Prevalence of Dementia and Cognitive Impairment in East Africa Region: A Scoping Review of Population-Based Studies and Call for Further Research
Abstract
Background:
Population-based research on the prevalence and determinants of dementia, Alzheimer’s disease, and cognitive impairment is scarce in East Africa.
Objective:
To provide an overview of community- and population-based studies among older adults on the prevalence of dementia and cognitive impairment in East Africa, and identify research gaps.
Methods:
We carried out a literature search using three electronic databases (PubMed, Scopus, Google Scholar) using pertinent search terms.
Results:
After screening 445 publications, we identified four publications on the population-based prevalence of dementia, and three on cognitive impairment. Prevalence rates varied from 6– 23% for dementia, and 7– 44% for cognitive impairment, among participants aged≥50–70 years. Old age and a lower education level were risk factors for dementia and cognitive impairment. Physical inactivity, lack of a ventilated kitchen, and history of central nervous system infections and chronic headache were associated with increased odds of dementia. Female sex, depression, having no spouse, increased lifetime alcohol consumption, low income, rural residence, and low family support were associated with increased odds of cognitive impairment. Potential misclassification and non-standardized data collection methods are research gaps that should be addressed in future studies.
Conclusions:
Establishing collaborative networks and partnering with international research institutions may enhance the capacity for conducting population-based studies on dementia and cognitive impairment in East Africa. Longitudinal studies may provide valuable insights on incidence, as well as potential risk and protective factors of dementia and cognitive impairment, and may inform the development of targeted interventions including preventive strategies in the region.
INTRODUCTION
Dementia is characterized by impairment in one or more cognitive domains that lead to functional decline.1 Dementia can have various causes, with the most common being Alzheimer’s disease.2Alzheimer’s disease is a neurodegenerative disease characterized by neuritic plaques, neurofibrillary tangles, and neuronal loss2,3 Cognitive impairment is an umbrella term that refers to an impairment in cognition such as memory, attention or executive function, language, and visuospatial skills.4For the purpose of this review, we mainly focused on mild cognitive impairment, which is the intermediate stage between normal cognitive aging and dementia, and is considered a high-risk state for progression to dementia. In contrast to dementia, persons with mild cognitive impairment have essentially normal functional activities.5
Dementia and cognitive impairment present significant public health challenges globally, particularly in aging populations,6,7 and can pose significant economic and caregiving burden on societies and families alike, particularly in low- and middle-income countries and regions.8 The burden of dementia is rising in Africa.9,10 In light of demographic changes and aging societies across the globe, by the end of 2050, the projected number of persons living with dementia in the eastern part of sub-Saharan Africa will increase by 357% [estimated range: 323%–395%], and this estimate is one of the highest compared to other low- and high-income countries.11However, to date, no nation in sub-Saharan Africa has developed a stand-alone or integrated national dementia strategic plan to direct the effort to improve dementia care.12
As populations continue to age and life expectancy increases, a better understanding of the prevalence of dementia and cognitive impairment is crucial for effective healthcare planning, resource allocation, and development of targeted interventions.11This is especially important in East Africa region, which has the highest number of older population compared to other regions of Africa.9 East Africa encompasses a number of countries including Burundi, Comoros, Djibouti, Ethiopia, Eritrea, Kenya, Rwanda, Seychelles, Somalia, South Sudan, Sudan, Tanzania, and Uganda.13 While East African countries share similarities in terms of sociodemographic and socioeconomic characteristics and level of healthcare systems,13 they also exhibit significant variations in lifestyle, cultural, and other factors that may be related to dementia and cognitive impairment.
Old age, lower education levels, limited access to healthcare services, and the presence of comorbid medical conditions such as hypertension and diabetes are associated with an increased risk of dementia and cognitive impairment.9,10,14–19 Cultural beliefs, stigma, and lack of awareness about dementia and cognitive impairment may also affect early detection and diagnosis, potentially leading to an underestimation of prevalence rates.20,21
Previous reviews conducted in sub-Saharan Africa showed that the reported prevalence of dementia varied substantially (range:<1%–21.6%).9,22–25 However, those reported prevalence rates may not accurately reflect the true prevalence of dementia in sub-Saharan Africa, including East, Central, West, and South Africa, for a number of reasons. For example, various cultures and languages exist within and between countries in the regions, which may have an impact on the (perceived) burden of dementia. In addition, previous reviews highlighted a number of limitations, including a lack of population-based studies, since most studies recruited participants from both patient care and population-based settings, and had an uneven representation of sub-Saharan Africa region.22–24 For instance, only four studies from East African countries were included in a previous review published in 2022.10 The projected increase in individuals living with dementia in the highly populous region of eastern sub-Saharan Africa emphasizes the need for improved characterization of the prevalence of dementia and cognitive impairment in this region. This is essential for several reasons. First, it provides a baseline for monitoring trends and projecting future healthcare needs in the region. Second, it informs policy development, allowing for the implementation of targeted interventions to improve diagnosis, treatment, and support services for affected individuals and their families. Third, it highlights the importance of research collaborations and capacity building initiatives to enhance local expertise in studying and addressing the complex factors contributing to dementia and cognitive impairment.
Therefore, the aim of this scoping review was to provide an overview of existing literature on the prevalence of dementia and cognitive impairment, and their associated factors based on population-based studies in East Africa, and to highlight research gaps that may inform future research studies and preventive strategies or initiatives in the region.
