Digital Technologies to Prevent Social Isolation and Loneliness in Dementia: A Systematic Review
Abstract
Background:
Dementia poses significant and sustained challenges to global society. Diagnosis can lead to increased feelings of loneliness and social isolation. People with dementia living alone are particularly at risk. Considering the growing number of technologies proposed to aid people with dementia address social isolation and loneliness, we reviewed the existing literature.
Objective:
To collate and summarize current evidence for digital technologies to prevent social isolation and loneliness for people with dementia.
Methods:
Following the PRISMA guidelines, we systematically searched five databases to identify studies of digital technologies designed to support or prevent social isolation or loneliness for people with dementia. Pre-specified outcomes included social isolation, loneliness, and quality of life. We used deductive thematic analysis to synthesize the major themes emerging from the studies.
Results:
Ten studies met our inclusion criteria where all studies reported improvements in quality of life and seven reported benefits regarding social inclusion or a reduction in loneliness. Technologies were varied across purpose, delivery format, theoretical models, and levels of personalization. Two studies clearly described the involvement of people with dementia in the study design and five technologies were available outside the research context.
Conclusion:
There is limited— but increasing— evidence that technologies hold potential to improve quality of life and reduce isolation/loneliness for people with dementia. Results presented are largely based in small-scale research studies. Involvement of people with dementia was limited and few research concepts are reaching implementation. Closer collaboration with people with dementia to provide affordable, inclusive, and person-centered solutions is urgently required.
INTRODUCTION
Over 55 million people live with dementia worldwide and this figure is expected to increase to 78 million by 2030 [1]. The condition poses significant and sustained challenges to societies on a global scale, limiting the functional ability of those affected, with wide reaching impacts across families and communities. Despite recent advances, we remain without disease modifying therapy for dementia [2, 3]. There is a continued global need to deliver high quality care across the dementia care pathway from diagnosis to end of life.
Much research has informed how to deliver high quality care for people with dementia. For example, the work of Kitwood highlights the importance of person-centered care and personhood which requires the person with dementia to be recognized as an individual with unique needs and preferences and to be treated with dignity and respect [4]. Personhood is rooted in a social context given that it is provided by the presence of others and therefore supported by inter-personal relationships [4]. The emphasis is placed on the person behind the diagnosis meaning that individuals will differ in their care needs and preferences for which tailored care is necessary. Accordingly, offering the tailored support at the right time and right place is documented in the current national dementia plans and policies that have been developed around the world [5].
Increasingly, there is a public health interest to improve delivery models of healthy aging- including to increase functional ability such as building and maintaining relationships for people with a significant ongoing loss in capacities [6]. Throughout life our social interactions help us to navigate the world, express our thoughts and feelings, and stay physically and mentally healthier [7]. The impact of social connectedness goes beyond conversations: it is about friendships, community, releasing stress and tensions, developing “belonging” and enhancing self-esteem and self-worth. While our personalities may influence how much social interaction we fundamentally “need”, many individuals do not enjoy their desired level of social connectedness. It is understood that half a million people in the United Kingdom (UK) do not see or speak to anyone for up to six days a week [8]. A diagnosis of dementia brings an increased risk of social isolation which can negatively impact quality of life (QoL) [9]. Moreover, feelings of loneliness are more likely for certain groups of people including those who live alone, and those over the age of 75 [10]. The UK Alzheimer’s Society data suggests that 62% of people with dementia who live alone feel lonely compared to 38% of all people with dementia [11]. Such issues have been further exacerbated by the recent COVID-19 pandemic, with disruption to in-person events and accompanying social restrictions [12].
Combatting social isolation in dementia is complex given the progressive and variable nature of the condition. It can be difficult for family and friends to know what kind of support to provide and when. While changes can occur quickly, people with dementia can also become socially isolated very gradually: seeing fewer people, leaving the house less frequently resulting in a loss of both independence and confidence post diagnosis [13]. Yet, it is understood that regular social interaction (even 10 minutes a day) can make a difference to overall QoL [14] but at present, the route to achieve equity in social connectedness remains unclear. There are many plausible arguments that the “digital age” could provide social benefits [15], e.g., increasing social connectedness across geographical locations, but it is unclear whether people with dementia are included as part of this narrative. For instance, in a systematic review, Heins et al. [16] showed that technology-based interventions may be able to alleviate loneliness in older people without cognitive decline, but few studies (n = 3) focused on people with dementia. Further, there was no clear conclusion regarding the effectiveness of technological interventions for people with dementia. Instead, this study highlighted a knowledge gap around the accessibility and implementation of these interventions for people with dementia [16]. Another scoping review identified a broad range of technological solutions (n = 11) for people with Alzheimer’s disease [15]. However, the authors established that none of these technologies were developed to support social connection, rather, the majority (n = 8) were developed for passively “monitoring” the person with dementia without their direct involvement. Taken collectively, a total absence of active input from people with dementia is concerning when noting the principles of Kitwood [4] (outlined above) around human rights, which is further supported by the United Nations’ Decade of Healthy Ageing [6], and a right to be respected as an individual beyond the disease itself.
Taken collectively, further work is required to collate knowledge on digital technologies used for social isolation and loneliness in dementia. Therefore, we set out to undertake a systematic review to: 1) describe the current digital technologies to \nobreak support or prevent social isolation or loneliness in people with dementia, 2) summate evidence surrounding the effectiveness of these interventions, and 3) assess the reported study quality alongside readiness for implementation.
METHODS
Search strategy
We followed the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines [17]. The protocol was registered in the International Prospective Register of Systematic Reviews under protocol number CRD42020191065 (https://www.crd.york.ac.uk/PROSPEROFILES/191065_STRATEGY_20201011.pdf). A comprehensive search was performed in the bibliographic databases CINAHL (via Ebsco), PubMed, Embase.com, APA PsycInfo (via Ebsco), and Scopus from inception to December 11, 2020 in collaboration with a medical librarian. Search terms included controlled terms (MeSH in PubMed, Emtree in Embase, CINAHL Headings and Thesaurus terms in PsycInfo). The following terms were used (including synonyms and closely related words): “dementia” and “loneliness” or “social isolation” and “eHealth” or “technology” (see Table 1). The full search strategies for all databases can be found in the supplementary materials. The search was performed without date or language restrictions. Duplicate articles were excluded using EndNote x9.2 (Clarivatetm).
