The Use of Music Playlists for People with Dementia: A Critical Synthesis
Abstract
The use of pre-recorded music to ease behavioral and psychological symptoms associated with dementia is popular in health-care contexts in both formal music therapy settings and in non-therapist led interventions. However, further understanding of how non-therapist led interventions compare to therapist led interventions is needed. This paper reviews 28 studies that used pre-recorded music with people with dementia using a critical interpretive synthesis model. Results revealed that pre-recorded music can be effective in reducing a variety of affective and behavioral symptoms, in particular agitation, even where a trained music therapist is not present. However, the results are not universally positive, suggesting the need for further clarification of protocols for music use and closer investigation of variables that influence individual responseto music.
INTRODUCTION
Since dementia is incurable, quality of life is a key treatment goal for people with dementia. However, people with dementia typically report decreased quality of life due to social isolation, issues of self-hood and self-esteem, changing family relationships, and a declining ability to perform activities of daily living [1]. These changes often result in depression and anxiety in people with dementia and their caregivers. Non-pharmacological approaches to dealing with the psychological and behavioral changes associated with dementia are desirable because of the high rate of adverse effects of pharmacological treatments in people with dementia [2].
One of the most common non-pharmacological approaches to treating the behavioral and psychological symptoms of dementia is the use of music [3]. A mounting body of evidence suggests that music therapy can be useful in addressing neuropsychiatric and behavioral symptoms in people with dementia [4]. Music therapy can include both active forms of musical engagement such as songwriting, singing, and playing musical instruments, as well as receptive forms of musical engagement such as listening to live or pre-recorded music. In such interventions, a trained and registered music therapist tailors the program of musical engagement to the needs of the patients involved based on established therapeutic practice. The patient-therapist relationship is also a crucial part of music therapy practice [5]. ‘Music therapy’ in the sense used in this paper, is thus distinct from more incidental exposures to music in health-care settings and from planned interventions using music that are not administered in a therapist-supportedenvironment.
However, interest in the use of pre-recorded music in non-therapist-led interventions and music programs is increasing, in part due to anecdotal evidence of music’s effectiveness such as in the documentary Alive Inside [6]. Programs utilizing pre-recorded music typically involve the creation of musical playlists by researchers, health-care workers, or caregivers, which are played to individuals or groups of patients in a health-care context. Some of the aforementioned playlist interventions are based on trademarked programs such as “Music and Memory”, while others may be less formally derived. Some advantages of using pre-recorded music outside of formal music therapy settings are the relative ease of access and affordability of pre-recorded music, and that it can be used as frequently as needed, when needed.
Nevertheless, there has been relatively little empirical study of the effectiveness of non-therapist led playlist interventions in comparison to music therapy. Studies in other populations suggest that the effects of music on mood are not universally beneficial especially where mental health issues may be a concern. Garrido and Schubert [7, 8], for example, have demonstrated that adolescents and young adults with depression can respond differently to some music compared to participants without depression, being more susceptible to the triggering of dysphoric moods. In a music therapy setting, the therapist can facilitate this exploration of emotions in a safe and supported environment, providing some containment for the emotions experienced in response to music [9]. However, there is a need to understand more clearly the effects of using music as a therapy in vulnerable populations where a trained therapist is not present.
Despite this important distinction between music therapy and other interventions involving music, previous reviews of musical interventions in people with dementia often fail to distinguish between therapist-led interventions and those that do not involve a therapist. Konno and colleagues [10], for example, review nine instances of musical intervention without providing any information about whether they were therapist-led or not. In fact, there is often some confusion over the distinction in the literature, with the term ‘music therapy’ being sometimes used to encompass all kinds of musical engagement in health contexts. Other reviews provide helpful distinctions between music therapy and other kinds of music interventions in their introductions, but group the results of both kinds of interventions together in their analysis [11, 12].
A further aspect of interest in exploring the value of playlist interventions is the question of whether listening to music holds the same value as more active forms of engaging with music such as singing orplaying musical instruments. Logic would suggest that active engagement can provide additional physical and psychological benefits to patients over merely listening to it. However, in practice, music listening is rarely passive, with listeners typically becoming physically engaged by moving their bodies or singing along in a spontaneous way. Nevertheless, the value of pre-recorded music is less clear and requires closer examination [13]. Furthermore, other variables have the potential to influence the impact of music interventions, such as the type of music selected, and the time of day and setting in which it was played.
Questions also exist over whether people with different types of dementia respond to music in the same way. Behavioral and psychiatric symptoms tend to differ between different forms of dementia, with people with dementia with Lewy bodies for example, tending to experience greater agitation and anxiety than those with Alzheimer’s disease or vascular dementia, while those with Alzheimer’s disease might have greater impairments of short-term memory than people with other forms of dementia [14]. We could thus expect that people with different forms of dementia would not only have different therapeutic needs, but also may respond to music differently. This has not been explored in previous reviews however.
The aim of the current review, therefore, is to examine evidence of the effectiveness of using pre-recorded music to reduce the behavioral and psychological symptoms of dementia, as well as to explore the influence of other variables such as the type of dementia of the patients involved and the details of the music intervention itself. This will help to clarify the usefulness of playlist interventions for people with dementia, and to identify further areas requiring future investigation.
Research question
1. How useful are music interventions using pre-recorded music in addressing psychological and behavioral symptoms in people with dementia?
2. Do other variables such as the type of dementia involved, the presence of a therapist, the type of music played or the setting in which it was played have an influence on the impact of playlist interventions?
METHODS
The methodological framework used for this review was that of a Critical Interpretive Synthesis (CIS) as outlined by Dixon-Woods and colleagues [15]. The aim of this method is to integrate studies from diverse fields that use a range of researchmethods into a single overarching narrative. The research reviewed can include studies reporting both qualitative and quantitative data, and these are typically analyzed in a way that considers both the data and the disciplinary perspectives of the authors ofthe various studies [16].
Literature search
The original search was a systematic scan of the following databases: JSTOR, PsychInfo, PubMed, and ProQuest, using the search terms “music AND dementia” in the title and abstract. An initial 765 articles were collated from this search.
Selection of studies for inclusion
Purposive sampling [17] was used to select the articles from health and psychology disciplines. All identified references were screened according to the following inclusion criteria: 1) participants had to have some form of dementia or be caring for someone with dementia, 2) the intervention studied must involve the use of pre-recorded music alone or in combination with other musical activities, and 3) the research had to be published between 2006–2016.
Articles not meeting the above inclusion criteria were excluded. Studies relating solely to people with mild cognitive impairment were also excluded, as were opinion or general discussion papers or review papers and studies involving only active forms of musical engagement such as singing, playing musical instruments, or songwriting. While the focus of the current review was not music therapy, where music listening was used in a formal music therapy setting, these were also included because of the potential for such studies to further illuminate the value of music listening for people with dementia.
All types of evaluative studies were eligible for inclusion. While articles were appraised for scientific quality according to conventional standards such as the Joanna Briggs Institute’s critical appraisal tools (2016), methodological quality did not form a basis for exclusion since a critique of the reliability of studies in the field was viewed as a central part of the function of the critical analysis and formulation of a synthesizing argument. Abstracts were screened according to these criteria in an initial screening process, leaving a total of 37 articles for review.
