Abstracts of the 26th European Workshop on Neonatology, September 2–5, 2018, Cappadocia, Turkey
Thyroxin Threshold Linked to Impaired Outcome in Preterm Infants: A Retrospective Cohort Study
Jean Michel Hascoet1, Stephanie Coquelet1, Helene Deforge2
1Department of Neonatology, Regional Maternity, CHRU Nancy, France
2EA3450- DevAH, University of Lorraine, France
Introduction: It remains controversial whether transient hypothyroxinemia of prematurity influences short- and long-term outcomes. Thus, we aimed to define a thyroxin threshold associated with neonatal clinical impairment and outcome at 3 years of age.
Methods: We retrospectively analyzed medical records of infants born at a gestational age (GA) of < 29 weeks. A thyroxin threshold value was defined by ROC curve analysis in a cohort of infants born from 10/2008–12/2012, and validated in a second cohort of infants born from 01/2014–12/2016 in our institution.
Results: Our analysis included 460 patients (mean GA, 26.7 ± 1.3 weeks; mean birth weight, 935 ± 206 g). Thyroxin (FT4) measurements were available for 196/274 infants from the early time period, among whom 35 exhibited neonatal clinical impairment. ROC curve analysis indicated an FT4 threshold of 10 pmol/L, with a sensitivity of 85.7%, and a specificity of 49.1%. FT4 measurements were available for 176/186 infants from the second time period: neonatal clinical impairment occurred in 20/78 infants with FT4 = 10 pmol/L versus 3/98 with FT4 > 10 pmol/L (P <.001). Three-year follow-up data were available for 147/196 eligible infants. Poor outcome occurred in 65% (58/89) with FT4 = 10 pmol/L versus 34% (20/58) with FT4 > 10 pmol/L (OR, 3.555; 95% CI, 1.774–7.128; P <.001).
Conclusion: We defined and validated a FT4 threshold of 10 pmol/L as a significant risk factor for neonatal clinical impairment, and a good predictor of poor outcome at 3 years of age.
Keywords: premature infants; hypothyroxinemia; outcomes
Cardiovascular risk profile in former very preterm infants at a preschool age
Ursula Kiechl-Kohlendorfer1, Anna Posod1, Irena Odri Komazec2, Daniela Baumgartner3
1Department of Pediatrics II (Neonatology), Medical University of Innsbruck, Innsbruck, Austria
2Department of Pediatrics III (Pediatric Cardiology, Pulmonology, Allergology and Cystic Fibrosis), Medical University of Innsbruck, Innsbruck, Austria
3Department of Pediatrics, Clinical Division for Cardiology, Medical University of Graz, Graz, Austria
Introduction: Cardiovascular disease is the leading cause of death worldwide. Evidence points towards an unfavorable cardiovascular risk profile of former preterm infants in adolescence and adulthood. Aim of the study was to determine whether cardiovascular risk predictors are already present at a preschool age.
Methods: We investigated five- to seven-year-old children born with a gestational age < 32 weeks (n=76) and a control group of same-aged children born at term (n=79). Basic data were collected by means of follow-up databases and standardized questionnaires. At study visit, anthropometric data, blood pressure readings, blood samples after an overnight fast, aortic intima-media thickness and aortic elastic properties were obtained.
Results: Compared with children born at term, the preterm group showed significant differences in blood pressure readings, fasting glucose levels, homeostasis model assessment index, cholesterol levels (p<0.05, each), differences in amino acid profiles and lipid metabolism. The preterm group showed significantly reduced distensibility and increased stiffness of the descending abdominal aorta (p<0.05).
Conclusions: Clinical follow-up of preterm infants including cardiovascular parameters might be useful for tailoring early prevention programs and counteracting cardiovascular risk in adulthood.
Keywords: Cardiovascular risk, preschool age, very preterm infants
Relevance of oral glucose tolerance test (OGTT) in pregnancy and other maternal and fetal measures for discrimination between LGA infants and infants of diabetic mothers
Roland Hentschel1, Martine Thill1, Alexandra Krause2, Julia Trost1, Mirjam Kunze3, Karl Otfried Schwab2
1Dept. of General Pediatrics and Adolescent Medicine, Division of Neonatology/Intensive, Care Medicine Medical Center and Medical Faculty - University of Freiburg, Germany
2Dept. of General Pediatrics and Adolescent Medicine, Division of Endocrinology/Diabetes, Medical Center and Medical Faculty - University of Freiburg, Germany
3Dept. of Obstetrics and Gynecology, Medical Center and Medical Faculty - University of Freiburg, Germany
Introduction: Newborns may be large-for-gestational-age infants (LGA) from constitutional (ethnic) phenotype (fetal macrosomia (FM)), or as a consequences of inadequately controlled gestational diabetes mellitus (GDM) or preexisting diabetes mellitus (DM). It might be prudent to identify infants from a diabetic mother (IDM) as early as possible, because of their specific perinatal problems or the heritability of the diabetic predisposition.
Methods: Observational study on pregnant women with DM, GDM or suspected FM using fetal ultrasound, medical history, OGTT and further variables. Collection of anthropometric and metabolic data (mothers/infants). Measurement of fructosamine, IGF-1, insulin, leptin and retinol-binding-protein-4 from cord blood. Statistics: Mann-Whitney U test, Fisher’s exact test, logistic regression.
Results: 63 mother-infant dyads with GDM/DM, 17 with FM, and 47 controls (C) were enrolled. There was a good compliance with guidelines for diabetes screening in pregnancy in all 3 groups (only 9.5% of IDMs >P90). OGTT was able to discriminate between GDM and FM, or GDM and C (p<0.001). Mean of weight, length and abdominal circumference at birth was highest in FM, lower in GDM and lowest in C (p<0.001). In multiple linear regression analysis leptin and IGF-1 were both associated with birth weight (p<0.001), however, all 5 serum markers were unable to discriminate between LGA and FM.
Conclusion: High compliance with medical recommendations for GDM may lead to vanishing LGA phenotype of IDM, and biochemical parameters may be normal. Cord blood leptin and IGF-1 may be suitable to distinguish between IDMs and FM infants in a less well controlled cohort.
Keywords: infant of diabetic mother, large-for-gestational age, fructosamine, leptin, RBP4, IGF-1
4 years period analysis of newborns with Oesophageal atresia in Latvia
Renate Zarina, Alexandra Yurash
Clinic of Neonatology, University Children’s Hospital, Riga, Latvia
Introduction: Oesophageal atresia (OA) is complicated congenital anomaly what is associated with complex and long term treatment. Our objective was to describe the incidence of OA, patient characteristics and short term outcomes for patients treated in our Neonatal clinic in Latvia. METHODS: Retrospective analysis of clinical charts and case records of all neonates with diagnosed OA in Latvia, treated in University Children’s hospital during 2013-2017.
Results: We enrolled 24 neonates, 3 of them from twin pregnancy (12,5%),14 boys (58,3%), 10 girls (41,6%), 41,6% premature. Mortality - 8.3% (associated with other congenital pathologies). 23 neonates had OA with distal tracheoesophageal fistula (TEF), 1- without TEF. For 20 infants oesophagoplasty was done with primary anastomosis and ligation of TEF,4 patients had “long-gap” with delaying primary repair. Postsurgical mechanical ventilation (MV) – median time 5 days (2>51),boys needed longer MV (p<0.05),all received parenteral nutrition(PN)– average 22,7 days. Early complications included pneumothorax-10 patients, sepsis 10 cases, surgical wound infection 1. Recurrent TEF and anastomotic leaks in 7 patients (29,1%). Mean hospital stay was 42 days (16 to 120), for OA with “long-gap” - 65.25 vs 37.45 days p=0.054. Preterm neonates had longer MV (5,2 vs 16.2 days ), PN (6.75 vs 32.1 days) and also hospital stay duration (27.14 vs 63 days), p>0.05.
Conclusions: This study describes population characteristics (incidence 1:4447), management and outcomes (the most common early postoperative complications were right-sided pneumothorax and sepsis) of OA patients treated in Latvia in 4 years period. Longer hospital stay correlated with prematurity and “long-gap” OA.
Keywords: Oesophageal atresia, neonates, early postoperative complications.
