Predictors of Time to Discontinuation of Levodopa-Carbidopa Intestinal Gel Infusion: A Retrospective Cohort Study
Abstract
Background:
Continuous intra-duodenal infusion of levodopa-carbidopa intestinal gel (LCIG) is a well-established therapy for patients with advanced Parkinson’s disease (PD) suffering from motor complications despite optimized treatment with oral dopaminomimetics. However, time to discontinuation of treatment with LCIG varies considerably between patients, ranging from a few months to more than ten years. To improve the selection of candidates for LCIG, knowledge of prognostic factors is of paramount importance.
Objective:
To explore baseline predictors of time to discontinuation of LCIG.
Methods:
In this two-center retrospective cohort study, we reviewed the medical files of 98 PD patients treated with LCIG between April 2006 and December 2015 (53% male; mean age: 66.2 years; mean disease duration: 12.3 years). Baseline patient characteristics were used as covariates in Cox regression models.
Results:
During follow-up (mean observation time: 2.6 years; range: 0.1–9.3) eighteen patients discontinued treatment (18.4%), while seven patients died (7.1%). Median duration of treatment with LCIG, estimated with Kaplan-Meier analysis, was 7.8 years (95% CI: 6.7–9.0). Disease duration (in years) at baseline was a statistically significant predictor of time to discontinuation of LCIG (HR: 0.85; 95% CI: 0.75–0.96, p = 0.006). All other characteristics studied, e.g. age >70 years, did not show statistically significant associations with the total duration of treatment with LCIG.
Conclusion:
Our findings show a low overall rate of discontinuation of LCIG infusion, with a median duration of treatment of 7.8 years. Shorter disease duration at baseline appeared to be a predictor of earlier discontinuation of LCIG.
INTRODUCTION
Within ten years of treatment with oral dopaminomimetics, many patients with Parkinson’s disease (PD) develop disabling motor complications consisting of at random on-off fluctuations as well as troublesome dyskinesias [1–3], These phenomena can be partly explained by variations in the levodopa plasma concentration, caused by, e.g., variable gastric emptying, among several other reasons [4].
Since 2004, continuous intra-duodenal infusion of levodopa-carbidopa intestinal gel (LCIG) has been available to alleviate motor complications not adequately controlled by oral therapy [5, 6]. LCIG infusion provides stable levodopa concentrations in plasma, thereby reducing off time and increasing on time without troublesome dyskinesias [7, 8]. LCIG does also appear to reduce non-motor symptoms [9]. LCIG infusion is well-tolerated in the long term, as evidenced by an average overall duration of treatment of 7.6 years [10].
However, time to discontinuation differs considerably among patients, ranging from a few months to more than ten years [10, 11]. This variation suggests individual differences in the overall effectiveness of LCIG, since the total duration of treatment reflects the therapeutic benefits in relation to undesirable effects [12]. Indeed, reasons for discontinuation of LCIG are most commonly device-related complications, lack of efficacy, patient dissatisfaction, drug-related adverse events and death (unrelated to LCIG) [10, 13–16]. Identifying patient characteristics related to the heterogeneity of overall effectiveness of LCIG under real-word conditions is crucial to improving patient selection criteria [17, 18].
Several small and medium-sized cohort studies identified baseline characteristics associated with early discontinuation of LCIG infusion. A Swedish cohort study with 135 patients reported that longer disease duration at baseline was a risk factor for discontinuation [10]. In addition, smaller follow-up studies (20 to 59 patients) observed associations with high age at implant (>70 years), low severity of pre-pump dyskinesias, and female sex [15, 19, 20]. However, none of the identified predictors have been confirmed by other studies.
Therefore, we studied a cohort of cohort of 98 PD patients to establish whether baseline characteristics are predictors of time to discontinuation of LCIG.
MATERIALS AND METHODS
Design and setting
This was a retrospective cohort study conducted in two departments of neurology in the Netherlands, both specialized in movement disorders and each serving a PD population of 500–700 patients. Both centers offer all three advanced PD therapies, namely continuous apomorphine infusion (CAI), LCIG and deep brain stimulation (DBS). In both hospitals, the initiation and management of LCIG is carried out by a dedicated team consisting of a movement disorder specialist, a specialized PD nurse, a gastroenterologist and an interventional radiologist. The local standard operating procedures are updated annually in accordance with the most recent scientific evidence.
This study was reported as per the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline [21].
Ethical approval
The study protocol was approved by the ethical review committee of the Zuyderland Medical Center, whereas an exemption was granted by the ethical review board of the University Medical Center Groningen. All medical charts were reviewed in accordance with the prevailing regulations on data protection and privacy.
Patients and medical charts
PD patients who started treatment with LCIG infusion between April 1st, 2006 and December 31st, 2015 (study cut-off date) were included. The included patients fulfilled the UK Brain Bank criteria for the diagnosis of idiopathic PD [22]. In addition, all patients had advanced PD with motor fluctuations, often with dyskinesias, despite optimal oral/transdermal drug treatment. A minority of the studied patients had already been treated with DBS, CAI or both.
The decision to start treatment with LCIG was made after careful consideration of other treatment options (continuing oral treatment, DBS or CAI). The patients and their caregivers were involved in this decision-making process after they had been informed about the options. LCIG infusion (levodopa (20 mg/mL) and carbidopa (5 mg/mL) in methylcellulose)) was initiated in accordance with the standard operating procedures of both hospitals. In one of the centers, a nasojejunal test phase was performed in all patients, whereas in the other hospital this was left to the discretion of the treating neurologist. Patients who did not continue LCIG infusion after an initial nasojejunal test phase were excluded from the cohort, as well as patients whose medical files could not be retrieved.
The electronical medical charts comprised all reports of hospitalizations, outpatient care visits, drug changes, radiological examinations and invasive procedures, as well as medical correspondence between hospitals.
