Proportion of Dementia Explained by Five Key Factors in Jamaica
Abstract
Background:
Dementia has no known cure and age is its strongest predictor. Given that populations in the Caribbean are aging, a focus on policies and programs that reduce the risk of dementia and its risk factors is required.
Objective:
To estimate the proportion of dementia in the Jamaican setting attributable to key factors.
Methods:
We analyzed the contribution of five modifiable risk factors to dementia prevalence in Jamaica using a modified Levin’s Attributable Risk formula (low educational attainment, diabetes, smoking status, depression, and physical inactivity). Four sources of data were used: risk factor prevalence was obtained from the Jamaica Health and Lifestyle Survey, 2008, relative risk data were sourced from published meta-analyses, shared variance among risk factors was determined using cross-sectional data from the Health and Social Status of Older Persons in Jamaica Study. Estimated future prevalence of dementia in Jamaica was sourced from a published ADI/BUPA report which focused on dementia in the Americas. We computed the number of dementia cases attributable to each risk factor and estimated the effect of a reduction in these risk factors on future dementia prevalence.
Results:
Accounting for the overlapping of risk factors, 34.46% of dementia cases in Jamaica (6548 cases) were attributable to the five risk factors under study. We determined that if each risk factor were to be reduced by 5% –10% per decade from 2010–2050, dementia prevalence could be reduced by up to 14.0%.
Conclusion:
As the risk factors for dementia are shared with several of the main causes of death in Jamaica, a reduction in risk factors by even 5% can result in considerable public health benefit.
INTRODUCTION
Dementia has no known cure and advanced age is its strongest predictor [1]. As dementia progresses, disability and dependency increase as it not only affects memory and cognitive abilities but also behavior and the ability to perform tasks of daily living [1]. Over 50 million people worldwide are estimated to have the condition with over US$800 billion spent on treatment and management [2]. This figure is projected to increase to well over 70 million people by 2030 [2] with most new cases occurring in low- and middle-income countries [3, 4]. A focus on dementia risk reduction is therefore justified as research has shown that targeting modifiable lifestyle factors such as smoking habits, diet, physical activity, midlife hypertension, and depression can result in reduced population prevalence [5–7].
The calculation of population attributable risk (PAR) takes into consideration the prevalence of risk factors and their relative risks in relation to a specific disease outcome and helps to identify the most effective public health strategies that aim to reduce future disease burden [8]. The pool of studies which have calculated PAR of dementia/AD although relatively small, covers both groups of and singular countries across a variety of geographical locations. Recently, PAR estimates of dementia were reported for the 10/66 survey countries which looked at the contribution of education in early life (<45 years), hearing loss, hypertension and obesity in midlife (45–64 years), and smoking, depression, physical inactivity, social isolation, and diabetes in later life (≥65 years) on dementia prevalence in China, India, and a group of Latin American countries [9]. In all 10/66 study countries, low education levels were attributable to the greatest proportion of dementia cases: China: 8%, India: 13.6%, and Latin America: 10.9% [9]. The contribution of hypertension, hearing loss, and obesity in midlife, and physical inactivity in later life were also noteworthy in all study countries [9]. In an earlier multi-country study, the PAR of Alzheimer’s disease (AD) was calculated worldwide as well as for the US, Europe, and the UK [8]. Using relative risks from published meta-analyses, the authors examined the contribution of diabetes, midlife hypertension, midlife obesity, physical inactivity, depression, smoking, and low educational attainment. Similar to the 10/66 survey, worldwide results showed that low educational attainment accounted for the greatest proportion of AD cases [8]. Country specific estimates for the US, Europe, and the UK, however, showed that the greatest proportion of AD was attributable to physical inactivity (21.0%, 20.3%, and 21.8%, respectively). The authors highlighted that worldwide, the seven factors studied account for an estimated 9.6 million AD cases when they are combined and that any intervention able to reduce the prevalence of each of them by 10% per decade has the potential to reduce the worldwide prevalence of AD in 2050 by 8.3% [8].
