Identifying Unmet Needs of Family Dementia Caregivers: Results of the Baseline Assessment of a Cluster-Randomized Controlled Intervention Trial
Abstract
Background:
Caregivers providing informal care for people with dementia (PwD) often report unmet needs, burden, and health impairments. Optimal support for family dementia caregivers will likely benefit from better understanding and assessment of the prevalence and types of caregivers’ unmet needs and associated socio-demographic and clinical characteristics.
Objective:
The present study investigates 1) the number and types of caregivers’ unmet needs, 2) socio-demographic and clinical characteristics of both PwD and caregivers, and 3) caregivers’ burden and health-related outcomes that are related to caregivers’ unmet needs.
Methods:
The present analyses are based on cross-sectional data of n = 226 dyads of caregivers and their community-dwelling PwD participating in a comprehensive standardized, computer-based caregivers’ needs assessment within a general practitioner (GP)-based, cluster-randomized intervention trial.
Results:
A total of n = 505 unmet needs were identified for n = 171 caregivers from the intervention group at baseline. Only 24.3% caregivers reported no unmet need (n = 55), whereas 75.7% caregivers had at least one unmet need (n = 171). Caregivers had on average 2.19 unmet needs (mean = 2.19, SD = 2.15). Specifically, 53.1% of caregivers had one up to three unmet needs (n = 120), 18.6% (n = 42) had three up to six unmet needs, and 4.0% (n = 9) had more than six unmet needs.
Discussion:
Our results underline the importance of a comprehensive needs assessment for family dementia caregivers to develop and implement concepts that can provide family dementia caregivers with optimal support.
INTRODUCTION
The majority of people with dementia (PwD) are cared for at home mainly by family caregivers such as spouses, children/offspring, daughters- and sons-in-law, or friends [1]. Caring for PwD as for many other chronic diseases poses a major burden due to its progressive nature, long duration, and the lack of disease modifying treatments. In addition, the change in PwD cognitive abilities and in personal traits is particularly burdensome for the family caregivers. Family caregivers play an important role in providing nursing care as well as physical and emotional support, assisting with medication use, and coping with behavioral symptoms, personality changes, and loss of communication, as well as coordinating health care services for PwD [2]. The amount of time, informal labor, and resources depends in particular on the symptoms of the disease (e.g., types, severity), comorbidity, as well as social, personal, and relationship-related factors of PwD and their caregivers [2]. Previous evidence revealed that family dementia caregivers reported high levels of physical, psychological, emotional, and social burden as well as health impairments [3]. In addition, caregivers’ burden and health impairments are associated with worse outcomes for PwD including behavioral and psychiatric symptoms, early institutionalization, low quality of life, and higher mortality [4, 5].
Overall, the level of burden and associated health-impairments of caregivers caring for PwD are on average higher than for almost all other diseases of old age [6]. Furthermore, previous studies indicate that caregivers of PwD demonstrate higher levels of unmet needs as well as lower levels of service utilization and lower identification rates of unmet needs by professionals compared to other family caregivers, which hamper family dementia caregivers’ physical and mental health [7]. For example, a recent study showed that medical practitioners underestimate physical and psychological conditions of dementia family caregivers at a doctor’s visit [8]. One third of caregivers with serious mental disorders was overlooked by physicians. Consequently, neither had they access to professional help nor were they advised to seek professional help for their condition [8]. PwD prefer to remain in their familiar environment as long as possible. At the same time, health policy supports community-dwelling of PwD due to lower health care costs [9]. Therefore, one may expect that the social and economic value of family dementia caregiving will increase considerably in the future. However, in order to fulfill their role, caregivers must have access to support fitting their needs. This requires comprehensive assessment of caregivers’ unmet needs.
There are different approaches to identify family dementia caregivers’ unmet needs (for reviews, see [10, 11]). Referring to these reviews, a common approach involves solely the perspective of caregivers. This approach identifies the burden experienced by caregivers of PwD focusing on several types of burden (e.g., Zarit Burden Interview, Caregiver Burden Inventory) or physical and psychological outcomes (e.g., Geriatric Depression Scale). While these approaches provide estimates of the magnitude of the burden and health impairments experienced by the caregivers, they do not cover the extent to which caregivers or health care professionals perceive that they require support. A different approach focusses on the perspective of health care professionals by rating the unmet needs of caregivers [12]. Previous studies indicate considerable discrepancies between professionals’ assessment of caregivers’ unmet needs and caregivers’ own appraisal of their unmet needs revealing that in isolation this approach may not fully capture the unmet needs of family caregivers of PwD [13]. Assessing unmet needs of caregivers for PwD should involve both the caregiver and the professional perspective, given the high discrepancy between both perspectives.
Accordingly, recent reviews suggest the importance of needs assessments that identify caregivers’ needs in different areas [10, 11]. A comprehensive needs assessment allows an estimation of the prevalence of caregivers’ needs and the magnitude of help required. That, in turn, enables researchers to develop targeted, individualized interventions for caregivers [14]. It is valuable for interventional health care research, because it enables the identification of domains within caregivers reported needs for support. Thus, a comprehensive assessment permits targeting support and interventions necessary for caregivers to fulfill the demanding caregiving role.
By investigating 85 empirical studies of dementia family caregivers’ unmet needs measurements [10] a recent review emphasized four measures of family dementia caregivers’ unmet needs: primary subjective stressor [15], unmet needs measure [16], caregivers’ needs checklist for dementia [17], and caregivers needs assessment for dementia [18]. The review highlights the need for measures to assess the unmet needs of family dementia caregivers that include a comprehensive range of domains (i.e., caregivers’ own physical, emotional, social, and support needs, as well as caregivers’ need for help when providing care to PwD). While most of the measures include caregivers’ need for information, emotional support, services support, financial/legal support, managing symptoms and activities of daily living, no measure assesses other important caregiving tasks such as advocating on behalf of PwD in healthcare systems, assisting in maintaining functional independence and self-determination as well as providing emotional support to PwD (for reviews, see [10, 11]). Referring to a previous review [10], the measures focus on aspects of the caregiving role, but none of these measures includes caregivers’ own physical, emotional, social, and psychological health outcomes. Accordingly, the authors call for a measure that focusses on both the caregiving role domains and health-related outcomes to ensure that the caregivers’ unmet needs are comprehensively represented.
In absence of comprehensive primary data concerning unmet needs of community-dwelling family dementia caregivers on caregiving domains and health-related outcomes, the objective of the present study is to describe the number and types of unmet needs among family dementia caregivers and associated socio-demographic and clinical factors. Furthermore, the dimensions of caregivers’ burden as well as their physical and mental health are analyzed.
MATERIALS AND METHODS
Trial design
This study examined cross-sectional baseline data on n = 226 dyads of caregivers and community-dwelling PwD retrieved from a comprehensive standardized, computer-based needs assessment within a general practitioner (GP)-based, cluster-randomized intervention trial (ClinicalTrials.gov Identifier: NCT01401582). The goal of this GP-based, cluster-randomized intervention trial with two arms (i.e., intervention versus control “care as usual” group) was to evaluate a collaborative Dementia Care Management (DCM) program that aims to provide optimum care to community-dwelling PwD in Germany. The study protocol was approved by the Ethical Committee of the Chamber of Physicians of Mecklenburg-Western Pomerania, Germany (registry number BB 20/11). The design, eligibility and inclusion criteria of the overall trial have been defined elsewhere [19].
