The Impact of a Mental Health Game (eQuoo) on the Resilience of Young Adults: A Case Series Study
Abstract
Background:
mHealth apps are showing promise as an accessible means to improve mental health and wellbeing. However, there is limited evidence for their efficacy, particularly in periods after their initial usage, and in non-Western cultures.
Objective:
In this study, we explored the impact of eQuoo, an emotional fitness application which gamifies self-reflection and learning, in terms of its ability to build resilience in a sample of young people in Vietnam.
Materials and Methods:
Individuals (n = 264, M = 25.65 years, SD = 4.84; 52% female) completed self-reports consisting of three different measures of resilience (the Rugged Resilience Measure, Adult Resilience Measure, Brief Resilience Scale). Assessments were taken at the start and end of a five-week use period, and also three months after baseline.
Results:
Comparison tests indicated various improvements in resilience between baseline and five weeks and at three months, depending on the subgroup of participants (whether male or female or younger or older), as well as in terms of the way resilience was operationalised (e.g., ability to ‘bounce back’ or the protective factors associated with managing adversity).
Conclusion:
The study indicates that eQuoo can build resilience and can therefore provide a convenient means of supporting the mental health and wellbeing of young adults.
INTRODUCTION
The prevalence of mental health disorders in young people has been steadily rising over the past decade, with around 20% of the world’s young people currently living with a mental health condition [1]. In 2019 it was estimated that one in seven adolescents, or 166 million young women and men around the world experienced some form of mental disorder [2]. Depression, anxiety, and behavioural disorders are among the leading causes of illness and disability for young people globally [1]. Recent events such as the COVID-19 pandemic have further exacerbated this problem by contributing to levels of anxiety and depression while simultaneously decreasing young people’s ability to access in-person support [3, 4].
Mental health apps (herein referred to as mHealth apps) are a potentially beneficial resource for young people to both recover from disorder and maintain good mental wellbeing. Such apps are accessible for young people, who typically have high levels of cell phone use across a variety of sociodemographic domains [5]. They also have the potential to circumvent significant barriers such as stigma associated with seeking psychological help, a desire to manage symptoms on one’s own, and circumvent negative perceptions of treatment [6]. As pharmacological treatments can cause adverse effects and therefore are not suitable for everyone, mHealth apps as a nonpharmacological treatment may stand to serve a wide population of affected individuals [7].
While many mental health apps directly target symptoms of mental health issues, such as those that explore emotions and anxiety levels for individuals affected by anxiety [8] and those challenging beliefs and tracking mood for depression [9], an alternative approach to improving mental health is by building resilience. More than half of individuals under 18 years have reported experiencing at least one form of adversity [10–12], and over a quarter of all mental health problems are said to result from adverse events in childhood, such as neglect or abuse [12]. Resilience is the ability to overcome or adapt to adversity [13–15] and is receiving increasing interest due to the link between resilience and mental health [16, 17]. In sum, if many individuals experience adversity and these are linked to mental health problems, then building resilience as a means to help manage and overcome adversity can contribute to better mental health.
The way that resilience has been conceptualised, however, has implications for mHealth apps. Far from days when resilience was associated with innate personality traits [18], it is generally now considered a process of drawing on resources to overcome or adapt to adversity [19]. These resources, otherwise known as protective factors or resilience-enablers [20, 21] may be found within individuals (e.g., self-efficacy, self-regulation, future orientation) but also in the individual’s environment (e.g., community cohesion, safety, access to employment). As all of these factors, both internal and external, have been shown by resilience researchers to be modifiable [see, for example, 22], mHealth apps can work to improve a number of factors at once.
One particularly innovative mHealth app that builds resilience is eQuoo (https://www.equoogame.com/). eQuoo gamifies elements of psychoeducation, storytelling, Cognitive-Behavioural Therapy (CBT), and positive psychology to help users improve their mental health [6]. It differentiates itself from many other mHealth apps by presenting itself predominantly as an online quest (further details about the app given later), which increases the likelihood of uptake (especially among young people) and may also lead to continuing engagement, which is a problem for all forms of psychological services including apps [see 23, 24]. eQuoo is now in its second iteration and includes modules specifically addressing resilience factors. In addition to strengthening psychological resilience, eQuoo now promotes social-ecological resilience such as engaging with one’s community, exploration of culture and traditions, and seeking opportunities to use one’s talents.
Initial trials of the effectiveness of eQuoo have garnered positive results. A recent randomised controlled trial in the UK lasting five weeks found that users of the app significantly reduced self-reported levels of anxiety while increasing their resilience, positive growth, and social relationships, when compared to a control group and participants who used a non-gamified mental health app [6]. Furthermore, the 90% level of continuous engagement by participants over the intervention period was 21% higher than the rates of attrition in the control groups. Although promising, further testing is still required, including exploration of the longer-term impact of the app and its effect among populations residing in low- and middle-income countries (LMIC), as a large portion of mHealth studies have taken place only in high-income countries (HIC) in North America and Europe [7, 25].