High dose caffeine in very preterm infants: A systematic review and meta-analysis
Petter Brattström1, Chiara Russo2, David Ley3, Matteo Bruschettini4
1Lund University, Lund, Sweden
2Genoa University, Genoa, Italy
3Department of Pediatrics, Lund University, Lund, Sweden
4Department of Pediatrics, Lund University, Lund, Sweden; Cochrane Sweden
Introduction: Observational studies suggest that maintaining high blood concentrations of caffeine in very preterm infants is associated with improved respiratory outcomes.
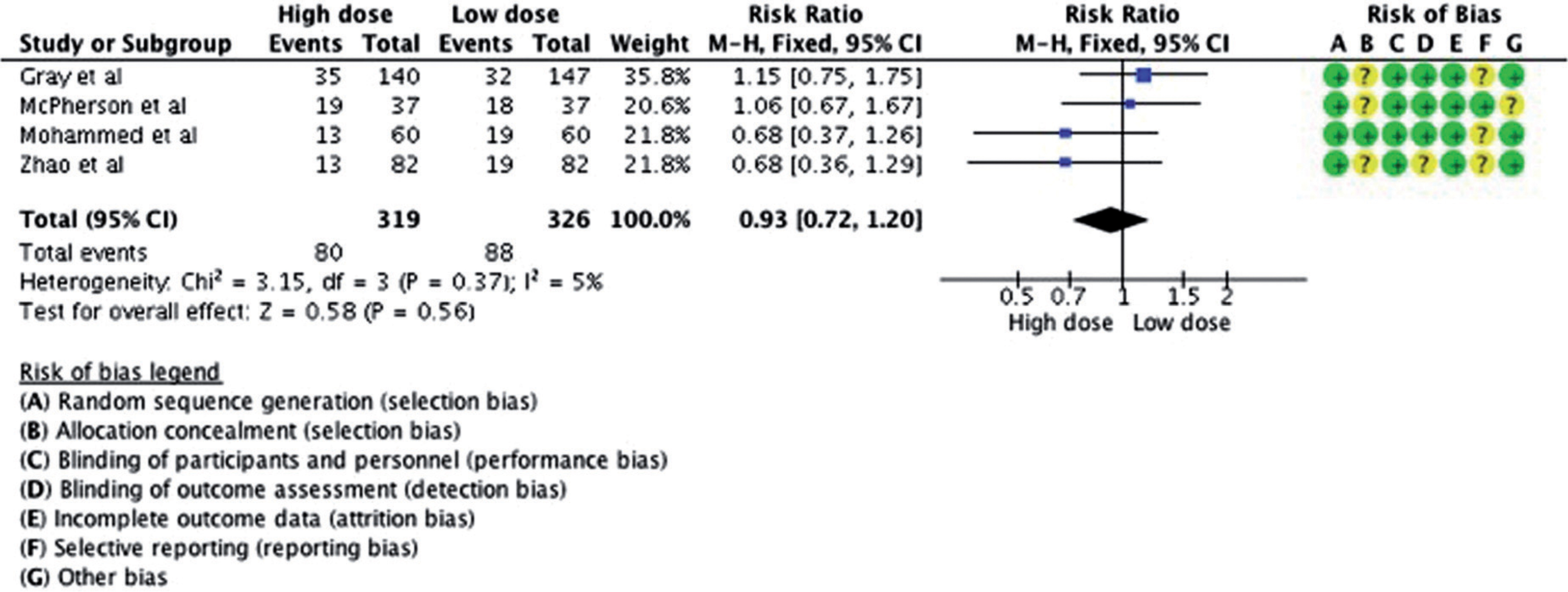
Methods: A systematic review was conducted to assess the efficacy and safety of high (loading dose >20 mg/Kg and maintenance >10 mg/Kg/day) versus low dose of caffeine. MEDLINE, EMBASE, Central, and conference proceedings for randomized controlled trials (RCTs) and quasi-RCTs were searched. A fixed-effect model was used. The quality of evidence was assessed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE).
Results: Amongst the six included trials, the loading and maintenance doses varied between 20-80 mg/kg/day and 3-20 mg/kg/day, respectively. Overall, caffeine administration was started within 3-4 days of life and lasted 25-30 days. The use of high dose had no impact on mortality (RR: 0.85; 95% CI: 0.53-1.38; studies = 4) or bronchopulmonary dysplasia (RR: 0.93; 95% CI: 0.72-1.20; studies = 4). There were fewer cases of extubation failure and apneic spells in the high dose group. The quality of the evidence was low due to imprecision of the estimates (GRADE). We identified one ongoing trial which is conducted in China (estimated completion date October 2018).
Conclusion: High dose of caffeine might improve short-term respiratory function without reducing bronchopulmonary dysplasia. However the optimal information size has not been reached. Future trials should ameliorate allocation concealment and outcome reporting.
High dose caffeine was not better than low dose for preventing bronchopulmonary dysplasia (RR: 0.93; 95 % CI: 0.72;1.20)
Acknowledgements: We thank Matthias Bank (Library and ICT-services - Lund, Sweden) for defining and running the search strategy; Cochrane Austria for providing methodological training to Petter Brattström.
Keywords: methylxanthine, dose-response, cerebral palsy, Cochrane, prevention, evidence-based medicine
Timing and Progression of Oxygen-Induced-Retinopathy by Recurrent Intermittent Hypoxia and Desaturations in a Neonatal Rat Model
Kay D. Beharry, Gloria B. Valencia, J. V. Aranda
Department of Pediatrics and Ophthalmology,State University of New York Downstate Medical Center, New York, USA 11203
Introduction: The 3rd Global Epidemic of Retinopathy of Prematurity (ROP) is underway and warrants pharmacologic and other interventions to prevent it. The exact timing of retinal damage to guide strategic interventions remains unknown. We tested the hypothesis that repeated exposures of immature retina to Intermittent Hypoxia (IH) simulating neonatal apnea-desaturations produce early retinal damage and define key time points for pharmacologic intervention.
Methods: Newborn rats were exposed to IH within 2 hours of birth (P0) until P14, or allowed to recover in room air (RA) from P14 to P21 (IHR). Retinal integrity (by retinal flatmounts stained with ADPase, fluorescein-dextran, GFAP for astrocytic template, retinal thickness) and angiogenesis biomarkers (VEGF, sVEGFR-1, IGF-1) were progressively assessed before (P0), during IH (P7, P14) and post IH recovery in RA (P21), or IH recovery-reperfusion (IHR) and compared to normoxic age-matched controls.
Results: Retinal damage occurred as early as day 3 of neonatal IH, consistent with vascular abnormalities and marked early pathology of astrocytic template which worsened during IHR. IH-group showed retinal endothelial cells penetrating the inner limiting membrane to violate the vitreous fluid as early as P1 and worsening at P3.
Conclusions: Pharmacologic and other interventions to prevent ROP should be started shortly after birth in high risk preterm neonates. Drug screening using a 3-D scaffold human retinal endothelial cell cultures may help identify effective and safe drugs for targeted clinical drug development to prevent ROP. Early intervention may prevent or decrease severity of ROP and avert a lifetime of blindness or visual impairment.
Postnatal temporal changes in thickness of retinal and nerve fi ber & ganglion cell layer in room air and Intermittent hypoxia

Keywords: Retinopathy of Prematurity, oxygen induced retinopathy, intermittent hypoxia, neonatal apnea, timing of retinal damage
Study of neonatal platelet function with PFA-100 in neonates of pregnancies complicated with intrauterine growth restriction, gestational diabetes and perinatal hypoxia
Nicoletta M Iacovidou1, Theodora Boutsikou1, Elina Isaakidou1, Vasiliki Mougiou1, Maria Kollia1, Maria Boutsikou1, Rozeta Sokou1, Serena Valsami2, Marianna Politou2
1Neonatal Department, Aretaieio Hospital, National and Kapodistrian University of Athens
2Hematology Laboratory-Blood Bank, Aretaieio Hospital, National andKapodistrian University of Athens
Introduction: PFA-100(Platelet Function Analysis) is an in-vitro test that assesses platelet-related hemostasis(aggregation and agglutination) by measuring Closure Times (CTs), which are decreased in healthy term neonates vs adults. We hypothesized that certain high-risk neonates, prone to hemostatic disorders, may present with compromised platelet function. We aimed at performing PFA-100 in offspring of pregnancies with IUGR(Intrauterine Growth restriction), Gestational Diabetes Melitus(GDM) and Perinatal Hypoxia(PH) and correlate the results withperinatal parameters.
