Bedside Treatment Decisions: An Evaluation of the Factors Physicians Take into Consideration When Making Complex Rationing Decisions
Abstract
Background:
The budget limitations that are imposed on health care providers often force caregivers to become rationers, and physicians are required to select which patients receive treatments and which go without on a daily basis. This involves making highly complex decisions, and physicians are required to evaluate both relevant and irrelevant parameters to ensure the final decision is sound.
Objective:
This research examined which of seven parameters physicians used to make rational decisions as to which of a group of five patients in need received treatment.
Method:
An experiment was conducted in which the decision relevance of objective parameters and additional information about the needy, such as gender or smoking habits, were investigated.
Results and conclusion:
The findings indicated that physicians focus on central disease-related criteria very well and, thus, arrive at a comprehensive rationing decision, even in complex situations.
INTRODUCTION
Health care systems all over the world have the same target: To provide people with access to the essential health care services they need. For various reasons, including the availability of new expensive treatment options and the aging population of societies, health care resources are becoming increasingly scarce. This problem results in questions emerging as to who should be treated, which patients have priority, and which therapy is adequate; i.e., prioritization and rationing. On a macro level, prioritization and rationing are often determined by politics; for example, specific services are openly excluded from funding or more patients are allocated to a given hospital. As such, in most cases, a transparent and distinct process is in place. However, prioritization and rationing decisions are more complicated on a micro level in that the caregiving physician is required to make bedside decisions relating to aspects such as how much time to spend with each patient and when to prescribe or withhold an expensive therapy [1]. Accordingly, this decision-making process is much less transparent, and different interests can have an influence on the choices that are made; for example, the physician may make decisions that aim to save money for the hospital he is working for, i.e., to release a patient from hospital earlier, maximize his own earnings in situations in which he is compensated for every single surgery he performs, and/or eradicate or reduce the suffering of his patients and enhance their quality of life by implementing the most appropriate, yet most complex and expensive, treatment [2].
However, it is not just these varying interests that make physicians’ day-to-day decision-making processes complex. To arrive at a valid diagnosis and treatment plan, they must consider various information, parameters, and aspects concerning the condition of the individual being treated. The more holistically physicians observe all facets, the more probable it is that they will ultimately take actions that result in the patient achieving the best level of care. However, in addition to ensuring all relevant aspects are taken into consideration, it is also essential that physicians make sure that any information that is not relevant to the treatment process is ignored to avoid any specific groups being discriminated against or unfairly treated [1]. Consequently, rationing care at the bedside involves a complex decision-making process that requires maximal attention and continuous reflection on self-leading motives and decision patterns.
In the literature presented so far, various potential prioritization and rationing criteria have been discussed. Objective criteria especially presented to medical staff for example concern medical or sociodemographic aspects. Also included are valuing criteria. Participants here evaluate the relevance of compliance, social contribution and self-infliction [1, 6]. Further studies work with participants without medical expertise [3– 5]. Presented criteria also include objective aspects such as severity of disease and anticipated health state after treatment. However, subjects refused valuing criteria such as socio-economic status, age, social responsibility or a positive cost-utility-ration. Summing up, opinions of the relevance of socio-economic differences strongly varied across the people who were questioned. However, this could be attributed to the fact that the authors of these studies implemented different methods, including discrete choice experiments and interviews, as part of the research process.
Despite the differences in methodologies employed, the existing studies have typically involved methods that ask participants to either imagine themselves in the shoes of a physician who is required to ration or to generally report which criteria they perceive to be decision relevant. Thus, these studies do not provide insights into real decision-making behavior as applied to real situations in which individuals are in need.
This study aimed to complement the existing studies using an experimental approach; a method that remains lacking in the related literature [7]. Therefore, in our laboratory, we arranged real decision situations in which one physician decided which of five patients in need would receive treatment. The research question was as follows: When available treatment resources are limited, which individual attributes do physicians take into consideration to arrive at a rationing decision?