Table 1
Strategy for systematic search in PubMed (adapted for other databases)
| Search | Search Term Query | Results |
| #1 | “Dementia”[Mesh] OR “dementi*”[tiab] OR “alzheimer*”[tiab] OR “mild cognitive impair*”[tiab] OR “MCI”[tiab] | 265,571 |
| #2 | “Loneliness”[Mesh] OR “Social Isolation”[Mesh] OR “Social Participation”[Mesh] OR “Community Participation”[Mesh] OR “Quality of Life”[Mesh] OR “Independent Living”[Mesh] OR “loneliness”[tiab] OR “lonely”[tiab] OR “social isolation”[tiab] OR “social engagement”[tiab] OR “social inclusion”[tiab] OR “participation”[tiab] OR “involvement”[tiab] OR “quality of life”[tiab] OR “life qualit*”[tiab] OR “living qualit*”[tiab] OR “quality of living”[tiab] OR “qol”[tiab] OR “hrql”[tiab] OR “hrqol”[tiab] OR “wellbeing”[tiab] OR “well-being”[tiab] OR “independent liv*”[tiab] | 1,031,523 |
| #3 | “Computers, handheld”[Mesh] OR “Mobile Applications”[Mesh] OR “Internet”[Mesh] OR “Robotics”[Mesh] OR “Technology”[Mesh] OR “Wearable Electronic Devices”[Mesh] OR “technolog*”[tiab] OR “mobile health*”[tiab] OR “mhealth*”[tiab] OR “m-health*”[tiab] OR “telehealth*”[tiab] OR “telehealth”[tiab] OR “digital health”[tiab] OR “app”[tiab] OR “apps”[tiab] OR “smartphone*”[tiab] OR “phone application*”[tiab] OR “telephone application*”[tiab] OR “mobile application*”[tiab] OR “health application*”[tiab] OR “internet*”[tiab] OR “world wide web*”[tiab] OR “ipad”[tiab] OR “ipads”[tiab] OR “laptop*”[tiab] OR “palmtop*”[tiab] OR “palm top*”[tiab] OR “personal digital assistant*”[tiab] OR “interactive voice response*”[tiab] OR “multimedia”[tiab] OR “Mhapps”[tiab] OR “mobile phone*”[tiab] OR “iphone*”[tiab] OR “android”[tiab] OR “game*”[tiab] OR “gaming”[tiab] OR “gamification”[tiab] OR “whatsapp*”[tiab] OR “e-coach*”[tiab] OR “wearable*”[tiab] OR “smartwatch”[tiab] OR “social media”[tiab] OR “online social network*”[tiab] OR “exergam*”[tiab] OR “serious gam*”[tiab] OR “chatbox*”[tiab] OR “chat*”[tiab] OR “robot*”[tiab | 1,085,324 |
| #4 | #1 AND #2 AND #3 | 1,329 |
Screening
All study types were included in this systematic review to be inclusive of efforts that were in an early stage of development. The title and abstract of each study were screened using Rayyan (https://www.rayyan.ai/): a specialist software tool designed for performing systematic reviews. These were reviewed by two independent reviewers according to the pre-specified inclusion/exclusion criteria. Systematic reviews of relevance were also inspected for additional studies of interest, but studies were subject to the same inclusion/exclusion criteria. Studies were screened and categorized as one of the following: ‘included’, ‘excluded’, or ‘maybe’. Where studies were classed as ‘maybe’, full texts were obtained before a decision was made on inclusion or exclusion. Disagreements were resolved through further discussion on abstracts (DK and HR). Where a decision could not be reached, the full text of the article was reviewed in detail and/or consultation with another team member took place to act as third reviewer (AMP/KE). Therefore, the final included list was generated through at least two team members independently confirming inclusion.
Inclusion criteria
• Digital technologies defined as an umbrella term for computer-based products and solutions (e.g., mHealth, eHealth, apps, online interventions) that are:
∘ developed for people with mild cognitive impairment/dementia;
∘ designed for, or have a strong rationale for hypothesized impact upon social isolation/loneliness;
∘ stand-alone or integrated into other physical materials (e.g., furniture, clothing);
∘ used by a person with dementia alone, or with support from others;
• Any trial design providing that there is a measure of social loneliness/isolation assessed;
• Studies published in English or Dutch.
Exclusion criteria
Studies were excluded if they met any of the following criteria where digital technologies were:
∘ a non-critical component of a complex intervention (e.g., the use of digital technology is not essential in the overall design);
∘ developed for older populations only (e.g., not dementia/cognitive impairment specific);
∘ used “around” the person with dementia (without their direct involvement);
∘ telephone or face-to-face-based services.
Data extraction
Data were extracted into MS Excel to describe studies in full (e.g., study design, population, intervention). Study features (e.g., human and digital elements) were thematically analyzed following Braun and Clarke’s thematic analysis [18] creating major themes across all identified studies. To appraise individual study quality, we applied the Mixed Methods Appraisal Tool (MMAT) in order to assess the quality [19] instead of the Downs and Black methodological quality checklist as stated in our original systematic review protocol. MMAT allows for the methodological appraisal of qualitative, quantitative, and mixed method studies using a single tool and provides a process to appraise using specific checklist-based criteria for each study type. MMAT was chosen as it allowed use of a single tool for all of the included studies which followed a variety of different study designs. Since it is discouraged to calculate an overall score from the ratings of each criterion [19], a description of the quality for each study is described based on the number of criteria met in each checklist. We also appraised the readiness of implementation through collecting information on the availability and accessibility of technologies. This information was either provided as part of the study or was searched for online via an online search engine.