Study procedures and participants
From a total of n = 854 GPs in five municipalities of Mecklenburg-Western Pomerania, n = 136 GPs (16%) gave written informed consent to participate in this trial and were randomized into the control or the intervention group (1:1 randomization). GPs systematically screened patients for dementia (eligibility criteria: age≥70 years, living at home) using a screening instrument for cognitive impairment in dementia (DemTect, [20]). Patients who were screened positive for dementia (DemTect < 9) and met the inclusion criteria were comprehensively informed about the study and were invited to participate. The DemTect screening procedure is a personal interview-based instrument including five tasks (i.e., recall of word list, number transcoding task, word fluency task, digit span reverse and delayed recall of word list) and is widely used for dementia screening in GPs in Germany [21]. However, our previous studies revealed that only 40% of patients who were screened positive for dementia (DemTect < 9) had been formally diagnosed with dementia which is in the range of international reference data ranging from 20% to 50% [22]. Specifically, in our sample, 58% of patients with mild cognitive impairment, 48% of patients with moderate cognitive impairment, and 46% of patients with severe cognitive impairment remained undiagnosed [22]. Regarding the distribution of differential diagnoses, unspecified dementia was diagnosed in 53%, vascular dementia in 24%, and Alzheimer’s disease in 19% of the participants [22]. Furthermore, our previous studies showed that screening improved the identification of dementia considerably with an increase from 40% before screening to 70% after a positive DemTect screening (69% with “unspecified dementia”) [23]. According to the medical files of the participating GP practices in our trial, more than 53% of the newly diagnosed patients received their formal diagnosis on the day of the screening [23]. Patients who received a formal diagnosis after screening were significantly more functionally impaired, more likely to be female, and more often treated with anti-dementia drugs [24].
A total of n = 407 people screened positive for dementia gave written informed consent to participate. Of these, n = 317 people screened positive for dementia provided contact to a caregiver. Caregivers were informed by the treating GP of the PwD at the GP practice and by our dementia-specific qualified study nurses at patients’ homes. They were asked to participate and had to provide written informed consent. We only included family dementia caregivers who are the primary caregivers and excluded professional caregivers.
At baseline, n = 226 caregivers and people screened positive for dementia dyads were randomized to the intervention group and n = 91 caregivers and people screened positive for dementia dyads to the control group. Since the assessment of unmet needs was conducted solely in the intervention group, the present analysis is based on these n = 226 dyads of people screened positive for dementia and their caregivers. Thus, we did not investigate the baseline data of the control group. While the main focus of our study is to investigate 1) the number and types of caregivers’ unmet needs, 2) socio-demographic and clinical characteristics of both PwD and caregivers, and 3) caregivers’ burden and health-related outcomes that are related to caregivers’ unmet needs, we did not analyze the efficacy of the intervention in the present study. The efficacy of the intervention has already been published (including power estimation, flow charts, drop out analysis, and the effect of the intervention on primary outcomes such as quality of life, behavioral, and psychological symptoms of dementia, pharmacotherapy with antidementia drugs, and use of potentially inappropriate medication) [25].
In this GP-based, cluster-randomized intervention trial, dementia-specific qualified study nurses performed a comprehensive needs assessment in the intervention group with family dementia caregivers at the participants’ home to identify their individual unmet needs and developed a tailored intervention plan to address these needs in close cooperation with the caregiver. A comprehensive standardized computer-based assessment of unmet needs included a battery of standardized questionnaires and tests. Additionally, the dementia-specific qualified study nurses (for a detailed overview of the qualification and curriculum, see [26]) could identify additional unmet needs and included these in their assessments.
We developed the qualification in seven steps, starting with an expert survey to evaluate: 1) the scope of tasks of the Dementia Care Manager, 2) the training needs based on a comparison with the vocational nursing training, and 3) the specific qualification contents [21]. Based on the results of this survey, the pilot of the curriculum was developed, followed by 4) the pilot implementation of the theoretical qualification modules, 5) practical work as Dementia Care Managers, and 6) the evaluation of the curriculum to revise the DCM curriculum [26]. Our results revealed the requirements for a specific qualification for nurses to assure a need-oriented care for PwD. The qualification includes seven modules (i.e., basics of health care supply of PwD and their caregivers, medical aspects, nursing, communication and counselling techniques, network associated dementia health care supply, computerized needs assessment, practice period) [26].
Measures
In the present analysis, an unmet need is defined as a need that was either 1) identified automatically by the computerized needs assessment and confirmed by dementia-specific qualified study nurses or 2) additionally identified by dementia-specific qualified study nurses as a need that should be addressed [27]. The present caregivers needs’ assessment includes a comprehensive range of domains (i.e., social integration, mental and physical health, social, legal, and financial affairs) focusing on both the caregiving role domains and health-related outcomes (e.g., HABC-Monitor [28]). A detailed description of the entire assessment of the present study is given in Table 1.
Table 1
Domains, categories, and measurements of caregivers’ unmet needs
| Domain | Category | Measurements |
| Social Integration | Caregiver supporting groups | Berlin inventory of caregivers’ burden with dementia patients- BIZA-D [30] |
| Personal constraints and challenges of caregiver | Berlin inventory of caregivers’ burden with dementia patients- BIZA-D [30] | |
| Professional role conflicts of caregiver | Berlin inventory of caregivers’ burden with dementia patients- BIZA-D [30] | |
| Family role conflicts of caregiver | Berlin inventory of caregivers’ burden with dementia patients- BIZA-D [30] | |
| Mental health | Depression and anxiety of PwD | HABC-Monitor [28] |
| Aggression and resistance of PwD | HABC-Monitor [28] | |
| Hallucination and delusion of PwD | HABC-Monitor [28] | |
| Sleep disturbance of PwD | HABC-Monitor [28] | |
| Repetitive behavior of PwD | HABC-Monitor [28] | |
| Impulsive behavior of PwD | HABC-Monitor [28] | |
| Safety of PwD | HABC-Monitor [28] | |
| Behavior change of PwD | Berlin inventory of caregivers’ burden with dementia patients- BIZA-D [30] | |
| Changes in personality and relationship between PwD and caregiver | Berlin inventory of caregivers’ burden with dementia patients- BIZA-D [30] | |
| Quality of life and mental health of caregiver | HABC-Monitor [28] | |
| Physical health | Mobility, balance and falls of PwD | HABC-Monitor [28] |
| Physical health of caregiver | HABC-Monitor [28] | |
| Social, legal, and financial affairs | Social, legal, and financial issues of caregiver | HABC-Monitor [28] Berlin inventory of caregivers’ burden with dementia patients- BIZA-D [30] |
The development of the needs assessment is based on German guidelines for evidence-based diagnostics and treatment of dementia, a review of current literature, meetings, and symposia with experts in the field, as well as the scientific advisory board of DelpHi-MV [27]. The needs assessment comprises three key areas: 1) management of treatment and care, 2) medication management, and 3) caregiver support and education. A detailed description of the comprehensive unmet needs assessment is published elsewhere [29]. Each identified unmet need consists of defined algorithms that contain the trigger condition(s) derived from standardized baseline and/or in-depth assessment that activate(s) a specific intervention task and at least one criterion for successful completion of that task [29].
