Geroscience and the Fight Against Alzheimer’s Disease: Between Myth and Reality
Abstract
Aging is associated with a gradual decline in cellular stability, leading to a decrease in overall health. In the brain, this process is closely linked with an increased risk of neurodegenerative diseases, including Alzheimer’s disease. Understanding the mechanisms of brain aging is crucial for developing strategies aimed at enhancing both lifespan and health span. Recent advancements in geroscience, the study of the relationship between aging and age-related diseases, have begun to redefine our understanding of Alzheimer’s disease, guiding the development of preventive medical strategies that target the aging process itself rather than merely addressing the symptomatic manifestations of the disease.
Over the last fifty years, substantial improvements in social and health frameworks have significantly extended the human lifespan. Several factors have played pivotal roles in enhancing longevity, including advancements in healthcare, better disease control, improved nutrition, widespread vaccination efforts, medical innovations, and increased levels of education.1 These medical advancements have enriched the lives of older persons, improving their healthcare and overall life quality, which in turn has boosted the average lifespan.2
However, the extension of life expectancy has also led to a rise in chronic conditions associated with aging, including dementia, with Alzheimer’s disease (AD) accounting for 60–70%.3 More than a century ago, Alois Alzheimer first identified the distinct pathology and symptoms of a young woman with dementia. Her brain exhibited unique histopathological markers later associated with AD, described as “neuritic plaques” and “neurofibrillary tangles”.4,5 Despite extensive research, the fundamental mechanisms behind these neuropathological changes are still not fully understood, and a cure for AD is taking longer than expected.5 Promising new treatments focus on multiple targets, including, among others, amyloid processes (involving secretases, Aβ42 production, amyloid deposition, and immunotherapy), tau proteins (addressing tau phosphorylation/aggregation and immunotherapy), and neuroinflammation.6 Despite significant advancements in understanding AD’s pathophysiology, the Food and Drug Administration (FDA) has approved, since the beginning of 2000, only two new treatments, proposed as disease-modifying drugs, whose evidence of efficacy in the long run.7 This underscores the critical need for novel approaches to combat this longstanding disease.
Undoubtedly, advancing age represents the main risk factor for AD,8 except in cases of the early-onset forms, mainly due to genetic factors.9 Aging is a complex and multifactorial phenomenon characterized by a gradual decline in organ functions and an elevated risk of age-related diseases.10–13 From a biological point of view, aging is a heterogeneous process related to cumulative damage from every single cell to tissues, organs, and systems, driven by various mechanisms and pathways in part identified as the “hallmarks” of aging.11 Accumulation of damage from environmental, genetic, and lifestyle factors results in epigenetic changes, telomere shortening, DNA damage, and mitochondrial dysfunction, all leading to the induction and accumulation of senescent cells.14,15 Senescent cells, in turn, cause age-related decline by limiting stem cell and tissue regenerative capacity and increasing low-grade inflammation.15 These represent biomolecular and time-related alterations that occur during the process, facilitating studies aimed at potentially slowing down aging.11 The hallmarks of aging are characteristic of every aging cell in the body, the result being changes at the level of the different organs and systems. Interestingly, the recognized hallmarks of aging are closely linked to a heightened risk of developing neurodegenerative diseases.16 The brain, made up of both mitotic and postmitotic cells, is particularly vulnerable to the effects of aging, which are expressed as structural and cognitive changes. Brain aging typically begins in the late twenties, with about a 5% reduction in brain volume per decade after the age of 40.17 This decline is underpinned by structural and neurophysiological changes such as reductions in brain weight, neuron numbers, dendritic fields, cerebral blood flow, myelination, and synapse numbers. Age also impacts neurotransmitter levels, including those of dopamine and acetylcholine, affecting attention and memory.16
While some individuals experience healthy brain aging, many others are affected by age-associated diseases. ‘Healthy brain aging’ is characterized by absence (resistance) or abnormal aging hallmarks that remain within the body’s manageable range (resilience) and do not induce adverse effects. On the other hand, ‘pathological brain aging’ occurs when these abnormal aging markers exceed the body’s control threshold. Thus, brain aging is a highly individualized process influenced by a complex interplay of genetic, environmental, and lifestyle factors.18 Unlike chronological aging, which measures the passage of time, the rate and way the brain ages can vary significantly from one person to another. Biological aging, rather than chronological aging, is identified as a primary risk factor for AD.18,19 Recent research has shown that biological aging in mammals can be modulated and delayed.20 However, most studies on the impact of aging on clinical outcomes in humans have focused solely on chronological age.21 Geroscience seeks to understand how biological aging contributes to increased morbidity and to identify new therapeutic targets that could help maintain body function and delay the onset of age-related diseases. The field aims to leverage the pillars or hallmarks of aging to pinpoint molecular targets that could slow the aging process, thereby potentially preventing multiple diseases simultaneously.