RESULTS
Search results
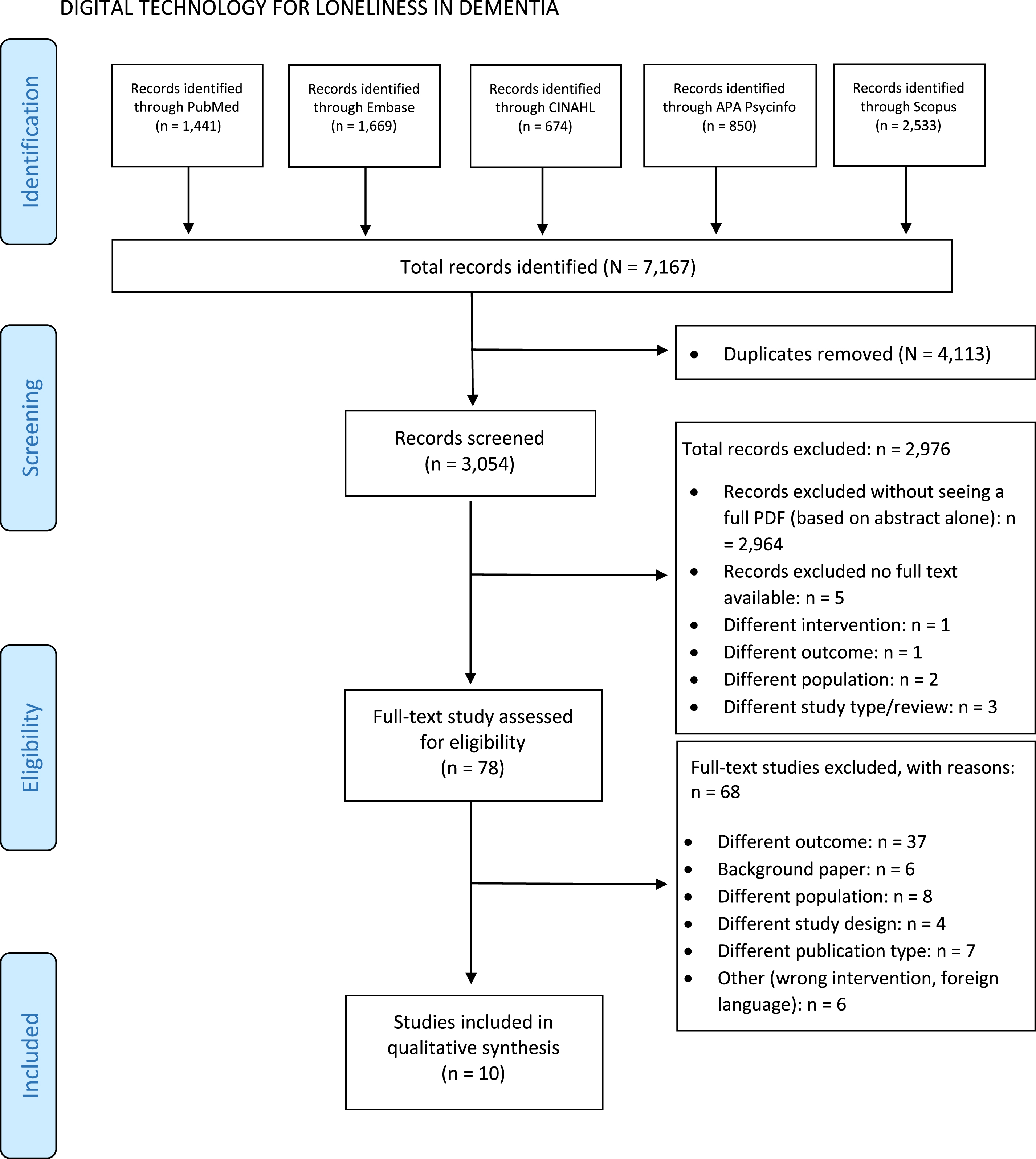
Our search identified 7,167 individual studies across five databases (see Fig. 1 for breakdown). After removal of duplicates, 3,054 studies were eligible for screening. Of these 2,976 were initially excluded, leaving 78 studies assessed as full texts. Ultimately, a total of ten studies were taken forward for analysis. Analysis of related systematic reviews did not yield any additional studies. Each study identified described a single digital technology (see below).
Fig. 1
Flow diagram of study selection.
Description of the digital technologies for social isolation and loneliness
Of the ten digital technologies described: four were categorized as humanoid and animal companion robots (MARIO, NAO, Giraff, JustoCat) [20–23], three were categorized as multi-sensory, touch-screen technology (Active Cues Tovertafel, Skype-on-Wheels, GeriJoy) [24–26], two were assistive technology systems (Assistive Home Technology (AHT) system, TV-AssistDem) [27, 28], and a single technology was based on Virtual Reality (VR, Oculus Rift) [29]. These technologies differed in terms of their purpose and delivery format, underlying theoretical models and psychological techniques, levels of personalization, co-designing with people with dementia, and accessibility and implementation as described below.
Purpose and delivery format
Digital technologies were designed for a range of different purposes, including: (i) providing companionship and/or reminiscence using digital pets or humanoid social robots (four studies) [20, 21, 23, 26]; (ii) improving communication and social connections between family members or other residents (three studies) [20, 22, 25]; (iii) improving engagement and physical activity through multi-sensory stimulation (two studies) [24, 29]; (iv) remote monitoring and support to improve well-being (one study) [27]; (v) providing support with assistive functions (one study) [28]. In terms of delivery format interventions comprised of: (i) a combination of audio, video, and pictures (five studies) [20, 22, 25–27]; (ii) immersive audio-visual stimuli or projections (two studies) [24, 29]; (iii) auditory feedback with physical movements (two studies) [21, 23]; and one intervention respectively for (iv) Live chat [27] and; (v) automated delivery of assistive functions [28].
Theoretical underpinnings and psychological techniques
Four out of ten studies described underpinning psychological theories used. This included the Tovertafel [24], JustoCat [23], NAO robot [21], and Skype-on-Wheels [25]. Bruil et al. [24] combined elements of multisensory stimulation and reminiscence therapy within the Tovertafel, including the discussion of memories and past experiences using prompts, in its activities to improve QoL [24, 30]. Reminiscence therapy also served as the framework for JustoCat: Gustafsson et al. [23] stated that a robotic cat was assumed to appeal to individuals’ memories of cats [23]. The NAO robot is based on the participatory arts model which requires the person with dementia to actively engage in ‘creating’ art rather than ‘observing’ art which may lead to a positive impact on mood and loneliness [21]. For Skype-on-Wheels, Zamir et al. [25] refer to Porges’ social engagement and attachment theory [31] which posits that face-to-face interactions are crucial for good quality social interactions and to sustain new and existing relationships [25]. The researchers also emphasize the benefits of socialization in general on cognitive functioning, e.g., being able to remember conversations.
Personalization
All ten technologies included personalization at least in part using human elements. This was achieved through the involvement of: (i) professional staff (six studies) [23–26, 28, 29], (ii) researchers (three studies) [20, 21, 27], and (iii) family carers (one study) [22]. For instance, Bruil et al. [24] involved a professional carer as part of the Tovertafel who guided people with dementia through the activities and promoted engagement with the content [24]. Similarly, for Skype-on-Wheels, a professional carer facilitated group quiz sessions by asking the questions and moving the device towards participants [25] whereas family members operated the Giraff robot remotely [22].
In addition to personalization through human involvement, six technologies included digital personalized approaches elements where all six tailored content according to individual interests and needs [23, 24, 26–29] although this was achieved in different ways. Baker et al. [29] tailored the VR experiences as part of the Oculus Rift based on individual feedback and interests and people using the technology found these personalized experiences more interesting than the existing selection. The range of activities included in the Tovertafel were pitched to individual interests and abilities and thus, could be tailored according to the stage of dementia as well [24]. Demiris et al. [26] incorporated personalized images and videos as part of GeriJoy and the touch-screen app [26]. TV-Assistdem was adapted to provide tailored support during the COVID-19 pandemic depending on the individual’s country of residence [27]. People with dementia received a personalized introduction to JustoCat from a professional carer which also involved social interactions based on a common memory (e.g., discussion on memories of having a pet cat [23]). Lastly, the different features within the AHT system could be personalized depending on the individual’s need e.g. lighting in living areas or the set-up of life circles designed to allow for residents to access different areas in the home or across the care center [28].
