How Information Affects Patients with Parkinson’s Disease: A Scoping Review of the Literature
Abstract
Background:
Patients with Parkinson’s disease (PD) need to receive adequate information to manage their disease. However, little is known about how information provision affects patients.
Objective:
To conduct a scoping review of the literature on the relationship between content, timing, manner of delivery, and source of PD-specific information on the one hand, and patient outcomes on the other.
Methods:
All literature reporting about original data and published until April 2024 in peer-reviewed journals was searched in MEDLINE (Ovid), Embase (Ovid) and PsychInfo (Ovid). Subsequently, data were extracted and synthesized.
Results:
40 publications describing the effects of information provision or patients’ evaluation thereof were retrieved. Four categories of patient outcomes were described, namely 1) evaluation and experience of information provision; 2) physical functioning; 3) psychosocial well-being; and 4) quality of life. In intervention studies, patients generally valued the provided information. Findings from cross-sectional and qualitative studies showed the importance of tailoring information to individuals’ needs and capabilities. Due to variation in study designs and outcomes, no unambiguous conclusions could be drawn regarding the relationship between information and outcomes.
Conclusions:
This scoping review identified how PD patients acquire information and revealed a lack of systematic research into the effect of information on patient outcomes. Future studies should assess 1) what information is currently provided by clinicians; 2) what additional information might be beneficial to provide; and 3) how information can be effectively aligned to benefit patients. This will eventually yield insight into how information might optimally empower PD patients.
INTRODUCTION
Parkinson’s disease (PD) is a chronic progressive neurodegenerative disorder, which can lead to severe disability and irreversibly alters patients’ lives over time [1, 2]. PD patients need disease-specific information to manage their day-to-day disease throughout their illness [3, 4].
Clinicians provide patients with relevant information, to support them in anticipating possible symptoms and making well-considered (treatment) choices [5]. However, 30–46% of PD patients have reported feeling sub-optimally informed throughout their disease course [6–11].
Various factors may contribute to patients feeling sub-optimally informed. First, patients’ information needs and processing capacity vary and therefore the general content and manner of information provision have to be personalized [12]. Second, the relevance of information varies between PD patients and over time, due to heterogenic symptom manifestation and unpredictable progressive nature of the disease [13]. Last, PD patients can acquire information via different sources (e.g., internet, social media, books, or other healthcare providers), which are abundant, not aligned and which may present contradictory information, potentially leading to confusion [13–15].
Previous research into PD patients’ experiences regarding information provision reveals their need for information and patient education [16]. Specifically, the content, timing, manner, and source of information provision might affect various patient outcomes (e.g., information recall, psychosocial functioning, and satisfaction) [11, 17]. Overall, patients who feel well informed are known to feel less anxious, have better information recall, and report a higher health-related quality of life [18, 19]. PD patients are expected to self-manage their disease and are thus dependent on adequate information.
However, a comprehensive overview of the associations between various aspects of information provision regarding PD and patient outcomes is missing. Therefore, it is currently unknown how disease-specific information should be provided to optimally support patients. This is problematic, as PD patients are expected to self-manage their disease and thus are dependent on adequate information. It is necessary to get better insights into the effects of information provision (e.g., the content, timing, manner, and source of information) to PD patients, to ultimately empower the patient in their disease management. Therefore, we conducted a scoping review of the literature, to establish the available evidence on PD-specific information provision in relation to PD patient outcomes.
METHODS
Search
A comprehensive search was performed in the databases: Medline (Ovid), Embase (Ovid), and PsychInfo (Ovid), initially from inception to 1 October 2022. The search was updated on 5 April 2024. The PRISMA-ScR guidelines for conducting and reporting scoping reviews were used (Appendix A) [20]. The search included controlled terms and free text terms: 1) Parkinson’s disease; 2) information, education, (e–)consultation, healthcare professional, clinician; 3) inform, search, provide; and 4) support, disclose, explain, consult. The search was limited to publications in English, including original data. The full search strategies can be found in appendix B. Duplicate articles were excluded by an in-house made deduplication tool. The review was registered in the OSF database (osf.io/9f6k3).
Publication selection
Two out of three authors (EK, LV, MH) independently screened and discussed all titles and abstracts, using Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia). Primary studies reporting on 1) patients with idiopathic Parkinson’s disease, 2) who acquired any disease-specific information and 3) any patient outcomes were included. Publications reporting on studies with non-human subjects, case reports, without available full text, or published without peer review were excluded. Discrepancies between screening authors were solved through discussion. Hereafter, pairs of the same three authors (EK, LV, MH) screened the full texts of all included publications, using a narrower scope. Included publications: 1) specified the studied information (which could include any aspect or intervention related to information provision or gathering) in the aims, methods, or main themes (the latter for qualitative research); 2) described a relation between the specified aspects of information and any patient outcomes; and 3) reported on outcomes for PD patients specifically. Any discordances were discussed and resolved in consensus meetings. If consensus could not be reached, a third researcher (MH) was consulted. Reference lists of all included publications were screened for additional relevant publications.
Extraction and narrative synthesis
One reviewer (EK) performed data extraction. Extraction criteria were defined during an iterative process with four researchers (EK, LV, MH, JD). Publications were categorized into three main types based on study design: 1) intervention studies; 2) cross-sectional survey studies; and 3) qualitative studies. The extracted data entailed author, year of publication, reported study aim(s), specific study design, sample characteristics, and setting. Moreover, for each type of publication, relevant findings were extracted. If the aims of included studies partially overlapped with our review aims, we extracted both the general study aims and review-specific aims. For intervention studies, extracted data entailed a description of information provision in the intervention and its relation to patient outcomes. For cross-sectional survey and qualitative studies, findings on the relation between (aspects of) information and outcomes from the perspective of patients were extracted. If multiple publications presented data collected in the context of one study, these data/findings were combined. All extracted data were reviewed and discussed between four researchers (EK, LV, MH, JD). Afterwards, one reviewer (EK) further categorized the extracted data based on study type, type of information and patient outcomes, and discussed the results with the other authors (LV, MH, JD).
