The Causes and Impact of Crisis for People with Parkinson’s Disease: A Patient and Carer Perspective
Abstract
Background:
The reasons for acute hospital admissions among people with Parkinson’s disease are well documented. However, understanding of crises that are managed in the community is comparatively lacking. Most existing literature on the causes of crisis for people with Parkinson’s disease (PwP) uses hospital data and excludes the individual’s own perspective on the crisis trigger and the impact of the crisis on their care needs.
Objective:
To identify the causes and impact of crises in both community and hospital settings, from a patient and carer perspective.
Methods:
A total of 550 UK-based PwP and carers completed a survey on (a) their own personal experiences of crisis, and (b) their general awareness of potential crisis triggers for PwP.
Results:
In addition to well-recognised causes of crisis such as falls, events less widely associated with crisis were identified, including difficulties with activities of daily living and carer absence. The less-recognised crisis triggers tended to be managed more frequently in the community. Many of these community-based crises had a greater impact on care needs than the better-known causes of crisis that more frequently required hospital care. PwP and carer responses indicated a good general knowledge of potential crisis triggers. PwP were more aware of mental health issues and carers were more aware of cognitive impairment and issues with medications.
Conclusion:
These findings could improve care of Parkinson’s by increasing understanding of crisis events from the patient and carer perspective, identifying under-recognised crisis triggers, and informing strategies for best recording symptoms from PwP and carers.
INTRODUCTION
Parkinson’s disease is the second most-common neurodegenerative disease in older people, affecting between 1.3 and 1.5%of persons aged over 60 years [1]. As the worldwide population ages, the number of people with Parkinson’s disease is set to increase, and with it the need for health and care resources. People with Parkinson’s disease (PwP) are significantly more likely to visit their GP and visit or be admitted to hospital than people in the general population [2, 3]. There is no standardised definition of ‘crisis’ and previous attempts to produce one have revealed the idiosyncratic use of the term [4]. For the purposes of this study, we define ‘crisis’ as a sudden or unexpected increase in the care required by the PwP. This has similarities to previous definitions that identify a “stressor” or “serious occasion or turning point” that lead to an obstacle requiring resolution [5, 6]. Our definition is based on the concept of a “serious occasion”, but with an emphasis on the care required to resolve it. The definition used here is the same as the lay definition provided to the participants, and includes events leading to a sudden or unexpected increase in community- and hospital-based care.
Three systematic reviews, including one meta-analysis, have been carried out into the causes of hospital admissions for PwP [7–9]. These studies most commonly identify falls, an exacerbation of motor and non-motor symptoms associated with the condition, cardiovascular complications, and infections to be the leading causes of hospitalisation for PwP [7–9]. Of the 17 studies featured in these systematic reviews, only 3 indicate the inclusion of patient-recorded data in their methodology [10–12]. In all of these, patient perspectives are reduced into pre-determined categories. The reasons for crises that are managed in the community have received much less attention in the literature. This research tends to focus on the causes of crises that are managed within primary care services within the context of cost and resource utilisation analysis [13, 14].
The present study sought to take a holistic approach to understanding the causes and impact of crises for PwP from the perspective of patients and carers, including events managed in the community, in hospital and both. The study focussed on PwP’s and carers’ personal experiences of crisis and on their general awareness of potential crisis triggers, utilising free text responses to allow the participants’ perspectives to be recorded in their own words. The aim of the study was to increase understanding on how best to identify those at risk of crisis.
MATERIALS AND METHODS
Recruitment of participants
PwP and carers were invited to take part in a survey through NHS clinics and local Parkinson’s UK support groups across the south and south west of England, and information was posted on the national Parkinson’s UK website in order to achieve national geographical spread. The survey was open to any PwP and any person who cared for a person with Parkinson’s. Carers were described to participants as a family member, partner or friend who knows the patient well and provides care, assistance or support due to their neurological condition. As the research aimed to shed light on the causes of crisis from the perspective of those with everyday lived experiences of the condition, paid carers were not included in the study.
The PwP and carers were not paired. The survey was offered online, on paper or over the phone. Participants received the participant information sheet (PIS) via email, through the post or downloaded from the survey webpage. Participants were required to confirm they had read the PIS and consented to participating in the study by ticking a checkbox before proceeding to the survey questions. There was no minimum or maximum time period between receiving the PIS and completing the survey. The data was collected between December 2016 and February 2020. The study received full ethical approval from the University of Southampton (ERGO 23026) and South Central Hampshire A-Research Ethics Committee (reference number 203783). We aimed to achieve a sample size of 500 participants.
Data collection
The survey asked about participants’ experiences of crisis, defined as a sudden or unexpected increase in care needs, and asked about individuals’ general awareness of causes of crisis.