Table 1
Overview of previous studies that have investigated the application of prioritization criteria when making medical decisions
| Participants | Relevant/ rejected criteria for prioritization | Method | Reference | ||
| Care-givers | Physicians | Medical criteria | Qualitative interviews | [1] | |
| Cost-effectiveness | |||||
| Age | |||||
| Compliance | |||||
| Social contribution | |||||
| Physicians and nurses | Medical criteria | Semistructured interviews | [6] | ||
| Self-infliction of disease | |||||
| Sociodemographic criteria | |||||
| Samples without medical background | Students | Healthy lifestyle | Conjoint analysis | [4] | |
| Social class | |||||
| Life expectancy after treatment | |||||
| Quality of life after treatment | |||||
| General public | Life threatening disease Acute disease | Rejected: Socio-economic status | Questionnaire, Discrete choice experiment | [3] | |
| General public | Severity of disease Treatment effectiveness | Rejected: | Postal survey of random sample | [5] | |
| Age | |||||
| Social responsibility | |||||
| Positive cost-utility-ratio | |||||
METHOD
Experimental design
The task
Sixteen physicians with a minimum of 6 months work experience in a hospital participated in this research, and each one was allocated to a group of five subjects (henceforth patients). A pain dose was randomly allocated to each patient; i.e., the parameters of the cold pressor test (cp. Paragraph on pain induction): water temperature and hand immersion duration. These doses varied for every patient. In addition, we randomly allocated treatment costs to every patient. The physician was allocated a fixed budget of five Euros, which he was free to invest in treatments for the patients awaiting pain as he saw fit. The allocation was realized with an algorithm that ensured that, with his restricted budget, the physician could treat i. e. select up to three or four patients, but never all of them (cp. Tab. 2b). Treatment costs were not linearly related to pain doses because, in reality, there is not necessarily a positive correlation between the severity of the pain and the cost of the treatment. In addition, the budgets that were available to treat the patients were not related to the final payment the physicians received for participating in the experiment. This was purposely designed to replicate the standard payment system that is in use in the majority of public hospitals, where the monthly salary is fixed, irrelevant of the number of patients treated or performance against budget. Accordingly, any remaining credit expired.
Table 2
a: Criteria that was available for rationing decisions (left), b: Examples of allocated costs to pain doses (right)
| Criteria | Description | Levels | Allocation of costs (examples) | |
| Water temperature Immersion duration in cold water | Randomly allocated to every participant at the beginning of the experiment, coupled with immersion duration | 4°Celsius for 1 minute | 0,80EUR | 0,80EUR |
| 4°Celsius for 3 minutes | 0,50EUR | 1,00EUR | ||
| 7°Celsius for 2 minutes | 1,00EUR | 2,00EUR | ||
| 9°Celsius for 2,5 minutes | 1,30EUR | 1,30EUR | ||
| 12°Celsius for 3 minute | 4,50EUR | 3,00EUR | ||
| Costs to be treated | Randomly allocated to every participant independent from water temperature and immersion duration in each session | Varying between 0,80 EUR and 4,S0 EUR | ||
| Sex | Information given by the participant himself | M/F | ||
| Smoking habits | Information given by the participant himself | Smoking / non smoking | ||
| Birth place | Information given by the participant himself | City/country | ||
| Academic parents | Information given by the participant himself | At least one parent with a university degree yes / no | ||
Real consequences for decisions
The experiment was designed to ensure that the decisions the physicians made had real consequences. A live video camera link was established so that the physicians could immediately observe the pain caused to the patients that they chose not to treat due to lack of budget. This made the physicians aware of the relevance and consequence of their decisions, even in a laboratory situation.
Pain induction
For the purposes of this research, we opted to use a pain-induction procedure that is particularly appropriate for simulating chronic pain [8]: the cold pressor test [9]. This test involves a subject immersing his or her hand in a bowl of cold water. A water temperature of around 16° Celsius induces slight pain; the colder the water is, the stronger the pain.
Application of criteria (1 and 2)
The physicians were provided with seven criteria to enable their rationing decision on who finally must suffer from cold pressor pain and who is treated, i. e. wont suffer from the pain. The first three criteria were allocated randomly, the remaining four were based on the indications of each patient (Table 2).
To establish which of these criteria they applied to arrive at their decisions, we implemented two different procedures: (1) A subjective approach involving an individual rating of the criteria, and (2) an objective approach, via a software called Mouse Lab [10].