RESULTS
Study characteristics of included publications
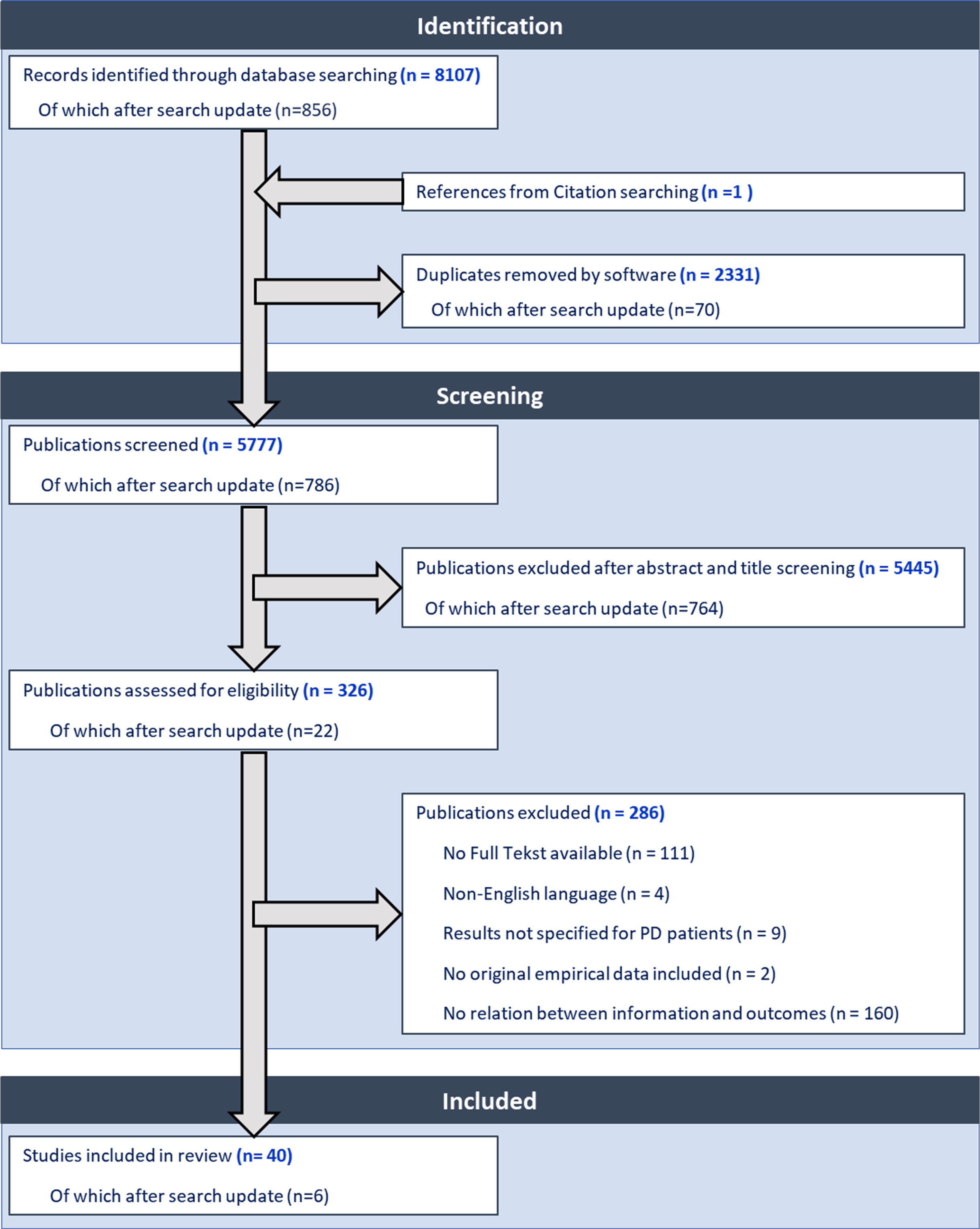
Forty publications were included, reporting results of 38 studies: 27 intervention studies, 4 cross-sectional survey studies, and 9 qualitative studies. Figure 1 shows the publication selection flowchart. Sample size of included publications varied widely (i.e., Intervention studies: N = 10–525; Cross-sectional survey studies: N = 422–1775; Qualitative studies: N = 9–55). One study was published in 1994 and all other studies between 2003 and early 2024. An overview of study characteristics and main findings per study are provided in Supplementary Tables 1a–c (Intervention studies), Supplementary Table 2 (Cross-sectional survey studies), and Supplementary Table 3 (Qualitative studies).
Fig. 1
Selection flowchart.
Assessed patient outcomes
We grouped patient outcomes into four main categories (Table 1). In our narrative synthesis below, the relations between different aspects of disease-specific information with these four categories of patient outcomes are described consecutively.
Table 1
Patient outcomes grouped in four main categories
| # | Patient outcome category | Included outcomes |
| 1 | Evaluation and | –Evaluation of information |
| experiences of | –amount | |
| information provision | –disease-specific topics | |
| –timing | ||
| –overall | ||
| –Experienced barriers/ facilitators in care-management | ||
| –understanding/knowledge | ||
| –involvement in decision making | ||
| –coping behavior | ||
| –Satisfaction with care | ||
| 2 | Physical functioning | –Activity of daily living (ADL) |
| –Motor performance | ||
| –Physical activity | ||
| –Medication use | ||
| 3 | Psychosocial well-being | –Mood |
| –Depression | ||
| –Need for psychosocial help | ||
| –Non-motor aspects of PD | ||
| –Optimistic expectations regarding oneself | ||
| –Sense of coherence | ||
| –Psychological impact of genetic testing | ||
| 4 | Quality of life (QoL) | –PD specific quality of life |
| –General quality of life |
Narrative synthesis
Intervention studies on the relation between information and patient outcomes
Intervention studies (N = 22) assessed various aspects of disease-specific information, which were grouped into three types: 1) group-based patient education programs (n = 11) (Supplementary Table 1a); 2) information provision to individuals (n = 9) (Supplementary Table 1b); and 3) information provided in combination with medical treatment to study placebo effects (n = 2) (Supplementary Table 1c).
Group-based patient education programs
Twelve publications reported on group patient education programs (Supplementary Table 1a), of which seven (N = 16–167) concerned variations of the same patient education program [21–27]. This program was first published in 2006 as ‘called EduPark’ [21] and later renamed ‘Patient Education Program Parkinson (PEPP)’. This patient education program consisted of 7 or 8 live group sessions of 90 minutes aimed at empowering patients in living with PD. Discussed information topics regarded 1) self-monitoring of symptoms; 2) stress, anxiety, and depression; 3) (social) support; and 4) future life with PD. The five other intervention studies (N = 22–181) deviated from EduPark/PEPP, e.g., because meetings were optional for patients, or because the content of information differed [16, 28–31]. Intervention studies assessed the impact of information within patient education programs on all four categories of outcomes, i.e., patients’ evaluation and experiences of information, physical functioning, psychosocial well-being, and their qualityof life.
Regarding patients’ evaluation and experiences of information, two publications testing PEPP in single groups reported that patients (N = 16 and N = 151) evaluated the provided information overall positively, and that respectively 54% and 100% experienced an improved understanding of PD [21, 22]. In a publication testing different education interventions on oral health, all patients’ knowledge unexpectedly decreased, rather than increased over time (p < .001). Patients who received pictorial information had higher knowledge than patients who only received lecturers or demonstrations (M diff in change = 8.8%, p = .03) [31]. In one publication that qualitatively explored patients’ evaluation regarding the provided information, patients (N = 25) reported appreciating the fruitful exchange of knowledge and experiences within the group, while also realizing that symptoms varied considerably between participants [26]. Regarding the timing of the provided information, patients thought it would be most useful within one year after diagnosis [26].