Co-designing with people with dementia
Two of the ten studies identified, stated that co-design with people with dementia had taken place [22, 24], whereas eight studies did not state this [20, 21, 23, 25–29]. Where such information was available (two studies) Bruil et al. [24] stated that Tovertafel was developed in collaboration with people with dementia. Similarly, Moyle et al. [22] highlighted prototypes were iteratively improved through feedback from people with dementia as part of a separate research project. However, neither of these studies describe the specific impact or the point at which people with dementia were able to make such contributions (e.g., ideation, evaluation). Within the studies, people with dementia were invited to engage with the technology independently though staff were available to provide assistance and support when needed (six studies) [21, 23, 26–29]. The remaining four studies involved group interactions as part of the intervention either with other people with dementia [24, 25] or with family and friends [20, 22].
Accessibility and implementation readiness
We appraised the accessibility of technologies initially across cost and whether they were readily available. Five technologies are available for purchase [21–25] with three having a product website containing more information about the technology [22–24]. Costs were described for two of these (USD): the NAO robot is priced at $9,000 [21] and the Giraff robot at $10,000 [22]. While the Oculus Rift retails at $300 this does not include the necessary hardware required (e.g., high-performance PC). Additionally, it was unclear whether this could be purchased with the relevant VR software preloaded for people with dementia [29]. The Skype software for Skype-on-Wheels is free to download but needed additional materials at hand, e.g., a desk chair and touch-screen tablet to create the Skype-on-Wheels device [25]. As described previously, all digital technologies described within studies require human supports at least to some extent and many have physical space requirements. While the MARIO robot [20] and JustoCat [23] could be used independently after an initial introduction, eight of ten technologies (80%) required either a family member or professional carer to be trained in its use, provide assistance with set up, and guide the intervention. Some technologies also required the involvement of engineers for installation or trouble-shooting problems (e.g., the AHT system) and adjustment to the environment can also be required [20, 24, 25]. D’Onofrio et al. [20] suggest that the MARIO robot should be used in a quiet area to minimize distractions, Tovertafel [24] requires a table big enough for at least six participants and therefore a sizable room. Physical space was also important for Skype-on-Wheels so that group participants can navigate the device between them [25]. Another consideration included a requirement for access to the Internet which was explicitly stated in three studies [22, 25, 26]. Lastly, the majority of technologies (n = 8) identified [20–25, 28, 29] have been evaluated in the care home or assisted living environment.
Study characteristics
Population
Of the ten included studies, eight were single studies that took place in a single location with one group of participants. The remainder [20, 28] involved multiple study sites. All studies were conducted in high-income country settings across a total of eight countries including the UK (one study), the Netherlands (two studies), Australia (two studies), the USA (two studies), Sweden (one study), Spain (one study), and a single multinational study taking place across the UK, Ireland, and Italy. All people with dementia who took part in the studies were aged 65 or over, where the most prevalent average age group were individuals in their mid-80 s (five studies [21–24, 28]) and mid-70 s (three studies [20, 26, 27]). Baker, et al. [29] reported an age range from 74 to 88 years, while Zamir et al. [25] only report participants as being older than 65 years. Eight out of ten studies also had a majority of female participants (range 61–100%).
Five studies [21–24, 27] reported the stage of dementia of participants where Goodman-Casanova et al. [27] and Moyle et al. [22] focused on mild dementia, Fields et al. [21] covered mild to moderate dementia, Bruil et al [24] included moderate to severe dementia, and Gustafsson et al. [23] included people in the late stages of dementia. Two out of ten studies reported the type of dementia where D’Onofrio et al. [20] only included people with Alzheimer’s disease and Lauriks et al. [28] reported over half of the participants being diagnosed with Alzheimer’s disease. The study also included individuals with mixed dementia or vascular dementia. Finally, three studies explored the participant’s familiarity with technologies: where Baker et al. [29] reported none of the participants as being familiar with common technology such as tablets or phones; Demiris et al. [26] reported 80% of participants as being ‘somewhat or very comfortable’ using technology; and Fields et al. [21] reported a majority of participants had no prior experience with the technology used in the intervention.
Local settings
The majority of the studies took place at a residential care facility, nursing home or medical ward [20–25, 28, 29] where two studies took place at the home of a person with dementia [26, 27]. The only study that required participants to travel away from their home was the UK based participants of the study by D’Onofrio et al. [20] where the workshop was conducted at a testing venue as participants lived outside the community. Participants based in Ireland and Italy completed the intervention at home.
Quality of life and social connectedness measures
All studies reported some improvement to participant QoL and/or social connectedness as a result of engaging with the technology. However, most studies were small-scale in nature with eight out of ten studies having less than 40 participants (see Table 2 for further details). QoL was recorded in all ten studies with each of them reporting benefits. Regarding the measures, seven studies [20–24, 26, 28] implemented existing tools to measure a range of metrics to determine a participant’s QoL. These include dementia specific QoL measures (Discomfort scale-Dementia of Alzheimer Type, quality of life in late-stage dementia, Quality of Life for People with Dementia, Quality of Life in Alzheimer’s Disease, self-rated Quality of Life domains) (four studies) as well as measures of metrics including: depression (Cornell Scale for Depression in Dementia, Geriatric Depression Scale, Patient Health Questionnaire-9) (three studies); emotional responses (Comfort from Digital Companion Animals Scale, the Face Scale, Observed Emotion Rating Scale) (three studies); agitation (Cohen-Mansfield Agitation Inventory) (one study); anxiety (Generalised Anxiety Disorder Assessment) (one study); loneliness (UCLA loneliness Scale) (one study); sleep quality (Medical Outcomes Study Sleep Scale) (one study); and perception of social support (Multidimensional Scale of Perceived Social Support). Further details are available in Table 2. The remaining three studies used their own methods of measuring QoL including: a custom ‘smiley face emotion’ (emoji) chart to evaluate participants responses [29]; measuring physical, intellectual, recreational, and social aspects [27]; during the intervention or extracting the results using thematic analysis [25]. Social connectedness measures were also recorded in seven of the ten studies [21, 22, 24–26, 28, 29]. These studies reported improvements to social inclusion and/or interaction (five studies) [24–26, 28, 29] as well as the reduction of loneliness and social isolation (four studies) [21–22, 25, 28].
