Telehealth in pediatric rehabilitation medicine: A survey of clinician reported utilization and experience
Abstract
PURPOSE:
Telehealth services have been touted to improve access to specialty pediatric care. COVID-19 accelerated the adoption of telehealth across many medical specialties. The purpose of this study was to examine telehealth utilization and satisfaction among pediatric physiatrists.
METHODS:
Using Google Forms, a voluntary survey was created and administered to pediatric physiatrists. The survey collected information on practice setting, telehealth utilization, provider satisfaction, perceived satisfaction of patients and families, and the anticipated role of telehealth in pediatric rehabilitation going forward.
RESULTS:
Seventy-eight respondents completed the survey. There was a significant reported increase in telehealth utilization since COVID-19 from 14.5% to 97.4%. Eighty-two percent of participants reported feeling comfortable utilizing telehealth, 77% felt confident in the quality of the care provided, and 91% believed patients were satisfied with telehealth visits. Responses indicate that telehealth is expected to play a role in future pediatric physiatry and interest in telehealth continuing medical education is prevalent. Most pediatric physiatrists plan to continue or expand telehealth offerings after COVID-19.
CONCLUSION:
Telehealth adoption has been expedited by COVID-19. Physician interest in and satisfaction with telehealth is high. Patient and family perceptions, outcomes of care, and barriers to implementation limiting program expansion deserve further study.
1.Introduction
Decades before the current global outbreak of coronavirus disease 19 (COVID-19), telehealth was utilized to expand delivery of healthcare services by means of information technology [1]. The declaration of COVID-19 as a pandemic by the World Health Organization on March 11, 2020 triggered widespread measures to mitigate transmission including isolation of suspected and confirmed cases, monitoring of contacts, and public quarantine [2]. In order to preserve critical supplies, expand hospital capacity, and protect the medical workforce, the Centers for Disease Control and Prevention (CDC) advocated prioritization of urgent and emergency care and procedures which entailed the delay and rescheduling of routine visits [3]. The CDC’s current guidance for outpatient and ambulatory care settings promotes increased utilization of telehealth services to decrease the number of persons seeking care in facilities [4].
In rehabilitation, telemedicine services have been utilized alone and in combination with traditional care for treatment of conditions including stroke, traumatic brain injury, multiple sclerosis, chronic pain, hip and knee total arthroplasty, and medical conditions such as congestive heart failure and rheumatologic disease [5]. Evidence supports that telehealth services are well received by patients, do not increase caregiver burden, and may confer functional benefits for certain patients; however, interpretation of the available literature is limited by variation in methodology and approaches [5]. In the pediatric population, telehealth has been utilized for the provision of early intervention and school-based therapy services [6]. Associated studies have identified concerns with the quality of services delivered, patient privacy, security, and the lack of evidence supporting telehealth efficacy [6].
Pediatric physiatrists play an essential role in the comprehensive care of children and adults with pediatric onset disability. Unfortunately, many children with medical complexity are left with unmet needs owing to a national shortage of PRM physicians in the United States [7]. With the flourishing of information technology capabilities, telehealth has been an area of increasing focus as a means to extend medical expertise to the underserved.
As an impact of the COVID-19 crisis, healthcare providers across the globe have been thrust into unfamiliar roles and challenged with the task of delivering care in the context of tight institutional and social restrictions. Accordingly, the Pediatric Physiatry community at large has turned to telehealth assets to continue to reach patients. The aim of this study was to explore the experiences, comfort level, and attitudes of Pediatric Physiatrists utilizing telehealth. Analysis of perspectives provided by experienced and trainee clinicians may provide a valuable foundation upon which to base much needed investigations of telehealth applicability, outcomes, cost efficacy, and best practice in pediatric physiatric medicine.
2.Methods
Using Google forms, an IRB exempt online survey was created to obtain information about the utilization and implementation of telehealth related to care of pediatric patients. Questions were designed to capture the role, practice setting, and telehealth utilization of providers before and after COVID-19 related practice changes. Additionally, queries used a Likert scale to ascertain opinions on telehealth in pediatric physiatry broadly, its effect on workflow efficiency, comfort level of providers using telehealth visits, comparison to standard in person visits in terms of visit quality by the provider and the providers’ perceived impact of the visit on their patients. Also included were questions on the intent to continue telehealth visits after the COVID-19 crisis and the potential to expand telehealth capabilities in the future for patients with remote or difficult access to clinics. The survey was limited to 11 questions to facilitate completion, and is included in the appendix.
The survey was created and completed via Google forms. The intended respondents were pediatric physiatrists and pediatric physiatry fellows. The survey was disseminated via a pediatric rehabilitation Facebook group as well as by email to program directors at all ACGME pediatric physical medicine and rehab fellowship programs with request to forward to their respective departments. All responses to the survey were anonymous, and no identifiable information was collected as part of this survey.
Completion of this voluntary survey was undertaken with implied consent.
