Telemedicine in Neuromuscular Diseases During Covid-19 Pandemic: ERN-NMD European Survey
Abstract
Background:
Telemedicine (TM) contributes to bridge the gap between healthcare facilities and patients’ homes with neuromuscular disease (NMD) because of mobility issues. However, its deployment is limited due to difficulties evaluating subtle neurological signs such as mild weakness or sensory deficits. The COVID-19 pandemic has disrupted healthcare delivery worldwide, necessitating rapid measures implementation by health care providers (HCPs) to protect patients from acquiring SARS-CoV-2 while maintaining the best care and treatment.
Objectives:
Given the challenges faced by remote healthcare assistance of NMD patients, we aim to evaluate the use of TM in NMD during the COVID-19 pandemic.
Methods:
Based on the Model for Assessment-of-Telemedicine-Applications (MAST), we conducted a survey amongst clinicians of the ERN EURO NMD (European-Reference-Network-for-Rare-Neuromuscular-Diseases).
Results:
Based on 42 responses over 76 expected ones, our results show that the COVID-19 pandemic significantly increased the number of HCPs using TM (from 60% to 100%). The TM types most used during the COVID-19 period are teleconsultation and consultation by phone, particularly in the context of symptoms worsening in NMD patients with COVID-19 infection. Most European HCPs were satisfied when using TM but as a complementary option to physical consultations. Many responses addressed the issue of technical aspects needing improvement, particularly for elderly patients who need caregivers’ assistance for accessing the TM platform.
Conclusions:
TM has been essential during COVID-19, but its use still presents some limitations for NMD patients with cognitive deficits or for first-time diagnosis. Thus, TM should be used as complement to, rather than substitute, for face-to-face consultations.
INTRODUCTION
Neuromuscular diseases (NMD) are mostly chronic by nature, which requires a regular follow-up by neurologists because of the progressive loss of muscle strength, their association with complications pertaining to the disease itself or by relating to disease-specific medication. This follow-up may include a regular check of the body weight with a constant adjustment of the diet by nutritionists in patients with swallowing difficulty, as well as a regular control of muscular performance by physiotherapists. Clinical and physical aspects of this follow-up is often combined with a regular check of the mental-health state of patients, as many research studies show a significant impact of NMD, such as Myotonic Dystrophy type 1, on the psychological state as well as on the cognitive performances, of NMD patients [1–5]. Furthermore, some NMD patients with Duchenne Muscular Dystrophy, Spinal Muscular Atrophy or Facioscapulohumeral muscular dystrophy (FSHD) may need to be monitored by speech therapists and occupational therapists. In NMDs patients with multisystem involvement, cardiac and pulmonary regular monitoring is also essential since symptoms related to cardiac or respiratory dysfunctions generally occur at advanced stages, but may also appear earlier in the disease evolution [6].
Thus, the health management of NMD patients needs to be performed at hospitals using a multidisciplinary approach that takes into account all the needs of NMD patients operated by clinicians and by a paramedical team with an expertise in neuromuscular disorders.
In March 2020, the World Health Organization (WHO) declared the coronavirus disease (COVID-19) outbreak as a pandemic due to an infectious disease caused by the SARS-CoV-2 virus, [7] (https://worldometers.info). This pandemic has disrupted every aspect of health care delivery, the global healthcare system, as well as the economy of many countries [8–11], which induced multiple periods of confinements and increased periods of quarantine. Patients with NMD, are particularly vulnerable to COVID-19 disease because the COVID-19-induced cardiomyositis and/or chronic respiratory infections can be aggravated in patients with NMD, especially in those who are ventilated, have bulbar dysfunction and/or are immunocompromised [12–14]. Most patients felt the urgency to keep away from the SARS-CoV-2 virus. Therefore, in order to closely monitor the NDM patients at home during the COVID-19 pandemic, many health care services have adopted the use of telemedicine (TM) [8, 10, 15–17].
TM uses telecommunication technology, which provides access to healthcare and to specific medical expertise, thereby minimizing disparities caused by geographic or physical barriers [18]. This clinical application has been first setup for patients with difficulties accessing healthcare facilities with relevant clinical expertise, or facing a lack of means of transportation especially in rural areas [19]. Compared to conventional methods of care, TM has been proven to be very useful and effective and therefore appreciated by both clinicians and patients [20, 21] especially in the context of diagnosis, treatment and follow-up of patients with chronic diseases. For example, the use of TM was efficient for the follow-up and treatment of facioscapulohumeral dystrophy (FSHD) patients, by reducing the number of their hospital admissions and improving their quality of life [19]. Following the quick spread of the SARS-CoV-2 virus, TM has been quickly adopted by a large number of healthcare services [8, 10, 16] especially for NMD patients with myasthenia gravis (MG) or with myositis, for whom monitoring is essential because of the risk of imminent respiratory failure related to respiratory and bulbar muscle weakness, and the use of immunosuppressive medication [22–25].
Despite the benefits of TM for the remote treatment and follow-up of NMD patients, some clinicians have been reluctant to set up TM platforms because of the perceived limitations linked to remote clinical evaluations, such as physical examination with an accurate evaluation of muscle strength. Thus, according to some HCPs, TM appears beneficial only for a certain type of NMD patients who are clinically stable and with a well-known diagnosis, especially when it comes to remote assessment of subtle neurological signs such as mild weakness or sensory deficit [16]. Despite these significant limitations in the use of TM in the field of NMD, a recent publication suggests that functional evaluation of neuromuscular patients by telemedicine is possible, especially if the alternative is not to see NMD patients at all [8]. For example, clinicians assessed the ability of patients to stand still without assistance in order to evaluate “stance and balance”.
Given the heterogeneous nature of opinions regarding the use of TM in the field of NMD, we designed a survey with the help of the European Reference Network (ERN) network of Neuromuscular Disease (ERN-EURO-NMD) to evaluate the efficiency and the global satisfaction level of European HCPs on the use of TM during the COVID-19 pandemic.