Other single country studies have also been conducted to determine the PAR of dementia. These include studies in Australia and Barbados. In Australia, using data from the Australia Diabetes, Obesity and Lifestyle Study, 48.4% of dementia cases were found to be attributed to seven modifiable risk factors (midlife obesity–1.7%, physical inactivity–17.9%, smoking–4.3%, low education levels–14.7%, diabetes mellitus–2.4%, midlife hypertension–13.7%, and depression–8.0%) [10]. The authors further surmised that a reduction in the prevalence of each of these factors of between 5% and 20% per decade would have the effect of reducing future dementia prevalence by between 1.6% and 30.7% from 2020 to 2050 [10]. In the Caribbean island of Barbados, a similar study was conducted using data from the “Survey on Health, Well-being and Aging in Latin America and the Caribbean” to calculate the PAR of dementia for six risk factors (midlife obesity, physical inactivity, smoking, low educational attainment, diabetes mellitus, and midlife hypertension) [11]. These factors were estimated to be attributable to 50.9% of dementia cases (midlife hypertension–24.4%, midlife obesity–18.3%, physical inactivity–16.3%, low educational attainment–10.9%, diabetes mellitus–8.0%, and smoking–2.5%). According to the study estimates, if each risk factor were reduced by 5% –20% every 10 years, dementia prevalence in Barbados could be reduced by as much as 15.2% in 2030 and 31.8% in 2050 [11].
Our study therefore aims to add to the body of knowledge related to PAR of dementia and to expand the understanding of the contributors to the disease in the Caribbean region. In addition, our study is novel as to our knowledge it is the only one to determine the contribution of key risk factors to dementia prevalence in Jamaica. As we have taken into consideration the effect of overlapping risk factors, our estimates while more conservative, are more realistic since we have used a modified Levin’s formula [8]. We have also calculated the number of cases of dementia that could be prevented if there was investment in a dementia risk reduction program able to reduce the risk factors under study by either 5% or 10%, such information is useful to program planners and policymakers.
Finally, our study allows us to compare our findings to those previously published. Such cross-national comparisons are important as they allow for more nuanced examination of the effects exerted by the social determinants of health and differences that exist across social, ethnic, cultural, and geographical groups on dementia prevalence.
METHODS
Four sources of data were used in the present study. Firstly, the population prevalence of each risk factor was obtained from the Jamaica Health and Lifestyle Survey (JHLS), 2008 [12]. This survey has been conducted since 2000 and provides estimates of the country’s health status with emphasis on non-communicable diseases and their risk factors. While the last version of this survey was conducted in 2016/17, findings have not been officially released; as such we have utilized the 2008 estimates. The 2008 JHLS utilized a cross-sectional design with questions being administered by an interviewer (n = 2,848; age range: 15–74). The survey also included anthropometric measurement and testing of fasting blood glucose and cholesterol [12]. Secondly, global relative risks for dementia were obtained from the 2014 World Alzheimer Report [13]. Thirdly, in STATA version 15.1, shared variance among risk factors was estimated using the Health and Social Status of Older Persons in Jamaica Study (see key demographic characteristics of the study population in Table 1) [14].
Table 1
Key demographic characteristics of the study population
| Variable | Sex % (n) | Total % (n) | |
| Male | Female | ||
| Age Groups (y) | |||
| 60–69 | 48.0 (673) | 40.7 (618) | 44.2 (1291) |
| 70–79 | 32.6 (457) | 34.8 (529) | 33.8 (986) |
| ≥80 | 19.3 (271) | 24.4 (371) | 22.0 (642) |
| Parish of Residence | |||
| St. Andrew | 41.1 (581) | 52.7 (806) | 47.1(1387) |
| St. Catherine | 51.0 (720) | 36.9 (564) | 43.6 (1284) |
| St. Thomas | 7.0 (99) | 7.8 (119) | 7.4 (218) |
| Kingston | 0.8 (12) | 2.7 (41) | 1.8 (53) |
| Highest level of Education | |||
| No formal schooling | 6.9 (97) | 4.6 (69) | 5.7 (166) |
| Primary | 70.4 (988) | 73.5 (1114) | 72.0 (2102) |
| Secondary | 12.9 (181) | 11.9 (181) | 12.4 (362) |
| Technical/vocational | 5.5 (77) | 3.8 (58) | 4.6 (135) |
| University | 4.3 (61) | 6.2 (94) | 5.3 (155) |
Conducted in 2012, the cross-sectional Health and Social Status of Older Persons in Jamaica Study was conducted across four parishes in Jamaica (Kingston, St. Andrew, St. Catherine, and St. Thomas), used a mixed methodology including quantitative, qualitative, and clinical components, and aimed to assess the health and social status of older Jamaicans and to identify their needs (n = 2,943, age range: 60–103 years) [14]. These parishes were selected as St. Catherine has been documented to have a profile said to be representative of much of Jamaica, while the other parishes allowed for the comparison of the health and social status of older persons in predominantly urban (Kingston & St. Andrew) and rural (St. Thomas) settings [14]. Fourthly, estimated future prevalence of dementia was obtained from a published ADI/BUPA report which focused on dementia in the Americas [15]. Five risk factors were identified for inclusion in the study based on their established association with dementia [13, 16, 17] and because risk factor prevalence data was readily available using the data sources previously identified. Risk factor definitions are provided in Table 2.
