If Art Were a Drug: Implications for Parkinson’s Disease
Abstract
Parkinson’s disease (PD) is a chronic and complex neurodegenerative disorder. Conventional pharmacological or surgical therapies alone are often insufficient at adequately alleviating disability. Moreover, there is an increasing shift toward person-centered care, emphasizing the concept of “living well”. In this context, arts-based interventions offer great promise, functioning as platforms for creative expression that could provide novel mechanisms to promote quality of life. Here we present a qualitative review of arts-based interventions for PD, including music, dance, drama, visual arts, and creative writing. For each, we discuss their applications to PD, proposed mechanisms, evidence from prior studies, and upcoming research. We also provide examples of community-based projects. Studies to date have had relatively small sample sizes, but their findings suggest that arts-based interventions have the potential to reduce motor and non-motor symptoms. They may also empower people with PD and thereby address issues of self-esteem, foster personal problem-solving, and augment holistic well-being. However, there is a paucity of research determining optimal dosage and symptom-specific benefits of these therapies. If art were a drug, we would have to perform appropriately powered studies to provide these data before incorporating it into routine patient care. We therefore call for further research with properly designed studies to offer more rigorous and evidence-based support for what we intuitively think is a highly promising approach to support individuals living with PD. Given the possible positive impact on people’s lives, arts-based approaches merit further development and, if proven to be effective, systematic inclusion within integrated management plans.
INTRODUCTION
Parkinson’s disease (PD) is a chronic neurodegenerative disease marked by motor and non-motor symptoms, impacting both physical and mental well-being [1]. In addition to symptoms, people with PD often experience social isolation, stigma, and reduced self-esteem [2–4]. Current pharmacological or surgical interventions fall short of adequately treating these multiple facets of PD [5, 6]. Arts-based interventions are emerging as therapeutic modalities with the potential to enhance quality of life by uniquely tackling aspects of the disease that conventional treatments cannot address.
PD involves the central dopaminergic system [1] which can be linked to artistic inclinations [7–9], and there is an intriguing interplay between art and PD [10, 11]. The neurodegenerative process in PD leads to reduced dopaminergic transmission, which may be expected to lead to reduced creativity. However, pharmacotherapy with dopaminergic agents and deep brain stimulation (DBS) for PD can alter this system, leading to noticeable changes, either decreasing or increasing creativity (Fig. 1). For example, Pelowski et al. [7] reported cases of individuals with PD experiencing changes in creative prowess; these shifts were attributed either to neurodegeneration itself or to enhanced stimulation of the mesolimbic dopaminergic pathways by dopamine replacement therapies. Artists with PD can experience varying degrees of changes in their art, including in style or artistic domain, sometimes due to altered creativity or directly due to motor difficulties or both (Fig. 2). As creative individuals, artists with PD often discover ways to adapt or compensate for dysfunction due to their disease (Fig. 3). In visual arts, studies have documented shifts in abstractness, symbolism, and color choices [12–15]. While many reports highlight an increase in creativity (typically following the initiation of dopaminergic treatments), transforming “unremarkable” creations to artworks deemed exhibition-worthy [16], some studies also noted a decline in creativity [17]. Decrease in artistic creativity after DBS has been related to the reduction of dopamine replacement therapy post procedure, specifically dopamine agonists [18].
Fig. 1
Example of the effects of dopaminergic therapies on creativity in PD. Steven Iseman is a 58-year-old man who was diagnosed with PD at age 47. He worked as a lawyer and had no artistic interests prior to his diagnosis. After starting treatment with levodopa and pramipexole, he developed new creative abilities which he applies to sculptural art using 3D printing. These three pieces titled Zeus’s Workshop (left), Mother and Child (middle), and Spring Forest Riot (right) demonstrate the diversity of his work. His substantial artistic output can be appreciated on his website (www.stevenisemanart.ca). All materials published with permission from Steven Iseman.

Fig. 2
Example of changes in the work by an artist with PD over the disease course. (A) Zus Keulemans-Goosen (1932–2023) was a self-taught artist who dedicated herself to drawing, painting, and ceramic work starting in her 50 s. She was diagnosed with PD at age 71 and changed her artistic mediums and methods with the progression of her disease. (B) She initially favored large canvases for painting, but the constraints imposed by PD led her to transition to smaller formats. An early large painting and a small painting from later in her disease are juxtaposed here. An interview (in Dutch) in which one of the authors (BRB) interviews the artist’s daughter, Elianne Keulemans, provides further insights into how PD affected the artist (www.vimeo.com/864883633/880431a3d2). All materials published with permission from Elianne Keulemans.
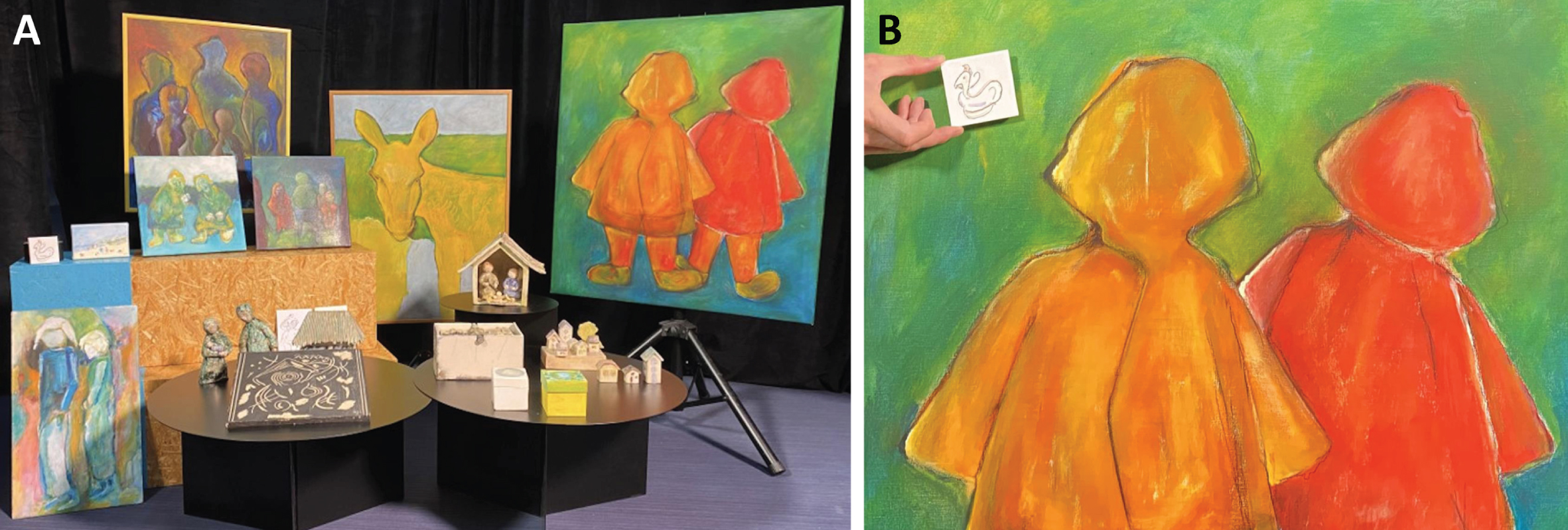
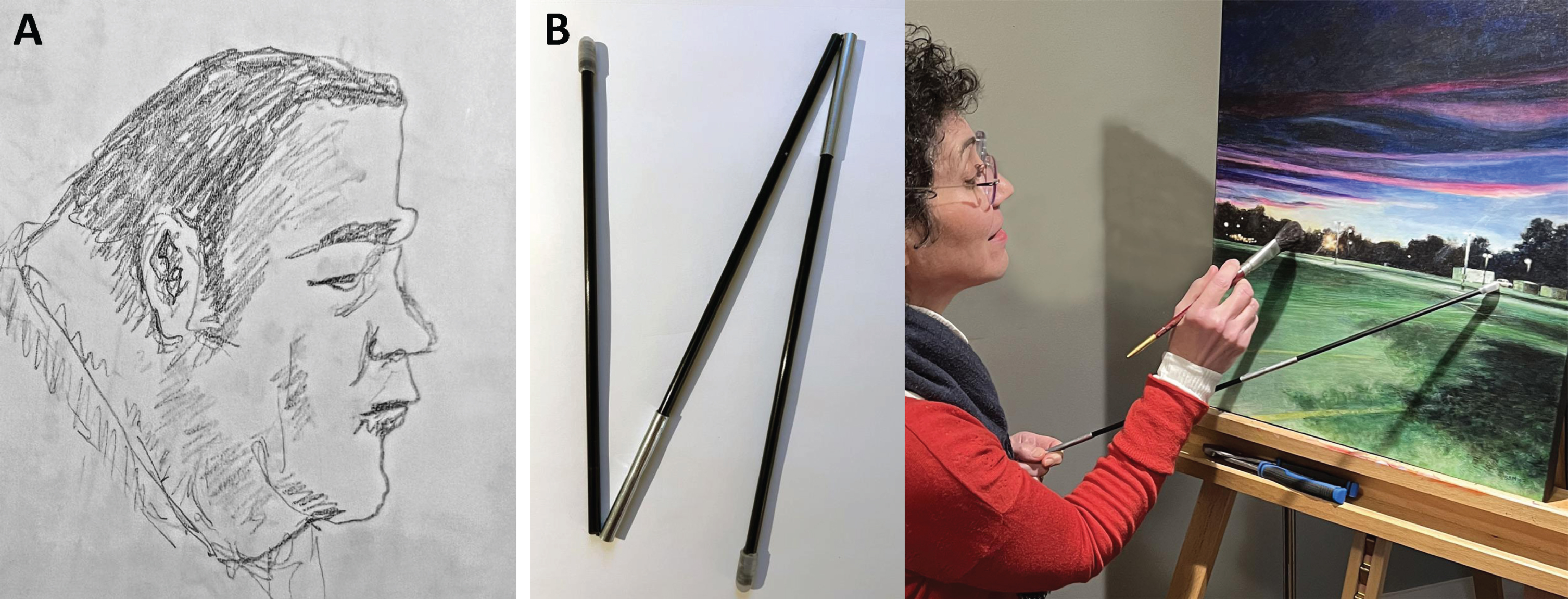
Fig. 3
Example of adaptations made by an artist with PD. Barbara Salsberg Mathews is a 64-year-old woman who was diagnosed with PD at age 60. She has been an artist since childhood, both in the realm of visual arts (www.salsbergmathews.com) and theater (www.mimeovermind.com). Two examples of adaptations she has made with her drawing and painting since developing PD include (A) exploiting her hand tremor by allowing the involuntary rhythmic movements to produce pencil shading and (B) using a folding stick to support her affected arm and prevent the hand from smudging pencil or touching wet paint. All materials published with permission from Barbara Salsberg Mathews.