Our previous studies compared the identified unmet needs and the interventions that were recommended before and after the implementation of the computerized needs assessment [27]. After the implementation of the computerized needs assessment, the number of identified needs increased by 85% [27]. These results emphasize the difficulty of systematically detecting unmet needs of PwD and family caregivers within the complexity of their home caring situations. Furthermore, the implementation of computerized needs assessment resulted in an improved adherence to the intervention protocol and increased the comprehensiveness of dementia care management [27]. To evaluate the feasibility and acceptability of the computerized needs assessment, a survey was conducted among the dementia-specific qualified study nurses (n = 6) [27]. The dementia-specific qualified study nurses evaluated the computerized needs assessment as very helpful and would like to use it in the future work [27].
Caregivers’ needs assessment was entered directly into a tablet-PC by the dementia-specific qualified study nurses and immediately processed. The caregivers’ needs assessment comprises 19 categories with (a) four categories focusing on social integration, (b) ten categories directed to mental health, (c) four categories concentrating on physical health, and (d) one category containing social, legal, and financial affairs. Based on the identified unmet needs of each individual caregiver and their PwD at the baseline assessment, the computer-based system generates an individual preliminary list of recommendations to encounter these unmet needs [27]. To check adherence to the study protocol as well as to assess the adequateness of the predefined categories, this list was discussed and validated in a weekly interdisciplinary case conference (including a nursing scientist, a neurologist/psychiatrist, a psychologist, and a pharmacist). Specifically, a summary of the caregivers’ needs assessment, clinical characteristics, and the list of recommendations were presented by the dementia-specific qualified study nurses in the interdisciplinary case conference [27]. During the case conference, an interdisciplinary expert panel debated in an open discussion the concordance of findings between the computerized caregivers’ needs assessment, the evaluation of the dementia-specific qualified study nurses, and the list of recommendation (including clarifications, opinions, justifications, operational definitions, and categories). By the end of the case conference, the interdisciplinary expert panel had agreed to or changed the predefined categories by a majority consensus [27]. For the present analysis, the variables under investigation concerning caregivers were age, sex, relation to the PwD, education, hours spent for caregiving, employment status, income per month, caregiver burden (Berlin inventory of caregivers’ burden with dementia patients- BIZA-D [30]), physical and mental health (12-Item Short Form Survey [31]), as well as syndromes of somatization, depression, and anxiety (Brief Symptom Inventory 18 [32]).
Since previous research revealed that caregiver burden among PwD caregivers is a multifaceted and highly complex concept [33], we investigated several caregiver burden dimensions and health-related outcomes of caregivers in detail. However, previous studies often use one-dimensional constructs and measuring instruments that do not distinguish between these multifaceted caregivers’ burden dimensions. Thus, generating a summary score of caregivers’ burden in contrast to differentiate between multifaceted caregivers’ burden dimensions leads to vague findings and difficulties in interpreting and applying these results in scientific and clinical practice [30]. Given the fact that previous research has shown caregiver burden to be composed out of different dimensions, failing to distinguish between these dimensions may negatively affect comparability, analysis, and interpretation of results as well as their associated implications. Thus, conceptualization and development of assessments, prevention, and intervention programs necessarily depend on an understanding and classification of the sources of burden (i.e., caregivers’ burden dimension) and their consequences (i.e., health outcomes).
Referring to PwD, we analyzed age, sex, living situation (alone/not alone), living in a partnership, cognitive status assessed by Mini Mental State Test (MMST) [34], functional status using the Bayer Activities of Daily Living Scale (B-ADL) [35], and depression assessed by the Geriatric Depression Scale [36]. These variables were selected in compliance with our per protocol analysis. In addition, these variables were shown to be associated with family dementia caregivers’ unmet needs in previous studies (for reviews, see [9, 10]).
Statistical analyses
The reporting of this study follows the CONSORT-statement and its extensions regarding cluster-randomized, pragmatic trials with non-pharmacological treatments. The design, eligibility, inclusion criteria, and statistical analyses plan of the overall trial have been described in detail elsewhere [19] (ClinicalTrials.gov Identifier: NCT01401582). Data analysis and management were conducted using Stata/IC Version 13.1. Missing data was imputed by multiple imputations via chained equations. Given the fact, that all data was obtained by dementia-specific qualified study nurses in a personal interview at patients’ home, we have a relatively low rate of missing data ranging from 0% (e.g., caregivers’ gender, caregivers’ age) to 3.98% (depression of PwD). We investigated the number and type of unmet needs across different domains and categories in Table 2. Metric variables were summarized by means as well as standard deviations (SD) and nominal variables were presented by proportion in Table 3.
Table 2
Number and types of caregivers’ unmet needs (n = 226)
| Type of caregivers’ unmet needs | Number of caregivers’ unmet needs | Proportion (%) |
| Total | 505 | 100 |
| Social Integration | ||
| Caregiver supporting groups | 96 | 19.0 |
| Personal constraints and challenges of caregiver | 2 | 0.4 |
| Professional role conflicts of caregiver | 4 | 0.8 |
| Family role conflicts of caregiver | 4 | 0.8 |
| Mental health | ||
| Depression and anxiety of PwD | 39 | 7.7 |
| Aggression and resistance of PwD | 18 | 3.6 |
| Hallucination and delusion of PwD | 14 | 2.8 |
| Sleep disturbance of PwD | 10 | 2.0 |
| Repetitive behavior of PwD | 15 | 3.0 |
| Impulsive behavior of PwD | 28 | 5.5 |
| Safety of PwD | 69 | 13.7 |
| Behavior change of PwD | 17 | 3.4 |
| Changes in personality and relationship between PwD and caregiver | 13 | 2.6 |
| Quality of life and mental health of caregiver | 85 | 16.8 |
| Physical health | ||
| Mobility, balance and falls of PwD | 67 | 13.3 |
| Physical health of caregiver | 12 | 2.4 |
| Social, legal, and financial affairs | ||
| Social, legal, and financial issues of caregiver | 12 | 2.4 |
Multiple entries per caregivers were possible.