MATERIALS AND METHODS
Search strategy
We conducted a scoping review (rather than a systematic review) since we did not formulate a specific research question but aimed at providing an overview of available evidence, and highlighting research gaps. Literature search was done using three electronic databases (i.e., PubMed, Scopus, Google Scholar). The search terms included variations and combinations of pertinent keywords such as “dementia”, “cognitive impairment”, “prevalence”, and “East Africa”. Studies on the prevalence of dementia and/ or cognitive impairment conducted in East Africa and published prior to November 30, 2023 were considered in the review. We also screened reference lists of detected studies. Please refer to Supplementary Material 1 for more information on the search strategy.
Inclusion and exclusion criteria
Inclusion criteria: 1) Original studies published in English on research conducted in East African countries, i.e., Burundi, Comoros, Djibouti, Ethiopia, Eritrea, Kenya, Rwanda, Seychelles, Somalia, South Sudan, Sudan, Tanzania, and Uganda. We did not include studies published in French or any other language spoken in East Africa since we assumed that findings from pertinent epidemiological studies would be published in English rather than French or any other (local) language, and manuscripts published in French or any other (local) language likely have an English abstract which we would have detected through our search; 2) studies reporting the prevalence of dementia and/ or cognitive impairment; 3) studies conducted in community/ population-based settings; and 4) studies conducted among participants aged≥50 years. We excluded conference abstracts, commentaries, (systematic) reviews and letters to the editors.
Screening, selection, and data extraction
We used EndNote x9 software to merge search results from different databases and remove duplicates. Screening of publications by titles, abstracts and finally full texts was conducted independently by two authors (MAY and BFG). Any disagreement was resolved by discussion. A data extraction sheet was prepared and approved in consultation with the senior author (YEG). The data extraction sheet included information on first author, publication year, study setting, study design, sample size, prevalence of dementia and/ or cognitive impairment, and potential factors associated with dementia or cognitive impairment.
Data synthesis
We synthesized data and information from included studies based on the following themes: 1) prevalence of dementia (including information on the diagnostic tool/ assessment); 2) prevalence of cognitive impairment (including information on the diagnostic tool/ assessment); 3) determinants of dementia and cognitive impairment; and 4) knowledge gaps in the East Africa context.
Reporting
This scoping review followed the Preferred Reporting Items for Systematic Review and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) checklist and reporting guideline26 to ensure transparent and comprehensive reporting of the review process. The extracted data, including prevalence rates and associated risk factors, are summarized and presented in tables and text.
RESULTS
Characteristics of included studies
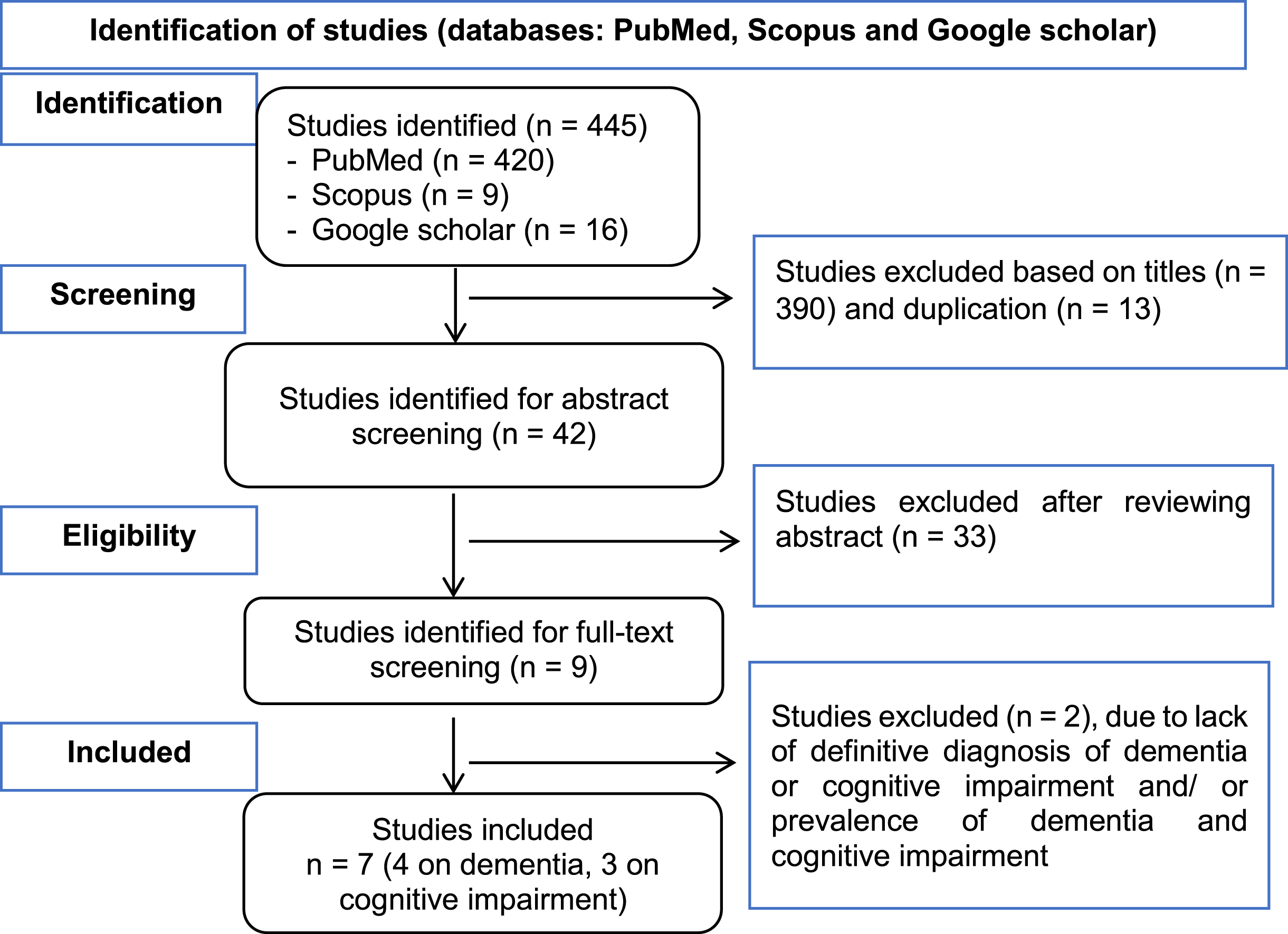
The search yielded a total of 445 studies (420 from PubMed, 9 from Scopus, and 16 from Google Scholar). Thirteen duplicate studies were removed. After title, abstract, and full-text screening, 7 studies were finally included in the review (please refer to Fig. 1 for a flow chart of the screening process). Three studies were from Tanzania,27 - 29two from Uganda,30,31 and two from Ethiopia.32,33 With regard to study design, two were follow-up (longitudinal) studies, and the remaining were cross-sectional studies.