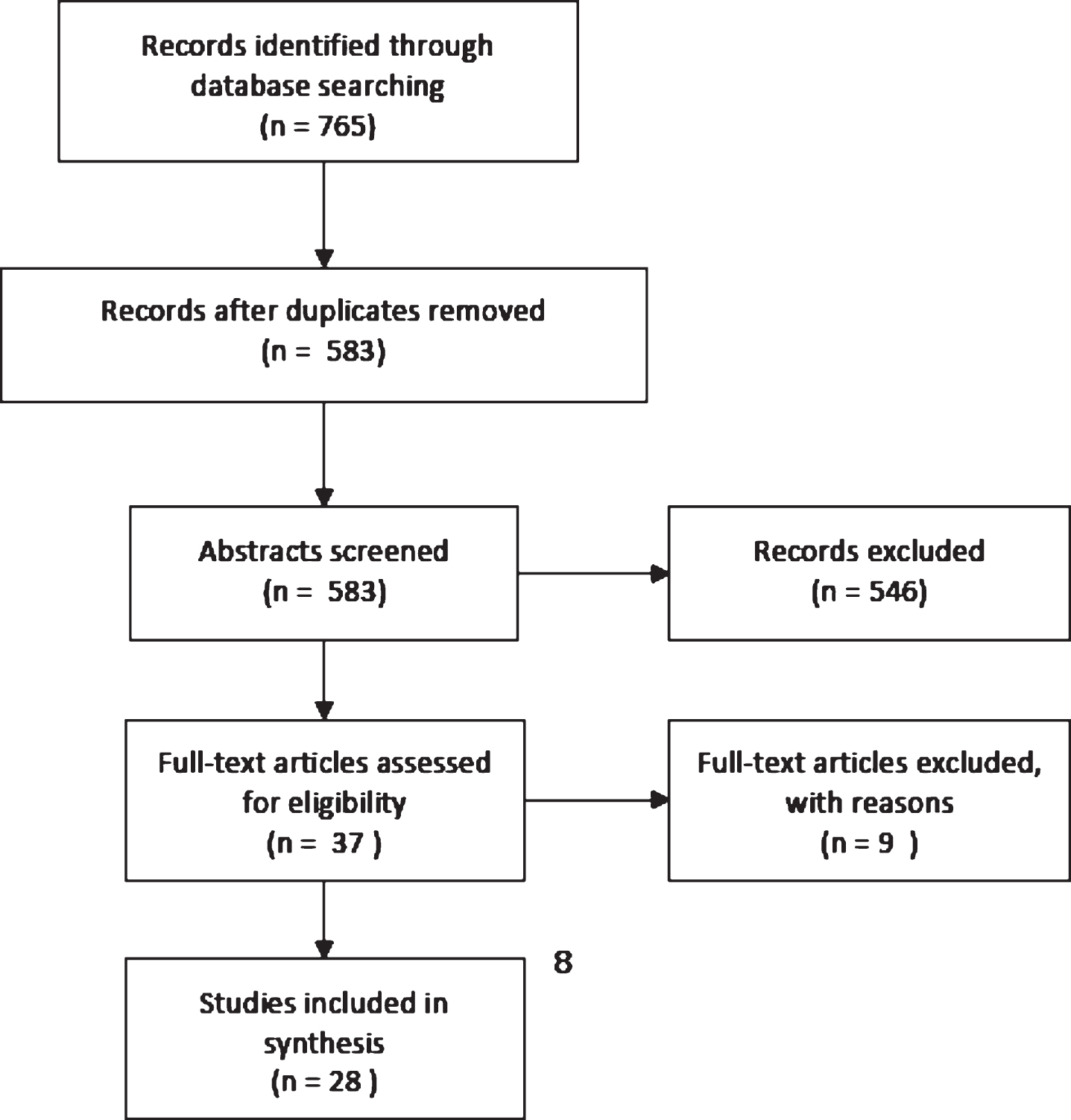
Titles and abstracts to be considered were then uploaded to Covidence, an online platform for conducting systematic reviews (http://www.covidence.org). Since abstracts did not always provide enough information to assess the studies according to the inclusion criteria, full texts of articles were then subjected to a closer appraisal for relevance by two reviewers, after which a further 9 were excluded, leaving 28 studies for inclusion in the review (Fig. 1).
Fig.1
PRISMA flowchart of article selection.
Data extraction
Evidence summary templates were created in Covidence and used for data collection regarding the characteristics of studies, participants, interventions and final outcomes. The data extracted also included details about:
• The type of dementia that participants had been diagnosed with
• Details about the type of music used in the intervention and selection procedures
• Whether the music was heard individually or in group settings
• Whether the music was played over speakers or on headphones
• Times when the music was played
• The involvement of a music therapist or non-therapist facilitator
• The duration of the music sessions
• Time points at which outcome measures were administered.
Evaluation of studies
It was expected that the studies identified would be quite heterogeneous, and that a lack of comparable methodologies and outcome measures would mean the reviewed studies would not be amenable to a meta-analysis. Thus, a narrative synthesis model was used in exploring the data [15, 18]. This approach uses words and text to explore relationships in the data and to develop a theory based on a synthesis of the findings in the reviewed studies [19]. The studies were critically appraised by two authors independently of each other on the basis of methodology, sample size, the appropriateness of the musical intervention tested, and the appropriateness of the conclusions drawn to the results reported and other criteria drawn from the Health Care Practice Research and Development Unit (HCPRDU) evaluation tool for quantitative studies [20]. This tool was developed to assist in the critical appraisal of research studies, and is particularly useful for reviews that include both qualitative and quantitative studies. The two authors who conducted this appraisal subsequently discussed their relative assessments and reached agreement about the relative weight of the studies discussed. Studies were then grouped and sub-grouped as described below for comparative purposes, according to study design, intervention type, the outcomes reported and other study features. The lead author prepared a narrative analysis based on these findings and discussions, giving greater emphasis to the more robust studies considered, which was then checked independently by all other authors.
RESULTS
General characteristics of the reviewed studies
The 28 studies considered in this review were published in journals representing 8 different disciplines and fields of specialty (see Fig. 2), but were primarily found in health-related journals. A summary of the characteristics contained in this study can be found in Table 1. The studies originated from 13 different countries, representing Europe, Asia, North America, and Australasia. A large proportion of studies did not report the specific type of dementia that their participants had been diagnosed with (n = 13, 46%). A number reported focusing on participants with Alzheimer’s disease (n = 7, 25%), while the balance of studies reported that their participants were made up of those with Alzheimer’s disease and ‘other’ forms of dementia (n = 8, 29%). None of the studies distinguished between people with different forms of dementia within their results. Sample sources included residential aged care facilities (nursing homes) (n = 18, 64%), home care situations (n = 4, 14%), day activity centers for people with dementia (n = 2, 7%), hospitals (n = 2, 7%), and an assisted living facility (n = 1, 4%). One study did not report the source of theparticipants.
