Neonatal necrotizing enterocolitis due to COVID-19. A case report
Abstract
Digestive symptoms have been reported in an important proportion of children with COVID-19, and the clinical expression of critical patients with COVID-19 is thought to result from progressive increase of inflammation and an unusual trend of hypercoagulation. We report a newborn received with abdominal distension, green vomiting and imaging suggestive for enterocolitis. He had a close contact with COVID-19 and the PCR for SARS-CoV-2 came back positive. Despite the supportive measures, his condition deteriorated and a surgery was decided. The surgical exploration found an ischemic bowel. The therapeutic measures were ineffective as the child passed away a few hours after surgery despite the resuscitation treatment performed. The confirmed enterocolitis happening within the period of acute infection by SARS-CoV-2, the NEC was likely a manifestation of COVID-19.
1Introduction
The current 2019 coronavirus disease (COVID-19) is the world’s largest and most pervasive public health emergency in more than one hundred years. Providers are continuing to identify the spectrum of disease and symptoms across age groups, and the pathogenesis of COVID-19 is gradually being comprehended [1]. Angiotensin converting enzyme 2 (ACE2) was identified as a functional receptor for SARS-CoV, and there are many ACE 2 receptors in small intestines especially in ileum and colon. The clinical expression of critical patients with COVID-19 is thought to result from two distinctive features: progressive increase of inflammation and an unusual trend of hypercoagulation [2, 3]. Until now, children are considered as the population that is minimally affected by COVID-19. However, in this group, COVID-19 presents as a wide spectrum of disease states, from asymptomatic infection to multi-system inflammatory syndrome [4–6]. Digestive symptoms have been reported in an important proportion of children with COVID-19, and SARS-CoV-2 RNA has been detected in stool samples of children recovering from it [3, 7]. In children and in adults, intestinal manifestations of COVID-19 discovered include intestinal inflammation, bowel wall thickening, fluid-filled colon, pneumatosis intestinalis (PI), pneumoperitoneum, intussusception, and bowel ischemia [8]. To our best knowledge, only one neonatal necrotizing enterocolitis-like in infant with COVID-19 has been reported till now, and medically managed [9]. However several cases of PI attributed to severe COVID-19 were described, presumed due to the viral replication in the gastrointestinal epithelium, during an extended period of time, using the numerous ACE2 receptors for its entry process, and often not severe [3, 9–11]. Our case adds to the evolving COVID-19 literature as we report a unique case of a term and healthy newborn, infected with COVID-19, and who presented a severe and confirmed necrotizing enterocolitis (NEC).
2Case report
We report the case of a 4 weeks old male, born at 38 weeks of gestation, via simple vaginal delivery, with an APGAR score of 7,9, and 10 at 1, 5 and 10 minutes, normal birth weight, good tolerance of feeds with breast milk completed by formula-milk, and a normal growth and development till the age of 27 days, when he presented to the emergency room (ER) with low-grade fever (38°C), abdominal distension, green vomiting, and dehydration. He had medical history of an early presumed sepsis at day 3 of life with a history of maternal fever the days before delivery without documented infection, reduced sucking. Physical examination was unremarkable with normal neurological and general examination, but a bloodstained diapers has been noticed with soft and not distended abdomen. CBC was normal, and CRP at 12 mg/l. The PT was 50%. LP had not been done, and culture was not available in the hospital the days of admission. Chest and abdominal X-rays were normal. The diagnosis of neonatal sepsis associated to a classical and mild hemorrhagic disease of newborn was presumed and IV cephalosporin and gentamicine with vitamin K was initiated. After 72 hours, the child condition, CRP, and PT normalized. He received 10 days of IV antibiotics with discharge in a good condition, and a close follow up showed a normal baby with an appropriate growth, normal development, and no other abnormalities, especially no gastro-intestinal or hematologic symptoms during almost 3 weeks. During the week preceding the baby’s admission, several family cases of COVID 19 occurred, including his mother, all confirmed and mild to moderate according to the family. Parents reported that the baby had unusual and repeated episodes of emesis at 27 days of age, the day before his admission, but according to the mother he was otherwise well with normal appetite, normal stools, and no notable respiratory symptoms. A few hours before they brought him, at the age of 28 days, he started totally refusing feeds and having dark and green vomits with distended abdomen with no bowel movement during 24 hours.