Table 2
Study characteristics of the included papers
| Author, Year | County | Population (age, gender, and dementia) | Intervention: Digital technology | Intervention: Human element | Intervention: Setting | Comparison | Outcomes |
| Baker et al. 2020 [29] | Australia | N = 5 PwD/MCI (3 males, 2 females, aged 74–88). | Oculus Rift: VR headset with controllers that displays a range of commercial VR software. | Engaging PwD to explore VR environments to encourage them to engage more and avoid self-isolation. Participants completed the task independently though could request assistance from the observing staff when required. | Inside at residential aged care facilities. | Traditional social activities organized at the care facility. | Interactions were deemed of great interest to participants that found traditional activities uninteresting. VR was deemed as a way to encourage more participation of PwD in social activities. |
| Bruil et al. 2017 [24] | Netherlands | N = 34 PwD (13 males, 21 females, average age of 86.5, SD = 6.2) diagnosed with moderate to severe dementia. | Active Cues Tovertafel: a projector which projects animations and various games on a table. These projections respond to touch. | Group intervention for PwD and volunteers to evoke physical activity, social interaction, and a sense of wonder. | Inside the nursing home. Users interacted with the Tovertafel for 15 min every day for one week. | N/A | QUALIDEM showed a small to medium benefit one week after the intervention in the ‘negative affect’, ‘restlessness’, ‘tense behavior’ and ‘positive self-image’ subscales (p≤0.04). The DS-DAT showed improvements 1 h after the intervention compared to 15 min before the intervention (p < 0.001). |
| Demiris et al. 2017 [26] | USA | N = 10 female, community-dwelling people with MCI (average age of 78.3). | GeriJoy: Digital companion in the form of a virtual pet displayed on a tablet. | Users interact with the virtual pet via voice and touch at their leisure. Following a ‘Wizard of Oz’ approach, the virtual pet was controlled remotely by staff members. These staff members would follow an assigned script of responses that the virtual pet can perform and would also monitor the participants during the study. | Inside the participant’s home, accessible 24/7 over a 3-month period. | N/A | Findings showed reduced depressive symptoms (PHQ-9), increase in both cognition (MoCA) and positive social interactions (MOS-SS). 50% of participants described themselves as attached or very attached to the digital pet using the Comfort from Digital Companion Animals Scale. Participants with high attachment reported higher levels of anxiety using GAD-7 at the end of the intervention compared to their baseline scores. |
| D’Onofrio et al. 2019 [20] | Ireland, Italy &UK | N = 38 people with Alzheimer’s disease (14 males, 24 females, average age of 77.08, SD = 9.91). | MARIO robotic platform: a tablet PC on a robot torso that displayed apps included music, reminiscence, news, games, calendar, social engagement, and health assessment. | PwD were encouraged to interact with MARIO for 10–15 min at a time taking part in reminiscence &social engagement. Participants completed the task independently though could request assistance from the observing staff when required. | Inside nursing home in Ireland. Inside a Geriatric unit/an acute medical ward in Italy. Inside a specific testing venue in UK (participants had to travel here). | N/A | Findings showed benefits in terms of resilience (RS-14). Other outcomes included CSDD, QoL-AD, MSPSS but did not show improvements. |
| Fields et al. 2021 [21] | USA | N = 15 (4 males, 11 females, average age of 85.80, SD = 4.47). 8 without cognitive impairment (independent living) and 5 with MCI and 2 with moderate cognitive impairment (supported living). | NAO Robot: humanoid robot that can listen, speak, and perform various movements and gestures. | PwD took part in a routine with NAO and a specialist trained moderator who oversaw the session. Participants completed the task independently though could request assistance from the observing staff when required. | Inside an activity room set up specifically for the study. Sessions lasted for 10 min, 3 min guided by moderator, 7 min at leisure. | N/A | Findings showed improvements in mood using the Face Scale, loneliness using the UCLA loneliness scale and depression using the GDS. Improvements were slightly greater in those without dementia. |
| Goodman-Casanova et al. 2020 [27] | Spain | N = 93 people with MCI or mild dementia (33 males, 60 females, average age of 73.34, SD = 6.07). | TV-AssistDem: a tailored support technology for PwD delivered via TV including live chat, home exercises, and advice on how to combat COVID. | PwD were supported via a telephone support line that participants could contact at any time when help was required. | Inside participant’s home. Accessible 24/7 and at the participants leisure. | Standard treatment. | TV-AssistDem was effective as a cognitive stimulation and telehealth tool especially where face to face meetings were not possible due to COVID. Access to it and other devices that facilitate connectedness and communication may reduce feelings of isolation. |
| Gustafsson et al. 2015 [23] | Sweden | N = 4 people with late stage dementia (2 males, 2 females aged 82 to 90). | JustoCat: an interactive robot cat that responds to touch as well as being held and petted. | PwD were supported by professional caregivers as they interacted with JustoCat. Occupational therapist also supervised the professional caregivers during the intervention. | Inside the care home. Intervention was used for 7 weeks. | N/A | QUALID (QoL) and CMAI (agitated behavior): results showed improved QoL (n = 4). Qualitative interviews with relatives/carers indicated positive effects such as increased interaction, communication, stimulation, relaxation, peace, and comfort to individuals with dementia. |
| Lauriks et al. 2020 [28] | Netherlands | N = 54 PwD (includes Alzheimer’s disease, vascular dementia and multiple etiologies), 30 in test group (mean age 84.3) and 24 in control (mean age 83.1). | AHT: automated sun blinds, lighting, alerts as well as pathway lighting and life circles. | Participants used the technology at home while being supported by caregivers trained to use the technology. | Inside the care home. | Control group (no AHT). | Group homes with AHT reported positive effects using QUALIDEM and DQoL on: ‘social isolation’, ‘having things to do’, ‘aesthetics’, and ‘quality of life appreciation’ as a result of additional freedom of movement’. |
| Moyle et al. 2014 [22] | Australia | N = 5 people with mild to moderate dementia (1 male, 4 female, aged 79 to 89). | Giraff robot: telepresence robot with a screen for the person with dementia and accompanying software for family members so they can operate Giraff remotely. | Connect a family member and a PwD as a means of enhancing communication between these two parties. Staff observed user interaction and rated using the Observed Emotion Rating Scale. | Inside at long-term care facility (resident’s room or quiet common area). Used for a minimum of 6 times over a 6-week period. | N/A | The main advantage cited by family and staff was the ability of the Giraff to reduce social isolation and increase connection by enabling residents and families to “visit” each other. Enjoyment was mentioned as well by family members (observed by staff using OERS). A general state of positive emotions was observed among residents through video. |
| Zamir et al. 2020 [25] | UK | N = 22 residents, 7 with dementia or signs of cognitive decline. 15 residents without cognitive decline (5 males, 17 females, aged 65+). | Skype-on-Wheels: a wheeled device designed to hold an iPad. | PwD took part in group video calls and activities with other PwD at other care homes. These sessions were facilitated by staff who could provide assistance when required. | Inside care homes. 8 sessions total. 30 min quiz with 15–20 min Meet and Greet. | N/A | Improved peer interactions within and across care homes, e.g., forming new social contacts. In addition, improved quality of social ties with fellow residents by learning more about each other’s backgrounds and interests, which were unknown before the start of the activity. There are some qualitative findings: re-relating to others, inclusion, being able to share stories and overcoming situational loneliness. |
AHT, Assistive Home Technology; CMAI, Cohen-Mansfield Agitation Inventory; CSDD, Cornell Scale for Depression in Dementia; DS-DAT, Discomfort scale-Dementia of Alzheimer Type; DQoL, self-rated Quality of Life domains; GAD-7, Generalised Anxiety Disorder Assessment; GDS, Geriatric Depression Scale; MCI, mild cognitive impairment; MoCA, Montreal Cognitive Assessment; MOS-SS, Medical Outcomes Study Sleep Scale; MSPSS, Multidimensional Scale of Perceived Social Support; OERS, Observed Emotions Rating Scale; PHQ-9, Patient Health Questionnaire-9; PwD, people with dementia; QoL, Quality of Life; QoL-AD, Quality of Life - Alzheimer’s Disease; QUALID, quality of life in late-stage dementia; QUALIDEM, Quality of Life for People with Dementia; RS-14, 14-ITEM Resilience Scale; VR, virtual reality.
