Pediatric telerehabilitation medicine: Making your virtual visits efficient, effective and fun
Abstract
The COVID-19 pandemic has accelerated many changes in medicine including the transition from providing care in person to providing care via technology enabled telemedicine. The benefits of telemedicine visits with a Pediatric Rehabilitation Medicine (PRM) provider, also known as telerehabilitation medicine visits, are numerous. Telerehabilitation medicine provides an opportunity to deliver timely, patient and family-centric rehabilitation care while maintaining physical distance and reducing potential COVID-19 exposure for our patients, their caregivers and medical providers. Telerehabilitation medicine also allows for access to PRM care in rural areas or areas without medical specialty, virtual in-home equipment evaluation, and reduced travel burden. Because of these and many other benefits, telerehabilitation medicine will likely become part of our ongoing model of care if barriers to telemedicine continue to be lowered or removed. This paper is intended to establish a foundation for pediatric telerehabilitation medicine visit efficiency and effectiveness in our current environment and into the future.
1.Introduction
The COVID-19 pandemic has accelerated many changes in medicine including the transition from providing care in person to providing care via technology enabled telemedicine, given the need to protect the health of patients and providers [1]. Telemedicine is defined as “the use of electronic information and communications technologies to provide and support health care when distance separates participants.” [2]. Prior to the COVID-19 pandemic, universal use of telemedicine was hampered by insurance restrictions, low reimbursement, HIPPA regulations, and equipment and software constraints [3]. With the enactment of the Coronavirus Preparedness and Response Supplemental Appropriations Act, the Centers for Medicare and Medicaid Services and the Health and Human Services Office for Human Rights reduced these barriers, though only temporarily [4, 5]. The acceleration in telemedicine availability has also impacted our clinic vocabulary by inserting terms such as “virtual visit” and “telerehabilitation” and also changed our documentation requirements. Virtual interactions with patients and families, new vocabulary, and changes to documentation may cause hesitation and uncertainty about how to provide high-quality care in this unchartered territory. However, telemedicine is not new. To date, telemedicine has been tried and even regularly used in a variety of clinical situations such as stroke evaluation [6], psychiatric care [7], newborn resuscitation [8], multidisciplinary care [9], and some areas of Physical Medicine and Rehabilitation [10, 11, 12].
For families who live in rural or medically underserved areas and have access to internet and technology, telemedicine is a tool to provide access to medical care. Telemedicine can also increase patient and caregiver satisfaction through reduced travel and clinic wait time and increased potential for appointment time flexibility [13, 14]. For families of children with disabilities, virtual visits via telemedicine with a Pediatric Rehabilitation Medicine (PRM) provider, also known as telerehabilitation medicine, reduces the burden of bringing the child’s equipment to a medical appointment, finding care for other children in the home, and taking time off work [10]. There are times when a hands-on in person exam is necessary in the evaluation of our patients; however, virtual visits provide a unique opportunity to see the challenges and limitations patients experience in their homes along with the potential to develop more individualized solutions. Telehealth visits that include other community providers, such as a local therapist or durable medical equipment (DME) vendor, offer additional benefits to the child and their families, including convenience and reduced potential community exposure to COVID-19. The accelerated use of telerehabilitation medicine during the COVID-19 pandemic has highlighted the benefits virtual visits can provide in the care of our PRM patient population. If the barriers to telerehabilitation medicine are permanently removed, virtual visits may become part of our ongoing model of care and may influence the frequency of in person visits.
There are many resources available to guide some aspects of a telemedicine visit, including the American Telemedicine Association “Operating Procedures for Pediatric Telehealth” [15], an overview on adult rehabilitation telemedicine visits [16], telemedicine for pediatric gastroenterologists [17], and a how-to for the adult telemedicine musculoskeletal exam [18]. While these resources can help a PRM provider with telerehabilitation medicine visits for certain diagnoses or clinical scenarios, these resources do not provide specific guidance for pediatric telerehabilitation medicine. Therefore, the aim of this paper is to provide the PRM provider a comprehensive “playbook” to help make pediatric telerehabilitation medicine visits efficient, effective and fun. In this paper we will address: 1) pre-visit preparations for the patient/care giver and the provider, 2) tips and tricks for virtual physical exams, and 3) potential assessment tools for virtual gait and spasticity evaluations. Telerehabilitation medicine is a rapidly evolving practice for which the tests, exams, and assessments that are typically performed in person have not been validated or standardized in the virtual encounter. With guidance on patient- or caregiver-performed physical exam maneuvers, we provide a starting point for standardizing and trying to maintain the essential physical exam components. Furthermore, we provide documentation templates outlining “normal” virtual physical exams for a child and an infant.
Table 1
Video visit preparation checklist for patient and caregiver
| Preparing the virtual exam room |
| Adequate space for exam (walking, jumping, etc.) |
| Flat surface for the child to lie down during exam |
| Background noise minimized (TV, radio, etc.) |
| Other young children occupied for the duration of the exam |
| Second adult or responsible older child available for assistance |
| Items that may be needed |
| DME (wheelchair, walker, gait trainer, orthoses, splints, etc.) |
| Shoes, socks, and clothes with buttons or zippers |
| Beverage and snack such as cereal |
| Kitchen utensils |
| Favorite toys and books |
| Paper and crayons or writing utensils |
| Rubber spatula for testing reflexes |
| Favorite stuffed animal or toy for show and tell |
| Any other item related to a skill the child/teen is having difficulty with and would like evaluated |
| Preparing the child |
| Child is appropriately dressed (tank top or t-shirt and shorts for older children, easily removable clothing for younger children) |
| Child is fed, well rested, and, if needed, freshly diapered |
| Child has been told what to expect with the virtual visit |
| Technical preparation |
| Reliable internet connection (WiFi or Cellular Data) |
| Most portable, functioning device with necessary capabilities (webcam, microphone, and speakers) |
| Backup device or cell phone |
| Online patient account is set up and accessible, if available |
| Review instructions sent ahead of time for how and when to access the virtual platform |
2.Preparing for a pediatric telerehabilitation medicine visit
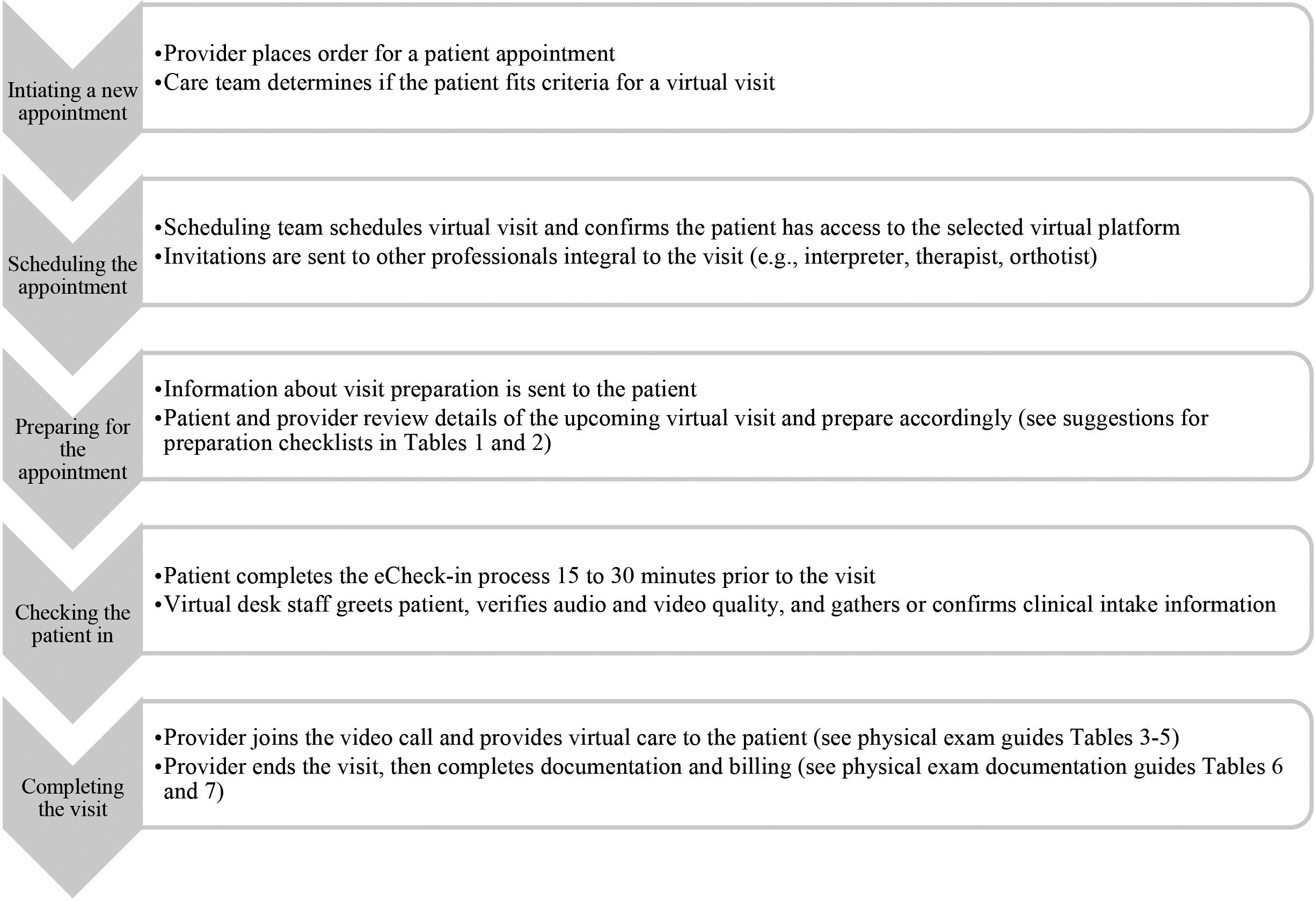