Regarding patients’ physical functioning, three publications reported on the impact of information in multi-session group patient education programs on patients’ daily physical impairments and their motor performance. Of the three publications on patients’ activities of Daily Living (ADL), two randomized controlled trials (RCTs; N = 120 and N = 44) reported improvements in the intervention vs. worsening the control group (M change on UPDRS-II = –0.96 vs. 1.37 points, p < 0.01, and –5.0 vs. 0.4 points, p < 0.001), while one publication that tested a PEPP in a single group (N = 22) reported no significant change (UPDRS-II) [28–30]. Patients’ motor performance (UPDRS-III) was assessed in these same three studies, of which one RCT (N = 44) reported larger improvements in the intervention vs. the control group (M change = –12.8 vs. –1.1, p < 0.001), eight weeks after the intervention. One publication reported that an oral health educational intervention led to reduced amounts of dental plaque (F = 11.5, p < 0.001) [31]. Two other publications (RCT, N = 120 and single group, N = 22) reported insignificant results [28–30].
Regarding patients’ psychosocial well-being, five publications reported improvements of patients’ mood, of which four (testing mood before and after each session in single group designs (N = 15–61)) reported temporary changes after each session (mean pre and post session changes on mood 100-VAS: between 5.6 and 11.2, p < 0.05). One RCT (N = 44) reported a sustained improvement in the intervention vs. control group on mood after 8 weeks (M change 100-VAS = 20.3 vs. 0.2, p < 0.001) [21–24, 28]. Five publications assessed patients’ need for psychosocial help, of which two RCTs (N = 57 and N = 61) and one study with a single group design (N = 16) reported insignificant results [21, 23, 25]. The other two single-group design studies (N = 151 and N = 181) reported a decreased need for psychosocial help (M change on BELA-P-k = –5.7, p < 0.001) or psychosocial impact (M change on SCOPA-PS = –0.8, p < 0.001) [16, 22]. Two publications assessed patients’ non-motor disease aspects (UPDRS-I), of which one RCT (N = 120) reported improved non-motor aspects in the intervention vs. worsening in the control group (M change = –0.4 vs. 0.4, p < 0.01), while the other study with a single group design (N = 22) reported insignificant results [29, 30]. All six publications (three RCTs (N = 67–161) and three single group designs (N = 16–151)) studying the effects of a patient education program on patients’ feelings of depression, reported insignificant results [21–25, 30].
Regarding patients’ quality of life (QoL), five publications reported significant improvements over time. Two of these (RCTs, N = 61 and N = 67) found improvements in the intervention vs. worsening in the control group directly after the intervention (M change on PDQ-39-SI = 3.1 vs. –1.8, p < 0.05 (authors used reversed scoring) and –4.3 vs. 3.7, p < 0.1) [23, 25]. In one of these, patients’ QoL was also assessed three months later, showing sustained improvement in QoL in the intervention group vs. worsening in the control group (M change = –3.6 vs. 3.4, p < 0.05). In one RCT (N = 44) patients’ QoL, assessed eight weeks after the intervention, had improved more in the intervention vs. the control group (M change on PDQ-39 = –14.0 vs. –0.1, p < 0.001) [28]. Two other publications with a single-group design (N = 41 and N = 151), of which one tested PEPP in clinical practice, also found improved QoL directly after the intervention (M change on PDQ-39-SI = 3.8, p < 0.05 (authors used reversed scoring) and PDQ-8 = –3.8, p < 0.001) [16, 24]. The study testing PEPP in clinical practice reported that patients’ QoL returned to base level after six months [24]. Four publications (N = 16–151), including one RCT, reported insignificant intervention effects on QoL [21, 22, 29, 30].
Information provision to individuals
Thirteen publications reported on the relation between information provision to individual patients and their outcomes (Supplementary Table 1b). Participating patients received information on their disease progression so far, genetic counseling, treatment options, and/or overviews of possible health services. Information was offered in booklets, on video, or through exclusive internet websites [32–41]. Six studies provided verbal information to patients, for example via (online) consultations [33, 38, 40, 42–44]. The thirteen publications reported on various patient outcomes, mainly regarding patients’ evaluation and experiences of information, physical functioning, psychosocial well-being, and quality of life. Regarding patients’ evaluation and experiences of information provision, four publications studied patients’ overall evaluation and understanding of the provided information. Provided information entailed a table-based education module on medication (single group design, N = 47); a dashboard visualizing patients’ disease trajectory, to be reviewed by patients and their clinicians during consultations (single group design, N = 17); an home-based personalized information visit regarding PD and self-help organizations (RCT, N = 53); and an information package (single group design, N = 108). All four reported positive overall experiences, and two additionally reported an improved understanding [32, 36, 37, 41]. Moreover, one publication (randomized pilot, N = 525) reported more patients being satisfied with genetic counseling received from local clinicians with limited experience, compared to with genetic counselors with extensive experience (93% vs. 86%, p = 0.05) [43]. Regarding patients’ physical functioning, one out of six publications reported negative effects. In this RCT (N = 84), patients received a personalized educational home visit with written tailored information regarding PD and self-help organizations. Patients who received this information were more likely to have reported falls in the following year compared to the control group (OR 10.89, p < 0.05) and reported feeling more disabled one year after the intervention (which was not compared to the control group (M change on NEADL = 2.48, p < 0.01)) [33]. One publication reported about a fall prevention intervention (single group, N = 15), including individualized recommendations during virtualized home-safety tours. The majority of recommendations were met after two weeks (87% fully met, 9% partly met, 2% not met) and after four months (91% fully met, 9% partly met) [44]. Patients’ motor performance (UPDRS-III) was assessed in three publications, of which two RCTs (N = 15 and N = 69) reported insignificant results of information provision regarding sleep hygiene and the continuous dopaminergic theory [38, 40]. In the other RCT (N = 290), patients received tailored written information packages and exercise recommendations. Compared to the control group, there was an improved self-reported motor performance in the intervention group (M change on UPDRS = 2.5, p < 0.5), an improved self-reported amount of exercise (M change = 9.4%, p < 0.05), and lower reported daily levodopa dose (M change = –62.1 mg, p < 0.05) [34]. Two other studies assessed medication adherence, of which one RCT (N = 69) reported a median difference in timing adherence pre to post intervention between the two groups of 23.1% in favor of the intervention group (p < 0.001) after education upon the continuous dopaminergic theory. One other study (single group design, N = 92) reported insignificant results after one-time education regarding medication adherence by a pharmacist during consultations at the neurology outpatient clinic [38, 39].