Methods: The study comprised of 179 umbilical cord(UC) blood samples:43 IUGR, 53 GDM and 43 PH vs 40 from uncomplicated pregnancies serving as control. COLEPI and COLADP cartridges were used as platelet activators providing 2 CTs for each sample.
Results: No significant differences in COLEPI values were observed between each of the 3 groups vs controls. COLADP was significantly lower in the GDM and PH vs control(b=-3.045, CI95%-5.841-(-0.249), p=0.033 and b=-3.773, CI95%-6.033-(-1.514), p=0.001 respectively). In the IUGR group COLADP was significantly increased in female neonates and decreased in vaginally delivered neonates (b=0.53, CI95% 0.010- 0.097, p=0.018, and b=-0.58, CI95% - 0.106-(-0.011), p=0.016, respectively. The lack of difference in COLEPI between each group vs control could possibly be attributed to variable compensatory mechanisms apart from platelet function, like increased hematocrit. Platelet hyperreactivity commonly presenting in diabetes and hypoxia, could possibly explain lower COLADP in the respective groups.
Conclusion: In IUGRs, COLADP prolongation in female fetuses could be attributed to the inhibitory effect of estrogens on PLT aggregation; the COLADP decrease in vaginally delivered neonates reflects PLT activation due to documented cytokine elevation present during vaginal delivery.
Keywords: neonates, IUGR, IDM, PH, PFA-100
Clinical factors influencing endogenous carbon monoxide production in newborns
Jana Lozar Krivec, Darja Paro Panjan
Division of Paediatrics, Department of Neonatology, University Medical Centre Ljubljana, Slovenia
Introduction: COHb is an index of endogenous CO formation during heme degradation catalyzed by hemo-oxygenase-1 (HO-1). We previously reported that COHb measured with CO-oximetry could be used to confirm hemolysis in newborns with AB0 incompatibility. The influence of other clinical factors, which are reported to upregulate HO-1, on COHb in newborns, has not yet been fully investigated. We aimed to evaluate the influence of sepsis, respiratory distress and postnatal age on COHb values.
Methods: We retrospectively analyzed COHb measurements determined with CO-oximetry in term, less than 14 days old newborns, classified into 4 groups: sepsis (A), respiratory distress (B), hemolysis (C), healthy newborns (D).
Results: Overall there were 737 COHb measurements performed in newborns during two-year period. 137 fulfilled the inclusion criteria. The mean COHb values were 1.41% (SD0.26), 1.32% (SD0.27), 2.5% (SD0.69) and 1.27% (SD0.19) in groups A (n=8), B (n=37), C (n=16) and D (n=76) (p<0,0005). Post hoc analysis showed that COHb in Group C was significantly higher than in other groups, the differences in COHb between groups A, B and D were not statistically important. There was a negative correlation between postnatal age and COHb in healthy newborns. The cutoff level 1.7% had 93% (95%CI, 89-97%) sensitivity and 94% (95%CI, 90-98%) specificity for diagnosis of hemolysis.
Conclusion: COHb in newborns with sepsis and respiratory distress was higher than in healthy newborns, the differences were small and statistically insignificant. COHb in newborns with hemolysis was significantly higher. The COHb values are higher during first days of life.
Keywords: newborn, CO, carboxyhemoglobin, CO-oximetry, sepsis, respiratory distress.
Using measurements of ventilation/perfusion ratio to estimate the alveolar surface area in prematurely born infants
Theodore Dassios
Neonatal Intensive Care Centre, King’s College Hospital NHS Foundation Trust, London, UK
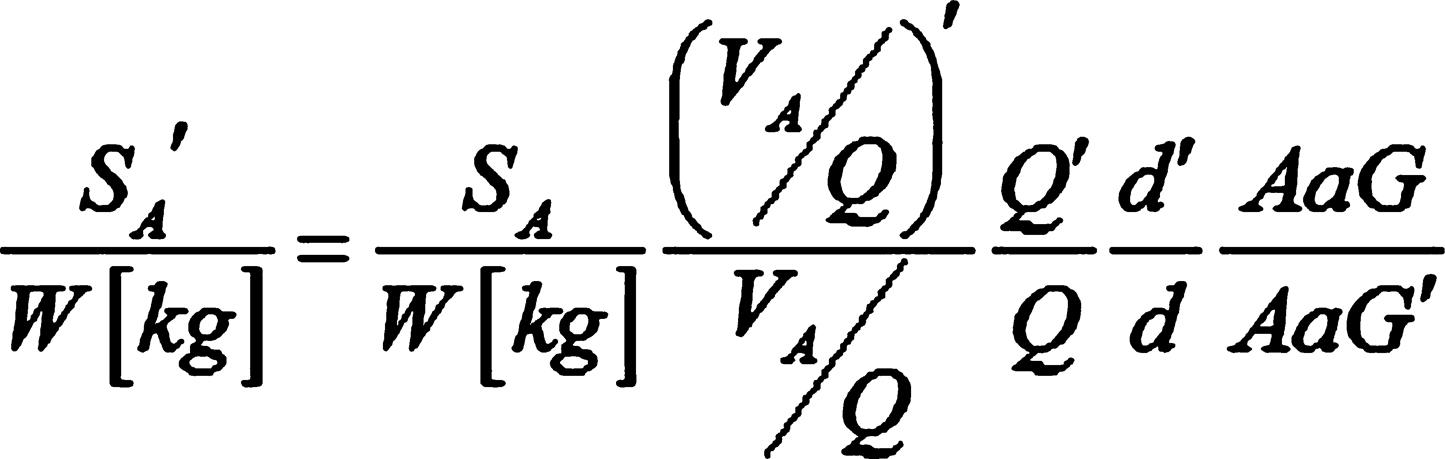
Introduction: Conventionally, the alveolar surface area (Sa) has been measured by using post-mortem morphometry. Such studies have highlighted that Sa in prematurely-born infants is markedly smaller when compared to term-born infants as a result of postnatal impairment or arrest of alveolar development. We herein explore how, non-invasive measurements of the ventilation/perfusion ratio (Va/Q) can be used to estimate Sa in prematurely-born surviving, convalescent infants. We also compare Sa in prematurely-born infants measured at term-corrected age, to term-born infants using previously published datasets of Va/Q.
Methods: Fick’s first law of diffusion is employed for the conversion of Va/Q measurements to Sa values after correcting for differences in pulmonary perfusion (Q), thickness of the respiratory membrane (d) and alveolar-arterial gradient (AaG).
Results: Using the dodecahedral structure to estimate the alveolar shape we develop a mathematical formula to correct for differences in the thickness of the respiratory membrane between term and prematurely-born infants studied at term. We correct for differences in pulmonary perfusion and alveolar-arterial gradient using previously published datasets. We present a generic equation to estimate the Sa in prematurely born infants studied at term (figure 1). Using previously published datasets we report that Sa is fivefold smaller in prematurely-born compared to term-born infants.
Conclusions: We conclude that non-invasive measurements of Va/Q can be used for the functional estimation of Sa which could, in turn, be used as a future outcome measure in respiratory studies of prematurely-born infants.
Keywords: alveolar surface area, premature infants, alveolar development
Figure 1
The equation used to estimate the Sa. Primed variables are used for prematurely born infants studied at term and unprimed symbols for term infants.
Combined use of probiotic Lactobacillus rhamnosis GG and vitamin D in very low birth weight infants
Stanislava Georgieva Hitrova Nikolova, Boryana Pertova Slancheva, Lilia Georgieva Vakrilova, Elena Petrova Shopova, Petja Angelova Radulova, Tanja Velikova Pramatarova, Nelly Georgieva Jekova, Nina Lubomirova Yarakova, Aneta Krasteva Popivanova, Zdravka Emilova Drenkova
Department of Neonatology, University Hospital of Obstetrics and Gynecology,Maichin dom’’, Faculty of Medicine, Medical University of Sofia, Bulgaria
Introduction: Probiotic supplementation can improve intestinal function in premature newborns and can be potentially beneficial to their health.