The connections between artistry and the dopaminergic system make arts-based therapies particularly suitable for PD. This aligns with the trend towards person-centered care, emphasizing multimodal approaches [19], and thus advantageous for the multifaceted nature of PD. These interventions also foster a sense of belonging, self-value, and cognitive engagement [20]. Arts are a way for persons living with PD to express themselves as creative individuals, rather than as patients. Moreover, arts offer a unique way of expanding a person’s world which is otherwise constantly shrinking due to the effects of PD, such as progressive immobility, dysarthria, and cognitive dysfunction, among others [21].
Here we provide a descriptive, qualitative review of the recent literature on prominent arts-based interventions for PD: music, dance, drama, visual arts, and creative writing. We focus on studies published within the last three years to highlight the latest findings and identify current trends. We discuss their relevance for healthcare, potential targets of impact to be further investigated, and major gaps in the field. Moreover, we highlight some upcoming research and current community-based projects to inform the research community as well as stakeholders such as people with PD, caregivers, community organizations, among others. Our objective is to advocate for the potential integration of arts-based methods in the current management of PD. More than symptom mitigators, these interventions can enhance personalized therapy while empowering individuals [19, 20, 22]. We recognize that, if art were a drug, evidence for its efficacy, safety, and cost-effectiveness would be required to routinely recommend it as a treatment option in daily care. We therefore also critically review the evidence to support existing art interventions. Based on this, we call for further research, including properly designed studies, to offer rigorous and evidence-based support for what we intuitively view as a highly promising approach to support individuals living with PD.
METHODS
A non-systematic literature review was performed in PubMed. A combination of the following terms was used: “music”, “dance”, “drama or theater”, “visual arts or painting or sculpture or drawing”, “creative writing or writing or journaling” and “Parkinson’s disease”. Articles published in the past 3 years were favored, when possible, but no date restriction was imposed. Articles were selected by a single author (PG) for their relevance in describing the corresponding arts-based intervention and their influence on motor and non-motor symptoms of PD. ChatGPT, version 3.5, a language model developed by OpenAI (www.openai.com), was used for language refinement of this manuscript.
ART INTERVENTIONS FOR PARKINSON’S DISEASE
Music
Types of music interventions: Sihvonen et al. [23] define music therapy as “music-based interventions delivered in a clinical setting by a credentialed music therapist that use various musical elements (e.g., singing, creating, moving to, or listening to music)”. This review extends beyond music therapy, encompassing various music interventions for PD in the literature. Music is currently used for a variety of neurological conditions such as stroke, epilepsy, multiple sclerosis, among others [23, 24]. It includes passive activities like listening to music and active participation through singing, playing instruments, or engaging in specific methods like the Ronnie Gardner Rhythm and Music Method [25, 26]. In addition, there is music-based physical therapy or exercise which has been studied (Fig. 4) [26].
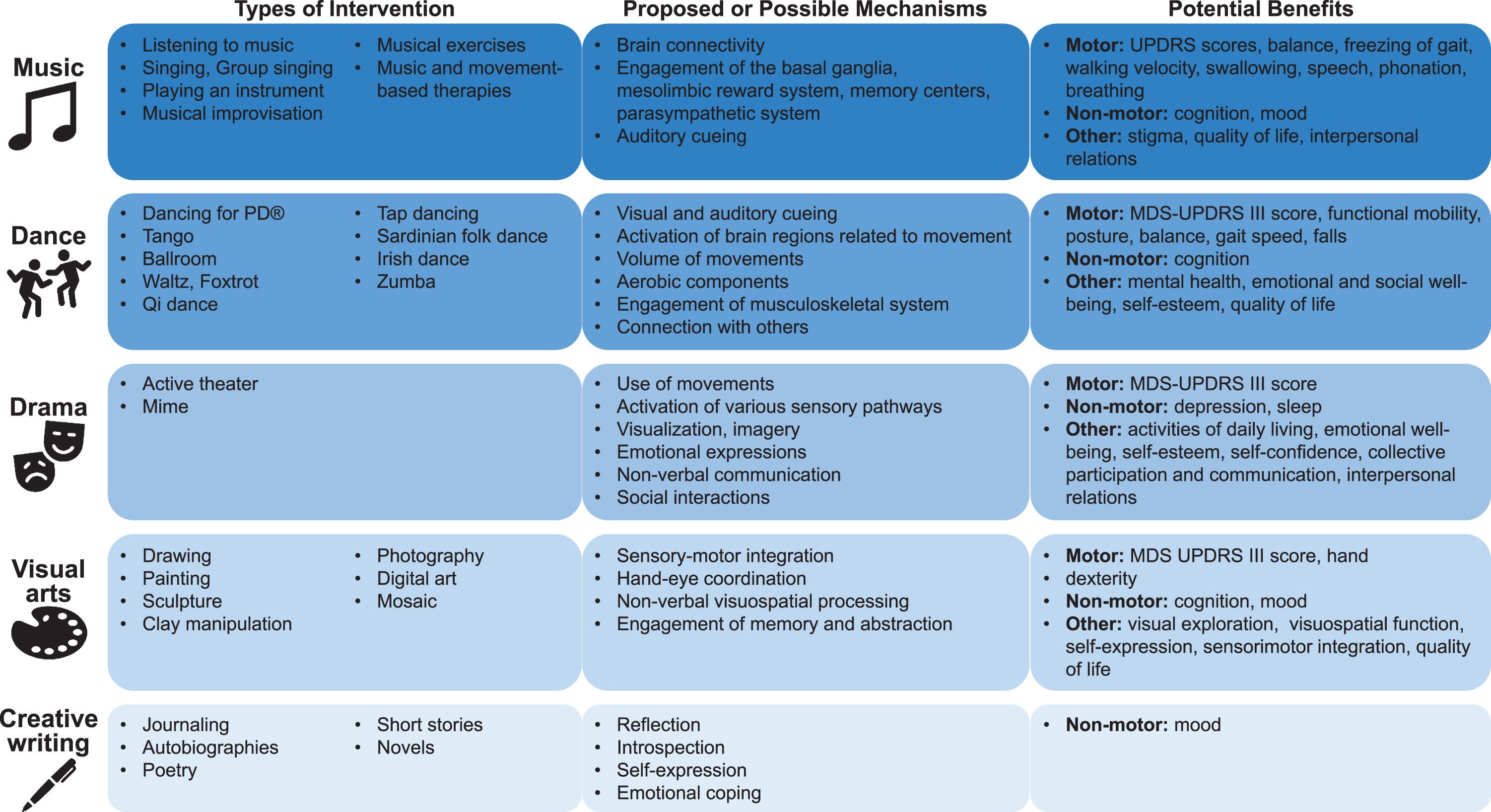
Fig. 4
Arts-based interventions for PD. There are multiple types of interventions including music, dance, drama, visual arts, and creative writing. Small studies (i.e., analogous to phase 1 and 2a drug trials) have demonstrated several potential benefits for people with PD. Further research is needed to understand the mechanisms underlying these potential benefits, and larger and more rigorous studies (i.e., analogous to phase 2b or 3 drug trials) are needed. UPDRS, Unified Parkinson Disease Rating Scale; MDS-UPDRS, Movement Disorders Society Unified Parkinson Disease Rating Scale.