Fig.2
Fields of origin of reviewed studies.
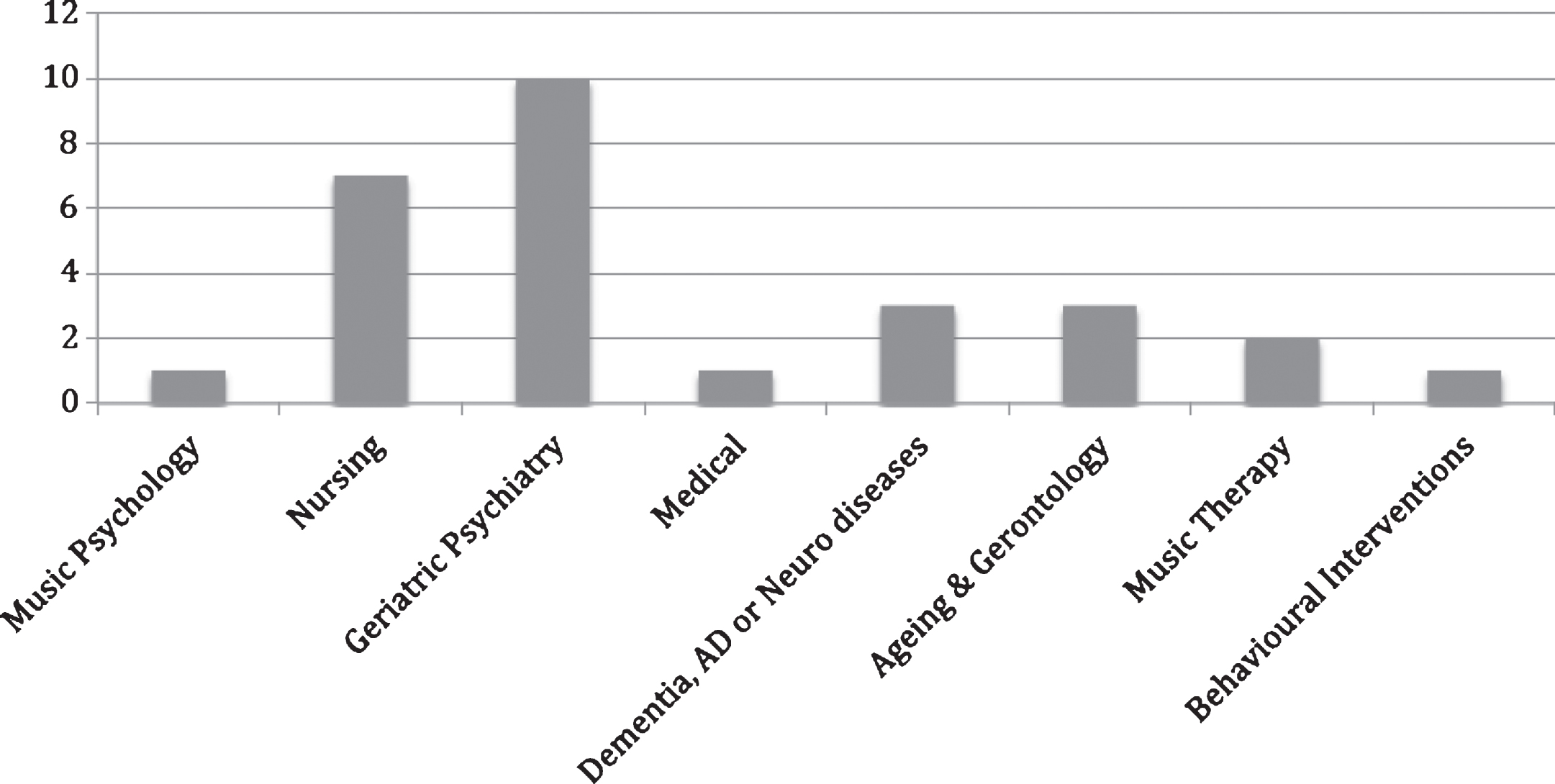
Table 1
Studies and key features
| Ref | Study design | Sample size | Type of dementia | Measurement time-points | Intervention characteristics | Intervention duration and frequency |
| 5 | RCT, parallel groups | MT = 31 ML = 32 C = 35 | Not reported | Baseline, post and 2 month follow up | Researcher selected music based on participant preferences. Played individually and in group music therapy sessions. | 30-min session; twice weekly for 10 weeks |
| 24 | Single case, crossover design | n = 1 | Early-onset AD | During listening | Researcher-selected individual playlists based on popular music from the 50s and 60s; speakers and headphones | 5 in sessions; 8–10 times per condition |
| 25 | Cross-over design | n = 15 | AD | 30 min before, during, and 30-min post | Researcher-selected individual playlists based on participant preferences. | 30-min sessions; twice weekly for 8 weeks (2 weeks on, 2 weeks off) |
| 26 | RCT, parallel groups | MT = 27 ML = 29 C = 27 | Not reported | Baseline, post and 6-month follow up | Selection criteria not specified, listening sessions occurred with caregiver. | 1.5-h sessions, once weekly for 10 weeks |
| 28 | Single group, pre-post | n = 41 | Not reported | Daily | Nature music; played to groups at lunch time. | 1-h sessions, daily on alternative weeks for 8 weeks |
| 29 | Pre-post, single group | n = 22 | Not reported | Baseline and daily for up to 2 weeks post. | Researcher composed music played to groups at mealtimes through speakers. | 1-h sessions; twice daily for 4 weeks |
| 30 | RCT, parallel groups | MT = 13 ML = 13 C = 12 | AD | 5 min pre, 5 min post, and 2 week follow up | Researcher-selected individual playlists based on period best recalled by participant. | 30-min sessions; once weekly for 10 weeks |
| 31 | Controlled trial with no randomization, parallel groups | n = 20 C = 21 | AD | Baseline and post | Mozart in the morning and Pachelbel’s Canon before sleep; headphones | 30-min sessions; daily for 6 months |
| 32 | Controlled trial, crossover design | n = 75 | Not reported | Daily over 12 weeks with 2-week washout at end. | Baroque music, played to a group in the evenings through speakers. | 4-h sessions; daily for 24 weeks per condition; 2-week washout |
| 33 | Cross-over with standard order | n = 5 | Not reported | During music listening | Dean Martin or religious music; played to individuals when agitated | Length of sessions not reported, 2 weeks per condition, 16–18 each condition |
| 34 | Cross-over with standard order | n = 6 C = 9 | AD + other | 1 week before and 1 week after | Pre-defined list of music. Played to individuals through speakers. | 90-min session; once per week, with 4-week washout |
| 35 | RCT, cross-over design with order randomization | n = 32 | Not reported | Continuous throughout sessions | Age-appropriate; Played to groups through speakers. | 30-min sessions; 1 session per condition |
| 36 | RCT, parallel groups | n = 18 C = 19 | AD + mixed | Baseline, during, post, 2-week follow up and 4-week follow up | Age-appropriate music; speakers; Mixed active and receptive | 1-h sessions; twice weekly for 4 weeks |
| 37 | 1 group time-series design | n = 55 | AD, vascular + Lewy-body | 12 months before, 3 months before and during. | Researcher-selected popular songs from 30s–60s and classic relaxation tunes. Played to groups at meal times. | 2-h session; twice daily for 3 months |
| 38 | Cross over design experiment | n = 9 | AD + other | During music listening | Researcher selected playlists based on family recommendation and popular songs from the 20s–60s. Listened through speakers with caregiver during morning routine. | 6–22-min sessions; 1 session per condition |
| 39 | RCT, parallel groups | n = 13 C = 11 | AD | Baseline, 4 weeks, 8 weeks, post, and 8 week follow up. | Researcher-selected individual playlists based on participant preference. Played through headphones. | 20-min session; once per week for 6 weeks |
| 40 | Cross-over design | n = 28 | AD | During listening | Researcher- selected music based on music therapist recommendation; played to group through speakers | 17 min sessions; once weekly for 6 weeks |
| 41 | Cluster randomization; parallel design | n = 32 c = 25 | Not reported | Baseline and post | Selected by nurses based on participant preference. Played to individuals’ mid-afternoon | 30-min sessions; twice weekly for 6 weeks |
| 42 | Cross-over with randomization | n = 30 | Not reported | 2-min intervals before, during and post | Researcher selected individual playlists based on family recommendation using headphones. | Unreported length of session; 3 times per week with 3 baseline and 3 music sessions |
| 43 | RCT, crossover within treatment group, parallel control group | n = 41 | Not reported | 10 min before, during and 60 min post. | Researcher-selected individual playlists based on caregiver information. Played at times of agitation through speakers. | 10-min session; 1 session per condition |
| 44 | Cluster randomization; parallel design | n = 29 C = 23 | Not reported | Baseline and post | Selected by nurses based on participant preference. Played to individuals’ mid-afternoon; speakers | 1-h session; twice daily for 4 weeks |
| 45 | Cross-over design | n = 15 | Not reported | 30 min before, during, and 30 min post | Researcher-selected individual playlists based on participant preference. Played at times of peak agitation. | 30-min sessions; daily for 6 months |