Fig. 1
Flow chart of the selection process for the studies included in the scoping review.
Four studies reported the prevalence of dementia,28–31and three reported the prevalence of cognitive impairment.16,19,27 The age of study participants varied across studies, e.g., participants aged≥70 years were included in a study to determine the prevalence of dementia in Tanzania, while participants aged≥50 years were included in studies to determine the prevalence of dementia and cognitive impairment in Uganda and Ethiopia, respectively (Table 1).
Table 1
Reports of prevalence and risk factors of dementia and cognitive impairment in East Africa from population-based studies
| Studies on dementia | |||||||
| Authors, y | Settings | Sample size | Population | Screening tool | Diagnostic criteria | Prevalence | Risk factors |
| Longdon, 201329 | Tanzania, rural | 1,198 | ≥70 y, 56.2% female | CSI-D | DSM-IV; 10/66 Dementia research group | 6.4% (DSM-IV); 21.6% (10/66 Dementia Research Group) | Old age: aOR (95% CI) 4.0 (1.85–8.78) |
| Yoseph, 202128 | Tanzania, rural | 3,011 | ≥60 y, 57.3% female | IDEA six-item screen and IDEA IADL (brief version) | DSM-V | 6.1% (4.6% age-adjusted) in those aged≥60 y 10.2% (8.6% age-adjusted) in those aged≥70 y | Old age: aOR (95% CI) 5.06 (1.68–15.26) |
| Mubangazi, 202030 | Uganda, rural | 400 | ≥60 y, 59.5% female | Brief CSI-D | 19.5% | Old age: aOR (95% CI) 1.02 (1.01–1.03); formal education: aOR (95% CI) 0.68 (0.49–0.96); physical inactivity: aOR (95% CI) 2.27 (1.39–3.70); lack of a ventilated kitchen: aOR (95% CI) 1.35 (1.30–4.17) | |
| Benyumiza, 202331 | Uganda | 434 | ≥50 y, 65.9% female | CSID | 23.0% (95% CI, 19.2–27.3) | Old age: aOR (95% CI) 2.5 (1.5–4.1); positive history of nervous system infections (cerebral malaria: aOR (95% CI) 5.6 (2.6–12.0) and Herpes Simplex Virus-I: aOR (95% CI) 2.1 (1.1–4.1)); chronic headache: aOR (95% CI) 1.73 (1.04–2.87) | |
| Studies on cognitive impairment | |||||||
| Authors, y | Settings | Sample size | Population | Screening tool | Diagnostic criteria | Prevalence | Risk factors |
| Fekadu, 202232 | Ethiopia, Urban | 423 | ≥60 y, 38.8% female | MMSE | 42.1% (95% CI, 37.5–46.7) | Having no spouse: aOR (95% CI) 1.76 (1.08–2.86); depression: aOR (95% CI) 3.04 (1.80–5.14); lifetime alcohol use: aOR (95% CI) 2.90 (1.19–7.07); having low family support: aOR (95% CI) 3.07(1.35–6.96) | |
| Gela, 202233 | Ethiopia, Urban | 393 | ≥50 y, 42.5% female | MMSE | 43.8% (95% CI, 38.8–48.7) | Old age: aOR (95% CI) 7.03 (2.78–17.77); low literacy (inability to read and write): aOR (95% CI) 5.05 (2.04–12.50); low-income level: aOR (95% CI) 2.60 (1.26–5.20); female sex: aOR (95% CI) 2.52 (1.50–4.26); poor social support: aOR (95% CI) 2.5 (1.30–4.81); rural residence: aOR (95% CI) 2.39 (1.26–4.51) | |
| Paddick, 201527 | Tanzania, rural | 296 | ≥70 y | CSI-D | 7.0% (6.3% age-adjusted prevalence of MCI) | ||
CSI-D, Cognitive Screening Instrument for Dementia; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders IV; IDEA, Identification and Intervention for Dementia in Elderly Africans; IADL, instrumental activities of daily living; MMSE, Mini-Mental Status Exam; MCI, mild cognitive impairment; aOR, adjusted Odds Ratio; 95% CI, 95% confidence interval.