MATERIAL AND METHODS
We conducted a survey amongst HCPs representatives of the ERN-EURO-NMD. The survey was a retrospective study on the use of TM in NMD patients. Surveys were sent as a word document via email to all participants in August 2021 and responses were collected and analyzed during the months of September through December 2021. Surveys included basic information such as: the European country of the HCP, name of hospital/clinic and years of experience of HCPs as well as the field of NMD (Muscle, nerve, motor neuron, neuromuscular junction or mitochondrial) and the specific number of NMD patients seen annually in each HCP’s center. In another section, of the survey posed specific questions on the type and context of TM used before and during the COVID-19 pandemic. In addition, some general questions such as the age of the patient, and their level of education were raised. TM can be distinguished into five modes: teleconsultations (which allows a medical professional to advice a patient remotely via communication technologies for the purpose of providing diagnostic or therapeutic advice); tele-expertise (practice in which a physician benefits from professional advices provided by other physicians via Information and Communication Technologies (ICT) to improve a patient’s clinical health status, which can be achieved outside the presence of the patient); tele-monitoring (allows a medical professional to monitor and supervise a patient remotely via ICTs); tele-assistance (allowing a medical professional to assist remotely another medical professional during an intervention via ICTs); medical responses (used to provide quick and efficient emergency services; the paramedics support the medical response of both air and ground ambulances). The final section of the survey addressed the evaluation of TM through different criteria of the Model for Assessment of Telemedicine Applications (MAST) [26], such as the technical feasibility, the accessibility of TM and the quality of care. Some questions of the survey required a response on a Likert scale from 1 (“ I completely disagree with the statement”) to 10 (“I completely agree”). A version of this survey is illustrated in Supplementary Figure 1. We also asked HCPs to indicate the age category of NMD patients seen via different types of TM (tele-monitoring, teleconsultation, or by phone).
Before statistical analysis, data were extracted and classified in an Excel sheet as qualitative or quantitative variables. Pie charts and histograms represent the analysis of descriptive data. Quantitative data are presented in histograms with additional standard error of mean (SEM). Comparative data analysis was done on qualitative variables using the Chi-square test and quantitative variables using non-parametric tests (Mann Whitney). These comparative analyses of the data were performed using the Prism-GraphPad software. For the analysis of this exploratory survey, the statistical significance of P-values is described as follows: *p < 0.05; **p < 0.01 and ***p < 0.001.