Two publications assessed patients’ psychosocial well-being, of which one (single group design, N = 30), reported that most patients felt supported by online medication instructions to reduce their burden (63%) [42]. The other publication (randomized pilot, N = 525), found no significant impact of genetic counseling on patients’ psychological well-being [43]. Three publications assessed patients’ quality of life (QoL), of which one reported an improvement (non-specified by authors) three months after patients (single group design, N = 92) received one-time education by a pharmacist during consultations at the neurology outpatient clinic. The other two RCTs (N = 15 and N = 69) reported insignificant results regarding patients’ QoL after information provision regarding respectively sleep hygiene and the continuous dopaminergic theory [38–40].
Information provided in combination with medical treatment changes
Two publications (both double-blinded RCTs) reported on the impact of providing accurate vs. inaccurate information regarding the applied therapy (i.e., levodopa dosage or deep brain stimulation (DBS) settings) on patients’ motor performance (Supplementary Table 1c). In one publication, patients (N = 45) who received half a dose of levodopa while being told they had received a full dose, improved more in motor performance compared to the group that was aware of their half dose. Motor performance in this study was clinically assessed pre and post medication using the UPDRS-III (M change = 62% vs. 44%, p < .001) and using the number of finger flexions to lift a weight per minute (M change = 29% vs. –13%, p < 0.5) [45]. In the other publication (N = 10), in which DBS settings (i.e., turned on vs. turned off) were tested, patients who were unaware of their DBS turned off, had lower UPDRS-III scores (implying better motor functioning) than patients who were aware of these settings (M change between intervention vs. control = –3.1, p < 0.05) [46].
Cross-sectional studies on the relation between patient-perceived information and patient outcomes
Supplementary Table 2 shows the four publications regarding three studies presenting cross-sectional survey data. All describe patient satisfaction with the perceived amount of information provided by various types of clinicians in various types of consultations (e.g., during decision-making or during diagnostic consultations) [9–11, 47]. In one publication (N = 422) patients reported more often to have received insufficient information from general practitioners than from neurologists (30.6% vs. 16.2%, p < 0.001) [9]. In another publication (N = 726), patients were more satisfied with the information they received from PD specialists than from general neurologists (72.5% vs. 40.9%, p < 0.001) [10]. Last, two publications reporting about one study found that more perceived information in (diagnostic) consultations was associated with higher satisfaction with care (r = 0.24, <0.001 and r = 0.29, p < 0.001) [11, 47].
Qualitative studies on the relation between patients’ experiences regarding information provision and care
Nine qualitative publications describe how patients with a disease duration up to 24 years experienced the impact of various types of information (e.g., from various clinicians, from the internet) on their daily lives (Supplementary Table 3) [48–56]. Patients’ evaluation of the amount of provided information varied widely. Patients who perceived too little information felt hampered in self-managing their disease, for example because receiving insufficient information about treatment options was experienced as a barrier to reach a decision [48–50, 52, 54, 55]. Four studies reporting about interviews with Canadian and European patients in 2016, 2017, and 2023 explicitly found that patients consulted other information sources (e.g., the internet), which was experienced as dissatisfying. Patients ascribed their dissatisfaction to the lacunas in information provided by clinicians, which led them to search for scattered information [48, 49, 52, 56]. Too much perceived information, on the other hand, was reported to overwhelm patients and hamper their ability to cope with the received bad news of PD and the subsequent self-management of their disease [51, 55]. One ethnographic study reported how patients felt supported in their decision making through online informational answers from other patients on a forum regarding deep brain stimulation [53].
DISCUSSION
This scoping review highlights that research on the impact of information provision on patients with PD is highly variable and scattered. Our synthesis underlines that the content, timing, manner of delivery, and source of information might determine how information affects patients in terms of their evaluation and experiences of information, physical functioning, psychosocial well-being, and quality of life. Included publications were highly heterogenic, which made it challenging to draw consistent conclusions. Variation in methodologies, outcome measures, and participant characteristics limited the comparability of findings, emphasizing the need for cautious interpretation and recognition of the need for systematicresearch.
This review identified two main sources from which patients acquire information: provided by clinicians during clinical encounters, and through complementary means such as online sources or education programs. Concerning clinicians’ information provision, this review shows that patients feel more empowered in managing their disease on a day-to-day basis when clinicians provide information tailored to their individual and current needs. Cross-sectional survey studies unanimously found that patients who reported receiving more information during clinical encounters were more satisfied [9–11, 47]. However, more is not always better, as qualitative studies emphasized patient preferences for tailored amounts of information [48–51, 55]. It was found that if patients perceived information provided during clinical consultations as insufficient, this hampered them in making decisions and plans, while abundant information overwhelmed them and hindered them in coping with PD. All these publications focused on patients’ perceived content of information, while various studies in other specialties (e.g., oncology, primary care, cardiology) indicate that patient perceptions of information provision do not accurately reflect the actual provided information. Indeed, patients generally misunderstand or forget 30–80% of information provided by clinicians [57, 58]. PD patients might be specifically prone to impaired understanding since information about PD is often complex, overwhelming, and multi-interpretable due to unpredictable symptom manifestations, treatment reactions, and disease progression [59]. Moreover, clinicians feel they lack skills to adequately tailor information to patients’ needs and abilities [57, 60]. Unfortunately, clinical guidelines regarding PD lack recommendations for clinicians on how to optimally educate patients [25]. It is known that effective information provision is not only determined by the content of information but even more by how such information is provided [60]. A recent scoping review showed that clinicians can use various communication strategies (e.g., simplification, structuring, or teach-back) to improve patients’ understanding and recall of provided information [61]. However, none of the publications included in our review assessed the direct relation between clinicians’ actual (observed) information provision during clinical encounters and patient outcomes. Therefore, to enhance clinicians’ tailored information provision, we need insight into their current practice of information provision (i.e., what information they provide, and how they provide it) and in what manner this affectspatients.
This review moreover indicates that patients might value information that they have acquired complementary to clinicians’ information (e.g., via online sources or education). Patients may experience extra support when complementary information is provided in a group setting. Although patients realized that symptoms varied considerably between participants, they experienced a fruitful exchange of information and experiences with fellow patients [26]. Moreover, patients appreciated printed or online information as a future resource [22, 25, 26, 34–37]. One reviewed publication confirmed the common knowledge that patient education should be provided in clear and simple language, with the use of both text and visual aids, and using interactive tools [31, 62, 63]. Unfortunately, this review could not identify which specific aspects of complementary information provision improve patients’ outcomes, for various possible reasons. First, studied interventions were often multifactorial (e.g., containing multiple sessions and/or several components), and the effects of isolated components were not assessed. Second, none of the studied interventions assessed information that patients acquired additionally on their own initiative, while it is known that patients seek for information themselves [14]. Third, most interventions did not assess patients’ understanding or recall of the provided information. Therefore, if publications reported improved patient outcomes such as physical functioning, it remained unclear how these were influenced by the information. Last, comparing results between studied interventions was difficult because studies used different methods and outcomes. For example, similar outcomes (e.g., motor performance), were assessed using various measurements. Systematic reviews regarding information provision in other neurological diseases also concluded a lack of knowledge on the most effective components of complementary information [64, 65].