Demographic information
Participants completed sociodemographic questions and the EQ-5D-3L health status questionnaire.
Personal experience of crisis
Participants were asked to detail up to three events that had caused a sudden increase in care need for the PwP (‘crises’) in the past five years (or since diagnosis if less than five years). The participants were asked what event had occurred that led to the PwP requiring extra care. Participants were asked follow-up questions regarding the location of care received, the extent of the increase in care needs, and the duration of the increased care requirement. Participants could indicate whether the crisis was managed in the community, in hospital, in both the community and hospital, or in another location. Participants were asked whether they considered the increase in care required to be small, medium or large, and whether the increase in care was temporary and lasted less than three months, temporary but lasted more than three months, or permanent.
General awareness of crisis
Participants were later asked to list up to eight events that they were aware of that could lead to a sudden increase in care requirements for PwP in general.
Data analysis
All responses for the causes of crisis (both experienced and identified through general awareness) were analysed using conventional content analysis, adopting an inductive, data-driven thematic coding method to allow “the categories and names for categories to flow from the data” [15]. Responses were analysed to identify the cause of crisis from the perspective of the patient or carer, before creating themes and then meta themes. The coded items and themes were reviewed by a research physiotherapist and a clinical research fellow with expertise in Parkinson’s disease. The data were also presented at a Parkinson’s UK support group with research participants present for respondent validation. Coded items and themes were revised during these validation processes. The thematic data were analysed: to identify the causes of the crisis that participants had experienced personally; to identify the causes of crisis of which participants had a general awareness; to compare patient and carer responses; to compare the causes of crisis identified through experience and through general awareness. The coding map created and used in the thematic analysis can be found in the Supplementary Material.
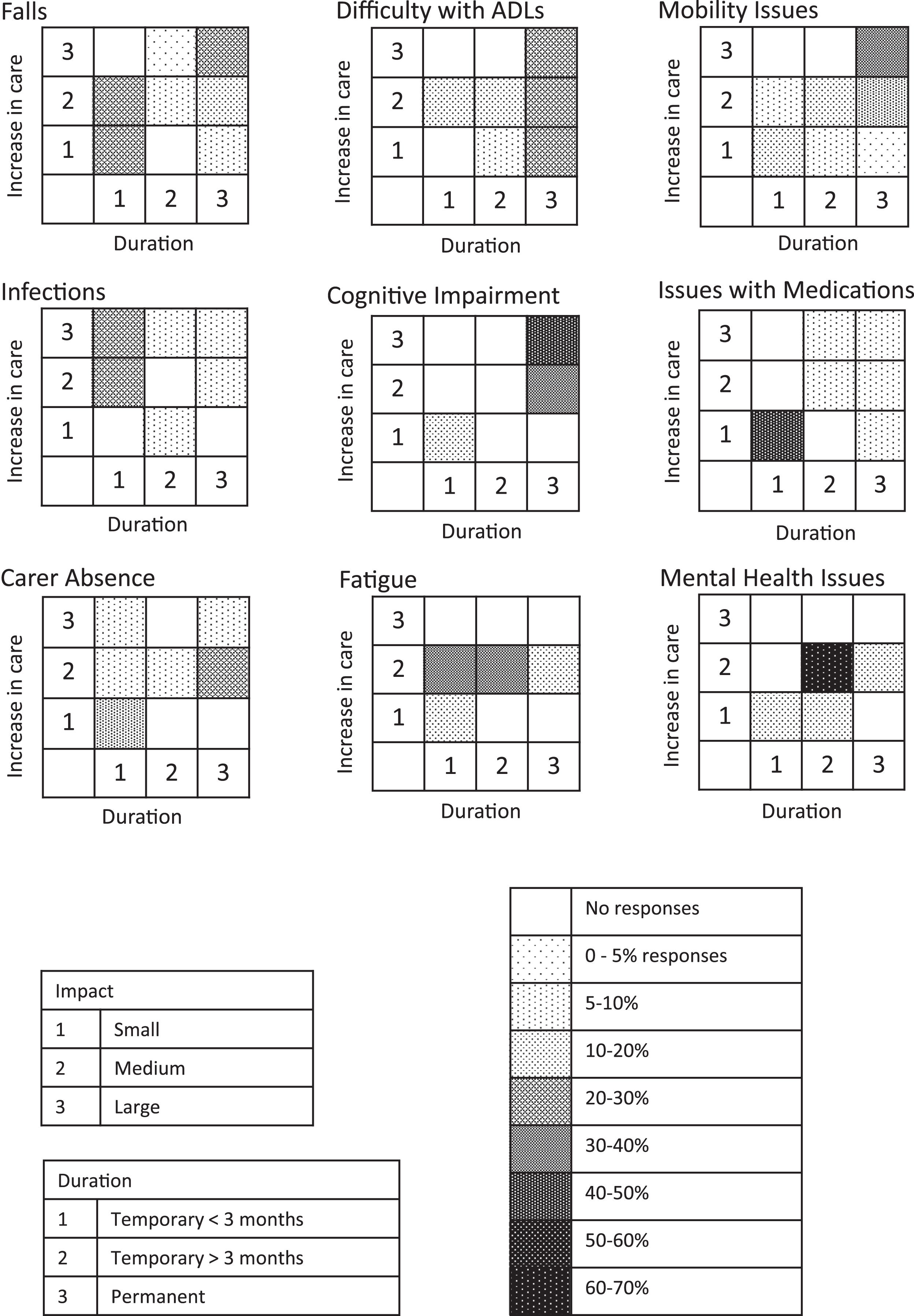
The data on the extent and duration of the increase in care needs were analysed using descriptive statistics to produce heat map plots in order to compare tendencies among different causes of crisis.