RESULTS
Forty-two over seventy-six HCPs of the ERN-EURO-NMD residing in European countries responded to the survey that is attached to the manuscript as Supplemental Figure 1. Respondents were unequally distributed across European countries (Fig. 1A). The majority of respondents have either 1 to 5 or 21 to 30 years of professional experience in NMD (Supplementary Figure 2A). Supplementary Figure 2B showed that the highest percentage of HCPs worked in the field of “Muscle” (31%) followed by ‘Motoneuron’ (21%), 18% and 17% of HCPs, respectively, worked in the field of Neuromuscular Junction and Nerve, and 13% of HCPs had an expertise in Mitochondrial myopathies. It is important to mention that most HCPs had more than one filed of expertise but this result was not captured in the pie-chart of Supplementary Figure 2B. In Supplemental Figure 2C, we show that 52% of HCPs follow more than 800 NMD patients annually, 24% between 200 and 400 NMD, 14% between 400 and 800 NMD and 15% either 20 to 200 or more than 2000 of NMD patients).
Fig. 1
European Health Care Providers (HCPs) respondents. A. Name of European country and number of HCPs participants to the survey per country. B. Percentage of HCPs using Telemedicine (TM) before and during COVID-19. Note that 100% of HCPs have responded “Yes” to the use of TM during COVID-19 (p < 0.0001; Chi2; test n = 42). C. Average number of NMD patients seen via TM during COVID-19 (p < 0.001; Mann Whitney test; n = 13).
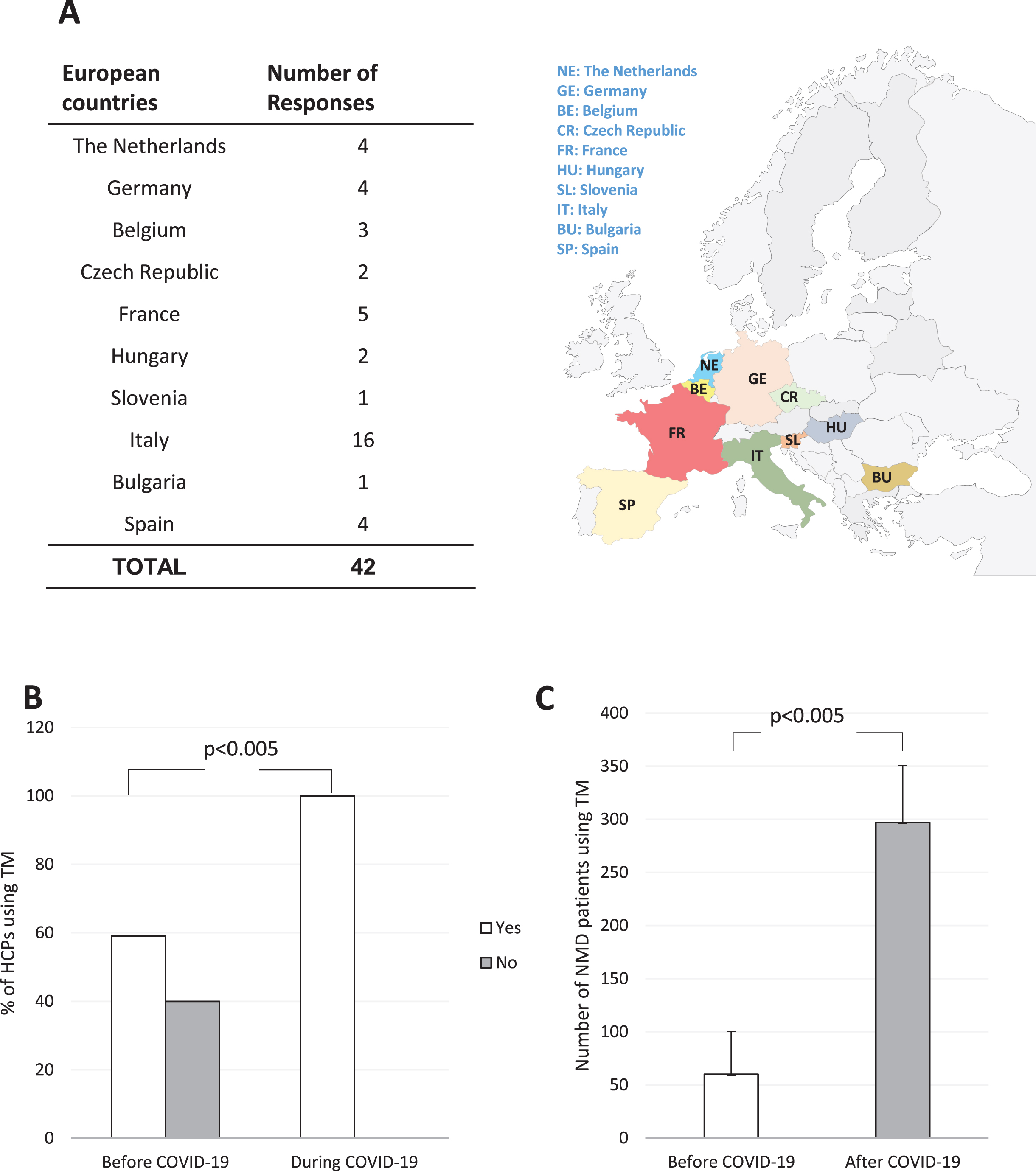
To assess the use and effectiveness of TM during the COVID-19 pandemic, we asked all HCPs whether they had used TM before and during the pandemic of COVID-19. Before COVID-19, 40% of HCPs had not had experience with TM while 60% of HCPs reported to have used TM. In contrast, during the COVID-19 pandemic, all respondents (100% of HCPs) of this survey have used TM. Figure 1B showed a significant increase in the percentage of HCPs using TM during the COVID-19 pandemic (p < 0.0005 Chi2 test n = 42). Consistently, the number of NMD patients seen by HCPs via TM increased from 61±40 before to 297±54 during COVID-19, (p < 0.0005, Mann Whitney test, n = 13, Fig. 1C)
Teleconsultation and consultations by phone, both TM types mostly used during the COVID-19 pandemic are represented in Fig. 2. There was a significant increase in HCPs using teleconsultations (from 28% before to 78% during COVID-19, p < 0.0005 Chi2 test, n = 42, Fig. 2A) as well as a significant increase in HCPs performing consultations by phone (from 52%, before to 85% of HCPs responses, during the COVID-19 pandemic, p < 0.005, Chi2 test, n = 42, Fig. 2A). Telemonitoring, tele-assistance and tele-expertise were less often used (Fig. 2A).