Prevalence and determinants of dementia
Two studies from Tanzania reported low population-based prevalence rates of dementia (6.1% and 6.4%), and two studies from Uganda reported slightly higher prevalence rates (19.5% and 23.0%). In the same study population using different diagnostic criteria for dementia in Tanzania, low (6.4%) and high (21%) prevalence of dementia was reported using Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV) and the 10/66 Dementia Research Group criteria, respectively. With regard to determinants examined in the studies, older age (adjusted Odds Ratio, aOR: 1.02–5.06), physical inactivity (aOR: 2.27; 95% confidence interval, CI, 1.39–3.70), and lack of a ventilated kitchen (aOR: 1.35; 95% CI, 1.30–4.17) were associated with increased odds of having dementia; whereas, formal education was associated with decreased odds of having dementia (aOR: 0.68; 95% CI, 0.49–0.96). In addition, having a history of central nervous system infections (i.e., cerebral malaria (aOR: 5.6; 95% CI, 2.6–12.0) and Herpes Simplex Virus-I (aOR: 2.1; 95% CI, 1.1-4.1)) and chronic headaches (aOR: 1.73; 95% CI, 1.04–2.87) were also reported as determinants of dementia (Table 1).
Prevalence and determinants of cognitive impairment
Two studies from Ethiopia reported high prevalence rates of cognitive impairment (42.1% and 43.8%), and one study from Tanzania reproved low prevalence of cognitive impairment (6.3%). With regard to determinants examined in the studies, older age (aOR: 7.03; 95% CI, 2.78–17.77), female sex (aOR: 2.52; 95% CI, 1.50–4.26), a lower level of literacy (aOR: 5.05; 95% CI, 2.04–12.50), having depression (aOR: 3.04; 95% CI, 1.80–5.14), having no spouse (aOR: 1.76; 95% CI, 1.08–2.86), increased lifetime alcohol consumption (aOR: 2.90; 95% CI, 1.19–7.07), and having low family support (aOR: 2.5–3.07) were associated with increased odds of having cognitive impairment. Furthermore, having low income (aOR: 2.60; 95% CI, 1.26–5.20) and rural residence (aOR: 2.39; 95% CI, 1.26–4.51) were also documented as determinants of cognitive impairment (Table 1).
DISCUSSION
Our review shows that the prevalence of dementia in East Africa based on four population-based studies ranges from 6.1% to 23%.29–31,34 Similarly, inconsistencies on prevalence estimates of dementia in population-based studies were also reported for other regions of Africa.10,23 The prevalence rates in our review are up to two times higher compared to prevalence (11.0%) reported in Southern Africa.35Relatively lower prevalence rates of dementia have also been reported in Western Africa, i.e., Benin (2.6% –3.7%)36,37 and Nigeria (4.9%),38and in Central Africa Republic (7.6%–8.1%).39,40 The prevalence of dementia is also reported to vary in Eastern Mediterranean countries, e.g., 3.8% and 14.3% in Egypt, and 12.2% in Morocco.41 These geographical variations in the prevalence estimates of dementia could be due to different diagnostic criteria used, and/ or methodology employed,19 including also linguistic differences in how symptoms are described in native languages. Furthermore, differences in prevalence rates might also be attributed to potentially modifiable risk factors that may vary between regions, such as proportion of education level, physical activity and social support.9,42
In addition to dementia, our review also includes three studies on the population-based prevalence of cognitive impairment in East Africa, with rates ranging from 7% to 44%. Interestingly, the prevalence of cognitive impairment in Tanzania (6.3%) among community-dwelling persons aged≥70 years was considerably lower than in Ethiopia (43%) among persons aged≥50 years. This large variation is in part attributable to misclassification bias as the study in Ethiopia used only Mini-Mental-Status Examination, a screening instrument which was not designed to diagnose cognitive impairment. Similar to dementia, inconsistent findings on the prevalence of cognitive impairment in population-based studies were also reported in other regions of Africa, e.g., Benin (10.2%),36 Congo (28.5%),19 the Central African Republic (37.9%),39 Nigeria (20.9%),43 Cameroon (33.3%),17 and South Africa (16.9%).44 Variations and differences in prevalence estimates across studies might be due to different diagnostic tools used to assess cognitive impairment, lack of established criteria for cognitive impairment (like they exist for dementia), and socio-demographic and economic differences between participants from different studies. For example, a community screening interview was used for studies in Central Africa Republic and Republic of Congo, and the Mini-Mental-Status Examination was used in Ethiopia. In addition, the age of included participants ranged considerably between studies. For example, individuals aged≥50 years were included in the studies conducted in Ethiopia32 and Cameroon,17while individuals aged≥60 years were included in another study in Ethiopia,33 and individuals aged≥65 years were included in the study in Benin.36
In our review, old age (with aOR ranging between 1.02 and 7.03) is a common, non-modifiable risk factor of dementia30,31,34 and cognitive impairment,33 which is consistent with prior research.10,35,44 Potential mechanisms underlying the association between higher age and increased risk of cognitive impairment and dementia have been discussed in the literature, including but not limited to a decrease in neurotransmitters, gray matter volume, and neocortical synapses as a result of aging.45,46 Cerebrovascular reactivity is also impaired with increasing age, which may result in brain hypoperfusion,47and the risk of having multimorbidity increases, which may in turn increase the risk of cognitive impairment and dementia.9,48
In addition, female sex was associated with increased odds of cognitive impairment, which is also consistent with previous studies.9,10,17–19 Observed sex differences in cognitive impairment and decline may be due to a variety of factors such as socioeconomic (e.g., literacy, income and and longevity), lifestyle, geographic, and environmental factors.18 Cognitive changes and complaints are also more common during menopause due to changes in sex hormone levels which have an impact on brain health and cognitive function.49 In addition, age at menopause and presence of hormone replacement therapy are associated with incidence of vascular cognitive impairment.50 In our review, high rates of illiteracy along with low income was common among females. On the other hand, females tend to live longer than males which may result in higher prevalence of cardiovascular diseases,9 and may impact the risk of cognitive impairment.
