFIM), and Goal Attainment Scale (GAS).
RESULTS:
There were 586 iRehab admissions between August 11, 2011, and December 31, 2018. Admissions were divided by diagnosis: Cerebral Palsy (228, 38.5%), Acquired Brain Injury (125, 21.3%), Spinal Cord Disorders (91, 15.5%), and Other (141, 24.2%). Mean COPM Performance increased by 2.78 points from admission to discharge (95% CI 2.58 to 2.98, p < 0.001). Mean COPM Satisfaction was 3.29 points higher at discharge than admission (95% CI 3.07 to 3.51, p < 0.001). Mean total WeeFIM score improved by 6.51 points between admission and discharge (95% CI 5.56 to 7.45, p < 0.001), and by 3.33 additional points by six months post discharge (95% CI 2.14 to 4.53, p < 0.001). Mean GAS T-scores increased by 27.85 (95% CI 26.73 to 28.97, p < 0.001) from admission to discharge, and by 29.64 (95% CI 28.26 to 31.02, p < 0.001) from admission to six months post discharge, representing improvement consistent with team expectations.
CONCLUSION:
This study describes a model by which intensive rehabilitation can be delivered in a day rehabilitation setting. A diverse population of young people who experienced disability achieved significant improvements in occupational performance, independence, and goal attainment after accessing intensive day rehabilitation. Improvements were measured in all diagnostic subgroups and were maintained six months after discharge.
1Background
Paediatric rehabilitation is a child-centred interdisciplinary process which aims to improve and maintain functioning in young people who experience disability due to illness or injury [1, 2]. Rehabilitation is one of the five essential pillars of modern healthcare alongside health promotion, illness prevention, treatment, and palliation [3]. It is based on a biopsychosocial approach to illness and health and tailors the process to the individual, mindful of the interplay between personal factors, environmental factors, and body structure and function as espoused in the World Health Organization’s (WHO) International Classification of Functioning, Disability and Health for Children and Youth (ICF-CY) model [1, 4–7]. A rehabilitation programme’s success may be assessed by measuring the achievement of realistic and meaningful patient goals and functional improvements [1, 2].
Rehabilitation is known to improve long-term outcomes for patients and reduce healthcare and homecare costs [1, 6]; current evidence for cost-effectiveness is stronger for adults than for children [6]. Specific rehabilitation approaches are heterogeneous, reflecting the large number of potential approaches to rehabilitation internationally which can be influenced by differences in staffing, training, resources, infrastructure, and population needs [4, 5]. This is a barrier to clarity in evidence, and there is scant evidence demonstrating the superiority of one model of rehabilitation over another [4–6, 8]. Increased rehabilitation intensity has been associated with improved outcomes [4, 9]. A reflective approach on individual specialist rehabilitation unit practices is important in the effort to improve and standardize rehabilitation for children and enable benchmarking, research, and knowledge translation [10].
Improved survival after moderate and severe neurological injuries has not been consistently met with an increase in provision of rehabilitation services [10–12]. Access to early intensive rehabilitation has been identified by service users as a high priority in Western Australia, where this study was conducted [13]. In this context, it is increasingly important to contribute to the evidence for different models of intensive rehabilitation for children and young people and document the outcomes of those who access them [10, 14, 15].
A recent global WHO study has refuted the commonly held position that rehabilitation is a niche service model only needed by small numbers of people [16]. Making services more accessible is a key step in increasing rehabilitation provision worldwide [16, 17]. Models of care that enable earlier discharge from hospital while maintaining rehabilitation input have the potential to be effective, to reduce inpatient bed costs, and to improve access to rehabilitation.
1.1Intensive rehabilitation in Western Australia
Kids Rehab WA is based at Perth Children’s Hospital (PCH), the sole tertiary paediatric hospital for Western Australia (population 2.7 million), and provides comprehensive inpatient, outpatient, and intensive day rehabilitation services to young people who experience disability. Access is not restricted by diagnosis and includes young people with cerebral palsy (CP), acquired brain injury (ABI), spina bifida, spinal cord injury, and other conditions which lead to functional impairments; these include neurological, neuromuscular, musculoskeletal, and metabolic conditions, amongst others (see Supplemental Information 1).
The Intensive Rehabilitation Service (iRehab) is a specialist multidisciplinary day rehabilitation programme for children and adolescents based on the ICF-CY model [7]. It was established in 2011. Patients receive early and intensive rehabilitation beyond what is available in the community but without inpatient admission. Admission to iRehab may directly follow an inpatient admission at PCH (e.g., due to acquired brain injury or following orthopaedic surgery for children with CP) or outpatient referral in the context of loss of function or to access specific therapy tools, such as robotics, hydrotherapy, or augmented communication. Any young person with functional limitations who could benefit from a period of intensive rehabilitation is deemed eligible for referral to iRehab. Patients attend for multiple sessions per day (typically 2–4 sessions lasting one hour each) for periods of 2–8 weeks, with involvement from at least two therapy disciplines. Medical and therapeutic input is directed at the pursuit of identified child and family goals and priorities based on standardized assessment and measurement practices (see Methods). Due to the variety of different diagnoses addressed by the iRehab programme, the content of rehabilitation received by each child varies widely and is tailored to the individual. Accommodation near PCH is provided for families travelling long distances, which is common given the large geographical area of Western Australia.
The iRehab team includes paediatric rehabilitation medicine specialists, a clinical coordinator, physiotherapists, occupational therapists, speech pathologists, clinical nurse specialists, allied health assistants, clinical psychologists, neuropsychologists, teachers, and social workers. Team members have annual training for fidelity of interventions and assessments as well as discipline-specific competencies. A standardized admission procedure including outcome measures and formalized goal setting is used for all patients (see Materials and Methods).
There is little published literature describing the outcomes of patients attending services comparable to iRehab. Worldwide, it is acknowledged that paediatric rehabilitation services are less developed than those for adults [9]. Evidence is growing about the significant incidence of disability in children following critical illness and injury, as well as increasing survival rates [10, 12, 14–19]. In this context, reporting rehabilitation outcomes for children who experience disability is a matter of public health importance to help guide future service development [10, 14–17]. With reference to this context, this study aimed to examine the characteristics of the young people accessing iRehab with regard to age, gender, primary diagnosis, and comorbidities. It also aimed to evaluate their rehabilitation goals and outcomes as defined by the Children’s Functional Independence Measure (WeeFIM), Canadian Occupational Performance Measure (COPM), and Goal Attainment Scale (GAS).
2Material and methods
This study was conducted by review of the iRehab service database, comprised of data routinely collected prospectively as part of standard procedure during admissions (see below). Admissions to iRehab for multidisciplinary input between August 11, 2011, and December 31, 2018, were considered for inclusion.