Table 2
Risk Factor Definitions
| Risk Factor | Definition |
| Smoking | The proportion of adults who currently smoke (based on self-report) |
| Low educational attainment | The proportion of adults who have a primary and/or secondary school education (based on self-report) |
| Physical inactivity | The proportion of adults engaging in physical fitness activity 6 times or less per week (based on self-report) |
| Diabetes mellitus | The prevalence of diabetes mellitus among adults (based on self-report and biomedical data) |
| Depression | Mental health was assessed by enquiring about levels of satisfaction with life, involvement in activities for relaxation and the presence of symptoms of depression. Depression was then characterized as the presence of five or more depressive symptoms and or expressions of suicidal ideations. (DSM-V criteria). |
Published meta-analyses examining the association between dementia and the five risk factors of interest were used to obtain relative risk data [13]. Table 3 shows the relative risk and prevalence data utilized in this study and their sources.
Table 3
Prevalence and Relative Risk data sources
| Risk Factor | Prevalence (%) | Relative Risk | Communality (%) |
| Smoking | 14.5 | 1.28 (0.99–1.60) | 24.50 |
| Low educational attainment | 37.7 | 1.72 (1.52–1.96) | 11.50 |
| Physical inactivity | 46.0 | 1.39 (1.16–1.67) | 20.00 |
| Diabetes mellitus | 7.6 | 1.50 (1.33–1.70) | 23.67 |
| Depression | 3.1 | 1.97 (1.67–2.23) | 14.94 |
Ethics approval and consent to participate
The Health and Social Status of Older Adults in Jamaica study was approved by the Ethics Committee of the University of the West Indies. Written informed consent was obtained from all participants at baseline and follow-up.
Statistical analysis
The proportion of dementia cases attributable to individual risk factors was calculated using Levin’s formula [18]:
(1)
where P = population prevalence and RR = relative risk.
The combined effect of individual risk factors was calculated using the formula below [19]:
(2)
Similar to other studies [8, 9], we accounted for individuals having overlapping risk factors by using a previously published modified formula which takes into account the unique contribution of each risk factor ‘w’ [8]:
(3)
Factor analysis using Stata version 15.1 was used to estimate communality for each risk factor using data from the Health and Social Status of Older Persons in Jamaica Study (2012). More specifically, similar to other published work [8–11], we calculated the tetrachoric correlation in order to obtain correlation coefficients and a correlation matrix. Factor analysis was then performed on the matrix to obtain eigenvalues. Components with eigenvalues of at least 1 were retained in the model, so that only eigenvectors that held the most information about the data distribution were retained. Communality was calculated as the sum of the square of all factor loadings [10].
Total number of dementia cases related to each of the five risk factors was calculated as the product of their individual PARs and dementia prevalence.
Using published dementia prevalence estimates [20], the effect of reducing the relative prevalence of each risk factor by 5% and 10% per decade on the future prevalence of dementia in Jamaica was calculated.
RESULTS
PAR calculations are shown in Table 4. Confidence limits for PAR and the number of attributable cases were calculated using a published substitution method [21].
Table 4
PAR of dementia for each risk factor and number of cases attributable in 2010
| Risk Factor | Prevalence of Risk Factor | PAR % (95% CI) | Number of attributable cases in 2010 (95% CI) |
| Smoking | 14.5 | 3.9 (–0.14–8.00) | 741 (–27–1521) |
| Low educational attainment | 37.7 | 21.35 (16.39 –26.57) | 4056 (3114–5049) |
| Physical inactivity | 46.0 | 15.21 (6.86–23.56) | 2890 (1303–4476) |
| Diabetes mellitus | 7.6 | 3.66 (2.45–5.05) | 696 (465–960) |
| Depression | 3.1 | 2.9 (2.03–3.67) | 555 (387–698) |
| Combined | - | 40.06 (25.47–52.77) | 7612 (4838–10027) |
| Adjusted combined | - | 34.46 (21.99–45.69) | 6548 (4178–8680) |
Dementia cases 2010 = 19,000 [15].