There are unique preparations for the provider as well as the patient and their caregiver in anticipation of the virtual pediatric telerehabilitation medicine encounter. The vast majority of pediatric telerehabilitation medicine visits will be performed in the patient’s home. However, regardless of the patient’s location, preparation includes gathering DME, toys, and other household items to aid in the exam, readying the patient and their caregiver(s), and navigating technical factors in using a virtual platform. Providers must be prepared to take certain steps before, during, and at the conclusion of the encounter in order to promote high-quality patient care. All of these considerations are meant to facilitate a successful interaction, foster the provider-patient relationship, and take advantage of the distinctive opportunities afforded by assessing a pediatric patient in their own environment. A video appointment workflow is outlined in Fig. 1 [19]. A preparation checklist that can be provided to the patient and family and a checklist for the provider are included in Tables 1 and 2, respectively.
Table 2
Video visit preparation checklist for provider
| Technical preparation |
| Provider training modules completed |
| Reliable internet connection |
| Functioning and reliable equipment (computer, headset, speakers, microphone) |
| Familiarity with the chosen virtual platform |
| Familiarity with how to place virtual follow-up appointment orders |
| Before the visit |
| Background is appropriate with adequate lighting |
| Professional clinical attire with visible clinic affiliated name badge |
| Minimize background noise and risk of interruptions (consider “virtual visit in progress” door sign), including cell phones, pagers, etc. |
| Prepare to share screen with results to be shared with the patient (diagnostic imaging, labs, etc.) |
| Gather toys suited to the patient’s age |
| Beginning the visit |
| Physical exam observation begins when child appears on screen |
| Welcome, introduction, and identification |
| Ensure the patient can hear you well |
| Adjust the camera so that you are at a comfortable distance – not so far that the patient can see your entire torso, but not so close that only |
| your face is visible |
| Complete virtual visit informed consent |
| Reassurance of quality, value, convenience, safety, and privacy of virtual visit |
| Orient the patient to the virtual visit, and ask if they are new to this type of care |
| Confirm accurate contact information (i.e., telephone number) as a backup plan if the video fails |
| Confirm street address of patient’s location in case of emergency during the visit |
| During the visit |
| Smile, talk slowly and in a normal volume, and look at the camera |
| Simplify and explain movements when you are doing something off camera |
| Listen and empathize as you would in an in person visit |
| Connect with the child – play peek-a-boo, share toys each of you have, give virtual high-fives, etc. |
| Improvise and be flexible when the child does not cooperate |
| Remember to stay positive and have fun |
| Closing the visit |
| Establish the plan and next steps in care |
| – Consider whether an in person visit is necessary |
| – Place orders – equipment, therapy, medication prescriptions, and consultations as appropriate |
| – Tap into your facility’s ability to send patient education materials via the EMR |
| Thank the patient and caregiver for their time and for allowing you to visit with them in their home |
| Answer any questions they may have |
| Complete documentation and billing |
Figure 1.
Video appointment workflow.
These suggestions are meant to address the general pediatric rehabilitation visit. Since not all suggestions will be appropriate for each interaction, the provider should use their clinical judgment in each case. Each child is unique in their development and personality, and just as an in person visit is tailored to best connect with that individual child, the virtual visit should be individualized as well. Furthermore, to enable continuous improvement of care provided via telerehabilitation medicine, clinicians should consider surveying patients and their caregivers regarding their virtual visit experience. For example, Gordon et al identified patient challenges and concerns via a qualitative survey regarding communication, physical exam and attention, which resulted in changes to their pre-visit interventions and provider training [20].
2.1For the patient/caregiver
To promote an efficient, productive, and child-centered interaction, there are a few considerations for the environment where the visit is conducted. The child should feel comfortable and safe, and ideally be easily entertained. The caregiver should ensure adequate floor space for the child to demonstrate gross motor skills, including sitting, creeping, walking, running, jumping, and/or skipping as appropriate for age and development. It is helpful to have a flat surface where the child can lie down or sit for examination of range of motion, strength, and postural reactions. Ideally, two caregivers will be present, one assisting with equipment and exam elements as well as audio and video operation, while the other caregiver focuses on the child and provider. It is helpful to reduce potentially distracting background noises and activities from sources such as other family members, pets and television. On the other hand, just as in the office, plan for the unexpected, such as a child’s meltdown or a chaotic environment. Always remember to thank the family for inviting you into their home.
Prepare families prior to the visit to have all equipment that needs to be evaluated during the visit on hand, such as DME. For the provider, seeing patients use their equipment in their home environment allows for assessment of fit as well as a greater understanding of current level of function along with potential barriers in that setting.
Prepare families to have other items readily available to help the child demonstrate age-appropriate gross and fine motor skills. For example, have them gather shoes and socks so the child can demonstrate donning and doffing of footwear or a beverage and snack if feeding or swallowing are concerns. For an assessment of fine motor skills, favorite toys in different sizes with features that can be pushed, pulled, opened, pieced together or otherwise physically manipulated can aid in the assessment. Clothing with buttons or zippers, books for turning pages, and paper and crayons or writing utensils can serve a similar purpose. For older children, a rubber spatula may facilitate testing reflexes. For adolescents, if there are certain activities that are a challenge, such as independence with putting their hair in a ponytail, having a hair brush and ponytail holder available to demonstrate the challenges is helpful. Some of these activities may also require the virtual visit to move to a different room of the house in order to be able to perform the activity.
Finally, it is important to prepare the child for the virtual visit. In order to transition quickly to the physical exam when the time comes, dressing infants and toddlers in easily removable clothing and older children and teenagers in shorts and a t-shirt or tank top prior to the start of the visit is recommended. In addition, suggesting that young children are rested, fed, and freshly diapered in advance of the visit helps to create a more enjoyable overall experience for the child. Preparation of the child goes beyond their physical needs. As much as possible, the caregiver should verbally prepare the child for what to expect with a live video interaction. As many children have participated in video visits with family members through various online technology platforms, most will have some familiarity with interacting with an individual using technology. If the child has a favorite toy, they should be encouraged to bring this to their virtual appointment for a “show and tell” with the provider. Ideally, this builds the child’s excitement and their eagerness to demonstrate what they can do during the visit.