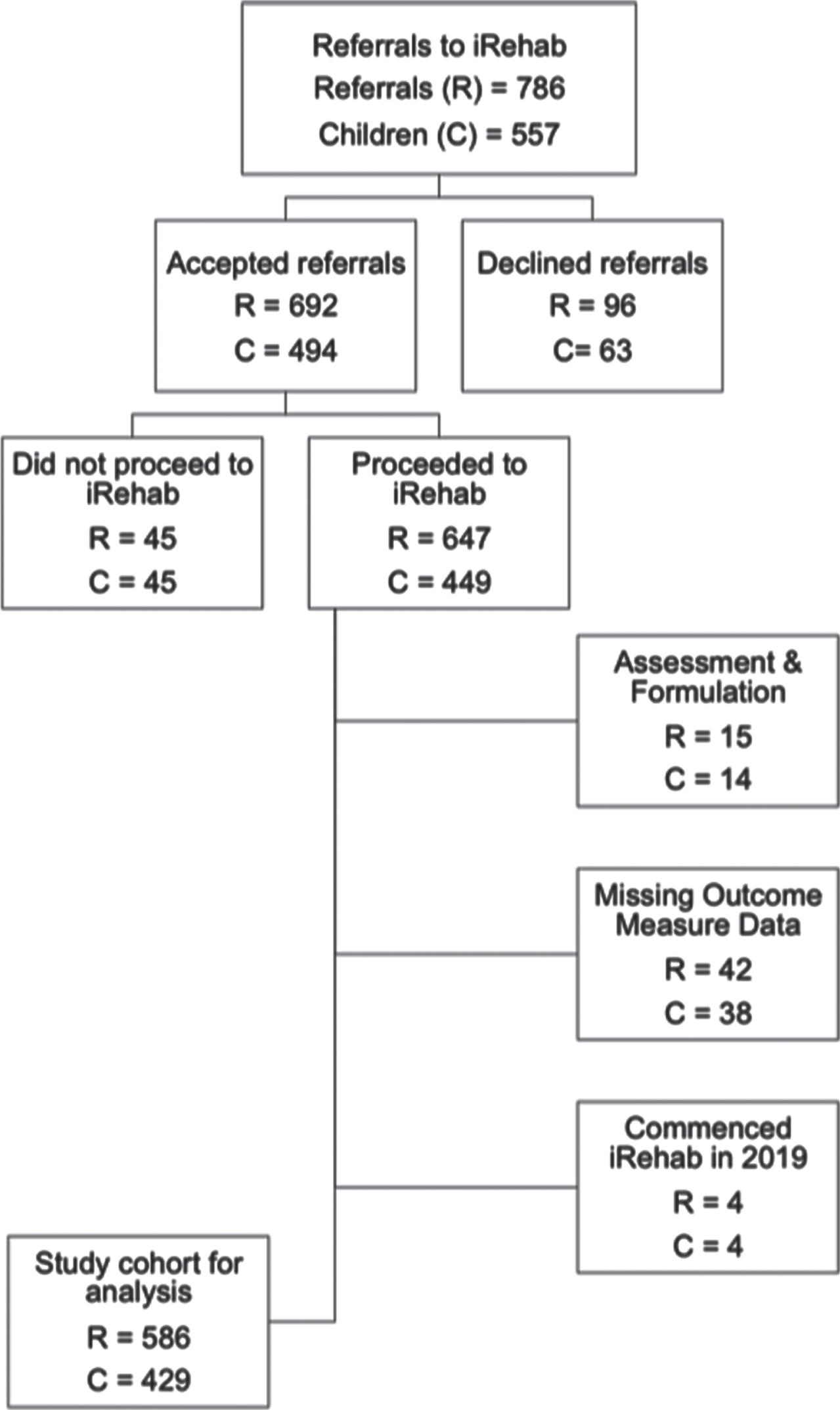
Patients admitted for “Assessment & Formulation” were excluded: these were brief admissions for the purpose of conducting a series of assessments (rather than interventions) with the aim of understanding an individual patient’s reported difficulties; outcome measures were not included in the standardized process for these admissions. Patients with incomplete data or ongoing active admissions at the time of data retrieval were also excluded (Fig. 1).
Fig. 1
Study flow.
The use of anonymised clinical data for research was approved by the institutional Clinical Governance Unit and registered as a Quality Activity within the Governance Evidence Knowledge Outcomes framework.
Each admission was allocated to one of four diagnostic subgroups (CP, ABI, Spinal, or Other) based on primary diagnosis.
All iRehab admissions involved the use of a suite of three measures to assess functional independence, performance, and goal attainment.
WeeFIM [20] measures a young person’s functional independence and need for assistance from helpers and/or devices. A trained tester scores them on a scale of 1 (fully dependent) to 7 (independent) across 18 skills in the domains of self-care, functional mobility, and cognition. WeeFIM has strong validity, inter-rater reliability and sensitivity to change [20].
COPM [21] identifies occupational performance issues of importance to a young person and their family. A semi-structured interview is performed to assist a child and their family to report their level of current Performance (1 = cannot do it at all, 10 = can do it perfectly) and Satisfaction (1 = very unsatisfied, 10 = completely satisfied) for each domain discussed. Considering COPM scores for multiple domains allows rehabilitation goals for a specific patient programme to be identified.
GAS [22, 23] is a method used to design personalized evaluation scales to quantify progress towards personal goals. It measures the degree to which goals are achieved compared to team expectations. Personalized graded scales of potential goal attainment from “–2” (indicating “current level of functioning” at the time of goal setting) to “+2” (indicating “significantly more progress than expected”) are used to calculate a “T-score” for every goal; scores of 40–60 are within the range of improvement consistent with team expectations [23].
These three tools are administered in a standardized fashion for all admissions to iRehab. COPM is administered to identify occupational performance issues and rate Performance and Satisfaction in these domains. WeeFIM is used to establish baseline functional independence and to detect changes in functional independence over time. GAS is then used to specify precise, measurable goals related to occupational performance issues and areas of dependence, the attainment of which is evaluated at the conclusion of the admission alongside reassessment of COPM Performance and Satisfaction and WeeFIM scores. All children attending iRehab for multidisciplinary input have these three tools administered at admission, discharge, and at six months post discharge.
Results of WeeFIM, COPM, and GAS at admission, discharge, and six months post discharge were analysed to detect changes in these scores between iRehab admission and discharge, and between discharge and six months post discharge. Mean differences between COPM scores at admission, discharge (reference level), and six months post discharge were modelled with linear mixed effects regression [24].
Effect estimates for WeeFIM and GAS were modelled with generalized additive mixed models [25] as error residuals violated the assumptions of linear regression. To account for repeat patient admission into iRehab, all mixed models were constructed with a nested random effect structure of unique admission identifier and date referred to the programme; regression models were not adjusted for other variables.
Analyses were performed to examine the potential confounding variable of patient age and length of iRehab admission. The mean difference between admission and discharge (i.e., monitoring the immediate change in score resulting from iRehab), and between discharge and six-month follow-up (i.e., monitoring sustained improvement following iRehab) were reflected in the regression analysis; while changes between admission and six-month follow up can be inferred, a direct statistical comparison could not be made. Data wrangling, figure creation, and modelling were completed in the R programming language [26].
3Results
There were 586 multidisciplinary iRehab admissions included in the analysis (315 male, 53.8%). Study population characteristics are shown in Table 1. The only observed gender imbalance was in the ABI group, largely due to a male:female ratio of approximately 2 : 1 for traumatic brain injury as is commonly reported [27–29]. The Other group accounted for more admissions than the Spinal or ABI groups.
Table 1
Demographics
| n (%) | |
| Admissions | 586 |
| Age ranges (at admission to iRehab) | |
| Median age | 9.1 years |
| Age range | 0.7–17.7 years |
| 0–4 years | 99 (16.9) |
| 5–8 years | 181 (30.9) |
| 9–12 years | 150 (25.6) |
| 13–16 years | 142 (24.2) |
| > 17 years | 14 (2.4) |
| Indigenous | 31 (5.3) |
| Cerebral Palsy | 228 (38.9) |
| Bilateral lower limb (diplegia) | 111 (48.7) |
| Unilateral (hemiplegia) | 29 (12.7) |
| Four limb (quadriplegia) | 68 (29.8) |
| n/a | 20 (8.7) |
| Acquired Brain Injury | 125 (21.3%) |
| Trauma | 35 (28) |
| Tumour | 32 (25.6) |
| Stroke | 19 (15.2) |
| Infection | 9 (7.2) |
| Inflammation | 6 (4.8) |
| Hypoxia/Ischaemia | 6 (4.8) |
| Epilepsy surgery | 3 (2.4) |
| n/a | 15 (12) |
| Spinal Cord Disorders | 91 (15.5) |
| Spinal Cord Injury | 45 (49.4) |
| Trauma | 14 (15.3) |
| Transverse myelitis | 12 (13.2) |
| Tumour | 8 (8.8) |
| Other | 11 (12.1) |
| Congenital | 46 (50.6) |
| Other | 141 (24.2) |
| Neurological | 57 (40.4) |
| Musculoskeletal | 30 (21.3) |
| Neuromuscular | 10 (7.1) |
| Deconditioning | 9 (6.4) |
| Metabolic | 7 (5) |
| Miscellaneous | 28 (19.9) |
Analysis of comorbidities revealed significant medical complexity (Supplemental Information 2). The most prevalent comorbidities were epilepsy (23% of admissions), intellectual disability (22.9%), visual impairment (18.4%), scoliosis (12.8%), and hearing loss (7.8%).