Studies reported additional measures which may have had an indirect effect on participants’ QoL or social connectedness as a result of engaging with the technology. These include potential improvements to cognition and general stimulation [23, 26, 27, 29]; reductions in feelings of depression [21, 26]; improvements to behaviors were also reported including improvements to participant’s resilience [20] self-image [24], and positive emotions [22]; and, reductions in problematic behaviors such as restlessness, agitation and tense behavior [23, 24]. One study noted participants found relaxation, peace, and comfort as a result of the robot cat intervention [23], while another study noted participants’ ‘appreciation’ and enjoyment of the ‘aesthetics’ of assistive home technologies in addition to a significant reduction of fall incidents that could lead to injuries that would impact QoL [28].
Study quality assessment
Following the MMAT procedures, studies were assessed using the following checklists: mixed methods (four studies) [22, 23, 26, 27], non-randomized studies checklist (three studies) [20, 21, 24], qualitative studies (two studies) [25, 29] and the randomized controlled trials checklist (one study) [28]. See the Supplementary Material for further information. Two of a possible ten studies (20%) met the full criteria and were considered to have high methodological quality [25, 29]; four studies (40%) met the majority of the criteria and had medium to high methodological quality [20–23], and four studies (40%) met the minority of the criteria suggesting medium to low methodological quality [24, 26–28].
DISCUSSION
Here we set out to: 1) collate current knowledge on digital technologies available to people with dementia to support or prevent social isolation or loneliness, 2) collate evidence surrounding their effectiveness, and 3) assess the reported study quality alongside readiness for implementation. To our best knowledge, this is the first work of its kind and our results suggest that there is a limited body of published work on this topic— ten studies which varied in their study characteristics such as the design and setting, and in the types of technologies such as their purpose, delivery format, and accessibility. All technologies demonstrate some level of improvements on measures of QoL with a number of improvements across outcomes regarding social inclusion, social isolation, and loneliness. However, it remains challenging to directly compare impacts because of the high level of variation surrounding technology maturity, content, and evaluation approaches. Moreover, there were some concerns that limit the generalizability of positive findings presented. These include the general lack of reported information on digital technologies in terms of the theoretical underpinnings, the absence of co-design with people with dementia, alongside barriers to accessibility and implementation, e.g., many studies require staff support. Technologies presented here are clearly complex. Human elements form a core part of delivery reflecting the work of Kitwood and Bredin [4] who state that inter-personal relationships and the presence of others are required to retain personhood which is a human right. The technologies used ranged from cutting edge/experimental (e.g., VR) to adaptation of well recognized solutions that are already in reach of many (e.g., Skype). The most common choice to support or prevent social isolation or loneliness were different types of companion robots including humanoid or animal robots and robots that could connect people with dementia to their own social networks. For instance, Demiris et al. [26] developed a virtual pet companion accessible on a touch-screen tablet whereas, D’Onofrio et al. [20] and Fields et al. [21] both developed physical robots which users could interact with directly through speech, touch, and movement. While the description of the technologies used were generally clear, the majority of the studies did not state the theory or established intervention underpinning the developed technology however, four studies did highlight different theories and models [21, 23–25]. For example, there was reference to elements of reminiscence therapy [23, 24] that has a growing evidence base around improving cognition, communication and QoL of people with dementia [30]. Established theories form a key part of the description and/or rationale for complex interventions: ensuring these are rooted within an existing evidence based remains essential. Such a focus can help interventions to reach higher levels of effectiveness, to improve utility for user groups and to better understand under what optimal circumstances these desired outcomes can be achieved [32]. It is of note that technologies here are often not focused on an individual component of interaction design but instead focus on a range of modalities such as voice, touch, time, and behavior [33]. The variation and design choices emphasize a need for detailed explanation of founding theories as to not just “why” a complex intervention would achieve desired benefits, but also cements the “how” technologies (and/or human elements) are supporting optimal means to deliver it.
It is encouraging to see that the work of Kitwood around personhood and personalization is represented in many studies; however, the reliance on in person and face to face elements presents both challenges and opportunities for the field. For example, human based supports add personnel requirements for implementation and upscaling. This may be particularly challenging where people with dementia live alone/are in remote settings. All technologies required another person to either make the introduction to the technology and/or guide the person with dementia while using it which helped to offer tailored information and care where needed but there were also technologies that require technical support or long-term involvement from professionals/carers to deliver the use of the technologies. Some technologies went beyond this and offered personalized elements within the developed technology itself [23, 24, 26–29]. Examples include content tailored to the level of dementia or a wide range of activities to cater to individual interests. However, a lack of reported co-design activities is likely to limit accessibility. An approach rooted in user-involvement is important when considering the challenges of using digital technologies with dementia and cognitive impairment [34].
In terms of effectiveness, one must be careful to interpret findings with caution. The majority of studies were small-scale where observational, qualitative, and quantitative methods were used to evaluate the technology. Large-scale, evidence-based studies to assess formal effectiveness were generally lacking, with only one RCT included in this review where there was no a priori power analysis [28]. Given that digital technologies are now widespread, this is surprising, as there remains increasing scope for large-scale observational studies; however, the indication from published literature is that few digital technology efforts are focusing on social isolation or loneliness for people with dementia. Despite such limitations, all studies demonstrated some level of improvement on the QoL for people with dementia following the use of a range of technologies, e.g., companion robots, multi-sensory, touch-screen technologies, and assistive technologies. More specifically, the majority also reported benefits in terms of social inclusion or social interaction and the reduction of loneliness and isolation [21, 22, 24–26, 28, 29]. These findings were mostly linked to technologies consisting of humanoid and animal robots which facilitated social interactions with the technology itself or with family members and friends. Increased engagement in social interactions potentially had an impact on reducing feelings of loneliness and decreasing a sense of social isolation among people with dementia. Although identifying such benefits is encouraging, it would be interesting to define the impact on people with dementia in the longer term, particularly outside of a formal study setting (i.e., demonstrate external validity). Other benefits found for the included technologies consisted of improvements in cognitive functioning and mental stimulation, [23, 26, 27, 29], resilience [20], self-image [24], positive emotions [22], feelings of depression [21, 26], and agitation and restlessness [23, 24].