2.2For the provider
The provider should take care to create a professional and inviting virtual space. This includes dressing in professional attire and maintaining a well-groomed appearance with a visible clinic name badge as one would in an in person clinic visit. The provider’s workspace should be clean, professional, quiet and well lit. Consider having a few toys on hand to share and discuss with the child. If available within your virtual platform and appropriate, an interesting virtual background, such as one including animals or nature, can help to capture the child’s attention. The ability to share a screen is a helpful option for reviewing imaging studies and test results with the patient and caregiver.
Despite the differences from an in person encounter, fostering a therapeutic provider-patient relationship remains vital. To that end, begin the encounter with a warm greeting to both the patient and the caregiver. Identify yourself, your institution, and your medical specialty, and then confirm the identity of the patient and anyone else who may be in the room with them. If not done by support staff prior to your visit, obtain a phone number to be used as a call back number if you get disconnected. Confirm the location address of the patient in the unlikely event that the child or care provider experiences a medical emergency during your visit for which emergency services needs to be notified. As a matter of informed consent, briefly discuss the uniqueness of the telerehabilitation medicine encounter, including the limitations of the physical exam when not performed in person. Patients and caregivers may have some fears or reservations about the quality of care given the limitations of a virtual visit. Take a moment to orient them to how the visit will proceed and reassure them of the benefits of the virtual visit. As with an in person visit, begin observing the child as soon as the visit begins, noting the child’s candid behaviors, which can be clues to developmental milestones and level of function.
Table 3
Multisystem child/infant physical examination guide
| System | How to examine via telemedicine | Tips and tricks |
|---|---|---|
| Vital signs | ||
| Temperature | Ask caregiver to use home thermometer. | Send caregiver instructions ahead of your appointment to complete before visit. |
| Height | Ask caregiver to measure height or review record for last measurement in office. | If available, send caregiver institutional video or written instructions on how to accurately measure an infant/child to complete before visit. |
| Weight | Ask caregiver to weigh or review record for last weight in office. | Send caregiver instructions ahead of your appointment to complete before visit. |
| Pulse | Instruct adult to find pulse, then have them count while you keep time on a stopwatch. | |
| Respiratory rate | When patient is calm, observe if rate appears fast, normal, or depressed. | Time out 15 seconds on a timer and have caregiver count the number of times the child’s chest rises and falls in that time. Multiply by 4 to determine if rate is fast, slow or normal. |
| Blood pressure | If pediatric blood pressure cuff is available at home, ask caregiver to check blood pressure. | Send caregiver instructions ahead of your appointment to complete before visit. |
| General | Observe overall appearance. | Comment on where the visit is taking place and who is present with the child. Ask caregiver what size onesie or shirt and pants they wear. |
| HEENT | Observe for dysmorphic features, facial asymmetry including ear placement, and head shape asymmetry. For infants, instruct caregiver to palpate the anterior fontanelle, sutures, and neck muscles. | Observe if child is wearing glasses, has a tracheostomy, or is using oxygen. Ask to see transverse view of head from the top when evaluating head shape. Have the caregiver place a finger on each ear to visualize displacement. |
| Skin | Observe skin when patient is undressed during musculoskeletal exam. | Make sure to ask caregiver to remove braces to observe for signs of pressure. Ask caregiver to point out any birthmarks or surgical scars. |
| Respiratory | Observe effort of breathing, sound of breathing, and if patient is cyanotic. | Comment if breathing is noisy. Ask child to pretend to blow out birthday candles or give an effortful cough to demonstrate ability to forcefully expire. |
| Cardiovascular | Ask caregiver to feel if extremities are subjectively warm or cool and if temperature is symmetric. Compare size of bare legs. Ask caregiver to push with one finger on bottom of shin and observe for depression. Inspect fingers and toes. | |
| Abdomen | Observe for distension, ask caregiver to palpate for painful areas in each of the four quadrants and comment if gastric tube is present. | Ask child if they can show you their belly button. |
| Medical equipment | Ask caregiver to show provider equipment with and without child using it, especially if something needs to be replaced. | If easily accessible, ask to see equipment not typically brought to the office such as standing frame or commode chair. |
During the encounter, be creative and engage the child as much as possible. While older patients may appreciate their provider’s head steadily centered on screen, young children might enjoy a game of on screen peek-a-boo. There is some evidence that at about 16 months of age children are able to engage more interactively with the video screen [21]. Remember to smile, speak at a normal volume and tone as you would in the in person setting, and talk to the child as well as their caregivers. Looking directly at the camera, the virtual equivalent of making eye contact with the patient, is even more important when interacting with the child. Narrate any actions you take off camera, such as looking up records on another screen or writing notes, as this could be interpreted as being distracted. Non-verbal cues remain a significant part of communication, even remotely. When children have difficulty cooperating during the visit, remain calm, empathize with the caregiver, and improvise your information gathering and exam while prioritizing the child’s best interests. Flexibility is key.
Table 4
Musculoskeletal and neurologic child physical examination guide
| System | How to examine via telemedicine | Tips and tricks |
|---|---|---|
| Neurologic | ||
| Mental status | Observe behavior, mood, attention, orientation, and level of participation during appointment. | To keep child’s attention, move around the screen, change to a virtual background, or play peak-a-boo. |
| Speech and language | Observe verbal interaction with caregiver, ask child to identify body parts, and ask them to talk to you about their favorite toy. | Have familiar items or toys with you and ask the child to name them. |
| Cranial nerves | Ask caregiver to cover one eye at a time, then show child an item to see if they can name it or count fingers. Use a colorful object and ask child to track it to evaluate eye movements. Ask child to copy your facial expressions to test strength. Ask child to protrude tongue and move back and forth. Observe if shoulder shrug is symmetric. | Try having a “staring contest” with the child or ask them to make a silly face to look for facial weakness. Observe the child eating a snack. Comment if child has observable drooling or a voice that sounds wet. |
| Gait | Observe child walking towards and away from the camera paying attention to symmetry and joint alignment. If able, ask them to walk on toes and heels. Observe for indications of weakness, sensory loss, incoordination, spasticity, malalignment, and asymmetry. | Ask the caregiver to place the camera on ground to get a better view of feet during gait. To quantify gait, consider using a rating scale suggested in the “Gait Assessment” section of this paper. |
| Balance | Instruct child to perform Romberg then ask child to stand on one leg and tandem walk. | |
| Gross motor | Observe movements during play, noting any dystonia or tremor. Ask child to run, skip, gallop, broad jump, and hop on one foot. | Play “Simon Says”. Let the child show off! Ask them to show you their favorite thing to do or how high they can jump. If able, watch the child go up and down stairs. |
| Fine motor | Observe the child’s hand as the caregiver gives them a small item such as a sticker to demonstrate pincer grasp. Ask child to trace age-appropriate shape, draw, or write. | If child is not in the mood to draw, ask caregiver to show you some art they have made. Ask child to demonstrate turning pages of a book, using a utensil, playing with Legos, buttoning buttons, or using a zipper. Offer cereal and observe how they bring it to their mouth. |
| Strength | Observe child getting off the floor, jumping, and lifting a toy over their head. Ask caregiver to perform manual muscle testing for asymmetry of strength (position arms as when performing “chicken wings” to assess shoulder abduction, arms like boxer to assess elbow flexion, etc.) in upper and lower limbs. Instruct child to perform forearm rolling (satelliting) to look for subtle hemiparesis. Observe for dynamic knee valgus during single leg squat. | Make it a game by asking child to walk like a duck or jump like a frog. In an older child, ask to march in place, pretend to kick a ball, do a wall pushup, or do triceps dips. |