In contrast to traditional medical research that typically addresses diseases in isolation, the geroscience approach recognizes that aging supports most chronic diseases, which often manifest concurrently in late life. Geroscience supports the concept that aging is a modifiable process and posits that successful interventions targeting disorders of aging could significantly extend lifespan, health span, and brain span. The insights gained from geroscience have profound implications for preventive medicine. Rather than targeting AD after its onset, preventive strategies can be implemented at earlier stages of life to modify risk factors associated with the aging process.22 This includes lifestyle interventions such as diet, exercise, and cognitive training. In the absence of a definite cure, patients at high risk could greatly benefit from early detection of risk factors, potentially reducing the likelihood of developing AD.23 In a few words, we need to move even in clinical practice from Panacea to Hygeia. Hygeia and Panacea, the two daughters of Asclepius, the godman of medicine, symbolize the contrast between two concepts of health that are “so close, yet so far apart”: lifestyle and medication. These concepts represent two perspectives on health. Hygeia is associated with the prevention of disease and the continuation of good health. Hygeia’s approach focuses on lifestyle choices as integral to maintaining health and preventing disease, reflecting a holistic view that health is deeply influenced by a person’s environment and habits. Panacea, on the other hand, is known for her ability to provide a remedy for every illness through a single potion or treatment, reflecting the idea of a cure-all solution. This aligns with the more modern, medicine-focused approach to health that looks to scientific advancements and pharmaceuticals to treat conditions and diseases. These two contrasting views include a broad debate in health and medicine: whether emphasis should be placed more on preventive measures, lifestyle, and environmental factors (the approach of Hygeia), or on the development and use of drugs and other medical interventions to cure diseases (the approach of Panacea). In this context, following the Hygeia track, preventive medicine is a branch of medical science focused on avoiding diseases and maintaining health rather than treating diseases once they have developed.24 This field emphasizes the overall wellness of individuals, communities, and defined populations. Its goal is to protect, promote, and maintain health and well-being and to prevent morbidity, disability, and death.
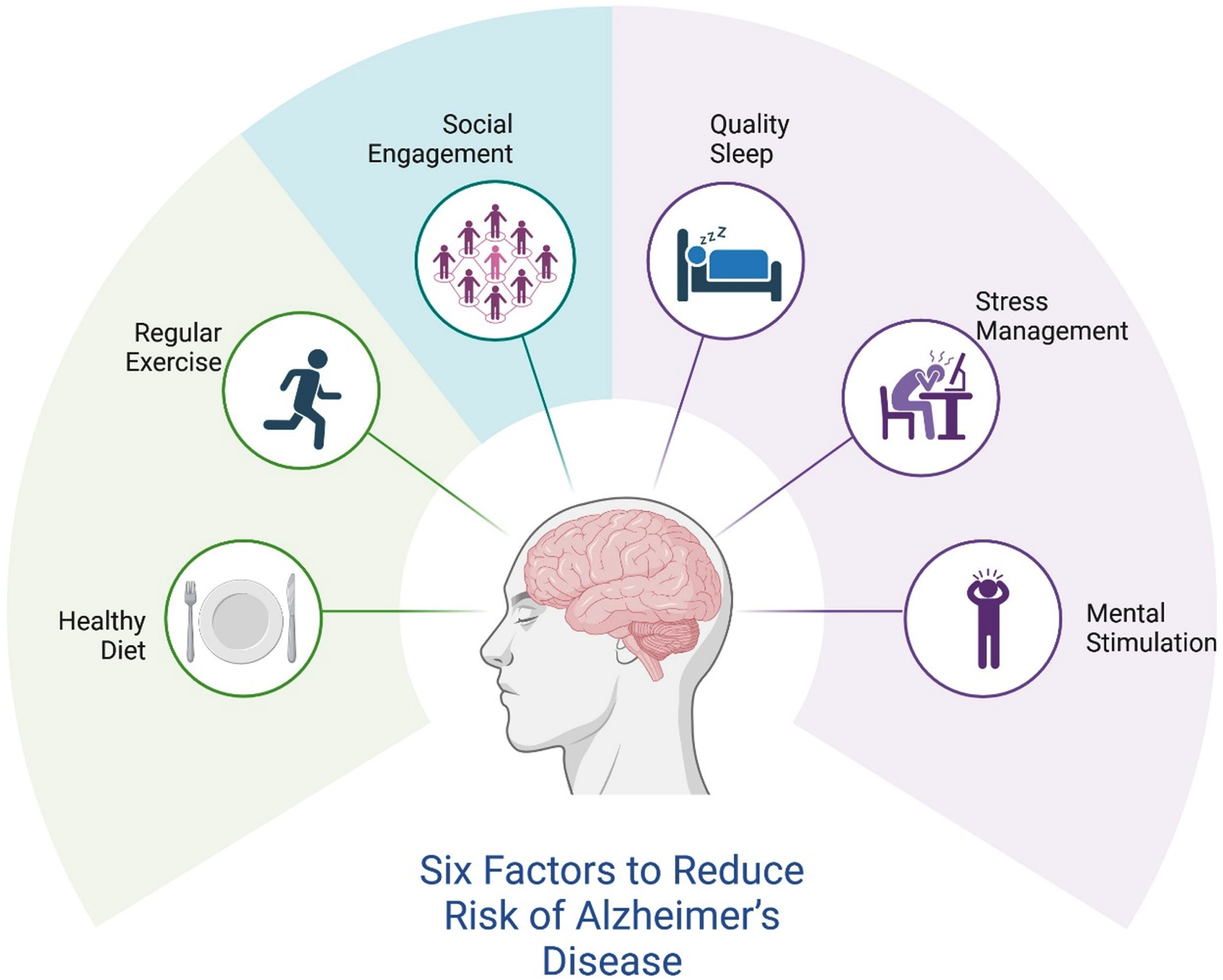