The purpose of this study, then, was to examine the longer-term resilience-building capacity of the eQuoo mHealth app in a LMIC. An opportunity to conduct such a study arose when CLEAR (a Unilever brand of hair care products) adopted eQuoo as part of their initiative to address the mental health challenges of young people in a number of Asian countries. Specifically, the company launched an awareness campaign aimed at young people across their target markets, one of which was Vietnam. This was supported by data-gathering efforts to help further evaluate the app. Rates of youth mental illness in Vietnam are significant, with several studies indicating high levels of depression, suicidal behaviour, and associated risk-taking such as alcohol abuse [26]. Access to mental health support also remains low in the country, with poor geographic distribution of trained professionals, a lack of adequate training to screen and diagnose mental illness, shortages of psychotropic medications, and only 1.01 psychiatrists per 100,000 people (compared to 15.6 in OECD countries) [26]. mHealth interventions such as eQuoo therefore offer a potential means to address the treatment gap in Vietnam. Furthermore, in response to the COVID-19 pandemic, the government of Vietnam invested heavily in mHealth applications, which aligns with findings that indicate a readiness by Vietnamese to accept and utilize mHealth apps [27].
In this exploratory study, we expected levels of resilience to improve over time for participants who used the app. Specifically, we anticipated that there would be an improvement in resilience scores between baseline (T1) and the end of the app use period five weeks later (T2). To explore the longer-term impact of the app, we also compared baseline scores (T1) to scores taken three months later (T3), and compared scores at T2 and T3 to determine whether any improvements remained stable.
MATERIALS AND METHOD
Design
This study involved secondary analyses of a dataset compiled by a research and analytics company Asia Monitor (http://www.asiamonitor.com.my/) on behalf of CLEAR. CLEAR had sought to independently evaluate the impact of the eQuoo app, and so released the dataset to Dalhousie University’s Resilience Research Centre (RRC) which had the capacity and experience to analyse the data. The study adopted a repeated measures design, where participants used the eQuoo app over the course of five weeks (a week for each module) and completed a survey at baseline (T1; prior to using the app), at the end of the five-week period (T2), and then again three months after baseline (T3).
The study conforms to guidelines for nonrandomized studies of treatment effects using secondary data sources [28], as registered with the EQUATOR network [29]. As a case series study, it also conforms to the PROCESS guidelines [30]. The original data collection process conducted by Asia Monitor complied with the Market Research Society Professional Code of Conduct and data protection laws in Vietnam. The secondary analyses of the dataset were approved by Dalhousie’s Research Ethics Board (#2021-5516) and were registered at the Research Registry (UIN: researchregistry8504).
eQuoo
The eQuoo app is a five-week course taught by an avatar, Dr. Joy, and two associate avatars. After completion of the introductory course, players are invited to build their own avatar and begin a choose-your-own-adventure story in which they practice the skills they learned during the five-week course. The plot is based on a fictional world in which greed, corruption and pain have brought the world to a place of darkness known as “The Quavering”. Players are tasked with collecting five gems (each representing one dimension of emotional health: personal growth, anti-depression, anti-anxiety, relationship skills, and resilience) which they use to fight The Quavering.
Participants and procedure
There were 300 individuals initially recruited for the trial. However, Asia Monitor had excluded 25 (8%) who did not complete all three assessments. As our analyses involved grouping individuals by sex (see below), 11 individuals who did not indicate being male or female were also excluded as there were too few to constitute another group. The study sample therefore comprised 264 individuals (aged M = 25.65 years, SD = 4.84; 52% female) who were selected from four of the five tier one cities in Vietnam (Cantho, Danang, Hanoi, Ho Chi Minh City; Table 1). As per the normal market research functions Asia Monitor carries out for its clients, each city was divided into sections and landmarks where there was known to be considerable foot traffic. At these locations, participants were convenience sampled by being approached on the street by project assistants who invited the individual to take part in the study. At this initial point of contact, participants gave consent for their data to be analysed for research purposes and then completed the baseline survey. They were then given the link to the app, downloaded it to their phone, and were asked to complete the first unit by the end of the week. The project assistants re-contacted the participants to verify they had completed each unit. After five weeks, they were contacted again to request they complete the survey again, and again three months after baseline.
