Causes of Death in People with Dementia from 2002 to 2015: A Nationwide Study
Abstract
Background:
Dementia is associated with increased mortality. However, it is not clear whether causes of death in people with dementia have changed over time.
Objective:
To investigate if causes of death changed over time in people with dementia compared to the general elderly population.
Methods:
We included longitudinal data from nationwide registries on all Danish residents aged≥65 years to 110 years who died between 2002 to 2015. We assessed the annual frequency of dementia-related deaths (defined as a dementia diagnosis registered as a cause of death) and of underlying causes of death in people registered with dementia compared to the general elderly population.
Results:
From 2002 to 2015, 621,826 people died, of whom 103,785 were diagnosed with dementia. During this period, the percentage of dementia-related deaths increased from 10.1% to 15.2% in women, and from 6.3% to 9.5% in men in the general elderly population. From 2002 to 2015, dementia became the leading, registered underlying cause of death in people diagnosed with dementia. Simultaneously, a marked decline in cardiovascular and cerebrovascular deaths was observed in people with and without dementia.
Conclusion:
This is the first study to investigate if the causes of death change over time in people diagnosed with dementia compared with the general elderly population. The increase in the registration of dementia as an underlying cause of death could reflect increasing awareness that dementia is fatal.
INTRODUCTION
Dementia was the third leading cause of death in high-income countries in 2016 [1]. From 2000–2015, the number of estimated deaths from dementia more than doubled, making dementia the seventh leading cause of death globally in 2015 [2]. In theUnited Kingdom and Australia, dementia has become the leading cause of death in women [3, 4]. Thus, dementia as a registered cause of death is increasing globally, while the number of people living with dementia is rapidly increasing [5]. However, only few studies have reported nationwide age-specific time trends for dementia-related deaths [6]. Since mortality and dementia risk increase with age, performing an age-specific time trend analysis of dementia-related deaths is important to identify which age groups contribute to the observed increase in dementia-related deaths.
While the number of dementia-related deaths is increasing, dementia may be underreported as cause of death in people with a known dementia disease [7]. A review based on seven population-based studies included people with dementia and concluded that only 7.2%–41.8% had a dementia diagnosis registered on their death certificates [7]. It also found that people with Alzheimer’s disease were more likely to have a dementia diagnosis registered on their death certificates than people with unspecific dementia or vascular dementia [7].
The literature is quite consistent when investigating registered causes of death in people with dementia. Studies based on data from death certificates list, besides dementia, the most frequent causes of death as either cardiovascular disease or pneumonia/respiratory diseases [8–11]. Even though the literature is quite consistent when reporting causes of death in people with dementia, no previous studies have investigated if a change has occurred over time.
Thus, the objective of this study was to perform a thorough descriptive time trend analysis assessing population-based data on dementia-related causes of death in the general elderly population as well as in people with dementia using national registry data on the entire Danish population.
METHODS
Study design, study period, and study population
This study used a cohort design. We defined the study period from January 1, 2002 to December 31, 2015. We chose the first year to be 2002, as new procedures for coding causes of death were introduced this year. All Danish residents aged 65 years to 110 years who died within the 14-year period were included. People aged 110 and older were excluded from the study due to risk of misregistration (although rare).
Data sources
Data was provided by the: 1) Danish Civil Registration System [12]; 2) National Patient Registry [13]; 3) Central Psychiatric Register [14]; 4) National Prescription Registry [15]; 5) Danish Register of Causes of Death [16]; and 6) Statistics Denmark. Since 1968, all Danish residents have been assigned a unique, personal identification number that enables linkage of personal data from different registries [17].
The Danish Register of Causes of Death includes data on all deaths among Danish residents occurring in Denmark since 1970 [16]. Danish death certificates are filled out according to standards set by the World Health Organization (WHO) [18]. Medical doctors fill out the death certificates and, since 1994, causes of death have been registered according to the International Classification of Diseases, 10th Revision (ICD-10) [16]. The causes of death are listed as a chain of events: 1) the immediate cause of death, 2) up to two (optional) contributing causes of death, and 3) the underlying cause defined as the disease or condition leading to death (Supplementary Figure 1). According to WHO, the underlying cause of death is defined as “(a) the disease or injury which initiated the train of morbid events leading directly to death, or (b) the circumstances of the accident or violence which produced the fatal injury” [19].
Furthermore, up to four contributing conditions or diseases can be listed as contributing causes of death. These are defined as conditions that may have led to reduced resistance or increased vulnerability placing the person at higher risk due to the conditions causing death.
For unknown reasons, it was technically possible to list four additional contributing causes of deaths in the calendar years 2002 and 2005.
In 2002, the Danish National Board of Health introduced a new international decision-making tool, the Automated Classification of Medical Entities (ACME), for coding causes of death [16]. Using decision-making tables based on an international standard, ACME determines the underlying cause of death by deciding if a causal link can be established between the immediate, contributing, and underlying cause of death [20]. In cases where ACME has been shown to be imprecise, coding specialists manually evaluated selected groups of causes of death. Since 2007, death certificates have been electronically submitted in Denmark.
The other above-mentioned registries have been described previously elsewhere [21]. All data was made available through Statistics Denmark, which also provided data on immigration, civil status, and date of death.
Identification of people with dementia
Dementia was defined as either a registered dementia diagnosis (primary or secondary) in the Danish National Patient Registry or the Psychiatric Central Research Register (Table 1 presents the diagnostic codes), or based on filling an antidementia drug prescription (Table 2 presents the Anatomical Therapeutic Chemical codes). As we wished to investigate death in late-onset dementia, dementia was defined as being registered in people≥65 years, while people registered with a dementia diagnosis < 65 years were excluded. In this study, we will refer to people registered with dementia according to this definition as people diagnosed with dementia.
Table 1
ICD-8 and ICD-10 diagnosis codes for identification of dementia
| Disease name | ICD-8 | ICD-10 |
| Alzheimer’s disease | 290.10 | F00.0–00.9; G30.0–30.9 |
| Vascular dementia | 293.09–19 | F01.0–01.9 |
| Frontotemporal dementia | 290.11 | F02.0 |
| Dementia without specification | 290.09; 290.19 | F03.9; G31.9 |
| Other dementias | 290.18 | G31.8 |
ICD, International Classification of Diseases.