Individual rating (1)
For the rating, the physicians worked with a chart that listed each criterion together with a scale that ranged from one, “criterion was irrelevant for my decision” through to 10, which represented the maximum relevance of the criteria to ration the patients. The physician rated the criteria immediately after making his decisions.
Mouse Lab software (2)
To ensure that the subjective self-assessment of criteria usage was not confounded by any bias, we also employed a software program that measured two aspects: The frequency with which one criterion was looked at and the time spent looking at this criterion. Therefore, the seven criteria for the five patients were presented as demonstrated in Fig. 1.
Fig.1
Mouse Lab interface through which the physician could get to know all details about the patients.
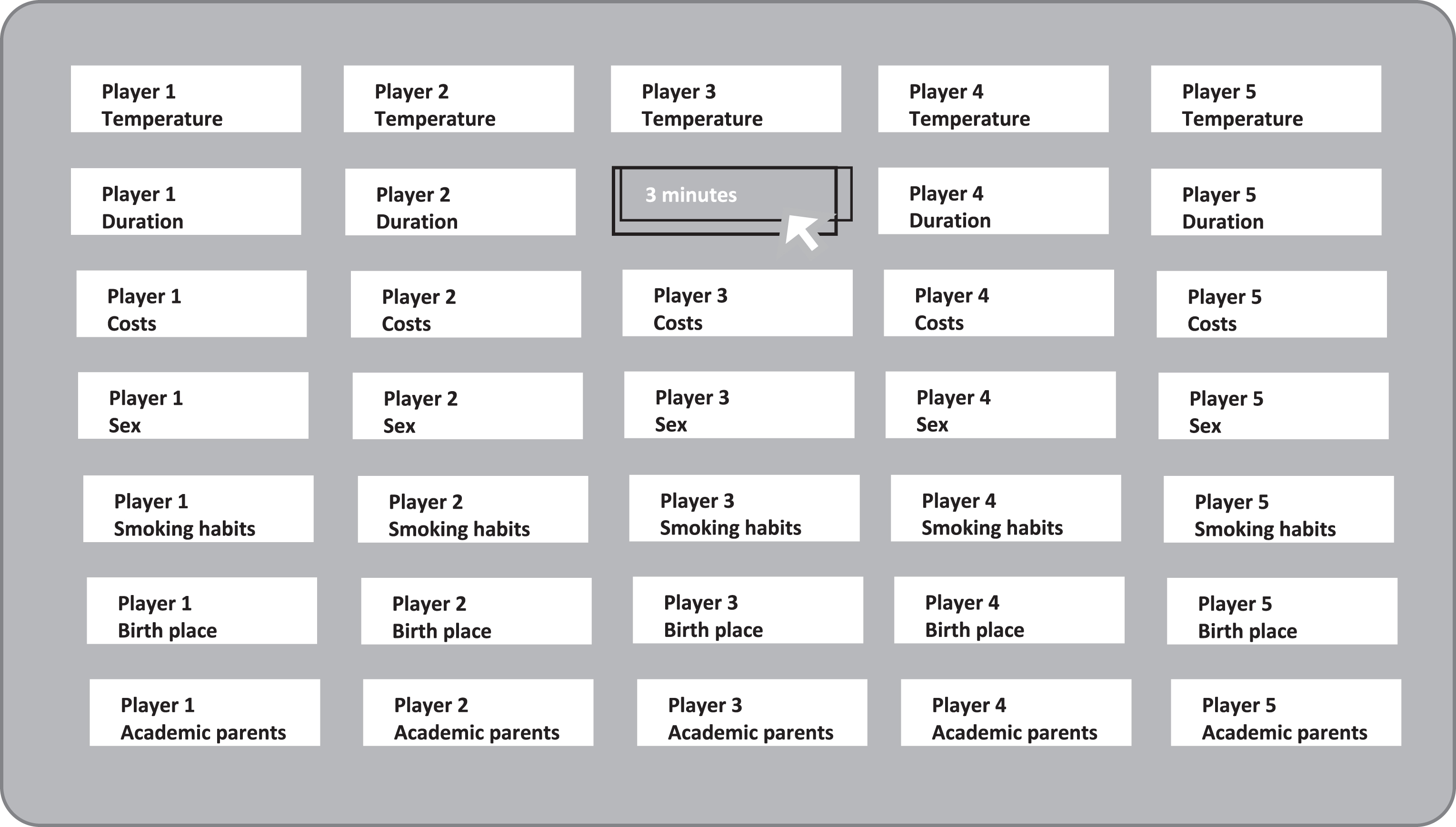
Simply moving the cursor on a button opened the concrete information for the individual in the corresponding category.