Fig. 2
Different types and contexts of telemedicine used by HCPs before and during COVID-19. A. Histogram showing different types of telemedicine used by HCPs with NMD patients before and during COVID-19. Note the significant increase in the use of teleconsultation, and consultation by phone during COVID-19. B. Histograms summarizing all contexts during which teleconsultations, consultations by phone and tele-monitoring have been used before and during COVID-19. Note the significant increase in the context of therapy, advice for physical therapy, diagnosis and general follow-up particularly during the acts of teleconsultations. A new context related to the worsening of NMD during COVID-19 appeared in each type of TM (teleconsultations, consultations by phone and telemonitoring).
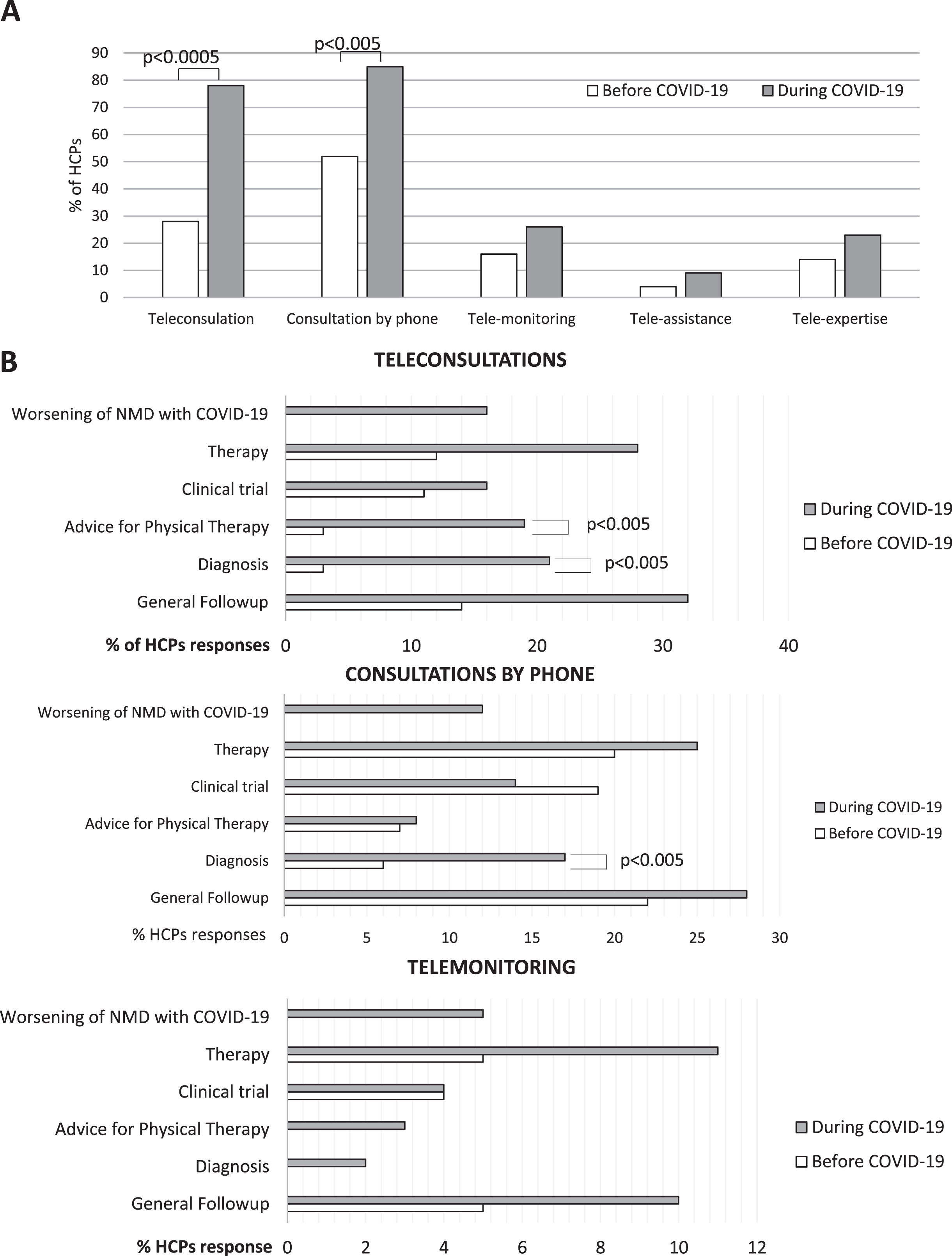
Participants also had to specify the context during which TM practices (teleconsultations, consultations by phone or tele-monitoring) had been performed before and during COVID-19. As shown in Fig. 2B, 16% of the HCPs reported that teleconsultations were used in the context of NMD symptoms worsening in patients with COVID-19. There was also a significant increase in the use of teleconsultation for therapy (from 12% before to 28% during COVID-19, p < 0.0005, Chi2 test), for advice on physical therapy (from 3% before to 19% during COVID-19, p < 0.0005, Chi2 test), for diagnosis (from 3% before, to 21% during COVID-19, p < 0.0005, Chi2 test), and for general follow-up visits (from 14% before, to 32% during COVID-19, p < 0.05, Chi2 test). Regarding consultations by phone, 6% of HCPs have used it in the context of diagnosis before COVID-19 and 17% of HCPs have used it during COVID-19, p < 0.05, Chi2 test). The practice of telemonitoring was used for different reasons, but no significant difference was observed between the period before and during COVID-19. As for other types of TM, we have seen a new context related to NMD symptoms worsening in patients with COVID-19 appeared during the period of COVID-19, Fig. 2B).
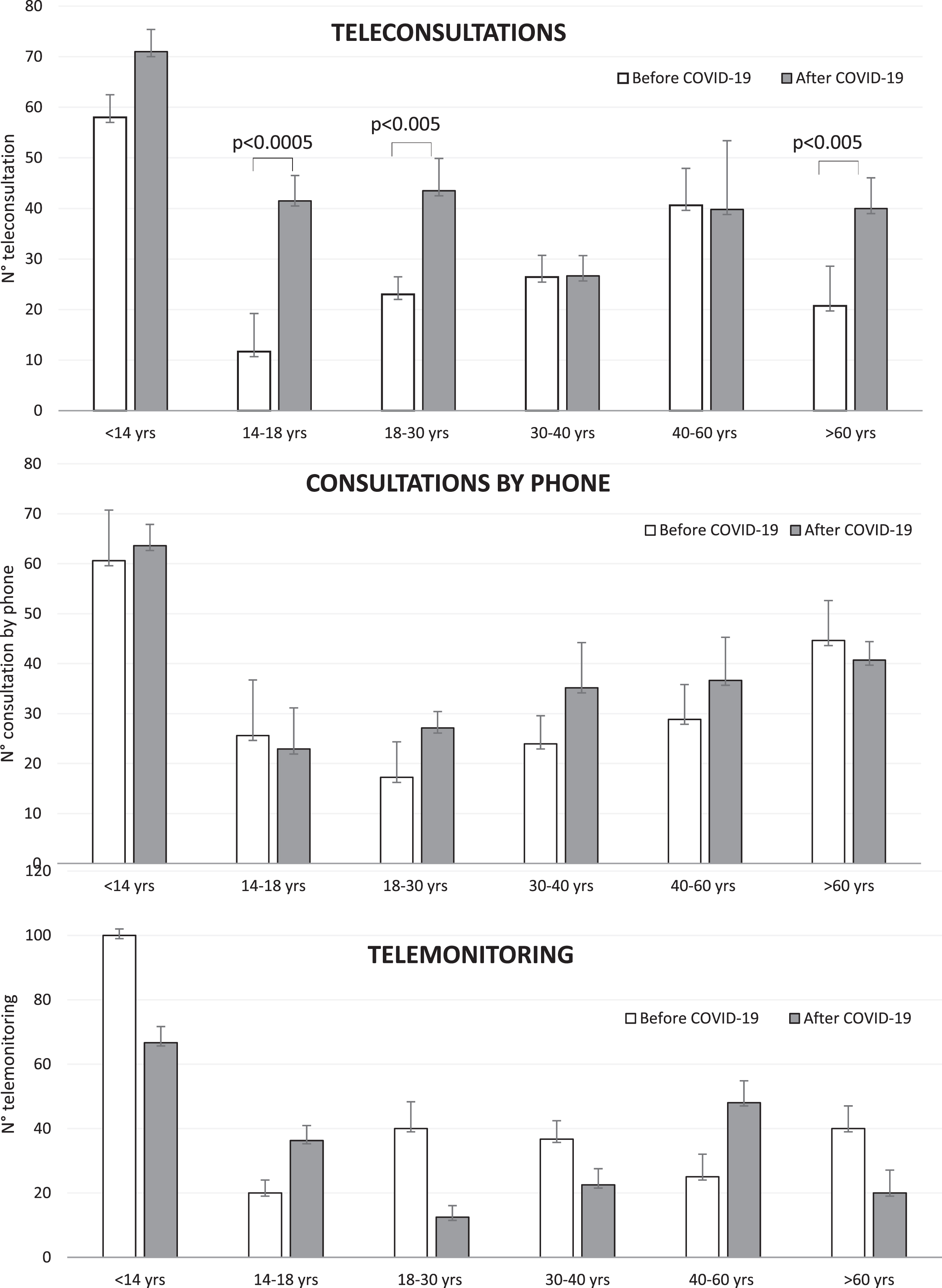
As shown in Fig. 3, we found a significant increase in the use of teleconsultations during the COVID-19 pandemic for NMD patients with the following age ranges: 14–18, 18–30 and beyond 60 years old (For 14–18 years old: an increase of HCPs responses from 11.6±7.54% to 41.5±5%, p < 0.0005; for 18–30 years old: an increase of HCPs responses from 23±3.49% to 43.5±6.4%, p < 0.005; for >60 years old: an increase of HCPs responses from 20.71±7.86% to 40±6.04%, p < 0.005, Chi2 test). However, no significant changes were found in the use of TM for these age ranges for other TM modes such as tele-monitoring, or phone consultation.