Table 1
Participant characteristics
| Characteristic | N | % |
| Sex | ||
| Female | 127 | 48 |
| Male | 137 | 52 |
| Age | ||
| 19–25 | 138 | 52 |
| 26–34 | 126 | 48 |
| Location | ||
| Ho Chi Minh City | 70 | 27 |
| Hanoi | 93 | 35 |
| Danang | 53 | 20 |
| Cantho | 48 | 18 |
| Education level | ||
| Some secondary school or equivalent | 9 | 3 |
| Vocational school/technical college | 94 | 36 |
| Some university/higher education | 47 | 18 |
| University degree | 107 | 41 |
| Postgraduate degree | 1 | <1 |
| Prefer not to say | 6 | 2 |
| Employment status | ||
| Working full-time | 149 | 56 |
| Working part-time | 26 | 10 |
| Studying full-time | 66 | 25 |
| Studying part-time | 7 | 3 |
| Unemployed | 7 | 3 |
| Other/prefer not to say | 9 | 3 |
| Household income | ||
| <15 million VND | 99 | 38 |
| =>15 million VND | 164 | 62 |
| Total | 264 | 100 |
Measures
We drew on three measures which assess different aspects of resilience, reflecting the complex and multisystemic nature of the construct [e.g., 14, 15]. The first was a modified version of the Brief Resilience Scale [BRS; 31], which is a six-item measure (score range 6–30) prompting participants to reflect on past experiences in terms of their ability to ‘bounce back’ following experiences of adversity. The measure’s items had been modified to make the BRS prospective, such that individuals were prompted to consider how likely they believed they would be to bounce back if they experienced adversity in the future (e.g., “I usually come through difficult times with little trouble” had been modified to read “If I encountered difficult times in the future, I would probably come through them with little trouble”) (present study reliability: α = 0.74, ω = 0.74). The modification was made to intervention testing since the original wording of the items could lead participants to consider a period of time prior to the intervention, meaning that their scores at T2 and T3 may not reflect changes attributable to the app. The second resilience measure was the Rugged Resilience Measure [RRM; 32], which contains 10 items (score range 10–50) and reflects psychological skills and strengths that are considered protective factors that facilitate resilience following experiences of adversity (e.g., problem-solving ability, emotion regulation) (α = 0.93, ω = 0.93). Similarly, the Adult Resilience Measure-Revised [33, 34] is a 17-item measure (score range 17–85) of resilience which assesses the availability and accessibility of social-ecological resources (e.g., community belonging, peer support) which facilitate resilience (α = 0.94, ω = 0.94). For the three measures, higher scores indicate higher levels of resilience. All the survey measures had been professionally translated from English to Vietnamese by Asia Monitor.
Analyses
There was a small amount of missing data across the study variables (T1 = 0.38%, T2 = 2.27%, T3 = 3.41%) thus no imputation was required. We specified individual linear mixed effects models for each of the outcomes, involving time (T1-T3), sex (male/female), and age group (19-24/26-34) as fixed factors (plus interactions), and we specified random intercepts for participants. We used planned comparisons to examine changes in the outcomes between time points. All p-values were Tukey corrected. Effect sizes were produced and interpreted using standard benchmarks (small: d = 0.2; medium: d = 0.5; large: d = 0.8; Cohen, 1988). All analyses were performed in R (v4.0.0) using lme4 (v4_1.1–27.1) and emmeans (v1.7.2) for pairwise comparisons and the calculation of effect sizes. The data and code for replicating analyses can be found at https://osf.io/yhjgc/.
RESULTS
Changes in BRS scores
There were no significant differences when contrasting BRS scores between baseline and the five-week end-of-app-use period, for males or females of either age group (Table 2). However, when comparing scores at baseline and the three-month time point, scores of 26-34-year-old males and females were found to significantly improve (males: MT1 = 19.68, SET1 = 0.42, MT3 = 21.45, SET3 = 0.42, p = 0.001; females: MT1 = 19.45, SET1 = 0.42, MT3 = 20.61, SET3 = 0.42, p = 0.038). The effect sizes for these improvements were medium (d = 0.668) and small to medium (d = 0.435; respectively). BRS scores for 16-25-year-old males and females did not significantly differ between baseline and five weeks, or between five weeks and three months.
Table 2
Average resilience scores at each time point with paired comparison tests
| M (SE) | T1 vs T2 | T1 vs T3 | T2 vs T3 | ||||||||||||
| T1 | T2 | T3 | t | df | p | d | t | df | p | d | t | df | p | d | |
| BRS | |||||||||||||||
| Males, 19–25 | 19.15 (0.41) | 19.54 (0.41) | 19.74 (0.41) | 0.825 | 515 | 0.688 | – | 1.254 | 515 | 0.422 | – | 0.429 | 515 | 0.904 | – |
| Females, 19–25 | 19.67 (0.39) | 19.48 (0.39) | 19.44 (0.40) | 0.423 | 521 | 0.906 | – | 0.517 | 522 | 0.862 | – | 0.096 | 517 | 0.904 | – |
| Males, 26–34 | 19.68 (0.42) | 20.61 (0.42) | 21.45 (0.42) | 1.960 | 515 | 0.123 | – | 3.717 | 515 | 0.001 | 0.668 | 1.757 | 515 | 0.185 | – |
| Females, 26–34 | 19.45 (0.42) | 20.30 (0.42) | 20.61 (0.42) | 1.796 | 515 | 0.172 | – | 2.461 | 515 | 0.038 | 0.435 | 0.665 | 515 | 0.784 | – |
| RRM | |||||||||||||||
| Males, 19–25 | 34.52 (0.83) | 36.05 (0.82) | 39.22 (0.82) | 1.643 | 516 | 0.229 | – | 50.062 | 516 | <0.001 | 0.892 | 30.436 | 514 | 0.002 | 0.603 |
| Females, 19–25 | 34.68 (0.78) | 37.69 (0.79) | 38.92 (0.79) | 3.422 | 520 | 0.002 | 0.572 | 4.795 | 521 | <0.001 | 0.805 | 1.384 | 516 | 0.350 | – |
| Males, 26–34 | 36.82 (0.84) | 37.61 (0.84) | 39.39 (0.84) | 0.837 | 514 | 0.680 | – | 2.716 | 514 | 0.019 | 0.488 | 1.879 | 514 | 0.146 | – |
| Females, 26–34 | 35.97 (0.83) | 39.38 (0.83) | 39.78 (0.83) | 3.665 | 514 | 0.001 | 0.648 | 4.102 | 514 | <0.001 | 0.725 | 0.437 | 514 | 0.900 | – |
| ARM | |||||||||||||||
| Males, 19–25 | 63.14 (1.23) | 64.69 (1.23) | 67.28 (1.23) | 1.166 | 515 | 0.474 | – | 3.104 | 515 | 0.006 | 0.545 | 1.939 | 515 | 0.129 | – |
| Females, 19–25 | 64.32 (1.16) | 67.17 (1.17) | 68.70 (1.18) | 2.245 | 520 | 0.065 | – | 3.439 | 522 | 0.002 | 0.578 | 1.200 | 517 | 0.454 | – |
| Males, 26–34 | 64.94 (1.26) | 66.90 (1.26) | 67.24 (1.26) | 1.442 | 515 | 0.320 | – | 1.690 | 515 | 0.210 | – | 0.0248 | 515 | 0.967 | – |
| Females, 26–34 | 66.91 (1.24) | 70.22 (1.24) | 69.86 (1.24) | 2.465 | 515 | 0.037 | 0.436 | 2.198 | 515 | 0.073 | – | 0.267 | 515 | 0.961 | – |
Note: Shaded cells foreground significant results. Effect sizes are only given for significant findings. M = Mean, SE = Standard Error, t = t-ratio, df = degrees of freedom, p = p-value, d = Cohen’s d effect size. p-values are Tukey corrected.