In the studies conducted in Tanzania and Uganda, low educational attainment was associated with increased odds of having dementia, and low formal education was also one modifiable risk factor for cognitive impairment in this review. Conflicting findings on the association between education and dementia have been reported in the literature,29,35,51,52 which may be due to differences in informal lifestyle choices shaped by culture that are thought to be protective against cognitive decline.
Physical inactivity, lack of a ventilated kitchen, and history of central nervous system infection and chronic headaches were also associated with increased odds of dementia in our review. Previous studies reported inconsistent findings on the association between these factors and dementia,53–58and more research is thus required. In addition, human immunodeficiency virus may be another important factor to consider in future studies, since rates of infection and access to treatment are relevant to dementia prevalence in East Africa, and should thus be considered in a holistic assessment of dementia prevalence rates. Finally, in this review, presence of depression, having no spouse, increased lifetime alcohol consumption, low income, rural residence and low family support were associated with increased odds of cognitive impairment, which has also been reported by otherstudies.14,42,59–62
Epigenetic alterations have been associated with dementia and cognitive impairment, especially at the level of DNA methylation, and such changes may help explain the observed interindividual variability in the development of these pathologies.63,64 Studies on the design of epigenetic biomarkers for disease detection, and for developing therapeutic strategies to improve cognitive impairment and dementia course are important.64 However, except for a convenience sample study that reported an APOE candidate gene in East Africa,65to the best of our knowledge, there is no population-based genetics or epigenetics research on dementia and cognitive impairment in East Africa. Indeed, such studies are needed to address the public health challenges of dementia and cognitive impairment.
Of note, only four studies on the prevalence of dementia, and three studies on the prevalence of cognitive impairment conducted in East Africa were included in this review. In addition, data has come from only three countries (i.e., Tanzania, Uganda, Ethiopia) out of 13 countries in the region. Thus, the conclusions derived from our review may not be regarded as representative for the entire East Africa region, and may need to be revised as more research on the prevalence of dementia and cognitive impairment conducted in East Africa becomes available in the future. The sparsity of studies might be due to lack of experts in related fields (i.e., neurologists, gerontologists and neuropsychologists),66,67 and less priority given to cognitive impairment and dementia by healthcare stakeholders in East African countries. As stated in the introduction, no nation in the sub-Saharan Africa region, which includes East Africa, has a stand-alone or integrated national dementia strategy to direct efforts to enhance dementia prevention or care nationally.9,10,68
This review therefore highlights the pressing need of research by employing rigorous methodology, including but not limited to the design and conduct of well-designed, population-based, observational studies such as cross-sectional and prospective cohort studies, and the use of standardized and validated diagnostic criteria including cognitive assessment, preferably by a neuropsychologist fluent in the native language, to establish a more accurate understanding of the prevalence and ultimately, the burden of dementia and cognitive impairment in the East Africa region. Population-based studies play a crucial role in providing reliable estimates of the prevalence of these conditions within a defined population, and findings may inform public health policies, healthcare planning, and resource allocation. Such studies also allow for comparisons between different regions and populations, contributing to a comprehensive understanding of dementia and cognitive impairment, in Africa and globally. Finally, population-based studies are resource intensive and require expertise from researchers with regard to their design and conduct. Collaborative efforts among researchers, healthcare institutions, governmental bodies in East Africa, and international investigators and research institutions may thus be vital for successfully conducting population-based studies on dementia and cognitive impairment in East Africa. Such collaborations may facilitate access to resources, expertise, and funding necessary for conducting large-scale studies. Engaging local communities and stakeholders throughout the research process is critically important to enhance the relevance, acceptability, and impact of the studies, ultimately leading to improved healthcare outcomes.
Furthermore, using advanced methods such as neuroimaging, biomarker ascertainment and genetics are also vital for identifying potential risk or protective factors associated with cognitive impairment and dementia, and for devising prevention and therapeutic strategies. In addition, the overall burden of dementia with regard to economic cost or social impact is also under-researched in East Africa. Longitudinal studies that follow individuals over time to understand the progression of dementia and its impact on individuals, families, caregivers, and communities are thus recommended.
In conclusion, only few population-based studies on the prevalence and potential determinants of dementia and cognitive impairment exist in East Africa, with prevalence rates ranging considerably across countries. Non-modifiable (i.e., age, female sex) and modifiable factors (i.e., lower level of education, chronic diseases, depression, physical inactivity, lack of a ventilated kitchen, history of central nervous system infection, chronic headaches, having no spouse, increased lifetime alcohol consumption, low family support) were documented as determinants of dementia and cognitive impairment in these studies. Governments, international organizations, and research institutions should allocate funding for population-based studies on dementia and cognitive impairment in East Africa. Establishing collaborative research networks in Africa, and partnering with international investigators and research institutions may enhance the capacity and expertise for conducting population-based studies on dementia and cognitive impairment. Longitudinal studies on dementia and cognitive impairment may provide valuable insights on incidence rates and risk factors of dementia and cognitive impairment, and may inform the development of targeted interventions including preventive strategies.