Experimental procedure
We conducted the experiments in the university medical center of the Otto-von-Guericke University Magdeburg, Germany. The entire experiment was implemented in accordance with the ethical standards of the Committee on Human Experimentation of the Otto-von-Guericke University. For each of the 16 sessions, we invited five students from various fields of study (our “patients”) and one physician with at least six months of work experience in a hospital setting. The physician and the patients were located in different rooms on the campus and never met at any time during the experiment. One experimenter led the full experiment in each room. Every room was equipped with a computer for each participant and coolers.
Patients
Upon arrival, we informed the patients that they would be involved in an experiment in which they would be subjected to real pain. We demonstrated the operation of the four coolers at different temperatures and explained the pain induction procedure. We explained that, depending on the decision of the player in the other room, some of them would endure pain. All 80 subjects agreed to participate including pain reception, none of them decided to leave the session without participation. They subsequently signed the consent form. After that, the patients randomly drew a number out of an urn. These numbers ranged from 1– 5 and denoted the water temperature (i.e., pain intensity) that the patient would be subjected to, the immersion duration, and the cost of their treatment.
All patients then read the detailed experiment instructions in their entirety to ensure they understood the full procedure. Within the experimental instructions for both, patients and physicians, we implemented neutral wording only (for example patient was replaced by player) to avoid participants to bring in stereotypes or schemes and experiences that might influence the decision-making situation.
The next stage involved collecting relevant personal background information about each patient including gender, origin, smoking habits, and their parents’ academic background. All information was directly entered into a computer that was connected to the room in which the physicians were located (Table 3).
Table 3
Experimental procedure for physicians and patients
| Room 1: Physician and Experimenter 1 | Room 2: Five patients and Experimenter 2 |
| Random allocation of immersion duration, water temperature, and costs for treatment | |
| Experimental instruction and test of water temperature | Experimental instruction and test of water temperature |
| Computer-based collection of personal background information (gender, origin, smoking habits, parents’ academic background) | |
| Rationing decisions based on the seven criteria | |
| Rating of criteria relevance for rationing decision | Treated subjects were paid for participation and left |
| Physician observed pain induction via a video camera | Untreated subjects underwent pain induction procedure |
| Physician was paid for participation and left | Untreated subjects were paid for participation and left |
Physician
The physicians were provided with an overview of their task and, like the patients, observed a demonstration of the use of a cooler to induce pain. The water temperature was 7° Celsius, which we deemed to be representative of the four different temperatures of the coolers in which the patients were asked to submerge their hands. We asked the physician to immerse one hand for 20 seconds as a means of gaining an impression of the pain intensity the patients would be subjected to and, thereby, ensuring the physicians did not underestimate the pain, which can be common in experiments of this nature.
In the meantime, the personal information of each of the five patients was shared with the physicians via Mouse Lab (Fig. 1), and the physician was subsequently asked to make his rationing decision.
Once the physician had made his decision, he was asked to complete a short questionnaire that included the seven criteria he had worked with to make his decision. The physician was then asked to evaluate which of the criteria had influenced his decision and to what extent.
Patients
As soon as the physician had made his decision, the experimenter informed the patients which of them would be going through the pain experience. Because of the restricted budget, the physicians could not select all patients but only three or four out of five. The remaining one or two patients not selected for treatment thus had to go through their disease, i. e. to experience the initially allocated pain doses. All others were paid 15 Euros and left the room. The remaining patients sat down on chairs close to the cooler that corresponded to their treatment. They immersed their hands in the water cooler of the allocated temperature as soon as the experimenter activated the stopwatch. When the different immersion durations were over, the experimenter gave a signal and one subject after the other finished the pain induction procedure. They were also paid 15 Euros and left the campus.