Seventy-one patients had more than one admission to iRehab, accounting for a total of 189 admissions (36.5% CP, 23.5% Other, 20% ABI, 20% Spinal). Thirty-one admissions (5.3%) were of indigenous patients, 23 of whom (74.1%) were male.
3.1Goals
Goals for iRehab admissions were set after the COPM was used to identify occupational performance issues, and categorized by domain (Fig. 2).
Fig. 2
Goals for iRehab by COPM domain. COPM: Canadian Occupational Performance Measure, ABI: acquired brain injury, PC: personal care, FM: functional mobility, CM: community management, S: socialisation, AR: active recreation, QR: quiet recreation, HM: household management, W: work, PSL: play/school leisure.
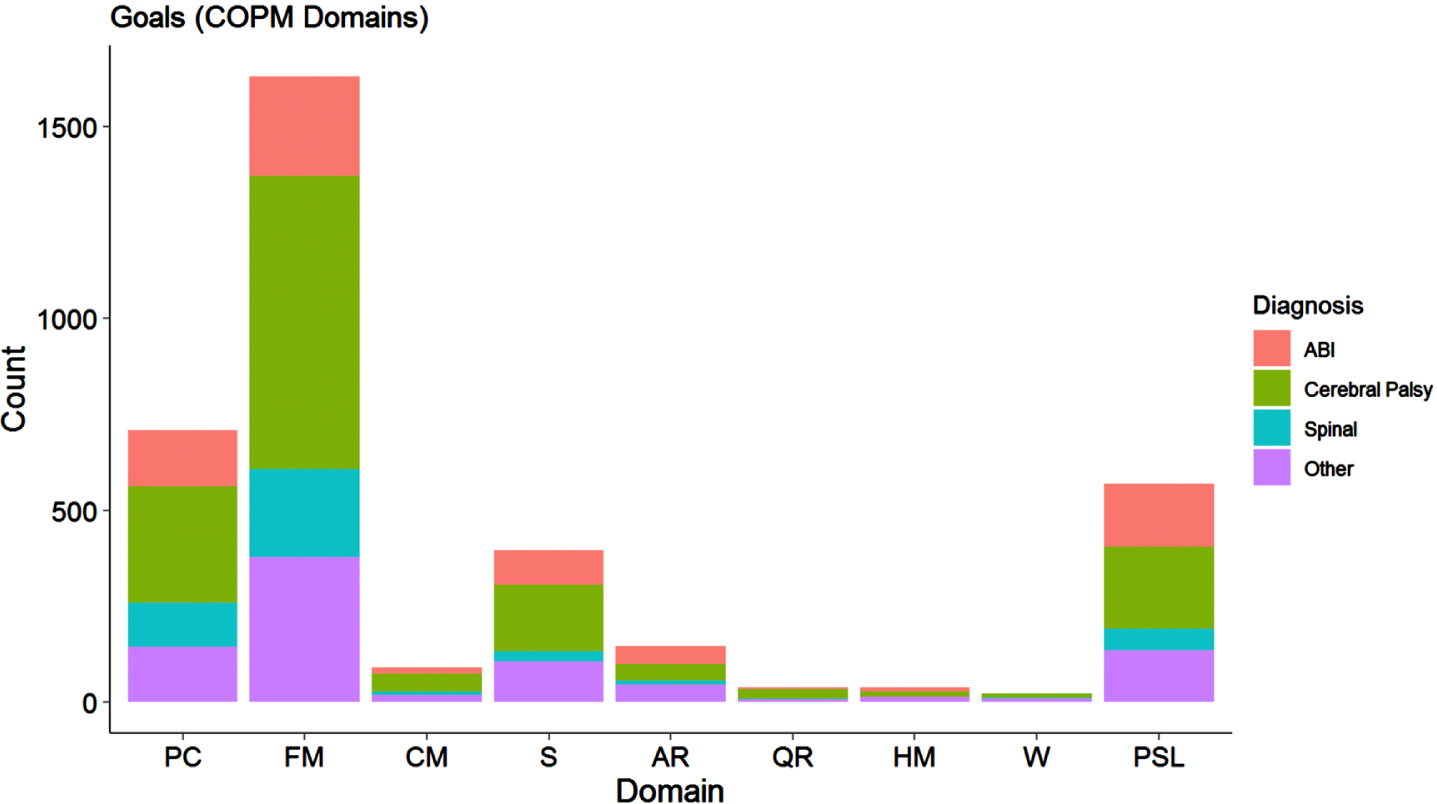
A total of 3,642 goals were set; Functional Mobility (1,630), Personal Care (709), Play/School Leisure (569), and Socialization (397) were the four most commonly identified domains, accounting for 90.7% of all goals identified. Functional mobility accounted for 44.7% of all goals and was the most frequently identified goal domain in all four groups, particularly in the CP and Spinal groups where it represented 48% and 51% of all goals, respectively.
3.2Outcomes
COPM Performance and Satisfaction scores for the whole group were analysed using linear mixed effects modelling and indicated statistically significant improvements from admission to discharge in Performance and Satisfaction scores (Table 2).
Table 2
Changes in Canadian Occupational Performance Measure scores at admission and six months post discharge, relative to discharge
| Performance Score | Satisfaction Score | |
| Discharge (intercept) | 6.01 (5.84, 6.19) | 6.64 (6.45, 6.84) |
| Admission | –2.78 (–2.98, –2.58) *** | –3.29 (–3.51, –3.07) *** |
| 6 months post discharge | 0.27 (0.01, 0.54) * | –0.12 (–0.41, 0.18) |
***p < 0.001; **p < 0.01; *p < 0.05.
Mean COPM Performance scores for the whole group increased by 2.78 points (95% CI 2.58 to 2.98, p < 0.001) from admission to discharge; mean COPM Satisfaction scores increased by 3.29 from admission to discharge (95% CI 3.07 to 3.51, p < 0.001). Performance and Satisfaction scores had similar profiles, and comparable improvements were seen in all four diagnostic subgroups (Fig. 3).
Fig. 3
COPM scores by diagnostic subgroup. Solid and dotted lines represent median and mean COPM values, respectively. COPM: Canadian Occupational Performance Measure, ABI: acquired brain injury.