| Sensation | Ask child where they feel numb or “funny”. With child’s eyes closed, instruct caregiver to touch child’s fingers and toes with a cotton ball and ask if they can feel the tickle. Ask caregiver to test temperature sensation with a cold item, or sharp and dull sensation with the two sides of a pencil. With eyes closed, ask the child to identify a small familiar object placed in their hand. Instruct caregiver how to test great toe proprioception. | |
| Coordination | Ask child to perform rapid alternating movements of hands and feet, finger-nose-finger, and heel to shin. | Ask child to perform camera-nose-camera with pointer finger. Ask caregiver to offer child cereal to observe for pincer grasp. Ask an older child to catch a ball. |
| Reflexes | Instruct caregiver how to use fingers or a rubber spatula to tap on tendons. Instruct caregiver to stroke lateral plantar aspect of foot with one finger and observe great toe movement. | Have a rubber spatula on hand to demonstrate reflexes on yourself first. |
|
Table 4, continued | ||
|---|---|---|
| System | How to examine via telemedicine | Tips and tricks |
| Muscle tone | Observe resting posture and look for posturing or co-contraction while child is engaged with an activity. Instruct caregiver how to test for ankle clonus. | Have child in view of camera as adult dons and doffs clothing to get a sense if tone is interfering. Consider adapting a physician observation scale to track over time such as the one suggested in the “Spasticity Assessment” section of this paper. |
| Musculoskeletal | ||
| Inspection | Observe for posture, limb symmetry, and skeletal deformities. | Caregiver may have to move camera to optimize angle if looking for subtle muscle atrophy or hypertrophy. |
| Palpation | Instruct caregiver to slowly and firmly palpate specific structures and report their observation while watching for pain behavior. | Ask caregiver or child to identify area of pain with just one finger. Make sure area being examined is in full view of camera. |
| Spine | Observe for scoliosis and symmetry of shoulder height, hip height, and asymmetric rib prominence. If child can follow instructions, ask them to demonstrate forward flexion, extension, and lateral bending. | Ask child to stand still in coronal and sagittal planes. If child looks asymmetric, instruct adult how to measure leg length. |
| Joint range of motion | Shoulder and elbow – Ask the child to reach for a toy or ask caregiver to assist to demonstrate full ROM in all planes. Wrist/hand – Instruct child to place hands in a prayer position or ask caregiver to passively flex and extend wrist and fingers. Hip – Instruct caregiver to demonstrate internal rotation, external rotation, and abduction while supine. Knee – Ask caregiver to demonstrate popliteal angle. Observe for recurvatum when standing and walking. Ankle – Observe alignment when standing and walking. Ask caregiver to dorsiflex ankles while knees are extended and bent. | Active ROM: Ask child to squat with heels glued to the ground, frog jump, sit cross legged, make arm circles, give examiner a virtual “high five”, and make a fist. Caregiver assisted passive ROM: Have child laying on a firm surface rather than couch. Hip ROM can be demonstrated while prone. If two caregivers are present, one can hold the camera from above and the other can demonstrate thigh foot angle while prone. Consider scoring the Beighton score: Oppose thumbs to forearm, place hands flat on the floor with knees straight and observe for elbow extension |
| Special tests | ||
| Cervical spine | Ask child to bend chin to chest and ask about symptoms. Ask caregiver to abduct arm above level of shoulder while extending shoulder, elbow, and wrist and ask about symptoms. | |
| Lumbar spine/SI | Instruct child to extend their lumbar spine and ask if this causes pain and where. Repeat while standing on one foot and ask child to localize pain if any. While supine, instruct child/caregiver with FABER and FADIR position. Instruct caregiver to perform straight leg raise. | Always examine the hip when a patient complains of back pain. FABER – Flexion, abduction, external rotation. FADIR – Flexion, adduction, internal rotation. Straight leg raise – While supine, caregiver passively lifts straight leg to observe for symptoms that travel below the knee to suggest radicular pain. |
| Shoulder | Observe for scapular winging and dyskinesis at rest and while demonstrating active range of motion. Instruct caregiver to assist in performing Neer, Hawkins, and O’Brien’s and place child’s arm in scarf position. | Neer – Position in 180 |
| Hip | While supine, instruct child/caregiver to perform FABER and FADIR position as well as Stinchfield. Instruct caregiver to position for Galeazzi test while supine and perform Ely’s test while prone. If able, child should single leg hop and indicate any area of pain. | Always examine the back when a patient complaints of hip pain. Ask caregiver if they feel or hear hip clicks when manipulating hips. Stinchfield – Resisted hip flexion with knee extended while supine to suggest intraarticular hip pathology. Galeazzi’s test – While supine, place child’s feet flat on the ground close to buttocks and observe relative knee height to check for apparent leg length discrepancy. Ely’s test – While prone, |
|
Table 4, continued | ||
|---|---|---|
| System | How to examine via telemedicine | Tips and tricks |
| flex knees to bring heels to buttocks and observe for hip flexion and assess heel to buttock distance to test flexibility of rectus femoris. | ||
| Knee | Observe knee for effusion and erythema by comparing to the opposite side. Observe for sag sign. With knee extended and quadriceps relaxed, observe adult pushing patella from side to side and palpate the patellar facets and medial and lateral femoral condyle. Instruct child to extend knee while seated to observe for J-sign. | Always examine the hip when a patient complaints of knee pain. Sag sign – While prone with knees bent 90 degrees and feet flat on the ground, observe for sagging of tibia relative to the femur to indicate PCL deficiency. J-sign – While seated with legs dangling, actively extend knee and observe for lateral shift of patella to indicate abnormal patellar tracking. |
| Ankle/Foot | When testing active ROM, consider having patient push against caregiver’s hand to elicit pain in ankle sprain. Ask child/caregiver to squeeze over the metatarsals and observe for pain and click. While child kneeling on chair, ask caregiver to perform Thompson test. | Having a child hop on the affected side may help them localize the pain. Thompson test – Squeeze calf and observe ankle motion to indicate if Achilles tendon is ruptured. |
When the history and exam are complete, partner with the patient/caregiver to determine the next steps. Consider a virtual or in person follow-up. Ensure all questions are answered. Utilize your facility’s ability to send patient education materials via the Electronic Medical Record (EMR). Complete any orders or prescriptions. End the visit with gratitude and appreciation toward the patient and the caregiver. Applaud the child for their participation. Many children will enjoy a virtual “high-five” as you say goodbye. Complete your documentation, including acknowledgement that the visit was performed virtually.
2.3Shared technical preparation
Technical preparations begin well in advance of the appointment time. For the patient and caregiver, utilizing a portable device with audio and video capabilities such as a smartphone, tablet, or lightweight laptop can allow for a more interactive visit than a stationary desk top computer, particularly during the exam. The home’s internet connection should be tested ahead of time in the area of the home where the visit will be streamed. Any troubleshooting should be done in advance. If there is no access to a reliable internet connection over WiFi or cellular data network in the home, alternative sites may include local schools, libraries, or medical facilities. To ensure video and audio quality, clinic support staff should connect with the patient 15 to 30 minutes prior to the appointment time. The check-in time leading up to the appointment can be used to verify patient identity, reason for the visit, medications, allergies, preferred pharmacy, insurance information, and contact information including a telephone number in the event the video call fails along with the patient’s current physical address in case of an emergency.
The provider should also run a trial of the platform to be used, ensuring connectivity, reliably functioning equipment, and familiarity with the interface days in advance of any upcoming video visits. Complete any provider training modules prior to your first video visit encounter to allow time for questions and trouble shooting. Identify a standard communication strategy so you are alerted when the patient is ready to be seen. Know where to get technical assistance and have the telephone number on hand.