Table 2
Anatomical Therapeutic Chemical (ATC) codes for identification of pharmaceutical treatment of dementia
| Drug name | ATC code |
| Memantine | N06DX01 |
| Donepezil | N06DA02 |
| Rivastigmine | N06DA03 |
| Galantamine | N06DA04 |
Causes of death
When investigating dementia-related deaths using death certificate data, we applied the list of ICD-10 codes as used when diagnosing dementia in people while still alive (Table 1). The underlying cause of death was defined as the ACME code. Contributing causes of death were defined as any of the ICD-10 codes listed as either immediate cause of death, any contributing causes of deaths, or underlying cause of death if it was different from the ACME code.
When investigating the underlying causes of death in people diagnosed with dementia compared with the general elderly population, the underlying cause of death was defined as the ACME code. Underlying causes of death were divided into eleven categories: 1) dementia; 2) cardiovascular disease; 3) cerebrovascular disease; 4) cancer; 5) pneumonia; 6) chronic respiratory diseases; 7) genitourinary diseases; 8) gastrointestinal diseases; 9) unnatural causes of death; 10) other causes of death, and 11) no registered underlying cause of death. Table 3 lists the ICD-10 diagnoses codes used for categorizing underlying causes of death. We defined dementia-related deaths as deaths where a dementia diagnosis was registered as the underlying or contributing cause of death on the death certificate.
Table 3
ICD-10 diagnosis codes for categorizing underlying causes of death, defined as the Automated Classification of Medical Entities generated code
| Disease category | ICD-10 codes |
| Dementia | F00.0–9, F01.0–9, F02.0, F03.9, G30.0–9, G31.8–9 |
| Cardiovascular diseases | I00–I59, I70–I99 R00–R01, Q20–Q28 |
| Cerebrovascular diseases | I60–I69 |
| Cancer | C00–C96 |
| Pneumonia | J10–J22 |
| Chronic respiratory diseases | J40–J47 |
| Genitourinary diseases | N00–N98, R30–R39 |
| Gastrointestinal diseases | K00–K93, R10–R19 |
| Unnatural causes | F11–F16, F19, F55, V00–X44, X50–X99, Y00–Y39, Y85–87.1, Y88–89 |
| Other causes of death | All remaining codes |
ICD, International Classification of Diseases.
Demographic variables
Age at death was defined as the number of days from date of birth to date of death divided by 365.25 days. Calendar year was defined as the year of death. Civil status at time of death was defined as: 1) married/civil partnership/separated; 2) single/divorced; or 3) widowed. Load of comorbidity was assessed using the Charlson Comorbidity Index (CCI) score on the day of death, where dementia was excluded from the standard CCI version [22].
Statistical analysis
Since our data comprises an entire population as opposed to a sample, a difference in, e.g., percentage of a distribution in two different groups, describes an actual difference.
We assessed the time trend of dementia-related deaths as the annual percentage of all deaths in the population. These analyses were carried out for women and men in five-year age strata (65–69 years, 70–74 years, 75–79 years, 80–84 years, 85–89 years, and≥90 years). The stratification in five-year age groups ensured that different calendar trends in age at death in the general population and among people diagnosed with dementia did not affect the results. Additionally, we assessed the annual distribution of dementia registered as underlying versus contributing cause of death in women and men in ten-year age groups (65–74 years, 75–84 years, and≥85 years). The same analyses were performed in people diagnosed with dementia. These annual distributions of dementia registered as an underlying and contributing cause of death were also assessed as age standardized percentages. The age standardization was performed using all deaths in the Danish elderly population as the standard for each of the investigated years.
Furthermore, we assessed the annual distribution as percentages of underlying causes of death in ten-year age groups (65–74 years, 75–84 years, and≥85 years) in women and men diagnosed with dementia compared with women and men in the general elderly population from 2002 to 2015. If a cause of death had≤5 observations a year, we combined the cause of death categories to preserve anonymity. Finally, we assessed the total number of people whose first dementia diagnoses was given on their death certificates during the study period.
All analyses were carried out using SAS, version 9.4 (SAS Institute Inc., Cary, NC, USA).
Data approvals
This study was approved by the Danish Data Protection Agency, Statistics Denmark, and the Danish Health and Medicines Authority. As all data comprised anonymized registry data, no ethical approval was needed, according to Danish law.
RESULTS
During the study period, 621,826 people died (women: 333,857; men: 287,969), of whom 103,785 were registered with dementia diagnoses prior to death (women: 64,879; men: 38,906). Table 4 presents descriptive data of the population.
Table 4
Descriptive distribution of demographics in the complete population, and women and men diagnosed with dementia
| Complete population | Women diagnosed with dementia | Men diagnosed with dementia | |
| Number (%) | 621,826 | 64,879 (62.5%) | 38,906 (37.5%) |
| Median age at death (interquartile range) | 82.5 (75.5–88.6) | 87.4 (82.8–91.5) | 84.4 (79.6–88.6) |
| Marital status married (%) | 214,352 (34.5%) | 9,431 (14.5%) | 19,799 (50.9%) |
| Divorced/ single (%) | 111,311 (17.9%) | 10,218 (15.8%) | 6101 (15.7%) |
| Widowed (%) | 285,434 (45.9%) | 45,199 (69.7%) | 12,969 (33.3%) |
| Missing (%) | 10,729 (2.1%) | 31 (0.1%) | 37 (0.1%) |
| Median CCI score at time of death (interquartile range) | 2 (1–5) | 1 (0–3) | 2 (1–4) |
CCI, Charlson Comorbidity Index.