Objectives: To monitor the clinical,microbiological safety and tolerance of the probiotic Lactobacillus rhamnosisGG+D3 in VLBWinfants and evaluate their vitamin D status.
Materials: A prospective study was carried out from July 2017 to February 2018 at Neonatology Clinic,University O&G hospital“Maichin dom”.The study included 25 newborns with average gestation age 30g.w. and average birth weight 1170 gr.Levels of 25OH-D have been measured at 10thday and 8thweeks,biochemical markers of bone metabolism (calcium, phosphorus, alkaline phosphatase,parathormone) and microbiological specimens (nasal, pharyngeal, and anal)at ten-day intervals.According to the blood levels vitaminDstatuswas defined as:normal>50nmol/l,insufficiency30-50nmol/l,and deficiency<30nmol/l.The intake of probiotic started of mean 13thday in a dose of 7 drops,containing L.rhamnosusGG1.4x109CFU/d+400IU/D3.The newborns received an additional dose D3500IU to a total dose of 900IU/d.
Results: At 10th day 72%VLBW infants have normal 25OH-D levels 85,7 ± 2,5nmol/l, 16% with insufficiency35±19,3nmol/l, and 12% with deficiency21,5±7,4nmol/l.At 8thweek, normal values of 25OH-D were maintained at 84% of infants 85,1±35.5nmol/l.Vitamin D insufficiency was found in 16% of patients 43,2±4,4nmol/l.The biochemical bone markers were within normal limits.Average duration of probiotic Waia-Lactobacillus rhamnosis GG+vitamin D is 36 days.The infants showed good tolerance of enteral feeding and ascending weight curve.Asymptomatic carrier of pathogenic intestinal flora(Klebsiella pneumonie ESBL+,Enterobacter aerugenosaESBL+,E.coliESBL+)was observed after the 20thday in 48% of patients.There is lower colonization with Candida in 20%of infants at the end of the period.NEC and late neonatal sepsis have not been established.
Conclusions: The administration of a probiotic containing Lactobacillus rhamnosisGG+ vitamin D in VLBWinfants is microbiologically safe and clinically well tolerated.
Keywords: Lactobacillus rhamnosis GG,vitamin D,VLBW
Do we give sufficient amounts of vitamin D to preterm infants?
Sophie Greim, Helmut Küster
Neonatology, University Medical Center Göttingen, Germany
Introduction: Vitamin D is given to every newborn and it may have multiple benefits well beyond neonatal age. Recommended doses vary and are independent of patient’s current weight. Vitamin D3 levels can be measured but this is not standard of care and normal levels have not been agreed on.
Methods: Prospectively we measured every two weeks vitamin D3 levels in all preterm infants with alkaline phosphatase >500 U/L and adapted vitamin D supplementation to achieve a vitamin D3 level of 60 to 100 μg/L.
Results: Between January 2013 and December 2015, 194 patients had at least one vitamin D3 level measured. After exclusion of 16 patients with incomplete datasets, 178 datasets were used for analysis: mean gestational age 29±3 weeks, birth weight 1191±517 g, 55 % male, 19 % small for gestational age; 3 % had necrotizing enterocolitis, 6 % nephrocalcinosis, only one infant died having trisomy 18. Up to 2500 IE vitamin D were needed to achieve the desired vitamin D3 levels (mean 56 μg/L). A level >60 μg/L was never achieved in 57 %, 21 % had at least one value >100 μg/L. Logistic regression analysis revealed oral vitamin D supplementation to be the most important early factor of influence for Vitamin D serum level (ROC 0.75).
Conclusion: Appropriate vitamin D3 levels are not achieved in almost 2/3 of a population individually supplemented with up to 2500 IE vitamin D. Higher than currently recommended doses of vitamin D seem to be needed, especially for very preterm infants.
Keywords: Vitamin D, alkaline phosphatase, preterm infants; nutrition, NICU
Tools and toys to study neonatal clinical pharmacology
Karel Allegaert
Department of Development and Regeneration, KU Leuven and Division of Neonatology, Erasmus MC-Sophia Children’s hospitals, Rotterdam
Introduction: Neonates are not just small children. Consequently, targets or biomarkers should be explored on their relevance in neonates.
Methods: recently conducted studies on vancomycin protein binding (AUCtotal target 400, converted to trough level of 10-15 mg/l) and on the systemic and cerebral hemodynamics of propofol for endotracheal intubation will illustrate the need to fully consider the neonatal physiology and setting when assessing the targets or (side)- effects of drugs in neonates.
Results: Median total and unbound vancomycin concentrations in 37 neonatal plasma samples were 14.25 (7.42-20.62) and 13.63 (7.17-22.47) mg/L, respectively. Median unbound fraction was 0.90, higher compared to children (0.81) and adults (0.62). This means that the adult AUCtotal of 400 reflects an AUCfree of 248. When this target is converted to the newborn, the AUCtotal in neonates might be 275 (0.9 x 248) instead of the 400 target generally aimed for. In a study on PK/PD of propofol in 22 neonates, intact cerebral autoregulation during permissive hypotension in the majority of cases was observed, accompanied by decreased cerebral metabolism. However, some cases displayed impaired autoregulation, despite the absence of systemic hypotension.
Conclusions: Integration of protein binding in future pharmacokinetic/pharmacodynamics (PK/PD) analyses is needed to determine population-specific vancomycin PD targets for neonates, while simultaneous collection of data on systemic and cerebral hemodynamics confirm that systemic hemodynamics do not fully reflect the cerebral hemodynamics. We hereby illustrated the need to fully consider the neonatal PK/PD when assessing the targets or (side)- effects of drugs in neonates.
Keywords:Tools, toys, clinical pharmacology
Determination of fetal age and date of delivery
Dag Bratlid
Department of Health Administration and Health Economics, Institute of Health and Society, Faculty of Medicine, University of Oslo, Norway
Introduction: Ultrasound (US) has gained a dominating position for determination of fetal age and expected date of delivery (EDD). Determination of fetal age by US has, however, significant flaws (1,2) as illustrated by the following pregnancy history (3). Patient FAL had a regular menstrual history. From biological parameters last menstrual period; positive ovulation test; date of conception; and missed next period, EDDb was 14.2.2017. EDDus from biparietal diameter (BPD), crown-rump length (CRL), and femur length (FL), varied from 28.2, 25.2 and 20.2, respectively. History Despite significant discrepancies between EDDb and EDDus, as pointed out by the parents, EDD was set at 28.2 based on BPD measurements according to advocated routines. At follow-ups on 20.1. and 3.2.2017, breech position was detected, and LAF was scheduled for turning of the fetus on February 6. However, on February 4, membranes ruptured and delivery was imminent. CT showed pelvis measurements too small for breech delivery, and c-section was performed. The girl weighed 3160 gram, head circumference 36 cm and length 46 cm. Due to medical complications after c-section, postnatal stay was 11 days
Discussion: Fetal US like BPD, CRL and FL results in different EDDus and also have large variations from mean. These technologies are therefore not better than a “correct” EDDb.
Conclusions: Negligence of EDDb can be harmful for mother and infant. If EDDb had been considered, breech position could have been corrected and c-section avoided with a better start for mother and infant.
Bratlid D Determination of birth term by early ultrasonic examination--wrong, wrong and wrong again?. Tidsskr Nor Laegeforen. 1991:111:1379-81.
Bratlid D Estimating date of delivery and gestational age - technology, biology or both? Tidsskr Nor Legeforen 2016; 136:1332.
Keywords: fetal age, date of delivery
Breast milk: to each his own. From nature the evidence of personalized nutrition.
Serafina Perrone1, Mariangela Longini1, Federica Lotti1, Fabrizio Proietti1, Francesco Bazzini1, Maria Tassini2, Antonio Vivi2, Serena Rossi1, Marco Calderisi3, Giuseppe Buonocore1
1Department of Molecular and Developmental Medicine, University of Siena, Siena, Italy
2NMR Center, University of Siena, Siena, Italy
3Kode-solutions, Pisa, Italy
Introduction: Human milk is the best nourishment for the healthy growth and development of infants. The composition of preterm milk is pretty different from the full term milk. The aim of this study is to test the hypothesis that milk metabolic profile from mothers delivering prematurely changes over time never resembling milk from mothers delivering at term.