Endpoints and predictor variables
The primary endpoint of this study was time to discontinuation of LCIG infusion (excluding death). As death was a so-called competing risk (i.e., a patient who dies during treatment with LCIG can no longer discontinue LCIG infusion), we chose time to all-cause discontinuation of LCIG infusion (including death) as a sensitivity analysis for the primary endpoint. Secondary endpoints were number of discontinuations, reasons for treatment discontinuation, and number of hospitalizations due to LCIG-related complications. A hospitalization was defined as an admission to the hospital for clinical observation or treatment for the duration of at least one day.
The following baseline variables were selected as potential predictors of time to discontinuation of LCIG infusion: gender, age at diagnosis PD, age at start of LCIG infusion, disease duration at start of LCIG, levodopa equivalent daily dose (LEDD), disease severity (Hoehn and Yahr stage), marital state, living situation (home or institution), subject to nasojejunal test phase (yes or no), presence of severe cognitive impairment, type of enteral access system (PEG-J or T-port), prior advanced therapies (DBS and/or CAI), and having ≥1 somatic comorbidity. The predictor variable age at the start of LCIG was dichotomized, using a cut-off of 70 years, in order to compare our data with the findings from previous studies [15, 23]. Potential predictor variables with large numbers of missing values (>30%) were not analyzed.
Data acquisition
Between November 2015 and January 2016, the medical files of all included patients were systematically reviewed by two authors (H.M. and J.G.).
Time to discontinuation (in months) was calculated as the time interval between initiation of LCIG and discontinuation of treatment. If patients died or were lost to follow-up (e.g., moved elsewhere) or were still on LCIG infusion at study cut-off, their durations of treatment were censored at the last available follow-up. For the sensitivity analysis of time to all-cause discontinuation, death was considered as a reason for discontinuation of treatment. In patients who restarted LCIG infusion after having discontinued LCIG, only the first treatment period was evaluated.
Disease duration was calculated as the number of months between the date of diagnosis and the start of LCIG infusion. If medical records only stated the year of PD diagnosis, the corresponding month was arbitrarily set on June.
Levodopa equivalent daily dose (LEDD) before start of LCIG and after initiation of LCIG was calculated using the formula described elsewhere [24]. In case the daily dosing times of LCIG could not be retrieved from the medical file, a 16-hour-treatment per day was assumed. Presence of severe cognitive impairment was deduced from the medical chart in case the wording ‘PD dementia’ had been included in the file by the treating neurologist, or in case the patient had ‘severe cognitive impairment’ and did use a cholinesterase inhibitor.
Reasons for treatment discontinuation were deduced from clinical reports and categorized as follows: treatment effect being less than expected; switch to DBS; switch to CAI; device-related side effects (e.g., events related to the intestinal tube, pump complications, or infusion-related events); or drug-related side effects (e.g., dyskinesia, neuropsychiatric side effects, severe neuropathy). Death was categorized as being either related or unrelated to LCIG infusion.
Statistical analyses
Patient demographics at baseline were summarized using descriptive statistics. Quantitative data were expressed as mean and standard deviation, whereas categorical variables were presented as counts and proportions (%). No attempts were made to impute missing values.
We used Kaplan-Meier curves to estimate the time to discontinuation of treatment and the overall median duration of treatment. This analysis accounted for censored observations. The number of LCIG-related hospitalizations was reported as an incidence rate (total number of hospitalizations divided by the cumulative observation time of the whole cohort), as to account for variations in observation time among the included patients.
To identify predictors of the time to discontinuation of treatment with LCIG, we used Cox proportional hazard models. The proportional hazards assumption was verified for all potential predictors by means of Schoenfield residual tests (performed in R version 3.3.1 with the package ‘Survival’) [25, 26]. Outcomes of the Cox regression analyses were reported as hazard ratios (HR) with corresponding 95% confidence intervals (95% CI).
Subsequently, a multivariable Cox regression analysis was performed including all potential univariable correlates (p < 0.157; Akaike information criterion) using a backward stepwise selection with a p value >0.05 for removal of variables [27]. Because of the pure predictive nature of this study, there was no need to consider confounding effects (i.e., no causal mechanisms were studied) [28].
Time-to-event analyses and the statistical analyses for the baseline table were carried out using IBM SPSS Statistics version 25 for Windows. We used STATA version 16 (StataCorp LLC) for Windows to calculate incidence rates. The significance threshold was set at p < 0.05.