2.1Analysis
First, practice role and practice setting of the survey sample were described. Then, the percentages of respondents were calculated based on positive, negative or neutral responses to the Likert questions of the sample. Results were analyzed and grouped by responses.
3.Results
There were 79 total responses, 78 of whom completed the survey. Of those who completed the survey, the vast majority, 87.2% (68 responses) were pediatric physiatry attending physicians, while 10.3% (8 responses) were pediatric physiatry fellows, and 2.6% (2 responses) were completed by physiatry residents. Excluding the resident trainees did not have any meaningful effect on the analysis.
Figure 1.
Telehealth practices before and after COVID-19.
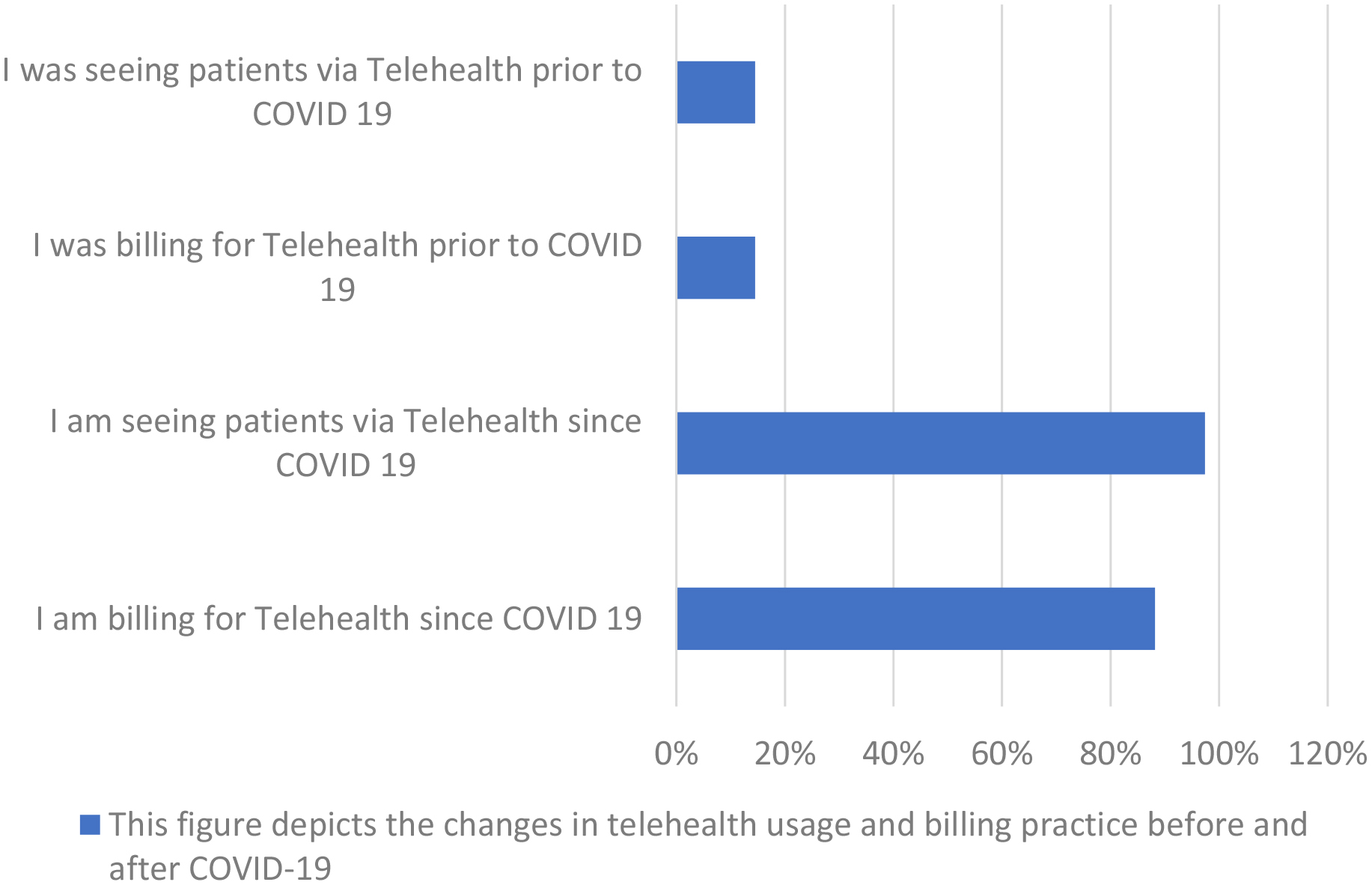
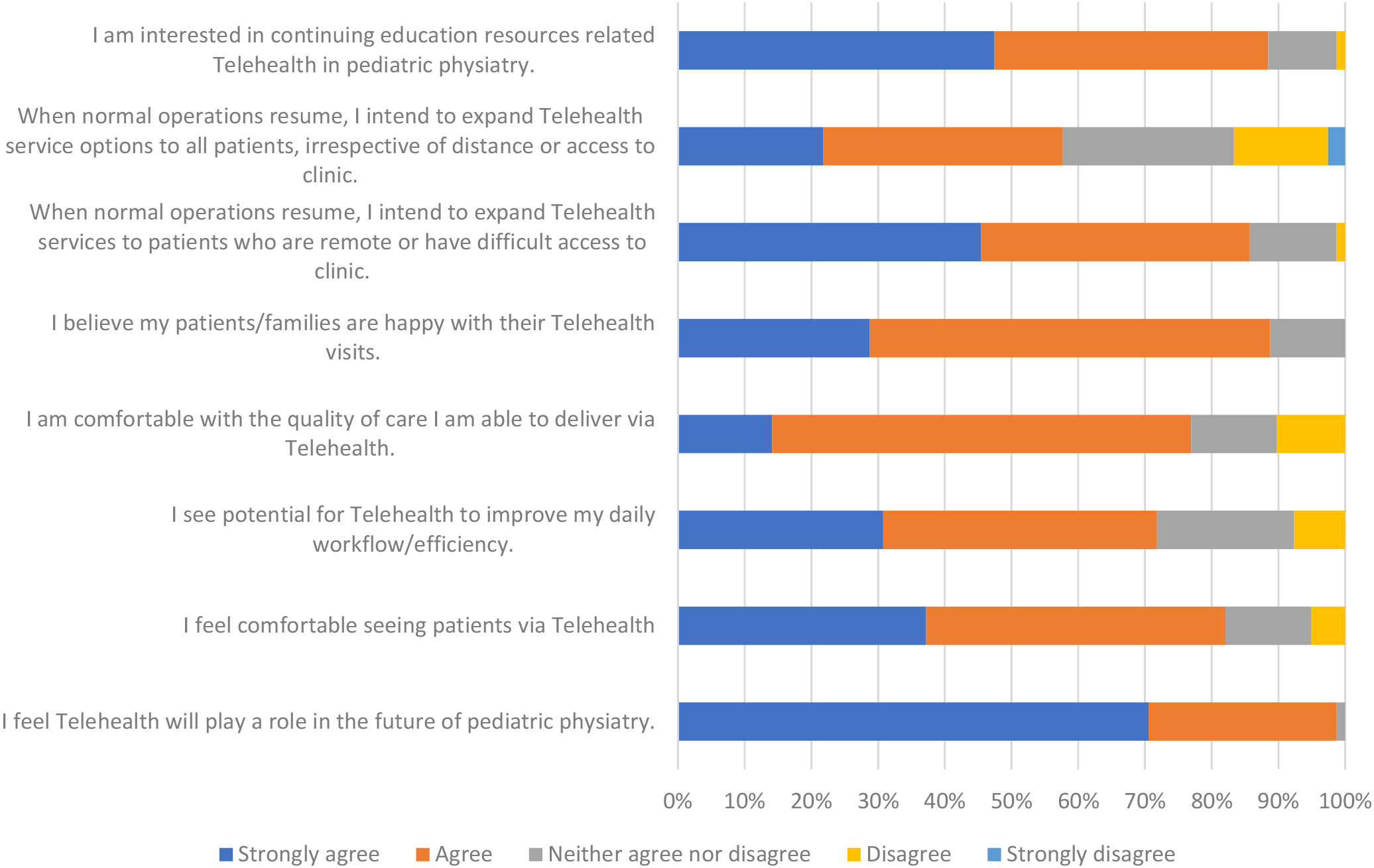
Figure 2.
Telehealth experiences and intentions. This figure depicts the responses regarding telehealth experiences and opinions.
In regard to practice setting of attending pediatric physiatrists, 80% (55 respondents) reported practicing in an academic medical center, 13% (9 respondents) in the hospital not associated with an academic medical center, and 7% (5 respondents) in private practice/other practice setting.