Changes in RRM scores
RRM scores for both age groups of females significantly improved during the app use period (16-25-year-old females: MT1 = 34.68, SET1 = 0.78, MT2 = 37.69, SET2 = 0.79, p = 0.002; 26-34-year-old females: MT1 = 35.97, SET1 = 0.83, MT2 = 39.38, SET2 = 0.83, p = 0.001), both with medium effect sizes (d = 0.572 and 0.648, respectively). These improvements remained stable, with no significant differences observed between the five-week and three-month time points (Fig. 1).
Fig. 1
Changes in average resilience scores over time for 16-25-year-old and 26-34-year-old males and females. Note: Error bars represent standard error.
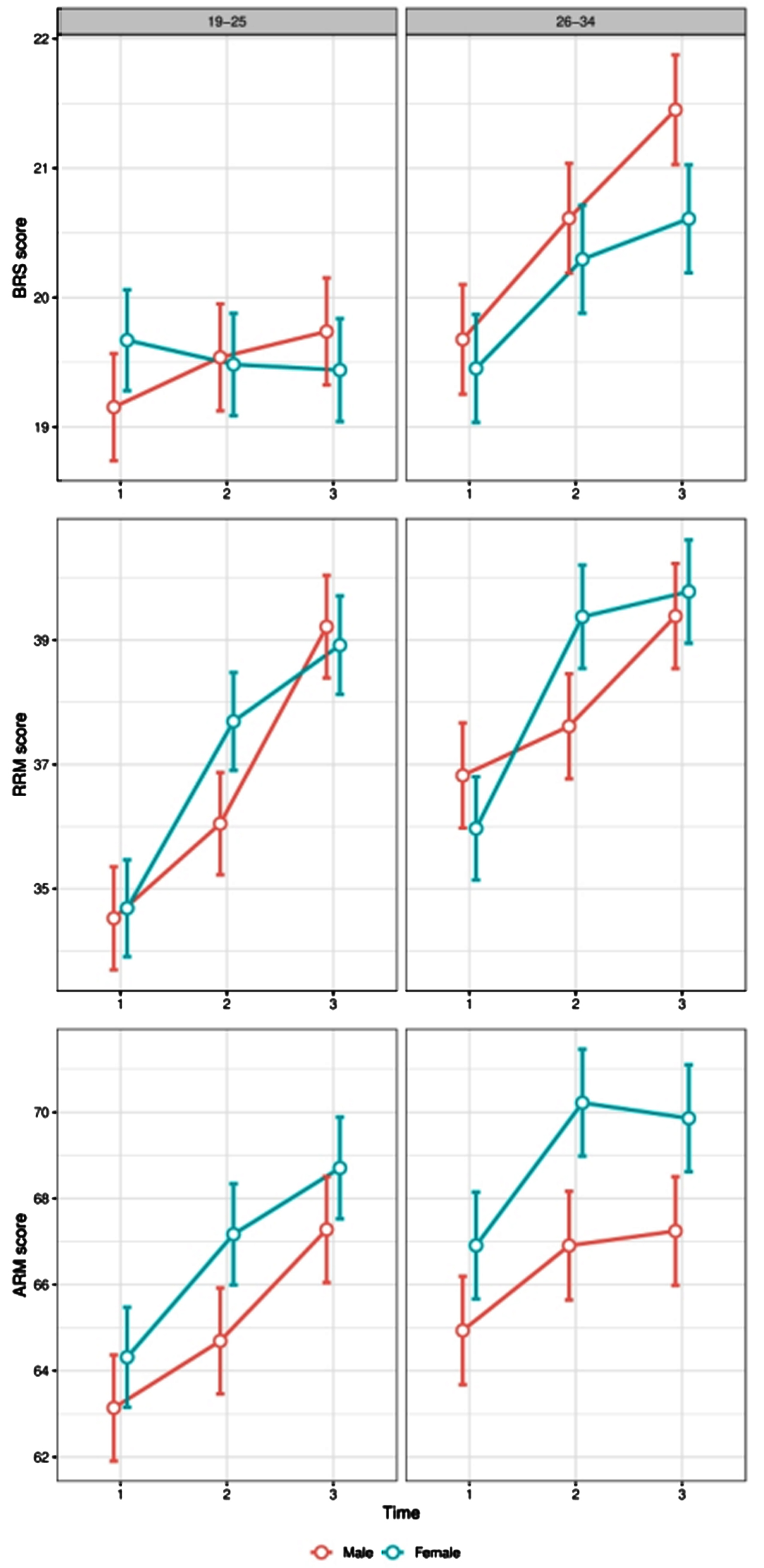
Although the RRM scores of 16-25-year-old male participants did not improve during the app use period, there was a significant improvement (large effect size) when comparing their baseline and three-month scores (MT1 = 34.52, SET1 = 0.83, MT3 = 39.22, SET3 = 0.82, p < 0.001, d = 0.892). A significant improvement (medium effect size) was also observed between the five-week and three-month time points (MT1 = 34.68, SET1 = 0.78, MT2 = 37.69, SET2 = 0.79, p = 0.002, d = 0.603).