| 46 | RCT, parallel groups | MT = 30 ML = 29 C = 30 | AD + mixed | Baseline, post, 1 month follow up, 3 month follow up, and 6 month follow up | Researcher-selected based on participant preferences. Listening with caregiver during daily routine. | 1.5-h sessions; once weekly for 10 weeks |
| 47 | Single group, pre-post. | n = 8 dyads | Not reported | Baseline and post | Researcher-selected based on caregiver information. Participants would listen with caregiver. Mixture of receptive and active. | 5-min sessions; 8–10 times per condition |
| 48 | Controlled trial, cross-over design | n = 17 | AD, vascular + mixed | Baseline, post and follow up (unknown length of time) | Researcher selected music based on participant preferences; played individually &in group music therapy sessions | 30-min session; twice weekly for 30 sessions with washout period between conditions |
| 49 | Controlled experiment parallel groups; no randomization | n = 26 C = 23 | AD + unknown | Baseline and post | Biographically relevant music; played to groups at fixed times at both a.m. and p.m. | 30-min session; once weekly for 10 weeks |
| 50 | Single group | n = 9 | AD + vascular | Continuously | Researched-selected individual playlists based on biographical details. | 1.5-h session; once weekly for 10 weeks |
| 51 | RCT parallel groups | n = 5 C = 6 | AD | Baseline, 4 weeks, 2 week follow up and 4 week follow up. | Sessions facilitated by psychologist, predefined music list, mixed active &receptive | 2-h session; 2 per week for 4 weeks |
RCT, randomized controlled trial; MT, music therapy; ML, music listening; C, control; AD, Alzheimer’s disease.
A diverse range of study designs were used in the reviewed studies including randomized controlled trials (RCTs) with parallel treatment groups (n = 7, 25%), an RCT with a cross-over design within the treatment group and a parallel control group (n = 1, 4%), controlled experiments with cluster randomization (n = 2, 7%), controlled experiments with parallel treatment groups but no randomization (n = 2, 7%), crossover designs with randomization of the order of conditions (n = 2, 7%), crossover designs with a standard order for conditions (n = 8, 29%), single group experiments with a pre-post design (n = 3, 11%), single group experiments with continuous observation (n = 2, 7%), and a single case crossover design (n = 1, 4%). Thus only 10 studies in total (36%) had both a control group or condition, and some kind of randomization included in the design (Table 2). Of the seven studies that used RCTs with parallel treatment groups, two compared similar interventions or used comparable outcome measures. Since the aim of our review was both to look at the effect of various interventions on particular psychological and behavioral symptoms, as well as to look at the relative influence of other variables, multiple studies that compared similar interventions under similar conditions would have been required to conduct a meta-analysis. Thus, it was decided that insufficient comparable studies were available for the purposes of a meta-analysis in this instance.
Table 2
Evaluation of studies included in the review
| Distinguished results based on dementia type | Distinguished results based on receptive or active | Adequate reporting of intervention procedures | Adequate reporting of music selection protocol | Control group or condition | Randomization (assignment to conditions or order of conditions) | Control group activities similar to music condition | Drop out rate less than 20% | Effect size reported or calculable | |||||||||||||
| Yes | No | Yes | No | N/A | Yes | No | Yes | No | Yes | No | Yes | No | N/A | Yes | No | N/A | Yes | No | Not reported | Yes | No |
| 0 | 28 | 7 | 5 | 16 | 13 | 15 | 19 | 9 | 23 | 5 | 10 | 13 | 5 | 21 | 2 | 5 | 16 | 7 | 5 | 6 | 22 |
Where control groups or conditions existed, comparisons were between music listening and other audio conditions such as reading (e.g., [21]), between active musical engagement or music therapy, and music listening (e.g., [22]), or between music and standard care [23]. A small number of studies (n = 2, 7%) did not appear to have control conditions that were well matched to the music listening group, with the control engaging in more passive or more solitary activities than the treatment group, making it difficult to attribute where effects of the interventionlay.
Overall sample sizes tended to be relatively small in many studies, although they ranged from 1–120 with a mean of 36.6. Where control groups were used, group sizes ranged from 5–40 participants with a mean of 22.6. A total of 13 studies (46%) had sample or group sizes of less than 20, and only 3 studies (11%) reported group sizes of 40 or more. An attempt was made to look at effect sizes of results in order to determine how sample sizes influenced the results. However, only 6 studies reported effect sizes or sufficient information to allow effect sizes to be calculated for within-subjects analyses (21%) (Table 2). Nevertheless, a number of studies that reported non-significant results did have relatively small sample sizes, suggesting that more definitive findings could have been obtained with large samples. Attrition rates also tended to be high with over half the studies reporting drop-out rates of more than20% (57%).