Physician
The physician observed the pain induction procedure by means of a video camera. To prove that we had conducted the experiment in real time, we displayed a newspaper showing the date and a mobile phone showing the time. After observing the pain induction process, the physicians were also paid 15 Euros and left the campus.
STATISTICAL ANALYSIS
Results
The average ratings for the 16 physicians are displayed in Fig. 2. As shown in Fig. 2, the three treatment-sprecific criteria, namely temperature, cost and duration of the treatment, on average appeared to be of higher relevance (relevance rating >7) than the other criteria; namely, whether the patient was a smoker and socio-demographic aspects such as birthplace, gender or academic background. The latter four criteria had relevance ratings smaller than 2.5.
Fig.2
Relevance rating of the seven criteria (ranging from 1 = no relevance to 10 = very high relevance).
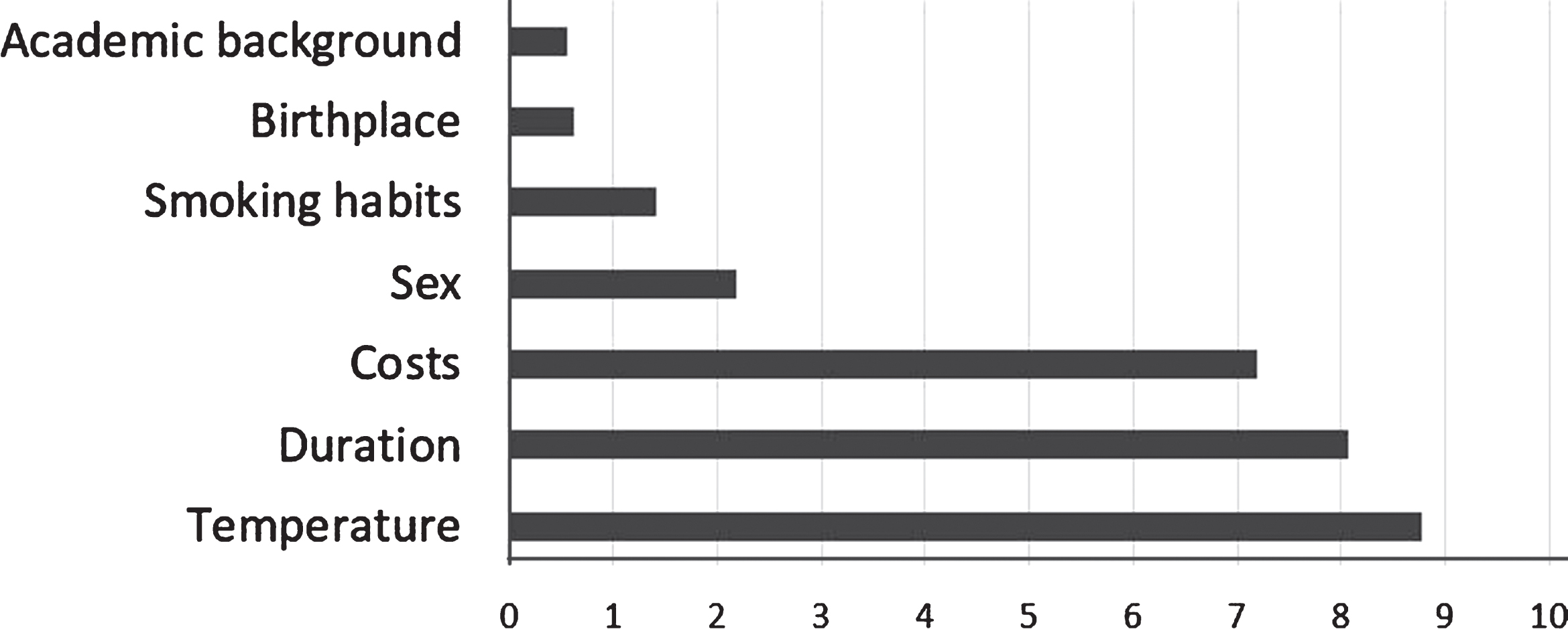
To calculate the average importance of each criterion from the physicians’ perspectives, we normalized the scores they had allocated (Fig. 2). That is, we divided each rating provided by a physician by the sum of all his ratings. This provided us with the relative importance of each criterion for the physician (see Table 4).