Operating independently, the five risk factors under study were estimated to be attributable to 40.06% of dementia cases in Jamaica, i.e., 7612 cases. When we took into consideration that risk factors often overlap, the five risk factors under study were found to contribute to 34.46% of dementia cases in Jamaica, i.e., 6548 cases.
Effect of risk factor reduction
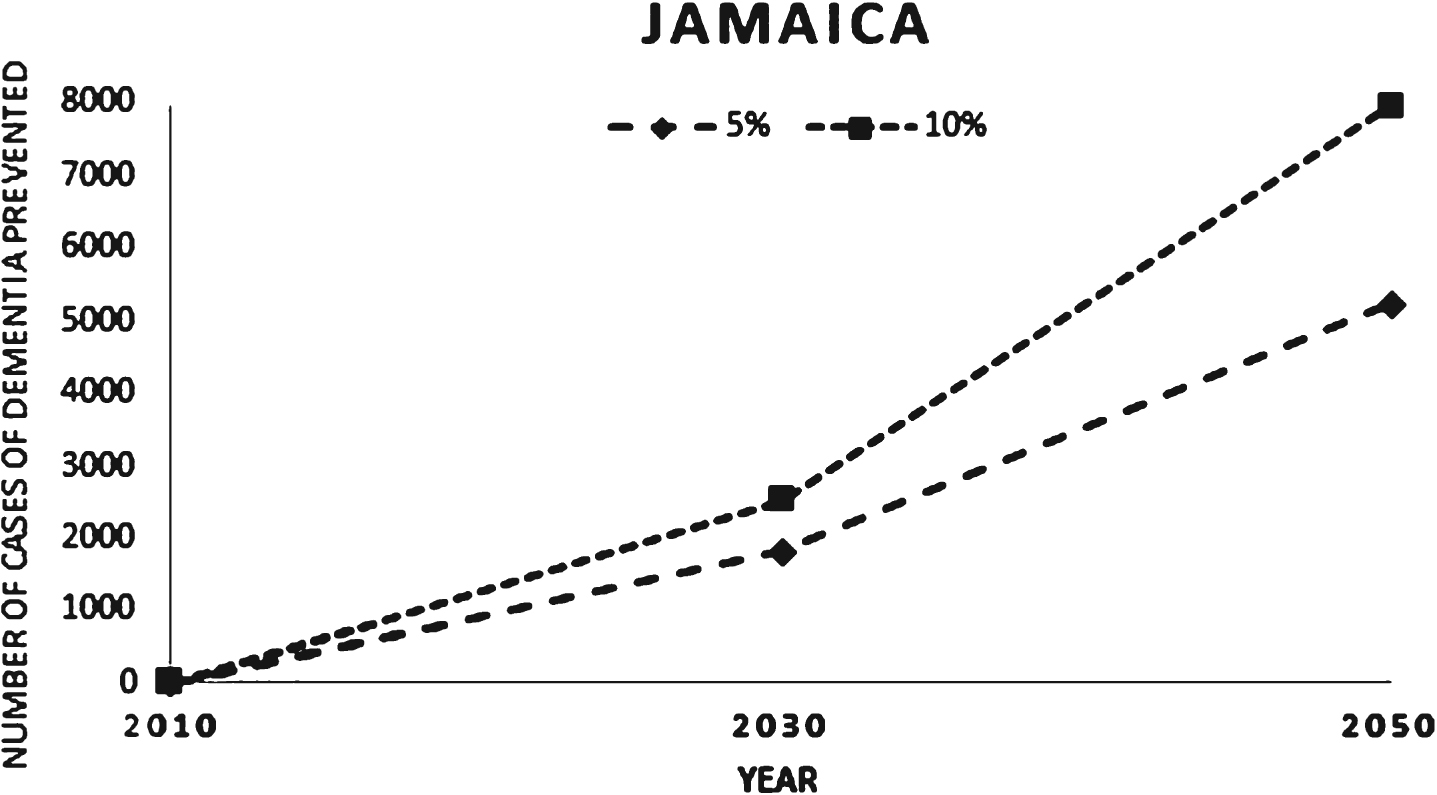
Table 5 and Fig. 1 below show the effect of a 5% and 10% per decade reduction in each risk factor on future dementia prevalence estimates.