In the total population, 65,012 (10.5%) people were registered with dementia as a cause of death (underlying: 36,181; contributing: 28,831). Dementia-related deaths were more frequent in women (12.7%) compared with men (7.9%) (Table 5). On average, from 2002 to 2015, the median age at death was 87.4 years (95% CI: 82.8; 91.5) in women with dementia, and 84.4 (95% CI: 79.6; 88.6) in men with dementia. From 2002 to 2015, median age at death increased more in the dementia groups compared with women and men without dementia (Supplementary Table 1). At time of death, 15.5% of women and 50.9% of men diagnosed with dementia were married, while 69.7% of women with dementia were widowed and only 16.6% of men with dementia were widowed.
Table 5
Distribution of causes of death in women and men not diagnosed with dementia, diagnosed with dementia, and all women and men
| Women | Men | |||||
| Not diagnosed with dementia | Diagnosed with dementia | All women | Not diagnosed with dementia | Diagnosed with dementia | All men | |
| Dementia-related causes of death (%) | 10,131 | 32,277 | 42,408 | 4,665 | 17,939 | 22,604 |
| (3.03%) | (9.67%) | (12.7%) | (1.62%) | (6.23%) | (7.85%) | |
| Other causes of death (%) | 258,847 | 32,602 | 291,449 | 244,398 | 20,967 | 265,365 |
| (77.53%) | (9.77%) | (87.3%) | (84.87%) | (7.28%) | (92.15%) | |
| Total (%) | 268,978 | 64,879 | 333,857 | 249,063 | 38,906 | 287,969 |
| (80.57%) | (19.43%) | (100%) | (86.49%) | (13.51%) | (100%) | |
Dementia-related deaths in the general elderly population