On the physical examination, vitals were initially stable, the abdomen very distended and tender, justifying immediate admission, IV hydration, and nothing given by mouth (NPO), while waiting for laboratory and radiological explorations, and for pediatric surgeon’s review. Within the few hours of workup, the child had several green and profuse vomits, his abdomen became more tense, gastric tube was inserted to decompress stomach. Despite the supportive treatment (IV hydration, bowel rest, gastric decompression, and IV antibiotics: cefotaxime, metronidazole and gentamycin), signs of shock appeared. The infant was admitted to the intensive care unit with a close observation. Abdominal radiograph showed distended bowels with air-fluid levels, thickened intestine wall and PI, without evident pneumoperitoneum (Fig. 1). Routine labs returned with CRP 6, white blood cell count 6.3, hemoglobin 15, platelets 272, urea and electrolytes, and INR at 1.19. RT-PCR for SARS-CoV-2 from a nasopharyngeal swab has been performed. The surgeon decided an urgent laparotomy, and the exploration showed an intestine very distended and damaged, with hyperemia, signs of ischemia, cracks and feeling of emphysema-like perceptions evoking a PI on the palpation of the intestine wall (Fig. 2 and 3). There was no volvulus of the intestine. The gut abnormalities started approximately from 50 cm after the duodenal flexure till the ileocecal valve, and are associated with a small intra-peritoneal liquid suggestive of a peritonitis. Given the extent of the lesions and the instability of the baby, rapidly deteriorating, only a quick cleansing was made with a stomy upstream from the lesions, hopping an improvement of the vascularization of the gut with rest and supportive medications. Unfortunately, the child condition continued its aggravation with a shock becoming refractory, despite the fluid resuscitation and the vasoactive drugs, leading to death within a few hours after surgery, and despite the multiple resuscitation procedures. The RT-PCR for SARS-CoV-2 came back positive after patient’s death.
Fig. 1
Abdominal radiograph showing distended bowels with air-fluid levels and thickened intestine wall and PI. PI: pneumatosis intestinalis.