Table 3
Characteristics of caregivers and their PwD (n = 226)
| Characteristic | Samples (n = 226) | Bivariate relationship to number of unmet needs |
| Caregiver | ||
| Gender | z = 0.136, p = 0.368 | |
| Female, % | 73.0 | |
| Male, % | 27.0 | |
| Age, mean (SD) | 64.55 (12.87) | r = – 0.002, p = 0.779 |
| Currently Working, % | 27.4 | z = – 0.023, p = 0.887 |
| Relationship with PwD, % | ||
| Spouse, life partner, Siblings | 46.9 | z = 0.703, p = 0.005 |
| Son/daughter, Son-in-law/daughter-in-law, Grandchildren | 49.6 | z = 0.172, p = 0.186 |
| Other | 3.5 | z = – 0.353, p = 0.385 |
| Education, % | ||
| Without degree | 2.7 | z = 0.757, p = 0.035 |
| Lower Secondary Education | 37.3 | z = 0.348, p = 0.272 |
| Higher Secondary Education | 31.1 | z = 0.062, p = 0.822 |
| Polytechnical Degree | 16.9 | z = 0.354, p = 0.249 |
| Advanced technical college certificate | 2.2 | z = 0.501, p = 0.126 |
| Higher education entrance qualification | 9.8 | z = 0.250, p = 0.434 |
| Income (net) per month, € (SD) | 1828.29 (740.29) | r = – 0.002, p = 0.545 |
| Hours spent for caring per month | 141.29 (224.21) | r = 0.001, p < 0.001 |
| Caregiver burden, mean (SD) | ||
| Objective burden due to caring) | 6.14 (0.36) | r = 0.023, p < 0.001 |
| Burden due to behavior change | 0.52 (0.06) | r = 0.140, p < 0.001 |
| Burden due to perceived conflicts between needs & | 0.55 (0.06) | r = 0.098, p < 0.001 |
| responsibilities to care | ||
| Burden due to role conflicts | 0.15 (0.04) | r = 0.196, p < 0.001 |
| SF-12 physical health of caregivers, mean (SD) | 47.43 (9.24) | r = – 0.009, p = 0.252 |
| SF-12 mental health of caregivers, mean (SD) | 52.80 (9.11) | r = – 0.034, p < 0.001 |
| BSI-18 somatization of caregivers | 1.41 (2.25) | r = 0.081, p < 0.001 |
| BSI-18 depression of caregivers | 1.04 (2.56) | r = 0.087, p < 0.001 |
| BSI-18 anxiety of caregivers | 1.50 (2.63) | r = 0.102, p < 0.001 |
| Person with Dementia (PwD) | ||
| Gender | z = 0.061, p = 0.627 | |
| Female, % | 61.6 | |
| Male, % | 38.4 | |
| Age, mean (SD) | 80.88 (5.56) | r = 0.016, p = 0.175 |
| Living in partnership, % | 54.0 | |
| Living situation (living alone), % | 47.8 | z = – 0.036, p = 0.776 |
| Severity of dementia (MMST), mean (SD) | 21.4 (5.45) | r = – 0.032, p = 0.005 |
| Depression (GDS) | z = 0.297, p = 0.072 | |
| Mild, % | 84.8 | |
| Moderate or severe, % | 15.2 | |
| Functional status (B-ADL), mean (SD) | 4.32 (2.70) | r = 0.112, p < 0.001 |
r, Spearman’s product-moment-correlation coefficient; z, Wilcoxon’s test coefficient (two-sided); p, p-values; MMST, Mini-Mental State Test ranging from 0– 30 (higher score indicates better cognitive functioning); B-ADL, Bayer Activities of Daily Living Scale ranging 0– 10 (lower score indicates better performance); GDS, Geriatric Depression Scale ranging 0– 15 (score≥6 indicates depression); SF-12, 12-Item short form survey assessing physical and mental health; BSI-18, brief symptom inventory short form assessing syndromes of somatization, depression, and anxiety.
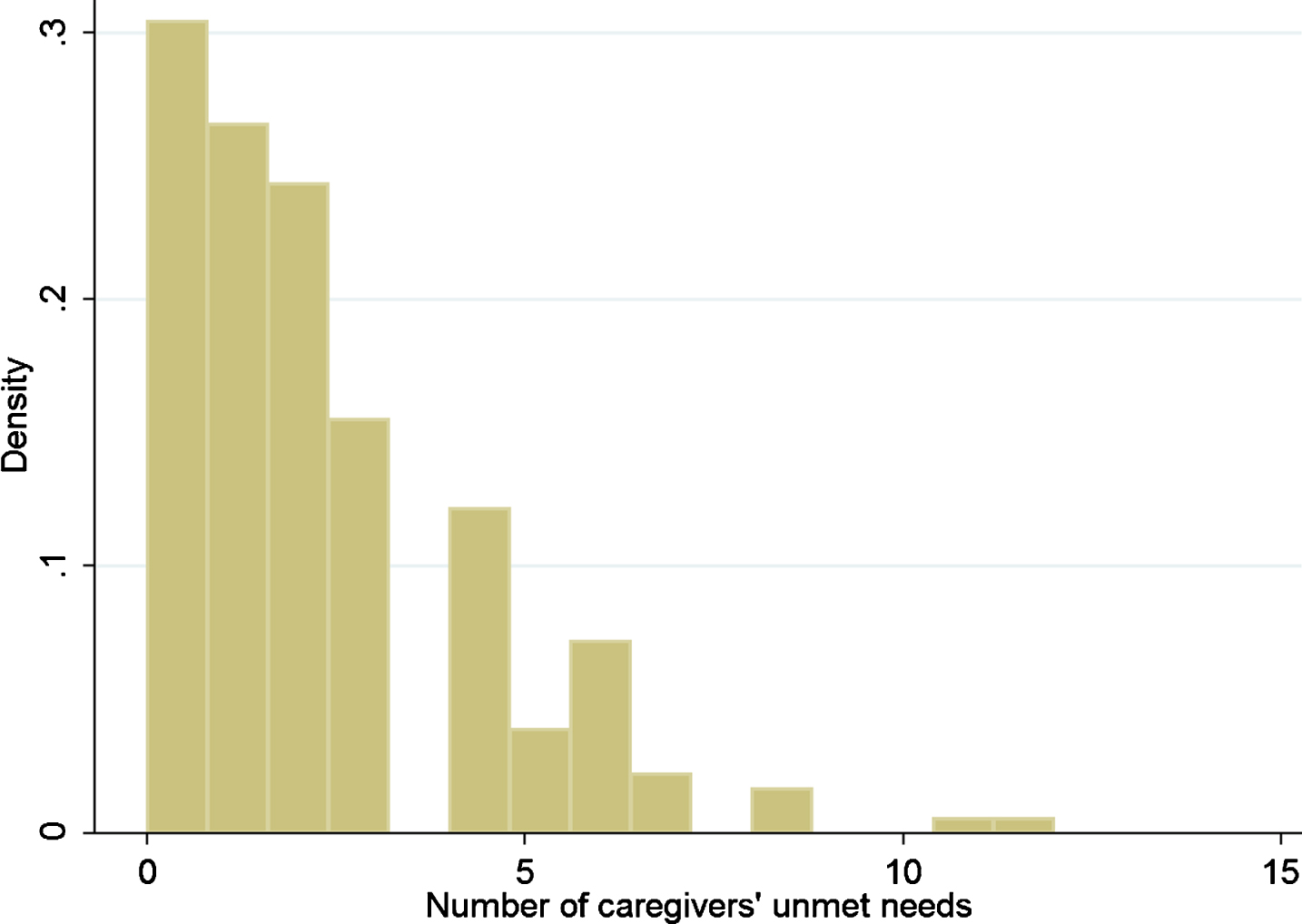
We tested the distribution of the data by graphical and numerical methods. We draw a histogram and computed the skewness and kurtosis. The histogram in Fig. 1 shows that the data are highly skewed to the right (i.e., left-leaning curve). The skewness (sk = 1.36) and the kurtosis (kurt = 5.39) confirm that the distribution is right-skewed. Furthermore, the variance of the dependent variable (var = 4.60) is nearly two times larger than the mean (m = 2.19). Thus the distribution of the number of unmet needs is displaying signs of overdispersion, that is, greater variance than might be expected in a Poisson distribution. We computed the likelihood ratio test to examine overdispersion parameter alpha. The overdispersion parameter alpha (chibar = 5.69, p = 0.01) is significantly different from zero and suggest that the dependent variable is over-dispersed and is not sufficiently described by the simpler Poisson distribution. Thus, the result of the likelihood ratio test reinforces the use of negative binomial regression.