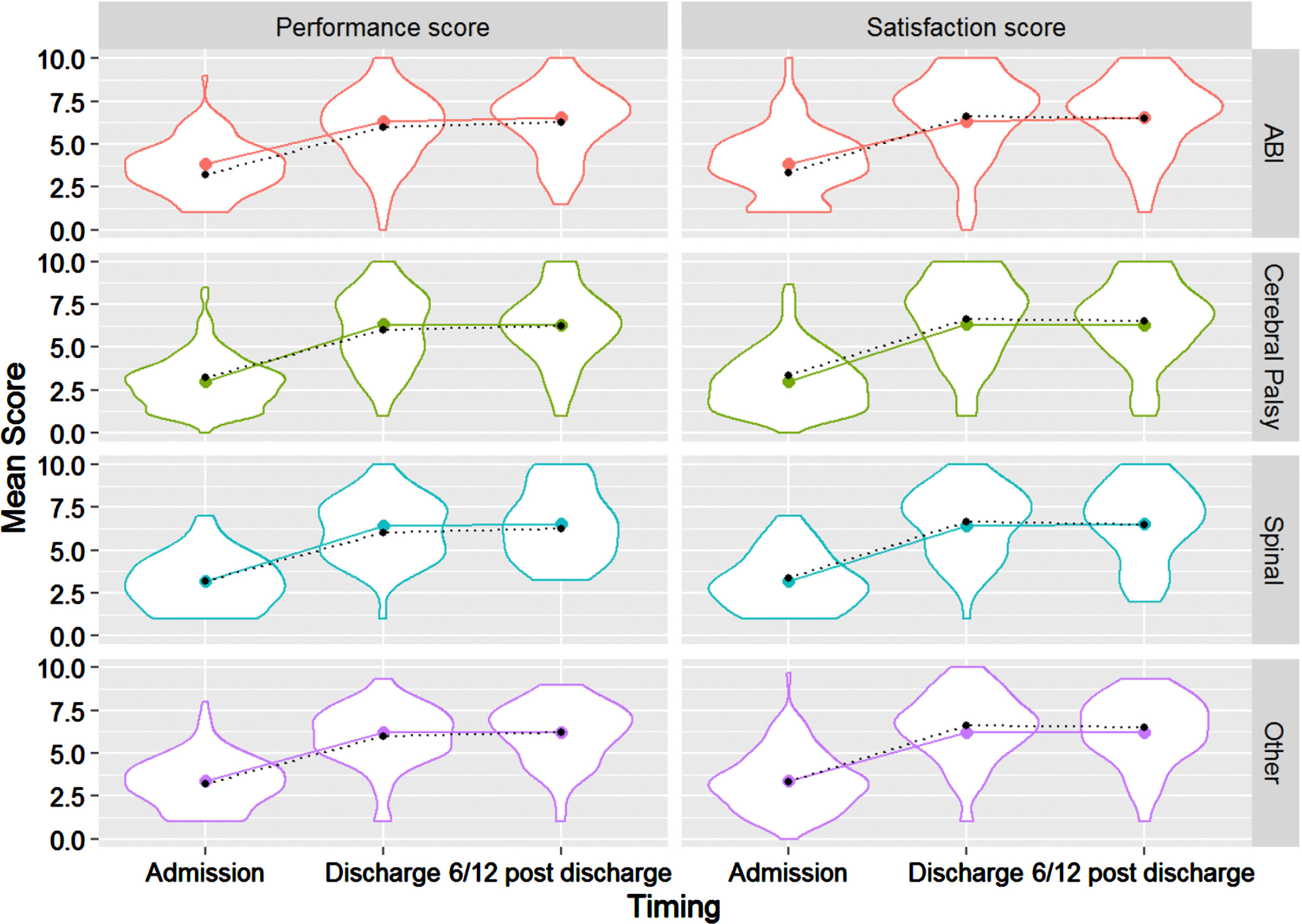
At six months post discharge, mean COPM Performance score was 0.27 points higher than at discharge (95% CI 0.01 to 0.54, p < 0.05); no statistically significant change in Satisfaction scores was measured. This indicated that improvements made during iRehab were maintained at six month follow-up; additional improvements after discharge appeared to be small and unlikely to be clinically significant.
The improvements measured between admission and discharge were also statistically significant for the individual COPM domains of Functional Mobility, Personal Care, Play/School Leisure, and Socialisation (p < 0.001 for all).
WeeFIM
WeeFIM scores for the whole study group are shown in Table 3. Scores at admission and six month follow-up were compared to scores at discharge from iRehab and showed significant and maintained improvements in all domains.
Table 3
Mean Children’s Functional Independence Measure (WeeFIM) scores: whole group. Effect estimates (95% confidence intervals) relative to WeeFIM score at discharge
| Self-care | Mobility | Cognitive | Total | |
| Discharge (Intercept) | 30.54 (28.97, 32.11) | 20.32 (19.36, 21.28) | 22.54 (21.58, 23.5) | 73.34 (70.14, 76.55) |
| Admission | –2.71 (–3.21, –2.21)*** | –2.89 (–3.37, –2.41)*** | –0.84 (–1.17, –0.51)*** | –6.51 (–7.45, –5.56)*** |
| 6 months post discharge | 1.60 (0.96, 2.23)*** | 1.37 (0.77, 1.98)*** | 0.34 (–0.07, 0.76) | 3.33 (2.14, 4.53)*** |
***p < 0.001; **p < 0.01; *p < 0.05.
Figure 4 shows changes in mean absolute WeeFIM scores at admission and six months post discharge compared to those at discharge (which are represented by 0.0). Horizontal bars represent 95% confidence intervals; those that do not include 0.0 suggest an observed change was statistically significant.
Fig. 4
Effect estimates and 95% confidence intervals of changes in mean Children’s Functional Independence Measure (WeeFIM) absolute score at admission and six months post discharge, compared to score at discharge.
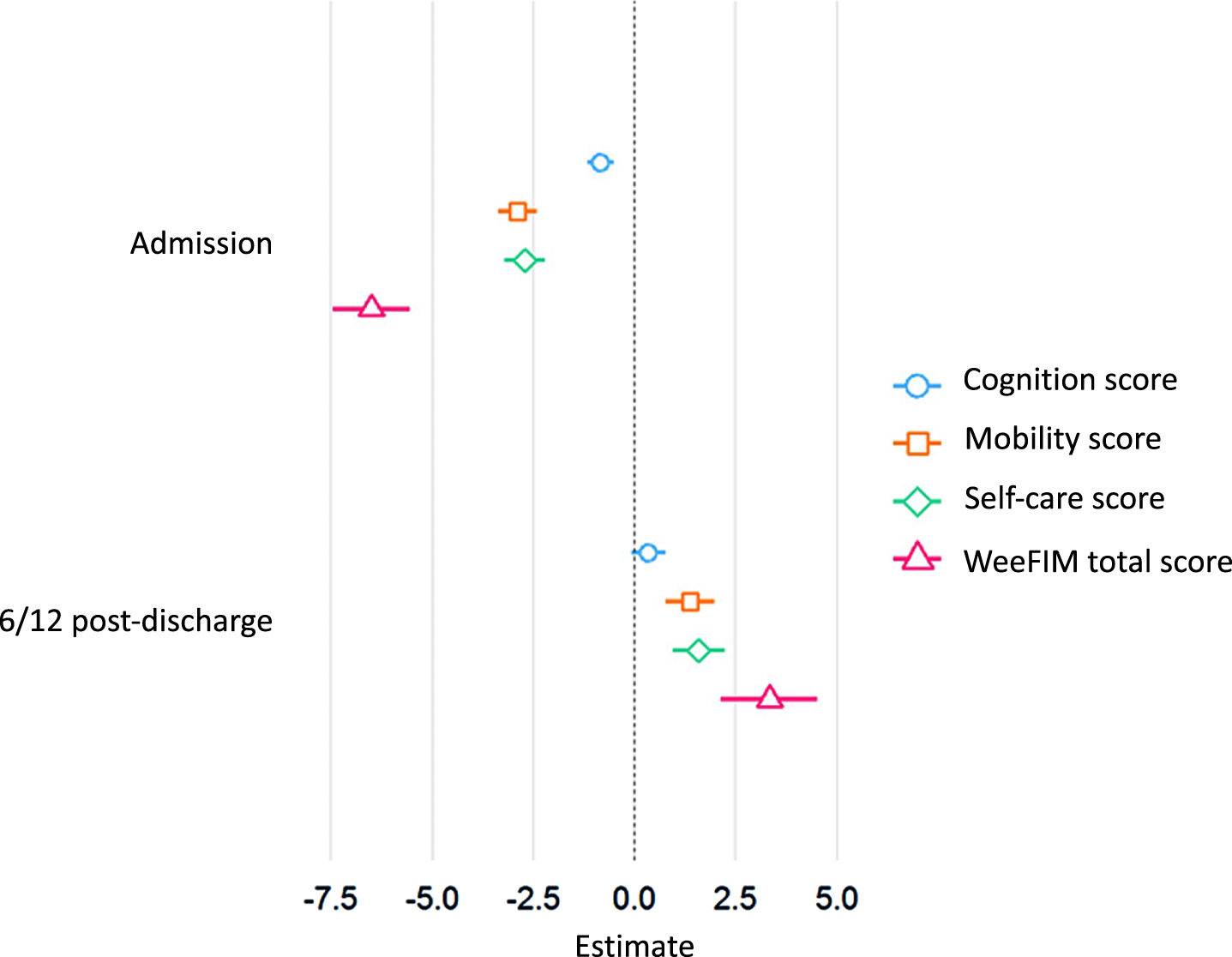
Total mean WeeFIM score for the study population improved between admission and discharge (6.51, 95% CI 5.56 to 7.45, p < 0.001), with further improvements observed between discharge and six month follow-up (3.33, 95% CI 2.14 to 4.53, p < 0.001). The average increase in total score from admission to six months post discharge was 9.84 (95% CI 8.64 to 11.03). Improvements in the individual WeeFIM domains of self-care, mobility, and cognition between admission and discharge were also individually significant (Table 3). Self-care and mobility scores also increased between discharge and six months post follow-up (p < 0.001 for both), but these changes were smaller than those seen between admission and discharge. Changes in cognitive scores from discharge to six months post discharge were not statistically significant (Table 3, Fig. 4).