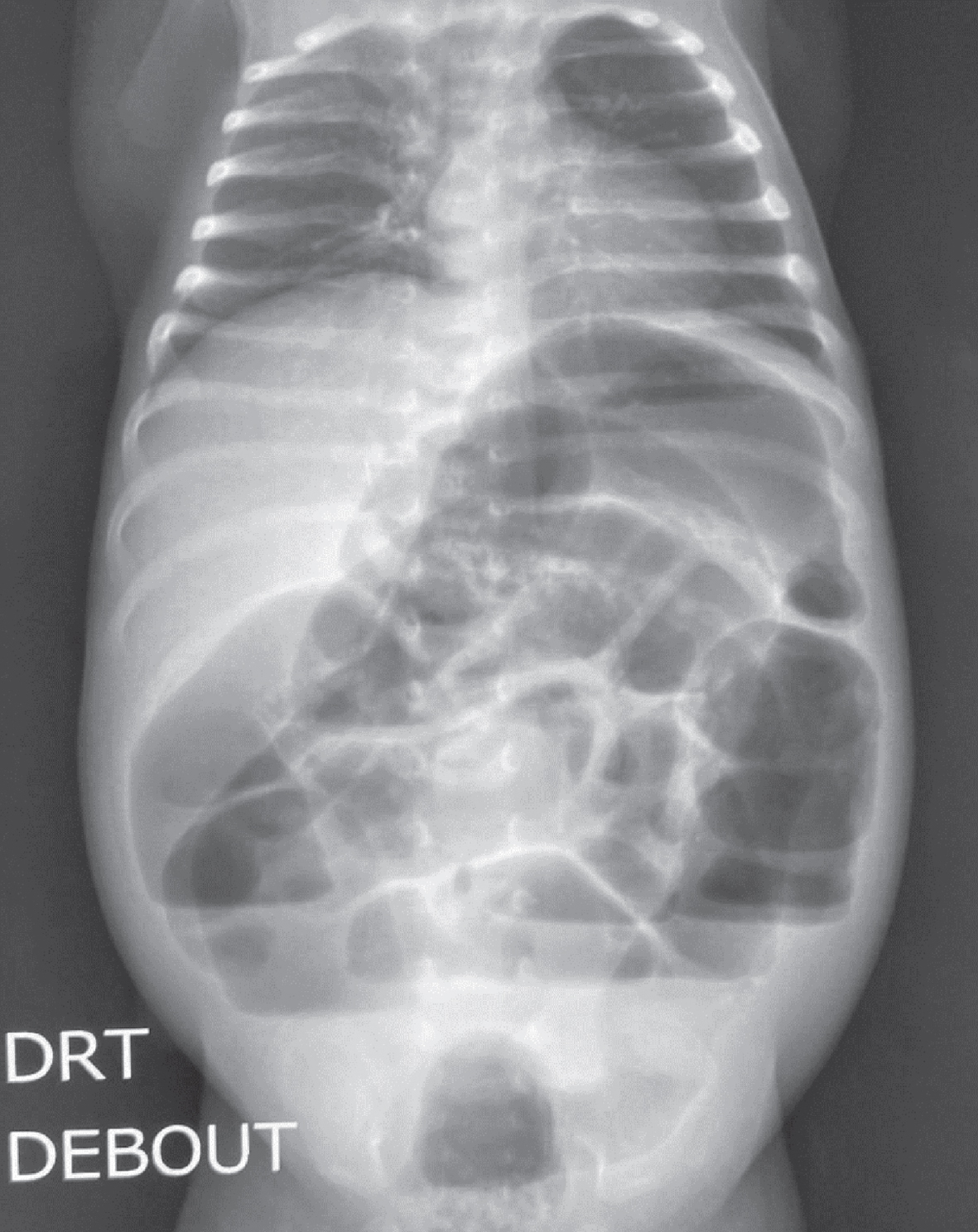
Fig. 2
Patient’s intestine on photos during the surgical intervention showing intestinal distension and hyperemia.

Fig. 3
Patient’s intestine on photos during the surgical intervention showing hyperemia, signs of ischemia, and cracks.

3Discussion
Our case describes a newborn diagnosed with COVID-19 who presented with an acute abdomen due to a severe NEC. A NEC epidemic in the 1980’s was thought to be secondary to Coronavirus after electron microscopy discovered Coronavirus viral morphology in neonatal stool samples and surgically resected specimens [12]. During the current COVID-19 pandemic, cases with solely digestive symptoms have been reported in both adults and children [12, 13]. However, only one case of presumed NEC has been reported to date in a 7 weeks baby [9]. Nevertheless, recent reports have identified cases of bloody stools associated gastroenteritis secondary to COVID-19 in adults, and isolated PI in moderate cases of COVID-19 [10–12]. NEC is characterized by ischemic necrosis of the intestinal mucosa with associated severe inflammation, invasion of enteric organisms, and dissection of gas along the bowel wall. It is well known that the incidence of NEC increases with decreasing birth weight and gestational age, and that term infants with NEC typically have associated comorbidities such as hypoxic newborns and congenital heart disease [9]. Case series regarding COVID-19 in neonates has primarily identified mild disease with severe disease limited to neonates and infants with associated comorbidities of prematurity or congenital cardiac disease [9]. Our patient was a term infant with no significant comorbidities or risk factors to develop NEC, and although he had been treated for presumed early sepsis during the first 2 weeks of life, he was considered as cured from it, as he fully recovered with absence of symptoms during 3 weeks with negative sepsis workup, and had completed 10 days of IV antibiotics, with a good weight gain and a normal development during the 3 weeks preceding the episode of NEC. Given that and the symptoms of NEC happening within the period of COVID-19, the confirmed enterocolitis was likely a manifestation of COVID-19.