A similar result was found for RRM scores of 26-34-year-old male participants, which also did not significantly improve between baseline and five weeks, but did show a small to medium effect size between baseline and three months (MT1 = 36.82, SET1 = 0.84, MT3 = 39.39, SET3 = 0.84, p = 0.019, d = 0.488).
Changes in ARM scores
Only the ARM scores of 26-34-year-old female participants significantly improved (small to medium effect size) during the app use period (MT1 = 66.91, SET1 = 1.24, MT2 = 70.22, SET2 = 1.24, p = 0.002, d = 0.436). This improvement remained stable, with no significant changes observed between the five-week and three-month time points. However, like with the RRM scores of male participants, ARM scores for both 16-25-year-old males and females that had not significantly improved between baseline and five weeks did so between baseline and three months (16-25-year-old males: MT1 = 63.14, SET1 = 1.23, MT3 = 67.28, SET3 = 1.23, p = 0.006, d = 0.545; 16-25-year-old females: MT1 = 64.32, SET1 = 1.16, MT3 = 68.70, SET3 = 1.18, p = 0.002, d = 0.578). No changes in scores were observed for 26-34-year-old male participants.
DISCUSSION
This study found that there are some short- and long-term improvements to resilience associated with using the mHealth app, eQuoo. Specifically, there were significant short-term increases in some resilience scores for female participants, while scores for both male and female participants continued to improve up to the three-month measurement point. This contributes to the body of evidence supporting the effectiveness of mHealth apps such as eQuoo [7, 36–39].
In particular, the findings of this study extend those of Litvin and colleagues [6] in their evaluation of the eQuoo app. That study found that resilience scores increased over the course of a five-week period while using the app when using the ARM to measure resilience. In the current study reported here, however, we only detected an increase in ARM scores for 26-34-year-old females during the five-week app-use period. Improvements for 16-25-year-old participants (both male and female) were only observed when comparing baseline to three-month time points. The discrepancy may be due to the different versions of the app under evaluation (Litvin and colleagues used an earlier version, which contained training on just ten psychological skills; for further details see Litvin et al., 2020) but may also be a feature of the sample. Litvin et al.’s sample were from the UK and included a broader age range (“16–24+”). Where culture and age have been accounted for in studies of resilience, there is always the possibility of finding distinctly local or age-related patterns to positive development even if the same themes (like the need for self-efficacy, empathy and sense of belonging) vary in how these aspects of positive development are expressed [40, 41].
Furthermore, the findings in this study are based on results from data collected over a longer period of time than in Litvin’s earlier evaluation of eQuoo. The longer time frame (three months) may be necessary to detect change in social-ecological resources associated with resilience, like relationships with family members and one’s community, factors measured by the ARM. Therefore, although use of the app may lead to individuals feeling more capable in terms of their ability to improve their resilience, actual improvements (as measured by the ARM) may require opportunities to build new resources or make better use of the resources already available, such as a broader social network or finding opportunities to use one’s talents [42].
Relatedly, RRM scores improved during the app use period for female participants, but improvements for male participants were only significant when comparing baseline to three-month scores. The RRM focuses on psychological protective factors associated with resilience, which may explain why scores for female participants improved during the app-use period while males took longer to integrate the learning. This pattern will need further investigation to understand better the link between sex, gender and cultural norms regarding how males and females in a LMIC like Vietnam perceive and express personal resilience.
Interestingly, perceptions of one’s ability to bounce back, as measured by the BRS, only showed improvement for 26-34-year-old participants when their baseline and three-month scores were used in the analysis. No significant improvements were detected for 16-25-year-old participants. Here again we see the need to, first, conduct an assessment of app effectiveness by including a number of different measures of positive outcomes if one is to detect the nuances of changes in individual and social resources associated with psychological growth. Second, we suspect that an app like eQuoo has a differential impact in different cultural spaces depending on the intersection of participant qualities like age, sex, gender, and cultural values and beliefs. Therefore, research exploring the impact of mHealth apps on resilience should take care to operationalise the construct appropriately and match measures accordingly (whether the capacity to bounce back, levels of psychological protective factors, or levels of social-ecological protective factors). Future studies should also include populations from more than one country context and use multiple measures of resilience if they are to inform a deeper understanding of which populations benefit most from apps like eQuoo that gamify lessons in positive development.