Information provision should strive to enable patients in participating in collaborative goal-setting, care planning, and disease management within a multidisciplinary team of health-care professionals. To that end, the information that clinicians provide should be tailored to patients’ individual needs and aligned with other information patients obtain [3, 17]. However, due to the scattered findings in this review, it remains unclear how the combination of clinicians’ information provision and complementary acquired information can support patients optimally in their day-to-day disease management. Moreover, how clinicians can optimally align their information with complementary information sources is unknown.
Recommendations for clinical practice and future research
Although based on the currently available evidence, uniform conclusions cannot be drawn regarding how to best provide information to support PD patients optimally, some recommendations for current practice and future research directions can be suggested. First, since patients prefer information tailored to their individual and current needs, clinicians may ask patients explicitly what information they need during clinical encounters [16, 37, 48–52, 55]. Research shows that clinicians adopt a more patient-centered communication style if patients actively participate [66]. However, as not all patients feel able to participate actively during clinical encounters, clinicians might need to involve PD patients more during information provision. In various other medical disciplines, the ‘Ask-Tell-Ask’ approach has been recommended to provide tailored information [67–69]. During the first ‘Ask’, clinicians explore patients’ baseline knowledge, values, and preferences by asking open-ended questions. Hereafter, clinicians can ‘Tell’ information tailored to patients’ baseline knowledge. With the next ‘Ask’ clinicians check if patients’ information needs are fulfilled [67]. Clinicians could try to explore not only what information patients need, but also how and when they want to receive the information. Second, PD patients might benefit from receiving complementary information, especially when provided in recurrent group sessions. Such additional information might be particularly helpful to inform patients about psychosocial aspects of PD, since patients see their neurologist as mainly responsible for the diagnosis and medication, and less for other aspects of PD [7, 48]. Moreover, it seems important to provide patients with printed or online information, as a future resource [22, 25, 26, 34–37]. Last, and most importantly, to empower patients optimally in their day-to-day disease management, these information provision recommendations should be incorporated in a patient-centered format to ensure alignment between different information sources [70]. However, it remains unknown which information is best provided during clinical encounters and which in complementary format, how to align this information optimally, and how patients can maximally benefit from this information.
Therefore, the following directions for future research are recommended. First, all information that patients currently acquire through various modes, should be assessed [14, 71]. To assess what information is currently provided during clinical encounters, observational studies with prospective, longitudinal designs are needed. Such research should focus on the content, amount, and manner of information provision. Moreover, such research should assess how information is tailored to patients’ a priori needs and capacities, and assess patients’ evaluation of this information. Second, to support tailored information provision during clinical encounters, research should focus on tools that assess which information is relevant to an individual patient, indicated by both patient-reported information needs and involved healthcare professionals’ reports of disease progression or complaints. Third, to distinguish effective from ineffective ways of information provision (both during clinical encounters and complementary), the impact of specific aspects of information on patient outcomes should be tested experimentally. Fourth, it could be relevant to research how newly developing technology such as artificial intelligence (AI) tools can be used to enhance information provision [72]. For example, since patients were found to value AI responses, one might use AI in the development of informational leaflets [73]. AI is already frequently used as an important source of information by patients with various diseases. Patients with diabetes who used ChatGPT, felt encouraged by the provided answers, and patients with prostate cancer using an AI-chatbot, reported increased knowledge [74, 75]. By improving knowledge, AI might empower patients in managing their disease [76]. However, for PD specifically, direct information provision through AI might be challenging due to high interpersonal variation regarding the disease course, as well as prevalent cognitive impairment. Moreover, this review underpins that patients value human interaction with their clinician. In our opinion, such interaction could and should not be fully replaced with AI. Still, AI is a promising resource that could support clinicians’ diagnostic and therapeutic reasoning and might serve as an additional tool to improve information provision for patients.
Ultimately, an interactive information provision system could be designed to enhance the process of tailored information provision by keeping track of patients’ acquired information and current information needs. This should be integrated into a larger multidisciplinary patient-centered management system, that also monitors disease progression and coordinates subsequent care [70].
Strengths and limitations
To our knowledge, this is the first review that assesses PD-specific information provision in relation to PD patient outcomes. Strengths are that this review included publications with various study designs (e.g., RCTs, non-RCT intervention studies, cross-sectional survey studies, and qualitative studies), to maximize our understanding of the impact of different aspects of information on PD patients. Moreover, the search and extraction were performed by a multidisciplinary research team, including both medical communication experts and a neurologist. Lastly, publications were systematically searched, selected, and extracted.
This review has several limitations that warrant consideration. First, the absence of a formal quality assessment for the included publications necessitates a cautious interpretation of their results. The decision to omit a quality assessment was made to maintain the broad and exploratory nature of a scoping review. The quality of certain included publications was questionable due to lacking methodological details, notable discrepancies in mean changes, and limited sample sizes, underscoring the imperative for more systematic research. Second, although a medical librarian was consulted who intensively helped set up a broad and comprehensive scope, we might still have missed publications. For example, publications might have been excluded if they reported (minor) relevant results only in their main manuscript and not in the abstract. Finally, our synthesis may involve a degree of subjectivity since extracted outcomes were often not the main outcomes of the included publications. Still, we strived for maximal objectivity by discussing the preliminary results with all the members of the research group.
Conclusion
This scoping review showed that systematic research regarding the impact of disease-specific information on patient outcomes in PD is lacking. PD patients feel supported in their disease management by information that complements clinicians’ information provision during clinical encounters. More observational research is needed to get insight into what information is currently provided by clinicians and in what manner, and how that impacts patient outcomes. In addition, the impact of complementary information provision on patient outcomes should be studied more systematically. That way, more insight will be obtained into how information might empower PD patients optimally in their day-to-day disease management.
ACKNOWLEDGMENTS
The authors have no acknowledgments to report.
FUNDING
All received fundings were paid to the institution. Financial support was received from ParkinsonNL, St. Universitas (AmsterdamUMC foundation), Amsterdams Universiteitsfonds, ZonMW, Alzheimer Nederland, Health-Holland, Topsector Life Sciences & Health, EISAI, Amsterdam Public Health research institute, Medtronic, Amsterdam Neuroscience, Stichting ParkinsonFonds and Stichting Bavalo.