In terms of telehealth utilization (Fig. 1), there was a large difference in the percentages reporting telehealth utilization and billing before and after COVID-19. Only 14.5% of respondents reported seeing patients via telehealth prior to COVID-19 with the same number reporting billing for these visits. In contrast, 97.4% (74 respondents) of those completing the survey reported seeing patients via telehealth since COVID-19. However, only 88.2% (67 respondents) reported billing for telehealth services since COVID-19.
Table 1
Comfort level with and perceived efficiency of telehealth visits
| Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | |
|---|---|---|---|---|---|
| “I feel comfortable seeing patients via telehealth.” | 29 (37.2%) | 35 (44.9%) | 10 (12.8%) | 4 (5.1%) | 0 |
| “I see potential for telehealth to improve my daily workflow/efficiency.” | 24 (30.8%) | 32 (41%) | 16 (20.5%) | 6 (7.7%) | 0 |
| “I feel telehealth will play a role in the future of pediatric physiatry.” | 55 (70.5%) | 22 (28.2%) | 1 (1.3%) | 0 | 0 |
| “I am interested in continuing education resources related to telehealth.” | 37 (47.4%) | 32 (41%) | 8 (10.3%) | 1 (1.3%) | 0 |
A summary of the results on physician comfort with telehealth visits perceptions of impact on efficiency and workflow.