Proposed mechanisms: Listening to music influences brain connectivity, engages the basal ganglia in rhythm perception, and activates memory centers [23, 27]. There is a small evidence base indicating that music may induce neuroplasticity in the normal developing brain [28] and in the adult brain [23, 28, 29]. For example, structural and functional differences in regions involved in music were found when musicians were compared to nonmusicians [28]. The mesolimbic reward system, including the nucleus accumbens, contributes to increased dopamine levels leading to the emotional responses and enjoyment experienced while listening to music, potentially interacting with the motor pathways [23]. Music is also thought to activate the parasympathetic system. The basal ganglia are responsible for timing and cueing in healthy individuals, and therefore those with PD may experience loss of rhythm when finger tapping, walking, or capturing rhythms [30]. The cueing related to music is thought to play a role in improving movement, including entrainment, gait speed, and stride length [31, 32]. The auditory-motor pathway connection underlies rhythmic auditory stimulation which was shown to improve gait quality, balance, and stride length as well as reduce fall frequency and freezing of gait (Fig. 4) [33–35].
Evidence from prior studies: A recent systematic review suggested that music therapy in PD may be associated with improved motor functioning, swallowing, breathing, communication, emotional factors, and quality of life [26]. Spina et al.[36] demonstrated benefits for cognition, including frontal function, although the effect was short-lived. Group singing, including chorale-based interventions, was found to enhance speech, such as phonation, voice-related quality of life, and interpersonal relationships [37–39]. Mohseni et al.[40] proposed that combining music therapy, mainly singing, with speech therapy was more effective than each therapy alone for improving swallowing in PD. Further, singing may influence motor scores on the Unified Parkinson Disease Rating Scale (UPDRS), as well as stigma, anxiety, and stress [41, 42]. Playing a musical instrument was found to improve outcomes in PD. GuitarPD, a randomized pilot study of non-traditional guitar classes, demonstrated an improvement in mood and anxiety in individuals with PD [43]. Studies evaluating group drumming showed partial increase in social satisfaction and improved quality of life, with variable benefits regarding mobility [44, 45]. Studies examining the Ronnie Gardner Rhythm and Music Method reported variable findings: one study showed improvements in mobility, cognition, and quality of life, while another revealed improvement only in quality of life, not in cognition, dual-tasking, or freezing of gait [25, 46]. A recent pilot study comparing music therapy and rehabilitation versus rehabilitation alone found that music therapy and rehabilitation may improve various aspects of quality of life, measured by using Parkinson Disease Questionnaire (PDQ-39) scores [47]. In a meta-analysis, Zhou et al. [48] concluded that music-based movement therapies, such as dancing, walking, or marching using music, was associated with improved balance, freezing of gait, walking velocity, but also mental health (Fig. 4). Several studies lacked a control group, and those that did include one either used a no intervention control group or, in a minority, another intervention like physiotherapy [26, 49]. Most studies indicate using a group-based intervention or do not mention the use of individualized interventions. A minority of studies explicitly offered a personalized intervention [50].
Upcoming research: Several researchers in the US are studying music therapy for individuals with PD, including a University of Washington group using classical guitar [51, 52]. A University of Massachusetts group is conducting a randomized controlled trial evaluating whether music therapy could prevent hospital-acquired delirium in individuals with PD and Lewy Body Dementia [53].
Examples of community-based projects: Community-based initiatives using music-based interventions are numerous. In Canada, Singing with Parkinson’s offers weekly online singing classes [54] and Signature Therapy as well as Music & Soul provide neurological music therapy sessions [55, 56]. Singing with Parkinson’s is a therapeutic choir and provides neurological music therapy in Atlanta, USA [57]. Parkinson’s Europe has recently partnered with Music Care, an app providing music therapy to individuals living with PD [58].
Dance
Types of dance interventions: The American Dance Therapy Association defines dance therapy as the “psychotherapeutic use of movement to promote emotional, social, cognitive, and physical integration of the individual, for the purpose of improving health and well-being” [59]. This review extends beyond dance therapy, encompassing the broader scope of dance interventions for PD described in the literature. Various types of dance interventions for individuals living with PD have been described, including the Dancing for PD method®, tango, Qi dance, tap dancing, Sardinian folk dance, Irish dance, among others (Fig. 4) [60].
Proposed mechanisms: Although music is an important component of dance that provides external auditory cueing, dance incorporates visual cueing; both elements are lost when the basal ganglia are lesioned [61]. Moreover, dance is associated with enhanced activation of areas related to movements, such as the frontoparietal action observation network, thought to be involved in the observation of familiar movements and production of movements [61, 62], as well as the cortico-striatal pathways involved in posture and movements. White matter diffusivity and neuroplasticity are also thought to play a role, although the evidence in PD is limited [61, 63]. Dance requires a dynamic control of balance, spatial awareness, task shifting, strength and flexibility [64]. It also requires an important volume of movements and, in itself, may lead to a greater amount of physical activity. Several types of dance involve variable degrees of aerobic activity, with subsequent potential benefits on the cardiovascular system, mood, and cognition [64]. Connection with others contributes to the enjoyment of dance, thus leading to motivation and potentially better adherence compared to other exercises (Fig. 4) [64]. Studies have shown that partnered and non-partnered dance is safe in mild and moderate PD, with a partner providing additional somatosensory cues and potentially mitigating fear of falling [65–68].
Evidence from prior studies: Several studies have reported that dance is associated with improved motor scores on the Movement Disorders Society UPDRS part III (MDS-UPDRS III), functional mobility as measured by the Timed Up & Go, gait speed, balance measured by the MiniBest Test, postural control, and falls [60, 69–74]. In a meta-analysis, Hasan et al. [75] found that dance compared to exercise improved the MDS-UPDRS III, Timed Up & Go, Berg Balance Scale, and the MiniBest Test, but found no difference with respect to freezing of gait and the 6-min walk test change. Dance was found to influence cognitive functions [70, 76–78], including executive function, episodic memory, spatial awareness, cognitive switching, and dual tasking [69, 76, 77]. Associations with improved mental health, including anxiety, depression, apathy, and emotional and social well-being, were also reported in most studies, although the evidence is mixed [71, 74–76, 78–81]. Results from a cohort study of 49 individuals living with PD suggested that dance improves self-esteem as measured by the Rosenberg Self-Esteem Score and health-related quality of life as measured by the PDQ-39 (Fig. 4) [74]. Most studies indicate using group-based interventions, rather than a personalized approach. Most studies included a control group, which either received usual care, a non-exercise intervention such as education, passive music appreciation or support groups, or a non-dance physical activity such as stretching or physiotherapy [37, 78].
Upcoming research: Recently, there has been an increased interest in online delivery of dance therapy, shown to be feasible and to enhance accessibility [82–84]. Safety measures, including home safety checklists and pre-intervention screenings, have been employed [82]. However, studies have not systematically included individuals with advanced PD, varying digital literacy, or other barriers to using the internet [85]. Several research groups have evaluated the feasibility of using wearable sensors or accelerometry to measure objective outcomes of movement or dance in trials [68, 86].
Examples of community-based projects: In Canada, Dancing with Parkinson’s offers free daily online dance classes as well as in-person dance classes [87]. Dance for PD® offers in-person dance classes in various parts of the USA and the world, as well as online options [88].
Drama
Types of drama interventions: As per the North American Drama Therapy Association, “drama therapy is the intentional use of drama and/or theater to achieve therapeutic goals” [89]. Typical theatre training sessions are described in Modugno et al. [90, 91] and Mirabella et al. [90, 91]. Individuals delve into their personal life experiences by employing acting and creativity, and they assume the roles of characters, utilizing storytelling to convey their narratives from within these personas [92]. This review encompasses various forms of drama-based interventions for PD found in the literature.
Proposed mechanisms: Although the mechanism is unclear in PD, active theater requires a combination of movements, activation of various sensory pathways, expression of emotions, and social interactions necessary to form a dialogue or story [90, 91]. It also involves aspects such as visualization, use of imagery, and nonverbal communication (Fig. 4). It is unclear which aspects are predominantly driving the potential benefit derived from theater in PD, as the number of studies to date are limited and have only been compared to physiotherapy.