From 2002 to 2015, the percentage of dementia-related deaths increased for women and men≥70 years (Fig. 1). The percentage of dementia-related deaths increased with age; however, this seemed to stabilize at age≥85 as the time trend graphs were similar for men and women for the age groups 85–89 and≥90 years. In people≥75 years, the percentage of dementia-related deaths was higher in women compared with men.
Fig. 1
Time trend of dementia registered as any cause of death, 2002–2015. Time trend of dementia registered as any cause of death of all deaths in women (A) and men (B) divided into five-year age groups.
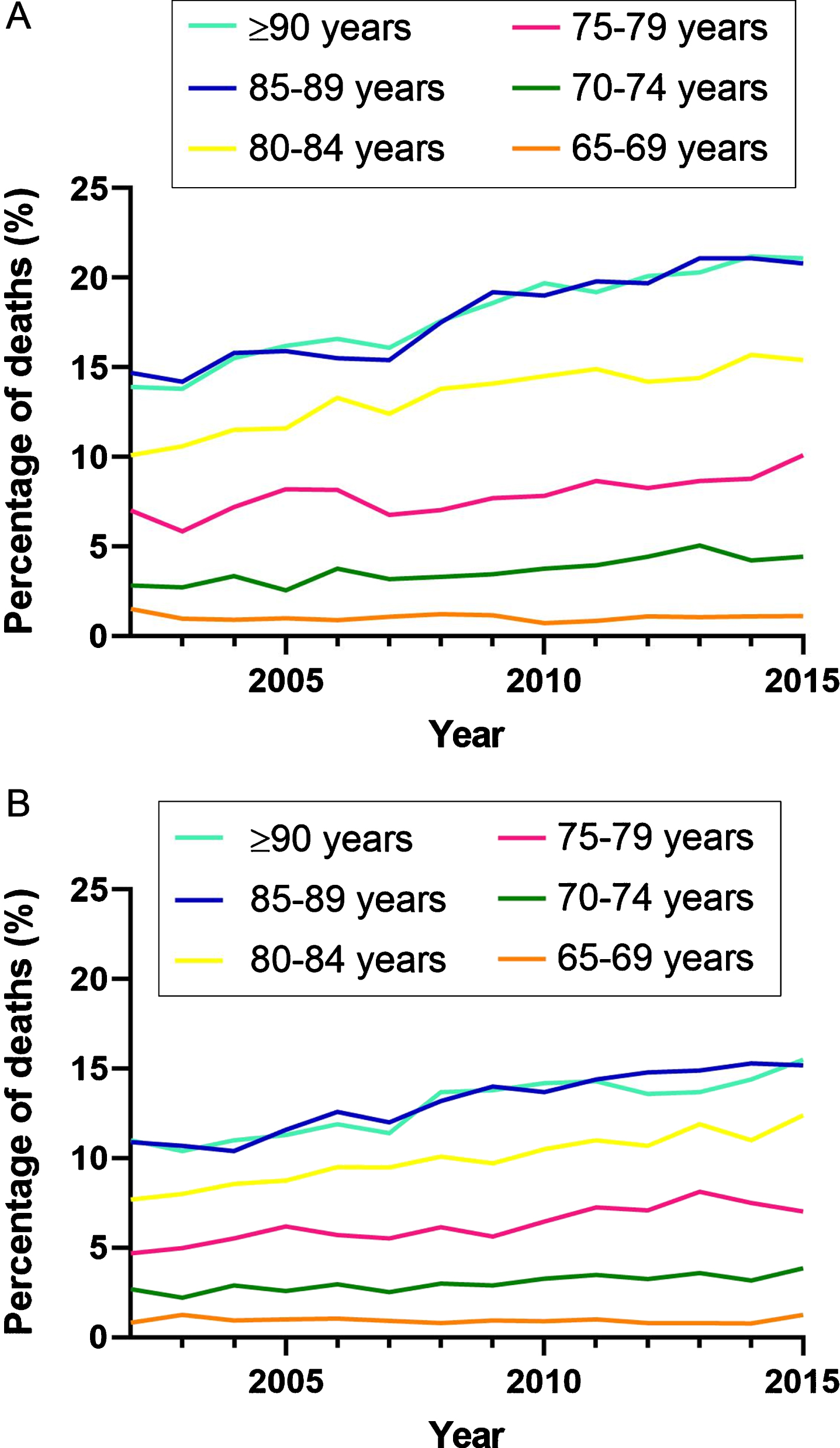
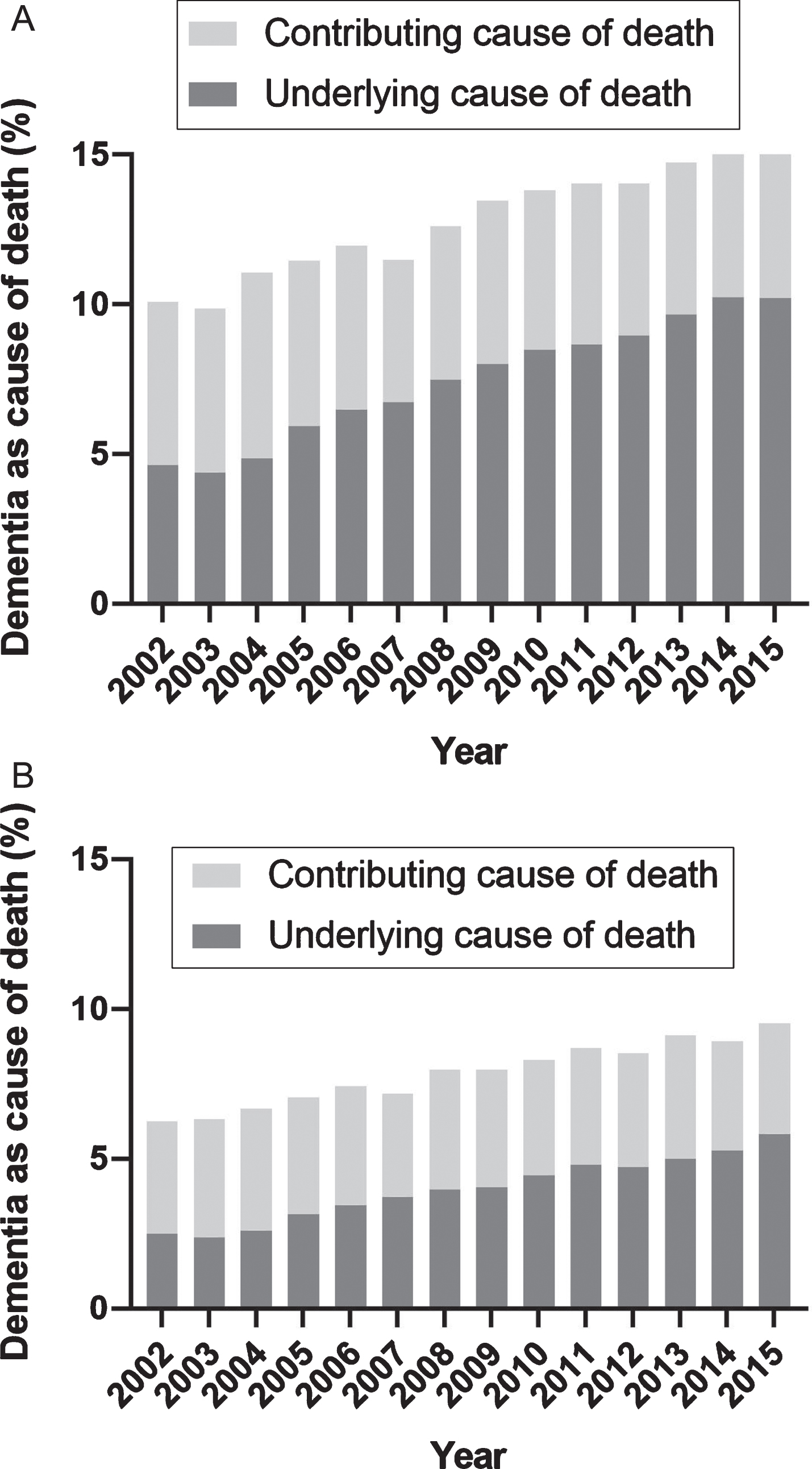
During the study period, there was an increase in the registration of dementia as an underlying cause of death as opposed to a contributing cause of death (Fig. 2). From 2002 to 2015, the percentage of dementia-related deaths increased from 10.1% (underlying: 4.6%) to 15.2% (underlying: 10.2%) in women, and from 6.3% (underlying: 2.5%) to 9.5% (underlying: 5.8%) in men. For women and men of all age groups, the percentage of contributing cause of death was quite stabile, while the increase in percentage of underlying cause of death primarily explained the overall increase in dementia-related deaths. The percentage of dementia-related deaths increased with age in both men and women (Supplementary Figures 2 and 3). Age standardizing only changed the results marginally in both men and women (Supplementary Tables 2 and 3).
Fig. 2
Time trend of the distribution of dementia as cause of death in the general elderly population. Time trend of the distribution of dementia registered as contributing or underlying cause of death in women (A) and men (B) in the general elderly population.