Previous related reviews in the field have drawn conclusions that align with the findings presented here. For example, despite some positive findings, researchers were unable to draw definite conclusions in their systematic review investigating the effectiveness of technological interventions for people with dementia in terms of social participation due to a lack of studies [16]. Another systematic review on information and communication (ICT) based applications designed to improve social health and social participation in people with dementia, concluded from their limited evidence that ICT-based interventions have better potential than non-ICT interventions to promote social behaviors [35].
There remain fundamental challenges around accessibility and implementation surrounding digital technologies for people with dementia. Existing technologies often have high costs and all technologies included in this review have certain environmental requirements— individually feasible but collectively challenging— such as finding a quiet/peaceful space, reliable internet connections, and human supports (including technical skills). Thus, the digital divide remains an ominous concern for living well with dementia alongside a need to ensure that interventions are safe for use [36]. There is a need to incorporate more observational studies to understand how people with dementia can thrive outside of long-term care facilities— particularly those who live alone or who are geographically isolated— a current knowledge gap in academic literature. As societies worldwide move to more data driven, and digital health and social care approaches- we need to ensure that overlooked groups such as people with dementia are not left behind. Such systemic challenges are being addressed in an increasing body of science focusing on translational failure of concepts to implementation. An example is the non-adoption, abandonment, scale-up, spread, and sustainability framework [37]. We need to find ways to incentivize entrepreneurial efforts that hold future value for sustainability and implementation. Ideally, such work will include and report on involvement of people with dementia at all study stages and during the development of the technology [38]. In addition, observational work should be undertaken to see how we may adapt existing technologies that are already in widespread use.
Strengths and limitations
While a main strength of this work is transparency and rigor of our collaborative approach (e.g., PRISMA), there are also limitations to recognize. For example, the definitions of technologies or living alone can prove challenging. Throughout, our “lens” was to take the viewpoint of a person with dementia who spends time alone/lives alone and the practicalities of digital technologies around this, explaining our heavy emphasis on co-design and implementation in wider settings. However, working with our constructs of interest can be complex: for example, there is no universally accepted definition of “social isolation” and “loneliness”. Although we attempted to be as inclusive as possible, a particularly prominent example of a technology within our review was PARO: a therapeutic robot seal. PARO has proven to be a successful digital technology in many different settings offering a range of benefits to people with dementia (e.g., including increased conversation in facilitated sessions). However, we did not find studies meeting our inclusion criteria with outcomes specifically on social isolation and loneliness (e.g., we would have included such a study if there were qualitative outcomes directly relating to a reduction in “social isolation”). Our emphasis a priori remained primarily on the more subjective outcome of social isolation/loneliness. This decision process highlights a wider challenge in the field of what is the best/most suitable measure of reporting loneliness in dementia, particularly over many weeks and months as dementia progresses. Lastly, included studies were in English or Dutch only due to language skills in the team. As with any systematic review it is plausible that studies may have been missed in our search or screening process. Nevertheless, our work was designed to be as inclusive as possible and we were able to describe technologies in detail, explore the future readiness for implementation and appraise the quality.
Study quality assessment using MMAT
We successfully appraised all included studies using the MMAT but there were a number of limitations. These included that the MMAT ‘screening questions for all types’ are required for all studies but are poorly defined with little or no support documentation. Accordingly, ambiguity on definitions of the MMAT criteria led to disagreement between reviewers over how studies were classified and interpretation remains difficult given that the use of an overall score is discouraged. It is for these reasons that we would recommend that further research is conducted into developing scales to appraise early phase studies so that objective and clear guidance can be used throughout.
Conclusion
Digital technologies have clearly reached widespread use and our reliance on these looks set to increase. Our review identifies a limited body of research with early indications of reductions in isolation and loneliness for people with dementia. However, data suggest that technology readiness remains low, the costs are high, and many solutions have a large dependency on human elements. Prolonged and widespread feelings of loneliness do not fit within a narrative of high-quality dementia care: it is time to explore how to make people with dementia the co-lead architects of digital technologies for social interactions that are affordable, usable, and inclusive for all.
ACKNOWLEDGMENTS
This work has been funded by an Alzheimer’s Society Alzheimer’s Society Travel Fellowship, MYCONNECTION-FRIEND (grant reference number 472). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/22-0438r1).
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JAD-220438.
REFERENCES
[1] | Gauthier S , Rosa-Neto P , Morais JA , Webster C ((2021) ) World Alzheimer Report 2021: Journey through the diagnosis of dementia, Alzheimer’s Disease International, LondonEngland. |
[2] | Arvanitakis Z , Shah RC , Bennett DA ((2019) ) Diagnosis and management of dementia: Review. JAMA 322: , 1589–1599. |
[3] | Cummings J , Aisen P , Lemere C , Atri A , Sabbagh M , Salloway S ((2021) ) Aducanumab produced a clinically meaningful benefit in association with amyloid lowering. Alzheimers Res Ther 13: , 98–98. |
[4] | Kitwood T , Bredin K ((1992) ) Towards a theory of dementia care: Personhood and well-being. Ageing Soc 12: , 269–287. |
[5] | National Institute for Health and Care Excellence (UK) ((2018) ) Dementia: Assessment, management and support for people living with dementia and their carers, National Institute for Health and Care Excellence, London. |
[6] | World Health Organization, Decade of Healthy Ageing 2020-2030, https://www.who.int/initiatives/decade-of-healthy-ageing, Accessed December 02, 2021. |
[7] | National Institute of Health, Social Wellness Toolkit, https://www.nih.gov/health-information/social-wellness-toolkit, Accessed October 28, 2021. |