While there is currently no evident cure for AD, research suggests that specific measures might influence the disease’s progression or mitigate its risk factors, as reported in Fig. 1. A nutritious diet is crucial for maintaining brain health. The Nutrition for Dementia Prevention Working Group advises reducing intake of trans and saturated fats while increasing consumption of plant-based foods such as whole grains, seeds, nuts, and leafy green vegetables.25,26 Emphasizing foods rich in antioxidants, vitamins, and omega-3 fatty acids, like those found in the Mediterranean diet, can help lower the risk of dementia.26 Conversely, high sugar intake and foods rich in saturated and trans fats should be minimized due to their negative impact on brain health. Engaging in regular exercise, particularly aerobic activities like brisk walking for forty minutes three times a week, has been shown to protect against neurodegenerative diseases by supporting brain plasticity and neurogenesis. Moderate-intensity exercise also promotes healthier glucose metabolism in the brain, which is crucial for those at risk of AD.27 Maintaining social connections is protective against late-life dementia. Prolonged social isolation can worsen neurological health and increase the risk of dementia.28 Engaging in social activities can mitigate this risk and slow cognitive decline in those already affected by AD. Consistent, high-quality sleep is essential for brain health. Disruptions in sleep patterns can increase brain proteins linked to AD.29 Chronic stress is associated with an increased risk of cognitive impairment. Managing stress and associated mental health conditions like anxiety and depression is critical for maintaining cognitive function.30 Indeed, keeping the brain active through activities such as reading, learning new languages, or playing musical instruments helps build cognitive reserves and strengthens neural connections.31 However, most of the evidence consists of cross-sectional and correlational studies, which primarily document associations rather than establish causation. While valuable for identifying potential links, this type of evidence falls short of demonstrating direct causal relationships. Moreover, few lifestyle studies successfully eliminate the possibility of reverse causation, employ experimental designs, or utilize advanced causal inference methods. Notably, evidence shows that cognitive decline often precedes and leads to lifestyle changes such as increased social isolation, reduced physical activity, decreased mental stimulation, and poorer dietary habits, rather than these lifestyle factors causing dementia.32 This suggests that the relationship between lifestyle factors and cognitive health may be more complex and bidirectional than previously thought. Therefore, it is crucial for future research to employ more robust methodologies, including longitudinal studies that track changes over time, randomized controlled trials to establish causality, and sophisticated statistical techniques to better understand the interplay between lifestyle factors and cognitive decline. This approach will provide a clearer and more accurate picture of how lifestyle influences cognitive health and aging, ultimately leading to more effective prevention strategies. Clinically, employing precision medicine could yield definitive results in reducing risk and enhancing patient outcomes. Emphasizing early-stage clinical trials could spotlight essential risk reduction and target cognitive decline.