Our patient was treated according to the NEC protocol with supportive care (resuscitation and bowel rest), broad-spectrum antibiotics, close monitoring with serial abdominal examinations, radiologic imaging, laboratory analysis, and surgical reviews. Crystalloid resuscitation was performed upon admission and continued. Finding that the clinical condition was rapidly worsening with successive bilious vomits, and increasing abdominal tenderness within a few hours, the surgical intervention was made urgently, and there was evidence of intestinal necrosis and ulceration, although no significant biological abnormalities usually associated with severe NEC. The intestine lesions’ is consistent with severe NEC and the surgeon made a stomy and decided to re-intervene after a few days of resuscitation and digestive tract rest, hoping to find less necrotic small bowel.
Limitations of our report are mainly due to the reduced local resources in our setting, and in the delay of arrival of our patient, coming in a rapidly worsening and severe condition, both not permitting to investigate totally his case. That is the reason for example the presence of SARS-CoV-2 and other pathogens in the stool samples couldn’t be tested. However, the positivity of the RT-PCR for SARS-CoV-2 from a nasopharyngeal swab suggestive of an acute phase of COVID-19 in a baby living in a family cluster of cases, and the absence of risk factors of NEC in our patient, made us considering this NEC as a manifestation of the COVID-19.
References
[1] | Krishnamurth G , Sahni R , Leone T , Kim F , Brooks MC , Morales SV , et al. Care of the COVID-19 exposed complex newborn infant. Semin Perinatol. (2020) ;44: (7):151282. |
[2] | Yuki K , Fujiogi M , Koutsogiannaki S . COVID-19 pathophysiology: A review. Clin Immunol. (2020) ;(215):108427. |
[3] | Rohania P , Karimib A , Tabatabaieb SR , Khalilic M , Sayyaria A . Protein losing enteropathy and pneumatosis intestinalis in a child with COVID 19 infection. J Pediatr Surg Case Rep. (2021) ;64: :101667. |
[4] | Honga H , Wanga Y , Chungb HT , Chenb CJ . Clinical characteristics of novel coronavirus disease 2019 (COVID-19) in newborns, infants and children. Pediatr Neonatol. (2020) ;61: (2):131–32. |
[5] | Zimmermann P , Curtis N . Coronavirus infections in children including COVID-19 an overview of the epidemiology, clinical features, diagnosis, treatment and prevention options in children. Pediatr Infect Dis J. (2020) ;39: (5):355–68. |
[6] | Rehman S , Majeed T , Ansari MA , Al-Suhaimi EA . Syndrome resembling Kawasaki disease in COVID-19 asymptomatic children. J Infect Public Health. (2020) ;13: (12):1830–2. |
[7] | Xiong LJ , Zhou MY , He XQ , Wu Y , Xie XL . The role of human coronavirus infection in pediatric acute gastroenteritis. Pediatr Infect Dis J. (2020) ;39: (7):645–9. |
[8] | Calcagno E , Sogunro O , Nepal P , Assaker R , Sapire J . COVID-19 induced mesenteric venous infarction. Case Report. Radiol. Case Rep. (2021) ;16: (8):1999–2002. |
[9] | Mehl SC , Whitlock RS , Marcano DC , Rialon KL , Arrington AS , Naik-Mathuria B . Necrotizing enterocolitis-like pneumatosis intestinalis in an infant with COVID-19. Pediatr Infect Dis J. (2021) ;40: (2):85–6. |
[10] | Meini S , Zini C , Passaleva MT , Frullini A , Fusco F , Carpi R , et al. Pneumatosis intestinalis in COVID-19. Case report. BMJ Open Gastroenterol. (2020) ;7: (1):e000434. |
[11] | Łaski D , Biernat K , Kaska Ł . Pneumatosis Intestinalis due to COVID-19 infection in kidney transplant recipient: A case report. Transplant Proc. (2021) ;53: (4):1215–8. |
[12] | Rousset S , Moscovici O , Lebon P , Barbet JP , Helardot P , Macé B , et al. Intestinal lesions containing coronavirus-like particles in neonatal necrotizing enterocolitis: An ultrastructural analysis. Pediatrics. (1983) ;73: (2):218–24. |
[13] | Galanopoulos M , Gkeros F , Doukatas A , Karianakis G , Pontas C , Tsoukalas N , et al. COVID-19 pandemic: Pathophysiology and manifestations from the gastrointestinal tract. World J Gastroenterol. (2020) ;26: (31):4579–88. |