RESULTS
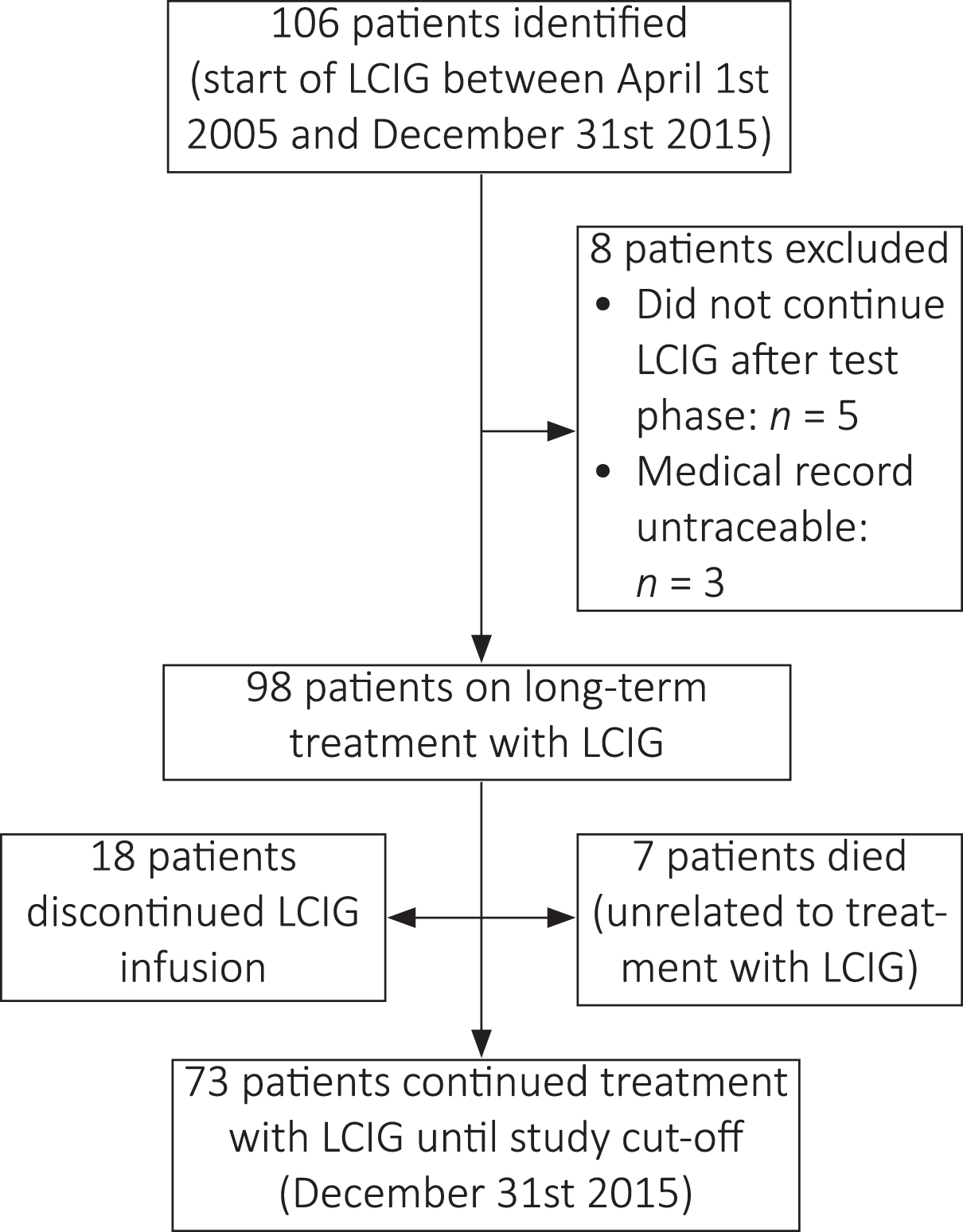
In the two hospitals, a total number of 106 eligible PD patients were identified. Of this group, five patients did not continue treatment with LCIG after the initial test phase, whereas three patients were excluded because their medical records could not be retrieved. Therefore, the final study cohort consisted of 98 patients (53.1% male) on long-term LCIG infusion (Fig. 1).
Fig. 1
Patient flow chart. LCIG, levodopa-carbidopa intestinal gel.
Baseline characteristics of the included patients are reported in Table 1. At start of LCIG therapy, the mean age was 66.2±8.2 years and the mean duration of PD was 12.3±5.4 years. A nasojejunal test phase was performed in 44 patients (44.9%). Most patients (85.7%) received LCIG infusion via a PEG-J tube. The others received a T-port [29].
Table 1
Demographic and clinical characteristics of study population at start of LCIG infusion
| Characteristic | N = 98 | Missing values |
| Male gender | 52 (53.1%) | |
| Age (years) | 66.2±8.2 | |
| Age≥70 years | 34 (34.7%) | |
| Duration of PD (years) | 12.3±5.4 | |
| Age at diagnosis PD (years) | 53.8±8.9 | |
| Hoehn-Yahr stage* | 3.2±1.0 | 48 |
| 1 | 0 (0.0%) | |
| 2 | 16 (32.0%) | |
| 3 | 11 (22.0%) | |
| 4 | 18 (36.0%) | |
| 5 | 5 (10.0%) | |
| Partner/relationship | 70 (75.3%) | 5 |
| Living situation | 4 | |
| Home | 84 (89.4%) | |
| Institution | 10 (10.6%) | |
| Nasojejunal test phase | 44 (44.9%) | 23 |
| Tube | ||
| PEG-J | 84 (85.7%) | |
| T-port | 14 (14.3%) | |
| LEDD oral medication | 1437±493 | 2 |
| LEDD using LCIG | 1649±611 | 3 |
| Previous advanced therapy | ||
| CAI | 24 (25.0%) | |
| Years before LCIG | 1.9±1.6 | |
| CAI and DBS§ | 5 (5.2%) | |
| Years before LCIG | 4.2±2.2 | |
| Severe cognitive impairment | 12 (12.2%) | 40 |
| Somatic comorbidity | ||
| ≥1 comorbidity | 45 (45.9%) | |
| Arthrosis | 16 (16.3%) | |
| COPD | 1 (1.0%) | |
| Coronary artery disease | 9 (9.2%) | |
| Diabetes mellitus | 11 (11.2%) | |
| Heart failure | 2 (2.0%) | |
| Hypertension | 8 (8.2%) | |
| Malignancy | 8 (8.2%) | |
| Stroke | 6 (6.1%) |
Variables are expressed as number (percentage) or mean±SD. CAI, continuous apomorphine infusion; DBS, deep brain stimulation; LCIG, levodopa-carbidopa intestinal gel; PD, Parkinson’s disease; PEG-J, percutaneous endoscopic gastrostomy with a jejunal tube; SD, standard deviation. *The proportions are calculated from the number of available observations (n = 50). §4 out of 5 patients had already been using CAI before starting with DBS.
Before starting with LCIG infusion, 29 patients (29.6%) had been treated with other advanced therapies, namely CAI (n = 24; on average 1.9±1.6 years before LCIG) or both CAI and DBS (n = 5; on average 4.2±2.2 years before LCIG). No patients continued CAI once they started with LCIG, though four of the five patients treated with DBS did combine this therapy with LCIG infusion.