The music interventions
The majority of studies included in the review related to musical interventions that were not led by a music therapist (n = 17, 61%). Six studies (21%) included sessions led by a music therapist, while 5 considered interventions involving music sessions facilitated by a caregiver after training by a music therapist. The length of single sessions of musical engagement across all studies ranged from 5 min to 4 h, m = 53.8 min. Several studies involved single listening sessions only (n = 3, 11%), while the majority involved daily (n = 4, 14%), twice daily (n = 1, 4%), weekly (n = 7, 25%), or semi-weekly (n = 11, 39%) sessions, over a period ranging from 3 weeks to 6 months. However, as demonstrated in Table 1, several studies (n = 15, 54%) did not adequately report the details of the intervention procedures in order for these details to be ascertained in eachcase.
Most studies involved individual music sessions (n = 15, 54%), 4 of which used headphones, while 6 played music over loudspeakers (5 did not report whether speakers or headphones were used). One study directly compared the use of headphones and speakers [24], with both conditions being found to have similar effects. However, this was a single case study. No other study attempted to assess the relative effects of using headphones versus use ofloudspeakers. Nine studies were group sessions in which only loudspeakers were used, and 4 studies involved caregiver and participant listening together.
A majority of studies selected ‘favorite music’ or music based on information from family members and caregivers (n = 14, 50%) (e.g., [25]). Of these studies, 9 did not use any specific protocol or give specific details about how these preferences or recommendations were sought, stating only, for example, that they used music that was biographically relevant (e.g., [26]). However, 5 studies used the Assessment of Personal Music Preference (APMP) established by Gerdner [27].
The remaining studies used music selected by the researcher (n = 11, 39%). Of these, one study used nature music (which included piano and sounds from nature such as birds, running water, and whale song) [28], one used music composed by the researcher [29], one used music from the era most often recalled by participants [22], two used classical or baroque music [30, 31], one compared Dean Martin and religious music [32], and five used music that was considered ‘age appropriate’ [33–37].
It was unclear in at least three of the studies that used researcher-selected music whether there was an attempt to select music designed to target specific symptoms. However, 6 attempted to match the music to the symptoms of interest, such as using calming music to reduce agitation (see for e.g., [29, 35]). Studies that used ‘favorite music’ did not attempt to match the music to any particular desired mood state, with the exception of Sakamoto and colleagues [22] who confined music selections to joyful music. Two studies used a combined approach, attempting to select music on the basis of both individual preferences and the specific mood effects desired[38, 39].
Relative effectiveness of different interventions
As demonstrated in Table 3, a number of studies (n = 11, 39%) reported positive outcomes from individual receptive music interventions that used either an established protocol for music selections or that was based on family recommendations, although one study did report positive results from classical music [30]. In non-therapist led sessions, several studies reported reduced agitation after the use of individualized playlists (n = 5, 18%) [40, 41]. Hicks-Moore and Robinson [42] for example found that listening to favorite music was effective in reducing agitation both alone and when combined with hand massage. Other studies reported reductions in anxiety [43], depression [5], and pain [44], and increases in quality of life [5] and performance on several cognitive domains [45]. Increases in caregiver satisfaction, relaxation, comfort, and happiness were also reported [46]. Where directly compared, there was little evidence that music therapy served advantages over non-therapist led listening [5, 47].
Table 3
Comparison of individual and group therapy, therapist versus non-therapist, and receptive versus active interventions
| Individual versus group | Therapist versus non-therapist | Receptive versus Active | Music Used | Positive outcomes | Negative outcomes | Non-significant outcomes |
| Individual Interventions | Therapist led | Receptive | Joyful music from era most recalled | Affective disturbance; anxiety & phobias; emotional state [30] | ||
| Gerdner protocol | Agitation and depression [39] | |||||
| Active | Joyful music from era most recalled | Affective disturbance, anxiety &phobias, paranoid &delusional ideation; aggressiveness; activity disturbance; emotional state [30] | ||||
| Family recommendation; no specific protocol | Behavior; quality of life; depression [5]; Quality of life [48] | |||||
| Mixed | Family recommendation; no specific protocol | Communication, well-being; positive affect [50] | ||||
| Non-therapist led | Receptive | Age appropriate | Agitation [34] | |||
| Gerdner protocol | Agitation [25, 43]; Anxiety [44] | Aggressive behaviors [44] | ||||
| Family recommendation; no specific protocol | Agitation [40–42]; Behavior [5, 40]; Quality of life, depression [5] | Agitation [41] | Disruptive vocalizations [24]; Quality of life [48] | |||
| Caregiver trained by music therapist | Receptive | Classical | Abstraction [31] | |||
| Gerdner protocol | Pain [45] | |||||
| Family recommendation; no specific protocol | Mood, episodic memory, quality of life, attention, executive functioning and general cognition [46]; Behavior [26] | Behavior, communication [38] | ||||
| Dean Martin &religious | Agitation [33] | |||||
| Active | Family recommendation; no specific protocol | Mood, episodic memory, attention, executive functioning and general cognition, short-term and working memory [46] | ||||
| Mixed | Predefined list selected from by caregiver | Caregiver satisfaction, relaxation, comfort, happiness [47] | ||||
| Group Interventions | Therapist Led | Mixed | Family recommended; no specific protocol | Agitation, depression, global functioning [49] | ||
| Age appropriate | Emotional state, behavior, caregiver distress [36] | |||||
| Predefined list added to by participants | Emotional state [51] | |||||
| Non-Therapist Led | Active | Age appropriate | Engagement [35] | |||
| Receptive | Nature music | Behavior [28] | ||||
| Baroque | Behavior [32] | |||||
| Age appropriate | Engagement [35] | |||||
| Researcher composed | Agitation [29] | |||||
| Caregiver trained by music therapist | Receptive | Age appropriate | Falls [37] |
However, results were not universally positive. Garland and colleagues [41], for example, found that while overall results of listening to favorite music in their study were positive, there was a widely divergent response from participants reporting that “a dramatic improvement in agitation for some was offset by neutral or negative outcomes for others” (p. 520).
Support for the value of group music listening interventions was less robust, with only two studies providing clear positive results for group receptive programs [29, 34]. One study found positive effects on emotional state for a music therapy group that mixed active and receptive, but no significant differences with the control group which participated in cooking activities [35].
Despite some positive results, some negative outcomes were also reported in relation to group receptive interventions. Nair and colleagues [31], for example, reported that after exposure to Baroque music, behavioral disturbances in residents of an aged care facility actually increased overall during weeks in which the music was played. The authors concluded that this was because the music used was not appealing to participants and that the use of individualized music selections would be more effective. Interestingly, Chang and colleagues [28] similarly found that behavioral symptoms were worse in weeks during which nature music was played to residents of an aged care facility. They argued that this may have been due to the fact that there was a time lag in the effect. However, most studies indicated that response to music tended to be immediate. Thus, the two papers taken together seem to suggest the relative ineffectiveness of researcher-selected music played in group settings in improving behavioral disturbances inpeople with dementia.