RESULTS
401 PwP and 149 carers completed the survey (total 550 participants). Of the PwP participants, 43%were women and 57%were men. Of the carer participants who answered questions about the PwP they supported, 74%were women and 26%were men, caring for 32%women and 68%men. Carer participants’ responses were based on a PwP cohort with a higher proportion of disability than the cohort of PwP participants (Table 1). Participants living in central southern England accounted for 77%of respondents, with 23%of participants recruited nationally. Just over half of respondents completed the survey online and just under half of respondents completed it on paper. Only 4 participants chose to complete the survey over the phone.
Table 1
Demographic information and health status of PwP by participant type
| PwP participants1 | Carer participants | PwP being cared for by carer participant | |
| Male | 226 (57%) | 39 (26%) | 101 (68%) |
| Female | 168 (43%) | 110 (74%) | 48 (32%) |
| Demographic and health status of PwP | |||
| Mean age (age range) | 70.7 years (40 –91) | 72.2 years (41 –89) | |
| Mean years since diagnosis | 6.1 years (0 –38) | 6.6 years (0 –18) | |
| (years since diagnosis range) | |||
| Self-reported by PwP | Reported by carer | ||
| EQ-5D - PwP has: | |||
| Problem with mobility | 68% | 76% | |
| Problem with self-care | 40% | 61% | |
| Problem with usual activities | 70% | 84% | |
| Pain and discomfort | 66% | 76% | |
| Anxiety and depression | 53% | 70% | |
17 PwP participants did not provide their gender.
The causes and impact of personally experienced crisis in Parkinson’s disease
PwP and carers reported 280 personally experienced moments of crisis. These events covered increases in care that were managed in the community (49%), at hospital (15%), in both the community and at hospital (31%), or other (5%), which included private hospital or therapists, community centre, charity or care home.
The most commonly identified events were falls, difficulty with activities of daily living, mobility issues, infections, cognitive impairment, issues with medications, carer absence, fatigue, and mental health issues (Table 2). Difficulty with activities of daily living (ADLs) included difficulties with self-care (including washing, dressing, toileting), housework (including cooking, laundry, cleaning), crossing roads, shopping, reading information, driving, and taking medications correctly.
Table 2
Causes of crises identified through the personal experiences of PwP and carers
| Number of cases (%of total cases) N = 280 | %of cases that required hospital care1 | |
| Motor complications | 90 (32) | 47 |
| Falls | 50 (18) | 54 |
| Loss of balance | 5 (2) | |
| Mobility issues | 26 (9) | 13 |
| Including hip/knee Replacements | 5 (2) | |
| Reduced dexterity | 2 (1) | |
| Involuntary movements | 2 (1) | |
| Difficulty with activities of daily living | 40 (14) | 18 |
| Co-occurring health conditions | 29 (10) | 38 |
| Infections2 | 13 (5) | 83 |
| Respiratory | 8 (3) | |
| Other | 5 (2) | |
| Cardiovascular conditions | 8 (3) | |
| Other illness or co-morbidity | 8 (3) | |
| Psychiatric symptoms | 21 (8) | 22 |
| Cognitive impairment | 11 (4) | 20 |
| Mental health issues | 10 (4) | 25 |
| Fatigue &sleep problems | 19 (7) | |
| Fatigue | 11 (4) | 9 |
| Sleep problems | 8 (3) | |
| Social and support | 13 (5) | 23 |
| Loss of social contact or social skills | 2 (1) | |
| Carer absence | 11 (4) | 27 |
| Issues with medications | 11 (4) | 36 |
| Speech &swallowing problems | 11 (4) | 25 |
| Problems with speech and communication | 9 (3) | |
| Problems with eating and swallowing | 2 (1) | |
| Incontinence | 8 (3) | |
| Constipation | 4 (1) | |
| Accidents and injuries | 7 (3) | |
| Progression of disease | 6 (2) | |
| Pain | 4 (1) | |
| Other3 | 17 (6) |
1Only causes of crisis with more than 10 cases where location of care was noted were analysed. 2Urinary tract infections are included in other infections. 3 Other responses reported more than once include fainting / losing consciousness (3), extra care required after hospitalisation (2), poisoning (2).