Time to discontinuation
The mean observation time of this study was 2.6±2.4 years, ranging from one month up to 9.3 years. In seventeen patients (17.3%) the observation time was more than 5.0 years.
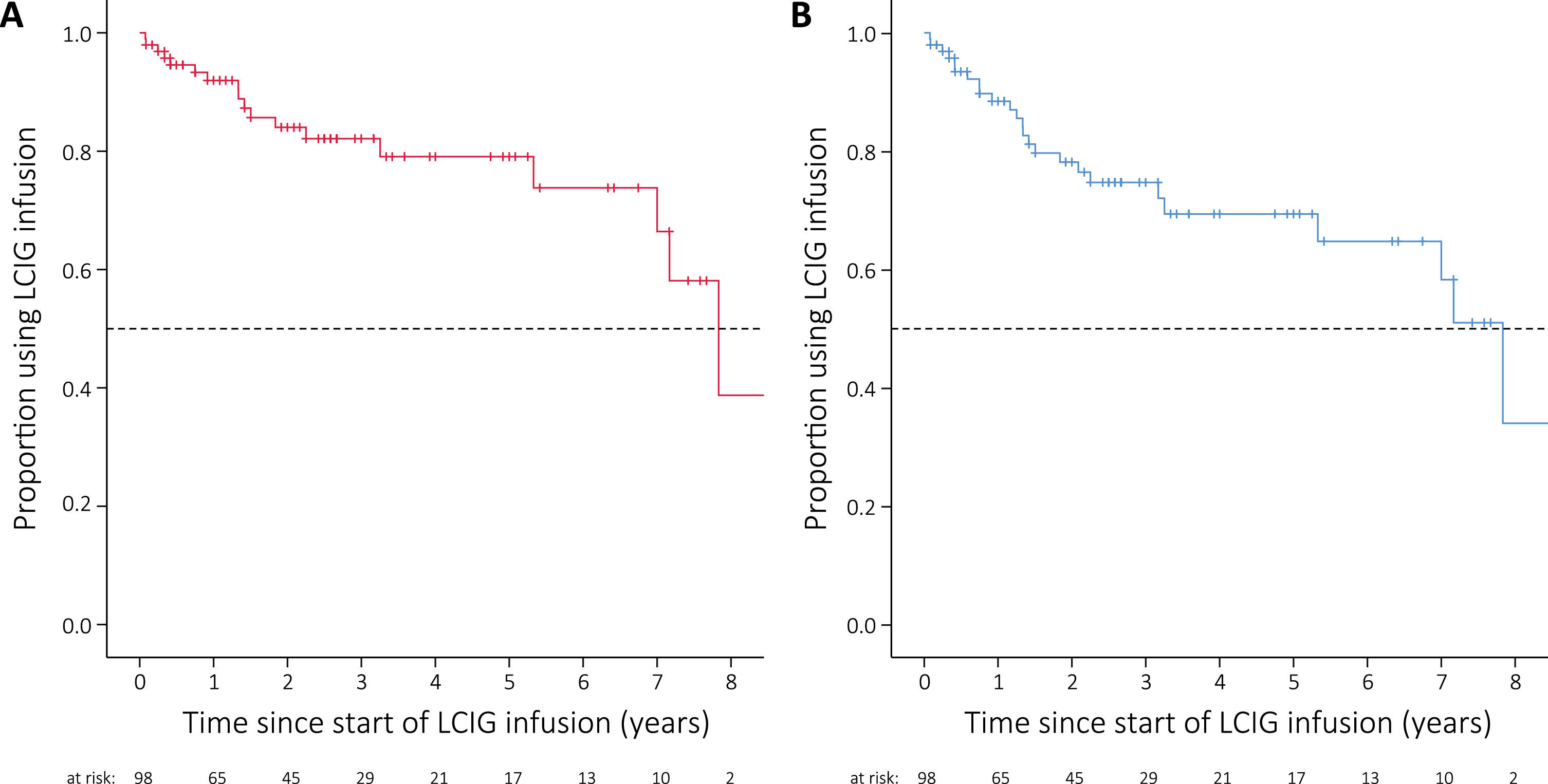
During the overall observation period, 18 patients (18.4%) discontinued LCIG infusion, while seven patients died (7.1%). The median time to discontinuation of treatment with LCIG, as estimated with Kaplan-Meier analysis, was 7.8 years (95% CI: 6.7–9.0; Fig. 2A). This result was similar in the sensitivity analysis in which death was considered a discontinuation of treatment (median time to all-cause discontinuation: 7.8 years; 95% CI: 6.8–8.9; Fig. 2B). The patient who had the longest observation time (9.3 years) was still using LCIG infusion at the last follow-up. The rate of discontinuation appeared to be higher during the first two years of treatment, judging from the steepness of the curve (Fig. 2A). The same holds for the sensitivity analysis (Fig. 2B).
Fig. 2
Kaplan-Meier curve showing time to discontinuation of levodopa-carbidopa intestinal gel (LCIG) infusion. The vertical tick marks denote censored observations. The horizontal dashed lines indicate the median time to discontinuation of treatment. A) Curve for the primary analysis of time to discontinuation (patients discontinued: n = 18); censored observations include deceased patients. B) Curve for the sensitivity analysis in which death is considered a discontinuation of treatment (patients discontinued or died: n = 25).
Among the 18 patients who discontinued treatment, four patients restarted LCIG infusion after a median duration of 0.8 years (range: 0.4–3.3), typically because their response fluctuations could not be managed adequately by either DBS or oral dopaminergic therapy.
Predictors of time to discontinuation
Outcomes of both the univariable and multivariable Cox regression models are shown in Table 2. Univariable analysis showed that duration of PD (in years) at start of LCIG was a significant predictor of treatment discontinuation (Hazard Ratio (HR): 0.85; 95% CI: 0.75–0.96; p = 0.006). An HR < 1 indicates a lower risk of discontinuation for every 1-year increase in disease duration at start of treatment. Higher age (in years) at baseline was also associated with a lower risk of discontinuation, although not statistically significant (HR: 0.95; p = 0.09). This variable was selected for the multivariable analysis based on the Akaike information criterion (p < 0.157). No other baseline characteristics studied were associated with time to discontinuation.