Seven studies directly compared active and receptive interventions, and tended to demonstrate that both types of musical engagement yielded some positive results. Positive results for both active and receptive were reported in 6 of the seven studies, although active engagement such as singing was reported as having stronger effects in 3 studies. Sakamoto and colleagues [22], for example, compared active musical engagement with a receptive intervention and a control group, each of which were administered by a group of trained facilitators including but not limited to music therapists. They found that while both active and receptive interventions caused increased parasympathetic nervous system activation, active engagement resulted in better overall improvements to mood. Holmes and colleagues [34] found that while participants demonstrated engagement with both the active and receptive music programs, engagement was greater for the active intervention.
Raglio and colleagues [47] also compared music listening with active music therapy, but found no significant differences between conditions, although trends in the data suggested that active music therapy had a greater effect on behavioral and psychological symptoms. However, while the brief report of this study states that no caregiver was present during the music listening, it did not clearly identify whether the music therapist also led the music selection for the listening condition. Therefore, while this study offers some support for the greater impact of active musical engagement on symptoms of dementia, it remains inconclusive about the necessity for a trained music therapist to be involved in facilitating music listening programs. In addition, the fact that the conditions compared active engagement with a therapist present, with receptive listening without anyone present makes it difficult to determine the degree to which the outcomes were influenced by the nature of the musical engagement involved, or by the personal contact with a therapist.
In a follow-up study [5], the same authors then compared music listening with active music therapy and a control group receiving standard care. It was found that all groups showed improvements in behavioral symptoms, depression, and quality of life, with no significant differences between groups. The authors attributed these results to the types of outcome measures used. However, this study also was not able to demonstrate that active music therapy serves any advantages over music listening.
Several studies did not clearly distinguish between active and receptive musical engagement in the results (e.g., [48, 49]). For example, Clement and colleagues [50] found that short-term benefits on emotional state were experienced by both the music and the cooking groups, while long-term benefit was experienced by the music group only. However, both the cooking and the music interventions involved active and receptive aspects, making it difficult to disentangle the relative effects.
A number of studies gave the reader only a vague idea of the level of involvement of a music therapist. For example in the study by Guetin and colleagues [38], a music therapist utilized software that produced individualized playlists designed to shape moods according to an inverted U-curve—with music initially intended to calm the listener and then to gradually increase arousal. The control group took part in a rest and reading session “under the same conditions and at the same intervals” (p. 38), but the study does not provide further details as to the reading condition, i.e., whether or not this was a live reading, a recorded reading, how the reading material was selected, or whether it too was designed to follow a particular mood curve. In addition, the authors noted that in their study the music sessions involved the development of a patient-therapist relationship, but did not describe whether the reading group was similarly facilitated by a therapist. The study reported significant improvements in anxiety and depression in the music group in comparison to the control group. However, while this was generally a robust study, the scarcity of detail in relation to the control group makes it difficult for the reader to judge whether or not the differing effects observed can be attributed to the music itself or to other situational variables.
An interesting sub-group of 5 studies concerned interventions where caregivers were trained by a music therapist to use music during their caregiving routine. For example, Särkämö and colleagues[26, 45] trained caregivers to use both singing and music listening, finding that both were able to improve mood, remote episodic memory and also had an effect on cognitive domains. The music listening group improved more than the control group in behavioral disturbances, although no significant group effects were observed on any scales at a 6-month follow up. However, 2 studies in which caregivers were trained to implement a music intervention were unable to report significant results, possibly due to methodological limitations.
DISCUSSION
The aim of this review was to determine whether there is evidence to support the use of pre-recorded music to reduce behavioral and psychological symptoms in people with dementia. We were also interested in the relative effects that other variables, such as whether the intervention was led by a music therapist, the music selection protocol, the type of dementia of participants, and the setting in which the music was played, would have on the reported outcomes.
Overall, the literature reviewed demonstrated that music listening could have significant positive effects on several domains. One of the most consistent findings was in relation to agitation with several studies demonstrating improvements in agitation levels in the music condition compared to control groups [39, 42], whether listening sessions were therapist-led or non-therapist led. Other studies demonstrated reductions in anxiety, behavioral symptoms, and depression relative to a control group [5, 43]. This was particularly so where personalized music selection protocols were utilized.
In fact, while there is an considerable evidence in support of the value of music therapy in literature not covered within the scope of this review [51], the studies concerning receptive interventions considered herein were unable to demonstrate a consistent advantage for music therapy over non-therapist led interventions. Some promising results were also found from studies in which caregivers were trained to use music within their caregiving routines, suggesting that this may be an area worthy of further investigation, particularly since this is likely to be a more accessible compromise between regular music therapy and non-therapist led interventions.
Similarly, studies that compared active music involvement with receptive music listening, while often demonstrating greater shifts in outcome measures from active engagement, still evinced significant improvements on several domains from music listening. Thus, while greater benefits may be obtained from music therapy or active engagement with music such as singing, notable benefits can be still be obtained from the use of pre-recorded music in individualized receptive interventions.
It is noteworthy, however, that even individualized interventions did not have universally positive results. Garland and colleagues [41] reported that decreases in agitation in some participants were offset by increases in agitation in others. It is impossible to know the degree to which this also happened in other studies which did not report it directly. This suggests the need for further research to investigate individual differences in the way people with dementia respond to music and the development of music selection protocols that take into account different response styles. Further investigation of the influence of other variables not considered in the studies reported on here is also warranted. Only one study looked at the relative advantages of headphones over speakers, a variable that is worthy of closer consideration. Furthermore, none of the studies examined in this review considered the possibility that music may have differing effects on people with different forms of dementia. There are over 100 different types of dementia in existence and large numbers of people with dementia do not receive a specific diagnosis [52], making studies that differentiate between types difficult to implement. However, studies comparing the more prevalent forms of dementia would add useful information to current understanding. For example, Alzheimer’s disease typically impacts memory and is generally associated with higher rates of depression than other types of dementia [53]. It could therefore be possible that people with this form of dementia may be more vulnerable to the effects of triggering painful autobiographical memories. On the other hand people with frontotemporal dementia are often more prone to disturbing behavior [53], and may therefore be more likely to respond positively to distractions or calming influences such as music. In fact, little is understood about the mechanisms involved in how music impacts the listener in both healthy populations and those with dementia, suggesting a need for more basic experimental research and theory development to inform the creation of interventions.
While the literature reviewed herein demonstrates that researchers appear to be responding to the evidence that music preferences play an important role in the design of music interventions in people with dementia, few seem to target the music to the symptoms for which relief is sought or to the mood state they are aiming to produce in the listener. Interventions tended to focus either on favorite music without taking into consideration the psychological symptoms of interest, or on particular symptoms such as agitation without considering the individual tastes of the participant. Two studies utilized a combined approach to playlist creation based on both participant preferences and music designed to target specific symptoms, with positive effects [22, 38]. This suggests that a consideration of both aspects shows promise for refinement of music selection protocols.
Although the majority of studies reported positive outcomes for a variety of different types of interventions and music selection protocols, the evidence did not tend to support the use of researcher-selected music in non-therapist led group interventions, with increases in undesirable behavioral symptoms being reported in two studies [28, 31]. These findings tend to confirm the need for caution in using music in group settings in a non-supported environment. Nevertheless, the use of individualized playlists using established protocols was most strongly supported in the literature, providing some evidence that pre-recorded music can effectively be used even without the presence of a therapist.