Figure 3.
Physician perceived quality of care and patient satisfaction. This figure shows the physicians’ comfort level with the quality of care provided as well as their perception of the patient satisfaction with the encounter.
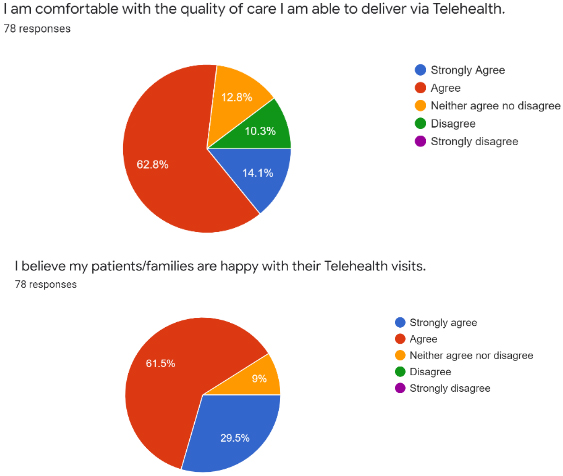
Figure 4.
Future plans for telehealth in pediatric rehabilitation. This figure concerns the respondents’ future plans for telehealth including for patients with limited mobility or access.
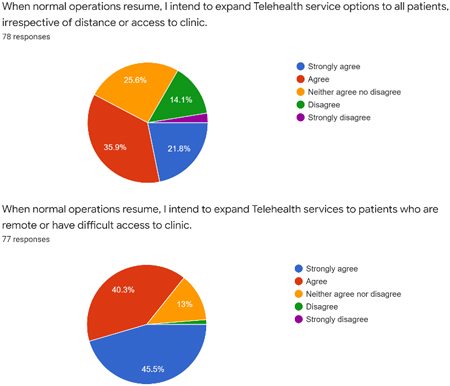
Figure 5.
Physician comfort, intention for expansion and the future of physiatric telehealth.
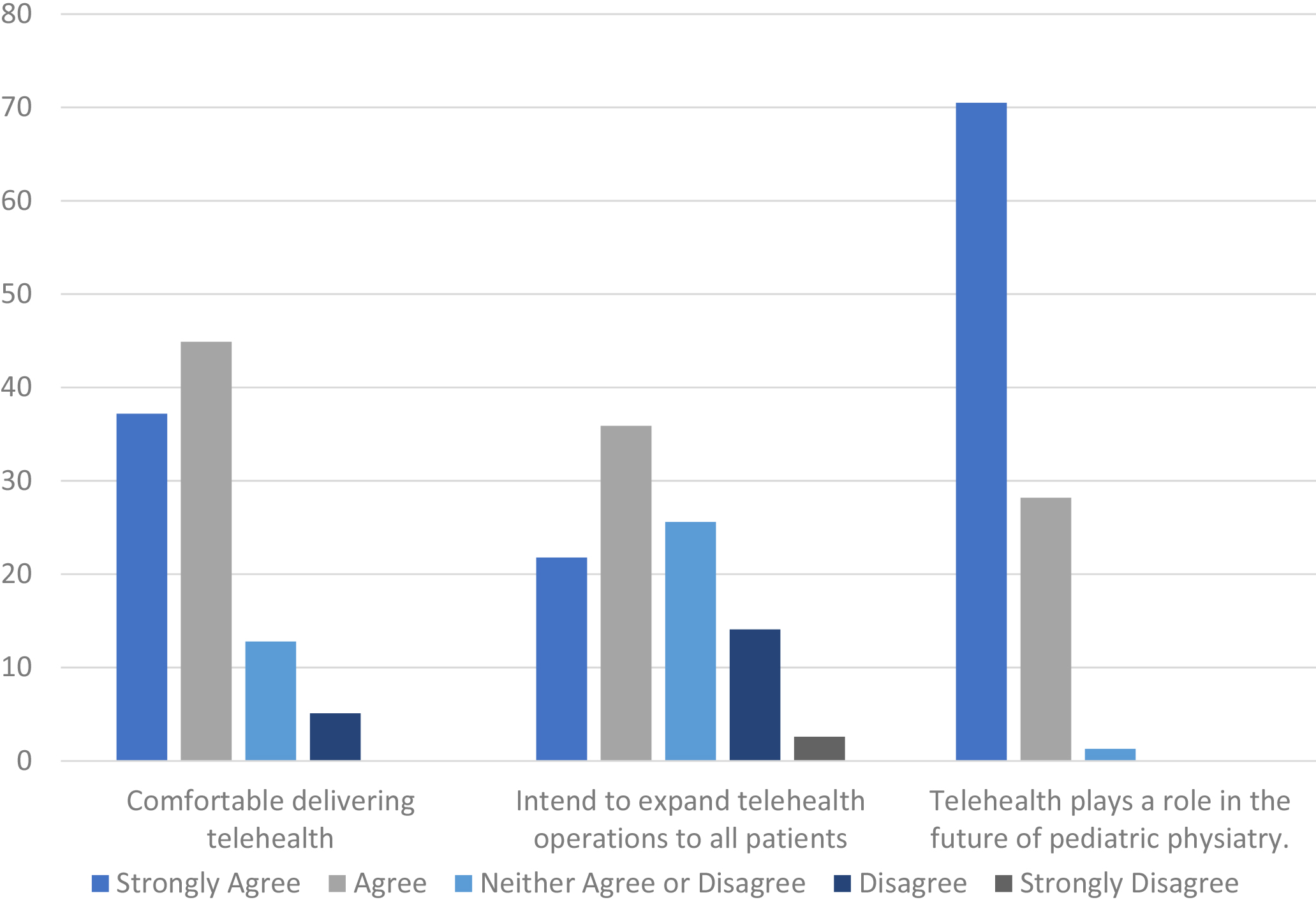
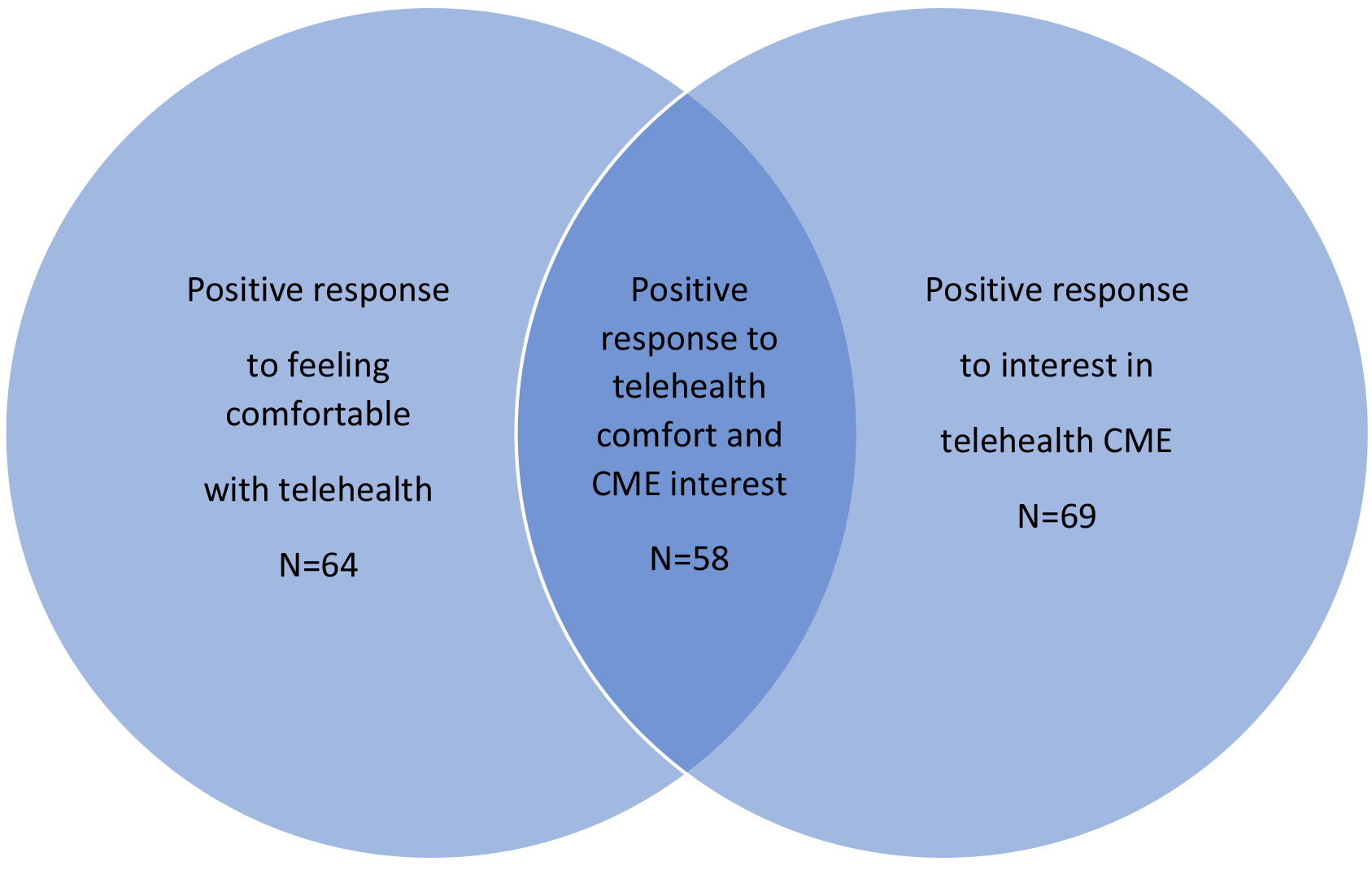
Figure 6.
Telehealth comfort and interest in continuing medical education. This figure shows the overlapping comfort with performing visits via telehealth and interest in telehealth CME.