Fig. 1
Six key factors to reduce the risk of Alzheimer’s disease. This figure highlights six key lifestyle factors that contribute to reducing the risk of Alzheimer’s disease. Illustrated around a central brain image, the factors include healthy diet, regular exercise, social ì engagement, quality sleep, stress management and mental stimulation. Collectively, these factors emphasize the importance of physical, mental, and social well-being in maintaining cognitive health. Created with BioRender.com.
In this context, the success of the FINGER trial33 led to the launch of World-Wide FINGERS (WW-FINGERS) in 2017, involving now over 64 countries and encompassing various preventative and risk-reduction trials.34 With growing evidence supporting the efficacy of preventive measures, clinicians are encouraged to educate themselves and advise their patients on various preventive options. Until a cure is found, clinicians must utilize all available strategies to help persons combat AD. Primary care clinicians need to be motivated to identify AD risk factors and early signs of cognitive decline; recognize that reducing AD risk is feasible; and recommend practical steps toward AD risk reduction, such as adopting healthy habits. Non-dietary lifestyle changes, such as increased physical activity and social interaction, could also sharpen cognitive performances.
However, the effectiveness of lifestyle prevention for dementia is a topic of considerable debate. While there is a consensus that lifestyle factors such as physical activity, a healthy diet, and mental stimulation can contribute to cognitive health, the real-world application of these preventive measures is fraught with challenges. Initiating and maintaining significant lifestyle changes is extremely difficult. Despite the best intentions, many individuals struggle to adopt healthier behaviors. Even when changes are made, they are rarely sustained over the long term. This inconsistency in maintaining lifestyle changes significantly undermines the potential benefits of prevention strategies aimed at reducing dementia risk. Cultural differences play a substantial role in accepting and implementing lifestyle changes. Cultural norms and beliefs can influence dietary habits, attitudes toward physical activity, and perceptions of mental health. Moreover, educational level significantly impacts an individual’s ability to understand and implement health advice. Higher education levels are generally associated with better health literacy, which is crucial for making informed decisions about lifestyle changes. Individuals with lower educational attainment may struggle to understand the importance of preventive measures or how to effectively integrate them into their daily lives. This can result in lower participation rates and reduced effectiveness of lifestyle interventions in this demographic. Access to nutritious food is a fundamental component of lifestyle prevention strategies for dementia. However, many individuals, particularly those in low-income or marginalized communities, face significant barriers to accessing healthy foods. Food deserts, areas with limited availability of affordable and nutritious food, exacerbate this issue. In these areas, individuals may rely on processed and unhealthy foods that are more readily available and affordable, contributing to poor dietary habits that increase the risk of cognitive decline. Another critical issue is the demographic composition of participants in prevention trials. These studies often recruit healthy, well-educated individuals who are highly motivated to improve their health. This selective recruitment can lead to overly optimistic estimates of the effectiveness of lifestyle interventions. When these interventions are tested at scale, the benefits observed in clinical trials do not always translate to the general population. This discrepancy is particularly pronounced among those who age most rapidly-individuals who are unhealthy, have lower levels of education, and are less inclined to engage in health-promoting behaviors. Indeed, the challenges posed by climate change and its impact on healthy aging should also be considered.35 The future will be both warmer and older. Climate change exacerbates environmental stressors, such as extreme temperatures and pollution, which disproportionately affect older adults due to their increased vulnerability and existing health conditions. These stressors can worsen chronic diseases, reduce mobility, and increase the risk of heat-related illnesses, complicating efforts to maintain health and participate in clinical trials. Effective science communication must address the interconnection between environmental health and aging, while also dispelling misconceptions about conflicts between climate science and geroscience.35