Furthermore, after reviewing recent meta-analysis studies, we did not encountered any that explored the potential differing impact of mobile interventions for mental health between older and younger individuals, or between sexes (e.g., [43–47]). Our findings, some of which varied depending on the age and sex of the individual, suggest that different groups may respond to apps in different ways, which may be an important focus for future research (i.e., to discover how and why) as well as promoting the importance of outcome analyses involving these subgroups.
Despite the nuances to our study’s results, overall, the findings indicate improvements to resilience as a result of using eQuoo. Furthermore, none of the improvements occurring by the end of the app-use period significantly declined at the three-month time point, indicating that improvements, when they occurred, were sustained. However, there was much heterogeneity in terms of the particular groups that benefited (males vs females, 26-34-year-olds vs. 16-25-year-olds), when improvements occurred, and depending on the particular resilience measure used.
Limitations and future directions
A clear limitation of this study was the lack of a control group. Without such a comparison, it is not possible to confirm whether improvements in scores were due to the app or another influence. Although this research study was exploratory, further hypothesis-testing research using a randomised control trial design would be important to confirm improvements in resilience as a result of using eQuoo.
Conclusion
There is growing interest in using apps to provide mental health care to populations under stress. While most of the effectiveness trials for these apps are taking place in HIC, there is growing interest in their use from many countries that lack a well-developed mental health care system. Who benefits most from their use, and which kinds of apps are likely to engage different populations most is still not known. This current study suggests that apps like eQuoo could have a positive effect on resilience, though a great many questions remain regarding measurement design, dose effects and contextual factors which influence participant outcomes. Future research will need to address these issues if these apps are to be relevant to culturally diverse populations.
ACKNOWLEDGMENTS INCLUDING SOURCES OF SUPPORT
Conflict of interests
The authors have no conflict of interest to report.
Acknowledgements
The authors would like to acknowledge the support of Clear for providing the dataset.
Funding
The authors have no funding to report.
AUTHORS’ CONTRIBUTIONS
PJ: Conceptualization (equal); methodology (equal); formal analysis (lead); writing –original draft (lead); writing –review and editing (equal).
AD: Writing –original draft (supporting); review and editing (equal).
MU: Conceptualization (equal); methodology (equal); writing –original draft (supporting); writing –review and editing (equal).
REFERENCES
[1] | World Health Organization. Adolescent mental health. 2021 [cited 15 Jul 2022]. Available: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health |
[2] | UNICEF. The State of theWorld’s Children 2021. UNICEF; 2021. Available: https://www.unicef.org/reports/state-worlds-children-2021 |
[3] | Eisenstadt M , Liverpool S , Infanti E , Ciuvat RM , Carlsson C . Mobile Apps That Promote Emotion Regulation, Positive Mental Health, and Well-being in the General Population: Systematic Review and Meta-analysis. JMIR Ment Health. (2021) ;8: :e31170. doi: 10.2196/31170 |
[4] | Shah SMA , Mohammad D , Qureshi MFH , Abbas MZ , Aleem S . Prevalence, Psychological Responses and Associated Correlates of Depression, Anxiety and Stress in a Global Population, During the Coronavirus Disease (COVID-19) Pandemic. Community Ment Health J. (2021) ;57: :101–10. doi: 10.1007/s10597-020-00728-y |
[5] | Seko Y , Kidd S , Wiljer D , McKenzie K . Youth mental health interventions via mobile phones: a scoping review. Cyberpsychology Behav Soc Netw. (2014) ;17: :591–602. doi: 10.1089/cyber.2014.0078 |
[6] | Litvin S , Saunders R , Maier MA , Lüttke S . Gamification as an approach to improve resilience and reduce attrition in mobile mental health interventions: A randomized controlled trial. PLOS ONE. (2020) ;15: :e0237220. doi: 10.1371/journal.pone.0237220 |
[7] | Abd-Alrazaq A , Alajlani M , Alhuwail D , Schneider J , Akhu-Zaheya L , Ahmed A , et al. The Effectiveness of Serious Games in Alleviating Anxiety: Systematic Review and Meta-analysis. JMIR Serious Games. (2022) ;10: :e29137. doi: 10.2196/29137 |
[8] | Balaskas A , Schueller SM , Cox AL , Doherty G . The Functionality of Mobile Apps for Anxiety: Systematic Search and Analysis of Engagement and Tailoring Features. JMIR MHealth UHealth. (2021) ;9: :e26712. doi: 10.2196/26712 |