[8] | Mortimer J ((2016) ) No one should have no one, Age UK, London. |
[9] | O’Rourke HM , Duggleby W , Fraser KD , Jerke L ((2015) ) Factors that affect quality of life from the perspective of people with dementia: A metasynthesis. J Am Geriatr Soc 63: , 24–38. |
[10] | Ortiz-Ospina E, Is there a loneliness epidemic? https://ourworldindata.org/loneliness-epidemic, Accessed December 02, 2021. |
[11] | Alzheimer’s Society, Alzheimer’s Society’s view on people with dementia living alone, https://www.alzheimers.org.uk/about-us/policy-and-influencing/what-we-think/dementia-living-alone, Accessed October 28, 2021. |
[12] | Curelaru A , Marzolf SJ , Provost JKG , Zeon HHH ((2021) ) Social isolation in dementia: The effects of COVID-19. J Nurse Pract 17: , 950–953. |
[13] | Alzheimer’s Society, The psychological and emotional impact of dementia, https://www.alzheimers.org.uk/get-support/help-dementia-care/understanding-supporting-person-dementia-psychological-emotional-impact, Accessed October 28, 2021. |
[14] | Ballard C , Corbett A , Orrell M , Williams G , Moniz-Cook E , Romeo R , Woods B , Garrod L , Testad I , Woodward-Carlton B , Wenborn J , Knapp M , Fossey J ((2018) ) Impact of person-centred care training and person-centred activities on quality of life, agitation, and antipsychotic use in people with dementia living in nursing homes: A cluster-randomised controlled trial. PLoS Med 15: , e1002500. |
[15] | Maresova P , Tomsone S , Lameski P , Madureira J , Mendes A , Zdravevski E , Chorbev I , Trajkovik V , Ellen M , Rodile K ((2018) ) Technological solutions for older people with Alzheimer’s disease: Review. Curr Alzheimer Res 15: , 975–983. |
[16] | Heins P , Boots LMM , Koh WQ , Neven A , Verhey FRJ , de Vugt ME ((2021) ) The effects of technological interventions on social participation of community-dwelling older adults with and without dementia: A systematic review. J Clin Med 10: , 2308. |
[17] | Page MJ , McKenzie JE , Bossuyt PM , Boutron I , Hoffmann TC , Mulrow CD , Shamseer L , Tetzlaff JM , Akl EA , Brennan SE , Chou R , Glanville J , Grimshaw JM , Hróbjartsson A , Lalu MM , Li T , Loder EW , Mayo-Wilson E , McDonald S , McGuinness LA , Stewart LA , Thomas J , Tricco AC , Welch VA , Whiting P , Moher D ((2020) ) The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 372: , n71. |
[18] | Braun V , Clarke V ((2006) ) Using thematic analysis in psychology. Qual Res Psychol 3: , 77–101. |
[19] | Hong QN , Pluye P , Fàbregues S , Bartlett G , Boardman F , Cargo M , Dagenais P , Gagnon M-P , Griffiths F , Nicolau B , O’Cathain A , Rousseau M-C , Vedel I ((2018) ) Mixed Methods Appraisal Tool (MMAT) version 2018, McGill University. |
[20] | D’Onofrio G , Sancarlo D , Raciti M , Burke M , Teare A , Kovacic T , Cortis K , Murphy K , Barrett E , Whelan S , Dolan A , Russo A , RicciardiF , Pegman G , Presutti V , Messervey T , Cavallo F , Giuliani F , BleadenA , Casey D , Greco A ((2019) ) MARIO Project: Validation and evidence ofservice robots for older people with dementia. J AlzheimersDis 68: , 1587–1601. |
[21] | Fields N , Xu L , Greer J , Murphy E ((2021) ) Shall I compare thee...to a robot? An exploratory pilot study using participatory arts and social robotics to improve psychological well-being in later life. Aging Ment Health 25: , 575–584. |
[22] | Moyle W , Jones C , Cooke M , O’Dwyer S , Sung B , Drummond S ((2014) ) Connecting the person with dementia and family: A feasibility study of a telepresence robot. BMC Geriatr 14: , 7. |
[23] | Gustafsson C , Svanberg C , Mullersdorf M ((2015) ) Using a robotic cat in dementia care: A pilot study. J Gerontol Nurs 41: , 46–56. |
[24] | Bruil L , Adriaansen MJM , Groothuis JWM , Bossema ER ((2017) ) Quality of life of nursing home residents with dementia before, during and after playing with a magic table. Tijdschr Gerontol Geriatr 49: , 72–80. |
[25] | Zamir S , Hennessy C , Taylor A , Jones R ((2020) ) Intergroup ‘Skype’ quiz sessions in care homes to reduce loneliness and social isolation in older people. Geriatrics (Basel) 5: , 90. |
[26] | Demiris G , Thompson HJL , Lazar A , Lin S ((2016) ) Evaluation of a digital companion for older adults with mild cognitive impairment. Proceedings of the American Medical Informatics Association, pp496–503. |
[27] | Goodman-Casanova JM , Dura-Perez E , Guzman-Parra J , Cuesta-Vargas A , Mayoral-Cleries F ((2020) ) Telehealth home support during COVID-19 confinement for community-dwelling older adults with mild cognitive impairment or mild dementia: Survey study. J Med Internet Res 22: , e19434. |
[28] | Lauriks S , Meiland F , Oste JP , Hertogh C , Droes RM ((2020) ) Effects of assistive home technology on quality of life and falls of people with dementia and job satisfaction of caregivers: Results from a pilot randomized controlled trial. Assist Technol 32: , 243–250. |
[29] | Baker S , Waycott J , Robertson E , Carrasco R , Neves BB , Hampson R , Vetere F ((2020) ) Evaluating the use of interactive virtual reality technology with older adults living in residential aged care. Inf Process Manag 57: , 102105. |
[30] | Woods B , O’Philbin L , Farrell EM , Spector AE , Orrell M ((2018) ) Reminiscence therapy for dementia., CD. Cochrane Database Syst Rev 3: , 001120. |
[31] | Porges SW ((2003) ) Social engagement and attachment: A phylogenetic perspective. Ann N Y Acad Sci 1008: , 31–47. |
[32] | Skivington K , Matthews L , Simpson SA , Craig P , Baird J , Blazeby JM , Boyd KA , Craig N , French DP , McIntosh E , Petticrew M , Rycroft-Malone J , White M , Moore L ((2021) ) A new framework for developing and evaluating complex interventions: Update of Medical Research Council guidance. BMJ 374: , n2061. |
[33] | Interaction Design Foundation, What is Interaction Design? Interaction Design Foundation, https://www.interaction-design.org/literature/article/what-is-interaction-design. |
[34] | Rai HK , Cavalcanti Barroso A , Yates L , Schneider J , Orrell M ((2020) ) Involvement of people with dementia in the development of technology-based interventions: Narrative synthesis review and best practice guidelines. JMIR 22: , e17531. |
[35] | Pinto-Bruno AC , Garcia-Casal JA , Csipke E , Jenaro-Rio C , Franco-Martin M ((2017) ) ICT-based applications to improve social health and social participation in older adults with dementia. A systematic literature review. Aging Ment Health 21: , 58–65. |
[36] | Livingston G , Sommerlad A , Orgeta V , Costafreda SG , Huntley J , AmesD , Ballard C , Banerjee S , Burns A , Cohen-Mansfield J , Cooper C , FoxN , Gitlin LN , Howard R , Kales HC , Larson EB , Ritchie K , Rockwood K , Sampson EL , Samus Q , Schneider LS , Selbæk G , Teri L , Mukadam N ((2017) ) Dementia prevention, intervention, and care. Lancet 390: , 2673–2734. |
[37] | Greenhalgh T , Maylor H , Shaw S , Wherton J , Papoutsi C , Betton V , Nelissen N , Gremyr A , Rushforth A , Koshkouei M , Taylor J ((2020) ) The NASSS-CAT tools for understanding, guiding, monitoring, and researching technology implementation projects in health and social care: Protocol for an evaluation study in real-world settings. JMIR Res Protoc 9: , e16861. |
[38] | Alzheimer Europe (2021) , Dementia in Europe Yearbook 2021: Dementia-inclusive Communities and Initiatives across Europe. |