Fig. 3
Age range of NMD patients using telemedicine. Histogram showing the range of age of NMD patients using different modes of telemedicine: teleconsultations, phone consultation or tele-monitoring before and during COVID-19. Note the significant increase of NMD patients at the age of 14–18 years old, of 18–30 years old and of elder age >60 years old using teleconsultations during COVID-19.
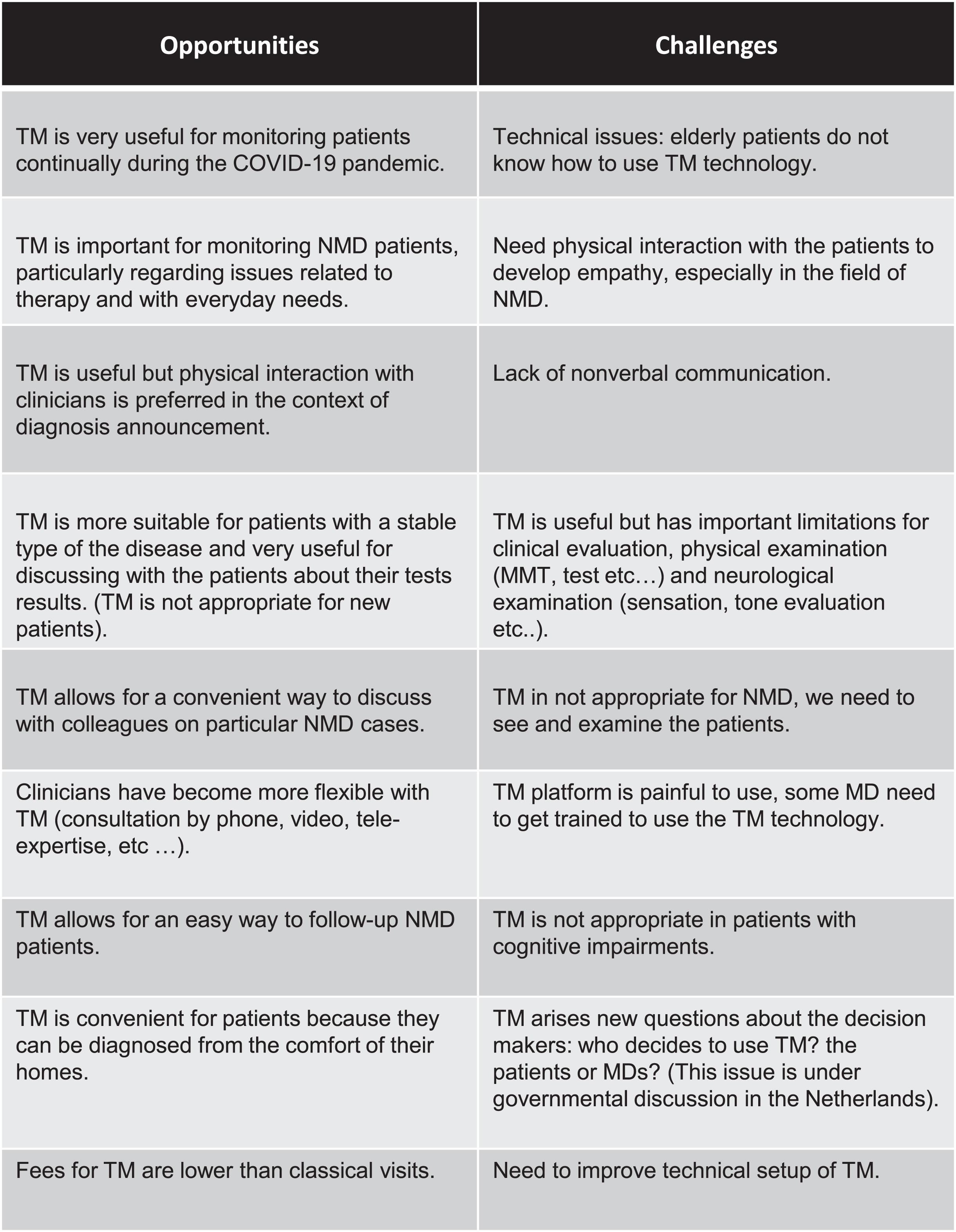
Finally, the last section of the survey included a questionnaire according to the Model for AS-sessment of Telemedicine application: MAST [26], in which participants of the survey had to respond to different categories of questions including the technical feasibility, the acceptability, the accessibility of the TM tool, as well as the quality of care of patients seen through TM. Participants of the survey also had to provide their global appreciation of using TM. All responses of HCPs are shown in the summary graph of Supplementary Figure 3, in which the appreciation of HCPs using TM application is expressed in percentage of satisfaction for all relevant criterion (technical feasibility, acceptability, quality of care, etc...) according to the MAST structure used for the assessment of TM applications [26]. The results show that the satisfaction level of HCPs for TM technical feasibility, which included for example the delay of connection to the platform of telemedicine or the quality of sound and images as well as the effectiveness of data transmission, reached 84±4%, suggesting that TM was technically effective in all European countries included in this survey. The general acceptability for using TM reached 59±9% by all HCPs. The safety of patients while using this remote type of health management was evaluated by asking the HCPs whether the use of TM resulted in immediate risk or harm for NMD patients. 61±7% reported that there was no immediate risk or harm. The assessment of the satisfaction and accessibility of TM through an evaluation of scheduling for teleconsultations led to 65±8% of satisfaction for accessibility to TM, and 66±2% for global appreciation of TM. In Fig. 4 the participants provides comments on the benefits and challenges of TM.