[9] | Stawarz K , Preist C , Tallon D , Wiles N , Coyle D . User Experience of Cognitive Behavioral Therapy Apps for Depression: An Analysis of App Functionality and User Reviews. J Med Internet Res. (2018) ;20: :e10120. doi: 10.2196/10120 |
[10] | Green JG , McLaughlin KA , Berglund PA , Gruber MJ , Sampson NA , Zaslavsky AM , et al. Childhood adversities and adult psychopathology in the National Comorbidity Survey Replication (NCS-R) I: Associations with first onset of DSM-IV disorders. Arch Gen Psychiatry. (2010) ;67: :113. doi: 10.1001/archgenpsychiatry.2009.186 |
[11] | Kessler RC , Davis CG , Kendler KS . Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychol Med. (1997) ;27: :1101–19. doi: 10.1017/s0033291797005588 |
[12] | Kessler RC , McLaughlin KA , Green JG , Gruber MJ , Sampson NA , Zaslavsky AM , et al. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br J Psychiatry J Ment Sci. (2010) ;197: :378–85. doi: 10.1192/bjp.bp.110.080499 |
[13] | Masten AS . Ordinary magic. Resilience processes in development. Am Psychol. (2001) ;56: :227–38. |
[14] | Ungar M . Multisystemic Resilience: Adaptation and Transformation in Contexts of Change. Oxford, New York: Oxford University Press; (2021) . |
[15] | Windle G . What is resilience? A review and concept analysis. Rev Clin Gerontol. (2011) ;21: :152–69. doi: 10.1017/S0959259810000420 |
[16] | Akeman E , Kirlic N , Clausen AN , Cosgrove KT , McDermott TJ , Cromer LD , et al. A pragmatic clinical trial examining the impact of a resilience program on college student mental health. Depress Anxiety. (2020) ;37: :202–13. doi: 10.1002/da.22969 |
[17] | Chmitorz A , Kunzler A , Helmreich I , Tüscher O , Kalisch R , Kubiak T , et al. Intervention studies to foster resilience—A systematic review and proposal for a resilience framework in future intervention studies. Clin Psychol Rev. (2018) ;59: :78–100. doi: 10.1016/j.cpr.2017.11.002 |
[18] | Anthony EJ . Children at high risk for psychosis growing up successfully. The invulnerable child. New York, NY, US: Guilford Press; (1987) . pp. 147–184. |
[19] | Ungar M , Theron L . Resilience and mental health: how multisystemic processes contribute to positive outcomes. Lancet Psychiatry. (2020) ;7: :441–8. doi: 10.1016/S2215-0366(19)30434-1 |
[20] | Pachter LM , Lieberman L , Bloom SL , Fein JA . Developing a Community-Wide Initiative to Address Childhood Adversity and Toxic Stress: A Case Study of The Philadelphia ACE Task Force. Acad Pediatr. (2017) ;17: :S130–S135. doi: 10.1016/j.acap.2017.04.012 |
[21] | Theron LC . Researching resilience: lessons learned from working with rural, Sesotho-speaking South African young people. Qual Res. (2016) ;16: :720–37. doi: 10.1177/1468794116652451 |
[22] | National Research Council (US) and Institute of Medicine (US) Committee on Integrating the Science of Early Childhood Development. From Neurons to Neighborhoods: The Science of Early Childhood Development. Shonkoff JP, Phillips DA, editors. Washington (DC): National Academies Press (US); 2000. Available: http://www.ncbi.nlm.nih.gov/books/NBK225557/ |
[23] | Duffy D , Enrique A , Connell S , Connolly C , Richards D . Internet-Delivered Cognitive Behavior Therapy as a Prequel to Face-To-Face Therapy for Depression and Anxiety: A Naturalistic Observation. Front Psychiatry. 2020;10. Available: https://www.frontiersin.org/articles/10.3389/fpsyt.2019.00902 |
[24] | Lippke S , Gao L , Keller FM , Becker P , Dahmen A . Adherence With Online Therapy vs Face-to-Face Therapy and With Online Therapy vs Care as Usual: Secondary Analysis of Two Randomized Controlled Trials. J Med Internet Res. (2021) ;23: :e31274. doi: 10.2196/31274 |
[25] | Hall CS , Fottrell E , Wilkinson S , Byass P . Assessing the impact of mHealth interventions in low- and middle-income countries–what has been shown to work? Glob Health Action. (2014) ;7: :25606. doi: 10.3402/gha.v7.25606 |
[26] | Sobowale K , Nguyen M , Weiss B , Van TTH , Trung LT . Acceptability of internet interventions for youth mental health in Vietnam. Glob Ment Health Camb Engl. (2016) ;3: :e22. doi: 10.1017/gmh.2016.18 |
[27] | Nguyen HL , Tran K , Doan PLN , Nguyen T . Demand for Mobile Health in Developing Countries During COVID- Vietnamese’s Perspectives from Different Age Groups and Health Conditions. Patient Prefer Adherence. (2022) ;16: :265–84. doi: 10.2147/PPA.S348790 |
[28] | Berger ML , Mamdani M , Atkins D , Johnson ML . Good research practices for comparative effectiveness research: defining, reporting and interpreting nonrandomized studies of treatment effects using secondary data sources: the ISPOR Good Research Practices for Retrospective Database Analysis Task Force Report–Part I. Value Health J Int Soc Pharmacoeconomics Outcomes Res. (2009) ;12: :1044–52. doi: 10.1111/j.1524-4733.2009.00600.x |