Fig.1
Histogram of the dependent variable.
To analyze the univariate associations of socio-demographic and clinical characteristics with the number of unmet needs in Table 2, we used non-parametric tests (i.e., Wilcoxon test and Spearman‘s product-moment correlation). For multivariate analyses in Tables 4 and 5, we fitted conditional negative binomial regression models with random effects for GP to account for over-dispersed count data. Due to the stochastic dependency of PwD treated by the same GP, the GP is included as a random effect variable in the conditional negative binomial regression models. In these models we included the following predictors: caregivers’ burden, caregivers’ physical and emotional health, as well as syndromes of somatization, depression, and anxiety of caregivers. Models were adjusted for age, sex, employment status of caregivers as well as for age, sex, living situation, cognitive status, functional status, and depression of the PwD.
Table 4
Health-related factors associated with the number of caregivers’ unmet needs (n = 226)
| b | z | p | CI95– | CI95 + | |
| Covariates | |||||
| Caregiver gender (female) | 0.118 | 0.68 | 0.493 | – 0.220 | 0.456 |
| Caregiver currently working | – 0.0389 | – 0.21 | 0.830 | – 0.394 | 0.316 |
| Caregiver age | – 0.004 | – 0.63 | 0.530 | – 0.017 | 0.009 |
| PwD gender | 0.057 | 0.35 | 0.728 | – 0.262 | 0.375 |
| PwD age | 0.002 | 0.19 | 0.851 | – 0.022 | 0.027 |
| PwD living situation (living alone) | – 0.275 | – 1.96 | 0.051 | – 0.551 | 0.001 |
| PwD severity of dementia (MMST) | 0.008 | 0.60 | 0.547 | – 0.018 | 0.035 |
| PwD depression (GDS) | 0.028 | 0.17 | 0.866 | – 0.296 | 0.351 |
| PwD functional status (B-ADL) | 0.096 | 3.21 | 0.001 | 0.037 | 0.154 |
| Predictors | |||||
| Caregivers SF– 12 physical health | – 0.0078 | – 1.02 | 0.308 | – 0.023 | 0.007 |
| Caregivers SF– 12 mental health | – 0.025 | – 2.84 | 0.005 | – 0.042 | – 0.008 |
| Caregivers BSI– 18 somatization | 0.009 | 0.36 | 0.716 | – 0.041 | 0.060 |
| Caregivers BSI-18 depression | – 0.028 | – 0.99 | 0.320 | – 0.083 | 0.027 |
| Caregivers BSI– 18 anxiety | 0.063 | 2.57 | 0.010 | 0.015 | 0.111 |
| R 2 | 0.25 |
Conditional negative binomial regression model with random effects for GP; Number of caregivers’ unmet needs was the predictor of interest; p-values are given one-sided; CI, Confidence interval; MMST, Mini-Mental State Test ranging from 0– 30 (higher score indicates better cognitive functioning); B-ADL, Bayer Activities of Daily Living Scale ranging 0– 10 (lower score indicates better performance); GDS, Geriatric Depression Scale ranging 0– 15 (score≥6 indicates depression); SF– 12, 12– Item short form survey assessing physical and mental health; BSI– 18, brief symptom inventory short form assessing syndromes of somatization, depression, and anxiety.
Table 5
Caregivers’ burden associated with the number of caregivers’ unmet needs (n = 226)
| b | z | p | CI95– | CI95 + | |
| Covariates | |||||
| Caregiver gender (female) | 0.029 | 0.18 | 0.857 | – 0.287 | 0.345 |
| Caregiver currently working | 0.165 | 0.92 | 0.357 | – 0.186 | 0.515 |
| Caregiver age | 0.002 | 0.30 | 0.764 | – 0.011 | 0.015 |
| PwD gender | 0.055 | 0.34 | 0.732 | – 0.262 | 0.373 |
| PwD age | – 0.004 | – 0.35 | 0.730 | – 0.027 | 0.019 |
| PwD living situation (living alone) | – 0.024 | – 0.18 | 0.859 | – 0.286 | 0.239 |
| PwD severity of dementia (MMST) | 0.027 | 1.99 | 0.047 | 0.000 | 0.053 |
| PwD depression (GDS) | – 0.066 | – 0.44 | 0.662 | – 0.362 | 0.230 |
| PwD functional status (B-ADL) | 0.003 | 0.10 | 0.919 | – 0.061 | 0.068 |
| Predictors | |||||
| Objective burden due to caring | 0.016 | 3.50 | 0.000 | 0.007 | 0.026 |
| Burden due to behavior change | 0.116 | 5.36 | 0.000 | 0.074 | 0.158 |
| Burden due to perceived conflicts between needs & | – 0.016 | – 0.75 | 0.453 | – 0.059 | 0.026 |
| responsibilities to care | |||||
| Burden due to role conflicts | – 0.005 | – 0.08 | 0.935 | – 0.130 | 0.120 |
| R 2 | 0.36 |
Conditional negative binomial regression model with random effects for GP; Number of caregivers’ unmet needs was the predictor of interest; p-values are given one-sided; CI, Confidence interval; MMST, Mini-Mental State Test ranging from 0– 30 (higher score indicates better cognitive functioning); B-ADL, Bayer Activities of Daily Living Scale ranging 0– 10 (lower score indicates better performance); GDS, Geriatric Depression Scale ranging 0– 15 (score≥6 indicates depression); SF– 12, 12– Item short form survey assessing physical and mental health; BSI– – 18, brief symptom inventory short form assessing syndromes of somatization, depression, and anxiety.
RESULTS
A total of n = 505 unmet needs were identified for n = 171 caregivers in our sample. Only 24.3% caregivers had no unmet need (n = 55), whereas 75.7% caregivers had at least one unmet need (n = 171). Caregivers had on average 2.19 unmet needs (SD = 2.15). The number of unmet needs per caregiver ranged from none to twelve. Specifically, 53.1% caregivers had one up to three unmet needs (n = 120), 18.6% (n = 42) had four up to six unmet needs, and 4.0% (n = 9) had seven or more unmet needs. Caregivers’ unmet needs were identified across 17 different categories.