AUTHOR CONTRIBUTIONS
Muluken A. Yenesew (Conceptualization; Data curation; Investigation; Methodology; Visualization; Writing – original draft); Janina Krell-Roesch (Writing – review & editing); Betelhem Fekadu (Conceptualization; Data curation; Investigation; Methodology; Supervision; Writing – review & editing); Dabere Nigatu (Data curation; Writing – review & editing); Aklilu Endalamaw (Data curation; Investigation; Writing – review & editing); Alemtsehay Mekonnen (Writing – review & editing); Mulugeta Biyadgie (Writing – review & editing); Gizachew Y. Wubetu (Writing – review & editing); Alemu T. Debiso (Writing – review & editing); Kassu M. Beyene (Writing – review & editing); Teshome S. Kelkile (Writing – review & editing); Daniel A. Enquobahrie (Writing – review & editing); Tesfaye B. Mersha (Writing – review & editing); Danielle E. Eagan (Writing – review & editing); Yonas E. Geda (Conceptualization; Investigation; Methodology; Supervision; Writing – review & editing).
ACKNOWLEDGMENTS
The authors have no acknowledgments to report.
FUNDING
Dr. Geda receives funding from Barrow Neurological Foundation and NIH (AG057708, AG069453).
CONFLICT OF INTEREST
The authors have no conflict of interest to report.
DATA AVAILABILITY
The studies included in this review are available from databases PubMed, Scopus, and Google Scholar.
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JAD-240381.
REFERENCES
1. | Cipriani G , Danti S , Picchi L , et al. Daily functioning and dementia. Dement Neuropsychol (2020) ; 14: : 93–102. |
2. | Soria Lopez JA , González HM and Léger GC . Alzheimer’s disease. Handb Clin Neurol (2019) ; 167: : 231–255. |
3. | Griffiths J , Kikafunda J , Musisi S , et al. Brain degeneration and dementia in Sub-Saharan Africa. New York: Springer, (2015) . |
4. | Sarraf S , Desouza DD , Anderson J , et al. MCADNNet: recognizing stages of cognitive impairment through efficient convolutional fMRI and MRI neural network topology models. IEEE Access (2019) ; 7: : 155584–155600. |
5. | Petersen RC . Mild cognitive impairment as a diagnostic entity. J Intern Med (2004) ; 256: : 183–194. |
6. | Pérez Palmer N , Trejo Ortega B and Joshi P Cognitive impairment in older adults: epidemiology, diagnosis, and treatment. Psychiatr Clin North Am (2022) ; 45: : 639–661. |
7. | Shih DC , Silver R , Henao OL , et al. Incorporating COVID-19 into acute febrile illness surveillance systems, Belize, Kenya, Ethiopia, Peru, and Liberia, 2020–2021. Emerg Infect Dis (2022) ; 28: : S34–S41. |
8. | Gao Y and Liu X . Secular trends in the incidence of and mortality due to Alzheimer’s disease and other forms of dementia in China From 1990 to 2019: an age-period-cohort study and joinpoint analysis. Front Aging Neurosci (2021) ; 13: : 709156. |
9. | Alzheimer’s Disease International. Dementia in sub-Saharan Africa: Challenges and opportunities. (2017) Alzheimer’s Disease International (ADI), London. September 2017. |
10. | Akinyemi RO , Yaria J , Ojagbemi A , et al. Dementia in Africa: Current evidence, knowledge gaps, and future directions. Alzheimers Dement (2022) ; 18: : 790–809. |
11. | GBD 2019 Dementia Forecasting Collaborators. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health (2022) ; 7: : e105–e125. |
12. | Ayele BA , Ali S , Anbessie M , et al. The need for a tailored national dementia plan in Ethiopia: A call for action. Front Neurol (2023) ; 14: : 1126531. |
13. | The African Development Bank (AfDB) Group. East Africa Regional Overview. https://www.afdb.org/en/countries/east-africa/east-africa-overview. Acessed date: January 8 2024. |
14. | Han F , Luo C , Lv D , et al. Risk factors affecting cognitive impairment of the elderly aged 65 and over: a cross-sectional study. Front Aging Neurosci (2022) ; 14: : 903794. |
15. | Zhang Y-R , Xu W , Zhang W , et al. Modifiable risk factors for incident dementia and cognitive impairment: An umbrella review of evidence. J Affect Disord (2022) ; 314: : 160–167. |
16. | Nianogo RA , Rosenwohl-Mack A , Yaffe K , et al. Risk factors associated with Alzheimer disease and related dementias by sex and race and ethnicity in the US. JAMA Neurol (2022) ; 79: : 584–591. |
17. | Tianyi FL , Agbor VN , Njamnshi AK , et al. Factors associated with the prevalence of cognitive impairment in a rural elderly Cameroonian population: a community-based study in Sub-Saharan Africa. Dement Geriatr Cogn Disord (2019) ; 47: : 104–113. |
18. | Levine DA , Gross AL , Briceño EM , et al. Sex differences in cognitive decline among US adults. JAMA Network Open (2021) ; 4: : e210169. |
19. | Mavrodaris A , Powell J and Thorogood M Prevalences of dementia and cognitive impairment among older people in sub-Saharan Africa: a systematic review. Bull World Health Organ (2013) ; 91: : 773–783. |