3.Conducting the history and physical exam
Take the patient’s history as you would in a typical in person visit. Although the telerehabilitation medicine physical examination may be challenging at first, an excellent examination can be completed through observation and partnering with a caregiver or parent. Video technology provides a window into the child’s home life and environment, so use this to your advantage. The child may actually be more active in their familiar environment than in your office. Toys and snacks are readily available. All of the child’s special equipment can be viewed, allowing the provider to assess condition, fit, and how the child uses it in their home. As always, tailor your examination to why you are seeing the child and the concerns raised by the family. Table 3 outlines strategies of how to conduct a comprehensive multisystem examination through observation and with assistance of an adult. Tables 4 and 5 outline the neurologic and musculoskeletal examination for a child and an infant, respectively. Suggested formats to document child and infant “normal” virtual physical examinations are listed in Tables 6 and 7, respectively.
Table 5
Musculoskeletal and neurologic infant physical examination guide
| System | How to examine via telemedicine | Tips and tricks |
|---|---|---|
| Neurologic | ||
| Mental status | Observe behavior, mood, and attention. Notice if infant is looking at caregiver or interacting with caregiver. Ask caregiver to smile at infant to observe for reciprocal smile. | Ask the caregiver when the child last napped and if they may be tired or hungry. |
| Speech and language | Listen for coos and babbles. Ask caregiver to see if child will mimic their noises. | |
| Cranial nerves | Ask caregiver to show infant a toy and observe if they will track it in all four quadrants. Observe for facial or bulbar weakness. Observe if infant reacts to a surprising noise. | Have a toy on hand to move around your screen while watching eye movements. |
| Balance | If infant has adequate head support, ask caregiver to place in supported seated position. | |
| Gross motor | Observe movement patterns during play, noting any dystonia or tremor. | If mobile, comment on preferred mode of mobility. |
| Fine motor | Observe the infant’s hands as the caregiver gives them a small item to hold, if they come to midline and to mouth, and if infant can pass an item between hands. | Ask caregiver to place pacifier in infant’s hand to observe if they can place in mouth. |
| Strength | While infant is supine, instruct caregiver to pull infant to sit to observe head lag. While prone, observe if infant lifts head, rolls, or crawls. Observe if infant bears weight though legs when held upright. | Watching how the supine child moves while taking a history can give you information. |
| Sensation | Ask caregiver to lightly touch area of interest and observe for infant’s reaction. | While infant is distracted, ask caregiver to passively place fingers or toes in abnormal position to see if they react to normalize position. |
| Reflexes | Instruct caregiver how to use fingers to tap on tendons. | |
| Primitive reflexes | Observe how child uses a pacifier. Instruct caregiver to gently stroke cheek and observe for rooting. Instruct caregiver how to elicit Moro reflex. Observe for palmar grasp when one finger placed in palm. Observe for plantar grasp when thumb puts pressure on plantar aspect of foot. | |
| Postural reflexes | If infant has adequate head control, observe for head righting, body righting, and arm movement while being held and while sitting. | |
| Muscle tone | Observe resting posture and look for posturing or co-contraction while child is engaged with an activity. Instruct caregiver how to test for ankle clonus. | Have child in view of camera as adult dons and doffs clothing to get a sense of if tone is interfering. Consider adapting a physician observation scale to track over time such as the one suggested in the “Spasticity Assessment” section of this paper. |
| Musculoskeletal | ||
| Inspection | Observe for posture, limb symmetry, skin fold symmetry, and skeletal deformities. | |
| Palpation | Instruct caregiver to slowly and firmly palpate specific structures and report their observation while watching for pain behavior. | Ask caregiver to identify perceived area of pain with one finger. Make sure area being examined is in full view of camera. |
| Joint range of motion | Instruct caregiver to stabilize the joint of interest while demonstrating the end ROM in all planes for upper and lower limbs. Hip – Instruct adult to demonstrate internal rotation, external rotation, and abduction while supine. Knee – Ask caregiver to demonstrate popliteal angle. Foot/ankle – If feet are in an abnormal position, ask caregiver to gentle manipulate them to a normal neutral position. Ask caregiver to dorsiflex ankles while knees are extended and bent. | Active: Observe how baby moves when lying supine. Passive: Have child laying on firmer surface rather than couch. Hip ROM can be demonstrated while prone. |
| Spine | Observe the child’s preferred resting posture. Instruct caregiver to gently perform passive cervical spine ROM, then ask caregiver to move a favorite toy to observe the child’s active motion. With clothing off, observe for scoliosis when prone and when held in standing position. | |
| Special tests | ||
| Hip | Instruct caregiver to position for Galeazzi test while supine. Instruct caregiver to abduct the hips to look for symmetry. Observe for thigh skin fold symmetry. | Ask caregiver if they feel or hear hip clicks when manipulating hips. Galeazzi’s test – While supine, place child’s feet flat on the ground close to buttocks and observe relative knee height to check for apparent leg length discrepancy. |
Table 6
Child normal physical examination documentation
| Disclaimer: We chose to include physical exam maneuvers that can reasonably be completed by the patient or caregiver with provider instruction and observation. The documentation below assumes that all hands-on maneuvers typically performed by the provider are completed by the caregiver to the best of their ability. Given that the virtual physical exam will typically not be performed by a trained clinician, findings should be documented and interpreted carefully and cautiously. You may consider putting a statement at the beginning of the exam stating, “Exam was performed virtually via my observation and/or instruction with the assistance of caregiver or self-performed by the patient.” |
| Vital Signs: |
| Temperature: Temperature of ___ taken by home thermometer. |
| Height: Height today is ___ OR height was ___ at last office visit on ___ (date). |
| Weight: Weight today is ___OR weight was ___ at last office visit on ___ (date). |
| Pulse: Pulse of ___ beats per minute. |
| Respiratory Rate: Patient is breathing comfortably and rate appears normal for age. |
| Blood Pressure: Blood pressure of ___ taken by home blood pressure cuff. |
| General: Well-developed, well-nourished child in no acute distress. Accompanied by ___ in their home for this video consultation. |
| HEENT: No dysmorphic features or significant facial asymmetry. Eyes appear normal without redness. No significant head shape asymmetry or abnormality. |
| Skin: Inspection grossly negative for erythema, breakdown, or concerning lesions in exposed area. |
| Respiratory: Breathing is comfortable and regular. No dyspnea or noisy breathing noted during examination. |
| Cardiovascular: Hands and feet are warm bilaterally. No apparent lower extremity edema. No observed clubbing or cyanosis of digits. |
| Abdomen: No abdominal distension or tenderness in any of the four quadrants. |
| Medical Equipment: Orthoses and/or mobility devices fit well and appear to be in good condition. |
| Neurologic: |
| Mental Status: Alert and interactive. Age appropriate mood, affect, and behavior. |
| Speech and Language: Normal speech and thought processing for age. |
| Cranial Nerves: Monocular vision and visual tracking intact for age. Extraocular movements intact. Facial movements appear symmetric and without facial or bulbar weakness. No ptosis or tongue fasciculations. Hearing grossly intact. Accessory nerve intact bilaterally. |
| Gait: Gait is non-antalgic and reveals normal cadence and stride. No apparent rotational abnormalities of hips, knees, or feet. Toe- and heel-walking are normal. |
| Balance: Tandem gait and Romberg tests are normal. Single leg stance is normal for age. |
| Gross Motor: Able to run, skip, and gallop. Able to broad jump and hop on one foot. |
| Fine Motor: Handwriting or coloring and grasp appropriate for age. |
| Strength: All major muscle groups of the bilateral upper and lower extremities have at least antigravity muscle strength as could be tested for child’s age via video examination. |
| Sensation: Normal light touch and temperature sensation, sharp and dull differentiation, graphesthesia, and proprioception throughout upper and lower extremities as could be tested for child’s age via video examination. |
| Coordination: Coordination appears normal in upper and lower extremities. |