Table 5
Effect of a 5% and 10% reduction in each risk factor on future dementia prevalence (2010–2050)
| Percent reduction | 2010 | 2030 | 2050 | ||
| n | % | n | % | ||
| Projected dementia cases | 19,000 | 31,000 | 100 | 55,000 | 100 |
| 5% decrease | NA | 29,176 | 6.25 | 59,766 | 8.77 |
| 10% decrease | NA | 28,469 | 8.89 | 57,049 | 13.94 |
Projected dementia cases were obtained from a report produced by Alzheimer’s Disease International and British United Provident Association [15].
Fig. 1
Reduction in dementia cases as a result of a 5% and 10% reduction in each risk factor per decade.
DISCUSSION
Our study is the first to report on the contribution of risk factors to dementia prevalence in Jamaica. There is a dearth of research in this area in the Caribbean region and our study aims to contribute to filling this gap and providing information to program implementers and policymakers. Considering that risk factors typically do not occur independently, we estimated that approximately 34.46% of dementia cases in Jamaica can be attributed to smoking, low education levels, physical inactivity, diabetes mellitus, and depression. Further, any dementia risk reduction program that is able to result in a 5% –10% decrease in each of these risk factors has the potential to prevent approximately between 6.0% and 14.0% of future dementia cases.
In Jamaica, having a low education level and physical inactivity contributed to the greatest proportion of dementia cases (21.35% and 15.21%, respectively) while depression and diabetes accounted for the smallest proportion (2.90% and 3.66%, respectively). These findings bear similarities to others that have been previously published. Mukadam et al. (2019) reported that for the 10/66 survey countries which examined the impact of nine risk factors on dementia prevalence worldwide as well as in China, India, and a group of Latin American countries, low education levels were attributable to the greatest proportion of dementia cases (Worldwide: 19.1%, China: 10.8%, India: 13.6%, and Latin America: 10.9%, respectively) [9]. Also similar to our study was the limited contribution of depression and diabetes to overall dementia prevalence. Worth noting though is that even though more risk factors were examined in the 10/66 study, their combined contribution to overall dementia prevalence was relatively modest in both China (39.5%) and India (41.2%) but more sizeable in Latin America (55.8%) [9]. The comparatively higher prevalence estimates at the population level for low education and physical inactivity than for depression and diabetes are likely contributors to the higher proportion of dementia cases explained by these factors. In a study by Norton et al. (2014), the authors also reported that worldwide low education levels contributed to the greatest proportion of dementia cases [8]. However, country specific estimates for the US, Europe, and the UK showed that the greatest proportion of dementia cases were found to be attributed to physical inactivity. Differences between these higher-income Western countries, and their Asian, Latin American, and Caribbean counterparts may be partially explained by their economic realities. In Jamaica, for example, although education is “free”, there are several “hidden” costs that may deter students from being able to complete their secondary school education (for example registration fees and transportation costs). With relatively high unemployment (7.2%) and poverty rates (19.0%), any additional cost can result in early school departure/drop out [22].
Using a lifecourse approach to examine the association between lifestyle factors and disease, the middle years (midlife) has emerged as a period of life that merits further study and greater investment in intervention programs [16]. As it relates to dementia, midlife obesity and hypertension have both been implicated in the development of late-life dementia [23, 24]. Findings from earlier population attributable risk studies in Barbados and Australia provide evidence to support a focus on this period [10, 11]. In our study, we were not able to account for the effect of hypertension and obesity in midlife due to data limitations related to prevalence and communality (the Health and Social Status of Older Adults in Jamaica Study collected data only from older adults). We note though that midlife cardiovascular factors may exert a significant effect on development of dementia in our setting given the results of a published study which highlighted that of the dementia cases in older adults in Jamaica, AD accounts for 62% and vascular dementia 32.5%. Further, in Jamaica it was found that vascular disease was prominent in 45.5% of the AD cases [20].