Evidence from prior studies: In a pilot randomized trial with 20 individuals with PD, Modugno et al. [90] reported that those in the theater arm, compared to physiotherapy, had improved non-motor symptoms based on various scales, including the Schwab and England scale, PDQ-39, Epworth Sleepiness Scale, and Hamilton Depression Rating Scale, as well as improved motor scores on the UPDRS, albeit to a lesser extent. In a subsequent pilot non-randomized study with 24 individuals with PD, the same group found that theater was associated with improved emotional well-being compared to physiotherapy, but there was no significant improvement in motor symptoms or cognition [91]. A small study conducted in Spain suggested a trend for improved depression in individuals living with PD (Fig. 4) [93].
Upcoming research: To our knowledge, there are no upcoming trials using these interventions.
Examples of community-based projects: The CHEER > UP program is a drama therapy program designed for individuals living with PD and caregivers that uses techniques such as improv, humor, mime, voice work, and skits [94]. A music and drama therapy program is offered through Creative Arts for Parkinson’s via Northwestern University’s Parkinson’s Disease and Movement Disorders Center in Chicago, USA [95]. Resources about drama therapy can be found on the North American Drama Therapy Association website [89]. Initiatives for individuals living with PD by individuals living with PD have emerged, such as Mime over Mind or Mime over Matter [96, 97], which use mime as therapy forPD.
Visual arts
Types of visual arts interventions: Visual arts therapy uses the creation and exploration of visual arts as an intervention to improve one’s well-being. It may include, but is not limited to, drawing, painting, sculpture, clay manipulation, photography, digital art, mosaic, among many others (Fig. 4) [98–101].
Proposed mechanisms: Although the mechanism is unclear in PD, art therapy promotes sensory-motor integration and hand-eye coordination [99]. It involves non-verbal visuospatial processing and other cognitive areas such as memory and abstraction (Fig. 4) [99, 102]. The proposed mechanisms behind artistic creativity are largely derived from the study of artists, who frequently demonstrate heightened perceptual skills and attention to details. These attributes correlate with advanced visual processing and memory, crucial for realistic depictions in visual arts. Their flexibility in attention allows for seamless switching between stimulus aspects, enhancing both creative and technical abilities. The ideation phase necessitates problem-solving and planning skills, areas where artists excel. High ideational fluency and openness are prevalent among artists, fostering the generation of diverse and original visual ideas. The neurobiological underpinnings of creative drive are linked to the brain’s reward circuits, particularly dopaminergic pathways. In PD, pharmacotherapies affecting these pathways may inadvertently modify artistic inclinations (Fig. 1). The ‘artistic brain’ encompasses regions involved in visuospatial processing, global attention, memory, and complex task planning, which are areas impacted by neuropathology in PD. The mesolimbic reward system’s role in emotional responses to art suggests a therapeutic mechanism, where artistic engagement may elevate dopamine levels and interact beneficially with motor pathways.
Evidence from prior studies: Cucca et al. [103] conducted a prospective exploratory observational study of 18 individuals with PD undergoing 20 sessions of art therapy, compared to healthy age-matched controls at baseline. Art therapy included clay manipulation, painting on canvas, collage, drawing, and figurative arts. Results indicated improved visual exploration and visuospatial function, based on improved fMRI visual connectivity networks markers and eye-tracking tests, as well as improved motor function measured by the UPDRS III. A study of 54 individuals living with PD showed that clay-based art therapy plus rehabilitation versus rehabilitation alone was associated with improvement in hand dexterity, self-expression, mood, depression, and quality of life (Fig. 4) [98]. Clay art requires three dimensional visuospatial processing and increased sensorimotor integration given the tactile aspect [98]. Passive art viewing, though less studied, is thought to influence mental health and cognition in the elderly, but limited data exists in PD [104].
Upcoming research: From 2022 onwards, a 5-year international European collaboration between Austria and the Netherlands called “Unlocking the Muse: Transdisciplinary Approaches to Understanding and Applying the Intersection of Artistic Creativity and Parkinson’s Disease”, has been ongoing, with a focus on addressing visual art as intervention tools for people with PD [105].
Examples of community-based projects: Various PD-related community organizations offer local information about visual arts therapy and art therapy in general [106]. Further information about art therapy and a repertoire of art therapists can be found on the American Art Therapy Association website [107]. Moreover, there are also webpages showing visual art from people with PD, specifically a film about pasta art [108], and also some film-productions, initiated by Filmwerk Films and filmmaker Bettina Rotzetter in cooperation with the Inselspital Bern in Switzerland [109, 110].
Creative writing
Types of creating writing interventions: Creative writing is the use of fictional or non-fictional writing for personal expression and communication [111]. It may take many forms including journaling, auto-biographies, poetry, short stories, and novels (Fig. 4).
Proposed mechanisms: Although the mechanism is unclear in PD, creative writing encourages reflection, introspection, and self-expression. It may also help individuals cope with emotions(Fig. 4).
Evidence from prior studies: No major studies have been performed in PD. A randomized study of 40 individuals with depression compared expressive writing workshops with non-emotional writing as control. The expressive writing group demonstrated improvement in depression as measured by the Beck Depression Inventory and Patient Health Questionnaire-9 scores [112]. Creative writing may also improve mood in cancer patients, although not on all outcome measures (Fig. 4) [113].
Upcoming research: There is no upcoming research using these interventions to our knowledge.
Example of community-based projects: Multiple PD associations provide tools on creative writing. Parkinson Europe, Parkinson’s UK, and Parkinson Society British Columbia offer advice on how individuals living with PD can get started on creative writing and comment on the potential benefits of this activity [114–116].
DISCUSSION
Findings and limitations of the research to date
Arts-based interventions have the potential to offer a holistic approach to manage various motor and non-motor symptoms of PD while also addressing self-esteem, fostering problem-solving, and enhancing overall well-being. Analogous to phase 1 or 2a drug trials, studies to date provide evidence to suggest significant potential and adequate safety. Small sample sizes, usually under 100 participants, may have led to underpowered studies [26, 37]. Larger and more rigorous studies (i.e., analogous to phase 2b or 3 drug trials) are needed to make more definitive conclusions. Our review highlights a need for well-designed research to determine efficacy, optimal dosage, and symptom-specific benefits. In addition, decisions on supervision, whether by any artists or specifically trained art therapists, remain unresolved to this date. Given the potential positive impact on individuals with PD, further research is necessary for systematic inclusion in therapeutic plans.
Challenges of trial designs with arts-based interventions
Dose, duration, and adherence to the intervention: Future studies need to explore optimal intervention doses and duration (intermittent versus lifelong engagement). While clinical trials testing pharmacological interventions offer apparent uniformity across treatment arms (e.g., swallowing a pill), arts-based interventions rely to a greater extent on active participant engagement, thus posing challenges for standardization. For example, the degree of physical exertion during a dance class depends on the individual’s efforts. To our knowledge, previous studies did not account for this. Wearables for objective measurement in dance interventions are gaining interest but are not widely used to measure intervention dose and adherence [68]. Another important element is the duration of the intervention. This concerns both the potential effectiveness, which may necessitate extended exposure to the art intervention, and adherence issues, potentially difficult for long-term interventions in a progressive condition like PD which is associated with ongoing new challenges for individuals.
Control groups: The selection of an appropriate control group for arts-based intervention trials is not always straightforward and should be carefully considered based on the hypothesis and research question that each study aims to answer. Selection will depend on the type of trials being designed; for example, “pragmatic” or “explanatory”. In pragmatic trials, the goal is to test the intervention in real-life routine practice settings. In contrast, explanatory trials aim to test the intervention under ideal conditions (i.e., “if and how an intervention works”[117]). Thus, it is common for pragmatic trials to include “usual care” as control groups (i.e., compare intervention versus no intervention) whereas explanatory trials may choose placebo or active controls in an attempt to eliminate important confounders [118]. We propose that there is value in comparing art-based interventions to usual care first to determine their additional benefits beyond the existing PD interventions used in current clinical practice. We argue that it may not be crucial to fully understand the specific component of the intervention that is responsible for the observed benefits until we have evidence that the intervention is associated with some measurable benefit. While pragmatic trials may not initially differentiate art-specific mechanisms from generic effects, such as those associated with social activities, subsequent research could address this in explanatory trials if warranted. In these trials, the control could be an activity requiring social engagement but without a creative component (e.g., support group) or an alternative creative activity engaging a different domain (e.g., dance versus visual arts). Another approach is to compare various intensities of the same art-based intervention. In the pharmacological world, platform trials have emerged as a judicious way to test multiple drugs simultaneously with a single control group, and similar trials for arts-based interventions could be considered in the future to facilitate explanatory trials [119].