Dementia-related deaths in people diagnosed with dementia
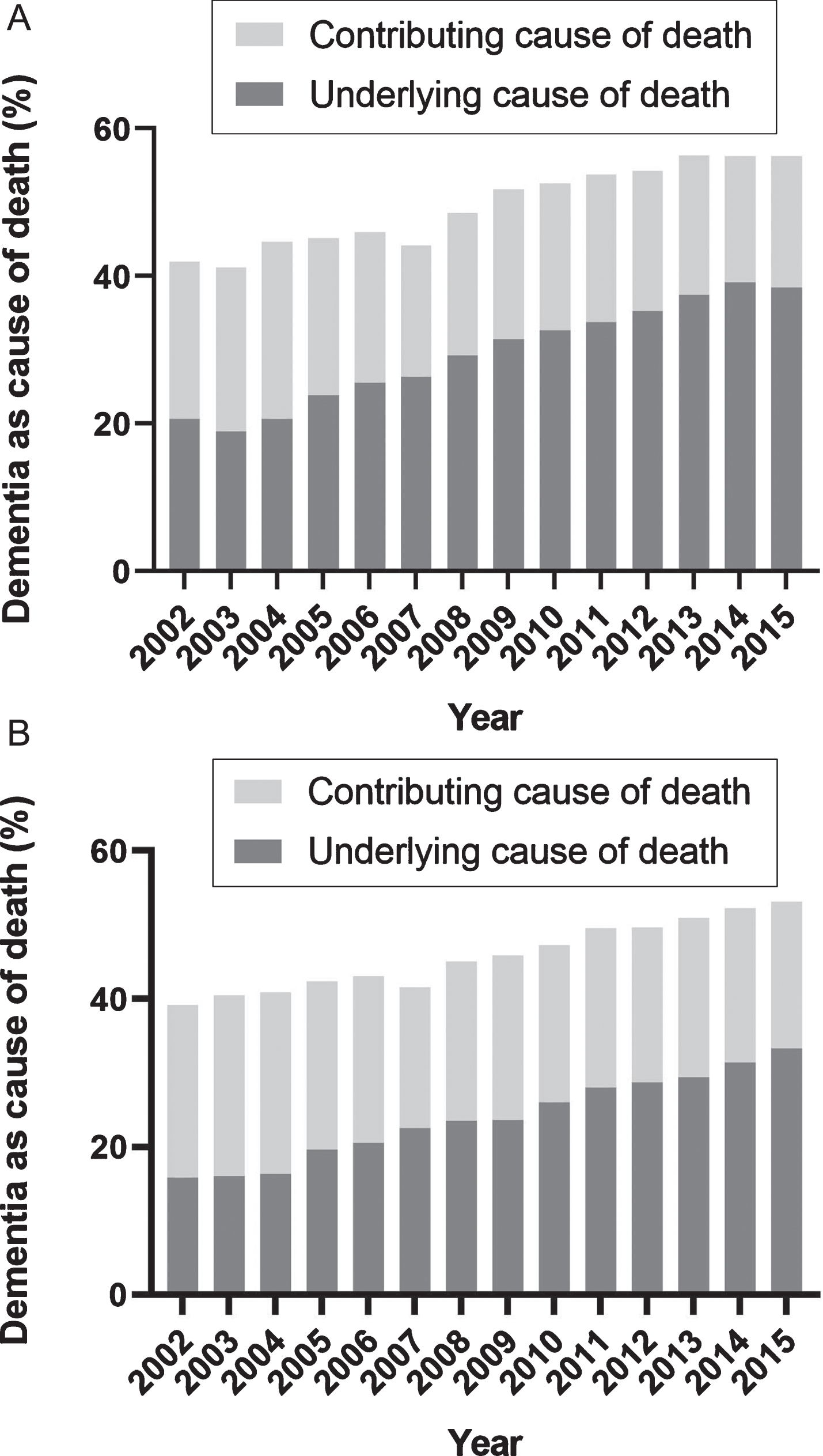
In people diagnosed with dementia, the percentage of registered dementia-related deaths increased from 41.9% (underlying: 20.6%) to 56.2% (underlying: 38.4%) in women, and from 39.2% (underlying: 15.9%) to 53.2% (underlying: 33.3%) in men from 2002 to 2015 (Fig. 3). The percentage of causes of death registered as dementia increased with age in both women and men (Supplementary Figures 4 and 5). Also, in people diagnosed with dementia, the age standardizing only changed the results marginally (Supplementary Tables 2 and 3).
Fig. 3
Time trend of the distribution of dementia as cause of death in women and men diagnosed with dementia. Time trend of the distribution of dementia registered as contributing or underlying cause of death in women (A) and men (B) with diagnosed dementia.
Causes of death in people with and without dementia
The leading underlying causes of death in women diagnosed with dementia were dementia (29.9%), cardiovascular disease (18.7%), and cerebrovascular disease (10.6%), whereas in women without dementia, the leading causes were cancer (26.8%), cardiovascular disease (23.3%), and cerebrovascular disease (8.7%). In men diagnosed with dementia, the leading underlying causes of death were dementia (24.3%), cardiovascular disease (19.2%), and cerebrovascular disease (11.1%), while in men without dementia, the leading underlying causes of death were cancer (31.5%), cardiovascular disease (24.1%), and respiratory disease (7%).
From 2002 to 2015, there was a change in the distribution of registered causes of death both in people with and without diagnosed dementia (Fig. 4). During the period, dementia became the leading underlying cause of death in women and men diagnosed with dementia. The proportions of cardio- and cerebrovascular disease as underlying cause of death declined for all women and men, though more markedly in women and men diagnosed with dementia. The registration of cancer as underlying cause of death increased markedly in women and men without dementia, whereas in women and men diagnosed with dementia, there was only a modest increase.
Fig. 4
Time trend of the distribution of registered underlying causes of death in women and men with and without diagnosed dementia.