This review also demonstrated the need for more robust and replicated research about the value of receptive music interventions that do not involve a music therapist. The literature that exists includes a number of studies with important methodological limitations including small sample sizes, lack of a control group, lack of randomization, and lack of blinding for behavioral raters. Few studies reported effect sizes or gave sufficient information for it to be calculated, making it difficult to assess their relative weight. Attrition rates were also a problem with several studies. While the lack of samples of an adequate size and a high attrition rate are likely inherent in the challenges associated with working with the particular population of interest, the review highlights the need for a greater number of carefully designedrandomized controlled trials in order to clearly establish the efficacy of receptive music interventions.
Similarly, there is a need for better matching of experimental conditions in order to eliminate confounding variables such as the presence of a therapist or the nature of the musical engagement involved. Researchers could also benefit from greater transparency and detail in describing study design. Numerous studies gave insufficient detail in reporting their methods for the reader to determine whether the results can indeed be attributed to the musical intervention or whether they could have been influenced by the human contact inherent in the intervention. These difficulties in the reviewed studies could partly have been overcome by greater clarity in the terminology used by researchers. For example, defining music therapy and clearly describing the role of the therapist or non-therapist-facilitator in the intervention could assist readers to ascertain the degree to which human input is related to the outcome. However, the use of the term ‘music therapy’ is commonly found in the literature where no trained music therapist is actually involved. Confusion could possibly be avoided in such a case by a clear distinction being made between ‘music therapy’ and ‘music as therapy’, or “health musicing” as it is described byBonde [54].
As music use is so prevalent in daily life and becoming more popular for use with people with dementia, it is important to gain an enhanced understanding of how music is able to reach even those with advanced levels of cognitive decline, and to develop more detailed protocols for its use that take into account both individual music taste, and the symptoms that the music is being used to address. By examining the mechanisms involved, it may be possible to establish a clearer basis for the creation of such protocols. We encourage researchers to conduct carefully designed studies in which conditions are carefully matched and that seek to overcome many of the limitations found in the literature that are discussed above.
ACKNOWLEDGMENTS
This project was funded by a Fellowship to the first author funded by the National Health and Medical Research Council and the Australian Research Council.
Authors’ disclosures available online (http://j-alz.com/manuscript-disclosures/17-0612r1).
REFERENCES
[1] | Logsdon RG , McCurry SM , Teri L ((2007) ) Evidence-based interventions to improve quality of life for individuals with dementia. Alzheimers Care Today 8: , 309–318. |
[2] | Douglas S , James I , Ballard C ((2004) ) Non-pharmacological interventions in dementia. Adv Psychiatr Treat 10: , 171–179. |
[3] | Mitchell G , Agnelli J ((2015) ) Non-pharmacological approaches to alleviate distress in dementia care. Nurs Stand 30: , 38–44. |
[4] | Särkämö T , Laitinen S , Tervaniemi M , Numminen A , Kurki M , Rantanen P ((2012) ) Music, emotion, and dementia: Insight from neuroscientific and clinical research. Music Med 4: , 153–162. |
[5] | Raglio A , Bellandi D , Baiardi P , Gianotti M , Ubezio MC , Zanacchi E , Granieri E , Imbriani M , Stramba-Badiale M ((2015) ) Effect of active music therapy and individualized listening to music on dementia: A multicenter randomized controlled trial. J Am Geriatr Soc 63: , 1534–1539. |
[6] | Rossato-Bennett M ((2014) ) Alive Inside: A Story of Music and Memory, 78 min. |
[7] | Garrido S , Schubert E ((2015) ) Moody melodies: Do they cheer us up? A study of the effect of sad music on mood. Psychol Music 43: , 244–261. |
[8] | Garrido S , Schubert E ((2015) ) Music and people with tendencies to depression. Music Percept 32: , 313–321. |
[9] | Bunt L ((2013) ), The Handbook of Music Therapy, Routledge. |
[10] | Konno R , Kang HS , Makimoto K ((2014) ) A best-evidence review of intervention studies for minimizing resistance-to-care behaviours for older adults with dementia in nursing homes. J Adv Nurs 70: , 2167–2180. |
[11] | Petrovsky D , Cacchione PZ , George M ((2015) ) Review of the effect of music interventions on symptoms of anxiety and depression in older adults with dementia. Int Psychogeriatr 27: , 1661–1670. |
[12] | Elliott M , Gardner P ((2016) ) The role of music in the lives of older adults with dementia ageing in place: A scoping review. Dementia (London), doi: 10.1177-1471301216639424 |
[13] | Holmes C , Knights A , Dean C , Hodkinson S ((2006) ) Keep music live: Music and the alleviation of apathy in dementia subjects. Int Psychogeriatr 18: , 623–630. |
[14] | Caputo M , Monastero R , Mariani E , Santucci A , Mangialasche F , Camarda R , Senin U , Mecocci P ((2008) ) Neuropsychiatric symptoms in 921 elderly subjects with dementia: A comparison between vascualr and neurodegenerative types. Acta Psychiat Scand 117: , 455–464. |
[15] | Dixon-Woods M , Cavers D , Agarwal S , Annandale E , Arthur T , Harvey J , Hsu R , Katbamma S , Olsen R , Smith L , RIley R , Sutton A ((2006) ) Conducting a critical interpretive review of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol 6: . |
[16] | Harden A , Thomas J ((2010) ) Mixed methods and systematic reviews: Examples and emerging issues. In Sage Handbook of Mixed Methods in Social & Behavioral Research, Tashakkori A, Teddlie C, eds, SAGE, Los Angeles. |
[17] | Marshall M ((1996) ) Sampling for qualitative research. Fam Pract 13: , 522–525. |
[18] | McFerran K , Garrido S , Saarikallio S ((2016) ) A critical interpretive synthesis of the literature linking music and adolescent mental health. Youth Soc 48: , 521–538. |
[19] | Popay J , Roberts H , Sowden A , Petticrew M , Arai L , Rodgers M , Britten N , Roen K , Duffy S ((2006) ) Guidance on the conduct of narrative synthesis in systematic reviews: Final report. Swindon, ESRC Methods Programme |
[20] | Long AF , Godfrey M , Randall T , Brettle A , Grant MJ ((2002) ) HCPRDU evaluation tool for quantitative studies. University of Leeds, Nuffield Institute for Health, Leeds, UK. |