20. | Naylor R , Vaitheswaran S , Nyame S , et al. Dementia in Sub-Saharan Africa, Asia and Latin America. In: Selin H (ed) Aging Across Cultures: Growing Old in the Non-Western World. Cham: Springer International Publishing, (2021) , pp.367–383. |
21. | Burkinshaw K , Tsourtos G and Cations MJ System and policy-level barriers and facilitators for timely and accurate diagnosis of young onset dementia. Int J Geriatr Psychiatry (2023) ; 38: : e5859. |
22. | Lekoubou A , Echouffo-Tcheugui JB and Kengne AP Epidemiology of neurodegenerative diseases in sub-Saharan Africa: a systematic review. BMC Public Health (2014) ; 14: : 653. |
23. | Olayinka OO and Mbuyi NN Epidemiology of dementia among the elderly in Sub-Saharan Africa. Int J Alzheimers Dis (2014) ; 2014: : 195750. |
24. | George-Carey R , Adeloye D , Chan KY , et al. An estimate of the prevalence of dementia in Africa: A systematic analysis. J Glob Health (2012) ; 2: : 020401. |
25. | Ojagbemi A , Okekunle AP and Babatunde O Dominant and modifiable risk factors for dementia in Sub-Saharan Africa: a systematic review and meta-analysis. Front Neurol (2021) ; 12: : 627761. |
26. | Tricco AC , Lillie E , Zarin W , et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med (2018) ; 169: : 467–473. |
27. | Paddick SM , Kisoli A , Samuel M , et al. Mild cognitive impairment in rural Tanzania: prevalence, profile, and outcomes at 4-year follow-up. Am J Geriatr Psychiatry (2015) ; 23: : 950–959. |
28. | Yoseph M , Paddick SM , Gray WK , et al. Prevalence estimates of dementia in older adults in rural Kilimanjaro 2019–2010 and 2018–2019: is there evidence of changing prevalence? Int J Geriatr Psychiatry (2021) ; 36: : 950–959. |
29. | Longdon AR , Paddick SM , Kisoli A , et al. The prevalence of dementia in rural Tanzania: a cross-sectional community-based study. Int J Geriatr Psychiatry (2013) ; 28: : 728–737. |
30. | Mubangizi V , Maling S , Obua C , et al. Prevalence and correlates of Alzheimer’s disease and related dementias in rural Uganda: cross-sectional, population-based study. BMC Geriatr (2020) ; 20: : 48. |
31. | Benyumiza D , Kumakech E , Gutu J , et al. Prevalence of dementia and its association with central nervous system infections among older persons in northern Uganda: cross-sectional community-based study. BMC Geriatr (2023) ; 23: : 551. |
32. | Fekadu B , Tareke M , Tadesse M , et al. Neurocognitive impairment and associated factors among elderly in the Bahir Dar City administration, Northwest Ethiopia. Front Aging Neurosci (2022) ; 14: : 888704. |
33. | Gela YY , Fekadu SA , Belsti Y , et al. Cognitive impairment and associated factors among mature and older adults living in the community of Gondar town, Ethiopia, 2020. Sci Rep (2022) ; 12: : 7545. |
34. | Tafesse T , Yoseph A , Mayiso K , et al. Factors associated with stunting among children aged 6– 59 months in Bensa District, Sidama Region, South Ethiopia: unmatched case-control study. BMC Pediatr (2021) ; 21: : 551. |
35. | de Jager CA , Msemburi W , Pepper K , et al. Dementia prevalence in a rural region of South Africa: a cross-sectional community study. J Alzheimers Dis (2017) ; 60: : 1087–1096. |
36. | Guerchet M , Houinato D , Paraiso MN , et al. Cognitive impairment and dementia in elderly people living in rural Benin, west Africa. Dement Geriatr Cogn Disord (2009) ; 27: : 34–41. |
37. | Paraïso MN , Guerchet M , Saizonou J , et al. Prevalence of dementia among elderly people living in Cotonou, an urban area of Benin (West Africa). Neuroepidemiology (2011) ; 36: : 245–251. |
38. | Adeloye D , Auta A , Ezejimofor M , et al. Prevalence of dementia in Nigeria: a systematic review of the evidence. J Glob Health Rep (2019) ; 3: : e2019014. |
39. | Guerchet M , M’Belesso P , Mouanga AM , et al. Prevalence of dementia in elderly living in two cities of Central Africa: the EDAC survey. Dement Geriatr Cogn Disord (2010) ; 30: : 261–268. |
40. | Guerchet M , Mouanga AM , M’Belesso P , et al. Factors associated with dementia among elderly people living in two cities in Central Africa: the EDAC multicenter study. J Alzheimers Dis (2012) ; 29: : 15–24. |
41. | Yaghmour SM , Bartlett R and Brannelly T Dementia in Eastern Mediterranean countries: a systematic review. Dementia (2018) ; 18: : 2635–2661. |
42. | Livingston G , Sommerlad A , Orgeta V , et al. Dementia prevention, intervention, and care. Lancet (2017) ; 390: : 2673–2734. |
43. | Adebiyi AO , Ogunniyi A , Adediran BA , et al. Cognitive impairment among the aging population in a community in Southwest Nigeria. Health Educ Behav (2016) ; 43: : 93s–99s. |