CONFLICT OF INTEREST
Leonie Visser (LNCV) has been an invited speaker at Schwabe Group, fees were paid to her institution. Other authors have no conflict of interest to report.
DATA AVAILABILITY
The data supporting the findings of this study are available within the article and/or its supplementary material.
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JPD-240073.
REFERENCES
[1] | Phillips LJ ((2006) ) Dropping the bomb: The experience of being diagnosed with Parkinson’s disease. Geriatr Nurs 27: , 362–369. |
[2] | Hoehn MM , Yahr MD ((1967) ) Parkinsonism: Onset, progression, and mortality. Neurology 17: , 427–427. |
[3] | Bloem BR , Henderson EJ , Dorsey ER , Okun MS , Okubadejo N , Chan P , Andrejack J , Darweesh SK , Munneke M ((2020) ) Integrated and patient-centred management of Parkinson’s disease: A network model for reshaping chronic neurological care. Lancet Neurol 19: , 623–634. |
[4] | Lorig KR , Holman HR ((2003) ) Self-management education: History, definition, outcomes, and mechanisms. Ann Behav Med 26: , 1–7. |
[5] | Kessler D , Liddy C ((2017) ) Self-management support programs for persons with Parkinson’s disease: An integrative review. Patient Educ Couns 100: , 1787–1795. |
[6] | Kleiner-Fisman G , Gryfe P , Naglie G ((2013) ) A patient-based needs assessment for living well with Parkinson disease: Implementation via nominal group technique. Parkinsons Dis 2013: , 974964. |
[7] | Kurpershoek E , Hillen MA , Medendorp NM , de Bie R , de Visser M , Dijk JM ((2021) ) Advanced care planning in Parkinson’s disease: In-depth interviews with patients on experiences and needs. Front Neurol 12: , 683094. |
[8] | McLaughlin D , Hasson F , Kernohan WG , Waldron M , McLaughlin M , Cochrane B , Chambers H ((2011) ) Living and coping with Parkinson’s disease: Perceptions of informal carers. Palliat Med 25: , 177–182. |
[9] | Buetow S , Giddings LS , Williams L , Nayar S ((2008) ) Perceived unmet needs for health care among Parkinson’s Society of New Zealand members with Parkinson’s disease. Parkinsonism Relat Disord 14: , 495–500. |
[10] | Dorsey ER , Voss TS , Shprecher DR , Deuel LM , Beck CA , Gardiner IF , Coles MA , Burns RS , Marshall FJ , Biglan KM ((2010) ) A U.S. Survey of patients with Parkinson’s disease: Satisfaction with medical care and support groups. Mov Disord 25: , 2128–2135. |
[11] | Schrag A , Khan K , Hotham S , Merritt R , Rascol O , Graham L ((2018) ) Experience of care for Parkinson’s disease in European countries: A survey by the European Parkinson’s Disease Association. Eur J Neurol 25: , 1410–e1120. |
[12] | Smets EM , Menichetti J , Lie HC , Gerwing J ((2023) ) What do we mean by “tailoring” of medical information during clinical interactions? Patient Educ Couns 119: , 108092. |
[13] | Jordan SR , Kluger B , Ayele R , Brungardt A , Hall A , Jones J , Katz M , Miyasaki JM , Lum HD ((2020) ) Optimizing future planning in Parkinson disease: Suggestions for a comprehensive roadmap from patients and care partners. Ann Palliat Med 9: , S63. |
[14] | Riggare S , Höglund PJ , Hvitfeldt Forsberg H , Eftimovska E , Svenningsson P , Hägglund M ((2019) ) Patients are doing it for themselves: A survey on disease-specific knowledge acquisition among people with Parkinson’s disease in Sweden. Health Informatics J 25: , 91–105. |
[15] | Ahmad F , Hudak PL , Bercovitz K , Hollenberg E , Levinson W ((2006) ) Are physicians ready for patients with Internet-based health information? J Med Internet Res 8: , 535. |
[16] | Derollez C , Carriere N , Kyheng M , Dujardin K , Faillon A , Haidon D , Peres S , Defebvre L ((2021) ) Factors that predict a change in quality of life among Parkinson’s disease patients participating in a patient education program. Rev Neurol (Paris) 177: , 1151–1159. |
[17] | van der Eijk M , Nijhuis FA , Faber MJ , Bloem BR ((2013) ) Moving from physician-centered care towards patient-centered care for Parkinson’s disease patients. Parkinsonism Rlated Disord 19: , 923–927. |
[18] | de Looper M , van Weert JC , Schouten BC , Bolle S , Belgers EH , Eddes EH , Smets EM ((2021) ) The influence of online health information seeking before a consultation on anxiety, satisfaction, and information recall, mediated by patient participation: Field study. J Med Internet Res 23: , e23670. |
[19] | Global Parkinson’s Disease Survey (GPDS) Steering Committee ((2002) ) Factors impacting on quality of life in Parkinson’s disease: Results from an international survey. Mov Disord 17: , 60–67. |
[20] | Tricco AC , Lillie E , Zarin W , O’Brien KK , Colquhoun H , Levac D , Moher D , Peters MD , Horsley T , Weeks L ((2018) ) PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med 169: , 467–473. |
[21] | Simons G , Thompson SBN , Smith Pasqualini MC ((2006) ) An innovative education programme for people with Parkinson’s disease and their carers. Parkinsonism Relat Disord 12: , 478–485. |
[22] | Macht M , Gerlich C , Ellgring H , Schradi M , Rusinol AB , Crespo M , Prats A , Viemero V , Lankinen A , Bitti PER , Candini L , Spliethoff-Kamminga N , de Vreugd J , Simons G , Pasqualini MS , Thompson SBN , Taba P , Krikmann U , Kanarik E ((2007) ) Patient education in Parkinson’s disease: Formative evaluation of a standardized programme in seven European countries. Patient Educ Couns 65: , 245–252. |
[23] | A’Campo LEI , Wekking EM , Spliethoff-Kamminga NGA , Le Cessie S , Roos RAC ((2010) ) The benefits of a standardized patient education program for patients with Parkinson’s disease and their caregivers. Parkinsonism Relat Disord 16: , 89–95. |
[24] | A’Campo LEI , Spliethoff-Kamminga NGA , Roos RAC ((2011) ) An evaluation of the patient education programme for Parkinson’s disease in clinical practice. Int J Clin Pract 65: , 1173–1179. |
[25] | Chlond M , Bergmann F , Guthlin C , Schnoor H , Larisch A , Eggert K ((2016) ) Patient education for patients with Parkinson’s disease: A randomised controlled trial. Basal Ganglia 6: , 25–30. |