Fig. 4
HCPs comments regarding the use of telemedicine (TM). General HCPs feedbacks on the PROS and CONS of TM collected in the survey.
DISCUSSION
Altogether, data collected from HCPs indicate that the the majority of NMD patients, despite some limitations associated with technological barriers appreciate the value and use for TM.
Consistent with previous studies, the results of this survey confirm that the COVID-19 pandemic resulted into an important reorganization of all European healthcare facilities in the field of NMD. The use of TM by European HCPs and NMD patients has significantly increased during the COVID-19 pandemic. Fourty-two HCPs from ten European countries have participated in this survey, which represent distinct areas of NMD including muscle, motoneuron, neuromuscular junction, nerve and mitochondria and they all made use of TM during the COVID-19 pandemic. In parallel, the number of NMD patients seen through TM during the pandemic has also significantly increased.
Given the heterogeneity in the number of HCPs per country in Europe, ranging from 1 in Slovenia and Bulgaria to 21 in Italy, many responses are from Italy. However, if we look at the percentage of centers that have answer to the survey (Italy (16/21; 76%), France (5/10; 50%), Belgium (3/5; 60%), Spain (4/6; 67%), Netherlands (4/6. 67%), Germany (4/10; 40%), Czech (2/2; 100%), Slovenia (1/1; 100%), Hungary (2/2; 100%), Bulgaria (1/1; 100%)), the response rate is similar between the different countries. Lastly, Italy was hit hard by Covid compared to other EU countries, hence an increased reactivity/response to this survey.
Our data also show that teleconsultations and phone consultation are the most frequent types of telemedicine used during the COVID-19 in different contexts such as: worsening of NMD, therapy or physical therapy advice, diagnosis and general follow-up. The worsening of NMD symptoms has been reported in a recent study that described NMD patients with pre-existing respiratory impairment, and/or suffering from swallowing difficulty, and/or on long-term immunosuppressive therapy, are classified “at high risk” for developing severe forms of COVID-19 [27]. Patients with motoneuron diseases (including spinal muscular atrophy), with associated ventilatory muscle deficit, may be particularly susceptible to the infection by SARS-CoV-2. In addition, some other type of NMD patients are also likely to be at increased risk of developing a severe form of COVID-19; for example patients with muscular dystrophies, including myotonic dystrophies, or metabolic myopathies (eg Pompe disease), with ventilatory muscle weakness and /or associated cardiomyopathy. Because of this increased risk during the COVID-19 pandemic, HCPs all over the world and in particularly in Europe have focused on reducing and limiting the exposure of patients to the coronavirus as much as possible. Thus virtual consultations which have replaced outpatient visits are mainly based on a face-to-face video conference or on interview by telephone. On the other hand, the presence of these patients on site is sometimes necessary because cardiac and/or respiratory measurements are mandatory for the follow-up of their state of health, which adds a limitation to the use of the TM.
European HCPs who participated to this survey have used teleconsultations, telemonitoring or consultations by phone with NMD patients at different ages (from <14 to >60 years old) before and during period of COVID-19. But during COVID-19, our data show an increase of patients using TM who are 14–18, 18–30 and beyond 60 years old, suggesting that TM technology is not restricted to fragile or elderly patients but has also been useful for young NMD patients.
The majority of HCPs who have responded to this survey recognized the effectiveness of TM while managing NMD patients during the COVID-19 pandemic. Based on their extensive professional experiences (from 5 to 45 years), European HCPs have used TM in multiple contexts during the COVID-19 pandemic. The use of TM is not only restricted to the patients’ follow-up only as suggested [28] but rather extended to interventions according to the need of NMD patients such as regular advice for physical therapy or diagnosis. It is possible that the guidelines for the care of NMD patients that have been published during the COVID-19 pandemic might have allowed HCPs to better deal with the NMD challenges by using TM [14, 29–32]. For example, the French Rare Health Care for Neuromuscular Diseases Network (FILNEMUS) has provided guidance to harmonize the management of neuromuscular patients during the COVID-19 pandemic and to limit the contamination of fragile NMD patients [14]. Some of these recommendations included to reschedule non-urgent appointments and/or, if appropriate, to replace face-to-face appointments by teleconsultations. Furthermore, if patients did not have the necessary equipment to perform teleconsultation, they could use consultation by phone. The American Academy of Neuromuscular and Electrodiagnostic Medicine (AANEM) has also issued guidelines for clinical visits and telemedicine during the COVID-19 pandemic in which the authors provided guidance on the tools and techniques of information and distance education, the use of which has spread very quickly for the care of neuromuscular patients [32]. An international working group [33] has published other guidance for the management of Myasthenia Gravis (MG) and Lambert-Eaton myasthenic syndrome (LEMS) during the COVID-19.