Methods-results:. 12 term milk samples, collected once at 7 days after birth, were compared to 18 preterm milk samples, collected weekly after delivery until the 4th week after birth. Metabolome pattern of all milk samples was analyzed. Principal Component Analysis (PCA) showed two distinct metabolites groups, one represented by the 18 preterm milk samples, and the other by the term milk samples (Fig 1). Lactose and oligosaccharides levels were significantly more represented in preterm than in milk term samples.
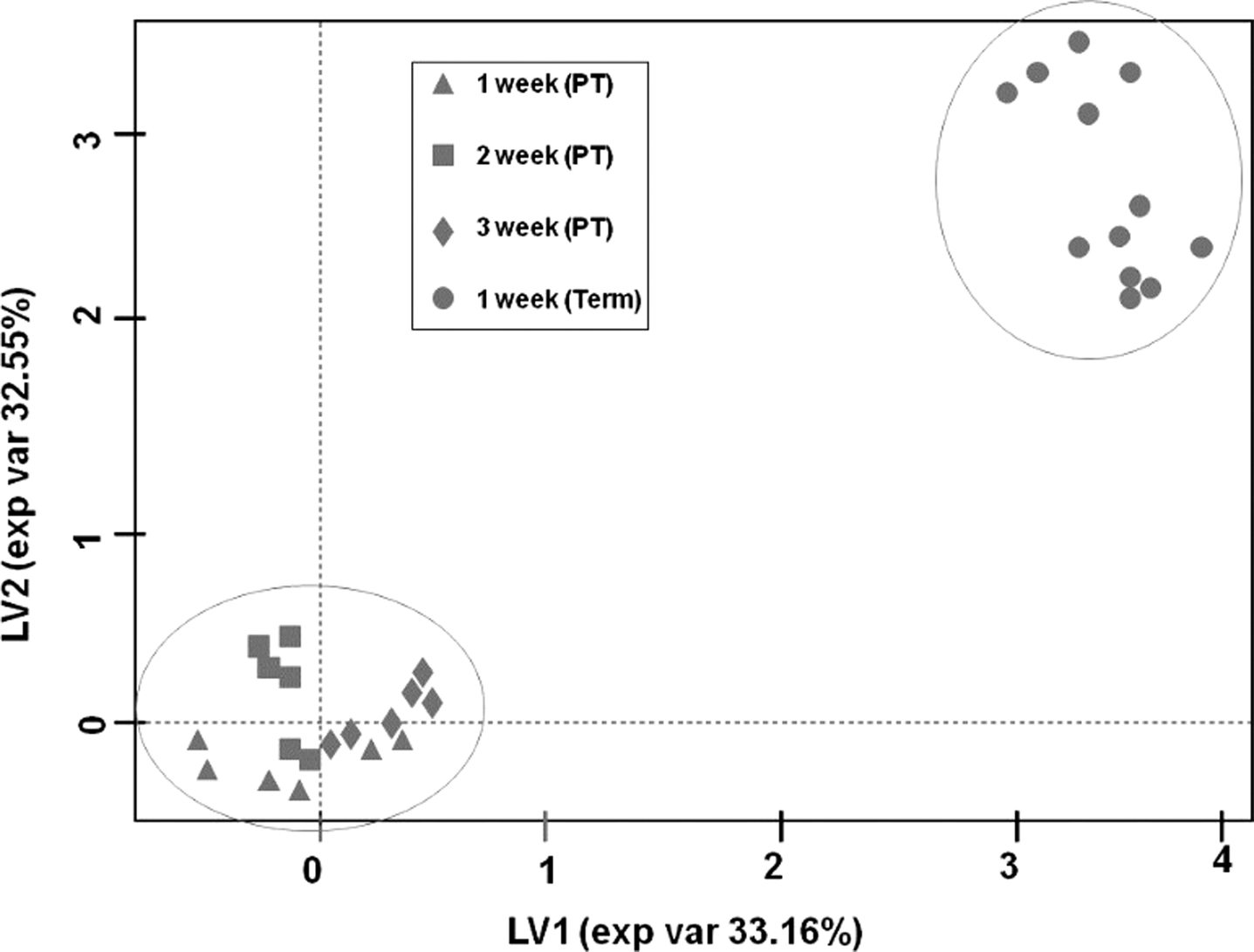
Conclusions: Preterm milk metabolome profile changes during the first 4 weeks after birth, but does not resemble the term milk pattern. The specific changes in preterm milk metabolic profile reflect the different nutritional requirement of preterm infants. This knowledge is crucial to move from standardized nutritional protocols to a tailored nutrition.
Keywords: Preterm milk
Increased plasma concentrations of NPBI in cord blood predict IVH in preterm newborns.
Serafina Perrone, Antonino Santacroce, Maria Luisa Tataranno, Simona Negro, Mariangela Longini, Fabrizio Proietti, Francesco Bazzini, Anna Picardi, Giuseppe Buonocore
Department of Pediatrics, Obstetrics and Reproductive Medicine, University of Siena, Italy.
Introduction: Intraventricular hemorrhage (IVH) predispose to long-term neurologic disability in preterm infants. Oxidative stress (OS) is a major risk factor in the pathogenesis of IVH. Non-protein bound iron (NPBI), a reliable markers of OS, was reported to be related to poor neurodevelopmental outcome. We test the hypothesis that NPBI concentrations in cord blood may predict IVH development in preterm infants.
Methods: NPBI was measured in arterial cord blood of 221 preterm newborns (GA = 32 weeks). According to the cerebral ultrasonography findings during the first 48 hours of life, the population was divided in IVH group (n=80) and non-IVH group (n=141). SPSS package was use for statistical analysis.
Results: IVH group had a lower GA (28.58±2.12 VS 29.6±2.02; p<0.001) and higher cord blood levels of NPBI (2.81±5.6 VS 1.23±2.37; p=0.006) than the non-IVH group. A binomial logistic regression analysis showed the significant relationship between NPBI and IVH (B=1.112, CI 95% 1.014-1.219; p=0.024). GA was protective against IVH onset (B=0.802, CI 95% 0.699-0.921; p=0.002).
Conclusion: Cord blood NPBI concentrations are increased in preterm newborns who develop IVH and may be useful for the identification of the risk for IVH before the appearance of related biophysical signs. Data also suggest the need of investigation about antioxidant strategies in perinatal period.
Keywords: plasma concentrations, NPBI, IVH
Early detection of developmental dysplasia of hip by ultrasound
Zita Gyurkovits1, G. Sohár2, A. Baricsa2, G. Németh1, H. Orvos1, B. Dubs1
1Department of Obstetrics and Gynaecology, University of Szeged, Hungary
2Department of Orthopaedics, University of Szeged, Hungary
Introduction: The aim of the study was to assess the effectiveness of early universal ultrasound screening of developmental dysplasia of the hip performed in the first days of life.
Methods: A prospective study of universal hip screening and treatment of all mature neonates was conducted during a one-year period at the Department of Obstetrics and Gynaecology, University of Szeged; 1636 newborns (3272 hips) had clinical examinations and sonographic tests with the Graf-technique, within the first three days of life. The incidence of DDH, risk factors, sensitivity and specificity of clinical examinations of the universal screening model were evaluated.
Results: At the first US examination 55 of 1636 newborns (3.36%) had either unilateral or bilateral hip dysplasia; in terms of hips 2.14% were positive. All newborns had physical examination: 67 of 3272 hips (2.05%) were Barlow or Ortolani positive, but among 67 hips, 14 (20.8%) were US positive, the remaining (79.2%) were declared negative according to the standard method of US. Taking into consideration the risk factors, female gender, breech presentation and positive family history proved to be significant. Interestingly, of the 55 newborns with DDH, 28 (50.90%) had neither positive physical signs nor any risk factors, except being a girl.
Conclusion: Universal US screening of the hip in the first days of life reduced the need of operative procedures remarkably, compared to the previously applied selective protocol. Physical examination proved to have low sensitivity.