Of the events reported by at least 10 participants, those that most commonly resulted in a visit to hospital were infections, falls, issues with medications, carer absence, mental health issues, and cognitive impairment (Table 2). Difficulty with activities of daily living, mobility issues and fatigue were comparatively less likely to result in a hospital visit.
The nine events reported by at least 10 participants were analysed to identify trends in the impact on the care needs of the PwP, focusing on the extent and the duration of the increase in needs. Falls tended to have either a small, short-term impact or a large, long-term impact. Difficulty with ADLs produced small, moderate, or large increases in care needs, but the increase tended to be long-term. Mobility issues varied in impact across cases, with a slightly greater number of cases producing a large, long-term impact, whereas infections tended to have a moderate to large but short-term impact. Issues with medications tended to produce a small, short-term impact, and cognitive impairment a moderate to high, long-term impact. Carer absence varied in impact across cases. The impact of fatigue tended to be moderate and of short- to medium-term and mental health issues caused a moderate, medium-term impact (Fig. 1). Thus falls, difficulty with ADLs mobility issues and cognitive impairment were more likely to cause a larger long-term impact on care needs.
Fig. 1
Plots depicting the impact of crises from a patient and carer perspective. Extent of increase in care and duration of increase in care by percentage of cases.
Causes of crisis in Parkinson’s disease: general awareness
PwP and carers were asked to list up to eight events that they were aware of that could lead to a sudden or unexpected increase in care requirements for a person with Parkinson’s disease. The total number of reported events was 1156.
Falls were the most commonly cited cause of crisis, followed by difficulty with activities of daily living, mobility issues, cognitive impairment, mental health issues, problems with eating and swallowing, carer absence, the loss of social contact or skills, and issues with medications (Table 3).
Table 3
Causes of crises identified through the general awareness of PwP and carers. Patient and carer responses analysed separately and combined
| Patient responses N = 830 n (%) | Carer responses N = 326 n (%) | Total patient and carer N = 1156 n (%) | |
| Motor complications | 344 (42) | 128 (40) | 472 (41) |
| Falls | 213 (26) | 94 (29) | 307 (27) |
| Loss of balance | 16 (2) | 2 (1) | 18 (2) |
| Mobility issues | 90 (11) | 26 (8) | 116 (10) |
| Reduced dexterity | 6 (1) | 1 (0.3) | 7 (1) |
| Involuntary movements | 19 (2) | 5 (2) | 24 (2) |
| Difficulty with activities of daily living | 111 (13) | 27 (8) | 138 (12) |
| Co-occurring health conditions | 60 (7) | 28 (9) | 88 (8) |
| Infections1 | 18 (2) | 8 (3) | 26 (2) |
| Respiratory | 8 (1) | 1 (0.3) | 9 (1) |
| Other | 10 (1) | 10 (3) | 20 (2) |
| Cardiovascular conditions | 13 (2) | 4 (1) | 17 (2) |
| Other illness or co-morbidity | 11 (1) | 5 (2) | 16 (1) |
| Psychiatric symptoms | 89 (11) | 39 (12) | 128 (11) |
| Cognitive impairment | 41 (5) | 27 (8) | 68 (6) |
| Mental health issues | 48 (6) | 12 (4) | 60 (5) |
| Fatigue &sleep problems | 20 (2) | 6 (2) | 26 (2) |
| Fatigue | 12 (1) | 3 (1) | 15 (1) |
| Sleep problems | 8 (1) | 3 (1) | 11 (1) |
| Social and support | 63 (8) | 22 (7) | 85 (7) |
| Loss of social contact or social skills | 30 (4) | 8 (3) | 38 (3) |
| Carer absence | 33 (4) | 14 (4) | 47 (4) |
| Issues with medications | 18 (2) | 16 (5) | 34 (3) |
| Speech &swallowing problems | 53 (6) | 15 (5) | 68 (6) |
| Problems with speech and communication | 14 (2) | 1 (0.3) | 15 (1) |
| Problems with eating and swallowing | 39 (5) | 14 (4) | 53 (5) |
| Constipation | 9 (1) | 6 (2) | 15 (1) |
| Incontinence | 7 (1) | 8 (3) | 15 (1) |
| Accidents and injuries | 12 (1) | 5 (2) | 17 (2) |
| Progression of disease | 13 (2) | 3 (1) | 16 (1) |
| Pain | 2 (0.2) | 3 (1) | 5 (0.4) |
| Other2 | 29 (4) | 20 (6) | 49 (4) |
1Urinary tract infections are included in other infections. 2Other responses reported more than once include fainting / losing consciousness (4), dehydration (3), loss of control (3), cold weather (2), road accident (2) and poisoning (2).