Specifically, the majority of unmet needs were related to caregiver supporting groups (19.0%), caregivers’ quality of life and mental health (16.8%), handling safety (13.7%), mobility, balance and falls of PwD (13.3%), coping with depression and anxiety of PwD (7.7%), as well as managing impulsive behavior of PwD (5.5%). The distribution of caregivers’ unmet needs across different domains and categories is shown in Table 2.
The majority of caregivers were women (73.0%) with a mean age of 64.6 years, with averaged 141.3 hours spent for informal caring per month and with lower (37.3%) or higher (31.1%) secondary education. Caregivers mostly cared for female PwD (61.6%) with an average age of 80.9 years, predominantly scoring in the range of mild dementia (MMSTmean = 21.4), and moderately impaired functional status (B-ADL mean = 4.32).
Referring to socio-demographic factors, the results of our univariate analyses showed that a higher number of caregivers’ unmet needs was statistically significantly associated with lower education of caregivers (z = 0.757, p = 0.035), being a spouse, life partner, or sibling of the PwD (z = 0.703, p = 0.005), higher degree of dementia severity (z = – 0.032, p = 0.005), and higher impairment of functional status of PwD (z = 0.112, p < 0.001). With reference to caregivers’ burden and health, the results of our univariate analyses showed that a higher number of caregivers’ unmet need was significantly associated with high levels of objective burden due to caring (z = 0.023, p < 0.001), subjective burden due to behavior change (z = 0.140, p < 0.001), subjective burden due to perceived conflicts between needs and responsibilities to care (z = 0.098, p < 0.001), subjective burden due to role conflicts (z = 0.196, p < 0.001), somatization (z = 0.081, p < 0.001), depression (z = 0.087, p < 0.001), anxiety (z = 0.102, p < 0.001), and lower levels of mental health (z = – 0.034, p < 0.001) of caregivers. The characteristics of caregivers and PwD as well as a bivariate relationship between these characteristics and the respective number of caregivers’ unmet needs are shown in Table 3.
The results of the multivariate analyses confirmed these findings. Specifically, the variable caregivers’ mental health has a coefficient of b = – 0.025 (p = 0.005, CI95– = – 0.042, CI95 + = – 0.008), which is statistically significant (see Table 4). This means that for each one-unit increase in caregivers’ mental health, the expected log count of the number of unmet needs decreases by 0.025. Furthermore, the variables caregivers’ anxiety (b = 0.063, p = 0.010, CI95– = 0.015, CI95 + = 0.111), caregivers’ subjective burden due to behavior change (b = 0.116, p < 0.001, CI95– = 0.074, CI95 + = 0.158), and caregivers’ objective burden due to caring (b = 0.016, p < 0.001, CI95– = 0.074, CI95 + = 0.158) show statistically significant coefficients (see Tables 4 and 5). Accordingly, for each one-unit increase in caregivers’ anxiety, subjective burden due to behavior change, and objective burden due to caring, the expected log count of the number of unmet needs increases by 0.025 (caregivers’ anxiety), 0.116 (caregivers’ subjective burden due to behavior change), and 0.016 (caregivers’ objective burden due to caring).
DISCUSSION
The present study provides empirical data concerning family dementia caregivers’ unmet needs of community-dwelling people in the primary care sector and investigates the relation between caregivers’ unmet needs and several caregivers’ burden dimensions as well as health-related outcomes. Thus, our results provide new information on family dementia caregivers’ unmet needs, with a particular focus on the relation between caregiver burden and health-impairments. By conducting a comprehensive caregivers’ needs assessment, we identified specific unmet caregiver needs that have been overlooked or underestimated in previous studies, and we revealed their relation to caregiver burden and health-impairments. Our study has a number of theoretical and practical implications. First, our findings are in line with previous research (for reviews, see [9, 10]) and highlight that family dementia caregivers with a higher number of unmet needs were at an increased risk for caregiver burden, as well as mental, and physical health-impairments. Accordingly, health care researchers should consider the prevalence, types, and relations of caregivers’ unmet needs in the development of targeted, multimodal intervention programs [37]. Specifically, our findings revealed that 75.7 % of family dementia caregivers had at least one unmet need and on average 2.19 unmet needs, which should be addressed more consequently in health care in order to provide appropriate support for caregivers. The number of unmet needs identified by a comprehensive standardized computer-based needs assessment ranged from none to the maximum of twelve unmet needs per caregiver. The majority of unmet needs were detected in the categories of lacking access to caregiver supporting groups, low caregivers’ quality of life and mental health, handling safety, mobility, balance, and falls of PwD, coping with depression and anxiety of PwD, as well as managing impulsive behavior of PwD. However, previous studies conclude that health care researchers developed effective, easily available and manageable support programs for family dementia caregivers, but criticize the inadequate translation in the German health care system as well as the associated limitations with respect to availability, usability, and financing for caregivers [37]. By revealing the high number of caregivers’ unmet needs and the associated high levels of caregiver’ burden and health-impairments, our study emphasizes the urgent need to provide easily available and manageable as well as financeable support programs that caregivers can easily access to use and benefit from.
Secondly, following the methodological recommendations of previous reviews, we developed a comprehensive needs assessment including a full range of caregivers’ unmet needs domains as well as caregivers’ own physical, emotional, social, and psychological health outcomes. Our results show that the number of unmet needs is related to several caregivers’ burden dimensions and caregivers’ own physical, emotional, social, and psychological health outcomes, confirming the need of assessing these different domains in caregivers’ needs assessment. Furthermore, we developed a comprehensive needs assessment allowing for determining the prevalence of caregivers’ needs and the magnitude of help required by caregivers. This comprehensive needs assessment enables health care researchers and providers to develop and provide targeted, individualized interventions for caregivers [14]. Specifically, our results reveal that a higher number of caregivers’ unmet needs is associated with less education, being a spouse, life partner or sibling of the PwD, caring for PwD with a higher degree of dementia severity, and higher impairment of functional status. We assume that caregivers with less education and older age (i.e., being a spouse, life partner, or sibling of the PwD) may lack access to health care as well as caregiver support and thus, may need a comprehensive identification of unmet needs and easily available support. Accordingly, health care researchers and providers should be aware of this underserved target population and may develop targeted, easily available and manageable support for the family dementia caregivers. In addition, our findings indicate that higher dementia severity (i.e., dementia severity, high impairment of functional status) is associated with a higher number of caregivers’ unmet needs. Our results demonstrate that caregivers need more support in the progression of the disease to fulfill their demanding role.