[26] | Hellqvist C , Dizdar N , Hagell P , Berterö C , Sund-Levander M ((2018) ) Improving self-management for persons with Parkinson’s disease through education focusing on management of daily life: Patients’ and relatives’ experience of the Swedish National Parkinson School. J Clin Nurs 27: , 3719–3728. |
[27] | A’Campo L , Wekking E , Spliethoff-Kamminga N , Stijnen T , Roos R ((2012) ) Treatment effect modifiers for the patient education programme for Parkinson’s disease. Int J Clin Pract 66: , 77–83. |
[28] | Guo L , Jiang Y , Yatsuya H , Yoshida Y , Sakamoto J ((2009) ) Group education with personal rehabilitation for idiopathic Parkinson’s disease. Can J Neurol Sci 36: , 51–59. |
[29] | Oki T , Sugawara N , Haruta H , Takanashi J ((2019) ) The educational programs for extrapyramidal disease and spinocerebellar degeneration patients and their families. Neurol Clin Neurosci 7: , 61–64. |
[30] | Canivet C , Costa N , Ory-Magne F , Arcari C , Mohara C , Pourcel L , Derumeaux H , Bérard E , Bourrel R , Molinier L ((2016) ) Clinical impact and cost-effectiveness of an education program for PD patients: A randomized controlled trial. PLoS One 11: , e0162646. |
[31] | Spurthi S , Sridharan S , Hosadurga R , Rao RJ , Prabhu S , Pal PK , Kamble N , Rakesh K , Kumar A ((2023) ) Effectiveness of oral hygiene educational interventional programs on participants with Parkinson disease: A randomized controlled study. Quintessence Int 54: , 428–437. |
[32] | Hellmers N , Barkan S , Auerbach G , Hanineva A , Popa P , Sarva H , Henchcliffe C ((2021) ) Tablet-based patient educational interventions in care and management of complex movement disorders. Disabil Rehabil Assist Technol 18: , 627–634. |
[33] | Ward CD , Turpin G , Dewey ME , Fleming S , Hurwitz B , Ratib S , von Fragstein M , Lymbery M ((2004) ) Education for people with progressive neurological conditions can have negative effects: Evidence from a randomized controlled trial. Clin Rehabil 18: , 717–725. |
[34] | Montgomery EB Jr. , Lieberman A , Singh G , Fries JF ((1994) ) Patient education and health promotion can be effective in Parkinson’s disease: A randomized controlled trial. PROPATH Advisory Board. Am J Med 97: , 429–435. |
[35] | Dinkelbach L , Möller B , Witt K , Schnitzler A , Südmeyer M ((2017) ) How to improve patient education on deep brain stimulation in Parkinson’s disease: The CARE Monitor study. BMC Neurol 17: , 36. |
[36] | Holloway M ((2006) ) Traversing the network: A user-led Care Pathway approach to the management of Parkinson’s disease in the community. Health Soc Care Community 14: , 63–73. |
[37] | Brown EG , Schleimer E , Bledsoe IO , Rowles W , Miller NA , Sanders SJ , Rankin KP , Ostrem JL , Tanner CM , Bove R ((2022) ) Enhancing clinical information display to improve patient encounters: Human-centered design and evaluation of the Parkinson d∖Disease-BRIDGE Platform. JMIR Hum Factors 9: , e33967. |
[38] | Grosset KA , Grosset DG ((2007) ) Effect of educational intervention on medication timing in Parkinson’s disease: A randomized controlled trial. BMC Neurol 7: , 20. |
[39] | Yi ZM , Willis S , Zhang Y , Liu N , Tang QY , Zhai SD ((2021) ) Impact of a collaborative pharmaceutical care service for patients with Parkinson’s disease. Front Pharmacol 12: , 793361. |
[40] | Leroi I , Baker P , Kehoe P , Daniel E , Byrne EJ ((2010) ) A pilot randomized controlled trial of sleep therapy in Parkinson’s disease: Effect on patients and caregivers. Int J Geriatr Psychiatry 25: , 1073–1079. |
[41] | Kehagia AA , Chowienczyk S , Helena van Velthoven M , King E , North T , Shenton D , Abraham J , Langley J , Partridge R , Ankeny U ((2024) ) Real-world evaluation of the feasibility, acceptability and safety of a remote, self-management Parkinson’s disease care pathway: A healthcare improvement initiative. J Parkinsons Dis 14: , 197–208. |
[42] | Shiraishi M , Kamo T , Kumazawa R , Sasaki N , Isahaya K , Akiyama H , Furusawa Y , Onodera R , Fernandez J , Otsuka M ((2023) ) A multicenter, prospective, observational study to assess the satisfaction of an integrated digital platform of online medical care and remote patient monitoring in Parkinson’s disease. Neurol Clin Neurosci 11: , 152–163. |
[43] | Cook L , Verbrugge J , Schwantes-An T-H , Schulze J , Beck JC , Naito A , Hall A , Chan AK , Casaceli CJ , Marder K ((2023) ) Providing genetic testing and genetic counseling for Parkinson’s disease to the community. Genet Med 25: , 100907. |
[44] | Afshari M , Hernandez AV , Joyce JM , Hauptschein AW , Trenkle KL , Stebbins GT , Goetz CG ((2024) ) A novel home-based telerehabilitation program targeting fall prevention in Parkinson disease: A preliminary trial. Neurol Clin Pract 14: , e200246. |
[45] | Carlino E , Piedimonte A , Romagnolo A , Guerra G , Frisaldi E , Vighetti S , Lopiano L , Benedetti F ((2019) ) Verbal communication about drug dosage balances drug reduction in Parkinson’s disease: Behavioral and electrophysiological evidences. Parkinsonism Relat Disord 65: , 184–189. |
[46] | Mercado R , Constantoyannis C , Mandat T , Kumar A , Schulzer M , Stoessl AJ , Honey CR ((2006) ) Expectation and the placebo effect in Parkinson’s disease patients with subthalamic nucleus deep brain stimulation. Mov Disord 21: , 1457–1461. |
[47] | Schrag A , Modi S , Hotham S , Merritt R , Khan K , Graham L , European Parkinson’s Disease Association ((2018) ) Patient experiences of receiving a diagnosis of Parkinson’s disease. J Neurology 265: , 1151–1157. |
[48] | Boersma I , Jones J , Carter J , Bekelman D , Miyasaki J , Kluger JK ((2016) ) Parkinson disease patient’s perspectives on palliative care needs What are they telling us? Neurol Clin Pract 6: , 209–219. |
[49] | Nijhuis FAP , Van Heek J , Bloem BR , Post B , Faber MJ ((2016) ) Choosing an advanced therapy in Parkinson’s disease; Is it an evidence-based decision in current practice? J Parkinsons Dis 6: , 533–543. |