Table 2
Associations between baseline characteristics and time to discontinuation of LCIG infusion
| Variable at start of LCIG infusion | Univariable regression | Multivariable regression | ||||
| HR | 95% CI | p-value | HR | 95% CI | p-value | |
| Gender (male vs female) | 0.88 | 0.35–2.24 | 0.79 | |||
| Age | ||||||
| (years) | 0.95 | 0.89–1.01 | 0.09 | 0.95 | 0.89–1.02 | 0.14 |
| (≥70 years vs <70 years) | 0.74 | 0.23–2.34 | 0.61 | |||
| Duration of PD (years) | 0.85 | 0.75–0.96 | 0.006* | 0.85 | 0.76–0.96 | 0.009* |
| Age at diagnosis PD (years) | 1.00 | 0.95–1.06 | 0.89 | |||
| Partner/relationship (yes vs no)§ | 1.21 | 0.34–4.27 | 0.77 | |||
| Living situation (home vs institution)¶ | 0.71 | 0.26–3.19 | 0.66 | |||
| Enteral access (PEG-J vs T-port) | 1.29 | 0.29–5.73 | 0.74 | |||
| LEDD oral medication (mg/day) | 1.00 | 0.99–1.00 | 0.62 | |||
| LEDD at remission from hospital (mg/day) | 1.00 | 0.99–1.00 | 0.60 | |||
| Prior advanced therapy (yes vs no) | 1.39 | 0.53–3.64 | 0.51 | |||
| Somatic comorbidity (≥1 vs 0) | 2.02 | 0.79–5.19 | 0.18 | |||
CI, confidence interval; HR, hazard ratio; LCIG, levodopa-carbidopa intestinal gel; PD, Parkinson’s disease; PEG-J, percutaneous endoscopic gastrostomy with a jejunal tube. * Statistically significant (p < 0.05). § N = 93; in total 17 discontinuations. ¶ N = 94; in total 18 discontinuations.
Disease severity (Hoehn & Yahr score) and presence of severe cognitive impairment were not analyzed as potential predictors because of the high number of missing values (49% and 41%, respectively).
The multivariate model yielded one independent baseline predictor for time to discontinuation, i.e. duration of PD at start of LCIG (HR: 0.85; 95% CI: 0.76–0.96; p = 0.009). The performed sensitivity analysis, in which death was considered a reason for discontinuation of treatment, confirmed the findings of the univariable and multivariable Cox regression analyses, i.e. duration of PD at baseline was the only variable associated with time to discontinuation ([univariable analysis] HR: 0.83; 95% CI: 0.75–0.92; p = 0.0004; [multivariable analysis with age as covariate] HR 0.83; 95% CI 0.75–0.92; p = 0.0005; data not shown).
Reasons for discontinuation and causes of death
In total, 18 patients (18.4%) discontinued LCIG infusion and seven patients died during treatment (7.1%). Based on the collected data, all patients died for reasons unrelated to treatment, although the cause of death was unknown in two patients (Table 3).
Table 3
Reasons for discontinuation of LCIG infusion and causes of death during treatment
| Reason for discontinuation | N = 18 |
| Device-related side effects | 5 |
| Effect less than expected by patient | 5 |
| Switch to DBS | 4 |
| Effect less than expected by clinician | 2 |
| Switch to CAI | 1 |
| Drug-related side effects of LCIG | 1 |
| Cause of death | N = 7 |
| LCIG-related | 0 |
| Device-related | 0 |
| Other (not specified) | 5 |
| Unknown | 2 |
Reasons for discontinuation and causes of death are expressed as numbers. DBS, deep brain stimulation; CAI, continuous apomorphine infusion; LCIG, levodopa-carbidopa intestinal gel; PD, Parkinson’s disease.
The other most common reasons for discontinuation were device-related side effects (n = 5; e.g. recurrent tube dislocations) and efficacy being less than expected by the patient (n = 5). Table 3 shows all reasons for discontinuation.
Number of hospitalizations
During follow-up, 32 patients (32.7%) were hospitalized due to complications of LCIG treatment. This group of patients needed 51 hospitalizations in total. Most hospitalizations were related to problems with the PEG-J tube or T-port, such as dislocations, infections, or malfunctioning (Table 4). One patient was hospitalized five times and stopped treatment after a total duration of 3.3 years because of device-related side-effects.
Table 4
Hospitalizations due to LCIG-related complications
| Reason | Number of hospitalizations |
| (N = 51) | |
| Related to device (N = 34) | |
| Dislocation PEG-J | 7 |
| Infection | |
| PEG-J | 4 |
| T-port | 6 |
| Gastrointestinal perforation PEG-J | 3 |
| Occlusion PEG-J | 3 |
| Pain | |
| After PEG-J placement | 1 |
| After T-port placement | 1 |
| Leakage | |
| PEG-J | 1 |
| T-port | 1 |
| Inadvertently pulled-out PEG-J | 1 |
| Removal of T-port due to infection | 1 |
| Tilting T-port | 1 |
| Other, PEG-J-related | 4 |
| Other (N = 17) | |
| Aggravation of dyskinesias needing re-titration | 5 |
| Severe off-symptoms needing re-titration | 5 |
| Subacute polyneuropathy | 3 |
| Hallucinations | 2 |
| Diarrhea | 1 |
| Falls | 1 |
Overall, the incidence of LCIG-related hospitalizations was 0.20 per person per year. Patients who discontinued LCIG infusion had a significantly higher rate of hospitalizations compared to patients continuing therapy (0.56 vs 0.13 hospitalizations per person year; difference: 0.43; 95% CI of difference: 0.20–0.65; p < 0.0001). This difference remained statistically significant after excluding patients who discontinued LCIG because of device-related side effects (0.41 vs 0.13 hospitalizations per person year; difference: 0.28; 95% CI of difference: 0.04–0.51; p = 0.003).