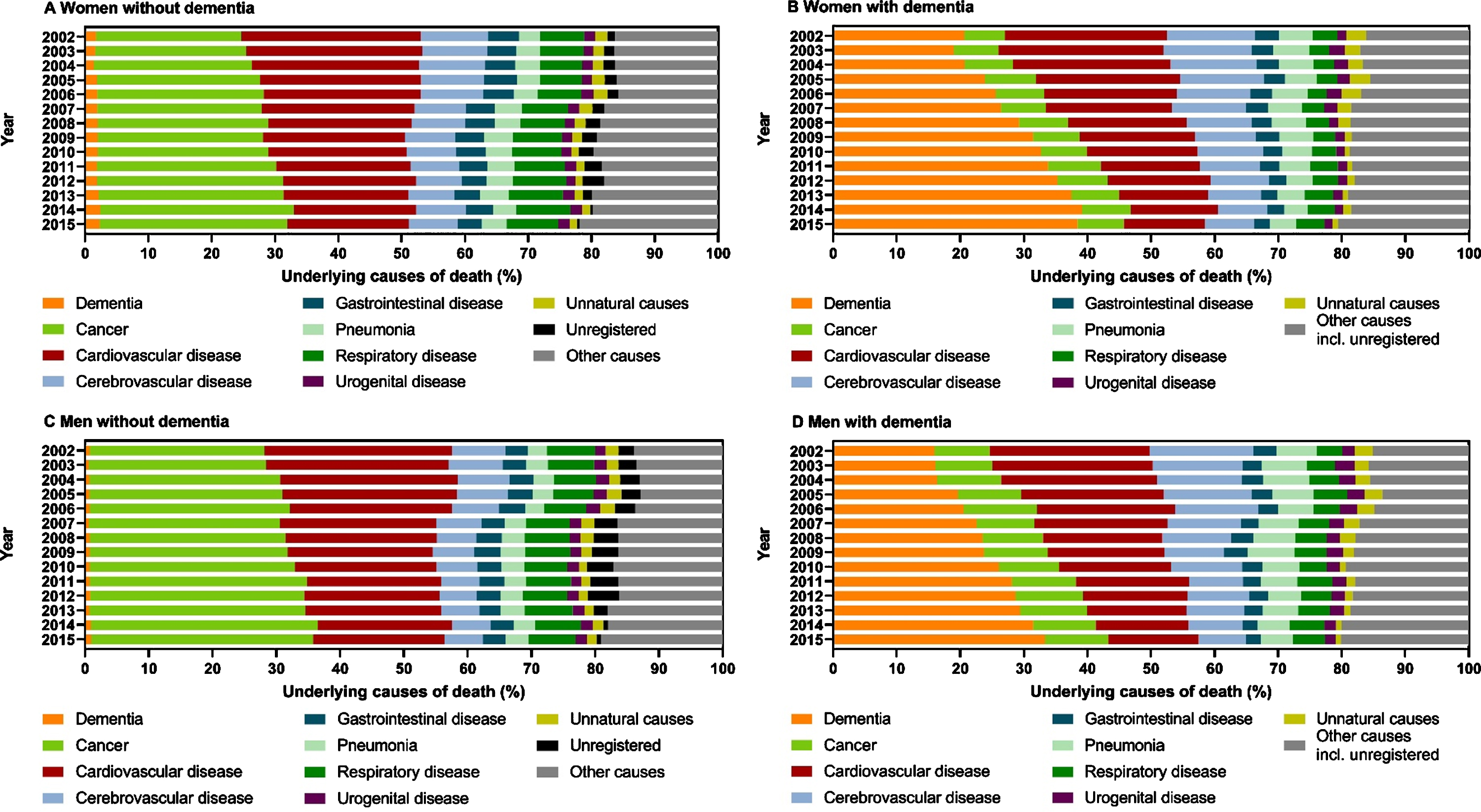
In women and men diagnosed with dementia, the percentage of pneumonia as the underlying cause of death declined, but was quite stable in women without dementia, though it increased in men without dementia. However, in 2015, pneumonia as the underlying cause of death was still more frequent in men diagnosed with dementia (5.1%) compared with men without dementia (3.7%), while in women the frequency was similar (dementia: 4.1%; no dementia: 3.9%).
There were 12,650 people (2%) without a registered underlying cause of death, and this was more frequent in people without dementia (n = 12,537) compared with people diagnosed with dementia (n = 113).
The Supplementary Material presents the time trend of underlying causes of death in men and women with and without dementia in ten-year age groups (Supplementary Figures 6 and 7).
During the 14-year study period, 14,593 people (women: 9,964, men: 4,629) were registered with their first-ever dementia diagnosis on their death certificates (Supplementary Tables 4 and 5), which is equivalent to 24.3% of all registered dementia-related deaths.
DISCUSSION
This is the first study to investigate the time trends of a range of underlying causes of death in people diagnosed with dementia. During the study period, dementia became the leading underlying cause of death in people diagnosed with dementia. From 2012 to 2015, cardio- and cerebrovascular disease as an underlying cause of death declined even more markedly in women and men diagnosed with dementia compared to those without. Cancer was registered less frequently as the underlying cause of death in people diagnosed with dementia compared with the general elderly population, and only increased very modestly in people diagnosed with dementia compared with elderly people without dementia. In the general elderly population, the proportion of dementia-related deaths increased markedly from 2002 to 2015. This was primarily driven by an increase in the registration of dementia as an underlying cause of death. In people diagnosed with dementia, we observed the same pattern of an increase in registering dementia as an underlying cause of death.
To the best of our knowledge, since no previous studies have investigated if the causes of death change over time in people with dementia, our findings cannot be compared with other studies. Since ischemic heart disease and dementia share common risk factors, we believe that the reduction in cardio- and cerebrovascular disease as the underlying cause of death in people diagnosed with dementia observed in our study could be related to a reduction in risk factors and an improvement in the treatment of cardiovascular risk factors [23]. This assumption is supported by the fact that the Framingham Heart Study, which reported a decline in the incidence of dementia, also reported a decline in vascular risk factors from the late 1970s to the early 2010s [23]. The study also found that the risk of dementia associated with stroke, atrial fibrillation, and heart failure decreased over time [23]. In Denmark, there was a marked improvement in the organization of treatment and an increase in the use of pharmacotherapy after myocardial infarction from 1997–1998 to 2009–2010, and the 90-day mortality decreased from 19.6% to 11.7% [24].
Autopsy studies are consistent in reporting pneumonia as the leading immediate cause of death (38%–66%) in people with dementia [25–29]. Also, studies based on death certificates identified pneumonia as a leading underlying cause of death in people with dementia [8, 10, 11, 30]. A meta-analysis found that people with dementia had higher odds (OR = 2.2; 95% CI: 1.44; 3.42) of dying from pneumonia compared with people without dementia [31]. Thus, we hypothesized that our study would confirm these findings. However, in our study, pneumonia was only registered as an underlying cause of death in 4.1% of women and 5.1% of men with dementia in 2015, making it comparable in women with and without dementia. Autopsy studies may show a clear difference in results because they primarily list the immediate cause of death. In contrast, studies based on death certificates either registered the underlying cause of death or multiple causes of death. Such studies show markedly lower prevalence of pneumonia as a cause of death, compared to autopsy studies. In our study, the percentage of people with pneumonia as the underlying cause of death was markedly lower compared to other studies, perhaps because of increased awareness of dementia as a cause of death.