| Reflexes: Bilateral upper and lower extremity muscle stretch reflexes appear physiologic and symmetric. Plantar responses downgoing bilaterally. |
| Tone: Normal resting posture. No posturing or co-contracture during activity. No hypertonia or hypotonia noted in axial or appendicular musculature. No ankle clonus. |
| Musculoskeletal: |
| Observation: No gross axial or appendicular deformities. |
| Palpation: Palpation of ___ did not cause pain. |
| ROM: Joint range of motion appears pain free without significant joint contractures in the major joints of all four extremities. Beighton Score:___. |
| Spine: Range of motion appears full and pain free. No gross axial skeletal deformities such as kyphosis, lordosis, or scoliosis. |
| Special Tests: |
| Cervical Spine: No L’hermitte’s sign or indication of upper limb neural tension. |
| Shoulder: No scapular winging or dyskinesis. Negative Neer, Hawkins, O’Brien’s, and scarf tests. |
| Lumbar Spine/SI: No radiating pain with lumbar extension or straight leg raise. No pain with FABER or FADIR position. |
| Hip: No pain with FABER or FADIR position. Negative Galeazzi sign and Stinchfield. Ely test normal. |
| Knee: No knee effusions. Negative patellar apprehension and facet tenderness. Patellar tracking appears normal. |
| Foot/Ankle: No pes planus or cavus. No pain with resisted active range of motion and metatarsal squeeze. Negative Thompson test. |
Table 7
Infant normal physical examination documentation
| Disclaimer: We chose to include physical exam maneuvers that can reasonably be completed by instructing the caregiver while the provider observes. The documentation below assumes that all hands-on maneuvers typically performed by the provider are completed by the caregiver to the best of their ability. If the caregiver is having difficulty properly performing a maneuver, go ahead and move on. Consider documenting as “attempted but unable to be performed,” especially if it is a maneuver potentially critical to your evaluation. Given that the virtual physical exam will typically not be performed by a trained clinician, findings should be documented and interpreted carefully and cautiously. You may consider putting a statement at the beginning of the exam stating, “Exam was performed virtually via my observations and/or instructions with the assistance of caregiver.” |
| Vital Signs: |
| Temperature: Temperature of ___ taken by home thermometer. |
| Height: Height today is ___ OR height was ___ at last office visit on ___ (date). |
| Weight: Weight today is ___OR weight was ___ at last office visit on ___ (date). |
| Pulse: Pulse of ___ beats per minute. |
| Respiratory Rate: Patient is breathing comfortably and rate appears normal for age. |
| Blood Pressure: Blood pressure of ___ taken by home blood pressure cuff. |
| General: Well-developed, well-nourished infant in no acute distress who is accompanied by ___ in their home for this video consultation. |
| HEENT: No dysmorphic features or significant facial asymmetry. Eyes appear normal without redness. No significant head shape asymmetry or abnormality. No palpable neck masses or ridging of sutures. Anterior fontanelle is open and flat. |
| Skin: Inspection grossly negative for erythema, breakdown, or concerning lesions in exposed area. |
| Respiratory: Breathing is comfortable and regular. No dyspnea noted during examination. |
| Cardiovascular: Hands and feet are warm bilaterally. No apparent lower extremity edema. No observed clubbing or cyanosis of digits. |
| Abdomen: No abdominal distension or tenderness in any of the four quadrants. |
| Medical Equipment: Orthoses and/or mobility devices fit well and appear to be in good condition. |
| Neurologic: |
| Mental Status: Alert and interactive. Age appropriate mood, affect, and behavior. |
| Speech and Language: Vocalization normal for age. |
| Cranial nerves: Visual tracking intact for age. Extraocular movements intact. Facial movements appear symmetric and without facial or bulbar weakness. Hearing grossly intact. |
| Strength: All major muscle groups of the bilateral upper and lower extremities have normal and symmetric muscle strength and bulk as could be tested for child’s age via video examination. |
| Sensation: Reacts to light touch in all four extremities. |
| Reflexes: Bilateral upper and lower extremity muscle stretch reflexes appear physiologic and symmetric. Babinski responses are normal for age |
| Primitive Reflexes: Sucking, rooting, and Moro reflexes appear normal for age. Palmar grasp and plantar grasp reflexes appear normal for age. ATNR is not obligatory. Hands open spontaneously. |
| Postural Responses: Postural responses appear normal for age. |
| Balance: Sitting balance appears normal for age. |
| Muscle Tone: Normal resting posture. No hypertonia or hypotonia noted in axial or appendicular musculature. No ankle clonus. |
| Gross Motor: Gross motor skills appear within normal limits for age. |
| Fine Motor: Fine motor skills appear within normal limits for age. |
| Musculoskeletal: |
| Inspection: No gross axial or appendicular deformities. |
| Palpation: Palpation to ___ did not cause pain. |
| Range of motion: Joint range of motion appears pain free without significant joint contractures in the major joints of all four extremities. |
| Spine: No torticollis. Normal pain-free range of motion. No gross axial skeletal deformities such as kyphosis, scoliosis, sacral dimpling, or hair tuft noted. |
| Special Tests: |
| Hips: Negative Galeazzi sign. Hip abduction and thigh skin folds are symmetric. |
Figure 2.
Patient or caregiver stiffness/spasm assessment (Spasticity screening tool items: final version Zorowitz et al. 2017 – Am J Phys Med Rehabil) [37].
![Patient or caregiver stiffness/spasm assessment (Spasticity screening tool items: final version Zorowitz et al. 2017 – Am J Phys Med Rehabil) [37].](https://content.iospress.com:443/media/prm/2020/13-3/prm-13-3-prm200748/prm-13-prm200748-g002.jpg)
4.Assessment tools
Rating scales have been adapted or developed for telemedicine assessments, such as The Unified Parkinson’s Rating Scale (UPDRS) which is a visual rating tool to follow the longitudinal course of Parkinson disease [22]. In a 2016 systematic review, Mani et al reported telerehabilitation-based physical therapy assessments in adults with caregiver assistance or self-administered tests were generally feasible with overall good validity and reliability, except for lumbar spine posture and some orthopedic tests [23]. Currently, we are unaware of any validated measures for pediatric telerehabilitation medicine-based gait or spasticity assessments. We have identified a few assessments that are relatively simple and quick to perform, adaptable for the pediatric population and virtual platform, and can be tracked across time and multiple visits (both virtual and in person). As always, it is most important to document what is observed.
This is also an opportunity for practice improvement studies and for development and validation of new tools assessing outcomes or tracking function in this population. Tools for pediatric telerehabilitation are virtually unexplored and future research is needed to develop qualitative and quantitative assessment and outcome tools for virtual visits. Examples could include assessment of tool reliability in pediatric telerehabilitation medicine (inter-location reliability comparing tools between virtual and in person visits), ease of tool use from both the patient/caregiver and provider perspective, tool use impact on care, and as previously noted, overall satisfaction and comfort level with care provided via the virtual visit.
4.1Gait assessment
The Physician Rating Scale (PRS) is an observational clinical gait evaluation tool originally proposed to assess change in gait and joint position in children with cerebral palsy after botulinum toxin injections [24]. It has been modified by many and compared to other observational gait assessments for reliability and validity in different patient populations. It typically has high intra-observer reliability but less favorable inter-observer reliability [25, 26, 27, 28, 29, 30]. The version used in Maathuis et al. takes minimal time, is straight forward to understand and use, is observation based and can be easily documented in the patient’s EMR [27]. If choosing to use this tool, observe the child’s gait in sagittal and coronal planes. Score each side as listed and document individual section scores and total scores for each side for future comparison [27].
Figure 3.
Physician global assessment (PGA) scale for spasticity (adapted from Pascoe et al. 2015 – JAMA Derm) [38].
![Physician global assessment (PGA) scale for spasticity (adapted from Pascoe et al. 2015 – JAMA Derm) [38].](https://content.iospress.com:443/media/prm/2020/13-3/prm-13-3-prm200748/prm-13-prm200748-g003.jpg)
Other possible telerehabilitation medicine friendly gait assessments include the Edinburgh Visual Gait Analysis [31], the Modified Wisconsin Gait Scale [32, 33] and modified versions of the PRS [25, 26, 28, 29, 30, 34]. These tests, as with the proposed PRS, have variable intra and inter-observer reliability. They also are considerably longer than the proposed PRS in terms of number of items, assessment completion time, and more complex documentation.