Keywords: Developmental dysplasia of the hip, neonatal screening, ultrasonography
Antenatal factors and cognitive development at school age in very preterm children: results from the Italian ACTION area-based cohort
Marina Cuttini, Lena Herich, Ileana Croci, Action Study Group
Pediatric Hospital Bambino Gesù, Rome, Italy
Introduction: Survival of very preterm (VP) infants has improved in the last decades but disability rates are still high, particularly below 28 weeks of gestational age (GA).
Methods: We assessed health and cognitive development at school-age (8-11 years) in a prospective area-based cohort of VP children (GA <32 weeks) in three Italian regions (Lazio, Tuscany and Friuli Venezia-Giulia). Cognition (Mental Processing Index, MPI) was measured using the Kaufmann-ABC, second edition. A total of 804 children were recruited (response rate 70.4%). We used multilevel multivariable Poisson regression to explore the relation between antenatal factors and below average MPI (<85). Region was included in the model as random effect.
Results: Cognition was assessed in 730 children; 140 (20.4%) had MPI<85. Rates were higher (27%) for those born below 28 weeks of gestational age (GA). Other variables significantly associated with below average MPI in multivariable analysis were male gender, possibly homozygous multiple birth, intrauterine growth retardation, presence of congenital anomalies, signs of prenatal infection, smoking in pregnancy and younger (<24 years) maternal age. Higher maternal education appeared protective.
Conclusions: Several biological, medical and socio-demographic antenatal factors may influence long-term cognitive development in very preterm infants. Further analyses will be necessary to assess the role of postnatal variables in the causal chain leading to long-term cognitive outcome.
Keywords: Antenatal factors, cognitive development
Effect of angiotensin converting enzyme gene polymorphism on respiratory muscle function and exercise capacity in childhood: preliminary results
G. Dimitriou, A. Vervenioti, S. Fouzas
Neonatal Intensive Care Unit, Department of Paediatrics, University Hospital of Patras, Greece
Background: It has been suggested that the I-allele of Angiotensin Converting Enzyme (ACE) gene is associated with superior exercise endurance in adults. We have previously shown that the I/I ACE genotype is also associated with increased respiratory muscles (RM) effectiveness in neonates. In this study, the relationship between ACE gene polymorphism, RM function, and exercise capacity in childhood has been investigated.
Methods: Twenty one children born at a mean gestational age (GA) of 35.6 weeks underwent RM function measurements and cardiopulmonary exercise testing at the age of 6 to 7 years. The pressure-time index of RM (PTimus) was calculated by the formula (Pimean/ Pimax) x (Ti/Ttot), where Pimean and Pimax are the mean and maximal inspiratory pressure, respectively, and Ti/Ttot is the respiratory duty cycle. Exercise capacity was assessed by means of maximum oxygen consumption (VO2max) using a cycle-ergometer protocol. ACE genotyping was performed using DNA from peripheral blood. None of the participants had a history of current asthma.
Results: Children with I/I genotype (N=3) had lower PTimus and higher VO2max compared to those with I/D or D/D genotype (N=18) (PTImus 0.063 ±0.006 vs. 0.096 ±0.017, P=0.005; VO2max 51 ±6 ml/kg/min vs. 33.4 ±6 ml/kg/min, P<0.001). In a stepwise multivariable regression model, the I/I genotype was the only significant determinant of both PTImus (coefficient 0.557; P=0.004) and VO2max (coefficient 0.734; P<0.001), independently of the effect of GA, sex, BMI and lung function at school age.
Conclusions: ACE gene polymorphism influences the RM function and determines the exercise capacity in childhood.
Keywords: ACE, gene polymorphism
Use of specialist health services and costs during the first two years of life in Estonian cohorts of very preterm infants
Liis Toome1, Anna Veera Seppänen2, Raul Allan Kiivet3, Helle Visk3, Heili Varendi4
1Clinic of Pediatrics, Tallinn Children’s Hospital, Tallinn, Estonia; Department of Pediatrics, Institute of Clinical Medicine, University of Tartu, Tartu, Estonia
2Obstetrical, Perinatal and Pediatric Epidemiology Research Team (Epopé), INSERM U1153, Paris, France
3Department of Public Health, Institute of Family Medicine and Public Health, University of Tartu, Tartu, Estonia
4Children’s Clinic of Tartu University Hospital, Tartu, Estonia; Department of Pediatrics, Institute of Clinical Medicine, University of Tartu, Tartu, Estonia
Introduction: Very preterm infants (VPI) require more health services than term infants in their childhood because of the health and neurodevelopmental risks associated with prematurity. No evidence-based guidelines exist on use of the specialists to follow up VPI. However, these services might have an impact on the health care quality and costs. The aim of the study was to describe medical specialist service use by VPI in Estonia after the introduction of national follow-up guidelines and the influence of systematic follow-up on the health care costs until two years of age.
Methods: Data on medical specialist use come from the EPICE cohort of births before 32 gestational weeks in 11 European countries. In Estonia, data for 138 VPI (98% of survivors at discharge) were collected through the parent questionnaire at two years of corrected age. Health service costs during the first two years of life were derived from the Estonian Health Insurance Fund for 2002–2003, 2007–2008 and 2011–2012.
Results: National follow-up guidelines for VPI were introduced in 2008. Of VPI born in 2011–2012, all were followed up by a pediatrician, 99% by an ophthalmologist, 96% by a physiotherapist and 42% by a developmental psychologist. The total health care costs did not increase over time from 2002–2003 to 2011–2012. Furthermore, rehospitalisations during the first year of life decreased significantly between cohorts (66%, 54%, 40%).
Conclusions: The Estonian experience shows that the systematic follow-up of VPI might decrease the rehospitalisation and not necessarily increase the costs.
Keywords: Very preterm infants, specialist health services, follow-up, health service costs
Improvement of the 5-year outcome of live births with extremely low birth weight (<1000 g) in Estonia
Heili Varendi1,3, Mairi Männamaa1,3, Krislin Lee2, Ülle Utsal1, Liis Toome2,3
1Children’s Clinic of Tartu University Hospital, Tartu, Estonia
2Clinic of Pediatrics, Tallinn Children’s Hospital, Tallinn, Estonia
3Department of Pediatrics, Institute of Clinical Medicine, University of Tartu, Tartu, Estonia
Introduction: Survival of very preterm infants (22+0–31+6 gestational weeks, GW) has increased from 78% in 2002–03 to 92% in 2011–2012 in Estonia that can bring along neurodevelopmental impairment (NDI) and health problems in survivors due to extreme prematurity. We assessed the 5-year unfavourable outcome of the national cohorts of children born alive with birth weight (BW) <1000 g and gestational age 22+0–28+6 GW in Estonia between 2002–2012.
Methods: At 5 years, child development and health of Estonian national cohorts born in 2002–2003, 2007 and 2011–12 (EPICE study) was assessed using Kaufman ABC or WPPSI-IV; Movement ABC tests, or by interviewing the parents (SHIPS study) with follow-up rate as 100%. The severe NDI (cerebral palsy without walking with aids, deafness, blindness or mental development below -3 SD) and death were considered as unfavourable outcome.
Results: Five-year survival of extremely low birth weight infants born before <29GW has increased from 42.5% to 80 % in Estonia within the 10-year study period. Unfavourable outcome of live births at 5 years has decreased from 62.5% to 20% (p < 0.05). Among survivors from the last period, EPICE study group, there were no children with severe NDI but boys performed in all domains of assessed developmental skills with significantly lower scores than girls.
Conclusion: The outcome of Estonian national cohorts of live-born infants with BW <1000 g and <29GW, has improved within 2002–2012 with no severe NDI at 5 years of age in the last cohort.
Keywords: extremely low birth weight, extreme prematurity, survival, outcome, development, neurodevelopmental impairment
Reference values of cranial volume – Chance to monitor postnatal head growth in preterm infants
Marjin J. Vermeulen1, Dimitrios Konstantelos2, Sascha Ifflaender2, Jorine A. Roelants1, Jürgen Dinger2, Mario Rüdiger2, Wolfram Burkhardt2
1Department of Neonatology and Pediatric Intensive Care Medicine, Clinic for Pediatrics, Medizinische Fakultät der Technischen Universität Dresden
2Erasmus MC, University Medical Center Rotterdam, Netherlands
Introduction: Neurodevelopment of preterm infants depends on postnatal brain growth, which is commonly estimated by head circumference (HC). However, HC poorly correlates to cranial volume (CrV).1 3D-Scanners represent a non-invasive and easy method to measure CrV. This study aimed to generate percentiles and reference charts for cranial volumes for postnatal brain growth monitoring in preterm infants.