In our study, cancer was less likely to be registered as the underlying cause of death in people diagnosed with dementia compared to the general elderly population, which is in line with findings from other studies [8, 10, 32]. The question can be asked whether people with dementia less frequently die from cancer, or whether there is a reluctance to diagnose cancer in people with dementia. One autopsy study reported that cancer was less frequent in people with dementia [26], while another found that 7% of those deceased with dementia had clinically undiagnosed neoplasms [29]. Thus, it is unclear whether cancer is underdiagnosed in dementia.
This study observed an increase in the registration of dementia as a cause of death, which is in line with findings from other studies [6, 33]. A UK study reported that in people with clinically diagnosed dementia, the percentage of dementia registered as cause of death increased from 39.9% in 2006 to 63.0% in 2013, but the study did not report other causes of death [33]. We also observed that during the study period, dementia was more likely to be registered as an underlying cause of death as opposed to a contributing cause, which is in line with findings from a national Norwegian study [6]. We find this change interesting, as it may reflect a changing medical view on dementia, and a paradigm shift toward perceiving that dementia is fatal. We believe our study emphasizes that dementia is underreported as a cause of death, and this calls for further improvements.
In our previous study involving a time-trend analysis of all-cause mortality in dementia, we found that the mortality rate, assessed as mortality rate ratios, declined at the same rate as in the general elderly population from 1996 to 2015 [34]. Some studies, however, base time trends in mortality on data from death certificates. This study underpins why this can be problematic. If we used the results from this study to evaluate dementia mortality rates, we would report an increase primarily related to the increase in recordings of dementia as a cause of death on death certificates.
Limitations
The most critical limitation of this study is that the data available from the Danish Register of Causes of Death has not been validated in autopsy studies. The most accurate way to establish causes of death is by performing autopsies, and the autopsy rate in Denmark is below 10% [16]. Thus, the data from death certificates depends on the individual doctor and on changes in recommendations about which diagnostic codes should be prioritized [16]. We handled this limitation by dividing causes of death into more broadly defined disease groups instead of using single diagnostic codes as outcomes.
Because dementia is a syndrome with many different etiologies, causes of death have been shown to vary with different dementia subtypes, both in studies based on death certificates [8, 35] and autopsies [25, 26]. Thus, optimally, it would have been best to assess causes of death by dementia subtypes. Unfortunately, though the validity of diagnoses for dementia syndrome is high, the subtype diagnoses are not accurate enough [36].
Dementia is underreported in the Danish health registries. A study estimated that in 2015, there were approximately 87,000 people in Denmark with dementia [37]. In our previous study, we were nevertheless only able to identify 36,129 people with dementia in 2015 using the same methodology as in this study [21]. Thus, we know that dementia is underreported in the national registries, which was emphasized by the fact 14,593 people were identified by registration with a first-time dementia diagnosis in the national registries on their death certificates from 2002 to 2015. We believe some patients are diagnosed by their general practitioner but diagnoses from the primary health care sector are not included in Danish national registries.
Strengths
This study comprised a large nationwide cohort, which made it possible to assess if the causes of death changed over time. Using the national healthcare registries, we were able to identify people diagnosed with dementia and make comparisons with the entire general elderly population without dementia. This was possible because the use of diagnoses for dementia syndrome in the Danish registries have been validated and found to be correct 85.6% of the time [36]. Last, the number of deceased without a registered underlying cause of death was low (2%).
CONCLUSION
This is the first study to investigate if causes of death change over time in people diagnosed with dementia. From 2002 to 2015, dementia became the most frequently registered underlying cause of death in people diagnosed with dementia. Additionally, dementia was more likely to appear as an underlying cause of death as opposed to a contributing cause in the latter years of the study period. We believe that this shift may reflect a positive change in diagnostic procedures and in perceiving dementia not only as a disease that contributes to mortality but as a disease that is actually fatal. Even though we observed an increase in the use of dementia as cause of death, we believe that dementia is still underreported on death certificates and that more can be done to increase awareness that dementia is fatal.
ACKNOWLEDGMENTS
The authors thank the Danish Ministry of Health for supporting the Danish Dementia Research Centre.
The Danish Dementia Research Centre is supported by the Danish Ministry of Health, which played no role in designing the study; in the collection, analysis, interpretation of the data, or in writing this manuscript.
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/20-1400r1).
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JAD-201400.
REFERENCES
[1] | World Health Organization, The top 10 causes of death, https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. Accessed on September 25, 2020 |
[2] | Jamison DT , Gelband H , Horton S , Jha P , Laxminarayan R , Mock CN , Nugent R , eds. (2017) Disease Control Priorities, Third Edition (Volume 9): Improving Health and Reducing Poverty, The World Bank. |
[3] | Office for National Statistics. Deaths registered in England andWales: 2018. 2019:1–11. https://www.ons.gov.uk/releases/deathsregisteredinenglandandwalesseriesdr2018 |