DISCUSSION
In our LCIG cohort we found a low rate of discontinuation with a median time to discontinuation of 7.8 years. The results confirmed the heterogeneity in total duration of treatment, varying from a few months to more than 9 years. At start of therapy, the only patient characteristic predictive for time to discontinuation appeared to be duration of PD. Patients who discontinued treatment had a higher incidence rate of hospitalizations than patients who remained on LCIG.
This study is the first overview of a cohort of Dutch PD patients treated with LCIG. The results of this study are similar to the findings of previous long-term studies reporting annual rates of withdrawal of 7–13% and an average overall duration of treatment of 7.6 years [10, 13, 14, 16, 30–32]. In addition, all baseline characteristics of our cohort, the reported reasons for discontinuation, and the considerably high number of LCIG-related hospitalizations (i.e., serious adverse events) are comparable to the observations in other large patient groups [9, 10, 13, 15, 16, 20, 32].
In the present study, time to treatment discontinuation was chosen as the primary outcome to study prognostic factors. We chose this outcome measure because of its simplicity and its comprehensiveness. Previously, it was argued that time to discontinuation serves as a measure of effectiveness in illnesses with a long-term course and need for long-term treatment [12]. Time to discontinuation encompasses lack of efficacy, intolerable side effects, dissatisfaction or a combination of the aforementioned reasons [33]. Staying on treatment for a longer period of time can be considered a success, as it may reflect adequate symptom reduction, fewer hospitalizations and a satisfactory quality of life [33]. Therefore, all discontinuations of LCIG display a lack of treatment success. This also holds for switching to DBS or CAI (n = 5), concerning patients not being satisfied with LCIG.
We believe that studying time to treatment discontinuation using survival analysis has several advantages. Firstly, survival analysis can effectively cope with the uncertainty caused by censored observations [34]. Therefore, this statistical technique can utilize the data of the whole cohort, in our case 98 patients, irrespective of whether a patient stopped treatment or not. Using all data contributes to the power of the statistical analyses. Secondly, time to discontinuation can be studied easily and reliably in retrospective cohorts, since discontinuation is an endpoint that will always be registered in medical charts. Nevertheless, this method has difficulties to account for competing risks, for example death, which might lead to overestimation of the risk of discontinuation. To overcome this problem, we chose to censor deceased patients and perform a sensitivity analysis in which we did the opposite [35].
The identified predictors of time to discontinuation do only partly resonate with previous publications. Firstly, the association between duration of PD at baseline and time to discontinuation appears to oppose the results of a Swedish cohort study [10]. While our findings imply that a longer duration of PD is a predictor of a longer total duration of treatment, patients discontinuing LCIG in Swedish cohort had a significantly longer duration of PD at start of therapy. This dissimilarity might be related to methodological differences, since our association was based on a Cox regression analysis while Nyholm et al. compared the characteristics of patients who stopped treatment with those who did not [10]. The latter did not take into account variation in time-to-event data. Although the observational design of the present study does not allow for causal inferences, the listed reasons for discontinuation (Table 3) do hint at possible explanations. One might speculate that patients with shorter disease durations are more inclined to stop with LCIG infusion because they have overly high expectations of the treatment benefits. Another likely explanation is that patients with shorter disease durations are more often still eligible for either DBS or CAI, while LCIG frequently is the last available option for patients who have had the diagnosis PD for a longer period of time.
Another dissimilarity between our results and previous studies concerns the prognostic value of age at start of treatment [15, 20, 23]. Our findings do not provide evidence for the claim that elderly patients are less suitable candidates for LCIG infusion [15]. In the present cohort, time to discontinuation of LCIG was equally distributed across all age groups. Patients aged ≥70 did not significantly differ from younger patients, with the estimated hazard ratio of 0.74 being in favor of older patients (no statistical significance). Therefore, it might be concluded that advanced age per se is not a contraindication for LCIG infusion.
The fact that this study has not been able to corroborate previously establish baseline predictors, while it did show possible new associations, may mean that there are no robust baseline predictors for treatment success. However, it seems unlikely that all patients are equally suitable for LCIG. Possibly, factors during treatment are of greater importance for treatment effectiveness. This assumption is supported by the higher rate of hospitalizations among patients from our cohort who discontinued treatment. In this regard, others have pointed out that a dedicated treatment team is the cornerstone of successful long-term treatment [20, 36].
The present study has several shortcomings. Firstly, because of the retrospective design, some patients might have been missed, which could have created an incomplete cohort. Secondly, the exploration of predictors was hampered by missing values, especially for the variables disease severity and presences of cognitive impairment. Thirdly, our analysis did not make a distinction between patients who discontinued treatment permanently and patients for whom the discontinuation was merely an intermission (n = 4). As a result, estimation of the total duration of treatment is slightly lower than the real cumulative time on LCIG. Fourthly, the number of LCIG-related hospitalizations is probably lower than the actual number of LCIG-related adverse events, since we did not count the number of complications that were handled at the outpatient clinic. Finally, we did not study the detailed reasons why LCIG infusion was chosen instead of an alternative advanced therapy (DBS or CAI), nor did we report data on clinical efficacy. Such data could have supported the generalization of the study findings.
In conclusion, LCIG infusion is well-tolerated in the long term. In our cohort, PD patients with a shorter disease duration at baseline were more likely to discontinue treatment earlier. In addition, elderly patients appeared to be equally good candidates for LCIG infusion. Future studies with larger patient groups, preferably with a prospective design or a meta-analysis, are needed to further improve our understanding of baseline predictors of LCIG discontinuation. Eventually, this type of research will help neurologists to decide which patient is a good candidate for LCIG infusion.