Methods: CrV was measured using 3D-Laserscaner (STARScanner, Orthomerica, Orlando, FL, USA)1 within the first 5 days of life in all infants born in our institution, measured between 34-43 weeks post-conceptionally. Newborns were excluded in case of intensive care treatment, congenital (skull) malformations or cerebral injury. CrV-percentiles were calculated by gestational age (GA), by birth weight (BW) and by HC for the total group and boys and girls separately.
Results: A total of 1893 newborns (49% female) were studied. Median GA was 39.4 [IQR 38.3-40.4] weeks, BW 3310 [2898-3650] g, HC 35.0 [34.0-36.0] cm, length 51.0 [49.0-52.0] cm. Median CrV was 423 [383-457] cm3 and was lower for girls than for boys (mean difference 26.4 cm3, p<0.001 adjusted for gestational age). Median cranial volume increased from 307 [286-331] at 34 weeks to 433.5 [406-462] cm3 at 40 weeks, with growth decreasing from 18 cm3/week at 34 weeks to 13 cm3/week at 40 weeks.
Conclusion: This study presents the first percentiles of normal CrV in newborns born between 34 to 42 weeks of gestation. The provided cranial volume reference charts can be used to monitor head growth in late preterm infants.
1 Ifflaender et.al.: PLoSOne2013:8;8(4)
Keywords: Brain Growth, Cranial Volume, Percentiles
Early versus conservative treatment: Preliminary data of the national registry on treatment option and its timing in patent ductus arteriosus
Ömer Erdeve1, Emel Okulu1, Begum Atasay1, Saadet Arsan1, On Behalf Of Interpda Study Group2
1Division of Neonatology, Department of Pediatrics, Ankara University School of Medicine, Ankara, Turkey
2INTERPDA Trial Group, Turkey
Introduction: Regarding to the management of patent ductus arteriosus (PDA) in preterm infants, no consensus on which PDA to treat, when to treat, or how to treat has been reached. A prospective, multicenter (22 units) trial has been conducted to compare the effects of conservative approach and early medical treatment options on ductal closure, surgical ligation, prematurity related morbidities and mortality in Turkey.
Methods: Infants with 24 0/7-28 6/7 gestation weeks were enrolled and their PDA management data were recorded through an online registry system.
Results: Among 497 enrolled infants (with mean gestational age of 26.8±1.3 wk and mean birthweight of 926±232 g), 31% (n=155) had no PDA, whereas 19% (n=94) had small PDA and 50% (n=248) had moderate-to-large PDA. 31% (n=107) of infants with PDA were managed conservatively in contrast to 69% (n=235) who received treatment at a mean age of 4.6±4.4 days. Prefered treatment options were ibuprofen (oral;36%, iv; 35%) and paracetamol (iv;23%, oral;6%). 23% (n=25) of conservatively managed infants required rescue treatment during the hospitalization. The rates of sepsis, necrotizing enterocolitis, retinopathy of prematurity, bronchopulmonary dysplasia and the length of hospitalization were similar between conservatively managed and treated infants (p>0.05), and no difference with treatment drugs were observed. Infants who were medically treated had higher surgical ligation (p=0.029) and home oxygen treatment (p=0.002) rates, whereas conservatively managed infants had a higher mortality rate (p=0.000).
Conclusion: Early medical treatment of PDA could not decrease the rate of surgical ligation but mortality was higher in conservatively managed infants.
Keywords: conservative; ibuprofen; paracetamol; patent ductus arteriosus; preterm.
Early postnatal care and gender impacts infant vaccination status in rural India
Sebastian Horn1, Mareike Schön1, Cara Ebert2, Esther Heesemann2, Sebastian Vollmer2
1Department of Pediatric Cardiology, Neonatology and Intensive Care, University Hospital Medical Center, Georg-August-University Göttingen, Göttingen, Germany
2Center for Modern Indian Studies, Georg-August-University Göttingen, Göttingen, Germany
Introduction: Despite recent advances in reducing newborn and infant mortality up to 40% of all newborn in low- and middle-income countries are at risk of dying within the first month of life or encounter a faltered early childhood development. Providing access to effective newborn care and early postnatal measures is known to improve the odds for a healthy development.
Methods: Questionnaire-based surveys have been conducted as well as sampling of anthropometric and early childhood development data of about 2000 families in 2016 and 2017 in Madhepura district, state of Bihar, India. Data sampling was performed with help of local enumerators using electronic data acquisition with CSPro®. Data analysis was performed using R® and Stata® software packages.
Results: Across all holders of vaccination cards completeness of vaccination status for newborn and infants at various time points was assessed. An incomplete vaccination status can be seen as a proxy for an increased risk for infection and poor development. Although vaccination within 24 hours seems equally performed gender wise with an OR (odds ratio) of 1.023 (1=male, 0=female, n=931, p=0.883) at the age of 31/2 months female infants tend to have a less complete vaccination status with an OR of 1.379 (n=931, p=0.019). Vaccination schemes are varying along national board recommendations hence we assessed vaccination completeness according to the National Swedish Vaccination Scheme.
Conclusion: Given the impact of a simple public health measure like vaccination it seems imperative to be aware of gender driven biases which will lead to defective health and development.
Keywords: early childhood development, vaccination, postnatal care, infant health, gender
Hydrocortisone (hc): efficacy and outcome at 18-22 months in ventilated infants < 28 weeks ga.
K A Nguyen, J. Bartholomew, A. Papageorgiou
Jewish General Hospital, McGill University, Department of Neonatology, Montreal, Quebec, Canada.
Introduction: HC has shown promising results in the prevention of BPD. However, the long term outcome is still under investigation.
Methods: We report response in 138 ventilated infants <28 weeks GA treated in our NICU. We also report follow-up at 18-22 months of 45 infants who received HC to 93 infants who did not receive HC. The total amount of HC that each infant received was 45 mg/Kg, with the exception of those who received a second course, making a group average of 57.02 mg/Kg.
Results: FIO2 requirements and mean airway pressure leading to extubation were dramatically improved, while BP and blood sugar remained normal. The Bayley III scores at 18-22 months indicated no difference between the 45 infants treated with HC and the 93 infants who were not treated with HC in cognition 94.9 vs 96.3, language 87.3 vs 89.3, motor scores 93.3 vs 97.0, hearing 2,2 vs 0.00, cerebral palsy 4.4 vs 2.2, and ROP 0 vs 0.
Conclusion: Based on our protocol, treatment with HC had no impact on neurodevelopmental outcome at 18-22 months on ventilated preterm infants compared to those non treated, while a significant improvement was noted on their respiratory parameters in the NICU. Our next evaluation will be done at 4½ years of age.
Keywords: hydrocortisone, BPD, Bayley III scores
Comparison of three different non-invasive ventilation modes in preterm infants with respiratory distress syndrome: prospective randomized study
Merih Cetinkaya1, Burcu Cebeci2, Seda Yilmaz Semerci1, Dilek Kurnaz1, Özge Saglam1
1Health Sciences University, Kanuni Sultan Suleyman Training and Research Hospital, Department of Neonatology, Istanbul, Turkey
2Health Sciences University, Haseki Training and Research Hospital, Department of Neonatology, Istanbul, Turkey
Introduction: Non-invasive respiratory support has been increasingly used for early management of respiratory distress syndrome (RDS) as an alternative for intubation and mechanical ventilation. The aim of this study was to compare the effects of nasal intermittent positive pressure ventilation (NIPPV), nasal continuous positive pressure (nCPAP) and high flow nasal canula (HFNC) for initial treatment of RDS in preterm infants.
Methods: Preterm infants admitted to NICU with RDS were randomized into: NIPPV vs. nCPAP vs. HFNC. The primary outcome was the need of intubation within 72 hours of life. The secondary outcomes were duration of respiratory support, duration of total oxygen, death, air leaks, and frequency of neonatal morbidities including bronchopulmonary dysplasia (BPD), retinopathy of prematurity (ROP), intraventricular hemorrhage (IVH), patent ductus arteriosus (PDA), necrotizing enterocolitis (NEC) and sepsis.