44. | Ramlall S , Chipps J , Pillay BJ , et al. Mild cognitive impairment and dementia in a heterogeneous elderly population: prevalence and risk profile. Afr J Psychiatry (Johannesbg) (2013) ; 16: : doi:10.4314/ajpsy.v16i6.58. |
45. | Legdeur N , Heymans MW , Comijs HC , et al. Age dependency of risk factors for cognitive decline. BMC Geriatr (2018) ; 18: : 187. |
46. | Harada CN , Natelson Love MC and Triebel KL Normal cognitive aging. Clin Geriatr Med (2013) ; 29: : 737–752. |
47. | Georgiadis D , Sievert M , Cencetti S , et al. Cerebrovascular reactivity is impaired in patients with cardiac failure. Eur Heart J (2000) ; 21: : 407–413. |
48. | Ndubuisi NE Noncommunicable diseases prevention in low- and middle-income countries: an overview of Health in All Policies (HiAP). Inquiry (2021) ; 58: : 46958020927885. |
49. | Conde DM , Verdade RC , Valadares ALR , et al. Menopause and cognitive impairment: A narrative review of current knowledge. World J Psychiatry (2021) ; 11: : 412–428. |
50. | Compton J , van Amelsvoort T and Murphy D HRT and its effect on normal ageing of the brain and dementia. Br J Clin Pharmacol (2001) ; 52: : 647–653. |
51. | Vadikolias K , Tsiakiri-Vatamidis A , Tripsianis G , et al. Mild cognitive impairment: effect of education on the verbal and nonverbal tasks performance decline. Brain Behav (2012) ; 2: : 620–627. |
52. | Lövdén M , Fratiglioni L , Glymour MM , et al. Education and cognitive functioning across the life span. Psychol Sci Public Interest (2020) ; 21: : 6–41. |
53. | Chang KH , Chang MY , Muo CH , et al. Increased risk of dementia in patients exposed to nitrogen dioxide and carbon monoxide: a population-based retrospective cohort study. PloS One (2014) ; 9: : e103078. |
54. | Zhang B , Weuve J , Langa KM , et al. Comparison of particulate air pollution from different emission sources and incident dementia in the US. JAMA Intern Med (2023) ; 183: : 1080–1089. |
55. | Rosa-Gonçalves P , Ribeiro-Gomes FL and Daniel-Ribeiro CT Malaria related neurocognitive deficits and behavioral alterations. Front Cell Infect Microbiol (2022) ; 12: : 829413. |
56. | Lopatko Lindman K , Hemmingsson ES , Weidung B , et al. Herpesvirus infections, antiviral treatment, and the risk of dementia— a registry-based cohort study in Sweden. Alzheimers Dement (N Y) (2021) ; 7: : e12119. |
57. | Qu H , Yang S , Yao Z , et al. Association of headache disorders and the risk of dementia: meta-analysis of cohort studies. Front Aging Neurosci (2022) ; 14: : 804341. |
58. | Wilker EH , Osman M and Weisskopf MG Ambient air pollution and clinical dementia: systematic review and meta-analysis. BMJ (2023) ; 381: : e071620. |
59. | Dasgupta A , Ghose S , Paul B , et al. Cognitive impairment and its predictors: A cross-sectional study among the elderly in a rural community of West Bengal. J Family Med Prim Care (2020) ; 9: : 4603–4612. |
60. | Waldron N , Laws H , James K , et al. The prevalence of cognitive impairment among older adults in Jamaica. WIMJ Open (2015) ; 2: : 71. |
61. | Chen LY , Wu YH , Huang CY , et al. Predictive factors for dementia and cognitive impairment among residents living in the veterans’ retirement communities in Taiwan: Implications for cognitive health promotion activities. Geriatr Gerontol Int (2017) ; 17: Suppl 1: 7–13. |
62. | Han R , Tang Z and Ma L Related factors of cognitive impairment in community-dwelling older adults in Beijing Longitudinal Study of Aging. Aging Clin Exp Res (2019) ; 31: : 95–100. |
63. | Pérez RF , Alba-Linares JJ , Tejedor JR , et al. Blood DNA methylation patterns in older adults with evolving dementia. J Gerontol A Biol Sci Med Sci (2022) ; 77: : 1743–1749. |
64. | Wu S , Yang F , Chao S , et al. Altered DNA methylome profiles of blood leukocytes in Chinese patients with mild cognitive impairment and Alzheimer’s disease. Front Genet (2023) ; 14: : 1175864. |
65. | Sayi JG , Patel NB , Premkumar DR , et al. Apolipoprotein E polymorphism in elderly east Africans. East Afr Med J (1997) ; 74: : 668–670. |
66. | Kissani N , Liqali L , Hakimi K , et al. Why does Africa have the lowest number of Neurologists and how to cover the gap? J Neurol Sci (2022) ; 434: : 120119. |
67. | Sci Dev Net. Africa’s brain specialist shortfall ‘risking lives’. Bringing science & development together through news & analysis. Access datae Decemebrer 28 2023. https://www.scidev.net/sub-saharan-africa/news/africas-brain-specialist-shortfall-risking-lives/. 2022. |
68. | Ddumba I Implementation of Global Action Plan on the Public Health Response to Dementia (GAPD) in Sub-Saharan Africa: Comprehensive reviews. Alzheimer Dement (2020) ; 16: (Supp 8):e043363. |