Furthermore, our results indicate the important relation between caregivers’ unmet needs and their burden as well as their health impairments. Thus, family dementia support programs and interventions should include the essential domains of objective (i.e., objective burden due to caring) and subjective burden (behavior change, perceived conflicts between needs and responsibilities to care, and role conflicts) as well as syndromes of somatization, depression, anxiety, and impaired mental health of caregivers as a minimum. In line with previous research and our findings, we suggest that dementia family caregivers’ unmet needs are multifaceted and highly complex, so that future studies should comprehensively investigate different domains of unmet needs, burden dimensions, and health-related outcomes to develop and provide individually tailored and effective caregiver support interventions and programs [33]. Referring to multifaceted caregivers’ burden dimensions, our results revealed that a higher number of caregivers’ unmet needs was statistically significantly associated with caregivers’ subjective burden due to behavior change and caregivers’ objective burden due to caring. A recent review [38] showed that caregivers’ burden caused by behavior change and caring is more stressful for caregivers than cognitive and functional problems of PwD due to their challenging nature. In this context, caregivers might be less prepared to handle such behavior changes and to provide care adequately in the course of the disease. Specifically, behavior changes negatively impact the personality of PwD and are associated with more caregiver stress, need for support and health impairments than other aspects of the disease [38].
Thus, our results emphasize the relevance to assess caregivers’ unmet needs and provide tailored support especially when caregivers are confronted with behavior changes of PwD and demanding care tasks to decrease caregivers’ burden and health-impairments.
Finally, the number of caregivers’ unmet needs in the present study is comparable with previous research reporting that 85% of caregivers have at least one unmet need (for reviews on prevalence, see [10] [11]) on average. Referring to the results of these reviews, our caregivers’ needs assessment is one of the first assessments that includes both caregiving role domains and health-related outcomes.
In summary, the present study showed that family dementia caregivers have a broad range of unmet needs with varying individual patterns. Our findings emphasize the importance of a comprehensive needs assessment that allows the identification of all unmet needs of caregivers as the basis for a tailored intervention that can address these individual caregivers’ needs.
Limitations
Our findings must be interpreted within the context of several limitations. First, the generalizability of our results might be limited to caregivers of community dwelling PwD in the earlier phases of the disease. Our sample scored in cognitive tests mainly in the range of mild to moderate dementia. Second, since our study data was analyzed cross-sectionally, causal relationships between caregivers’ unmet needs and their burden as well as health-impairments could not be investigated. Furthermore, caregiving for PwD includes diverse and challenging care tasks that are often associated with a broad range of unmet needs domains and health-related outcomes. Therefore, it is not possible to detect every specific existing unmet need in every family caregiver. Furthermore, previous research revealed that specific caregivers’ unmet needs domains differently impact caregivers’ burden (e.g., caregivers’ unmet need for social support and professional mental health care) [39]. While the present sample is underpowered to analyze these different effects, future studies should investigate the impact of different caregivers’ unmet needs domains on caregivers’ burden and health impairments.
Finally, there is a limitation in the comparability of our results to other health care systems and previous studies using different caregivers’ unmet needs assessments. The standardized, computer-based assessment allows a rather comprehensive needs assessment. However, it has been specifically developed for the present (GP)-based, cluster-randomized intervention trial and may not be comparable with previous instruments for needs assessment. Thus, to increase the comparability to other studies, internationally agreed upon and wider spread measures are necessary to compare and validate several caregivers’ unmet needs assessment in future studies.
Conclusion
Our results reveal that in order to provide efficient support for family dementia caregivers it is necessary to conduct a comprehensive needs assessment including domains of the caregiving role, caregiver burden as well as psychological and physiological health. A major strength of our study is that it emphasizes key domains of a comprehensive assessment for caregivers’ unmet needs in a home setting and provides a standardized, computer-based tool that can be applied in research and clinical settings. While there is an urgent need for easily manageable and available measurements of caregivers’ unmet needs, future studies might investigate barriers and facilitators for the translation of targeted interventions in national health care systems including health care services and public health policy.
ACKNOWLEDGMENTS
We would like to thank all caregivers and persons with dementia (PwD), general practitioners, and pharmacists for the committed cooperation. We would also like to thank the following experts (in alphabetical order): Ines Abraham, Kerstin Albuerne, Grit Assmann, Vaska Boehmann, Kathleen Dittmer, Thomas Fiss, Daniel Fredrich, Jana Hubert, Ulrike Kempe, Saskia Moll, Andrea Pooch, Henriette Rau, and Sabine Schmidt.
The study was funded by the German Center of Neurodegenerative Diseases (DZNE) and the University Medicine of Greifswald.
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/18-0244r2).
REFERENCES
[1] | Prince M , Comas-Herrera A , Knapp M , Guerchet M , Karagiannidou M ((2016) ) The role of primary care in the dementia healthcare system. In World Alzheimer Report 2016. Improving healthcare for people living with dementia, Prince M , Comas-Herrera A , Knapp M , Guerchet M , Karagiannidou M eds. Alzheimer’s Disease International, London, pp. 21–46. |
[2] | Chiao CY , Wu HS , Hsiao CY ((2015) ) Caregiver burden for informal caregivers of patients with dementia: A systematic review. Int Nurs Rev 62: , 340–350. |
[3] | Thyrian JR , Winter P , Eichler T , Reimann M , Wucherer D , Michalowsky B , Dreier A , Zarm K , Hoffmann W ((2017) ) The burden of caring for people screened positive for dementia in primary care - results of the DelpHi-study. Z Gerontol Geriatr 50: , 4–13. |
[4] | van der Lee J , Bakker TJ , Duivenvoorden HJ , Droes RM ((2014) ) Multivariate models of subjective caregiver burden in dementia: A systematic review. Ageing Res Rev 15: , 76–93. |
[5] | Etters L , Goodall D , Harrison BE ((2008) ) Caregiver burden among dementia patient caregivers: A review of the literature. J Am Acad Nurse Pract 20: , 423–428. |