WeeFIM data for each of the four diagnostic subgroups showed significant improvements in Mobility, Self-Care and total scores between admission and discharge; these improvements were maintained at follow-up (Supplemental Information 3).
3.3Goal attainment
Mean GAS T-scores for the whole group increased by 27.85 (95% CI 26.73 to 28.97, p < 0.001) from admission to discharge, and by 29.64 (95% CI 28.26 to 31.02, p < 0.001) from admission to six months post discharge (Table 4). These changes were statistically significant (p < 0.001 in all diagnostic groups) with all T-scores in the 40–60 range at discharge and six months post discharge, indicating goal attainment consistent with expectations (Fig. 5) [22, 23].
Table 4
Mean Goal Attainment Scale (GAS) T-scores: total group and subgroups. Effect estimates (95% confidence intervals) relative to GAS score at discharge
| ABI | Cerebral Palsy | Spinal | Other | Total | |
| Discharge | 50.26 | 51.57 | 53.52 | 52.14 | 51.67 |
| (Intercept) | (48.25, 52.28) | (50.21, 52.93) | (51.13, 55.92) | (50.38, 53.89) | (50.69, 52.56) |
| Admission | –27.12 | –27.5 | –29.58 | –28.01 | –27.85 |
| (–29.70, –24.54)*** | (–29.21, –25.78)*** | (–32.5, –26.67)*** | (–30.23, –25.79)*** | (–26.73, –28.97)*** | |
| 6 months post | 7.49 | 0.74 | –2.23 | 0.86 | 1.79 |
| discharge | (4.34, 10.64)*** | (–1.36, 2.85) | (–5.84, 1.39) | (–1.96, 3.68) | (0.4, 3.18) |
***p < 0.001; **p < 0.01; *p < 0.05. ABI: acquired brain injury.
Fig. 5
Goal Attainment Scale mean T-scores: whole group and diagnostic subgroups. ABI: acquired brain injury.
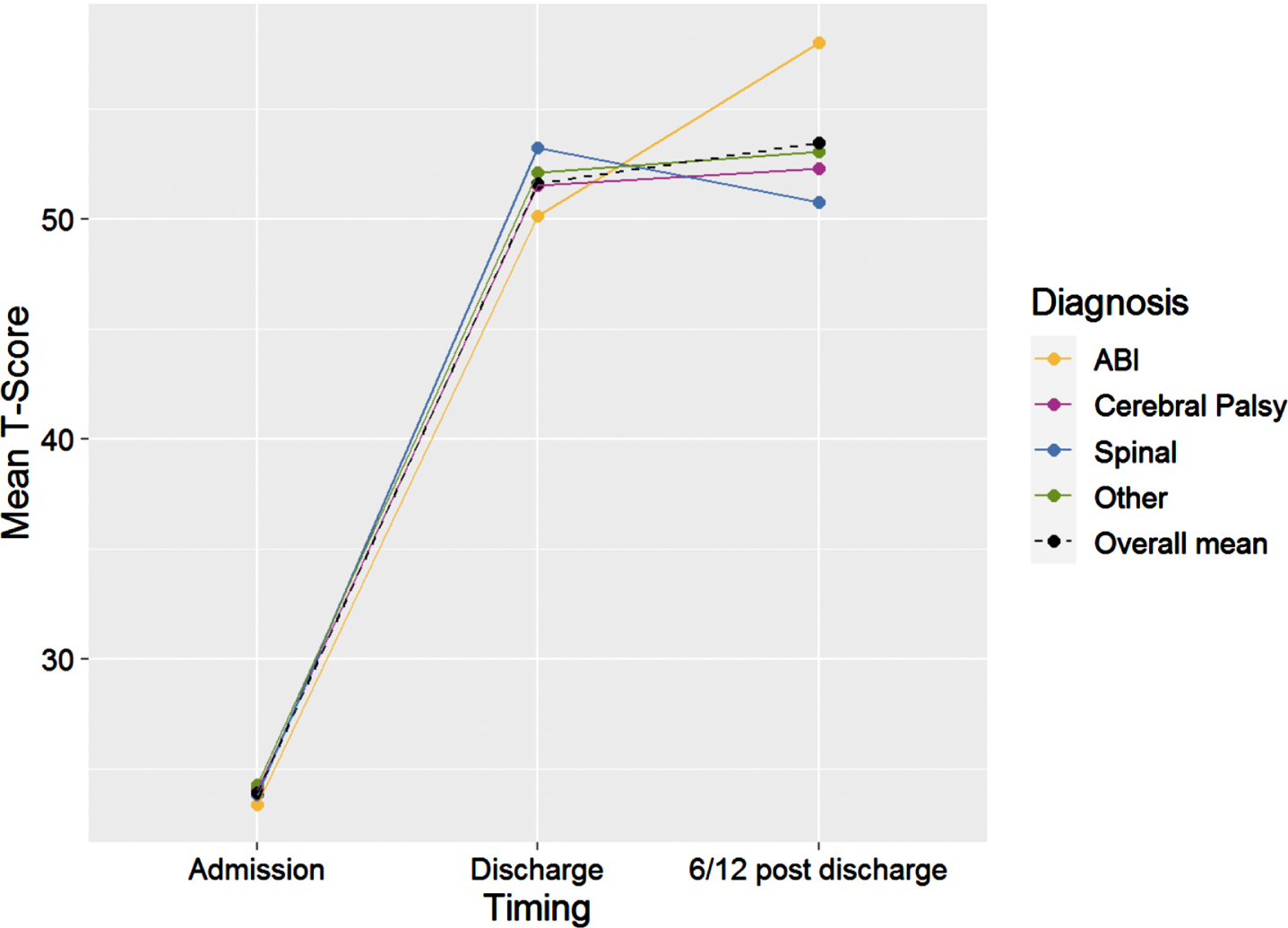
Further changes between discharge and six months post discharge were not statistically significant, except in the ABI group where further improvement was noted (7.49, 95% CI 4.34 to 10.64, p < 0.001).
Analysis was performed to examine the effect of patient age as a continuous variable on outcomes. Age had no effect on GAS or COPM scores. On average, total WeeFIM scores at all time points increased by 3.66 per additional year of age (95% CI 3.12 to 4.2) in patients in this study. This reflects the nature of the WeeFIM, as older children with more advanced development have higher levels of independence. The WeeFIM has ceiling effects for typically-developing children aged seven and older but is appropriate for use in older children in the context of disability which reduces independence [30].
No statistically significant effects of length of stay on GAS or WeeFIM scores were detected. Longer admission was associated with lower COPM Performance scores at discharge; compared to two week admissions, scores were 1.03 points lower at discharge for four week admissions (95% CI 0.23 to 1.82, p = 0.01), 0.95 points lower at discharge for five week admissions (0.27 to 1.62, p = 0.01), and 0.75 points lower at discharge for admissions of over six weeks (0.2 to 1.3, p = 0.01), holding all other variables consistent. Significant effects of length of stay on COPM Satisfaction scores were seen only for admissions of four weeks and those of over six weeks; four week admissions had Satisfaction scores 0.93 less than two week admissions (0.02 to 1.84, p = 0.05), while admissions greater than six weeks were associated with Satisfaction scores that were 0.71 less than those of two weeks (0.08 to 1.33, p = 0.03).
4Discussion
This paper describes the characteristics, goals, and outcomes of young people who attended a specialist intensive day rehabilitation service between 2011 and 2018, and demonstrates that a diagnostically diverse cohort achieved significant improvements in function, independence, and goal attainment which were maintained at follow-up. From admission to six months post discharge, young people gained an average of 9.84 WeeFIM points, approximately three points on COPM Performance and Satisfaction scores, and achieved their goals based on GAS T-scores. Significant improvements were seen for all diagnostic subgroups in relation to all outcomes measured.