Before COVID-19, the deployment of telehealth in neurology and in particular in neuromuscular medicine, has been slow [10, 34, 35]. The argument used to explain this delay was based on the need for a clinical examination with at least an assessment of muscle strength, sensory function, and tendon reflexes, all of which are difficult to implement from a distance. Some clinical performance scales have been developed and can be used for remote evaluation of activity limitation such as Brooke and Vignos, ONLS (Overall Neuropathy Limitation Scale), INCAT (Inflammatory Neuropathy Cause and Treatment), are being used during teleconsultations on a regular basis. In addition, online guidance can provide useful information on how to manage the interruption of physiotherapy support [14]. Indeed, maintaining muscle strength and flexibility is highly recommended in NMD through the help of physical therapy. However, during the COVID-19, restricted mobility of people in order to increase the resistance against the spread of COVID-19, led to the closure of private therapist’s practices, including physiotherapists, speech therapists, and occupational therapists. Because of the aggravation of symptoms that can occur in some NMD patients, tele-education of remote physical reeducation have been established to allow the continuity of patient support by online videos adapted to the age and degree of motor impairment of NMD patients. As most of HCPs centers have maintained tele-consultations activity, patients and caregivers were encouraged to contact healthcare centers to receive individualized support. In France, as in other European countries, the use of TM has been increasing during the COVID-19 pandemic and many educational tools technologies are available for each center who practice TM.
Our findings support the conclusion that TM has been very effective in expediting the care and follow-up of NMD patients in Europe during the COVID-19, improving health management of NMD patients. However, some limitations remain such as the contradiction between remote assessment and accurate clinical evaluation, which makes TM as a complementary tool rather than a substitute for face-to-face visits.
REFERENCES
[1] | Jacques MF , Stockley RC , Onambele-Pearson GL , Reeves ND , Stebbings GK , Dawson EA , et al. Quality of life in adults with muscular dystrophy. Health Qual Life Outcomes. (2019) ;17: :121. https://doi.org/10.1186/s12955-019-1177-y. |
[2] | Mennetrey C , Jambaqué I , Desguerre I , Angeard N . Phénotypes cognitifs dans la dystrophie musculaire de Duchenne: Revue de la littérature et perspectives (neuro) développementales. Can Psychol Can. (2020) ;61: :215–33. https://doi.org/10.1037/cap0000185. |
[3] | Gallais B , Montreuil M , Gargiulo M , Eymard B , Gagnon C , Laberge L . Prevalence and correlates of apathy in myotonic dystrophy type 1. BMC Neurol. (2015) ;15: :148. https://doi.org/10.1186/s12883-015-0401-6. |
[4] | Huerta E , Jacquette A , Cohen D , Gargiulo M , Servais L , Eymard B , et al. Forme infantile de la dystrophie myotonique de type 1 (DM1) et troubles du spectre autistique (TSA): Existe-t-il une comorbidité? Neuropsychiatr Enfance Adolesc. (2015) ;63: :91–8. https://doi.org/10.1016/j.neurenf.2014.11.005. |
[5] | Sayah S , Morin A . Retentissement des troubles cognitifs sur la vie sociale, professionnelle et émotionnelle des patients dans la forme adulte de la dystrophie myotonique de type I. Cah Myol. (2016) ;28–30. https://doi.org/10.1051/myolog/201613007. |
[6] | Mary P , Servais L , Vialle R . Neuromuscular diseases: Diagnosis and management. Orthop Traumatol Surg Res. (2018) ;104: :S89–95. https://doi.org/10.1016/j.otsr.2017.04.019. |
[7] | Huang C , Wang Y , Li X , Ren L , Zhao J , Hu Y , et al. Clinical features of patients infected with novel coronavirus in Wuhan, China. Lancet Lond Engl. (2020) ;395: :497–506. https://doi.org/10.1016/S0140-6736(20)30183-5. |
[8] | Saporta MA , Granit V , Lewis R , Benatar M . Yes, we can: Neuromuscular examination by telemedicine. Muscle Nerve. (2020) ;62: :E83–5. https://doi.org/10.1002/mus.27056. |
[9] | BokoloAJ . Exploring the adoption of telemedicine and virtual software for care of outpatients during and after COVID-19 pandemic. Ir J Med Sci. (2021) ;190: :1–10. https://doi.org/10.1007/s11845-020-02299-z. |
[10] | Keesara S , Jonas A , Schulman K . Covid-19 and Health Care’s Digital Revolution. N Engl J Med. (2020) ;382: :e82. https://doi.org/10.1056/NEJMp2005835. |
[11] | Rao SS , Loeb AE , Amin RM , Golladay GJ , Levin AS , Thakkar SC . Establishing telemedicine in an academic total joint arthroplasty practice: Needs and opportunities highlighted by the COVID-19 pandemic. Arthroplasty Today. (2020) ;6: :617–22. https:doi.org/10.1016/j.artd.2020.04.014. |
[12] | Angelini C , Siciliano G . Neuromuscular diseases and Covid- Advices from scientific societies and early observations in Italy. Eur J Transl Myol. (2020) ;30: :9032. https://doi.org/10.4081/ejtm.2019.9032. |
[13] | Kuba K , Imai Y , Rao S , Gao H , Guo F , Guan B , et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat Med. (2005) ;11: :875–9. https://doi.org/10.1038/nm1267. |