Table 4
Importance of criteria for the physician
| Percentage relevance of: | |||||||
| Physicians | Temperature | Duration | Costs | Gender | Smoker | Academic Background | Birthplace |
| 1 | 36.99% | 36.99% | 18.55% | 3.73% | 0.00% | 3.73% | 0.00% |
| 2 | 37.04% | 37.04% | 25.93% | 0.00% | 0.00% | 0.00% | 0.00% |
| 3 | 27.74% | 27.74% | 19.50% | 5.53% | 19.50% | 0.00% | 0.00% |
| 4 | 50.00% | 50.00% | 0.00% | 0.00% | 0.00% | 0.00% | 0.00% |
| 5 | 0.00% | 7.19% | 71.40% | 0.00% | 21.40% | 0.00% | 0.00% |
| 6 | 29.40% | 29.40% | 29.40% | 11.81% | 0.00% | 0.00% | 0.00% |
| 7 | 32.13% | 32.13% | 24.94% | 7.20% | 3.60% | 0.00% | 0.00% |
| 8 | 14.29% | 14.29% | 14.29% | 14.29% | 14.29% | 14.29% | 14.29% |
| 9 | 37.04% | 33.33% | 29.63% | 0.00% | 0.00% | 0.00% | 0.00% |
| 10 | 37.02% | 29.61% | 29.61% | 3.76% | 0.00% | 0.00% | 0.00% |
| 11 | 34.49% | 34.49% | 20.72% | 10.30% | 0.00% | 0.00% | 0.00% |
| 12 | 35.73% | 35.73% | 28.54% | 0.00% | 0.00% | 0.00% | 0.00% |
| 13 | 33.37% | 29.96% | 29.96% | 6.72% | 0.00% | 0.00% | 0.00% |
| 14 | 29.40% | 29.40% | 26.51% | 11.81% | 2.89% | 0.00% | 0.00% |
| 15 | 21.99% | 21.99% | 24.35% | 12.17% | 7.33% | 4.84% | 7.33% |
| Avg. | 30.44% | 29.95% | 26.22% | 5.82% | 4.60% | 1.52% | 1.44% |
Using the data in Table 4, we pairwise compared each criterion with the next more important criterion. We found that the relative importance of birthplace and academic background did not significantly differ (Wilcoxon Test, two-sided, Z = – 0.45, p = 0.655). Only 3 out of 16 physicians assigned these two criteria an importance greater than 0. Smoking status was not significantly more important than academic background (Wilcoxon Test, two-sided, Z = – 1.36, p = 0.173) or the patient’s birthplace (Wilcoxon Test, two-sided, Z = – 1.83, p = 0.068). The gender of the patient was significantly more important than birthplace (Wilcoxon Test, two-sided, Z = – 2.67, p = 0.008) and academic background (Wilcoxon Test, two-sided, Z = – 2.52, p = 0.012). Nevertheless, the gender of the patient was not more important than smoking habits (Wilcoxon Test, two-sided, Z = – 0.87, p = 0.386). In sum, although the participants rated gender to be more important than academic background and birthplace, there was no significant difference in the importance of smoking habits, academic background, and origin (see Table 5).