[21] | Guetin S , Porter F , Picot MC , Pommie C , Messaoudi M , Djabelkir L , Olsen AL , Cano MM , Lecourt E , Touchon J ((2009) ) Effect of music therapy on anxiety and depression in patients with Alzheimer’s type dementia: Randomised, controlled study. Dement Geriatr Cogn 28: , 36–46. |
[22] | Sakamoto M , Ando H , Tsutou A ((2013) ) Comparing the effects of different individualized music interventions for elderly individuals with severe dementia. Int Psychogeriatr 25: , 775–784. |
[23] | Särkämö T , Tervaniemi M , Laitinen S , Numminen A , Kurki M , Johnson JK , Rantanen P ((2014) ) Cognitive, emotional, and social benefits of regular musical activities in early dementia: Randomized controlled study. Gerontologist 54: , 634–650. |
[24] | Locke JM , Mudford OC ((2010) ) Using music to decrease disruptive vocalizations in a man with dementia. Behav Intervent 25: , 253–260. |
[25] | Park H , Specht J ((2009) ) Effect of individualized music on agitation in individuals with dementia who live at home. J Geront Nurs 35: , 47–55. |
[26] | Särkämö T , Laitinen S , Numminen A , Kurki M , Johnson JK , Rantanen P ((2016) ) Pattern of emotional benefits induced by regular singing and music listening in dementia. J Am Geriatr Soc 64: , 439–440. |
[27] | Gerdner LA ((2000) ) Evidence-based protocol: Individualized music intervention. In Series on evidence-based practice for older adults, Titler M, ed. University of Iowa, Iowa City: IA. |
[28] | Chang FY , Huang HC , Lin KC , Lin LC ((2010) ) The effect of a music programme during lunchtime on the problem behaviour of the older residents with dementia at an institution in Taiwan. J Clin Nurs 19: , 939–948. |
[29] | Ho SY , Lai HL , Jeng SY , Tang CW , Sung HC , Chen PW ((2011) ) The effects of researcher-composed music at mealtime on agitation in nursing home residents with dementia. Arch Psychiatr Nurs 25: , e49–e55. |
[30] | Li CH , Liu CK , Yang YH , Chou MC , Chen CH , Lai CL ((2015) ) Adjunct effect of music therapy on cognition in Alzheimer’s disease in Taiwan: A pilot study. Neuropsychiatr Dis Treat 11: , 291–296. |
[31] | Nair BK , Heim C , Krishnan C , D’Este C , Marley J , Attia J ((2011) ) The effect of Baroque music on behavioural disturbances in patients with dementia. Australas J Ageing 30: , 11–15. |
[32] | Dunn K , Riley-Doucet C ((2013) ) Comparative analysis of two musical genres within a multisensory environmental intervention. J Holist Nurs 31: , 62–70. |
[33] | Eggert J , Dye CJ , Vincent E , Parker V , Daily SB , Pham H , Watson AT , Summey H , Roy T ((2015) ) Effects of viewing a preferred nature image and hearing preferred music on engagement, agitation, and mental status in persons with dementia. SAGE Open Med 3: , 2050312115602579. |
[34] | Holmes C , Knights A , Dean C , Hodkinson S , Hopkins V ((2006) ) Keep music live: Music and the alleviation of apathy in dementia subjects. Int Psychogeriatr 18: , 623–630. |
[35] | Narme P , Clement S , Ehrle N , Schiaratura L , Vachez S , Courtaigne B , Munsch F , Samson S ((2014) ) Efficacy of musical interventions in dementia: Evidence from a randomized controlled trial. J Alzheimers Dis 38: , 359–369. |
[36] | Gill LM , Englert NC ((2013) ) A music intervention’s effect on falls in a dementia unit. J Nurse Pract 9: , 562–567. |
[37] | Gotell E , Brown S , Ekman SL ((2009) ) The influence of caregiver singing and background music on vocally expressed emotions and moods in dementia care: A qualitative analysis. Int J Nurs Stud 46: , 422–430. |
[38] | Guetin S , Portet F , Picot MC , Pommie C , Messaoudi M , Djabelkir L , Olsen AL , Cano MM , Lecourt E , Touchon J ((2009) ) Effect of music therapy on anxiety and depression in patients with Alzheimer’s type dementia: Andomised, controlled study. Dement Geriatr Cogn Disord 28: , 36–46. |
[39] | Ziv N , Granot A , Hal S , Dassa A , Halmov I ((2007) ) The effect of background stimulative music on behavior in Alzheimer’s patients. J Music Ther 44: , 329–343. |
[40] | Sung HC , Chang AM , Abbey J ((2006) ) The effects of preferred music on agitation of older people with dementia in Taiwan. Int J Geriatr Psychiatry 21: , 999–1000. |
[41] | Garland K , Beer E , Eppingstall B , O’Connor DW ((2007) ) A comparison of two treatments of agitated behaviour in nursing home redidents with dementia: Simulated family presence and preferred music. Am J Ger Psychiat 15: , 514–521. |
[42] | Hicks-Moore SL , Robinson BA ((2008) ) Favorite music and hand massage: Two interventions to decrease agitation in residents with dementia. Dementia 7: , 95–108. |
[43] | Sung HC , Chang AM , Lee WL ((2010) ) A preferred music listening intervention to reduce anxiety in older adults with dementia in nursing homes. J Clin Nurs 19: , 1056–1064. |
[44] | Park H ((2010) ) Effect of music on pain for home-dwelling persons with dementia. Pain Manag Nurs 11: , 141–147. |
[45] | Sarkamo T , Tervaniemi M , Laitinen S , Numminen A , Kurki M , Johnson JK , Rantanen P ((2014) ) Cognitive, emotional, and social benefits of regular musical activities in early dementia: Randomized controlled study. Gerontologist 54: , 634–650. |
[46] | Hanser SB , Butterfield-Whitcomb J , Kawata M , Collins BE ((2011) ) Home-based music strategies with individuals who have dementia and their family caregivers. J Music Ther 48: , 2–27. |
[47] | Raglio A , Bellandi D , Baiardi P , Gianotti M , Ubezio MC , Granieri E ((2013) ) Listening to music and active music therapy in behavioral disturbances in dementia: A crossover study. J Am Geriatr Soc 61: , 645–647. |
[48] | Fischer-Terworth C , Probst P ((2011) ) Evaluation of a TEACCH- and music therapy-based psychological intervention in mild to moderate dementia. GeroPsych (Bern) 24: , 93–101. |
[49] | Schall A , Haberstroh J , Pantel J ((2015) ) Time series analysis of individual music therapy in dementia. GeroPsych (Bern) 28: , 113–122. |
[50] | Clement S , Tonini A , Khatir F , Schiaratura L , Samson S ((2012) ) Short and longer term effects of musical intervention in severe Alzheimer’s disease. Music Percept 29: , 533–541. |
[51] | McDermott O , Crellin N , Ridder HM , Orrell M ((2012) ) Music therapy in dementia: A narrative synthesis systematic review. Int J Geriatr Psychiatry 28: , 781–794. |
[52] | Donegan K , Fox N , Black N , Livingston G , Sube, Burns A ((2017) ) Trends in diagnosis and treatment for people with dementia in the UK from 2005 to 2015: A longitudinal retrospective cohort study. Lancet Pub Health 2: , e149–e156. |
[53] | Cerejeira J , Lagarto L , Mukaetova-Ladinska EB ((2012) ) Behavioral and psychological symptoms of dementia. Front Neurol 3: , 73. |
[54] | Bonde LO ((2015) ) Health musicing - music therapy or music and health? A model, empirical examples and personal reflection. Music Arts Act 3: , 120–140. |