Most previous research has focused on improvements achieved during inpatient treatment [31]; these results show it is possible to achieve significant functional gains in an intensive day rehabilitation setting. There are few studies directly comparable to the present study due to the well-acknowledged heterogeneity of rehabilitation provided to patients [4–6, 8]. However, the degree of measured improvement seen here is broadly comparable to other studies [32, 33]. Previous studies have noted the advantages of intensive intervention but acknowledged the disruption to family life caused by extended inpatient hospital stays [34]. Day rehabilitation may have advantages for some families and healthcare systems over inpatient models of rehabilitation in this regard.
This study underlines the importance of a biopsychosocial approach to rehabilitation [1, 7]. Young people in this study identified a variety of rehabilitation goals, including many not addressed by a medical model of disability. While mobility goals were most common in all groups, there was a broad spectrum of other goals indicating a need to consider multiple potential priorities for each individual.
Data are not available for children, but a 2012 report estimated regular participation in physical activity among Australian adults with disabilities at 30%, compared to 65% of the non-disabled population [36]. In this context, external barriers to participation (unmeasured in this study) may contribute to the goals that a child and family choose to prioritise; it is possible that a higher proportion of children would have identified goals pertaining to active recreation if access to such pursuits were more equitable.
Active recreation accounted for only 4% of all occupational performance issues identified by COPM. This may suggest that leisure goals are not a high priority for a young person or their family in the context of acute rehabilitation, but complex barriers to activity for young people with chronic disabilities are also likely relevant [35].
CP accounted for the largest proportion (38.9%) of iRehab admissions of the four diagnostic groups. The CP group had an older age profile, reflecting the fact that need for therapy in this group typically increases in late childhood with evolving musculoskeletal deformity and mobility impairments [37]. Mean total WeeFIM at admission for young people with CP was 56 (SD 28.89), the lowest of any group (Supplemental Information 3). Patients with CP in this study had a higher prevalence of quadriplegia than the background CP population of Western Australia (32.7% v 14.3%) [38]. Children with CP made improvements in Mobility, Self-Care, and total WeeFIM scores at all time points. Improvements can be achieved in this population with intensive rehabilitation input, much of which occurred after orthopaedic surgery. The natural history of CP makes spontaneous improvements of this sort unlikely without intervention [39].
A 2 : 1 male:female ratio was noted for admissions with traumatic brain injury, consistent with existing research [27–29]. Approximately half of admissions were of children under nine years old. Younger age at injury is an adverse prognostic indicator [40]. Thus, younger patients who have higher levels of need may be over-represented in tertiary rehabilitation services.
Outcomes for young people after ABI are difficult to predict [4, 6, 40]. Many patients attended iRehab directly after an acute inpatient admission following ABI. Such patients typically experience a “sigmoidal” recovery phase, characterised by an initial period of slow progress, followed by a period of rapid progress, eventually followed by a chronic plateau phase when peak performance is reached [40], although slow improvements may continue for years following ABI [41]. It is unlikely that comparable progress would be made without rehabilitation, but some progress seen in patients admitted to iRehab following ABI occurred for physiological reasons rather than exclusively due to rehabilitation; the specific treatment effect of rehabilitation in general is difficult to quantify [4, 40]. It remains a challenge to know what degree of improvement would be expected in a given patient without treatment, which makes quantifying the added benefit of a particular rehabilitation programme difficult [8, 40].
The Other group accounted for almost one quarter of iRehab admissions. It included a broad range of medical conditions (Table 1 and Supplemental Information 1), many of which may not be traditionally considered as causes of disability outside of a rehabilitation setting. This group made similar gains to the others, indicating their suitability for rehabilitation and supporting the fact that an intensive specialist rehabilitation service can be provided by a single team to a diagnostically diverse cohort of children. This reinforces the perspective espoused in the ICF-CY [7] and WHO statements [16] that rehabilitation is of benefit to a greater proportion of the population than currently have access to it. Specialists in disability and rehabilitation may have more progressive attitudes to disability than those in other fields [42] and thus have an opportunity to advocate for the development of rehabilitation services for children beyond the traditional disability cohort.
There is little published research regarding the functional outcomes of young people accessing services comparable to iRehab. The novelty of this study is a strength, as is the large number of patients and the availability of data pertaining to a number of complementary, reliable, and valid outcome measures [43, 44]. Each of the measures used a different construct of disability; using them in combination gave a broad perspective on individual experiences and recognized the complex nature of disability which cannot be easily captured by a single measure. Balancing the need for a standardized approach with the fact that disability can impact nearly any aspect of the human experience is a challenge of measuring rehabilitation outcomes in any setting. Qualitative research has an important role capturing the stories of young people who experience disability.
Statistical significance and clinical significance cannot necessarily be conflated. The minimal clinically important difference (MCID) for a particular outcome measure will vary depending on population studied, clinical context, and type of intervention. MCIDs are not widely reported for the tools used in this paper in a way that is easily extrapolated to iRehab. One study of ambulatory children with CP reported WeeFIM to have an MCID of 2.3 for Mobility, 3.1 for Self-Care, and 3.4 for Cognition [45]; this study was based on two measurements at least a year apart (and not in the context of a specific intervention). Thus, the thresholds cannot be easily transposed to this study. The Canadian Association of Occupation Therapists (CAOT) have reported an MCID of 2 points for the COPM [46]. The validity of this threshold has been disputed [47], however, and the authors are unaware of any study conclusively demonstrating MCIDs for COPM in children. The CAOT also report that “the COPM is an individualized measure, so the meaning of the change scores may vary by individual” [46]. This is likely to also be true of WeeFIM scores, where even small changes in individual subscores could be highly meaningful for one child, depending on their context and the domain in which the improvement was made (e.g., moving from being supervised with a task [Level 5] to a level of modified independence [Level 6]).
Therefore, statistical significance should not be interpreted as automatically conferring meaningfulness of changes measured for any one person [20, 48, 49]. The suite of measures used in iRehab addressed that limitation by linking occupational performance issues to formalized goal setting while simultaneously assessing functional independence. While a specific MCID for COPM or WeeFIM for the study cohort cannot be stated, the fact that child-centred goals were achieved within the expected range using GAS alongside statistically significant changes in COPM and WeeFIM is evidence for the clinical importance of the changes measured.
These data should be interpreted in the context of their limitations. Without a control group, it is not possible to definitively attribute improvements in outcomes solely to iRehab; unmeasured factors (e.g., non-standardised therapy input provided in the community after iRehab discharge, or the effect of neurodevelopmental progress with increasing age on WeeFIM scores at six months post discharge) may also contribute [44]. This likely applies less to GAS, which involves setting goals and then designing a joint therapeutic strategy to attain them. One of the specific benefits of iRehab is enabling young people to work with a team to establish goals for themselves. Goals which are not formally set, as may have been the case without iRehab input, are unlikely to be reached. Rehabilitation outcomes are known to improve when patients are involved in the goal-setting process [22]. Due to its individualized nature, GAS has low concurrent validity but is highly sensitive to change [50]. The measures used in iRehab do not capture quality of life or family functioning (although psychosocial support is provided by case managers, social workers, clinical psychologists, and others), nor do they specifically measure the impact of executive functioning difficulties which are common after ABI. Retrospective data analysis may lead to under-reporting of individual data points and to biases which cannot easily be controlled [51, 52].