CONFLICT OF INTEREST
TvL received speaker fees from AbbVie and a non-restricted study grant for investigator initiated research. No other authors have any conflicts to report.
ACKNOWLEDGMENTS
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
REFERENCES
[1] | López IC , Ruiz PJG , del Pozo SVF , Bernardos VS ((2010) ) Motor complications in Parkinson’s disease: Ten year follow-up study. Mov Disord 25: , 2735–2739. |
[2] | Ahlskog JE , Muenter MD ((2001) ) Frequency of levodopa-related dyskinesias and motor fluctuations as estimated from the cumulative literature. Mov Disord 16: , 448–458. |
[3] | Fox SH , Lang AE ((2008) ) Levodopa-related motor complications—Phenomenology. Mov Disord 23: , S509–S514. |
[4] | Djaldetti R , Baron J , Ziv I , Melamed E ((1996) ) Gastric emptying in Parkinson’s disease: Patients with and without response fluctuations. Neurology 46: , 1051–1054. |
[5] | Nyholm D , Nilsson Remahl AIM , Dizdar N , Constantinescu R , Holmberg B , Jansson R , Aquilonius S , Askmark H ((2005) ) Duodenal levodopa infusion monotherapy vs oral polypharmacy in advanced Parkinson disease. Neurology 64: , 216–223. |
[6] | Wirdefeldt K , Odin P , Nyholm D ((2016) ) Levodopa-carbidopa intestinal gel in patients with Parkinson’s disease: A systematic review. CNS Drugs 30: , 381–404. |
[7] | Nyholm D , Askmark H , Gomes-Trolin C , Knutson T , Lennernas H , Nystrom C , Aquilonius SM ((2003) ) Optimizing levodopa pharmacokinetics: Intestinal infusion versus oral sustained-release tablets. Clin Neuropharmacol 26: , 156–163. |
[8] | Olanow CW , Kieburtz K , Odin P , Espay AJ , Standaert DG , Fernandez HH , Vanagunas A , Othman AA , Widnell KL , Robieson WZ , Pritchett Y , Chatamra K , Benesh J , Lenz RA , Antonini A ((2014) ) Continuous intrajejunal infusion of levodopa-carbidopa intestinal gel for patients with advanced Parkinson’s disease: A randomised, controlled, double-blind, double-dummy study. Lancet Neurol 13: , 141–149. |
[9] | Standaert DG , Rodriguez RL , Slevin JT , Lobatz M , Eaton S , Chatamra K , Facheris MF , Hall C , Sail K , Jalundhwala YJ , Benesh J ((2017) ) Effect of levodopa-carbidopa intestinal gel on non-motor symptoms in patients with advanced Parkinson’s disease. Mov Disord Clin Pract 4: , 829–837. |
[10] | Nyholm D , Klangemo K , Johansson A ((2012) ) Levodopa/carbidopa intestinal gel infusion long-term therapy in advanced Parkinson’s disease. Eur J Neurol 19: , 1079–1085. |
[11] | Devos D , French DUODOPA Study Group ((2009) ) Patient profile, indications, efficacy and safety of duodenal levodopa infusion in advanced Parkinson’s disease. Mov Disord 24: , 993–1000. |
[12] | Davis SM , Koch GG , Davis CE , LaVange LM ((2003) ) Statistical approaches to effectiveness measurement and outcome-driven re-randomizations in the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) studies. Schizophr Bull 29: , 73–80. |
[13] | Sensi M , Cossu G , Mancini F , Pilleri M , Zibetti M , Modugno N , Quatrale R , Tamma F , Antonini A , Aguggia M , Amboni M , Arca R , Bartolomei L , Bonetto N , Calandra-Buonaura G , Bove F , Calandrella D , Canesi M , Cannas A , Capecci M , Caputo E , Ceravolo MG , Ceravolo R , Cerrone G , Coletti Moja M , Comi C , Cortelli P , D’Antonio P , Dematteis F , Di Lazzaro V , Eleopra R , Fabbrini G , Fichera M , Grassi E , Guido M , Gusmaroli G , Latorre A , Malaguti MC , Marano M , Marano P , Marconi R , Mazzucchi S , Meco G , Minafra B , Morgante F , Pacchetti C , Pierantozzi M , Pontieri FE , Riboldazzi G , Ricchi V , Ricchieri G , Rinaldo S , Rispoli V , Rossi S , Rubino A , Russo A , Saddi MV , Stefani A , Simoni S , Solla P , Tambasco N , Tamburin S , Tessitore A , Torre E , Ulivelli M , Vita MG , Volonté MA ((2017) ) Which patients discontinue? Issues on Levodopa/carbidopa intestinal gel treatment: Italian multicentre survey of 905 patients with long-term follow-up. Parkinsonism Relat Disord 38: , 90–92. |
[14] | Buongiorno M , Antonelli F , Cámara A , Puente V , de Fabregues-Nebot O , Hernandez-Vara J , Calopa M , Pascual-Sedano B , Campolongo A , Valldeoriola F , Tolosa E , Kulisevsky J , Martí MJ ((2015) ) Long-term response to continuous duodenal infusion of levodopa/carbidopa gel in patients with advanced Parkinson disease: The Barcelona registry. Parkinsonism Relat Disord 21: , 871–876. |
[15] | Calandrella D , Romito LM , Elia AE , Del Sorbo F , Bagella CF , Falsitta M , Albanese A ((2015) ) Causes of withdrawal of duodenal levodopa infusion in advanced Parkinson disease. Neurology 84: , 1669–1672. |
[16] | Fernandez HH , Boyd JT , Fung VSC , Lew MF , Rodriguez RL , Slevin JT , Standaert DG , Zadikoff C , Vanagunas AD , Chatamra K , Eaton S , Facheris MF , Hall C , Robieson WZ , Benesh J , Espay AJ ((2018) ) Long-term safety and efficacy of levodopa-carbidopa intestinal gel in advanced Parkinson’s disease. Mov Disord 33: , 928–936. |