A comparison between patient and carer perspectives in general awareness, showed a notable consistency in the causes of crisis identified and the frequency with which each cause was identified between the two groups. However, carers were more than twice as likely to identify issues with medication than PwP and more than one and a half times more likely than PwP to identify cognitive impairment as a cause of crisis. PwP were marginally more likely than carers to identify mental health issues as a cause of crisis.
Causes of crisis: personal experiences and general awareness compared
There was a high degree of concordance between the causes of crisis identified through personal experiences of PwP and carers and through their general awareness, with 8 of the 10 top causes the same (Table 4). In both cases, falls, difficulties with ADLs and mobility issues made up over 40%of the total responses (42%for personal experiences and 49%for general awareness). Two areas appeared more frequently in experiences than in general awareness: fatigue and problems with speech and communication. Conversely, problems with eating and swallowing and the loss of social contact or skills appeared more frequently in general awareness than in personal experiences.
Table 4
Main causes of crisis identified through personal experiences and general awareness compared
| PwP and carer personal experiences | PwP and carer general awareness | ||
| Cause of crisis | %of total responses | Cause of crisis | %of total responses |
| Falls | 18 | Falls | 27 |
| Difficulty with activities of daily living | 14 | Difficulty with activities of daily living | 12 |
| Mobility issues | 9 | Mobility issues | 10 |
| Infections | 5 | Cognitive impairment | 6 |
| Cognitive impairment | 4 | Mental health issues | 5 |
| Issues with medications | 4 | Problems with eating and swallowing* | 5 |
| Carer absence | 4 | Carer absence | 4 |
| Fatigue* | 4 | Loss of social contact or skills* | 3 |
| Mental health issues | 4 | Issues with medications | 3 |
| Problems with speech and communication* | 3 | Infections | 2 |
*Factors that only appear either in personal experiences or in general awareness within the most common 10 causes of crisis.
DISCUSSION
Existing studies on the causes of crisis for PwP are largely focused on reasons for hospitalisation and most often use clinician recorded data. This study aims to better understand the patient and carer perspective on the causes and impact of crises that are managed in either the community, in hospital or both. The results identify less commonly recognised crisis triggers; reveal that crises managed in the community can have an equal or greater impact that those requiring hospital care; highlight differences between PwP and carer awareness of crisis triggers; and identify potentially under-recognised crisis triggers amongst the PwP and carer population.
Less commonly recognised crisis triggers
This study has identified three causes of crisis that do not appear in previous research: difficulty with activities of daily living, carer absence, and loss of social contact or skills. Together these accounted for around 20%of crises described by our participants.
Falls and difficulty with ADLs are identified as the two most common causes of crisis for PwP. Falls have featured prominently in the literature on causes of crisis, yet difficulties with ADLs have more often been studied in relation to quality of life [16, 17]. Whilst carer absence has not previously been explicitly identified as a cause of crisis, the absence of a carer has been associated with a lower quality of life for PwP and poorer patient outcomes [18]. Previous studies have identified that PwP are aware of their loss of social skills [19], often feel a stigma around the visual manifestations of their condition, and that this can lead to social challenges [20]. Less social engagement has been associated with more rapid motor decline in older people [21]. Our research builds upon the current literature, which associates difficulty with ADLs, carer absence and social isolation with a lower quality of life and poorer outcomes, to reveal that PwP and carers also link these factors directly to a moment of crisis.
One explanation for the more common identification of ADLs and carer absence in this study may be the fact that crises caused by difficulties with ADLs and carer absence appear from our data to be largely managed in the community and may therefore be less evident in hospital data. Neither difficulty with ADLs nor carer absence presented a smaller or shorter-term increase in care compared to other crisis triggers, which suggests that the relative paucity of these events in the literature is not due to a comparatively smaller impact. Another explanation may be that PwP and carer perspectives identify a crisis as emanating from a difficulty with ADLs or carer absence, while healthcare professionals may interpret or record the crisis differently, emphasising the medical reason for the reduced ability to carry out ADLs rather than the functional difficulty itself or the health consequences of the carer absence. For example, one participant cited the death of her husband leading directly to an increase in unsteadiness and an eventual fall. In this scenario, whilst the patient perspective emphasised the sudden absence of a carer as the crisis trigger, the event could be identified by a healthcare professional as a fall. In this case, the absence of the carer may be a precursor to another crisis event that is more readily recorded by healthcare professionals.