[29] | The EQUATOR Network. Good research practices for comparative effectiveness research: Defining, reporting and interpreting nonrandomized studies of treatment effects using secondary data sources. 2013 [cited 15 Feb 2022]. Available: https://www.equator-network.org/reporting-guidelines/good-research-practices-for-comparative-effectiveness-research-defining-reporting-and-interpreting-nonrandomized-studies-of-treatment-effects-using-secondary-data-sources-the-ispor-good-research-pr/ |
[30] | Agha RA , Sohrabi C , Mathew G , Franchi T , Kerwan A , O’Neill N , et al. The PROCESS Guideline: Updating Consensus Preferred Reporting Of CasE Series in Surgery (PROCESS) Guidelines. Int J Surg. (2020) ;84: :231–5. doi: 10.1016/j.ijsu.2020.11.005 |
[31] | Smith BW , Dalen J , Wiggins K , Tooley E , Christopher P , Bernard J . The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. (2008) ;15: :194–200. doi: 10.1080/10705500802222972 |
[32] | Jefferies P , Vanstone R , Ungar M . The Rugged Resilience Measure: validation of a brief measure of personal resilience. Appl Res Qual Life. 2021. doi:https://doi.org/10.1007/s11482-021-09953-3 |
[33] | Jefferies P , McGarrigle L , Ungar M . The CYRM-R: A Rasch-validated revision of the Child and Youth Resilience Measure. J Evid-Inf Soc Work. 2018. doi:https://doi.org/10.1080/23761407.2018.1548403 |
[34] | Jefferies P , Höltge J , Ungar M . Social Anxiety and Resilience: Associations Vary by Country and Sex. Advers Resil Sci. (2021) ;2: :51–62. doi: 10.1007/s42844-020-00026-2 |
[35] | Cohen J . Statistical power analysis for the behavioral sciences. New York, NY: Lawrence Erlbaum Associates; 1988. Available: http://www.utstat.toronto.edu/∼brunner/oldclass/378f16/readings/CohenPower.pdf |
[36] | Domhardt M , Messner E-M , Eder A-S , Engler S , Sander LB , Baumeister H , et al. Mobile-based interventions for common mental disorders in youth: a systematic evaluation of pediatric health apps. Child Adolesc Psychiatry Ment Health.. (2021) ;15: :49. doi: 10.1186/s13034-021-00401-6 |
[37] | Grist R , Porter J , Stallard P . Mental Health Mobile Apps forPreadolescents and Adolescents: A Systematic Review. J Med Internet Res. (2017) ;19: :e7332. doi: 10.2196/jmir.7332 |
[38] | Marshall JM , Dunstan DA , Bartik W . The role of digital mental health resources to treat trauma symptoms in Australia during COVID-19. Psychol Trauma Theory Res Pract Policy. (2020) ;12: :S269–S271. doi: 10.1037/tra0000627 |
[39] | Naslund JA , Marsch LA , McHugo GJ , Bartels SJ . Emerging mHealth andeHealth interventions for serious mental illness: a review of theliterature. J Ment Health Abingdon Engl. (2015) ;24: :321–32. doi: 10.3109/09638237.2015.1019054 |
[40] | Steinberg L . How to Improve the Health of American Adolescents. Perspect Psychol Sci J Assoc Psychol Sci. (2015) ;10: :711–5. doi: 10.1177/1745691615598510 |
[41] | Ungar M . Researching and theorizing resilience across cultures and contexts. Prev Med. (2012) ;55: :387–9. doi: 10.1016/j.ypmed.2012.07.021 |
[42] | Jefferies P , Höltge J , Fritz J , Ungar M . A Cross-Country Network Analysis of Resilience Systems in Young Adults. Emerg Adulthood. 2022;21676968221090040. doi: 10.1177/21676968221090039 |
[43] | Lecomte T , Potvin S , Corbière M , Guay S , Samson C , Cloutier B , et al. Mobile Apps for Mental Health Issues: Meta-Review of Meta-Analyses. JMIR MHealth UHealth. (2020) ;8: :e17458. doi: 10.2196/17458 |
[44] | Lu S-C , Xu M , Wang M , Hardi A , Cheng AL , Chang S-H , et al. Effectiveness and Minimum Effective Dose of App-Based Mobile Health Interventions for Anxiety and Depression Symptom Reduction: Systematic Review and Meta-Analysis. JMIR Ment Health. (2022) ;9: :e39454. doi: 10.2196/39454 |
[45] | Serrano-Ripoll MJ , Zamanillo-Campos R , Fiol-DeRoque MA , Castro A , Ricci-Cabello I . Impact of Smartphone App-Based Psychological Interventions for Reducing Depressive Symptoms in People With Depression: Systematic Literature Review and Meta-analysis of Randomized Controlled Trials. JMIRMHealth UHealth. (2022) ;10: :e29621. doi: 10.2196/29621 |
[46] | Wu A , Scult MA , Barnes ED , Betancourt JA , Falk A , Gunning FM . Smartphone apps for depression and anxiety: a systematic review and meta-analysis of techniques to increase engagement. Npj Digit Med. (2021) ;4: :1–9. doi: 10.1038/s41746-021-00386-8 |
[47] | Linardon J , Cuijpers P , Carlbring P , Messer M , Fuller-Tyszkiewicz M . The efficacy of app-supported smartphone interventions for mental health problems: a meta-analysis of randomized controlled trials. World Psychiatry. (2019) ;18: :325–36. doi: 10.1002/wps.20673 |