Our study adds to the sparse body of literature on the effect of risk factor prevalence in developing countries, such as those of the Caribbean, where an estimated 58.0% of people living with dementia reside [25]. These countries are known to have limited resources and a shortage of elder-care services, especially for those living with dementia and their caregivers. Any intervention able to delay or prevent the onset of dementia by targeting modifiable lifestyle factors has the potential to significantly reduce its future prevalence and the need for dementia-related health services and support [11]. Limitations of our study include our inability to include midlife hypertension, hearing loss, and midlife obesity as risk factors to be considered due to data limitations. Additionally, we have not been able to account for the contribution of modifiable risk factors which have now been implicated in recent meta-analyses using newly available evidence—excessive alcohol consumption, head injury, and air pollution [26]. Further, risk factor population prevalence data were obtained from the Jamaica Health and Lifestyle Survey 2008 which although over a decade old represents the most up-to-date and comprehensive estimates of the prevalence of NCDs and their risk factors (findings from the 2016/17 survey have not been published as yet). In addition, we acknowledge that it may have been possible for some participants from the Jamaica Health and Lifestyle Study to have also participated in the Health and Social Status of Older Adults Study. This may have had the effect of inflating our estimates. Finally, the prevalence of depression used in our calculations (3.1%) was also obtained from the aforementioned 2008 study and includes persons with other psychological disorders such as anxiety and psychosis [12]. Strengths of our study include our ability to add to the body of information on the topic and to provide meaningful data to policymakers who are tasked with developing and investing in public health programs. Our findings present a strong case for greater investment in education and increasing physical activity as both of these have been shown to be consistently significant contributors in the literature [9–11, 26]. Such interventions will result not only in lessened financial impact on individuals but also reduced public health expenditure. It is important to note though that dementia risk reduction programs can increase longevity which in itself is a risk factor for dementia (the longevity paradox) [27].
Further studies are needed to examine the complex interactions between risk factors and the key features of risk reduction programs that can result in sustainable behavior change.
Conclusion
Given the data available, dementia risk reduction programs, particularly those focused on increasing the education and physical activity levels of individuals, are likely to prevent the greatest proportion of dementia cases in Jamaica. Further studies are also required to further elucidate the effect of risk factors in midlife such as obesity and hypertension which we hypothesize make a significant contribution to dementia prevalence in Jamaica. Greater investment in programs that target these risk factors will result not only in cognitive health gains but also benefits as it relates to other major causes of death such as cardiovascular health and cancers.
DISCLOSURE STATEMENT
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/20-0601r2).
Availability of data and materials
Data which support the findings of this study are not publicly available, but access can be requested from the Mona Ageing and Wellness Centre.
REFERENCES
[1] | World Health Organization (2017) Global action plan on the public health response to dementia 2017–2025. https://www.who.int/mental_health/neurology/dementia/action_plan_2017_2025/en/, Accessed July 30, 2020. |
[2] | World Health Organization (2019) Risk reduction of cognitive decline and dementia: WHO guidelines. https://www.who.int/mental_health/neurology/dementia/guidelines_risk_reduction/en/, Accessed July 30, 2020. |
[3] | Prince M , Guerchet M , Prina M ((2015) ) The epidemiology and impact of dementia: Current state and future trends. World Health Organization, Geneva. |
[4] | Loy CT , Schofield PR , Turner AM , Kwok JB ((2014) ) Genetics of dementia. Lancet 383: , 828–840. |
[5] | Anstey KJ , Mack HA , Cherbuin N ((2009) ) Alcohol consumption as a risk factor for dementia and cognitive decline: Meta-analysis of prospective studies. Am J Geriatr Psychiatry 17: , 542–555. |