Table 5
Results of Wilcoxon Tests for all combinations of criteria (p-values followed by Z-values in brackets)
| Temperature | Duration | Costs | Gender | Smoker | Background | |
| Duration | 0.465 (– 0.73) | – | – | – | – | – |
| Costs | 0.028 (– 2.20) | 0.062 (– 1.87) | – | – | – | – |
| Gender | 0.001 (– 3.18) | 0.001 (– 3.30) | 0.001 (– 3.18) | – | – | – |
| Smoker | 0.002 (– 3.11) | 0.002 (– 3.17) | 0.002 (– 3.06) | 0.386 (– 0.87) | – | – |
| Background | 0.001 (– 3.18) | 0.001 (– 3.30) | 0.001 (– 3.18) | 0.012 (– 2.52) | 0.173 (– 1.36) | – |
| Birthplace | 0.001 (– 3.18) | 0.001(– 3.30) | 0.001 (– 3.18) | 0.008 (– 2.67) | 0.068 (– 1.83) | 0.655 (– 0.45) |
All treatment-specific aspects; i.e., temperature, duration, and costs, were perceived to be more important than the non-treatment specific aspects. Namely, the least important criterion, the costs, were significantly more important (Wilcoxon Test, two-sided, Z = – 3.18, p = 0.001) than the gender of the patient and the next more important criterion, the duration of the treatment. Both duration of the treatment (Wilcoxon Test, one-sided, Z = – 1.87, p = 0.031) and temperatue (Wilcoxon Test, two-sided, Z = – 2.20, p = 0.028) were, significantly more important than the costs. Finally, there was no difference in the importance between temperature and duration (Wilcoxon Test, two-sided, Z = – 0.73, p = 0.465).
DISCUSSION
The aim of this study was to establish how physicians make rationing decisions at the bedside; i.e., which criteria they apply in their decision-making processes. To answer the research question, we conducted an experiment with physicians who were asked to make decisions related to the well being of five subjects. Their decisions had immediate consequences for the participating subjects.
In sum, the physicians were concerned about the pain intensity, as represented by the water temperature, followed by pain duration. The cost of treatment was also relevant, but not as much. Of minor relevance was gender, while the smoking habits, origin, and academic background of parents were largely not taken into consideration during the decision-making process.
Based on expectations of social desirability [11], one could argue that this result is a little surprising and that attention, in fact, was spread quite differently. To evaluate this further, we employed the Mouse Lab software to control individual ratings.
The findings of the Mouse Lab were positively surprising. Data in terms of the frequency of criteria usage and duration were aligned with the results of the ratings. Self-assessments and objective measurements did not deviate from each other. We also found the same hierarchy here, with the cut between costs and gender being highly significant (Wilcoxon, 1% level).
The findings indicated that the physicians exhibited the ability to manage complexity when making decisions related to patient care. Physicians clearly took information that was relevant into consideration during their decision-making process and omitted aspects that were irrelevant, including factors related to the socio-economic background of the patient. The findings of the current study were different from the results of other studies that have examined the use of this type of information within prioritization and rationing decisions (Table 1). In the current study, the physicians focused on objective criteria, such as water temperature, immersion duration and costs. This is especially important as these two criteria are the same as those supported by the QALY concept (quality adjusted life years) [12, 13]. The healthcare organizations that are in operation in various countries throughout the world use this concept to make resource allocation decisions in the health care sector. To come to comparable values for different options to spend the disposable budget, related studies have investigated the expected improvement in well-being (analogous to our variation of the water temperature during the cold pressor pain) and the lifetime that is lived in the respected level of well-being (analogous to the immersion duration applied during our test). This product is then related to the necessary investments. The physicians involved in the current study also reported the use of cost information to make rationing decisions. The findings of the current study offer interesting insights in terms of the QALY concept. The experiment was conducted in Germany, a society and medical fraternity that has rejected the QALY concept because its general approach is deemed to be unethical [14]. Thus, Germany is not training prospective caregivers to adhere to this concept. However, the attitudes the physicians exhibited in the current study were aligned with the QALY concept. This is surprising and should contribute to the German discussion that implicit prioritization and rationing is an unacceptable permanent condition, especially for the physicians who are required to make important, life-changing decisions daily.
One could argue that the physicians in our experiment were directly observed in the decision-making process and, therefore, may have made the decisions they deemed to be socially acceptable. However, we believe that the fact that the Mouse Lab software confirmed the physician’s self-assessed rankings is a convincing argument against this claim. In the complex decision situation in which seven criteria need to be evaluated and applied to five cases, we believe most decision makers would not be able to fulfill the requirements of social desirability so perfectly. As such, in our opinion, there is a strong possibility that the decision process was more conscious because Mouse Lab asks the participants to actively decide which field to open.
During the decision-making process, some physicians voiced concerns that some of the female patients may suffer more pain than their male counterparts because of being exposed to the cold water. Thereby, our medical subjects further displayed their willingness to imagine how the patients must feel and, therefore, demonstrated that they were focused on arriving at the best decision possible. We think that concerns of this nature exposed the participants’ strong ability to reflect upon perspectives, situations, and options.