Outcome measures: The variability in findings from arts-based intervention trials is due, in part, to the lack of consistency in outcome measures across studies. One approach to address this issue is to establish a standardized, minimal set of core outcome measures. The MDS-UPDRS is currently the most commonly used scale for outcome measures in clinical trials. However, the MDS-UPDRS does not assess several outcomes, such as quality of life, stigma, loneliness, self-esteem, emotional well-being, interpersonal relations, which are often of high relevance in arts-based interventions. Measuring these additional outcomes is essential to understand and capture the multifaceted impact of creative activities. Thus, the unique dimensions impacted by arts-based interventions would need to be considered during the development of a set of core outcome measures. This approach will ensure a holistic evaluation of the interventions’ effectiveness. Further, if a standardized set of core outcomes is employed by all studies, this will facilitate comparative analysis across trials.
Personalizing the intervention: Personalized precision medicine is rapidly advancing in medicine, and we believe it is crucial for arts-based interventions. Most of the art-based therapy studies to date used a “one-size-fits-all” group approach and lacked individualization. Instead, we think that personalizing of art interventions is necessary, given that the production, perception, and appreciation of art is a highly individual experience. These interventions should be tailored to individual preferences and abilities. Although this poses challenges for future study designs, examples exist in the field of physiotherapy. For instance, PDSAFE, a personalized physiotherapy intervention for falls prevention in PD, used a customized approach to the specific fall mechanism and the participant’s functional presentation. Although this approach did not reduce falls (primary outcome), it improved balance, functional strength, and reduced near falls (secondary outcomes) [120, 121]. With this type of personalized medicine, individuals with PD could choose tailored art interventions, thus potentially enhancing adherence and efficacy. Although personalized delivery of these interventions may negate the need for rigid protocols, guidelines specific to PD individuals would bevaluable.
Limitations of this review
Firstly, certain articles might have been overlooked since this is a non-systematic literature review. Secondly, we acknowledge that, by broadly covering multiple arts-based interventions, we provided limited discussion about certain promising art interventions, such as specific visual arts categories (e.g., painting, sculpture) or diverse dance types (e.g., tango, tap dancing). Thirdly, the descriptions of upcoming research and community-based projects may be biased towards North American and European initiatives due to the authors’ locations. Lastly, we recognize the possibility of missing important initiatives on other continents and encourage readers to share with us updates on studies and initiatives not covered. This review primarily aims to inspire clinicians, researchers, and individuals with PD and their caregivers, serving as a call to action for further focus and research.
CONCLUSIONS
In summary, we provided a qualitative review of art-based interventions for individuals with PD, covering music, dance, drama, visual arts, and creative writing. These interventions show potential in enhancing both motor and non-motor symptoms, contributing to emotional, cognitive well-being, and overall quality of life. A unique feature of arts-based interventions is their adaptability to individuals’ specific needs, including existential aspects, fostering empowerment in dealing with PD. However, the heterogeneity and varying research quality limit firm conclusions and strong recommendations. Future studies should employ larger sample sizes and well-chosen control groups to enhance the reliability of the findings.
ACKNOWLEDGMENTS
We would like to express our sincere gratitude to Steven Iseman and Barbara Salsberg Mathews for graciously allowing us to publish the photos of their artwork. We thank Elianne Keulemans for generously permitting the publication of her late mother’s artwork.
FUNDING
PG received research support from the Canadian Health Institutes of Research, Parkinson Canada, and the Ontario Ministry of Health Clinician Investigator Program. BTMS received financial support as a postdoctoral researcher through the Unlocking the Muse project, funded by the #ConnectingMinds Grant from FWF der Wissenschaftsfond (CM1100-B). BRB is supported by a Center of Excellence grant of the Parkinson’s Foundation. LVK holds the Wolfond-Krembil Chair in Parkinson’s Disease Research.
CONFLICT OF INTEREST
PG and BTMS have no conflicts of interest relevant to the content of this article. BRB serves as co-editor-in-chief for the Journal of Parkinson’s Disease but was not involved in the peer-review process of this article nor had access to any information regarding its peer-review. LVK serves as co-editor-in-chief for the Journal of Parkinson’s Disease but was not involved in the peer-review process of this article nor had access to any information regarding its peer-review. LVK volunteers as a board member for the non-profit community organization Dancing with Parkinson’s.
REFERENCES
[1] | Bloem BR , Okun MS , Klein C ((2021) ) Parkinson’s disease, Lancet 397: , 2284–2303. |
[2] | Zhao N , Yang Y , Zhang L , Zhang Q , Balbuena L , Ungvari GS , Zang YF , Xiang YT ((2021) ) Quality of life in Parkinson’s disease: A systematic review and meta-analysis of comparative studies, CNS Neurosci Ther 27: , 270–279. |
[3] | Santos García D , de Deus Fonticoba T , Suárez Castro E , Borrué C , Mata M , Solano Vila B , Cots Foraster A , Álvarez Sauco M , Rodríguez Pérez AB , Vela L , Macías Y , Escalante S , Esteve P , Reverté Villarroya S , Cubo E , Casas E , Arnaiz S , Carrillo Padilla F , Pueyo Morlans M , Mir P , Martinez-Martin P ((2019) ) Non-motor symptoms burden, mood, and gait problems are the most significant factors contributing to a poor quality of life in non-demented Parkinson’s disease patients: Results from the COPPADIS Study Cohort, Parkinsonism Relat Disord 66: , 151–157. |
[4] | Lin J , Ou R , Wei Q , Cao B , Li C , Hou Y , Zhang L , Liu K , Shang H ((2022) ) Self-stigma in Parkinson’s disease: A 3-year prospective cohort study, Front Aging Neurosci 14: , 790897. |
[5] | Rukavina K , Batzu L , Boogers A , Abundes-Corona A , Bruno V , Chaudhuri KR ((2021) ) Non-motor complications in late stage Parkinson’s disease: Recognition, management and unmet needs, Expert Rev Neurother 21: , 335–352. |
[6] | Fox SH , Cardoso F ((2023) ) Unmet needs in Parkinson’s disease, Mov Disord Clin Pract 10: , S47–S49. |
[7] | Pelowski M , Spee BTM , Arato J , Dörflinger F , Ishizu T , Richard A ((2022) ) Can we really ‘read’ art to see the changing brain? A review and empirical assessment of clinical case reports and published artworks for systematic evidence of quality and style changes linked to damage or neurodegenerative disease, Physics Life Rev 43: , 32–95. |
[8] | Joutsa J , Martikainen K , Kaasinen V ((2012) ) Parallel appearance of compulsive behaviors and artistic creativity in Parkinson’s disease, Case Rep Neurol 4: , 77–83. |
[9] | Jung RE , Vartanian O , editors. In: ((2018) ) The Cambridge Handbook of the Neuroscience of Creativity, Cambridge University Press, Cambridge; 2018:i-ii. |
[10] | Lakke JPWF ((1994) ) Images of Parkinson’s disease, past and present, J Hist Neurosci 3: , 131–138. |
[11] | Pelowski M , Spee B , Richard A , Krack P , Bloem B ((2020) ) What Parkinson’s reveals about the artistic spark. Am Sci, 108: , 240. |
[12] | Kleiner-Fisman G , Lang AE ((2004) ) Insights into brain function through the examination of art: The influence of neurodegenerative diseases, Neuroreport 15: , 933–937. |