[6] | Morris M ((2009) ) The role of nutrition in Alzheimer’s disease: Epidemiological evidence. Eur J Neurol 16: , 1–7. |
[7] | Scarmeas N , Stern Y , Mayeux R , Manly JJ , Schupf N , Luchsinger JA ((2009) ) Mediterranean diet and mild cognitive impairment. Arch Neurol 66: , 216–225. |
[8] | Norton S , Matthews FE , Barnes DE , Yaffe K , Brayne C ((2014) ) Potential for primary prevention of Alzheimer’s disease: An analysis of population-based data. Lancet Neurol 13: , 788–794. |
[9] | Mukadam N , Sommerlad A , Huntley J , Livingston G ((2019) ) Population attributable fractions for risk factors for dementia in low-income and middle-income countries: An analysis using cross-sectional survey data. Lancet Global Health 7: , e596–e603. |
[10] | Ashby-Mitchell K , Burns R , Shaw J , Anstey KJ ((2017) ) Proportion of dementia in Australia explained by common modifiable risk factors. Alzheimers Res Ther 9: , 11. |
[11] | Ashby-Mitchell K , Burns R , Anstey KJ ((2018) ) The proportion of dementia attributable to common modifiable lifestyle factors in Barbados. Rev Panam Salud Publica 42: , e17. |
[12] | Wilks R , Younger N , Tulloch-Reid M , McFarlane S , Francis D ((2008) ) Jamaica Health and Lifestyle Survey 2007-8. Tropical Medicine Research Institute, University of the West Indies, Mona, Kingston. |
[13] | Prince MJ ((2014) ) World Alzheimer Report 2014: Dementia and risk reduction: An analysis of protective and modifiable factors. https://www.alz.co.uk/research/WorldAlzheimerReport2014.pdf, Accessed July 30, 2020. |
[14] | Eldemire-Shearer D , James K , Waldron N , Mitchell-Fearon K ((2013) ) National Health Fund Report: Older Persons in Jamaica. https://www.mona.uwi.edu/commhealth/sites/default/files/commhealth/uploads/EXECUTIVE%20SUMMARY.pdf, Accessed July 30, 2020. |
[15] | ADI/Bupa (2013) Dementia in the Americas: Current and future cost and prevalence of Alzheimer’s disease and other dementias. https://www.alz.co.uk/sites/default/files/pdfs/dementia-in-the-americas-ENGLISH.pdf, Accessed July 31, 2020. |
[16] | Livingston G , Sommerlad A , Orgeta V , Costafreda SG , Huntley J , Ames D , Ballard C , Banerjee S , Burns A , Cohen-Mansfield J ((2017) ) Dementia prevention, intervention, and care. Lancet 390: , 2673–2734. |
[17] | Orgeta V , Mukadam N , Sommerlad A , Livingston G ((2019) ) The lancet commission on dementia prevention, intervention, and care: A call for action. Irish J Psychol Med 36: , 85–88. |
[18] | Levin ML ((1953) ) The occurrence of lung cancer in man. Acta Unio Int Contra Cancrum 9: , 531–941. |
[19] | Barnes DE , Yaffe K ((2011) ) The projected effect of risk factor reduction on Alzheimer’s disease prevalence. Lancet Neurol 10: , 819–828. |
[20] | Eldemire-Shearer D , James K , Johnson P , Gibson R , Willie-Tyndale D ((2018) ) Dementia among older persons in Jamaica: Prevalence and policy implications. West Indian Med J 67: , 1–8. |
[21] | Daly LE ((1998) ) Confidence limits made easy: Interval estimation using a substitution method. Am J Epidemiol 147: , 783–790. |
[22] | The World Bank (2020) The World bank in Jamaica - Overview, https://www.worldbank.org/en/country/jamaica/overview, Accessed July 31, 2020. |
[23] | Pedditizi E , Peters R , Beckett N ((2016) ) The risk of overweight/obesity in mid-life and late life for the development of dementia: A systematic review and meta-analysis of longitudinal studies. Age Ageing 45: , 14–21. |
[24] | Peters R , Warwick J , Anstey KJ , Anderson CS ((2019) ) Blood pressure and dementia: What the SPRINT-MIND trial adds and what we still need to know. Neurology 92: , 1017–1018. |
[25] | Alzheimers Disease International (2015) Dementia Statistics. https://www.alz.co.uk/research/statistics, Accessed July 31, 2020. |
[26] | Livingston G , Huntley J , Sommerlad A , Ames D , Ballard C , Banerjee S , Brayne C , Burns A , Cohen-Mansfield J , Cooper C , Costafreda SG , Dias A , Fox N , Gitlin LN , Howard R , Kales HC , Kivimäki M , Larson EB , Ogunniyi A , Orgeta V , Ritchie K , Rockwood K , Sampson EL , Samus Q , Schneider LS , Selb æk G , Teri L , Mukadam N ((2020) ) Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 396: , 413–446. |
[27] | Anstey KJ , Kingston A , Kiely KM , Luszcz MA , Mitchell P , Jagger C ((2014) ) The influence of smoking, sedentary lifestyle and obesity on cognitive impairment-free life expectancy. Int J Epidemiol 43: , 1874–1883. |