A potentially interesting point that would be worth investigating in more depth in future studies related to the utility increase or decrease from various levels of water temperature and immersion duration. Using McFadden’s random utility theory, it could be possible to estimate marginal rates of substitution. Unfortunately, this was not possible in the current study due to a lack of the required data.
CONCLUSION
We conclude that physicians are more rational decision makers than previous studies in this domain have claimed. When making decisions in real-life settings in which individuals instantaneously suffer or benefit from their decisions, the physicians who participated in this study consistently applied the essential criteria.
CONFLICTS OF INTEREST
The authors have no conflict of interest to report.
ACKNOWLEDGMENTS INCLUDING SOURCES OF SUPPORT
The research described in this paper was funded by the European Regional Development Fund under the operation number XXX.
REFERENCES
[1] | Strech D , Synofzik M , Marckmann G . How physicians allocate scarce resources at the bedside: A systematic review of qualitative studies. The Journal of Medicine and Philosophy. (2008) ;33: (1):80–99. doi: 10.1093/jmp/jhm007 |
[2] | Marckmann G . Priorisierung im Gesundheitswesen. Zeitschrift für Evidenz, Fortbildung und Qualität im Gesundheitswesen. (2009) ;103: (2):85–91. doi: 10.1016/j.zefq.2009.02.012 |
[3] | Diederich A , Swait J , Wirsik N . Citizen participation in patient prioritization policy decisions: An empirical and experimental study on patients’ characteristics. PloS One. (2012) ;7: (5):e36824. doi: 10.1371/journal.pone.0036824 |
[4] | Schwappach DLB . Does it matter who you are or what you gain? An experimental study of preferences for resource allocation. Health Economics (2003) ;12: (4):255–67. doi: 10.1002/hec.713 |
[5] | Stumpf S , Hecker S , Raspe H . Kriterien für die Priorisierung medizinischer Leistungen im Licht eines regionalen Surveys - Ergebnisse und methodologische Fragen. Gesundheitswesen (Bundesverband der Ärzte des Öffentlichen Gesundheitsdienstes (Germany)). (2014) ;76: (4):221–31. doi: 10.1055/s-0033-1347267 |
[6] | Winkelhage J , Schreier M , Diederich A . Explorationsstudien zur Priorisierung medizinischer Leistungen: Kriterien und Präferenzen von Ärzten und Pflegepersonal. Priorisierung in der Medizin. Jacobs University Bremen, (2009) . |
[7] | van de MortelT. Faking it: Social desirability response bias in selfreport research. Australian Journal of Advanced Nursing. (2008) ;25: (4):40–8. |
[8] | Mitchell LA , MacDonald RAR , Brodie EE . Temperature and the cold pressor test. The Journal of Pain. (2004) ;5: (4):233–7. doi: 10.1016/j.jpain.2004.03.004 |
[9] | Hines EA , Brown GE . The cold pressor test for measuring the reactibility of the blood pressure: Data concerning 571 normal and hypertensive subjects. The American Heart Journal. (1936) ;11: :1–9. |
[10] | Willemsen M , Johnson E . Mouse Lab. Decision Science News (2006) . |
[11] | Adams A , Soumerai S , Lomas J , Ross-Degnan D . Evidence of self-report bias in assessing adherence to guidelines. International Journal for Quality in Health Care. (1999) ;11: (3):187–92. doi: 10.1093/intqhc/11.3.187 |
[12] | Weinstein MC , Stason WB . Foundations of cost-effectiveness analysis for health and medical practices. The New England Journal of Medicine. (1977) ;296: (13):761–21. doi: 10.1056/NEJM197703312961304 |
[13] | Weinstein MC , Torrance G , McGuire A . QALYs: The basics. Value in Health. (2009) ;12: (Suppl 1):5–9. doi: 10.1111/j.1524-4733.2009.00515.x |
[14] | Wiedeck C . Priorisierung in der Gesetzlichen Krankenversicherung. Zugl.: Freiburg, Univ., Diss., 2012/13, Vol. 94; 2015, München, Utz. |