Rehabilitation services are generally underdeveloped compared to demand [10, 16] and were among those hit the hardest by COVID-19, with provision severely disrupted worldwide [53]. COVID-19 has led to many people experiencing disability transiently, highlighting the fact that disability and rehabilitation services are not only relevant to those traditionally considered as disabled [7]. The cost-effectiveness of adult rehabilitation is supported by evidence but has not yet been definitively demonstrated for paediatric rehabilitation [6, 54]. It is extremely likely that the rehabilitation of children and young people is cost-effective given the many more years of life over which savings in health and social care will accrue. The true impact on society of ABI in childhood is almost certainly underestimated, considering the frequently unmeasured costs of homecare provided without remuneration by parents who may have given up paid employment, as well as the fact that many chronic sequelae of ABI in childhood (e.g., mental health difficulties, criminality, educational problems) go unattributed to the ABI that caused them. [55]. Development of quality specialist rehabilitation services to meet the demand in a timely manner is a key challenge for 21st century healthcare [2, 3, 16]. Recovery trajectories of children who experience disability due to acute illness or injury are different from the typical developmental trajectories of children who experience chronic disability from birth. These different trajectories are not always reflected in models of service design; services which are configured to provide for bursts of intense input in the context of a period of expected rapid improvement in function (e.g., following injury, illness, or surgical intervention) may have advantages over more generic service design [10]. The iRehab model is one example of an approach to rehabilitation which is feasible and associated with positive outcomes for young people.
The outcomes a service reports reflect its priorities. Measures of function and goal attainment offer a more meaningful insight into the experiences of patients than do statistics on length of stay, volume of service provision, or morbidity and mortality data. The use of multiple complementary measures in combination can identify changes at multiple levels of the ICF-CY framework [7]. Functioning is now recognised as the “third indicator” of health alongside morbidity and mortality, which are more frequently and readily reported internationally [56]. Regardless of the specific models employed, it is essential that paediatric rehabilitation services worldwide report on their processes and meaningful functional outcomes so as to grow the evidence base for paediatric rehabilitation and to enable benchmarking between centres in relation to meaningful patient outcomes [10, 15, 16].
Rehabilitation services are a mechanism by which states can uphold the rights of disabled people to participate in their own lives [1, 3, 16]. There is an urgent need to expand intensive rehabilitation systems to better provide for the rights of children and young people who experience disability [10, 11, 16] and to make such services available in a flexible manner beyond the inpatient setting. Young people with rehabilitation needs in other centres could benefit from access to an intensive specialist day rehabilitation service provided regardless of underlying medical diagnoses in the pursuit of meaningful child-centred functional goals.
Acknowledgments
The authors have no acknowledgments.
Conflict of interest
The authors have no conflict of interest to report.
Supplemental information
[1] The supplemental information is available in the electronic version of this article: https://dx.doi.org/10.3233/PRM-220102.
References
[1] | Wade DT . What is rehabilitation? An empirical investigation leading to an evidence-based description. Clin Rehabil. (2020) ;34: (5):571–83. doi: 10.1177/0269215520905112. |
[2] | World Report on Disability 2011. Geneva: World Health Organization; 2011. Available from: https://www.who.int/teams/noncommunicable-diseases/sensory-functionsdisability-and-rehabilitation/world-report-on-disability |
[3] | A Vision For Primary Healthcare in the 21st Century: Towards universal health coverage and the sustainable development goals. Geneva: World Health Organization, United Nations Children’s Fund; 2018. Available from: https://www.who.int/docs/default-source/primaryhealth/vision.pdf |
[4] | Forsyth R , Basu A . The promotion of recovery through rehabilitation after acquired brain injury in children. Dev Med Child Neurol. (2015) ;57: (1):16–22. doi: 10.1111/dmcn.12575. |
[5] | Novak I , McIntyre S , Morgan C , et al.. A systematic review of interventions for children with cerebral palsy: state of the evidence. Dev Med Child Neurol. (2013) ;55: (10):885–910. doi: 10.1111/dmcn.12246. |
[6] | Turner-Stokes L . Evidence for the effectiveness of multi-disciplinary rehabilitation following acquired brain injury: a synthesis of two systematic approaches. J Rehabil Med. (2008) ;40: (9):691–701. doi: 10.2340/16501977-0265. |
[7] | International classification of functioning, disability and health: children and youth version (ICF-CY). Geneva: World Health Organization; 2007. |
[8] | Kelly G , Mobbs S , Pritkin JN , et al.. Gross Motor Function Measure-66 trajectories in children recovering after severe acquired brain injury. Dev Med Child Neurol. (2015) ;57: (3):241–7. doi: 10.1111/dmcn.12592. |
[9] | Chen CC , Heinemann AW , Bode RK , Granger CV , Mallinson T . Impact of pediatric rehabilitation services on children’s functional outcomes. Am J Occup Ther. (2004) ;58: (1):44–53. doi: 10.5014/ajot.58.1.44. |
[10] | Hayes L , Shaw S , Pearce MS , Forsyth RJ . Requirements for and current provision of rehabilitation services for children after severe acquired brain injury in the UK: a population-based study. Arch Dis Child. (2017) ;102: (9):813–20. doi: 10.1136/archdischild-2016-312166. |
[11] | Fuentes MM , Wang J , Haarbauer-Krupa J , et al.. Unmet Rehabilitation Needs After Hospitalization for Traumatic Brain Injury. Pediatrics. (2018) ;141: (5):e20172859. doi: 10.1542/peds.2017-2859. |
[12] | Zonfrillo MR , Durbin DR , Winston FK , Zhao H , Stineman MG . Physical disability after injury-related inpatient rehabilitation in children. Pediatrics. (2013) ;131: (1):e206–e213. doi: 10.1542/peds.2012-1418. |
[13] | Kids Rehab WA Consumer Reference Group [communication] (Unpublished). |
[14] | Thomas-Stonell N , Johnson P , Rumney P , Wright V , Oddson B . Anevaluation of the responsiveness of a comprehensive set of outcomemeasures for children and adolescents withtraumatic brain injuries. Pediatr Rehabil. (2006) ;9: (1):14–23. doi: 10.1080/13638490500050097. |
[15] | Maas AIR , Menon DK , Adelson PD , et al.. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. (2017) ;16: (12):987–1048. doi: 10.1016/S1474-4422(17)30371-X. |
[16] | Cieza A , Causey K , Kamenov K , Hanson SW , Chatterji S , Vos T . Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2021) ;396: (10267):2006–17. doi: 10.1016/S0140-6736(20)32340-0. |
[17] | The Lancet The burden of traumatic brain injury in children. Lancet. (2018) ;391: (10123):813. doi: 10.1016/S0140-6736(18)30547-6. |
[18] | Knoester H , Bronner MB , Bos AP . Surviving pediatric intensive care: physical outcome after 3 months. Intensive Care Med. (2008) ;34: (6):1076–82. doi: 10.1007/s00134-008-1061-4. |
[19] | Garner AA , Mann KP , Fearnside M , Poynter E , Gebski V . The Head Injury Retrieval Trial (HIRT): a single-centre randomised controlled trial of physician prehospital management of severe blunt head injury compared with management by paramedics only. Emerg Med J. (2015) ;32: (11):869–75. doi: 10.1136/emermed-2014-204390. |