At 82.1%, a strong majority of physicians surveyed “agreed” or “strongly agreed” with the statement “I feel comfortable seeing patients via telehealth” (Fig. 2). Only approximately 5% disagreed with the statement, suggesting they are not comfortable performing visits in this fashion. Additionally, most respondents (71.9%) “agree” or “strongly agree” with seeing potential for telehealth to improve their daily workflow and efficiency. A small percentage at 7.7% disagreed with the statement. When examined by role, 84% (57 respondents) of attending physicians had a positive response to the statement, 10% (7 respondents) had a neutral response and 6% (4 respondents) had a negative response while in fellows surveyed, 63% (5 respondents) had a positive response, 37% (3 respondents) had a neutral response and 0% had a negative response.
Concerning the future of telehealth as it relates to pediatric physiatry, in response to the statement “I feel telehealth will play a role in the future of pediatric physiatry,” 98.7% of respondents answered with a positive “agree” or “strongly agree,” with only a single neutral answer and no negative responses.
With relation to subjective quality of care, 14.1% (11 respondents) strongly agreed, 62.8% (49 respondents) agreed, 12.8% (10 respondents) neither agreed nor disagreed, 10.3% (8 respondents) disagreed and 0% strongly disagreed with the statement “I’m comfortable with the quality of care I’m able to deliver via telehealth” (Fig. 3). When this question was broken down by role, attendings pediatric physiatrists answered with a positive statement 79% (54 respondents) of the time, neutral 10% (7 respondents) of the time and negative statement 10% (7 respondents) of the time. Fellow trainees answered with positive statement responses 63% (5 respondents), neutral statement 25% (2 respondents), and negative statements 12.5% (1 respondent).
When queried about perception of patients’ and families’ satisfaction with telehealth visits, 29.5% (23 respondents) strongly agreed, 61.5% (48 respondents) agreed, 9% (7 respondents) neither agreed nor disagreed and 0% disagreed or strongly disagreed with the statement “I believe my patients/families are happy with their telehealth visits” (Fig. 3). When the responses to this statement were broken down by training level, 93% (63 respondents) of attendings answered with a positive statement, 7% (5 respondents) with a neutral statement and 0% with a negative. Fellows responded in the positive 87.5% (7 respondents) and with the remaining 12.5% (1 respondent) with a neutral response to the statement.
Two statements concerning future plans for telehealth were included in the survey: “When normal operations resume, I intend to expand telehealth services to patients who are remote or have difficult access to clinic” and “when normal operations resume, I intend to expand telehealth service options to all patients, irrespective of distance or access to clinic.” In response to the former, 45.5% (35 respondents) strongly agreed, 40.3% (31 respondents) agreed, 13% (10 respondents) neither agreed nor disagreed, 1.3% (one respondent) disagreed and 0% strongly disagreed. To the latter question, 21.8% (17 respondents) strongly agreed, 35.9% (28 respondents) agreed, 25.6% (20 respondents) neither agreed nor disagreed, 14.1% (11 respondents) disagreed and 2.6% (2 respondents) strongly disagreed (Figs 4 and 5).
Similarly, a substantial majority of respondents expressed interest in continuing education resources related to telehealth and pediatric physiatry with 88.4% agreeing or strongly agreeing with the statement “I am interested in continuing education resources related to Telehealth in pediatric physiatry.” Only 11.6% responded with a neutral or negative response regarding interest in this type of training (Fig. 6).
4.Discussion
The present survey assessed telehealth adoption in pediatric physiatry, particularly in relation to the effect of COVID-19 on telehealth utilization. The challenges to traditional office visits posed by COVID-19 led to a rapid utilization of telehealth services in an effort to maintain continuity of care [8]. These results suggest a drastic increase in the number of pediatric physiatry practices employing telehealth since COVID-19. According to these results, prior to the pandemic approximately 14.5% of those surveyed were utilizing telehealth. This number is very similar to estimates obtained from pediatricians where it was reported that 15% had utilized telehealth in the year prior to a survey completed in 2016, with slightly higher numbers for specialists and those practicing in a rural setting [9]. In an article by North, among family physicians and pediatricians in the United States, there was an increase from 11.8% using telehealth from 2016 with an increase to 91% of primary care physicians using telehealth 2 months into the pandemic [10]. According to our survey findings, telehealth adoption also drastically increased to 97.4%. This may be related to the high percentage of respondents practicing in hospitals that are part of academic medical centers, the medical fragility of the patient population or the relative paucity of pediatric physiatrists in proportion to the number of patients requiring care. As telehealth becomes more common place in pediatric physiatric practice, access to care for those previously limited by distance, transportation or schedule may improve.