[13] | Inzelberg R ((2013) ) The awakening of artistic creativity and Parkinson’s disease, Behav Neurosci 127: , 256–261. |
[14] | Lakke JP ((1999) ) Art and Parkinson’s disease, Adv Neurol 80: , 471–479. |
[15] | Chatterjee A , Hamilton RH , Amorapanth PX ((2006) ) Art produced by a patient with Parkinson’s disease, Behav Neurol 17: , 105–108. |
[16] | Kulisevsky J , Pagonabarraga J , Martinez-Corral M ((2009) ) Changes in artistic style and behaviour in Parkinson’s disease: Dopamine and creativity, J Neurol 256: , 816–819. |
[17] | Drago V , Foster PS , Okun MS , Cosentino FII , Conigliaro R , Haq I , Sudhyadhom A , Skidmore FM , Heilman KM ((2009) ) Turning off artistic ability: The influence of left DBS in art production, J Neurol Sci 281: , 116–121. |
[18] | Lhommée E , Batir A , Quesada JL , Ardouin C , Fraix V , Seigneuret E , Chabardès S , Benabid AL , Pollak P , Krack P ((2014) ) Dopamine and the biology of creativity: Lessons from Parkinson’s disease, Front Neurol 5: , 55. |
[19] | Bellass S , Balmer A , May V , Keady J , Buse C , Capstick A , Burke L , Bartlett R , Hodgson J ((2018) ) Broadening the debate on creativity and dementia: A critical approach, Dementia 18: , 2799–2820. |
[20] | Groot B , de Kock L , Liu Y , Dedding C , Schrijver J , Teunissen T , van Hartingsveldt M , Menderink J , Lengams Y , Lindenberg J , Abma T ((2021) ) The value of active arts engagement on health and well-being of older adults: A nation-wide participatory study, Int J Environ Res Public Health 18: , 8222. |
[21] | Bloem BR , Volpe D ((2023) ) What art can tell us about the human brain, in health and disease: Comment on “Can we really ‘read’ art to see the changing brain?” by Matthew Pelowski et al, Phys Life Rev 45: , 52–55. |
[22] | Phillips L , Christensen-Strynø MB , Frølunde L ((2022) ) Arts-based co-production in participatory research: Harnessing creativity in the tension between process and product, Evid Policy 18: , 391–411. |
[23] | Sihvonen AJ , Särkämö T , Leo V , Tervaniemi M , Altenmüller E , Soinila S ((2017) ) Music-based interventions in neurological rehabilitation, Lancet Neurol 16: , 648–660. |
[24] | World Federation of Music Therapy ((2023) ) About WFMT. https://www.wfmt.info/about, Accessed October 18, 2023. |
[25] | Pohl P , Dizdar N , Hallert E ((2013) ) The Ronnie Gardiner Rhythm and Music Method – a feasibility study in Parkinson’s disease, Disabil Rehabil 35: , 2197–2204. |
[26] | Machado Sotomayor MJ , Arufe-Giráldez V , Ruíz-Rico G , Navarro-Patón R ((2021) ) Music therapy and Parkinson’s disease: A systematic review from 2015–2020, Int J Environ Res Public Health 18: , 11618. |
[27] | Zatorre RJ , Chen JL , Penhune VB ((2007) ) When the brain plays music: Auditory–motor interactions in music perception and production, Nat Rev Neurosci 8: , 547–558. |
[28] | Hyde KL , Lerch J , Norton A , Forgeard M , Winner E , Evans AC , Schlaug G ((2009) ) Musical training shapes structural brain development, J Neurosci 29: , 3019–3025. |
[29] | Schlaug G ((2015) ) Musicians and music making as a model for the study of brain plasticity, Prog Brain Res 217: , 37–55. |
[30] | Rose D , Cameron DJ , Lovatt PJ , Grahn JA , Annett LE ((2020) ) Comparison of spontaneous motor tempo during finger tapping, toe tapping and stepping on the spot in people with and without Parkinson’s disease, J Mov Disord 13: , 47–56. |
[31] | Ghai S , Ghai I , Schmitz G , Effenberg AO ((2018) ) Effect of rhythmic auditory cueing on parkinsonian gait: A systematic review and meta-analysis, Sci Rep 8: , 506. |
[32] | Rose D , Delevoye-Turrell Y , Ott L , Annett LE , Lovatt PJ ((2019) ) Music and metronomes differentially impact motor timing in people with and without Parkinson’s disease: Effects of slow, medium, and fast tempi on entrainment and synchronization performances in finger tapping, toe tapping, and stepping on the spot tasks, Parkinsons Dis 2019: , 6530838. |
[33] | Capato TTC , de Vries NM , IntHout J , Ramjith J , Barbosa ER , Nonnekes J , Bloem BR ((2020) ) Multimodal balance training supported by rhythmic auditory stimuli in Parkinson disease: Effects in freezers and nonfreezers, Phys Ther 100: , 2023–2034. |
[34] | Calabrò RS , Naro A , Filoni S , Pullia M , Billeri L , Tomasello P , Portaro S , Di Lorenzo G , Tomaino C , Bramanti P ((2019) ) Walking to your right music: A randomized controlled trial on the novel use of treadmill plus music in Parkinson’s disease, J Neuroeng Rehabil 16: , 68. |
[35] | Thaut MH , Rice RR , Braun Janzen T , Hurt-Thaut CP , McIntosh GC ((2019) ) Rhythmic auditory stimulation for reduction of falls in Parkinson’s disease: A randomized controlled study, Clin Rehabil 33: , 34–43. |
[36] | Spina E , Barone P , Mosca LL , Forges Davanzati R , Lombardi A , Longo K , Iavarone A , Amboni M ((2016) ) Music therapy for motor and nonmotor symptoms of Parkinson’s disease: A prospective, randomized, controlled, single-blinded study, J Am Geriatr Soc 64: , e36–e39. |
[37] | Barnish MS , Barran SM ((2020) ) A systematic review of active group-based dance, singing, music therapy and theatrical interventions for quality of life, functional communication, speech, motor function and cognitive status in people with Parkinson’s disease, BMC Neurol 20: , 371. |
[38] | Tamplin J , Morris ME , Marigliani C , Baker FA , Vogel AP ((2019) ) ParkinSong: A controlled trial of singing-based therapy for Parkinson’s disease, Neurorehabil Neural Repair 33: , 453–463. |
[39] | Hersh D , Kong SJ , Smith J ((2023) ) It’s quite good fun: A qualitative study of a singing/songwriting programme for people with Parkinson’s disease and their spouses, Int J Lang Commun Disord 58: , 2103–2116. |
[40] | Mohseni Z , Saffarian A , Mohamadi R , Abolghasemi J , Habibi SAH ((2023) ) Effect of conventional speech therapy combined with music therapy on swallowing in patients with Parkinson’s disease (telerehabilitation): A randomized-controlled trial, Middle East J Rehabil Health Stud 10: , e131572. |
[41] | Stegemöller EL , Hibbing P , Radig H , Wingate J ((2017) ) Therapeutic singing as an early intervention for swallowing in persons with Parkinson’s disease, Complement Ther Med 31: , 127–133. |
[42] | Irons JY , Hancox G , Vella-Burrows T , Han EY , Chong HJ , Sheffield D , Stewart DE ((2021) ) Group singing improves quality of life for people with Parkinson’s: An international study, Aging Ment Health 25: , 650–656. |
[43] | Bastepe-Gray S , Wainwright L , Lanham DC , Gomez G , Kim JS , Forshee Z , Kaas B , McCoy A , McGregor C , Moukheiber E , Rajan S , Suarez-Cedeno G , Wang J , Brennan S , Coughlin S , Kang K , Pantelyat A ((2022) ) GuitarPD: A randomized pilot study on the impact of nontraditional guitar instruction on functional movement and well-being in Parkinson’s disease, Parkinsons Dis 2022: , 1061045. |
[44] | Pantelyat A , Syres C , Reichwein S , Willis A ((2016) ) DRUM-PD: The use of a drum circle to improve the symptoms and signs of Parkinson’s disease (PD), Mov Disord Clin Pract 3: , 243–249. |
[45] | Wainwright L , Kang K , Dayanim G , Bedell C , Devlin K , Lanham D , Suarez-Cedeno G , Baker JA , Bastepe-Gray S , Bang J , Pantelyat A ((2023) ) DRUM-PD/HD: The impact of a pilot group drum-based music therapy intervention on quality of life and motor symptoms in Parkinson disease and Huntington disease, medRxiv, https://doi.org/10.1101/2023.05.04.23289514 [Preprint]. Posted May 05, 2023. |
[46] | Pohl P , Wressle E , Lundin F , Enthoven P , Dizdar N ((2020) ) Group-based music intervention in Parkinson’s disease – findings from a mixed-methods study, Clin Rehabil 34: , 533–544. |
[47] | Fodor DM , Breda XM , Valean D , Marta MM , Perju-Dumbrava L ((2021) ) Music as add-on therapy in the rehabilitation program of Parkinson’s disease patients-a Romanian pilot study, Brain Sci 11: , 569. |
[48] | Zhou Z , Zhou R , Wei W , Luan R , Li K ((2021) ) Effects of music-based movement therapy on motor function, balance, gait, mental health, and quality of life for patients with Parkinson’s disease: A systematic review and meta-analysis, Clin Rehabil 35: , 937–951. |