[20] | Ottenbacher KJ , Msall ME , Lyon N , et al.. The WeeFIM instrument: its utility in detecting change in children with developmental disabilities. Arch Phys Med Rehabil. (2000) ;81: (10):1317–26. doi: 10.1053/apmr.2000.9387. |
[21] | Law M , Baptiste S , Carswell A , McColl MA , Polatajko H , Pollock N COPM Canadian Occupational Performance Measure. 4th ed. Ottawa, ON: CAOT Publications ACE; 2005. |
[22] | Krasny-Pacini A , Hiebel J , Pauly F , Godon S , Chevignard M . Goal attainment scaling in rehabilitation: a literature-based update. Ann Phys Rehabil Med. (2013) ;56: (3):212–30. doi: 10.1016/j.rehab.2013.02.002. |
[23] | Turner-Stokes L . Goal attainment scaling (GAS) in rehabilitation: a practical guide [published correction appears in Clin Rehabil. 2010 Feb;24(2):191].. Clin Rehabil. (2009) ;23: (4):362–70. doi: 10.1177/0269215508101742. |
[24] | Bates D , Mächler M , Bolker B , Walker S . Fitting Linear Mixed-Effects Models Using lme4. Journal of Statistical Software. (2015) ;67: (1):1–48. doi: 10.18637/jss.v067.i01. |
[25] | Wood S , Scheipl F Gamm4: Generalized Additive Mixed Models Using ‘Mgcv’ and ‘Lme4’. 2020 [cited August 2020]. Available from: https://CRAN.R-project.org/package=gamm4 |
[26] | R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2020. Available from: https://www.R-project.org/ |
[27] | Trefan L , Houston R , Pearson G , et al.. Epidemiology of children with head injury: a national overview. Arch Dis Child. (2016) ;101: (6):527–32. doi: 10.1136/archdischild-2015-308424. |
[28] | Chen C , Peng J , Sribnick EA , Zhu M , Xiang H . Trend of Age-Adjusted Rates of Pediatric Traumatic Brain Injury in U.S. Emergency Departments from 2006 to 2013. Int J Environ Res Public Health. (2018) ;15: (6):1171. doi: 10.3390/ijerph15061171. |
[29] | Thurman DJ . The Epidemiology of Traumatic Brain Injury in Children and Youths: A Review of Research Since 1990. J Child Neurol. (2016) ;31: (1):20–7. doi: 10.1177/0883073814544363. |
[30] | Msall ME , Digaudio K , Duffy LC , LaForest S , Braun S , Granger CV . WeeFIM. Normative Sample Of An Instrument For Tracking Functional Independence In Children. Clin Pediatr (Phila). (1994) ;33: (7):431–8. doi: 10.1177/000992289403300709. |
[31] | Kramer ME , Suskauer SJ , Christensen JR , et al.. Examining acute rehabilitation outcomes for children with total functional dependence after traumatic brain injury: a pilot study. J Head Trauma Rehabil. (2013) ;28: (5):361–70. doi: 10.1097/HTR.0b013e31824da031. |
[32] | Christy JB , Chapman CG , Murphy P . The Effect Of Intense Physical Therapy For Children With Cerebral Palsy. J Pediatr Rehabil Med. (2012) ;5: (3):159–70. doi: 10.3233/Prm-2012-0208. |
[33] | Allen DD , Mulcahey MJ , Haley SM , et al.. Motor Scores On The Functional Independence Measure After Pediatric Spinal Cord Injury. Spinal Cord. (2009) ;47: (3):213–7. doi: 10.1038/Sc.2008.94. |
[34] | Lee SH , Shim JS , Kim K , Moon J , Kim M . Gross Motor Function Outcome After Intensive Rehabilitation In ChildrenWith Bilateral Spastic Cerebral Palsy. Ann Rehabil Med. (2015) ;39: (4):624–9. doi: 10.5535/Arm.2015.39.4.624. |
[35] | Verschuren O , Peterson MD , Balemans AC , Hurvitz EA . Exercise and physical activity recommendations for people with cerebral palsy. Dev Med Child Neurol. (2016) ;58: (8):798–808. doi: 10.1111/dmcn.13053. |
[36] | Participation in Sport and Physical Recreation, Australia 2012. Catalogue no. 4156.0. Canberra, Australia: Australian Bureau of Statistics; 2012. |
[37] | Graham HK , Harvey A , Rodda J , Nattrass GR , Pirpiris M . The Functional Mobility Scale (FMS). J Pediatr Orthop. (2004) ;24: (5):514–20. doi: 10.1097/00004694-200409000-00011. |
[38] | Report of the Australian Cerebral Palsy Register, Birth Years 1995–2012. Australian Cerebral Palsy Register Group; 2018. Available from: https://cpregister.com/wpcontent/uploads/2019/02/Report-of-the-Australian-Cerebral-Palsy-Register-Birth-Years-1995-2012.pdf |
[39] | Beckung E , Carlsson G , Carlsdotter S , Uvebrant P . The Natural History Of Gross Motor Development In Children With Cerebral Palsy Aged 1 To 15 Years. Dev Med Child Neurol. (2007) ;49: (10):751–6. doi: 10.1111/J.1469-8749.2007.00751.X. |
[40] | Forsyth RJ , Salorio CF , Christensen JR. . Modelling early recovery patterns after paediatric traumatic braininjury. Arch Dis Child. (2010) ;95: (4):266–70. doi: 10.1136/adc.2008.147926. |
[41] | Beretta E , Molteni E , Galbiati S , Stefanoni G , Strazzer S . Five-Year Motor Functional Outcome In Children WithAcquired Brain Injury. Yet To The End Of The Story? Dev Neurorehabil. (2018) ;21: (7):449–56. doi: 10.1080/17518423.2017.1360408. |
[42] | Shakespeare T , Iezzoni LI , Groce NE . Disability And The Training Of Health Professionals. Lancet. (2009) ;374: (9704):1815–6. doi: 10.1016/S0140-6736(09)62050-X. |
[43] | Williams KS , Young DK , Burke GAA , Fountain DM . Comparing the WeeFIM and PEDI in neurorehabilitation for children with acquired brain injury: A systematic review. Dev Neurorehabil. (2017) ;20: (7):443–51. doi: 10.1080/17518423.2017.1289419. |
[44] | Wallen MA , Ziviani JM . Canadian Occupational Performance Measure: impact of blinded parent-proxy ratings on outcome. Can J Occup Ther. (2012) ;79: (1):7–14. doi: 10.2182/cjot.2012.79.1.2. |
[45] | Oeffinger D , Bagley A , Rogers S , et al.. Outcome Tools Used For Ambulatory Children With Cerebral Palsy: Responsiveness And Minimum Clinically Important Differences. Dev Med Child Neurol. (2008) ;50: (12):918–25. doi: 10.1111/J.1469-8749.2008.03150.X. |
[46] | Frequently Asked Questions: Psychometric Properties and Scoring the COPM. The Canadian Occupational Performance Measure; 2023. Available from: https://www.thecopm.ca/faq/#Psychometric |
[47] | Enemark Larsen A . The Canadian Occupational Performance Measure (Copm): A Valuable Tool For Children With Cerebral Paresis. Dev Med Child Neurol. (2020) ;62: (10):1115. doi: 10.1111/Dmcn.14617. |
[48] | Hays WL Statistics For The Social Sciences. 2nd ed. New York: Holt, Rinehart & Winston; 1973. |
[49] | Hebert R , Spiegelhalter DJ , Brayne C . Setting The Minimally Detectable Change On Disability Rating Scales. Arch Phys Med Rehabil. (1997) ;78: :1305–8. doi: 10.1016/s0003-9993(97)90301-4. |
[50] | Steenbeek D , Ketelaar M , Galama K , Gorter JW . Goal Attainment Scaling In Paediatric Rehabilitation: A CriticalReview of The Literature. Dev Med Child Neurol. (2007) ;49: (7):550–6. doi: 10.1111/J.1469-8749.2007.00550.X. |
[51] | Creswell JW Qualitative Inquiry & Research Design: Choosing among Five Approaches. 3rd ed. Thousand Oaks, CA: Sage Publications Ltd.: 2013. |
[52] | Denzin NK , Lincoln YS Introduction: The Discipline and Practice of Qualitative Research. In: Denzin NK, Lincoln YS, editors. The Sage handbook of qualitative research. Thousand Oaks, CA: Sage Publications, Inc.: 2005. pp. 1–32. |
[53] | Rehabilitation considerations during the COVID19 outbreak. Pan American Health Organization; 2020. Available from: https://iris.paho.org/handle/10665.2/52035 |
[54] | Turner-Stokes L , Williams H , Bill A , Bassett P , Sephton K . Cost-efficiency of specialist inpatient rehabilitation for working-aged adults with complex neurological disabilities: a multicentre cohort analysis of a national clinical data set. BMJ Open. (2016) ;6: (2):e010238. doi: 10.1136/bmjopen-2015-010238. |
[55] | Forsyth RJ . Back to the future: rehabilitation of children after brain injury. Arch Dis Child. (2010) ;95: (7):554–9. doi: 10.1136/adc.2009.161083. |
[56] | Stucki G , Bickenbach J . Functioning: the third health indicator in the health system and the key indicator for rehabilitation. Eur J Phys Rehabil Med. (2017) ;53: (1):134–8. doi: 10.23736/S1973-9087.17.04565-8. |