Houtrow et al. [11] reported in 2010–2011 that almost 6 million children were considered disabled, comprising nearly 8% of the population. Additionally, the incidence rate of disability has increased in the period from 2001–2002 to 2010–2011 [9]. According to the American Board of Physical Medicine and Rehabilitation, since 2003, only 308 board certifications in Pediatric Physiatry have been issued [12]. Given the large disparity between the number of pediatric rehab physicians and children with disabilities, telehealth offers the possibility of efficient consultation and expert opinion for patients otherwise unable to attend a traditional office visit due to physical remoteness, financial burden, transportation, and mobility concerns. This is important as it has previously been demonstrated that medical complexity alone can be a deciding factor in unfulfilled healthcare needs [13].
In 2015, the American Academy of Pediatrics issued a policy statement on telehealth suggesting that telehealth implementation could increase access for patients and improve quality of care [14]. The policy recommended that barriers to telehealth implementation be reduced to allow for larger adoption. However, little guidance was provided on how this recommendation could be put into practice. Prior to COVID-19, there did not appear to be any large-scale trend towards telehealth adoption [15]. The reasons most commonly cited for not adopting telehealth into practice were insufficient payment, inability to bill for services and equipment costs [10, 16]. Interestingly, Sisk et al. [9] also found that the condition most likely to lead to adoption of telehealth was being paid for services, with 53% of non-users reporting they would consider using telehealth if they were adequately compensated. Relaxation of telehealth practice and billing regulations since COVID-19 as well as increased payments are likely contributors to the robust increase in telehealth adoption [17].
In spite of rapid adoption, practitioners seem to feel they are providing high quality care through leveraging telehealth with over three quarters of respondents agreeing with a statement regarding feeling comfortable with the quality of care they are able to provide and greater than nine of ten reporting their patients and patients’ families are satisfied with their telehealth visits. The statistics are in line with other pediatric research where workers reported 71% of physicians felt video visits enabled high-quality communication with patients and 97% of patients utilizing telehealth program were “highly satisfied” with the visit [18]. The results also demonstrated that attending pediatric physiatrists were more likely than fellow trainees to respond with a positive response to statements regarding feeling comfortable seeing patients via telehealth and feeling comfortable with the quality of care provided by their telehealth visits. Both attendings and trainees had a high perception of patient and family satisfaction. However, limited conclusions can be drawn from the attending-trainee comparison due to the small number of fellows completing the survey. Those surveyed also tended to think positively of telehealth’s potential on workflow and efficiency. Despite these generally optimistic perceptions, interest in telehealth-focused continuing medical education, even among those reporting feeling comfortable with telehealth visits, is high. This suggests belief that these types of visits can be further enhanced through education. This survey did not assess what specific topics within telehealth would be perceived as valuable to physicians. Further research would be helpful to elucidate the ways continuing medical education can improve patient care and satisfaction, physician efficiency and comfort, and optimize billing and documentation.
However, it is clear that the reporting community generally feels telehealth will play a future role in pediatric physiatry. Additionally, the data contributed to literature by documenting an increase in telehealth utilization from a minority of PRM physicians to near universal because of COVID-19. Though telehealth visits were initiated over a short time frame, the results suggest providers feel reasonably confident in their ability to provide adequate quality of care and perceive patient satisfaction to be high. Interest in continuing and expanding telehealth services after the challenges of COVID-19 have normalized is also substantial. This presents an opportunity to improve access to specialized pediatric care, cost efficiency, and quality while meeting the growing demand for limiting absences from work and school, improved access to providers and services and better coordination of care for patients and their families [13]. With appropriate education and continued easing of financial constraints to telehealth, this rapid increase in utilization may provide impetus for advances in remote patient visits and care [20].
4.1Limitations
This study has notable limitations. Due to the nature of the survey’s dissemination, the data is a from a convenience sample and may not be representative of the field. Though most of the participants were Pediatric Physiatrists, the sample included pooled data from trainees. No information was obtained as to why individuals utilizing telehealth were not billing during COVID-19. Minimal demographic information was included in the data. Also, it is possible respondents completed the survey more than once.
Lastly, some participants in the survey commented that a free text box would have been helpful to more clearly articulate feelings on quality and satisfaction of telehealth care provided by practitioners and experienced by patients and their families.
4.2Future directions
Perceived and discovered barriers to effective telehealth visits would have been interesting to include. Historically, inability to bill and insufficient payment were cited as barriers to telehealth adoption. In response to COVID-19, many financial barriers have been eased [4]. This could have particularly impacted pediatric physiatric practices as a disproportionately high number of patients may be receiving insurance coverage through Medicare and Medicaid.
While telehealth may have the potential to improve access to care for remote and low income populations, barriers including access to internet coverage, availability of devices and willingness to adopt telehealth by these populations should be explored.
Additionally, it may have been interesting to include age and gender demographics for the survey respondents to see what correlation, if any, this had with telehealth adoption.
Future research should examine limiting factors to implementation of telehealth in pediatric physiatry from the perspectives of both providers and patients.