[49] | Pacchetti C , Mancini F , Aglieri R , Fundarò C , Martignoni E , Nappi G ((2000) ) Active music therapy in Parkinson’s disease: An integrative method for motor and emotional rehabilitation, Psychosom Med 62: , 386–393. |
[50] | de Bruin N , Doan JB , Turnbull G , Suchowersky O , Bonfield S , Hu B , Brown LA ((2010) ) Walking with music is a safe and viable tool for gait training in Parkinson’s disease: The effect of a 13-week feasibility study on single and dual task walking, Parkinsons Dis 2010: , 483530. |
[51] | Clinicaltrials.gov, NMT for Parkinson’s Disease, https://clinicaltrials.gov/study/NCT03049033?cond=Parkinson%20Disease&intr=Music%20therapy&rank=3#contacts-and-locations, Accessed October 19, 2023. |
[52] | Clinicaltrials.gov, Classical Guitar for Parkinson’s Disease, https://clinicaltrials.gov/study/NCT05917704?cond=Parkinson%20Disease&intr=Music%20therapy&rank=9, Accessed October 19, 2023. |
[53] | Clinicaltrials.gov, Music Therapy to Prevent Hospital-acquired Delirium in Parkinson’s Disease and Dementia With Lewy Bodies, https://clinicaltrials.gov/study/NCT06063161?cond=Parkinson%20Disease&intr=Music%20therapy&page=2&rank=13, Accessed October 19, 2023. |
[54] | Singing with Parkinson’s, Singing with Parkinson’s, Led by Paula Wolfson, https://singingwithparkinsons.com/, Accessed Oct 19th, 2023. |
[55] | Signature Therapy, Signature Therapy and Rehabilitation, A creative approach to therapy, https://www.signaturetherapy.ca/about, Accessed October 19, 2023. |
[56] | Music & Soul, An Alternative Way to Wellness: MUSIC THERAPY & REIKI, https://www.music-soul.online/, Accessed October 19, 2023. |
[57] | Parkinson’s Foundation, The George Foundation’s Singing with Parkinson’s in Roswell, GA, https://www.parkinson.org/living-with-parkinsons/stories/singing-with-parkinsons, Accessed October 20, 2023. |
[58] | Parkinson’s Europe, What if music could contribute to improving the daily life of people with Parkinson’s? https://www.parkinsonseurope.org/latest/news/what-if-music-could-contribute-to-improving-the-daily-life-of-people-with-parkinsons/, Accessed October 20, 2023. |
[59] | American Dance Therapy Association, What is Dance/Movement Therapy? Defining Dance/Movement Therapy (DMT). https://adta.memberclicks.net/what-is-dancemovement-therapy, Accessed October 20, 2023. |
[60] | Carapellotti AM , Stevenson R , Doumas M ((2020) ) The efficacy of dance for improving motor impairments, non-motor symptoms, and quality of life in Parkinson’s disease: A systematic review and meta-analysis, PLoS One 15: , e0236820. |
[61] | Krotinger A , Loui P ((2021) ) Rhythm and groove as cognitive mechanisms of dance Intervention in Parkinson’s disease, PLoS One 16: , e0249933. |
[62] | Calvo-Merino B , Glaser DE , Grèzes J , Passingham RE , Haggard P ((2005) ) Action observation and acquired motor skills: An FMRI study with expert dancers, Cereb Cortex 15: , 1243–1249. |
[63] | Batson G , Migliarese SJ , Soriano C , H. Burdette J , Laurienti PJ ((2014) ) Effects of improvisational dance on balance in Parkinson’s disease: A two-phase fMRI case study, Phys Occup Ther Geriatr 32: , 188–197. |
[64] | McMahon J , Chazot P ((2020) ) Dance and Parkinson’s: Biological perspective and rationale, Lifestyle Med 1: , e15. |
[65] | de Dreu MJ , Kwakkel G , van Wegen EE ((2015) ) Partnered dancing to improve mobility for people with Parkinson’s disease, Front Neurosci 9: , 444. |
[66] | Pinto C , Figueiredo C , Mabilia V , Cruz T , Jeffrey ER , Pagnussat AS ((2023) ) A safe and feasible online dance intervention for older adults with and without Parkinson’s disease, J Dance Med Sci 27: , 253–267. |
[67] | Aguiar LPC , da Rocha PA , Morris M ((2016) ) Therapeutic dancing for Parkinson’s disease, Int J Gerontol 10: , 64–70. |
[68] | Gros P , Van Ooteghem K , Robichaud S , Beyer KB , Tran S , Fox SH , Lim ASP , McIlroy W , Kalia LV ((2022) ) Feasibility of Recruiting Parkinson Disease Participants into Dance Intervention and Using Accelerometers for Objective Outcome Measures of Dance – a Pilot Study for a Future Randomized Controlled Trial. In Pan American Parkinson’s Disease and Movement Disorders Congress, Miami, Florida. |
[69] | Ventura MI , Barnes DE , Ross JM , Lanni KE , Sigvardt KA , Disbrow EA ((2016) ) A pilot study to evaluate multi-dimensional effects of dance for people with Parkinson’s disease, Contemp Clin Trials 51: , 50–55. |
[70] | Rios Romenets S , Anang J , Fereshtehnejad SM , Pelletier A , Postuma R ((2015) ) Tango for treatment of motor and non-motor manifestations in Parkinson’s disease: A randomized control study, Complement Ther Med 23: , 175–184. |
[71] | Carapellotti AM , Rodger M , Doumas M ((2022) ) Evaluating the effects of dance on motor outcomes, non-motor outcomes, and quality of life in people living with Parkinson’s: A feasibility study, Pilot Feasibility Stud 8: , 36. |
[72] | Ismail SR , Lee SWH , Merom D , Megat Kamaruddin PSN , Chong MS , Ong T , Lai NM ((2021) ) Evidence of disease severity, cognitive and physical outcomes of dance interventions for persons with Parkinson’s Disease: A systematic review and meta-analysis, BMC Geriatr 21: , 503. |
[73] | de Almeida HS , Porto F , Porretti M , Lopes G , Fiorot D , Bunn PDS , da Silva EB ((2021) ) Effect of dance on postural control in people with Parkinson’s disease: A meta-analysis review, J Aging Phys Act 29: , 130–141. |
[74] | Feenstra W , Nonnekes J , Rahimi T , Reinders-Messelink HA , Dijkstra PU , Bloem BR ((2022) ) Dance classes improve self-esteem and quality of life in persons with Parkinson’s disease, J Neurol 269: , 5843–5847. |
[75] | Hasan SM , Alshafie S , Hasabo EA , Saleh M , Elnaiem W , Qasem A , Alzu’bi YO , Khaled A , Zaazouee MS , Ragab KM , Nourelden AZ , Doheim MF ((2022) ) Efficacy of dance for Parkinson’s disease: A pooled analysis of 372 patients, J Neurol 269: , 1195–1208. |
[76] | Kalyani HHN , Sullivan KA , Moyle G , Brauer S , Jeffrey ER , Kerr GK ((2019) ) Impacts of dance on cognition, psychological symptoms and quality of life in Parkinson’s disease, Neurorehabilitation 45: , 273–283. |
[77] | Kalyani HHN , Sullivan K , Moyle G , Brauer S , Jeffrey ER , Roeder L , Berndt S , Kerr G ((2019) ) Effects of dance on gait, cognition, and dual-tasking in Parkinson’s disease: A systematic review and meta-analysis, J Parkinsons Dis 9: , 335–349. |
[78] | Wang LL , Sun CJ , Wang Y , Zhan TT , Yuan J , Niu CY , Yang J , Huang S , Cheng L ((2022) ) Effects of dance therapy on non-motor symptoms in patients with Parkinson’s disease: A systematic review and meta-analysis, Aging Clin Exp Res 34: , 1201–1208. |
[79] | Hackney ME , Bennett CG ((2014) ) Dance therapy for individuals with Parkinson’s disease: Improving quality of life, J Parkinsonism Restless Legs Syndrome 14: , 17–25. |
[80] | Colombo B , Rigby A , Gnerre M , Biassoni F ((2022) ) The effects of a dance and music-based intervention on Parkinson’s patients’ well-being: An interview study, Int J Environ Res Public Health 19: , 7519. |
[81] | Zhang Q , Hu J , Wei L , Jia Y , Jin Y ((2019) ) Effects of dance therapy on cognitive and mood symptoms in people with Parkinson’s disease: A systematic review and meta-analysis, Complement Ther Clin Pract 36: , 12–17. |
[82] | Morris ME , McConvey V , Wittwer JE , Slade SC , Blackberry I , Hackney ME , Haines S , Brown L , Collin E ((2023) ) Dancing for Parkinson’s disease online: Clinical trial process evaluation, Healthcare (Basel) 11: , 604. |
[83] | Bek J , Groves M , Leventhal D , Poliakoff E ((2021) ) Dance at home for people with Parkinson’s during COVID-19 and beyond: Participation, perceptions, and prospects, Front Neurol 12: , 678124. |
[84] | Emmanouilidis S , Hackney M , Slade S , Heng H , Jazayeri D , Morris M ((2021) ) Dance is an accessible physical activity for people with Parkinson’s disease, Parkinsons Dis 2021: , 7516504. |