To address these challenges, it is crucial to develop and test more effective interventions specifically tailored to the needs and circumstances of high-risk groups. This includes designing programs that are accessible, culturally relevant, and capable of engaging individuals who may be less motivated or have fewer resources. Additionally, these interventions should be supported by policies that create environments conducive to healthy living, such as improved access to nutritious food, safe spaces for physical activity, and educational resources. Again, it is also necessary to incorporate climate resilience into trial designs, ensure adequate infrastructure, and provide resources to support the health and well-being of older adults in the face of a changing climate. The intersection of geroscience and preventive medicine offers a revolutionary perspective in the fight against AD. By targeting the aging processes that underlie many age-related diseases, we can hope to not only delay the onset of AD but also enhance the overall quality of life for aging populations. Future research should focus on translating geroscience discoveries into practical preventive strategies and implementing them in clinical settings to effectively combat the looming AD epidemic. In conclusion, while lifestyle prevention holds promise for reducing the risk of dementia, the practical challenges of achieving and sustaining behavior change, especially among high-risk populations, cannot be overlooked. The known limitations of current prevention trials highlight the need for more inclusive research and the development of tailored interventions. Acknowledging these challenges and striving for better, more equitable solutions will enhance the effectiveness of lifestyle prevention strategies and ultimately improve cognitive health outcomes for all individuals.
AUTHOR CONTRIBUTIONS
Virginia Boccardi (Conceptualization; Resources; Writing – original draft; Writing – review & editing); Roberta Cecchetti (Methodology; Visualization); Carmelinda Ruggiero (Methodology; Visualization); Patrizia Mecocci (Supervision; Writing – review & editing).
ACKNOWLEDGMENTS
The authors have no acknowledgments to report.
FUNDING
The authors have no funding to report.
CONFLICT OF INTEREST
Patrizia Mecocci is an Editorial Board Member of this journal but was not involved in the peer-review process of this article nor had access to any information regarding its peer-review.
All other authors have no conflict of interest to report.
REFERENCES
1. | Crimmins EM . Lifespan and healthspan: Past, present, and promise. Gerontologist (2015) ; 55: : 901–911. |
2. | Barbaccia V , Bravi L , Murmura F , et al. Mature and older adults’ perception of active ageing and the need for supporting services: Insights from a qualitative study. Int J Environ Res Public Health (2022) ; 19: : 7660. |
3. | Zissimopoulos JM , Tysinger BC , St Clair PA , et al. The impact of changes in population health and mortality on future prevalence of Alzheimer’s disease and other dementias in the United States. J Gerontol B Psychol Sci Soc Sci (2018) ; 73: (Suppl_1): S38–S47. |
4. | Deture MA and Dickson DW. The neuropathological diagnosis of Alzheimer’s disease. Mol Neurodegener (2019) ; 14: : 32. |
5. | Holtzman DM , Morris JC and Goate AM. Alzheimer’s disease: The challenge of the second century. Sci Transl Med (2011) ; 3: : 77sr1. |
6. | Zhang Y , Chen H , Li R , et al. Amyloid β-based therapy for Alzheimer’s disease: Challenges, successes and future. Signal Transduct Target Ther (2023) ; 8: : 248. |
7. | Athar T , Al Balushi K and Khan SA. Recent advances on drug development and emerging therapeutic agents for Alzheimer’s disease. Mol Biol Rep (2021) ; 48: : 5629. |
8. | Boccardi V , Comanducci C , Baroni M , et al. Of energy and entropy: The ineluctable impact of aging in old age dementia. Int J Mol Sci (2017) ; 18: : 2672. |