Difficulties with ADLs, carer absence and the loss of social skills and contact are currently associated with a lower quality of life. However, recognising that they might be the factors that PwP and carers use to describe the trigger to a crisis or that they might be the precursor to a health crisis can ensure that clinicians ask the right questions, using the right language when assessing a PwP for risk of crisis.
Impact of crisis on care needs
Interestingly, there was no evident correlation between a crisis trigger having an increased likelihood of hospital admission and an increased impact on care needs. This is despite evidence that stays in hospital are associated with poorer outcomes for PwP [22]. In terms of the size of the increase in care, from the PwP and carer perspective there was no discernible difference between community-managed and hospital-managed crises. In terms of duration of the increase in care, community-managed crises appeared to have an equal or greater duration than those that resulted in hospital care. We report that difficulty with ADLs, mobility issues and cognitive impairment tend to have a long-term impact; infections and falls tend to have a short-term and short or long-term impact respectively. This might suggest that difficulty with ADLs, mobility issues and cognitive impairment tend to be acute-on-chronic crises, whilst infections tend to be very acute, and falls are either very acute or acute-on-chronic.
With the care needs of people with Parkinson’s disease managed between home, the community and hospital, and the future potential for developing and implementing home-based digital self-management applications, it is important to recognise that the true impact of crisis events will be missed if we rely on hospital admission statistics to identify them.
PwP and carer general knowledge of causes of crisis
The high degree of concordance between the causes of crisis identified through personal experiences of participants and through their general awareness suggests that PwP and their carers possess a good, general knowledge of potential causes of crisis within and outside of their own personal experiences. Many participants were recruited from Parkinson’s clinics with associated patient and carer education programmes, and Parkinson’s UK, which provides extensive information on the condition to its members.
Our data suggest that PwP are more aware of mental health issues than carers. This is despite the tendency of PwP to under-report mental health issues to their clinicians [23]. This may be because mental health issues can be acutely personal. Conversely, carers appear from our data to be more aware of cognitive impairment; perhaps because it is more noticeable to those around PwP than to individuals themselves. Our findings support previous research showing patients underestimate their symptoms of dementia and identifying carers to be reliable informants, especially in domains such as memory loss and topographical disorientation (navigation) [24, 25]. Carers also appear to be more aware of medication issues. Non-adherence to medication is a significant problem in Parkinson’s disease [26] and carers have indicated a desire for more information on medication and its side effects [27]. Carers may therefore be more personally mindful of it in cases where the PwP experiences cognitive problems, and it may represent an area in which they feel more involved in the care of a PwP.
The increased occurrence of fatigue and speech and communication issues identified as causes of crisis through experiences compared to general awareness might suggest that these factors are possibly under-recognised by PwP and carers as potential triggers. Despite fatigue being reported to be the most bothersome symptom of Parkinson’s disease by a third of PwP [28], it is often under-recognised by clinicians [29], and our data would suggest that it is also under-recognised by PwP and carers as a potential trigger for crisis associated with the condition.
The differing frequencies of PwP and their carers in identifying mental health issues, cognitive impairment and issues with medications as potential causes of crisis point to an important area to consider when collecting patient/carer-recorded symptoms. The fact that PwP and carers appear to be less aware of fatigue and speech and language issues as potential crisis triggers might suggest areas for future education programmes.
Limitations
The researchers were aware of the limitations of asking participants about personal experiences and general awareness in the same survey and that response to one question may influence the other. To mitigate against this, participants were first asked about their personal experiences and later in the survey about general awareness.
The survey was anonymous and open nationally to all PwP and carers. We are unable to quantify the degree to which patient and carer data are paired and the potential for PwP and carer duplication of answers. Whilst the survey was available nationally, local support groups and NHS clinics were approached in the south of England so the population of the study was more heavily weighted to this geographic area. The higher proportion of participants who were recruited through national and local support organisations would likely be more informed about their condition than others, and this could bias the findings on participants’ general awareness of causes of crisis.
In the comparison of PwP and carer data, it is important to note that carer responses referred to slightly older and more progressed PwP than the data set provided by PwP themselves. This, combined with the lack of pairing between PwP and carers, presents significant limitations on the ability to compare the two groups. Although the differences in condition duration and progression were small, specific kinds of events may cause crisis at distinct stages of the disease; an increased awareness of cognitive impairment might be expected by the carer participants whose answers are based on more progressed PwP. It is also possible that carers may rate the PwP symptoms as more progressed than the PwP themselves.
The higher proportion of male PwP may be expected due to the increased prevalence of the disease amongst men [30], and female PwP were adequately represented in the sample population.