4.2Spasticity assessment
Spasticity can be difficult to assess. In the clinic, the Modified Ashworth Scale and the Modified Tardieu Scale can be used, although these have varying levels of inter-rater reliability [35, 36]. Additionally, these tools do not account for self or caregiver assessment of spasticity. For virtual visits, spasticity can be even more challenging to assess, given the need to physically examine the child to assess the velocity dependent component. However, there are some tools that may be adapted to provide insight into the degree of spasticity and impact on function for the child.
In lieu of a hands-on physical exam for spasticity, we propose a combination of measures including a self/caregiver administered screening tool completed before the visit and a graded scale performed by the caregiver during the visit. The combination of these tools is intended to provide an overall gestalt of the patient’s spasticity and potential treatment needs. The self/caregiver administered screening tool in Fig. 2, from Zorowitz et al., is a 13-item screening tool for adults with spasticity [37]. We propose the screening tool be completed by the patient and/or caregiver to identify the impact of spasticity on their physical function and quality of life. Ideally, it would be provided to the patient/caregiver in advance of the virtual appointment with instructions to interpret the questions from the patient or caregiver perspective (i.e. your/your child’s or you/your caregiver), as appropriate. To complement this self-assessment, a modified Physician Global Assessment (PGA) scale can be used for assessment of spasticity. The PGA is a 0–4 observational scale to assess disease severity, more commonly in Dermatology and Rheumatology [38, 39, 40]. The PGA in Fig. 3 was modified with 0–4 scale definition and rating description prompts to help the caregiver assess velocity dependent movement in upper and lower limbs. While these tools have not been validated for use in this population, this combination of measures may support spasticity assessment in the virtual environment. Additional tools that could be considered include the Penn Spasm Frequency scale and the Spinal Cord Injury Spasticity Tool (SCI-SET) [41, 42].
5.Conclusion
Telerehabilitation medicine provides an opportunity to deliver timely, patient and family-centric rehabilitation care while maintaining physical distancing and reducing potential COVID-19 exposure for our patients, their caregivers and medical providers. Families may prefer the convenience of seeing their PRM provider virtually in their own home. While there are no validated tools for conducting pediatric telerehabilitation medicine visits, the compilation of patient and provider preparation instructions, tips for the virtual physical exam, and potential assessments for gait and spasticity provide a starting point for conducting meaningful virtual visits. It is not clear if the barriers for telerehabilitation medicine virtual visits will return once the COVID-19 pandemic has eased or passed. However, if telerehabilitation medicine is executed efficiently and effectively, and patients/caregivers continue to demand it, it is possible that many of the previous barriers to these types of visits will not be reinstated. Therefore, now is the time to establish a solid foundation for pediatric telerehabilitation medicine and integrate this into our standard of care for pediatric patients with disabilities.
Conflict of interest
The authors have no conflict of interest to report.
References
[1] | Reeves JJ, Hollandsworth HM, Torriani FJ, Taplitz R, Abeles S, Tai-Seale M, et al. Rapid Response to COVID-19: Health Informatics Support for Outbreak Management in an Academic Health System. J Am Med Inform Assoc. (2020) Jun 1; 27: (6): 853-859. doi: 10.1093/jamia/ocaa037. |
[2] | of Telemedicine: A guide to assessing telecommunications for health care: . Washington, DC: National Academy Press, (1996) . |
[3] | Kruse CS, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare. (2018) Jan; 24: (1): 4-12. doi: 10.1177/1357633X16674087. |
[4] | Health and Human Services [hhs.gov]. OCR Announces Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency. [updated 2020 March 17; cited 2020 May 20]. Available from: https//www.hhs.gov/about/news/2020/03/17/ocr-announces-notification-of-enforcement-discretion-for-telehealth-remote-communications-during-the-covid-19.html. |
[5] | Health and Human Services [hhs.gov]. Secretary Azar Announces Historic Expansion of Telehealth Access to Combat COVID-19. [Published 2020; March 17; cited 2020 May 20] Available from: https//www.hhs.gov/about/news/2020/03/17/secretary-azar-announces-historic-expansion-of-telehealth-access-to-combat-covid-19.html. |
[6] | Nguyen-Huynh MN, Klingman JG, Avins AL, Rao VA, Eaton A, Bhopale S, et al. Novel Telestroke Program Improves Thrombolysis for Acute Stroke Across 21 Hospitals of an Integrated Healthcare System. Stroke. (2018) Jan; 49: (1): 133-139. doi: 10.1161/STROKEAHA.117.018413. |
[7] | Shore JH. Telepsychiatry: videoconferencing in the delivery of psychiatric care. Am J Psychiatry. (2013) Mar; 170: (3): 256-62. doi: 10.1176/appi.ajp.2012.12081064. |
[8] | Mayo Clinic [mayoclinic.org]. Mayo Foundation for Medical Education and Research; c1998-2020. Telemedicine brings neonatologists to high-risk newborns’ bedside. [cited 2020; May 20] Available from: https//www.mayoclinic.org/medical-professionals/pediatrics/news/telemedicine-brings-neonatologists-to-high-risk-newborns-bedside/mac-20422782. |
[9] | Edirippulige S, Reyno J, Armfield NR, Bambling M, Lloyd O, McNevin E. Availability, spatial accessibility, utilisation and the role of telehealth for multi-disciplinary paediatric cerebral palsy services in Queensland. J Telemed Telecare. (2016) Oct; 22: (7): 391-6. doi: 10.1177/1357633X15610720. |
[10] | Gregory P, Alexander J, Satinsky J. Clinical telerehabilitation: applications for physiatrists. PM R. (2011) Jul; 3: (7): 647-56; quiz 656. doi: 10.1016/j.pmrj.2011.02.024. |
[11] | Sarfo FS, Ulasavets U, Opare-Sem OK, Ovbiagele B. Tele-Rehabilitation after Stroke: An Updated Systematic Review of the Literature. J Stroke Cerebrovasc Dis. (2018) Sep; 27: (9): 2306-2318. doi: 10.1016/j.jstrokecerebrovasdis.2018.05.013. |
[12] | Tenforde AS, Hefner JE, Kodish-Wachs JE, Iaccarino MA, Paganoni S. Telehealth in Physical Medicine and Rehabilitation: A Narrative Review. PM R. (2017) May; 9: (5S): S51-S58. doi: 10.1016/j.pmrj.2017.02.013. |
[13] | Orlando JF, Beard M, Kumar S. Systematic review of patient and caregivers’ satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients’ health. PLoS One. (2019) Aug 30; 14: (8): e0221848. doi: 10.1371/journal.pone.0221848. |
[14] | Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. (2017) Aug 3; 7: (8): e016242. doi: 10.1136/bmjopen-2017-016242. |