[50] | Habermann B , Shin JY ((2017) ) Preferences and concerns for care needs in advanced Parkinson’s disease: A qualitative study of couples. J Clin Nurs 26: , 1650–1656. |
[51] | Shaw ST , Vivekananda-Schmidt P ((2017) ) Challenges to ethically managing Parkinson disease: An interview study of patient perspectives. J Patient Exp 4: , 191–196. |
[52] | Zizzo N , Bell E , Lafontaine A-L , Racine E ((2017) ) Examining chronic care patient preferences for involvement in health-care decision making: The case of Parkinson’s disease patients in a patient-centred clinic. Health Expect 20: , 655–664. |
[53] | Troisoeufs A ((2019) ) Deep Brain Stimulation (DBS) experiences: An ethnographic approach to their expression on the Internet forums. Med Health Care Philos 22: , 343–352. |
[54] | Fothergill-Misbah N , Walker R , Kwasa J , Hooker J , Hampshire K ((2021) ) “Old people problems”, uncertainty and legitimacy: Challenges with diagnosing Parkinson’s disease in Kenya. Soc Sci Med 282: , 114148. |
[55] | Shah R , Read J , Davies N , Nimmons D , Pigott J , Schrag A , Walters K , Armstrong M ((2022) ) People with Parkinson’s perspectives and experiences of self-management: Qualitative findings from a UK study. PLoS One 17: , e0273428. |
[56] | Tan QY , Roberts HC , Fraser SD , Amar K , Ibrahim K ((2023) ) What are the modifiable factors of treatment burden and capacity among people with Parkinson’s disease and their caregivers: A qualitative study. PLoS One 18: , e0283713. |
[57] | Kessels RP ((2003) ) Patients’ memory for medical information. J R Soc Med 96: , 219–222. |
[58] | van der Meulen N , Jansen J , Van Dulmen S , Bensing J , Van Weert J ((2008) ) Interventions to improve recall of medical information in cancer patients: A systematic review of the literature. Psychooncology 17: , 857–868. |
[59] | Marras C , Rochon P , Lang AE ((2002) ) Predicting motor decline and disability in Parkinson disease: A systematic review. Arch Neurol 59: , 1724–1728. |
[60] | Lie HC , Juvet LK , Street RL , Gulbrandsen P , Mellblom AV , Brembo EA , Eide H , Heyn L , Saltveit KH , Strømme H ((2022) ) Effects of physicians’ information giving on patient outcomes: A systematic review. J Gen Intern Med 37: , 1–13. |
[61] | Menichetti J , Lie HC , Mellblom AV , Brembo EA , Eide H , Gulbrandsen P , Heyn L , Saltveit KH , Strømme H , Sundling V ((2021) ) Tested communication strategies for providing information to patients in medical consultations: A scoping review and quality assessment of the literature. Patient Educ Couns 104: , 1891–1903. |
[62] | Meppelink CS , Smit EG , Buurman BM , van Weert JC ((2015) ) Should we be afraid of simple messages? The effects of text difficulty and illustrations in people with low or high health literacy. Health Commun 30: , 1181–1189. |
[63] | van Weert JC , Alblas MC , van Dijk L , Jansen J ((2021) ) Preference for and understanding of graphs presenting health risk information. The role of age, health literacy, numeracy and graph literacy. Patient Educ Couns 104: , 109–117. |
[64] | Köpke S , Solari A , Rahn A , Khan F , Heesen C , Giordano A ((2018) ) Information provision for people with multiple sclerosis. Cochrane Database Syst Rev 10: , CD008757. |
[65] | Langbecker D , Janda M ((2015) ) Systematic review of interventions to improve the provision of information for adults with primary brain tumors and their caregivers. Front Oncol 5: , 1. |
[66] | Cegala DJ , Post DM ((2009) ) The impact of patients’ participation on physicians’ patient-centered communication. Patient Educ Couns 77: , 202–208. |
[67] | Gaster B , Edwards K , Trinidad SB , Gallagher TH , Braddock CH III ((2010) ) Patient-centered discussions about prostate cancer screening: A real-world approach. Ann Intern Med 153: , 661–665. |
[68] | Grenon NN , Keersmaecker S , McGinley F ((2021) ) GUIDE Communication Framework: Developing Skills to Improve Nurse-Patient Interactions. Clin J Oncol Nurs 25: , 623–627. |
[69] | Shapiro J , Robins L , Galowitz P , Gallagher TH , Bell S ((2021) ) Disclosure coaching: An ask-tell-ask model to support clinicians in disclosure conversations. J Patient Saf 17: , e1364–e1370. |
[70] | van Halteren AD , Munneke M , Smit E , Thomas S , Bloem BR , Darweesh SK ((2020) ) Personalized care management for persons with Parkinson’s disease. J Parkinsons Dis 10: , S11–S20. |
[71] | Nijkrake MJ , Keus SH , Oostendorp RA , Overeem S , Mulleners W , Bloem BR , Munneke M ((2009) ) Allied health care in Parkinson’s disease: Referral, consultation, and professional expertise. Mov Disord 24: , 282–286. |
[72] | Meinert E , Milne-Ives M , Chaudhuri KR , Harding T , Whipps J , Whipps S , Carroll C ((2022) ) The impact of a digital artificial intelligence system on the monitoring and self-management of nonmotor symptoms in people with Parkinson disease: Proposal for a phase 1 implementation study. JMIR Res Protoc 11: , e40317. |
[73] | Ayers JW , Poliak A , Dredze M , Leas EC , Zhu Z , Kelley JB , Faix DJ , Goodman AM , Longhurst CA , Hogarth M ((2023) ) Comparing physician and artificial intelligence chatbot responses to patient questions posted to a public social media forum. JAMA Intern Med 183: , 589–596. |
[74] | Nakhleh A , Spitzer S , Shehadeh N ((2023) ) ChatGPT’s response to the diabetes knowledge questionnaire: Implications for diabetes education. Diabetes Technol Ther 25: , 571–573. |
[75] | Görtz M , Baumgärtner K , Schmid T , Muschko M , Woessner P , Gerlach A , Byczkowski M , Sültmann H , Duensing S , Hohenfellner M ((2023) ) An artificial intelligence-based chatbot for prostate cancer education: Design and patient evaluation study. Digit Health 9: , 20552076231173304. |
[76] | Alowais SA , Alghamdi SS , Alsuhebany N , Alqahtani T , Alshaya AI , Almohareb SN , Aldairem A , Alrashed M , Bin Saleh K , Badreldin HA ((2023) ) Revolutionizing healthcare: The role of artificial intelligence in clinical practice. BMC Med Educ 23: , 689. |