This research was a cross-sectional retrospective survey. The themes and issues identified here could be researched further in a longitudinal prospective study in order to increase reliability in the recording of events and gain a more detailed understanding of the impact on care needs of different types of crisis.
CONCLUSIONS
The findings of this study into the causes of crisis for PwP from a patient and carer perspective are significant for healthcare delivery in a number of areas. The identification of poorly recognised causes of crisis - difficulty with ADLs, carer absence, and the loss of social contact or skills –should help inform the questions and language used by healthcare professionals when assessing PwP for their risk of crisis.
A more comprehensive understanding of the impact of different causes of crisis from the PwP and carer perspective allows us to better understand how PwP are differentially affected by events. It broadens the perspective of measuring risk, from a hospital-centric model to further include care that is delivered in the community and the patient and carer perspective of the impact of crises.
The high degree of consistency between causes of crisis identified through personal experience compared with general awareness would suggest that PwP and their carers are well-informed of potential crisis triggers outside of their own personal experiences. The observations that patients are more aware of mental health issues and that carers are more attentive to cognitive impairment and issues with medication as causes of crisis suggest that in certain areas patients or the carer may be more reliable informants. Improved understanding of these differing levels of awareness can help healthcare professionals focus on areas that might otherwise be missed or misreported. The higher frequency of fatigue and speech and communication issues as causes of crisis in personal experiences compared to general awareness indicates that there may be a need for improved patient and carer awareness in these areas.
The results from this study emphasise the importance of asking questions in a way that is relevant to the individual’s experience and understanding, and for recognising the impact of crises on PwP irrespective of the setting. With an increase in online self-management interventions and support provision in the community, we recommend that health and social care providers ask the right questions to optimise care and avoid unnecessary crisis.
ACKNOWLEDGMENTS
This project has received funding from the Wessex Clinical Network and was supported by National Institute for Health Research (NIHR) Applied Research Collaboration (ARC) Wessex. H.C.R receives support from the National Institute for Health Research (NIHR) Southampton Biomedical Research Centre. Parkinson’s UK shared the research with their national members and facilitated contact with their local groups in the Wessex area. Dr Natalie Cox and Megan Liddiard reviewed the coding of the data. The research team thanks all of the participants who gave their time to complete the survey. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
CONFLICT OF INTEREST
The authors have no conflict of interest to report.
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JPD-212641.
REFERENCES
[1] | von Campenhausen S , Bornschein B , Wick R , Bötzel K , Sampaio C , Poewe W , Oertel W , Siebert U , Berger K , Dodel R ((2005) ) Prevalence and incidence of Parkinson’s disease in Europe. Eur Neuropsychopharmacol 15: , 473–490. |
[2] | Huse D , Schulman K , Orsini L , Castelli-Haley J , Kennedy S , Lenhart G ((2005) ) Burden of illness in Parkinson’s disease. Mov Disord 20: , 1449–1454. |
[3] | Parashos SA , Maraganore DM , O’Brien PC , Rocca WA ((2002) ) Services utilization and prognosis in Parkinson disease: A population-based study. Mayo Clin Proc 77: , 918–925. |
[4] | MacNeil Vroomen J , Bosmans JE , van Hout HP , de Rooij SE ((2013) ) Reviewing the definition of crisis in dementia care. BMC Geriatr 13: , 10. |
[5] | Hoff LA ((1995) ) People in crisis: Understanding and helping. Jossey-Bass, San Francisco. |
[6] | Liken MA ((2001) ) Caregivers in crisis: Moving a relative with Alzheimer’s to assisted living. Clin Nurs Res 10: , 52–68. |
[7] | Gerlach O , Winogrodzka A , Weber W ((2001) ) Clinical problems in the hospitalized Parkinson’s patient: Systematic review. Mov Disord 26: , 197–208. |
[8] | Kaoy L , Rose J , Abdelhafiz AH ((2018) ) Factors that lead to hospitalisation in patients with Parkinson disease –A systematic review. Int J Clin Pract 72: , e13039. |