[15] | American Telemedicine Association [www.americantelemed.org]. Operating Procedures for Pediatric Telehealth; 2017. [updated 2018; Sept 11; cited 2020 May 20]. Available from: https//www.americantelemed.org/resources/operating-procedures-for-pediatric-telehealth/. |
[16] | Verduzco-Gutierrez M, Bean AC, Tenforde AS, Tapia RN, Silver JK. How to Conduct an Outpatient Telemedicine Rehabilitation or Prehabilitation Visit. PM R. (2020) Jul; 12: (7): 714-720. doi: 10.1002/pmrj.12380. |
[17] | Berg EA, Picoraro JA, Miller SD, Srinath A, Franciosi JP, Hayes CE, et al. COVID-19 – A Guide to Rapid Implementation of Telehealth Services: A Playbook for the Pediatric Gastroenterologist. J Pediatr Gastroenterol Nutr. (2020) Jun; 70: (6): 734-740. doi: 10.1097/MPG.0000000000002749. |
[18] | Laskowski ER, Johnson SE, Shelerud RA, Lee JA, Rabatin AE, Driscoll SW, et al. The Telemedicine Musculoskeletal Examination. Mayo Clin Proc. (2020) Aug; 95: (8): 1715-1731. doi: 10.1016/j.mayocp.2020.05.026. |
[19] | Mayo Clinic [mayoclinic.org]. Mayo Clinic Center for Connected Care. Conducting a Video Anyplace Appointment: Overview (COVID-19; Response Version). [updated 2020 May 8; cited 2020 May 20]. Available from: https//collab.mayo.edu/team/CC/_layouts/15/WopiFrame.aspx?sourcedoc=/team/CC/Operations/Synchronous/Ops%20Guide%20Links/Care%20Anyplace/Training%20Presentation/Video%20Appointment%20at%20Home%20Overview%20Epic%20Integrated.pdf&action=default. |
[20] | Gordon HS, Solanki P, Bokhour BG, Gopal RK. “I’m Not Feeling Like I’m Part of the Conversation” Patients’ Perspectives on Communicating in Clinical Video Telehealth Visits. J Gen Intern Med. (2020) Jun; 35: (6): 1751-1758. doi: 10.1007/s11606-020-05673-w. |
[21] | McClure ER, Chentsova-Dutton YE, Holochwost SJ, Parrott WG, Barr R. Look At That! Video Chat and Joint Visual Attention Development Among Babies and Toddlers. Child Dev. (2018) Jan; 89: (1): 27-36. doi: 10.1111/cdev.12833. |
[22] | Weinstein RS, Krupinski EA, Doarn CR. Clinical Examination Component of Telemedicine, Telehealth, mHealth, and Connected Health Medical Practices. Med Clin North Am. (2018) May; 102: (3): 533-544. doi: 10.1016/j.mcna.2018.01.002. |
[23] | Mani S, Sharma S, Omar B, Paungmali A, Joseph L. Validity and reliability of Internet-based physiotherapy assessment for musculoskeletal disorders: a systematic review. J Telemed Telecare. (2017) Apr; 23: (3): 79-391. doi: 10.1177/1357633X16642369. |
[24] | Koman LA, Mooney JF, Smith B, Goodman A, Mulvaney T. Management of cerebral palsy with botulinum-A toxin: preliminary investigation. J Pediatr Orthop. Jul-Aug (1993) ; 13: (4): 489-95. doi: 10.1097/01241398-199307000-00013. |
[25] | Brown CR, Hillman SJ, Richardson AM, Herman JL, Robb JE. Reliability and validity of the Visual Gait Assessment Scale for children with hemiplegic cerebral palsy when used by experienced and inexperienced observers. Gait Posture. (2008) May; 27: (4): 648-52. doi: 10.1016/j.gaitpost.2007.08.008. |
[26] | Dickens WE, Smith MF. Validation of a visual gait assessment scale for children with hemiplegic cerebral palsy. Gait Posture. (2006) Jan; 23: (1): 78-82. doi: 10.1016/j.gaitpost.2004.12.002. |
[27] | Maathuis KGB, van der Schans CP, van Iperen A, Rietman HS, Geertzen JHB. Gait in children with cerebral palsy: observer reliability of Physician Rating Scale and Edinburgh Visual Gait Analysis Interval Testing scale. J Pediatr Orthop. May-Jun (2005) ; 25: (3): 268-72. doi: 10.1097/01.bpo.0000151061.92850.74. |
[28] | Mackey AH, Lobb GL, Walt SE, Stott NS. Reliability and validity of the Observational Gait Scale in children with spastic diplegia. Dev Med Child Neurol. (2003) ; 45: (1): 4-11. |
[29] | Rathinam C, Bateman A, Peirson J, Skinner J. Observational gait assessment tools in paediatrics – a systematic review. Gait Posture. (2014) Jun; 40: (2): 279-85. doi: 10.1016/j.gaitpost.2014.04.187. |
[30] | Wren TAL, Rethlefsen SA, Healy BS, Do KP, Dennis SW, Kay RM. Reliability and validity of visual assessments of gait using a modified physician rating scale for crouch and foot contact. J Pediatr Orthop. Sep-Oct (2005) ; 25: (5): 646-50. doi: 10.1097/01.mph.0000165139.68615.e4. |
[31] | Bella GP, Rodrigues NBB, Valenciano PJ, Silva LMAE, Souza RCT. Correlation among the visual gait assessment scale, Edinburgh visual gait scale and observational gait scale in children with spastic diplegic cerebral palsy. Rev Bras Fisioter. (2012) ; 16: (2): 134-40. |
[32] | Guzik A, Drużbicki M, Kwolek A, Przysada G, Bazarnik-Mucha K, Szczepanik M, et al. The paediatric version of Wisconsin gait scale, adaptation for children with hemiplegic cerebral palsy: a prospective observational study. BMC Pediatr. (2018) Sep 15; 18: (1): 301. doi: 10.1186/s12887-018-1273-x. |
[33] | Guzik A, Drużbicki M, Wolan-Nieroda A, Przysada G, Kwolek A. The Wisconsin gait scale – The minimal clinically important difference. Gait Posture. (2019) Feb; 68: : 453-457. doi: 10.1016/j.gaitpost.2018.12.036. |
[34] | Gor-García-Fogeda MD, Cano de la Cuerda R, Carratalá Tejada M, Alguacil-Diego IM, Molina-Rueda F. Observational Gait Assessments in People With Neurological Disorders: A Systematic Review. Arch Phys Med Rehabil. (2016) Jan; 97: (1): 131-40. doi: 10.1016/j.apmr.2015.07.018. |
[35] | Gracies JM, Burke K, Clegg NJ, Browne R, Rushing C, Fehlings D, et al. Reliability of the Tardieu Scale for assessing spasticity in children with cerebral palsy. Arch Phys Med Rehabil. (2010) Mar; 91: (3): 421-8. doi: 10.1016/j.apmr.2009.11.017. |
[36] | Mutlu A, Livanelioglu A, Gunel MK. Reliability of Ashworth and Modified Ashworth scales in children with spastic cerebral palsy. BMC Musculoskelet Disord. (2008) Apr 10; 9: : 44. doi: 10.1186/1471-2474-9-44. |
[37] | Zorowitz RD, Wein TH, Dunning K, Deltombe T, Olver JH, Davé SJ, et al. A Screening Tool to Identify Spasticity in Need of Treatment. Am J Phys Med Rehabil. (2017) May; 96: (5): 315-320. doi: 10.1097/PHM.0000000000000605. |
[38] | Pascoe VL, Enamandram M, Corey KC, Cheng CE, Javorsky EJ, Sung SM, et al. Using the Physician Global Assessment in a Clinical Setting to Measure and Track Patient Outcomes. JAMA Dermatol. (2015) Apr; 151: (4): 375-81. doi: 10.1001/jamadermatol.2014.3513. |
[39] | Rohekar G, Pope J. Test-retest reliability of patient global assessment and physician global assessment in rheumatoid arthritis. J Rheumatol. (2009) Oct; 36: (10): 2178-82. doi: 10.3899/jrheum.090084. |
[40] | Wells GA, Boers M, Shea B, Brooks PM, Simon LS, Strand CV, et al. Minimal disease activity for rheumatoid arthritis: a preliminary definition. J Rheumatol. (2005) ; 32: (10): 2016-24. |
[41] | Mills PB, Vakil AP, Phillips C, Kei L, Kwon BK. Intra-rater and inter-rater reliability of the Penn Spasm Frequency Scale in People with chronic traumatic spinal cord injury. Spinal Cord. (2018) Jun; 56: (6): 569-574. doi: 10.1038/s41393-018-0063-5. |
[42] | Adams MM, Ginis KAM, Hicks AL. The spinal cord injury spasticity evaluation tool: development and evaluation. Arch Phys Med Rehabil. (2007) Sep; 88: (9): 1185-92. doi: 10.1016/j.apmr.2007.06.012. |