5.Conclusions
Prior to COVID-19, the percentage of pediatric physiatrist employing telehealth was quite similar to pediatricians and pediatric subspecialists at approximately 15%. This number rose drastically to almost 100% in the months following. While physician comfort with telehealth, confidence in quality of care delivered and perceived patient satisfaction with telehealth visits were all high, there was still a high level of interest in telehealth specific continuing medical education. Major barriers to adoption of telehealth has generally been attributed to financial barriers, some of which were removed or improved through healthcare changes designed to improve access to care during COVID-19. Further research should be done to monitor the trends in telehealth use within pediatric physiatry as traditional visits resume and regulations change. Additionally, specific topics within telehealth should be explored to provide continuing medical education relevant to pediatric physiatry.
Conflict of interest
The authors have no conflicts of interest to disclose.
Appendix data
The Appendix files are available to download from http://dx.doi.org/10.3233/PRM-200762.
References
[1] | Wootton R, Craig J, Patterson V. Introduction to telemedicine. CRC Press; (2017) . |
[2] | Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill. (2020) Apr 2; 6: (2): e18810. doi: 10.2196/18810. |
[3] | Centers for Disease Control and Prevention, (CDC). Information for Healthcare Professionals about Coronavirus (COVID-19). (2020) ; Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/index.html. Accessed May 10, 2020. |
[4] | Centers for Disease Control and Prevention, (CDC). Outpatient and Ambulatory Care Settings: Responding to Community Transmission of COVID-19 in the United States. (2020) ; Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ambulatory-care-settings.html. Accessed May 10, 2020. |
[5] | Galea MD. Telemedicine in rehabilitation. Phys Med Rehabil Clin N Am. (2019) May; 30: (2): 473–483. doi: 10.1016/j.pmr.2018.12.002. |
[6] | Zylstra SE. Evidence for the use of telehealth in pediatric occupational therapy. Journal of Occupational Therapy, Schools, & Early Intervention. (2013) ; 6: (4): 326–355. |
[7] | Houtrow AJ, Pruitt DW. Meeting the growing need for pediatric rehabilitation medicine physicians. Arch Phys Med Rehabil. (2016) ; 97: (4): 501–506. doi: 10.1016/j.apmr.2015.09.024. |
[8] | Mehrotra A, Ray K, Brockmeyer DM. Rapidly converting to “virtual practices”: Outpatient care in the era of COVID-19. NEJM Catalyst 2020. |
[9] | Sisk B, Alexander J, Bodnar C, Curfman A, Garber K, McSwain SD, et al. Pediatrician attitudes toward and experiences with telehealth use: results from a national survey. Acad Pediatr. (2020) Jul; 20: (5): 628–635. doi: 10.1016/j.acap.2020.05.004. |
[10] | North S. Telemedicine in the time of COVID and beyond. J Adolesc Health. (2020) Aug; 67: (2): 145–146. doi: 10.1016/j.jadohealth.2020.05.024. |
[11] | Houtrow AJ, Larson K, Olson LM, Newacheck PW, Halfon N. Changing trends of childhood disability, 2001–2011. Pediatrics. (2014) ; 134: (3): 530–538. doi: 10.1542/peds.2014-0594. |
[12] | American Board of Physical Medicine and Rehabilitation. https://www.abpmr.org/. |
[13] | Kuo DZ, Goudie A, Cohen E, Houtrow A, Agrawal Carle AC, Wells N. Inequities in health care needs for children with medical complexity. Health Aff (Millwood). (2014) Dec; 33: (12): 2190–8. doi: 10.1377/hlthaff.2014.0273. |
[14] | Marcin JP, Rimsza ME, Moskowitz WB. The use of telemedicine to address access and physician workforce shortages. Pediatrics. (2015) ; 136: (1): 202–209. doi: 10.1542/peds.2015-1253. |
[15] | Kane CK, Gillis K. The use of telemedicine by physicians: still the exception rather than the rule. Health Aff (Millwood). (2018) ; 37: : 1923–1930. doi: 10.1377/hlthaff.2018.05077. |
[16] | Moore MA, Coffman M, Jetty A, Klink K, Petterson S, Bazemore A. Family physicians report considerable interest in, but limited use of, telehealth services. J Am Board Fam Med. May–Jun (2017) ; 30: (3): 320–330. doi: 10.3122/jabfm.2017.03.160201. |
[17] | Bajowala S, Milosch J, Bansal C. Telemedicine pays: billing and coding update. Curr Allergy Asthma Rep. (2020) Jul 27; 20: (10): 60. doi: 10.1007/s11882-020-00956-y. |
[18] | American Well. Telehealth index: 2019 consumer survey. Available from: https://static.americanwell.com/app/uploads/2019/07/American-Well-Telehealth-Index-2019-Consumer-Survey-eBook2.pdf. Accessed May 31, 2020. |
[19] | American Telemedicine Association. https://www.americantelemed.org/. |
[20] | Mann D, Chen J, Chunara R, Testa P, Oded Nov. COVID-19 transforms health care through telemedicine: evidence from the field. Am Med Inform Assoc. (2020) Jul 1; 27: (7): 1132–1135. doi: 10.1093/jamia/ocaa072. |
[21] | American Hospital Association. https://www.aha.org/. |