[9] | Okunoye O , Kojima G , Marston L , Walters K , Schrag A ((2020) ) Factors associated with hospitalisation among people with Parkinson’s disease - A systematic review and meta-analysis. Parkinsonism Relat Disord 71: , 66–72. |
[10] | Cosentino M , Martignoni E , Michielotto D , Calandrella D , Riboldazzi G , Pacchetti C , Frigo G , Nappi G , Lecchini S ((2005) ) Medical healthcare use in Parkinson’s disease: Survey in a cohort of ambulatory patients in Italy. BMC Health Serv Res 5: , 26. |
[11] | Vargas AP , Carod-Artal FJ , Nunes SV , Melo M ((2008) ) Disability and use of healthcare resources in Brazilian patients with Parkinson’s disease. Disabil Rehabil 30: , 1055–1062. |
[12] | Kessler I ((1972) ) Epidemiologic studies of Parkinson’s disease: ii. A hospital-based survey. Am J Epidemiol 95: , 308–318. |
[13] | Weir S , Samnaliev M , Kuo TC , Tierny TS , Walleser Autiero S , Taylor RS , Shrag A ((2018) ) Short- and long-term cost and utilization of health care resources in Parkinson’s disease in the UK. Mov Disord 33: , 974–81. |
[14] | Pressley JC , Louis ED , Tang MX , Cohen PD , Glied S , Mayeux R ((2003) ) The impact of comorbid disease and injuries on resource use and expenditures in parkinsonism. Neurology 60: , 87–93. |
[15] | Hsieh HF , Shannon SE ((2005) ) Three approaches to qualitative content analysis. Qual Health Res 15: , 1277–1288. |
[16] | van Uem JM , Marinus J , Canning C , van Lummel R , Dodel R , Liepelt-Scarfone I , Berg D , Morris ME , Maetzler W ((2016) ) Health-related quality of life in patients with Parkinson’s disease–A systematic review based on the ICF model. Neurosci Biobehav Rev 61: , 26–34. |
[17] | Kuhlman GD , Flanigan JL , Sperling SA , Barrett MJ ((2019) ) Predictors of health-related quality of life in Parkinson’s disease. Parkinsonism Relat Disord 65: , 86–90. |
[18] | Prizer LP , Kluger BM , Sillau S , Katz M , Galifianakis NB , Miyasaki JM ((2020) ) The presence of a caregiver is associated with patient outcomes in patients with Parkinson’s disease and atypical parkinsonisms. Parkinsonism Relat Disord 78: , 61–65. |
[19] | McNamara P , Stavitsky K , Durso R , Harris E ((2010) ) The impact of clinical and cognitive variables on social functioning in Parkinson’s disease: Patient versus examiner estimates. Parkinsons Dis 2010: , 263083. |
[20] | Jagota P , Jongsuntisuk P , Plengsri R , Chokpatcharavate M , Phokaewvarangkul O , Chirapravati V , Panyakaew P , Sringean J , Bhidayasiri R ((2020) ) If your patients were too embarrassed to go out in public, what would you do? - Public education to break the stigma on Parkinson’s disease using integrated media. Patient Relat Outcome Meas 11: , 143–148. |
[21] | Buchman AS , Boyle PA , Wilson RS , James BD , Leurgans SE , Arnold SE , Bennett DA ((2010) ) Loneliness and the rate of motor decline in old age: The Rush Memory and Aging Project, a community-based cohort study. BMC Geriatr 10: , 77. |
[22] | Gerlach OH , Broen MP , Weber WE ((2013) ) Motor outcomes during hospitalization in Parkinson’s disease patients: A prospective study. Parkinsonism Relat Disord 19: , 737–741. |
[23] | Schrag A , Taddei RN ((2017) ) Depression and anxiety in Parkinson’s disease. Int Rev Neurobiol 133: , 623–655. |
[24] | Ballard CG , Chithiramohan RN , Handy S , Bannister C , Davis R , Todd NB ((1991) ) Information reliability in dementia sufferers. Int J Geriatr Psychiatry 6: , 313–316. |
[25] | McLoughlin D , Cooney C , Holmes C , Levy R ((1996) ) Carer informants for dementia sufferers: Carer awareness of cognitive impairment in an elderly community-resident sample. Age Ageing 25: , 367–371. |
[26] | Leopold NA , Polansky M , Hurka MR ((2004) ) Drug adherence in Parkinson’s disease. Mov Disord 19: , 513–517. |
[27] | Boersma I , Jones J , Coughlan C , Carter J , Bekelman D , Miyasaki J , Kutner J , Kluger B ((2017) ) Palliative care and Parkinson’s disease: Caregiver perspectives. J Palliat Med 20: , 930–938. |
[28] | Friedman JH , Chou KL ((2004) ) Sleep and fatigue in Parkinson’s disease. Parkinsonism Relat Disord 10: (Suppl 1), S27–35. |
[29] | Shulman LM , Taback RL , Rabinstein AA , Weiner WJ ((2002) ) Non-recognition of depression and other non-motor symptoms in Parkinson’s disease. Parkinsonism Relat Disord 8: , 193–197. |
[30] | Wooten GF , Currie LJ , Bovbjerg VE , Lee JK , Patrie J ((2004) ) Are men at greater risk for Parkinson’s disease than women? J Neurol Neurosurg Psychiatry 75: , 637–638. |