[6] | Kim H , Chang M , Rose K , Kim S ((2012) ) Predictors of caregiver burden in caregivers of individuals with dementia. J Adv Nurs 68: , 846–855. |
[7] | Stirling C , Andrews S , Croft T , Vickers J , Turner P , Robinson A ((2010) ) Measuring dementia carers’ unmet need for services - an exploratory mixed method study. BMC Health Serv Res 10: , 122. |
[8] | Riedel O , Klotsche J , Wittchen HU ((2016) ) Overlooking informal dementia caregivers’ burden. Res Gerontol Nurs 9: , 167–174. |
[9] | McCabe M , You E , Tatangelo G ((2016) ) Hearing their voice: A systematic review of dementia family caregivers’ needs. Gerontologist 56: , e70–e88. |
[10] | Mansfield E , Boyes AW , Bryant J , Sanson-Fisher R ((2017) ) Quantifying the unmet needs of caregivers of people with dementia: A critical review of the quality of measures. Int J Geriatr Psychiatry 32: , 274–287. |
[11] | Bangerter LR , Griffin JM , Zarit SH , Havyer R ((2017) ) Measuring the needs of family caregivers of people with dementia: An assessment of current methodological strategies and key recommendations. J Appl Gerontol, doi: 10.1177/0733464817705959 |
[12] | Seddon D , Robinson C ((2015) ) Carer assessment: Continuing tensions and dilemmas for social care practice. Health Soc Care Community 23: , 14–22. |
[13] | Cohen-Mansfield J , Frank J ((2008) ) Relationship between perceived needs and assessed needs for services in community-dwelling older persons. Gerontologist 48: , 505–516. |
[14] | Meaney AM , Croke M , Kirby M ((2005) ) Needs assessment in dementia. Int J Geriatr Psychiatry 20: , 322–329. |
[15] | Bass DM , Judge KS , Snow AL , Wilson NL , Looman WJ , McCarthy C , Morgan R , Ablorh-Odjidja C , Kunik ME ((2012) ) Negative caregiving effects among caregivers of veterans with dementia. Am J Geriatr Psychiatry 20: , 239–247. |
[16] | Gaugler JE , Anderson KA , Leach CR , Smith CD , Schmitt FA , Mendiondo M ((2004) ) The emotional ramifications of unmet need in dementia caregiving. Am J Alzheimers Dis Other Demen 19: , 369–380. |
[17] | Vaingankar JA , Subramaniam M , Picco L , Eng GK , Shafie S , Sambasivam R , Zhang YJ , Sagayadevan V , Chong SA ((2013) ) Perceived unmet needs of informal caregivers of people with dementia in Singapore. Int Psychogeriatr 25: , 1605–1619. |
[18] | Wancata J , Krautgartner M , Berner J , Alexandrowicz R , Unger A , Kaiser G , Marquart B , Weiss M ((2005) ) The Carers’ Needs Assessment for Dementia (CNA-D): Development, validity and reliability. Int Psychogeriatr 17: , 393–406. |
[19] | Thyrian JR , Fiss T , Dreier A , Bowing G , Angelow A , Lueke S , Teipel SJ , Flessa S , Grabe HJ , Freyberger HJ , Hoffmann W ((2012) ) Life- and person-centred help in Mecklenburg-Western Pomerania, Germany (DelpHi): Study protocol for a randomised controlled trial. Trials 13: , 56. |
[20] | Calabrese P , Kessler J ((2000) ) Screening for cognitive impairment in dementia - the DemTect procedure. Eur Neuropsychopharmacol 10: , 369. |
[21] | Thyrian JR , Hoffmann W ((2012) ) Dementia care and general physicians-a survey on prevalence, means, attitudes and recommendations. Cent Eur J Public Health 20: , 270–275. |
[22] | Eichler T , Thyrian JR , Hertel J , Köhler L , Wucherer D , Dreier A , Michalowsky B , Teipel SJ , Hoffmann W ((2014) ) Rates of formal diagnosis in people screened positive for dementia in primary care: Results of the DelpHi-Trial. J Alzheimers Dis 42: , 451–458. |
[23] | Eichler T , Thyrian J , Hertel J , Michalowsky B , Wucherer D , Dreier A , Kilimann I , Teipel S , Hoffmann W ((2015) ) Rates of formal diagnosis of dementia in pimary care: The effect of screening. Alzheimers Dement 1: , 87–93. |
[24] | Eichler T , Thyrian JR , Hertel J , Richter S , Michalowsky B , Wucherer D , Dreier A , Kilimann I , Teipel S , Hoffmann W ((2018) ) Patient variables associated with the assignment of a formal dementia diagnosis to positively screened primary care patients. Curr Alzheimer Res 15: , 44–50. |
[25] | Thyrian J , Hertel J , Wucherer D , Eichler T , Michalowsky B , Dreier-Wolfgramm A , Zwingmann I , Kilimann I , Teipel S , Hoffmann W ((2017) ) Effectiveness and safety of dementia care management in primary care: A randomized clinical trial. JAMA Psychiatry 74: , 996–1004. |
[26] | Dreier A , Thyrian J , Eichler T , Hoffmann W ((2015) ) Dementia Care Management curriculum: An evaluation of the pilot qualification for nurses to care for patients with dementia and support their care givers in primary care. Nurse Educ Today 36: , 310–317. |
[27] | Eichler T , Thyrian JR , Fredrich D , Köhler L , Wucherer D , Michalowsky B , Dreier A , Hoffmann W ((2014) ) The benefits of implementing a computerized intervention-management-system (IMS) on delivering integrated dementia care in the primary care setting. Int Psychogeriatr 26: , 1377–1385. |
[28] | Monahan PO , Boustani MA , Alder C , Galvin JE , Perkins AJ , Healey P , Chehresa A , Shepard P , Bubp C , Frame A , Callahan C ((2012) ) Practical clinical tool to monitor dementia symptoms: The HABC-Monitor. Clin Interv Aging 7: , 143–157. |
[29] | Eichler T , Thyrian JR , Dreier A , Wucherer D , Kohler L , Fiss T , Bowing G , Michalowsky B , Hoffmann W ((2014) ) Dementia care management: Going new ways in ambulant dementia care within a GP-based randomized controlled intervention trial. Int Psychogeriatr 26: , 247–256. |
[30] | Zank S , Schacke C , Leipold B ((2006) ) Berliner Inventar zur Angehörigenbelastung - Demenz (BIZA-D). Z Klin Psychol Psychother 35: , 296–305. |
[31] | Ware J , Kosinski M , Keller SD ((1996) ) A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med Care 34: , 220–233. |
[32] | Derogatis LR , Melisaratos N ((1983) ) The Brief Symptom Inventory: An introductory report. Psychol Med 13: , 595–605. |
[33] | Zwingmann I , Hoffmann W , Michalowsky B , Dreier-Wolfgramm D , Hertel J , Wucherer D , Eichler T , Kilimann I , Thiel F , Teipel S , Thyrian R ((2017) ) Supporting family dementia caregivers: Testing the efficacy of dementia care management on multifaceted caregivers’ burden. Aging Mental Health 22: , 889–896. |
[34] | Kessler J , Markowitsch HJ , Denzler P ((1990) ) Mini Mental Status Test (German Version), Beltz Test GmbH, Göttingen. |
[35] | Hindmarch I , Lehfeld H , de Jongh P , Erzigkeit H ((1998) ) The Bayer Activities of Daily Living Scale (B-ADL). Dement Geriatr Cogn Disord 9: , 20–26. |
[36] | Gauggel S , Birkner B ((1999) ) Validity and reliability of a German version of the Geriatric Depression Scale (GDS). Z Klin Psychol 28: , 18–27. |
[37] | Wilz G , Pfeiffer K ((2017) ) Psychotherapie mit älteren pflegenden Angehörigen. Nervenarzt 88: , 1246–1251. |
[38] | Ornstein K , Gaugler JE ((2012) ) The problem with “problem behors”: A systematic review of the association between individual patient behavioral and psychological symptoms and caregiver depression and burden within the dementia patient-caregiver dyad. Int Psychogeriatr 24: , 1536–1552. |
[39] | Hughes TB , Black BS , Albert M , Gitlin LN , Johnson DM , Lyketsos CG , Samus QM ((2014) ) Correlates of objective and subjective measures of caregiver burden among dementia caregivers: Influence of unmet patient and caregiver dementia-related care needs. Int Psychogeriatr 26: , 1875–1883. |