Results: A total of 60 infants were randomized to NIPPV, nCPAP and HFNC. All groups were similar with respect to demographical features. No significant differences were detected between 3 groups in terms of the need for intubation within the first 72 hours of life, the incidences of BPD, ROP, IVH, NEC, sepsis, and air leaks. The duration of respiratory support was significantly higher in HFNC group compared with other groups (p=0.002).
Conclusion: Although NIPPV, NCPAP and HFNC showed similar efficacy for prevention of intubation, HFNC group had higher duration of ventilation peiod that may limit its usage. Therefore, we suggest that NIPPV and NCPAP may be preferred as initial respiratory support modes in preterm infants to shorten the duration of ventilation.
Keywords: non-invasive ventilation, nasal CPAP, nasal IPPV, high flow nasal cannula, RDS, preterm infant
Reducing preventable harm: attitudes towards patient safety in an irish tertiary neonatal unit
David Corcoran1, Liam Dwyer2, Aishling Smith3, Colm Breathnach3
1Trinity College Dublin
2Royal College of Surgeons in Ireland
3Rotunda Hospital Dublin
Introduction & Aims: Crew Resource management is widely used in aviation and is proven to be effective in reducing accidents. There is little published research investigating interventions to improve safety culture in neonatal units. This study aimed to explore the safety culture that exists within a level III Irish neonatal unit in order to identify areas for potential improvement.
Methods: This was a quantitative, cross-sectional study performed in the Rotunda Hospital, Dublin. A 30-item safety attitudes questionnaire (SAQ) was utilizedto analyze staff perceptions in areas including job satisfaction, working conditions and stress recognition. The scores were transformed into a numerical 100-point scale (Positive score >75).
Results: The ‘Stress Recognition’ domain received the highest score (75.3) followed by ‘Job Satisfaction’ domain with a mean score of 74.4. The lowest mean scale score in the neonatal unit was for ‘Perceptions of Management’, with a mean score of 50.7.Collaboration and Communication scores were high across all disciplines.
Conclusion: This SAQ has highlighted a number of important areas for quality improvement and staff satisfaction in our neonatal unit.
Keywords: patient safety, attitudes, survey, neonatal intensive care
Blood Glucose Fluctuations in Preterms After Reaching Full Enteral Nutrition
Meltem Aksu, Ebru Ergenekon, Ebru Özcan, Ibrahim Hirfanoglu, Canan Turkyilmaz, Yildiz Atalay, Esra Onal, Esin Koç
Division of Newborn Medicine, Gazi University, Ankara, Turkey
Introduction: Blood glucose homeostazis is only reached after the first few days of life in the preterm newborn. It is usually assumed that preterms have stable glucose levels within normal limits once they are on full enteral feeds. The aim of this study is to investigate whether this is true by measuring blood glucose at fasting and after feeding.
Methods: Preterms born = 32 weeks gestation were included after reaching full enteral feeding volume of 180ml/kg with fortified breast milk given at 3 hourly intervals. Blood glucose was measured with glucosticks before feeding and 1 hour after feeding at 3 occasions each. Normal blood sugar levels were accepted as between 70-120 mg/dl and low and high levels were defined based on these values.
Results: Eighteen preterms were included with median BW: 1192 g (630-1930 g) and gestational age 31 weeks (26-32 weeks). Full enteral nutrition was reached at median 12 days and 32 weeks gestation. Total of 62 fasting and 62 postprandial glucose measurements were made. During fasting, hypoglycemia was observed in 13 % and hyperglycemia was observed in 3 % of measurements. Postprandially hypoglycemia was observed in 8 % and hyperglycemia was observed in 22.5 % of measurements.
Discussion: This is a pilot study investigating the glucose homeostazis in preterms who are on full enteral feeds. Even in this small group hypo and hyperglycemia has been observed frequently both during fasting and postprandial periods. More studies performed with larger groups are needed.
Keywords: Enteral nutrition, hyperglycemia, hypoglycemia, preterm
Neonatal consequences of non-diabetic hyperglycemia during pregnancy
A. Kazancioglu1, E. Koc1, P. Calis2, M. Bayram2, I. M. Hirfanoglu1, E. Onal1, C. Turkyilmaz1, E. Ergenekon1
1Gazi University, Division of Neonatology, Ankara,Turkey.
2Gazi University, Department of Obstetric and Gynecology, Ankara,Turkey.
Introduction: It is controversial whether maternal hyperglycemia less severe than that in diabetes mellitus is associated with increased risks of adverse pregnancy outcomes. The aim of the study is to assess adverse outcomes of infants of mothers whose glucose intolerance are less severe than overt diabetes mellitus.
Methods: A total of 205 pregnant women underwent 75 gr oral glucose tolerance testing between 24-28. gestational weeks were enrolled. Infants of mothers with fasting glucose levels below 92 mg/dl, 1-h glucose levels below 180 mg/dl and 2-h glucose levels below 153 mg/dl were evaluated prospectively. Primary outcomes were birth weight above the 90th percentile for gestational age (LGA), primary cesarean delivery, hypoglycemia. Secondary outcomes were delivery before 37 weeks of gestation, birth injury and hyperbilirubinemia,
Results: The mean fasting, 1-hour, and 2-hour plasma glucose levels were 76 ± 7.2 mg/dl, 116±27.3 mg/dl, and 99±21.3 mg/dl respectively. LGA and primary ceserean delivery rates are significantly associated only with 1-h blood glucose values (p:0.002, p:0.019). Blood glucose levels of the mothers were not associated with hypoglycemia and hyperbilirubinemia (p> 0.05).
Conclusion: Our results indicate a significant association of maternal glucose levels below those diagnostic of diabetes with increased birth weight and cesarean delivery.
Keywords: hyperglycemia, pregnancy, newborn
Urinary Iodine Concentrations and Serum TSH, FT4 Levels in Neonates and Their Mothers in a Mild-Deficiency Area
Gozde Apaydin1, Mehmet Vural2, Olcay Evliyaoglu3, Fatih Aydin4, Canan Kucukgergin4, Tugberk Bakar5, Yildiz Perk2
1Istanbul University, Cerrahpasa Medical Faculty, Department of Pediatrics, Istanbul
2Istanbul University, Cerrahpasa Medical Faculty, Department of Pediatrics, Division of Neonatology, Istanbul
3Istanbul University, Cerrahpasa Medical Faculty, Department of Pediatrics, Division of Pediatric Endocrinology, Istanbul
4Istanbul University, Istanbul Medical Faculty, Department of Biochemistry, Istanbul
5Istanbul University, Cerrahpasa Medical Faculty, Department of Public Health, Istanbul
Background: Iodine is an essential element in thyroid hormone synthesis and normal development of neurological system. Urinary iodine concentration, serum TSH and FT4 levels can be appropirate indicators of body iodine status. Aim of the study: The aim of this study was to determine the urinary iodine concentrations, serum TSH and FT4 levels in neonates and their mothers to assess the nutritional iodine: status.
Method: A cross-sectional voluntary screening study was performed in Neonatology Unit in Cerrahpasa University Hospital. We collected serum samples and spot urine samples from 102 neonates and their mothers. Urinary iodine concentration (UIC) was calculated based on Sandell-Kolthoff reaction. Median urinary iodine level <100 μg/L was considered as iodine deficiency.
Results: The median urinary iodine concentrations in neonates and their mothers were 102,61 μg/L and 84,07 μg/L respectively. 41% of neonates and 49% of mothers had insufficient (<100 μg/L) urinary iodine concentration (UIC). The median levels of serum TSH and FT4 for neonates and their mothers were 12,31 mIU/L, 2,41 pg/dl; 2,26 mIU/L, 1,08 pg/dl respectively. 28% of neonates and 2% of mothers had increased serum TSH levels.
Conclusion: Iodine deficiency with low urinary iodine concentrations and high serum TSH levels was recognized among neonates and their mothers in Cerrahpasa, Istanbul in spite of the programme of salt iodization. This study suggests that national measures are required to correct iodine sufficiency with regular iodine supplementation during the pregnancy in this region.
Keywords: Urinary Iodine, Mild-Deficiency Area, TSH, FT4