9. | Knopman DS , Amieva H , Petersen RC , et al. Alzheimer disease. Nat Rev Dis Primers (2021) ; 7: : 33. |
10. | Tenchov R , Sasso JM , Wang X , et al. Aging hallmarks and progression and age-related diseases: A landscape view of research advancement. ACS Chem Neurosci (2024) ; 15: : 1–30. |
11. | López-Otín C , Blasco MA , Partridge L , et al. Hallmarks of aging: An expanding universe. Cell (2023) ; 186: : 243–278. |
12. | Jiménez AG . A revisiting of “the hallmarks of aging” in domestic dogs: Current status of the literature. Geroscience (2024) ; 46: : 241–255. |
13. | López-Otín C , Pietrocola F , Roiz-Valle D , et al. Meta-hallmarks of aging and cancer. Cell Metab (2023) ; 35: : 12–35. |
14. | Boccardi V and Mecocci P. Senotherapeutics: Targeting senescent cells for the main age-related diseases. Mech Ageing Dev (2021) ; 197: : 111526. |
15. | Boccardi V , Orr ME , Polidori MC , et al. Focus on senescence: Clinical significance and practical applications. J Intern Med (2024) ; 295: : 599–619. |
16. | Hou Y , Dan X , Babbar M , et al. Ageing as a risk factor for neurodegenerative disease. Nat Rev Neurol (2019) ; 15: : 565–581. |
17. | Grajauskas LA , Siu W , Medvedev G , et al. MRI-based evaluation of structural degeneration in the ageing brain: Pathophysiology and assessment. Ageing Res Rev (2019) ; 49: : 67–82. |
18. | Mattson MP and Arumugam TV. Hallmarks of brain aging: Adaptive and pathological modification by metabolic states. Cell Metab (2018) ; 27: : 1176–1199. |
19. | Lee J and Kim HJ. Normal aging induces changes in the brain and neurodegeneration progress: Review of the structural, biochemical, metabolic, cellular, and molecular changes. Front Aging Neurosci (2022) ; 14: : 931536. |
20. | Debès C , Papadakis A , Grönke S , et al. Ageing-associated changes in transcriptional elongation influence longevity. Nature (2023) ; 616: : 814–821. |
21. | Ferrucci L , Gonzalez-Freire M , Fabbri E , et al. Measuring biological aging in humans: A quest. Aging Cell (2020) ; 19: : e13080. |
22. | Kennedy BK , Berger SL , Brunet A , et al. Geroscience: Linking aging to chronic disease. Cell (2014) ; 159: : 709–713. |
23. | Cummings J , Osse AML and Kinney J. Geroscience and Alzheimer’s disease drug development. J Prev Alzheimers Dis (2023) ; 10: : 620–632. |
24. | Kaeberlein M , Rabinovitch PS and Martin GM. Healthy aging: The ultimate preventative medicine. Science (2015) ; 350: : 1191–1193. |
25. | Livingston G , Huntley J , Sommerlad A , et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet (2020) ; 396: : 413–446. |
26. | Yassine HN , Samieri C , Livingston G , et al. Nutrition state of science and dementia prevention: Recommendations of the Nutrition for Dementia Prevention Working Group. Lancet Healthy Longev (2022) ; 3: : e501–e512. |
27. | Wang S , Liu HY , Cheng YC , et al. Exercise dosage in reducing the risk of dementia development: Mode, duration, and intensity—a narrative review. Int J Environ Res Public Health (2021) ; 18: : 13331. |
28. | Penninkilampi R , Casey AN , Singh MF , et al. The association between social engagement, loneliness, and risk of dementia: A systematic review and meta-analysis. J Alzheimers Dis (2018) ; 66: : 1619–1633. |
29. | Shenker JI and Singh G. Sleep and dementia. Mo Med (2017) ; 114: : 311. |
30. | Peavy GM , Jacobson MW , Salmon DP , et al. The influence of chronic stress on dementia-related diagnostic change in older adults. Alzheimer Dis Assoc Disord (2012) ; 26: : 260–266. |
31. | Wolff L , Quan Y , Perry G , et al. Music engagement as a source of cognitive reserve. Am J Alzheimers Dis Other Demen (2023) ; 38: : 15333175231214833. |
32. | Dominguez LJ , Veronese N , Vernuccio L , et al. Nutrition, physical activity, and other lifestyle factors in the prevention of cognitive decline and dementia. Nutrients (2021) ; 13: : 4080. |
33. | Ngandu T , Lehtisalo J , Solomon A , et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. Lancet (2015) ; 385: : 2255–2263. |
34. | Kivipelto M , Mangialasche F , Snyder HM , et al. World-Wide FINGERS Network: A global approach to risk reduction and prevention of dementia. Alzheimers Dement (2020) ; 16: : 1078–1094. |
35. | Farrelly C . Geroscience and climate science: Oppositional or complementary? Aging Cell (2023) ; 22: : e13890. |