[14] | Solé G , Salort-Campana E , Pereon Y , Stojkovic T , Wahbi K , Cintas P , et al. Guidance for the care of neuromuscular patients during the COVID-19 pandemic outbreak from the French Rare Health Care for Neuromuscular Diseases Network. Rev Neurol (Paris). (2020) ;176: :507–15. https://doi.org/10.1016/j.neurol.2020.04.004. |
[15] | Haulman A , Geronimo A , Chahwala A , Simmons Z . The use of telehealth to enhance care in ALS and other neuromuscular disorders. Muscle Nerve. (2020) ;61: :682–91. https://doi.org/10.1002/mus.26838. |
[16] | Garibaldi M , Siciliano G , Antonini G . Telemedicine for neuromuscular disorders during the COVID-19 outbreak. J Neurol. (2021) ;268: :1–4. https://doi.org/10.1007/s00415-020-10063-7. |
[17] | Lurie N , Carr BG . The role of telehealth in the medical response to disasters. JAMA Intern Med. (2018) ;178: :745–6. https://doi.org/10.1001/jamainternmed.2018.1314. |
[18] | Hatcher-Martin JM , Adams JL , Anderson ER , Bove R , Burrus TM , Chehrenama M , et al. Telemedicine in neurology: Telemedicine work group of the American academy of neurology update. Neurology. (2020) ;94: :30–8. https://doi.org/10.1212/WNL.0000000000008708. |
[19] | Portaro S , Calabrò RS , Bramanti P , Silvestri G , Torrisi M , Conti-Nibali V , et al. Telemedicine for facio-scapulo-humeral muscular dystrophy: A multidisciplinary approach to improve quality of life and reduce hospitalization rate? Disabil Health J. (2018) ;11: :306–9. https://doi.org/10.1016/j.dhjo.2017.09.003. |
[20] | Ekeland AG , Bowes A , Flottorp S . Effectiveness of telemedicine: A systematic review of reviews. Int J Med Inf. (2010) ;79: :736–71. https://doi.org/10.1016/j.ijmedinf.2010.08.006. |
[21] | Wootton R . Twenty years of telemedicine in chronic disease management–an evidence synthesis. J Telemed Telecare. (2012) ;18: :211–20. https://doi.org/10.1258/jtt.2012.120219. |
[22] | Muppidi S , Guptill JT , Jacob S , Li Y , Farrugia ME , Guidon AC , et al. COVID-19-associated risks and effects in myasthenia gravis (CARE-MG). Lancet Neurol. (2020) ;19: :970–1. https://doi.org/10.1016/S1474-4422(20)30413-0. |
[23] | Restivo DA , Centonze D , Alesina A , Marchese-Ragona R . Myasthenia gravis associated with SARS-CoV-2 infection. Ann Intern Med. (2020) ;173: :1027–8. https://doi.org/10.7326/L20-0845. |
[24] | Businaro P , Vaghi G , Marchioni E , Diamanti L , Arceri S , Bini P , et al. COVID-19 in patients with myasthenia gravis: Epidemiology and disease course. Muscle Nerve. (2021) ;64: :206–11. https://doi.org/10.1002/mus.27324. |
[25] | Bos WH , van Tubergen A , Vonkeman HE . Telemedicine for patients with rheumatic and musculoskeletal diseases during the COVID-19 pandemic; a positive experience in the Netherlands. Rheumatol Int. (2021) ;41: :565–73. https://doi.org/10.1007/s00296-020-04771-6. |
[26] | Kidholm K , Ekeland AG , Jensen LK , Rasmussen J , Pedersen CD , Bowes A , et al. A model for assessment of telemedicine applications: Mast. Int J Technol Assess Health Care. (2012) ;28: :44–51. https://doi.org/10.1017/S0266462311000638. |
[27] | Clinique: Maladies neuromusculaires et COVID-19. Cah Myol. (2020) :34–5. https://doi.org/10.1051/myolog/202021012. |
[28] | Garibaldi M , Siciliano G , Antonini G . Telemedicine for neuromuscular disorders during the COVID-19 outbreak. J Neurol. (2021) ;268: :1–4. https://doi.org/10.1007/s00415-020-10063-7. |
[29] | Guidon AC , Amato AA . COVID-19 and neuromuscular disorders. Neurology. (2020) ;94: :959–69. https://doi.org/10.1212/WNL.0000000000009566. |
[30] | Al Hussona M , Maher M , Chan D , Micieli JA , Jain JD , Khosravani H , et al. The virtual neurologic exam: Instructional videos and guidance for the COVID-19 era. Can J Neurol Sci J Can Sci Neurol. (2020) ;47: :598–603. https://doi.org/10.1017/cjn.2020.96. |
[31] | Sobierajska-Rek A , Mański ł , Jabłońska-Brudło J , Śledzińska K , Ucińska A , Wierzba J . Establishing a telerehabilitation program for patients with Duchenne muscular dystrophy in the COVID-19 pandemic. Wien Klin Wochenschr. (2021) ;133: :344–50. https://doi.org/10.1007/s00508-020-01786-8. |
[32] | Kassardjian CD , Desai U , Narayanaswami P , AANEM Quality and Patient Safety Committee of the AANEM. Practical guidance for managing electromyography requests and testing during the COVID-19 pandemic. Muscle Nerve. (2020) ;62: :30–3. https://doi.org/10.1002/mus.26891. |
[33] | International MG/COVID-19 Working Group , Jacob S , Muppidi S , Guidon A , Guptill J , Hehir M , et al. Guidance for the management of myasthenia gravis (MG) and Lambert-Eaton myasthenic syndrome (LEMS) during the COVID-19 pandemic. J Neurol Sci. (2020) ;412: :116803. https://doi.org/10.1016/j.jns.2020.116803. |
[34] | Afshari M , Witek NP , Galifianakis NB . Education Research: An experiential outpatient teleneurology curriculum for residents. Neurology. (2019) ;93: :170–5. https://doi.org/10.1212/WNL.0000000000007848. |
[35] | Govindarajan R , Anderson ER , Hesselbrock RR , Madhavan R , Moo LR , Mowzoon N , et al. Developing an outline for teleneurology curriculum: AAN Telemedicine Work Group recommendations. Neurology. (2017) ;89: :951–9. https://doi.org/10.1212/WNL.0000000000004285. |