[17] | Odin P , Ray Chaudhuri K , Slevin JT , Volkmann J , Dietrichs E , Martinez-Martin P , Krauss JK , Henriksen T , Katzenschlager R , Antonini A , Rascol O , Poewe W ((2015) ) Collective physician perspectives on non-oral medication approaches for the management of clinically relevant unresolved issues in Parkinson’s disease: Consensus from an international survey and discussion program. Parkinsonism Relat Disord 21: , 1133–1144. |
[18] | Antonini A , Stoessl AJ , Kleinman LS , Skalicky AM , Marshall TS , Sail KR , Onuk K , Odin PLA ((2018) ) Developing consensus among movement disorder specialists on clinical indicators for identification and management of advanced Parkinson’s disease: A multi-country Delphi-panel approach. Curr Med Res Opin 34: , 2063–2073. |
[19] | Syed N , Murphy J , Zimmerman T , Mark MH , Sage JI ((1998) ) Ten years’ experience with enteral levodopa infusions for motor fluctuations in Parkinson’s disease. Mov Disord 13: , 336–338. |
[20] | Zibetti M , Merola A , Artusi CA , Rizzi L , Angrisano S , Reggio D , De Angelis C , Rizzone M , Lopiano L ((2014) ) Levodopa/carbidopa intestinal gel infusion in advanced Parkinson’s disease: A 7-year experience. Eur J Neurol 21: , 312–318. |
[21] | von Elm E , Altman DG , Egger M , Pocock SJ , Gøtzsche PC , Vandenbroucke JP , STROBE Initiative ((2007) ) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 370: , 1453–1457. |
[22] | Hughes AJ , Daniel SE , Kilford L , Lees AJ ((1992) ) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: A clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55: , 181–184. |
[23] | Sensi M , Preda F , Trevisani L , Contini E , Gragnaniello D , Capone JG , Sette E , Golfre-Andreasi N , Tugnoli V , Tola MR , Quatrale R ((2014) ) Emerging issues on selection criteria of levodopa carbidopa infusion therapy: Considerations on outcome of 28 consecutive patients. J Neural Transm 121: , 633–642. |
[24] | Esselink RA , de Bie RM , de Haan RJ , Lenders MW , Nijssen PC , Staal MJ , Smeding HM , Schuurman PR , Bosch DA , Speelman JD ((2004) ) Unilateral pallidotomy versus bilateral subthalamic nucleus stimulation in PD: A randomized trial. Neurol. 62: , 201–207. |
[25] | R Core Team (2016) R: A Language and Environment for Statistical Computing. |
[26] | Therneau T ((2015) ) A Package for Survival Analysis in S. version 2.38. URL http://CRAN.R-project.org/package=Surviv |
[27] | Collins GS , Reitsma JB , Altman DG , Moons KGM ((2015) ) Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis (TRIPOD): The TRIPOD Statement. Ann Intern Med 162: , 55–63. |
[28] | Moons KGM , Royston P , Vergouwe Y , Grobbee DE , Altman DG ((2009) ) Prognosis and prognostic research: What, why, and how? BMJ 338: , b375. |
[29] | Meppelink AM , Nyman R , van Laar T , Drent M , Prins T , Leenders KL ((2011) ) Transcutaneous port for continuous duodenal levodopa/carbidopa administration in Parkinson’s disease. Mov Disord 26: , 331–334. |
[30] | Fernandez HH , Standaert DG , Hauser RA , Lang AE , Fung VSC , Klostermann F , Lew MF , Odin P , Steiger M , Yakupov EZ , Chouinard S , Suchowersky O , Dubow J , Hall CM , Chatamra K , Robieson WZ , Benesh JA , Espay AJ ((2015) ) Levodopa-carbidopa intestinal gel in advanced Parkinson’s disease: Final 12-month, open-label results. Mov Disord 30: , 500–509. |
[31] | Antonini A , Yegin A , Preda C , Bergmann L , Poewe W ((2015) ) Global long-term study on motor and non-motor symptoms and safety of levodopa-carbidopa intestinal gel in routine care of advanced Parkinson’s disease patients; 12-month interim outcomes. Parkinsonism Relat Disord 21: , 231–235. |
[32] | Lang AE , Rodriguez RL , Boyd JT , Chouinard S , Zadikoff C , Espay AJ , Slevin JT , Fernandez HH , Lew MF , Stein DA , Odin P , Fung VSC , Klostermann F , Fasano A , Draganov P V , Schmulewitz N , Robieson WZ , Eaton S , Chatamra K , Benesh JA , Dubow J ((2016) ) Integrated safety of levodopa-carbidopa intestinal gel from prospective clinical trials. Mov Disord 31: , 538–546. |
[33] | Davis SM , Stroup TS , Koch GG , Davis CE , Rosenheck RA , Lieberman JA ((2011) ) Time to All-cause Treatment Discontinuation as the Primary Outcome in the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia study. Stat Biopharm Res 3: , 253–265. |
[34] | Altman DG , Bland JM ((1998) ) Time to event (survival) data. BMJ 317: , 468–469. |
[35] | Thabane L , Mbuagbaw L , Zhang S , Samaan Z , Marcucci M , Ye C , Thabane M , Giangregorio L , Dennis B , Kosa D , Debono VB , Dillenburg R , Fruci V , Bawor M , Lee J , Wells G , Goldsmith CH ((2013) ) A tutorial on sensitivity analyses in clinical trials: The what, why, when and how. BMC Med Res Methodol 13: , 92. |
[36] | Klostermann F , Bojarski C , Marzinzik F , Maier A , Schindlbeck KA , Ehlen F ((2017) ) Necessity of long-term alertness in levodopa-carbidopa intestinal gel infusion for PD patients. Mov Disord 32: , 300–301. |