[85] | Nimmons D , Armstrong M , Pigott J , Walters K , Schrag A , Ogunleye D , Dowridge W , Read J , Davies N ((2022) ) Exploring the experiences of people and family carers from under-represented groups in self-managing Parkinson’s disease and their use of digital health to do this, Digit Health 8: , 20552076221102261. |
[86] | Delextrat A , Bateman J , Esser P , Targen N , Dawes H ((2016) ) The potential benefits of Zumba Gold(®) in people with mild-to-moderate Parkinson’s: Feasibility and effects of dance styles and number of sessions, Complement Ther Med 27: , 68–73. |
[87] | Dancing with Parkinson’s Canada, Dancing with Parkinson’s, https://www.dancingwithparkinsons.com/, Accessed January 21, 2024. |
[88] | Dance for PD, Take a class, in person, global, https://danceforparkinsons.org/take-a-class/global/, Accessed October 23, 2023. |
[89] | North American Drama Therapy Association, What is Drama Therapy?, https://www.nadta.org/what-is-drama-therapy, Accessed October 23, 2023. |
[90] | Modugno N , Iaconelli S , Fiorlli M , Lena F , Kusch I , Mirabella G ((2010) ) Active theater as a complementary therapy for Parkinson’s disease rehabilitation: A pilot study, Scientific World Journal 10: , 2301–2313. |
[91] | Mirabella G , De Vita P , Fragola M , Rampelli S , Lena F , Dilettuso F , Iacopini M , d’Avella R , Borgese MC , Mazzotta S , Lanni D , Grano M , Lubrani S , Modugno N ((2017) ) Theatre is a valid add-on therapeutic intervention for emotional rehabilitation of Parkinson’s disease patients, Parkinsons Dis 2017: , 7436725. |
[92] | Keisari S ((2021) ) Expanding the role repertoire while aging: A drama therapy model, Front Psychol 12: , 635975. |
[93] | Mondolfi M , Savage M , Fernández-Aguayo S ((2021) ) Designing short-term drama therapy with people who have Parkinson’s disease in Vigo, Spain, Drama Ther Rev 7: , 37–59. |
[94] | Florida Hospital ((2018) ) 2018 Parkinson’s Empowerment Programs (pamphlet), ed. Florida Hospital Parkinson Outreach Center, p. 10. |
[95] | Rehacare International, Music and Drama Therapy for Parkinson’s Patients, https://www.rehacare.com/en/Archive/Archive_search/Music_and_Drama_Therapy_for_Parkinson_s_Patients, Accessed October 24, 2023. |
[96] | Mathews BS ((2023) ) Mime Over Mind – a therapeutic tool to help manage Parkinson’s (Blog), Journal of Parkinson’s Disease, https://www.journalofparkinsonsdisease.com/blog/guest-blog/mime-over-mind-therapeutic-tool-help-manage-parkinson%E2%80%99s. Accessed September 20, 2023. |
[97] | Mermin R ((2023) ) Mime Over Matter, https://robmermin.com/, Accessed October 24, 2023. |
[98] | Bae YS , Kim DH ((2018) ) The applied effectiveness of clay art therapy for patients with Parkinson’s disease, J Evid Based Integr Med 23: , 2515690x18765943. |
[99] | Ettinger T , Berberian M , Acosta I , Cucca A , Feigin A , Genovese D , Pollen T , Rieders J , Kilachand R , Gomez C , Kaimal G , Biagioni M , Di Rocco A , Ghilardi FM , Rizzo JR ((2023) ) Art therapy as a comprehensive complementary treatment for Parkinson’s disease, Front Hum Neurosci 17: , 1110531. |
[100] | Safar LT , Press DZ ((2011) ) Art and the brain: Effects of dementia on art production in art therapy. Art Therapy 28: , 96–103. |
[101] | Elkis-Abuhoff DL , Gaydos M ((2018) ) Medical art therapy research moves forward: A review of clay manipulation with Parkinson’s disease, Art Therapy 35: , 68–76. |
[102] | Pelowski M , Chamberlain R ((2023) ) Where do artists come from? A review of the ‘typical’ visually creative life and artistic brain as a basis for discussing neurodivergence or neurodegenerative change. In Art and Neurological Disorders: Illuminating the Intersection of Creativity and the Changing Brain, Richard A, Pelowski M, Spee BTM, eds. Springer International Publishing, Cham, pp, 25–63. |
[103] | Cucca A , Di Rocco A , Acosta I , Beheshti M , Berberian M , Bertisch HC , Droby A , Ettinger T , Hudson TE , Inglese M , Jung YJ , Mania DF , Quartarone A , Rizzo JR , Sharma K , Feigin A , Biagioni MC , Ghilardi MF ((2021) ) Art therapy for Parkinson’s disease, Parkinsonism Relat Disord 84: , 148–154. |
[104] | Ghadim MR , Daugherty L ((2021) ), Museum-based art therapy: A collaborative effort with access, education, and public programs, Routledge. |
[105] | Pelowski M, Crone JS, Spee BTM, in collaboration with Bloem B. Der Wissenschaftsfonds, #ConnectingMinds Programme with the short title: Unlocking the Muse. Grant Number: CM 1100-B. |
[106] | Parkinson’s Foundation, Painting with Parkinson’s: All About Art Therapy, https://www.parkinson.org/blog/research/art-therapy, Accessed October 25, 2023. |
[107] | American Art Therapy Association, American Art Therapy Association, https://arttherapy.org/, Accessed October 28, 2023. |
[108] | Bratschi U ((2023) ) The artistic view with Parkinson’s disease: In search of “why”. In Art and Neurological Disorders: Illuminating the Intersection of Creativity and the Changing Brain, Richard A, Pelowski M, Spee BTM, eds. Springer International Publishing, Cham, pp, 287–294. |
[109] | Bratschi U, Feeding the Spark, http://www.neurologie.insel.ch/de/unser-angebot/zentrum-fuer-parkinson-und-bewegungsstoerungen/feeding-the-spark, Accessed January 11, 2024. |
[110] | FernwerkFilms597, Fernwerk Films, https://www.youtube.com/@fernwerkfilms597/videos, Accessed January 11, 2024. |
[111] | King R , Neilsen P , White E ((2013) ) Creative writing in recovery from severe mental illness, Int J Ment Health Nurs 22: , 444–452. |
[112] | Krpan KM , Kross E , Berman MG , Deldin PJ , Askren MK , Jonides J ((2013) ) An everyday activity as a treatment for depression: The benefits of expressive writing for people diagnosed with major depressive disorder, J Affect Disord 150: , 1148–1151. |
[113] | Nesterova D , Zhu J , Kramer C , Vasekar M , Truica C , Joshi A , Hayes M , Kessler J , Saunders EFH , Drabick JJ , Joshi M ((2022) ) Group-led creative writing and behavioural health in cancer: A randomised clinical trial, BMJ Support Palliat Care 12: , 91–98. |
[114] | Parkinson’s Europe, Leisure, creativity and creative therapies, https://www.parkinsonseurope.org/living-well/wellbeing/leisure-creativity-and-creative-therapies/, Accessed October 27, 2023. |
[115] | Parkinson Society British Columbia, Writing & Journaling: A Fun Way to Rediscover Your Inherent Creativity, https://www.parkinson.bc.ca/resources-services/coronavirus/covid19-hobby-series/writing-journaling-a-fun-way-to-rediscover-your-inherent-creativity/, Accessed October 27, 2023. |
[116] | Parkinson’s UK ((2017) ) Express yourself, Your creative writing toolkit (pamphlet), London, UK, 25 pages. |
[117] | Patsopoulos NA ((2011) ) A pragmatic view on pragmatic trials, Dialogues Clin Neurosci 13: , 217–224. |
[118] | Thompson BT , Schoenfeld D ((2007) ) Usual care as the control group in clinical trials of nonpharmacologic interventions, Proc Am Thorac Soc 4: , 577–582. |
[119] | Foltynie T , Gandhi S , Gonzalez-Robles C , Zeissler M-L , Mills G , Barker R , Carpenter J , Schrag A , Schapira A , Bandmann O , Mullin S , Duffen J , McFarthing K , Chataway J , Parmar M , Carroll C , EJS ACT-PD Consortium ((2023) ) Towards a multi-arm multi-stage platform trial of disease modifying approaches in Parkinson’s disease, Brain 146: , 2717–2722. |
[120] | Hulbert S , Chivers-Seymour K , Summers R , Lamb S , Goodwin V , Rochester L , Nieuwboer A , Rowsell A , Ewing S , Ashburn A ((2021) ) ‘PDSAFE’ – a multi-dimensional model of falls-rehabilitation for people with Parkinson’s. A mixed methods analysis of therapists’ delivery and experience, Physiotherapy 110: , 77–84. |
[121] | Chivers Seymour K , Pickering R , Rochester L , Roberts HC , Ballinger C , Hulbert S , Kunkel D , Marian IR , Fitton C , McIntosh E , Goodwin VA , Nieuwboer A , Lamb SE , Ashburn A ((2019) ) Multicentre, randomised controlled trial of PDSAFE, a physiotherapist-delivered fall prevention programme for people with Parkinson’s, J Neurol Neurosurg Psychiatry 90: , 774–782. |