[4] | Australian Institute of Health andWelfare (2019) Deaths in Australia [Internet]. Canberra: Australian Institute of Health and Welfare. |
[5] | Prince M , Wimo A , Guerchet M , Ali G , Wu Y , Prina M ((2015) ) World Alzheimer Report 2015. The Global Impact of Dementia. Alzheimer’s Disease International, London. |
[6] | Hjellvik V , Engedal K , Handal M , Flaten TP , Langballe EM , Selmer R , Strand BH ((2012) ) Dementia in the national cause of death registry in Norway 1969-2010. Nor Epidemiol 22: , 217–224. |
[7] | Romero JP , Benito-León J , Louis ED , Bermejo-Pareja F ((2014) ) Under reporting of dementia deaths on death certificates: A systematic review of population-based cohort studies. J Alzheimers Dis 41: , 213–221. |
[8] | Van De Vorst IE , Koek HL , Bots ML , Vaartjes I ((2016) ) Evaluation of underlying causes of death in patients with dementia to support targeted advance care planning. J Alzheimers Dis 53: , 117–125. |
[9] | Garcia-Ptacek S , Kåreholt I , Cermakova P , Rizzuto D , Religa D , Eriksdotter M ((2016) ) Causes of death according to death certificates in individuals with dementia: a cohort from the Swedish Dementia Registry. J Am Geriatr Soc 64: , e137–e142. |
[10] | Chamandy N , Wolfson C ((2005) ) Underlying cause of death in demented and non-demented elderly Canadians. Neuroepidemiology 25: , 75–84. |
[11] | Romero JP , Benito-León J , Mitchell AJ , Trincado R , Bermejo-Pareja F ((2014) ) Under reporting of dementia deaths on death certificates using data from a population-based study (NEDICES). J Alzheimers Dis 39: , 741–748. |
[12] | Pedersen CB ((2011) ) The Danish Civil Registration System. Scand J Public Health 39: , 22–25. |
[13] | Schmidt M , Schmidt SAJ , Sandegaard JL , Ehrenstein V , Pedersen L , Sørensen HT ((2015) ) The Danish National patient registry: A review of content, data quality, and research potential. Clin Epidemiol 7: , 449–490. |
[14] | Mors O , Perto GP , Mortensen PB ((2011) ) The Danish Psychiatric Central Research Register. Scand J Public Health 39: , 54–57. |
[15] | Pottegård A , Schmidt SAJ , Wallach-Kildemoes H , Sørensen HT , Hallas J , Schmidt M ((2017) ) Data Resource Profile: The Danish National Prescription Registry. Int J Epidemiol 46: , 798–798f. |
[16] | Helweg-Larsen K ((2011) ) The Danish Register of Causes of Death. Scand J Public Health 39: , 26–9. |
[17] | Pedersen CB , Gøtzsche H , Møller JØ , Mortensen PB ((2006) ) The Danish Civil Registration System A cohort of eight million persons. Dan Med Bull 53: , 441–449. |
[18] | Sundhedsdatastyrelsen Dødsattesten - principperog vejledning i registrering af dødsåarsager og andre kliniske oplysninger i dødsattesten. version 1.0.3. 1-43. |
[19] | World Health Organization (1979) Medical certification of cause of death; instructions for physicians on use of international form of medical certificate of cause of death., 1-26, Geneva. |
[20] | Lu TH ((2003) ) Using ACME (Automatic Classification of Medical Entry) software to monitor and improve the quality of cause of death statistics. J Epidemiol Community Health 57: , 470–472. |
[21] | Taudorf L , Nørgaard A , Islamoska S , Jørgensen K , Laursen TM , Waldemar G ((2019) ) Declining incidence of dementia: A national registry-based study over 20 years. Alzheimers Dement 15: , 1383–1391. |
[22] | Thygesen SK , Christiansen CF , Christensen S , Lash TL , Sørensen HT ((2011) ) The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol 11: , 83. |
[23] | Satizabal CL , Beiser AS , Chouraki V , Chêne G , Dufouil C , Seshadri S ((2016) ) Incidence of dementia over three decades in the Framingham Heart Study. N Engl J Med 374: , 523–532. |
[24] | Gjesing A , Gislason GH , Køber L , Gustav Smith J , Christensen SB , Gustafsson F , Olsen AMS , Torp-Pedersen C , Andersson C ((2014) ) Nationwide trends in development of heart failure and mortality after first-time myocardial infarction 1997-2010: A Danish cohort study. Eur J Intern Med 25: , 731–738. |
[25] | Attems J , König C , Huber M , Lintner F , Jellinger KA ((2005) ) Cause of death in demented and non-demented elderly inpatients; an autopsy study of 308 cases. J Alzheimers Dis 8: , 57–62. |
[26] | Brunnström HR , Englund EM ((2009) ) Cause of death in patients with dementia disorders. Eur J Neurol 16: , 488–492. |
[27] | Kammoun S , Gold G , Bouras C , Giannakopoulos P , McGee W , Herrmann F , Michel JP ((2000) ) Immediate causes of death of demented and non-demented elderly. Acta Neurol Scand Suppl 102: , 96–99. |
[28] | Keene J , Hope T , Fairburn CG , Jacoby R ((2001) ) Death and dementia. Int J Geriatr Psychiatry 16: , 969–974. |
[29] | Magaki S , Yong WH , Khanlou N , Tung S , Vinters HV ((2014) ) Comorbidity in dementia: Update of an ongoing autopsy study. J Am Geriatr Soc 62: , 1722–1728. |
[30] | Cermakova P , Szummer K , Johnell K , Fastbom J , Winblad B , Eriksdotter M , Religa D ((2017) ) Management of acute myocardial infarction in patients with dementia: data from SveDem, the Swedish Dementia Registry. J Am Med Dir Assoc 18: , 19–23. |
[31] | Foley NC , Affoo RH , Martin RE ((2015) ) A systematic review and meta-analysis examining pneumonia-associated mortality in dementia. Dement Geriatr Cogn Disord 39: , 52–67. |
[32] | Ganguli M , Dodge HH , Shen C , Pandav RS , DeKosky ST ((2005) ) Alzheimer disease and mortality.. Arch Neurol 62: , 779. |
[33] | Perera G , Stewart R , Higginson IJ , Sleeman KE ((2016) ) Reporting of clinically diagnosed dementia on death certificates: Retrospective cohort study. Age Ageing 45: , 667–672. |
[34] | Taudorf L , Nørgaard A , Waldemar G , Laursen TM ((2021) ) Mortality in dementia from 1996 to 2015: a national registry-based cohort study. J Alzheimers Dis 79: , 289–300. |
[35] | Garcia-Ptacek S , Bahman F , Kåreholt I , Religa D , Cuadrado ML , Eriksdotter M ((2014) ) Mortality risk after dementia diagnosis by dementia type and underlying factors: a cohort of 15,209 patients based on the Swedish Dementia Registry. J Alzheimers Dis 41: , 467–477. |
[36] | Phung TKT , Andersen BBB , Høgh P , Kessing LV , Mortensen PBB , Waldemar G ((2007) ) Validity of dementia diagnoses in the Danish hospital registers. Dement Geriatr Cogn Disord 24: , 220–228. |
[37] | Jørgensen K , Waldemar G ((2014) ) Prævalens af demens i Danmark. Ugeskr Læger 177: , 1041–1044. |



